- 1Department of Global Pediatric Medicine, St. Jude Children’s Research Hospital, Memphis, TN, United States
- 2Department of Oncology, St. Jude Children’s Research Hospital, Memphis, TN, United States
- 3Department of Pediatric Oncology, Indus Hospital and Health Network, Karachi, Pakistan
- 4Pediatric Hematology Oncology Service, District Head Quarter Hospital (DHQ) Badin/Indus Hospital and Health Network, Badin, Pakistan
- 5Pediatric Oncology Unit, Sheikh Zayed Hospital/Indus Hospital and Health Network, Quetta, Pakistan
- 6Children Cancer Centre of Child Aid Association, National Institute of Child Health, Karachi, Pakistan
- 7Department of Oncology/Section of Pediatric Oncology, Aga Khan University Medical College, Karachi, Pakistan
- 8Paediatric Haematology Oncology Unit, University of Child Health Sciences, The Children’s Hospital, Lahore, Pakistan
- 9Department of Pediatric Oncology, Shaukat Khanum Memorial Cancer Hospital and Research Center, Lahore, Pakistan
- 10Department of Pediatric Oncology, Combined Military Hospital, Rawalpindi, Pakistan
- 11Department of Pediatric Medicine/Pediatric Oncology Unit, Pakistan Institute of Medical Sciences, Islamabad, Pakistan
- 12Department of Pediatric Oncology, Children’s Hospital and Institute of Child Health, Multan, Pakistan
- 13Department of Pediatric Medicine, King Edward Medical University, Lahore, Pakistan
- 14Department of Hematology Oncology, Children’s Hospital and Institute of Child Health, Faisalabad, Pakistan
- 15Department of Pediatrics, Bahawal Victoria Hospital, Bahawalpur, Pakistan
- 16Department of Pediatrics, Lahore General Hospital, Lahore, Pakistan
- 17Department of Pediatric Medicine, Mother and Child Hospital, Nawabshah, Pakistan
- 18Department of Pediatrics, Dr. Ruth K. M. Pfau Civil Hospital, Karachi, Pakistan
Task sharing is a pragmatic response to the growing shortage of pediatric oncologists globally, especially in low- and middle-income countries (LMICs). However, there have been limited evaluations of how task sharing has been implemented. In this study, we sought to determine the roles and responsibilities of task-sharing physicians (TSPs) in one LMIC, Pakistan. A multicenter cross-sectional study was conducted across 16 hospitals with secondary- to quaternary-level pediatric oncology facilities. An online survey was used to determine task-sharing models, the responsibilities of TSPs, and the level of supervision. Pediatric oncologists were present at 13 of the 16 centers, with a median of 2 pediatric oncologists per center. We found that TSPs included tiers of medical officers/general physicians and pediatricians. They provided inpatient, outpatient, overnight and emergency room coverage. TSPs could participate in defining cancer diagnosis and risk-stratification (n = 9; 56%), selecting initial chemotherapy plans for patients with newly diagnosed cancer (n = 6; 38%) and modifying chemotherapy on the basis of toxicities (n = 6; 38%) under supervision of a pediatric oncologist. In addition, TSPs could write intravenous chemotherapy orders (n = 10; 63%) and prescribe oral chemotherapy (n = 10; 63%). Furthermore, they could independently perform procedures, such as lumbar punctures (n = 15; 94%), intrathecal chemotherapy administration (n = 11; 69%), and bone marrow aspirates and biopsies (n = 11; 69%). TSPs are critical in the pediatric oncology workforce with responsibilities across the pediatric cancer care continuum.
Introduction
The overall survival rate for childhood cancer has exceeded 80% in high-income countries (HICs). However, this drops to around 30% in low- and middle-income countries (LMICs), where nearly 90% of children with cancer live (1, 2) and where health systems are not adequately equipped for the complexities of cancer care (3–5). A global shortage in human resources for health reduces access to quality care for the growing burden of childhood cancer (1, 2, 6). Although graduate medical education programs in pediatric oncology are of extreme value, they continue to be scarce or absent in many LMICs (7). Thus, in a system where the care of children with cancer is reliant on only pediatric oncologists to provide care for children with cancer, deficiencies will exist.
Task sharing is the process whereby care responsibilities are shared between specialists and non-specialists, under the oversight of specialists (8). Task sharing has been employed as a pragmatic response to health workforce shortages in different regions and for diverse diseases (9–16). However, how task sharing is being implemented in pediatric oncology has not been comprehensively assessed.
