- 1Department of Urology, The Second Affiliated Hospital of Zhejiang Chinese Medicine University, Hangzhou, Zhejiang, China
- 2Department of Urology, Zhejiang Hospital, Hangzhou, Zhejiang, China
- 3Department of Urology, The Third Affiliated Hospital of Wenzhou Medical University, Wenzhou, Zhejiang, China
Objective: To compare the efficacy of Retzius-sparing robot-assisted radical prostatectomy (RS-RARP) versus standard robot-assisted radical prostatectomy (S-RARP) in treating prostate cancer patients regarding urinary continence (UC) recovery, oncological control, and other complications.
Methods: An electronic search was performed on four databases with no restrictions on the language up to May 16th, 2024. The main outcomes were UC recovery positive, positive surgical margin (PSM), biochemical recurrence (BCR) and postoperative complications. Result robustness was enhanced based on the RoB and quality assessments.
Results: The final analysis included 3 randomized controlled trials, 2 prospective studies, and 4 retrospective studies. According to quantitative results, RS-RARP improved the UC recovery rates at catheter removal (OR=11.33, 95% CI=[1.29-99.69], P=0.03), at 1 month (OR=14.18, 95% CI=[1.34-150.44], P=0.03), 3 months (OR=3.64, 95% CI=[1.94-6.83], P<0.00001), 6 months (OR=3.18, 95% CI=[1.62-6.22], P=0.0007), but failed to present a better continence recovery rate at 12 months (OR=2.30, 95% CI=[0.77-6.85], P=0.14) postoperatively. The RS-RARP group presented higher overall PSM rates (OR=1.51, 95% CI=[1.15-1.98]) and PSM rates in ≥ pT3 tumors (OR=1.81, 95% CI=[1.18-2.77], P=0.006) versus the S-RARP group. Furthermore, the two groups did not present obviously different BCR rates (OR=0.58, 95% CI=[0.20-1.67], P=0.31), operating time (WMD=10.41 min, 95% CI=[-2.82-23.65], P=0.12), intraoperative estimated blood loss (WMD=-15.97 mL, 95% CI=[-41.53-9.58], P=0.22), serious postoperative complications (OR=1.04, 95% CI=[0.50-2.13], P=0.10).
Conclusions: Our meta-analysis revealed that although RS-RARP demonstrated accelerated urinary continence recovery, it showed a tendency toward higher PSM rates in patients with ≥pT3 tumors.
1 Introduction
An innovative surgical technique, named the Bocciardi technique, was first proposed by Galfano et al. in 2010, for robot-assisted radical prostatectomy (RARP) in which the prostate is approached posteriorly, together with an intact retzius space (1). Compared with the standard robot-assisted radical prostatectomy (S-RARP), an anterior surgical approach involving sequential entry into the Retzius space, incision of the endopelvic fascia, controlled division of the puboprostatic ligament, transection of the dorsal venous complex (DVC), and complete exposure of the prostate, the Retzius-sparing robot-assisted radical prostatectomy (RS-RARP) approach can preserve the endopelvic fascia, arcus tendinous, puboprostatic ligament, the detrusor apron, Santorini plexus, and deep dorsal vein plexus (2). Therefore, it facilitates earlier UC recovery and preserves erectile function, as evidenced in various randomized controlled trials (RCTs) and prospective studies (3–11). However, other studies found no benefit of the RS-RARP on longer-term UC recovery and potency recovery (12). Furthermore, its feature of preserving more anterior structures in the retzius space means a smaller workspace and fewer landmarks for surgeons. These factors may not only extend the surgeons’learning curve, but also results in larger positive surgical margins (PSM) (13, 14). PSM independently predicts the biochemical recurrence and primarily determines if salvage treatment is needed (15). Proper and early detection of biochemical recurrence rate (BCR) can timely guide the application of curative-intent salvage therapies. Therefore, the study aimed at comparing the performance of the two approaches in treating prostate cancer patients through a long-term follow-up from the perspectives of UC recovery and oncological control.
2 Materials and methods
The meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Two investigators identified relevant studies, screened and extracted the data as well as conducted validity assessment independently, and upon the emergence of any discrepancies in the data, a third reviewer would be invited to participate in the consultation.
2.1 Search strategy and selection criteria
The Pubmed, EMBASE, WoS and Cochrane Library were subjected to a systematic electronic literature search up to May 16th, 2024. The primary search strategy used the terms of: (((prostate) OR (prostatic)) AND ((((neoplasm) OR (cancer)) OR (carcinoma)) OR (malignancy))) AND ((((Retzius-sparing) OR (RARP)) OR (Retzius preservation)) OR (Bocciardi approach)) AND ((humans[Filter]) AND (all adult[Filter])).
To minimize the bias arising from the small number and sample size of RCTs, we included non-RCT studies in the meta-analysis. Consequently, the inclusion criteria were relaxed: (1) studies that enrolled adults with prostate cancers and (2) those that compared RS-RARP with S-RARP. Those found to be reviews, meta-analyses, replies, comments, case reports, conference reports, conference abstract, notes, book chapters, and non-comparative studies were excluded.
2.2 Risk-of-bias and study quality assessment
The risk of bias (RoB) among the identified RCTs and observational studies was determined by virtue of RoB 2.0 and ROBINS-I (16, 17). The RoB 2.0 comprises 5 domains, scored as “low”, “some concerns”, or “high”. In ROBINS-I, the RoB is scored as “low”, “moderate”, “serious”, or “critical”. All studies were rated by the Grades of Recommendation, Assessment, Development and Evaluation (GRADE), classified as “very low”, “low”, “moderate”, and “high” (18).
2.3 Data extraction and statistical analysis
The baseline characteristics extracted from each study included age, BMI, prostate size, pre-operative prostate-specific antigen, clinical stage, and pre-operative Gleason score. The oncological outcomes comprised the pathological stage (pT) and PSM, whereas functional outcomes included continence and potency recovery. We also recorded the perioperative operative time, EBL, and postoperative complication rates.
Statistical analysis relied on the Review Manager v5.3 software (Cochrane Collaboration, Oxford, UK). Presentation of continuous variables followed the mean ± standard deviation (SD) format, and that of categorical variables followed frequency and percentage format. If a continuous variable presentation followed the median and interquartile range (IQR) format, the numerical scales were employed to estimate data from such variables (19–22). The Weighted Mean Difference (WMD) with 95% CIs served as a summary measure for continuous data, and odds ratios (ORs) with 95% CIs were used for dichotomous data. A random-effect (RE) model explained the heterogeneity. Study heterogeneity was tested by calculating the P value and the I2 statistic, with a P value < 0.10 indicating high heterogeneity (23). P < 0.05 reported statistical significance.
3 Results
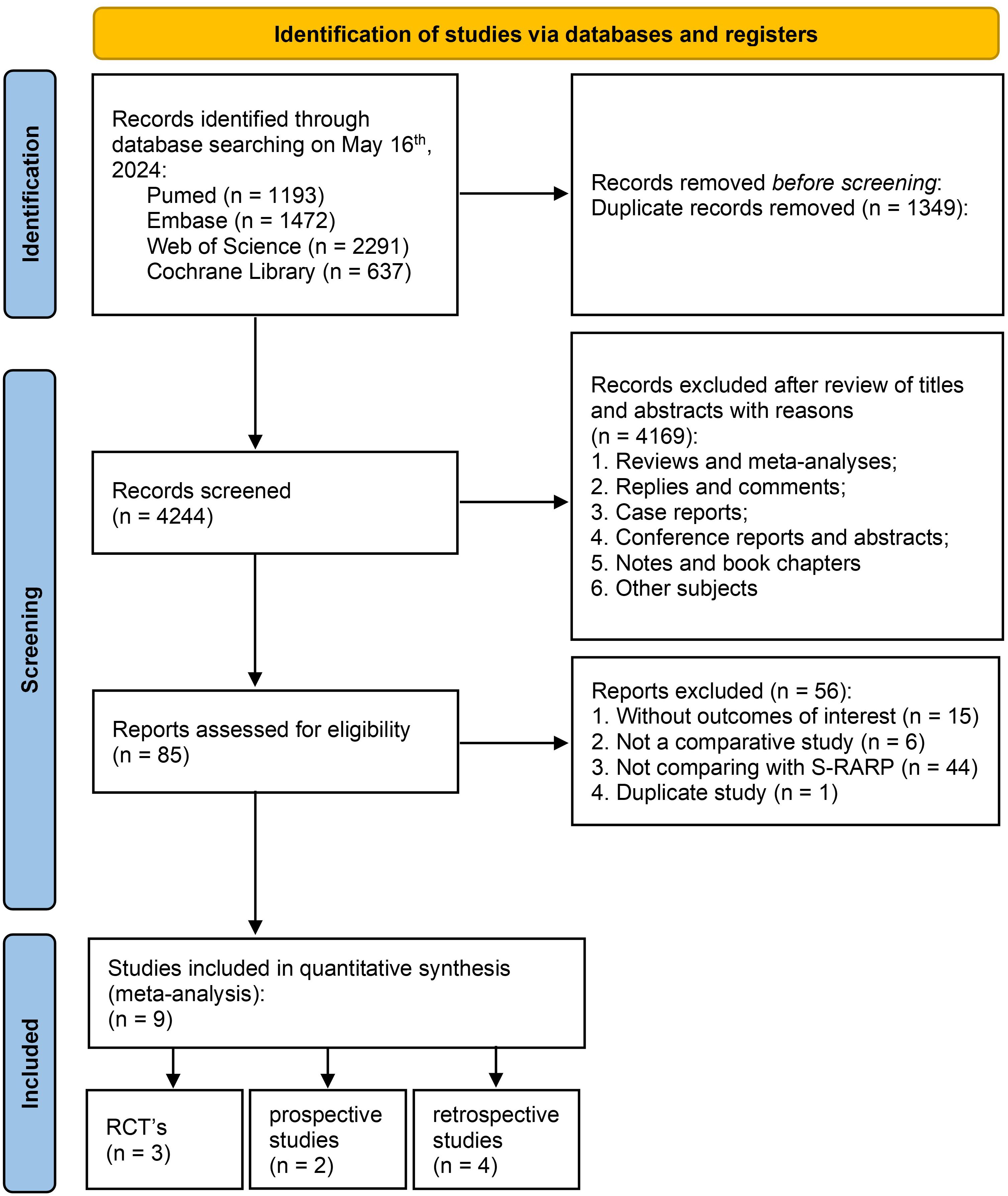
Nine relevant studies were identified from four electronic databases, including 3 RCTs, 2 prospective studies, and 4 retrospective studies. Figure 1 illustrates the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) flowchart regarding the search strategy. For duplicate studies reporting the same patient populations, the latest study was included.