Pakistan is the 5th most populous country in the world, with an estimated population of 241 million, 86 million (36%) of whom are younger than 14 years of age (17). Due to the lack of a national pediatric cancer registry, the exact incidence of pediatric cancer is not known. However, it is estimated that 8000-12000 new cases occur every year (18), though anecdotally less than 5000 are being diagnosed. There are currently 55 pediatric oncologists in the country; the ratio of new diagnoses to pediatric oncologists is thus much higher than the recommended number of 50 patients per specialist for LMICs (6, 19). Due to the lack of specialists in many centers, the responsibilities of pediatric oncologists are being assumed by physicians who lack dedicated training in pediatric cancer care.
In this study, we sought to determine the task-sharing models being used in pediatric oncology units in centers across Pakistan and the roles and responsibilities assigned to non-oncology trained physicians in these units.
Materials and methods
Context
Pakistan is administratively divided into four provinces, a federal capital territory, and two disputed territories. Pediatric cancer care is limited to a few centers across the country that have marked variability in their pediatric oncology infrastructure (20). In this study, we included all sixteen centers in Pakistan that had dedicated pediatric oncology units. We did not include centers that were seeing patients for only specific services such as radiation or surgery, and private hospitals that were sporadically seeing small numbers of children with cancer. Eight of the centers in our study were hospitals in central cities with established pediatric oncology teams, while the rest were smaller or newer set-ups, primarily in peripheral cities (Supplementary Figure S1). This study was part of an ongoing international collaboration for capacity building through workforce training between St. Jude Children’s Research Hospital (SJCRH) and Pakistan, where training opportunities will be created based on this and other assessments.
Study design and participants