3.1 Characteristics of included studies
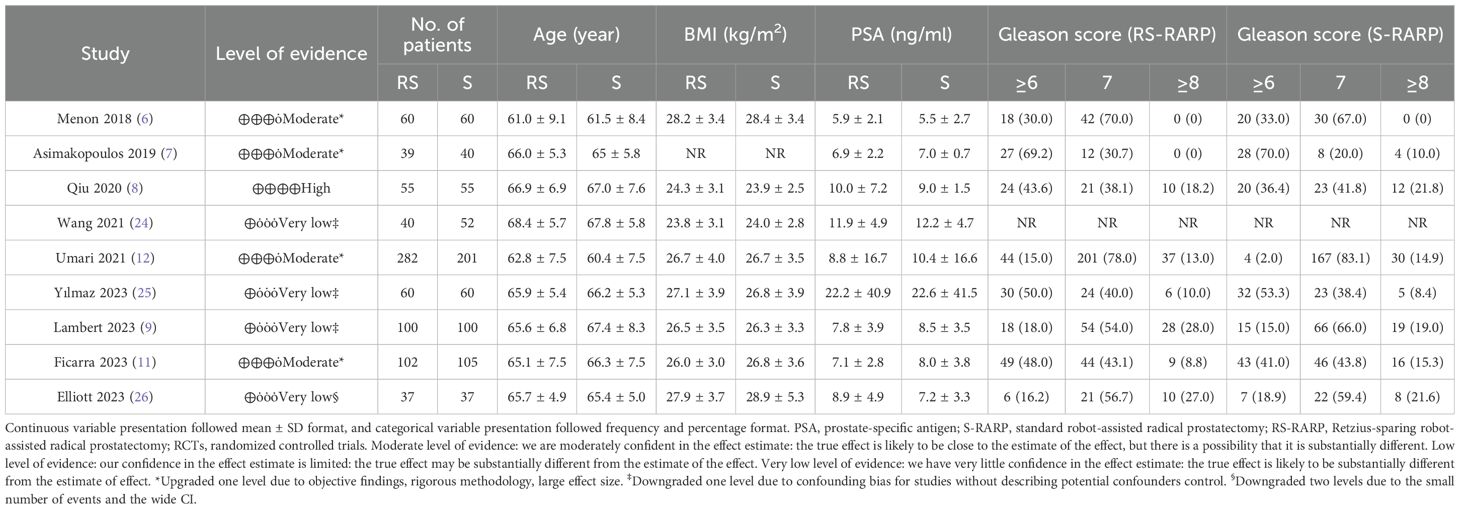
Based on the results of the RoB 2.0 test, 3 RCTs were considered to exhibit a high RoB (Figure 2a). The RoB results for 6 observational studies were assessed by ROBINS-I, and results are presented in Figure 2b. The 4 observational studies were considered to exhibit a high RoB, whereas another 2 observational studies showed a moderate RoB. Table 1 lists the level of evidence in all studies (6–9, 11, 12, 24–26). Overall, included studies involved 775 patients receiving RS-RARP and 775 patients receiving S-RARP.
3.2 Continence recovery
According to the strict continence definition (use of 0 pad each day), we found that the RS-RARP group showed a better cumulative continence recovery rate (CRR) at catheter removal (OR=11.33, 95% CI=[1.29-99.69], P=0.03, Figure 3a), 1 month (OR=14.18, 95% CI=[1.34-150.44], P=0.03, Figure 3b), 3 months (OR=3.64, 95% CI=[1.94-6.83], P<0.00001, Figure 3c), 6 months (OR=3.18, 95% CI=[1.62-6.22], P=0.0007, Figure 3d), but did not show a better CRR at 12 months (OR=2.30, 95% CI=[0.77-6.85], P=0.14, Figure 3e) postoperatively. However, when continence was defined by 0–1 pad per day, significant differences in 12-month continence recovery rates were found between the groups (OR=12.08, 95% CI=[1.59-91.72], P=0.02, Supplementary Figure S1).
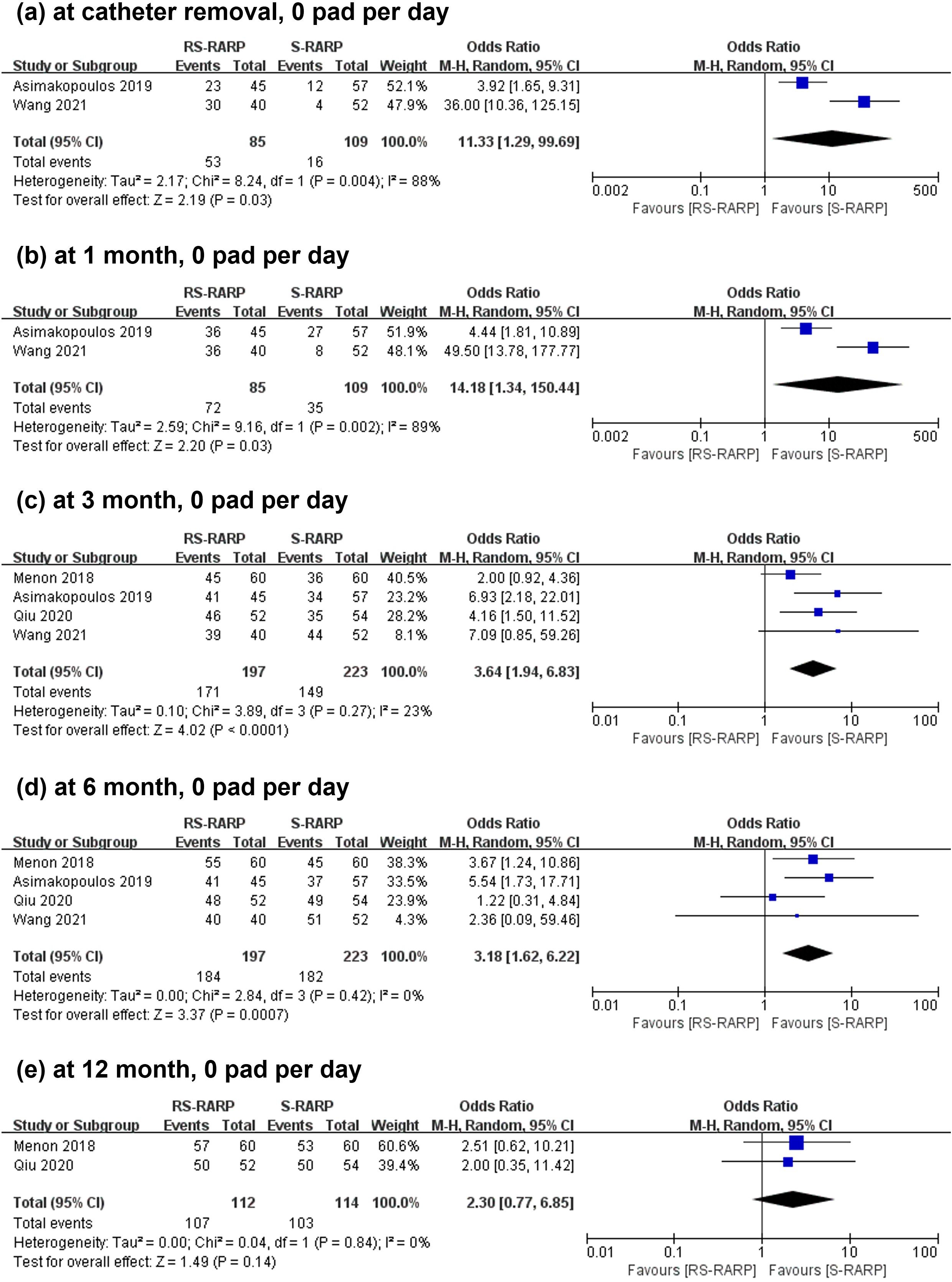
Figure 3. Forest plot showing the continence recovery rates post-operatively at catheter removal (a), 1 month (b), 3 months (c), 6 months (d), 12 months (e) between the RS-RARP group and the S-RARP group. M-H, Mantel-Haenszel.