A cross-sectional survey with 36 independent items was designed to determine site-specific models of task sharing (Supplementary File). Survey items were initially developed by the first authors (SKH and MRR) and a senior author (DCM), and iteratively revised by the research team. The survey was piloted at 2 institutions and modified before broader use for the centers in Pakistan. The survey included areas of cancer care infrastructure, including the type of hospital, volume of patients, and number of beds, the structure of the pediatric oncology physician workforce, including which physicians were charged with a modified scope of practice, the specific tasks and responsibilities of task-sharing physicians (TSPs), and the level of supervision. Questions about task sharing pertained to areas of clinical coverage, involvement in diagnostic evaluation and chemotherapy writing/prescribing, and expected decision-making knowledge and procedural skills. The survey was created by using Qualtrics (Provo, Utah) and electronically distributed to the department heads of pediatric oncology or pediatric units, as applicable. It was completed between June 2022 and March 2023.
All participants provided consent to participate in the study. The study was approved by the institutional review board at St. Jude Children’s Research Hospital (SJCRH), USA.
Analyses
Survey responses were included if at least 75% of the items were completed. Descriptive statistics were used to analyze all items. Because of the limited sample size, comparative tests were not conducted, as the primary objective was to provide a broad analysis of task sharing in Pakistan.
Results
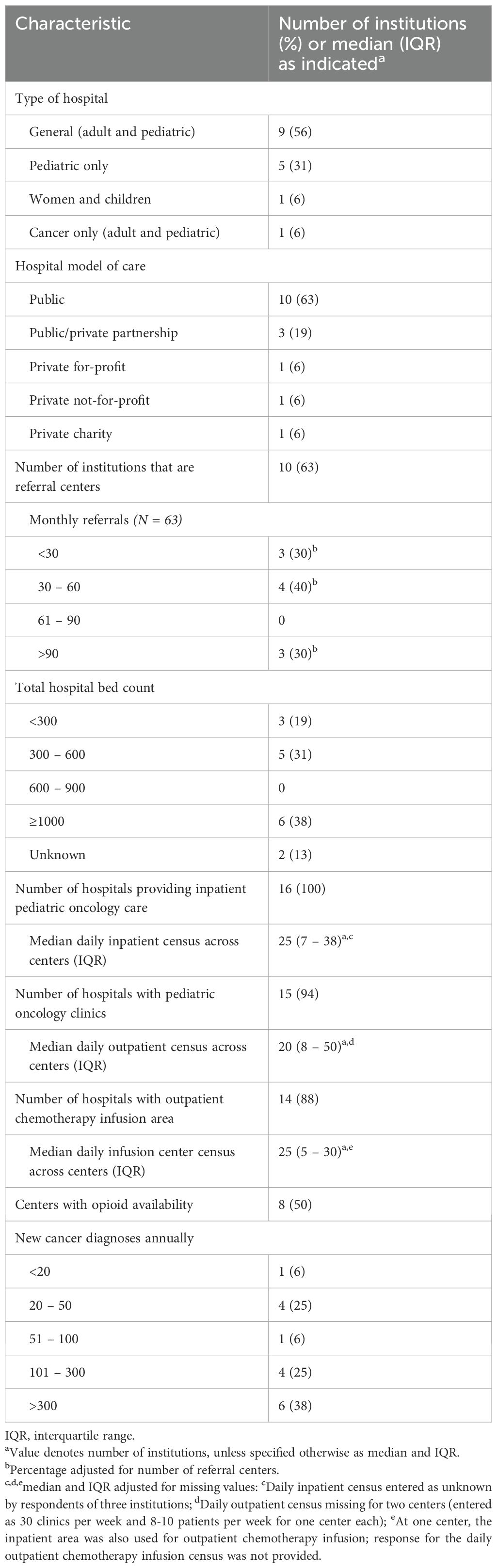
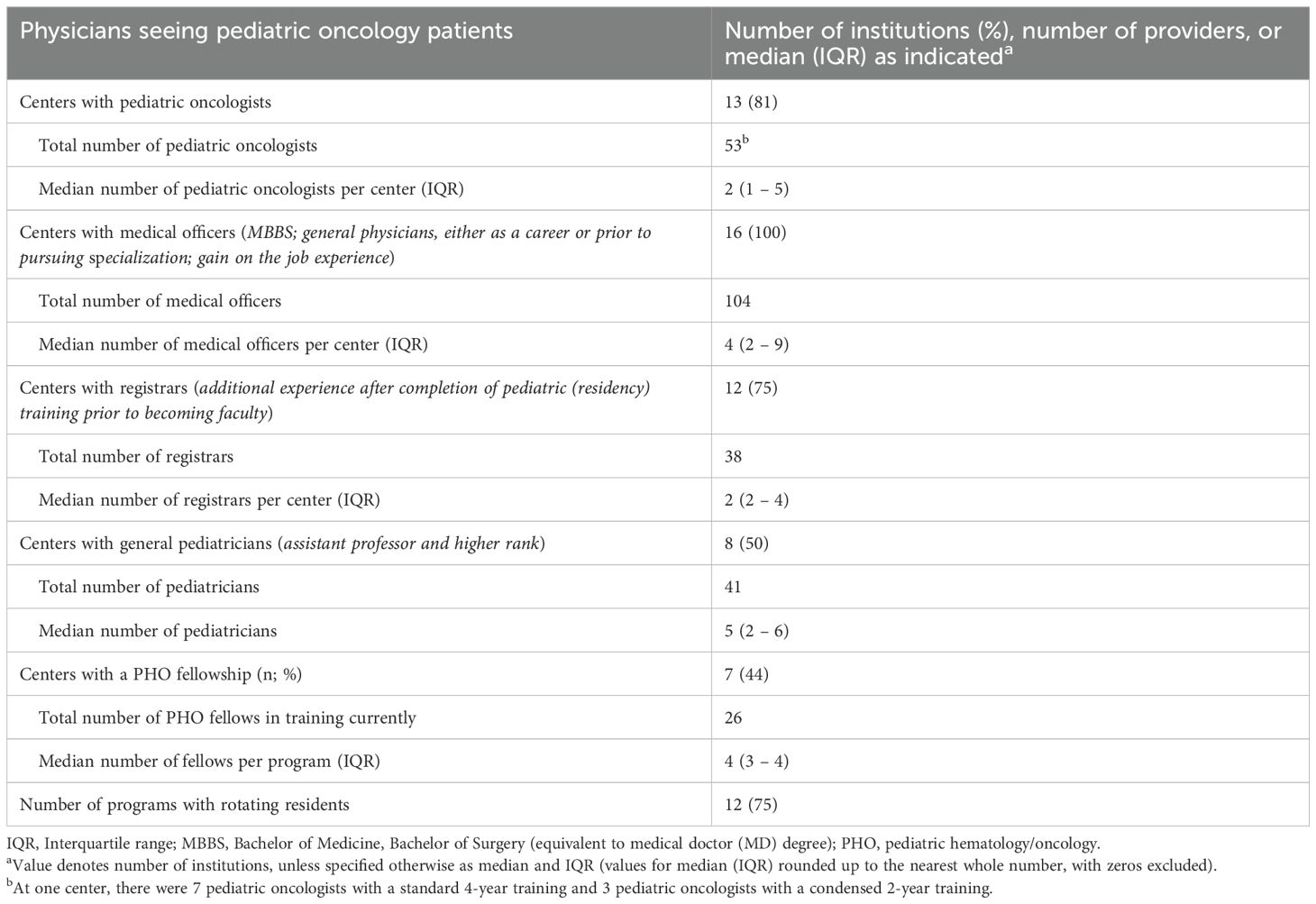
Pediatric oncology workforce infrastructure
The centers in our study included public and private hospitals with secondary- to quaternary-level pediatric oncology facilities (6). The hospitals varied in size, both in terms of the number of overall beds (195 to 1900) and the number of new pediatric cancer cases per year (n<20 to n>300). All had inpatient pediatric oncology care, and all except one had outpatient clinics. Fifteen of the 16 hospitals were able to administer outpatient chemotherapy infusions; at the hospital without outpatient clinics, inpatient beds were used for outpatient/day chemotherapy infusions (Table 1). Pediatric oncologists were present at 13 of the 16 centers, with a median of 2 pediatric oncologists per center (interquartile range [IQR] of 1 to 4). Seven centers had pediatric hematology-oncology fellowship programs with 3-5 fellows per program (Table 2). Twelve centers had rotating residents helping with coverage of pediatric oncology patients as well (Supplementary Table S1).