3.3 PSMs and BCR
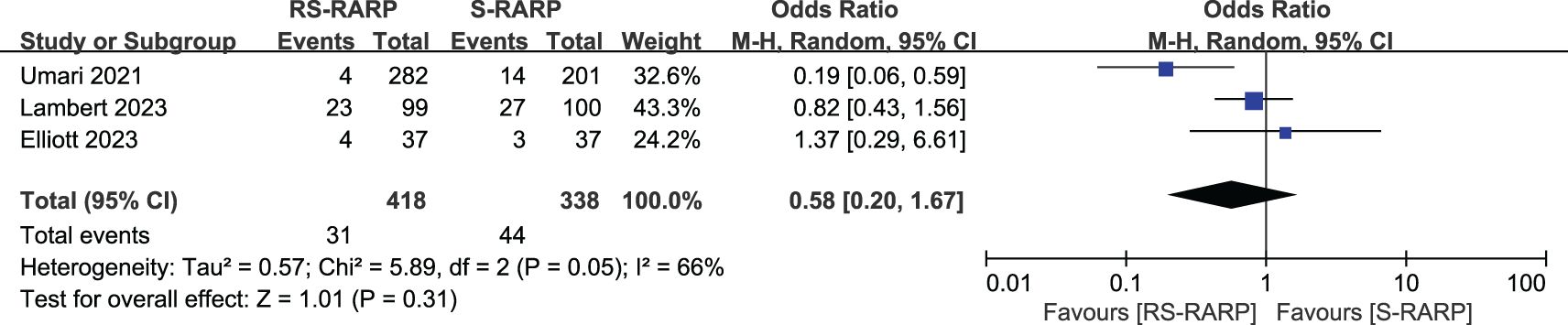
The RS-RARP group exhibited higher overall PSM rates (170 of 774 cases, 21.96%) versus the S-RARP group (115 of 710 cases, 16.20%) (OR=1.51, 95% CI=[1.15-1.98], P=0.003, Figure 4a). For < pT3 tumors, the two groups did not present obviously different PSM rates (OR=1.24, 95% CI=[0.77-1.98], P=0.37, Figure 4b). However, for≥ pT3 tumors, the RS-RARP group showed remarkably higher PSM rates versus the S-RARP group (OR=1.81, 95% CI=[1.18-2.77], P=0.006, Figure 4c). Furthermore, three studies reported the BCR rates at 1-year follow-up, and no significant difference in BCR rates was observed between the two groups (OR=0.58, 95% CI=[0.20-1.67], P=0.31, Figure 5).
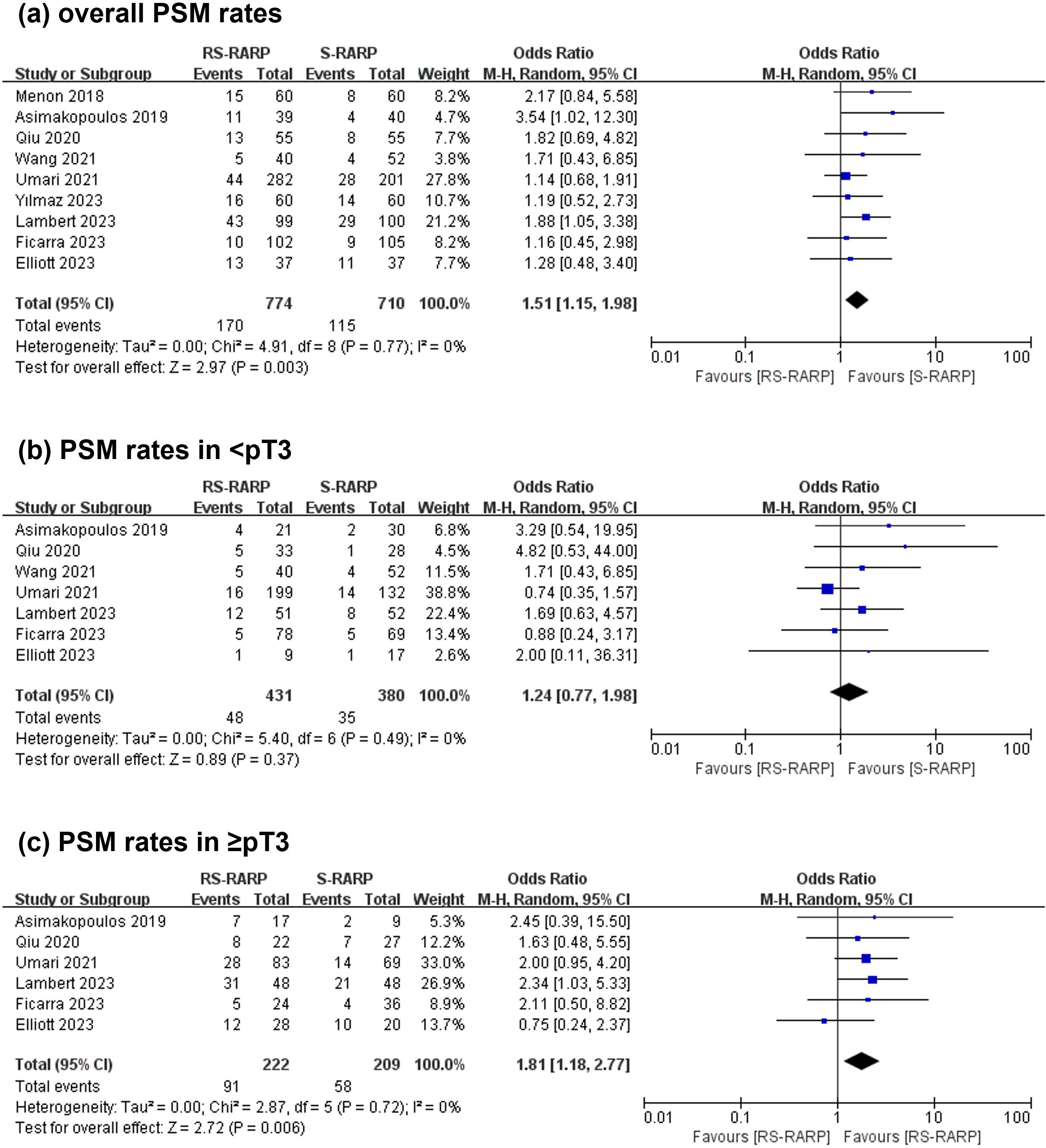
Figure 4. Forest plot showing the PSM rates post-surgery between the RS-RARP and the S-RARP groups. (a) Meta-analysis for the overall PSM rates. (b) Meta-analysis for the < pT3 PSM rates. (c) Meta-analysis for ≥ pT3 PSM rates.
3.4 Operating time, EBL and complications
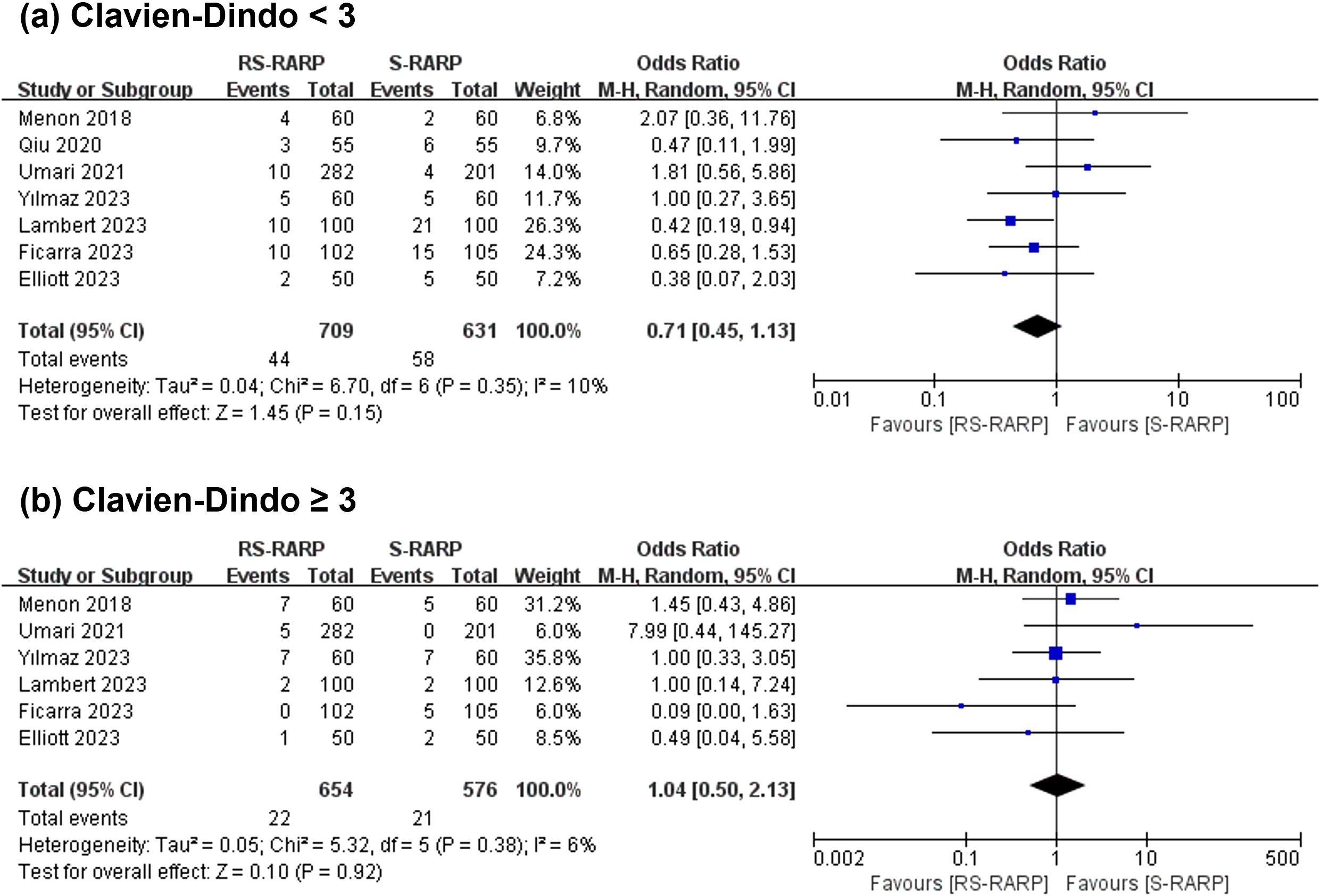
Seven studies reported operating time, and 6 studies provided data for the console time separately. The analysis revealed that the two groups did not present obviously different operating time (WMD=10.41 min, 95% CI=[-2.82-23.65], P=0.12, Figure 6a) and EBL intraoperatively (WMD=-15.97 mL, 95% CI=[-41.53-9.58], P=0.22, Figure 6b). In addition, 7 studies reported post-operative complications, graded by the standardized Clavien-Dindo classification. Notably, grade < 3 (OR=0.71, 95% CI=[0.45-1.13], P=0.15, Figure 7a) or grade ≥ 3 (OR=1.04, 95% CI=[0.50-2.13], P=0.10, Figure 7b) were considerably no different between the two groups.

Figure 6. Forest plot showing the intraoperative operating time (a) and estimated blood loss (b) between the two groups.
4 Discussion
As an innovative surgical technique, RS-RARP can protect the Retzius space, including the neurovascular bundle, which promotes early recovery of continence and erectile function. However, the long-term oncological efficacy and 12-month continence recovery for patients receiving this procedure are poorly understood (14, 27, 28). Therefore, the available evidence on the impact of RS-RARP on long-term continence recovery and oncological control was summarized by the systematic review. According to the result, the RS-RARP group exhibited a higher CRR versus the S-RARP group at catheter removal, 1 month, 3 months and 6 months postoperative with continence defined as 0 pad per day. However, the RS-RARP group also demonstrated a higher PSM rate versus the S-RARP group. Moreover, the two groups did not present significant different BCR rates, operation time, EBL, and complications.
Continence recovery is an important endpoint following radical prostatectomy, and can affect patients’ life quality. Most systematic reviews and meta-analyses found that due to its property of maintaining the normal pelvic anatomy, the RS-RARP had better early continence recovery versus the S-RARP technique. In our analysis, the RS-RARP group had higher continence rates after catheter removal and at 1, 3, and 6 months relative to the S-RARP group. However, whether continence recovery at 12 months is superior following the RS-RARP procedure remains to be determined. Several studies have demonstrated basically similar CRRs after surgery at 12 months between the two groups, while others found significant differences at 12 months between the two groups. In our analysis, when continence was defined as 0–1 safety pad per day, the RS-RARP group exhibited a higher CRR versus the S-RARP group (14, 27–30). However, the two groups showed a comparable CRR at 12 months with continence defined as 0 pad per day. We suggest that RS-RARP may improve the 1-year continence recovery, but this benefit is marginal.
Notably, surgical innovations for the management of solid cancer are evaluated based on their ability to provide sufficient oncological control. The PSM rate is considered a predictor for BCR, which indicates a poor oncological outcome for localized prostate cancer post-surgery. Conflicting evidence exists on PSM predictors. Several studies found PSM rates possibly because of the surgeons’ learning curve for the RS-RARP technique (15, 27). Several studies have identified a potential association between PSM occurrence in RS-RARP and the evolving competence of surgeons during the initial implementation phase of this robotic approach (31, 32). Nevertheless, its long-term therapeutic effects show variability depending on additional clinical parameters (15). In our analysis, the RS-RARP group exhibited dramatically higher overall PSM rates and PSM rates in localized ≥ pT3 tumors versus the S-RARP group. But the RS-RARP group did not exhibit a significant increase PSM rates in < pT3. It is likely that the difference between the two approaches may reflect by the higher proportion of pT3 disease in RS-RARP, as a higher tumor extension will result in increased risk of PSM (13, 33). Another factor to considered is the anatomic structure of the prostatic capsule. Xu J-N et al. found that anterior tumors are associated with higher PSM rates (34). However, in this analysis, the two groups showed comparable BCR rates, similar to findings from previous meta-analyses (14, 27, 28).
Moreover, the RS-RAPP group and the S-RAPR group did not present obviously different intraoperative conditions or postoperative complications. Regarding console time, one study by Lim et al. reported that the RS-RARP group had shorter console time versus the matched S-RARP group (3). Seven studies reported no differences in console time between the two groups, which may be due to the learning curve factor (35). Regarding postoperative complications, Lambert et al. found that the RS-RARP group had fewer complications relative to the S-RARP group, but no difference in Clavin-Dindo grade ≥ 3 between the two groups (9).
Despite abovementioned important findings, this study had several limitations. Firstly, although all evidence in the existing literature were included in our analysis, the number of RCTs and prospective studies was small. In addition, the sample size of included studies was relatively small. Secondly, even though we standardized the definitions and measurements of outcomes, methodological heterogeneity cannot be ruled out. Differences in surgeons’ learning curve of RS-RARP may also introduce bias. Thirdly, because different methods were used to assess erectile dysfunction without comparative date, the present study did not include sexual function recovery data.
Additionally, for the anterior approach several techniques (e.g. hood and sleeve technique) have been published describing the preservation of the anterior and anterolateral periprostatic structures (e.g. dorsovascular complex and pubovesical ligaments). RCTs comparing these techniques with RS-RARP are lacking, but a positive influence on the continence can be assumed.
In conclusion, RS-RARP achieves immediate continence recovery, but may be associated with an elevated risk of PSM rates in ≥ pT3 tumors. Reassuringly, the two approaches demonstrated comparable 1-year BCR rates. In future, the long-term oncological outcomes as well as the erectile function recovery of the two techniques should be confirmed in high-quality, multicenter RCTs.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
WG: Conceptualization, Data curation, Writing – original draft, Writing – review & editing, Investigation, Methodology, Visualization. JY: Supervision, Writing – review & editing. YC: Writing – review & editing, Investigation. DZ: Writing – review & editing, Investigation. YM: Supervision, Writing – original draft, Writing – review & editing, Conceptualization, Methodology, Project administration.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2025.1547687/full#supplementary-material
Supplementary Figure 1 | Forest plot illustrating continence recovery rates post-surgery at 12 months between the two groups when defined as 0–1 safety pad per day.
References
1. Galfano A, Ascione A, Grimaldi S, Petralia G, Strada E, Bocciardi AM. A new anatomic approach for robot-assisted laparoscopic prostatectomy: a feasibility study for completely intrafascial surgery. Eur Urol. (2010) 58:457–61. doi: 10.1016/j.eururo.2010.06.008
2. Galfano A, Secco S, Dell’Oglio P, Rha K, Eden C, Fransis K, et al. Retzius-sparing robot-assisted radical prostatectomy: early learning curve experience in three continents. BJU Int. (2021) 127:412–7. doi: 10.1111/bju.v127.4
3. Lim SK, Kim KH, Shin T-Y, Han WK, Chung BH, Hong SJ, et al. Retzius-sparing robot-assisted laparoscopic radical prostatectomy: combining the best of retropubic and perineal approaches. BJU Int. (2014) 114:236–44. doi: 10.1111/bju.2014.114.issue-2
4. Eden CG, Moschonas D, Soares R. Urinary continence four weeks following Retzius-sparing robotic radical prostatectomy: The UK experience. J Clin Urol. (2018) 11:15–20. doi: 10.1177/2051415817706635
5. Sayyid RK, Simpson WG, Lu C, Terris MK, Klaassen Z, Madi R, et al. Retzius-sparing robotic-assisted laparoscopic radical prostatectomy: A safe surgical technique with superior continence outcomes. J Endourol. (2017) 31:1244–50. doi: 10.1089/end.2017.0490
6. Menon M, Dalela D, Jamil M, Diaz M, Tallman C, Abdollah F, et al. Functional recovery, oncologic outcomes and postoperative complications after robot-assisted radical prostatectomy: an evidence-based analysis comparing the retzius sparing and standard approaches. J Urol. (2018) 199:1210–7. doi: 10.1016/j.juro.2017.11.115
7. Asimakopoulos AD, Topazio L, De Angelis M, Agrò EF, Pastore AL, Fuschi A, et al. Retzius-sparing versus standard robot-assisted radical prostatectomy: a prospective randomized comparison on immediate continence rates. Surg Endosc. (2019) 33:2187–96. doi: 10.1007/s00464-018-6499-z
8. Qiu X, Li Y, Chen M, Xu L, Guo S, Marra G, et al. Retzius-sparing robot-assisted radical prostatectomy improves early recovery of urinary continence: a randomized, controlled, single-blind trial with a 1-year follow-up. BJU Int. (2020) 126:633–40. doi: 10.1111/bju.v126.5
9. Lambert E, Allaeys C, Berquin C, De Visschere P, Verbeke S, Vanneste B, et al. Is it safe to switch from a standard anterior to retzius-sparing approach in robot-assisted radical prostatectomy? Curr Oncol. (2023) 30:3447–60. doi: 10.3390/curroncol30030261
10. Kadono Y, Nohara T, Kawaguchi S, Kadomoto S, Iwamoto H, Yaegashi H, et al. Postoperative functional and cancer control evaluation of conventional and Retzius-sparing robot-assisted radical prostatectomy: Comparison of selected cases by propensity score matching. Prostate. (2023) 83:773–80. doi: 10.1002/pros.24516
11. Ficarra V, Rossanese M, Gilante M, Foti M, Macchione L, Mucciardi G, et al. Retzius-sparing vs. standard robot-assisted radical prostatectomy for clinically localised prostate cancer: a comparative study. Prostate Cancer Prostatic Dis. (2023) 26:568–74. doi: 10.1038/s41391-022-00625-3
12. Umari P, Eden C, Cahill D, Rizzo M, Eden D, Sooriakumaran P. Retzius-sparing versus standard robot-assisted radical prostatectomy: A comparative prospective study of nearly 500 patients. J Urol. (2021) 205:780–90. doi: 10.1097/JU.0000000000001435
13. Stonier T, Simson N, Davis J, Challacombe B. Retzius-sparing robot-assisted radical prostatectomy (RS-RARP) vs standard RARP: it’s time for critical appraisal. BJU Int. (2019) 123:5–7. doi: 10.1111/bju.2019.123.issue-1
14. Barakat B, Othman H, Gauger U, Wolff I, Hadaschik B, Rehme C, et al. Retzius sparing radical prostatectomy versus robot-assisted radical prostatectomy: which technique is more beneficial for prostate cancer patients (MASTER study)? A systematic review and meta-analysis. Eur Urol Focus. (2022) 8:1060–71. doi: 10.1016/j.euf.2021.08.003
15. Yossepowitch O, Briganti A, Eastham JA, Epstein J, Graefen M, Montironi R, et al. Positive surgical margins after radical prostatectomy: a systematic review and contemporary update. Eur Urol. (2014) 65:303–13. doi: 10.1016/j.eururo.2013.07.039
16. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
17. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. (2016) 355:i4919. doi: 10.1136/bmj.i4919
18. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. (2011) 64:383–94. doi: 10.1016/j.jclinepi.2010.04.026
19. Shi J, Luo D, Wan X, Liu Y, Liu J, Bian Z, et al. Detecting the skewness of data from the five-number summary and its application in meta-analysis. Stat Methods Med Res. (2023) 32:1338–60. doi: 10.1177/09622802231172043
20. Shi J, Luo D, Weng H, Zeng X-T, Lin L, Chu H, et al. Optimally estimating the sample standard deviation from the five-number summary. Res Synth Methods. (2020) 11:641–54. doi: 10.1002/jrsm.v11.5
21. Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. (2018) 27:1785–805. doi: 10.1177/0962280216669183
22. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. (2014) 14:135. doi: 10.1186/1471-2288-14-135
23. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
24. Wang MC, Zhang YY, Yu SC, Zhu SB, Xu L, Ni KX, et al. An evidence-based analysis comparing two approaches of robot-assisted laparoscopic radical prostatectomy: the standard technique and Retzius-sparing technique. Zhonghua Yi Xue Za Zhi. (2021) 101:1083–7. doi: 10.3760/cma.j.cn112137-20200902-02546
25. Yılmaz K, Ölçücü MT, Özsoy Ç, Aksaray EE, Kılıç Ş, Ateş M, et al. Comparison of early urinary continence, oncological outcomes, and postoperative complications in retzius-sparing and standard approach robot-assisted radical prostatectomy. J Laparoendosc Adv Surg Tech A. (2023) 33:150–4. doi: 10.1089/lap.2022.0409
26. Elliott N, Pahouja G, Felice M, Capoccia E, Patel PM, Blanco Martinez E, et al. Transition from standard robotic prostatectomy to Retzius-sparing prostatectomy: feasibility and early outcomes. J Robot Surg. (2023) 17:2035–40. doi: 10.1007/s11701-023-01596-w
27. Checcucci E, Veccia A, Fiori C, Amparore D, Manfredi M, Di Dio M, et al. Retzius-sparing robot-assisted radical prostatectomy vs the standard approach: a systematic review and analysis of comparative outcomes. BJU Int. (2020) 125:8–16. doi: 10.1111/bju.v125.1
28. Tai T-E, Wu C-C, Kang Y-N, Wu J-C. Effects of Retzius sparing on robot-assisted laparoscopic prostatectomy: a systematic review with meta-analysis. Surg Endosc. (2020) 34:4020–9. doi: 10.1007/s00464-019-07190-2
29. Rosenberg JE, Jung JH, Lee H, Lee S, Bakker CJ, Dahm P, et al. Posterior musculofascial reconstruction in robotic-assisted laparoscopic prostatectomy for the treatment of clinically localized prostate cancer. Cochrane Database Syst Rev. (2021) 8:CD013677. doi: 10.1002/14651858.CD013677.pub2
30. Ferretti S, Dell'Oglio P, Ciavarella D, Galfano A, Schips L, Marchioni M, et al. Retzius-sparing robotic-assisted prostatectomy: technical challenges for surgeons and key prospective refinements. Res Rep Urol. (2023) 15:95–105. doi: 10.2147/RRU.S372803
31. Lee J, Kim HY, Goh HJ, Heo JE, Almujalhem A, Alqahtani AA, et al. Retzius sparing robot-assisted radical prostatectomy conveys early regain of continence over conventional robot-assisted radical prostatectomy: A propensity score matched analysis of 1,863 patients. J Urol. (2020) 203:137–44. doi: 10.1097/JU.0000000000000461
32. Egan J, Marhamati S, Carvalho FLF, Davis M, O'Neill J, Lee H, et al. Retzius-sparing robot-assisted radical prostatectomy leads to durable improvement in urinary function and quality of life versus standard robot-assisted radical prostatectomy without compromise on oncologic efficacy: single-surgeon series and step-by-step guide. Eur Urol. (2021) 79:839–57. doi: 10.1016/j.eururo.2020.05.010
33. Dalela D, Jeong W, Prasad M-A, Sood A, Abdollah F, Diaz M, et al. A pragmatic randomized controlled trial examining the impact of the retzius-sparing approach on early urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol. (2017) 72:677–85. doi: 10.1016/j.eururo.2017.04.029
34. Xu J-N, Xu Z-Y, Yin H-M. Comparison of retzius-sparing robot-assisted radical prostatectomy vs. Conventional robot-assisted radical prostatectomy: an up-to-date meta-analysis. Front Surg. (2021) 8:738421. doi: 10.3389/fsurg.2021.738421
35. Galfano A, Di Trapani D, Sozzi F, Strada E, Petralia G, Bramerio M, et al. Beyond the learning curve of the Retzius-sparing approach for robot-assisted laparoscopic radical prostatectomy: oncologic and functional results of the first 200 patients with ≥ 1 year of follow-up. Eur Urol. (2013) 64:974–80. doi: 10.1016/j.eururo.2013.06.046
Keywords: radical prostatectomy, Retzius-sparing, robot-assisted, prostate cancer, urinary continence
Citation: Gong W, Yan J, Cui Y, Zhang D and Ma Y (2025) Comparison of efficacy of Retzius-sparing radical prostatectomy versus standard radical prostatectomy in the treatment of prostate cancer: a systematic review and meta-analysis. Front. Oncol. 15:1547687. doi: 10.3389/fonc.2025.1547687
Received: 18 December 2024; Accepted: 18 April 2025;
Published: 14 May 2025.
Edited by:
Alexander Winter, Carl Von Ossietzky University Oldenburg, GermanyReviewed by:
Dimitrios Moschonas, Royal Surrey County Hospital, United KingdomJorn H. Witt, Urokompetenz - Die Klinik für Urologie, Germany
Copyright © 2025 Gong, Yan, Cui, Zhang and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yinfeng Ma, eWluZmVuZ19tYUAxNjMuY29t
 Weilun Gong
Weilun Gong Junfeng Yan2
Junfeng Yan2 Duojie Zhang
Duojie Zhang Yinfeng Ma
Yinfeng Ma