Task-sharing practices in pediatric oncology units
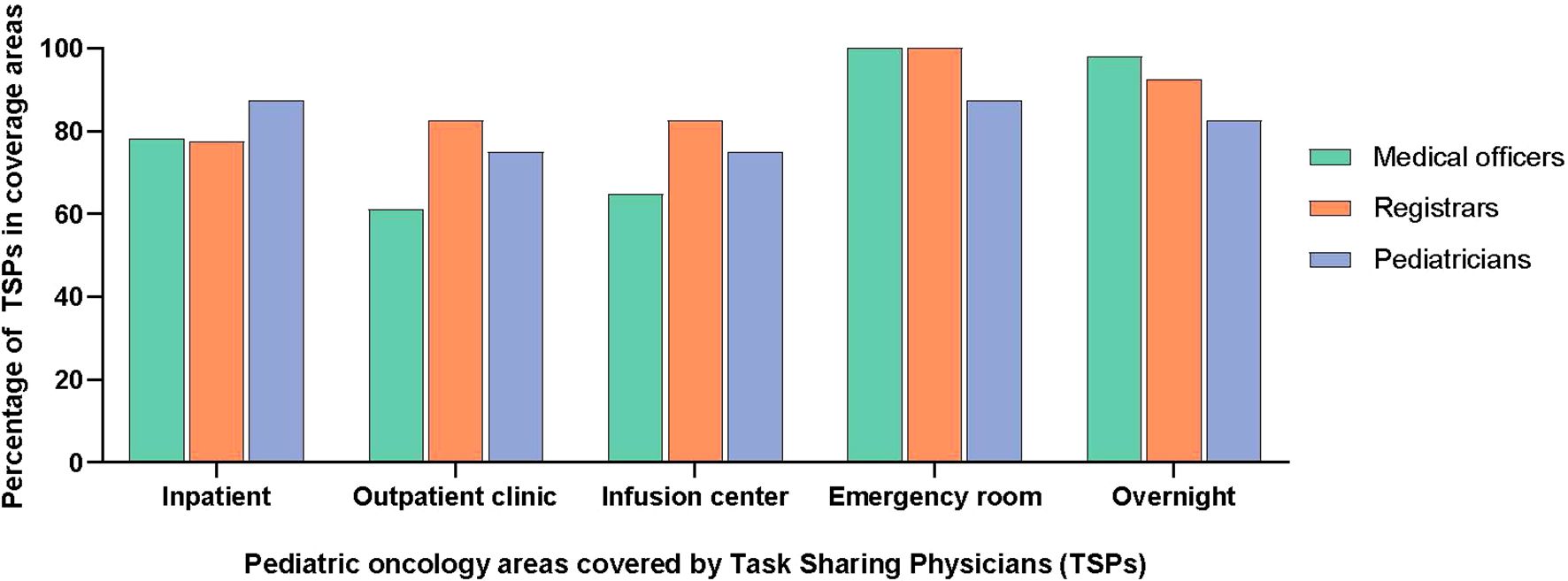
Of the non-specialist physicians engaged in pediatric oncology task sharing, medical officers (general physicians) were the most common and were present in all centers, followed by pediatricians. An outline of the physician training model in Pakistan is given in Supplementary Figure S2. The TSPs did not have any formal training in pediatric oncology but some centers provided on-the-job “orientation” such as overview of chemotherapy, treatment protocols and supportive care. In terms of clinical coverage, TSPs were managing patients in the inpatient units (n = 13; 81%) and in outpatient clinics/chemotherapy infusion areas (n = 12; 75%). They provided overnight coverage (n = 15; 94%) and triaged patients presenting to the emergency room as well (n = 16; 100%). The details of coverage, roles, and responsibilities of TSPs are included in Figures 1, 2.
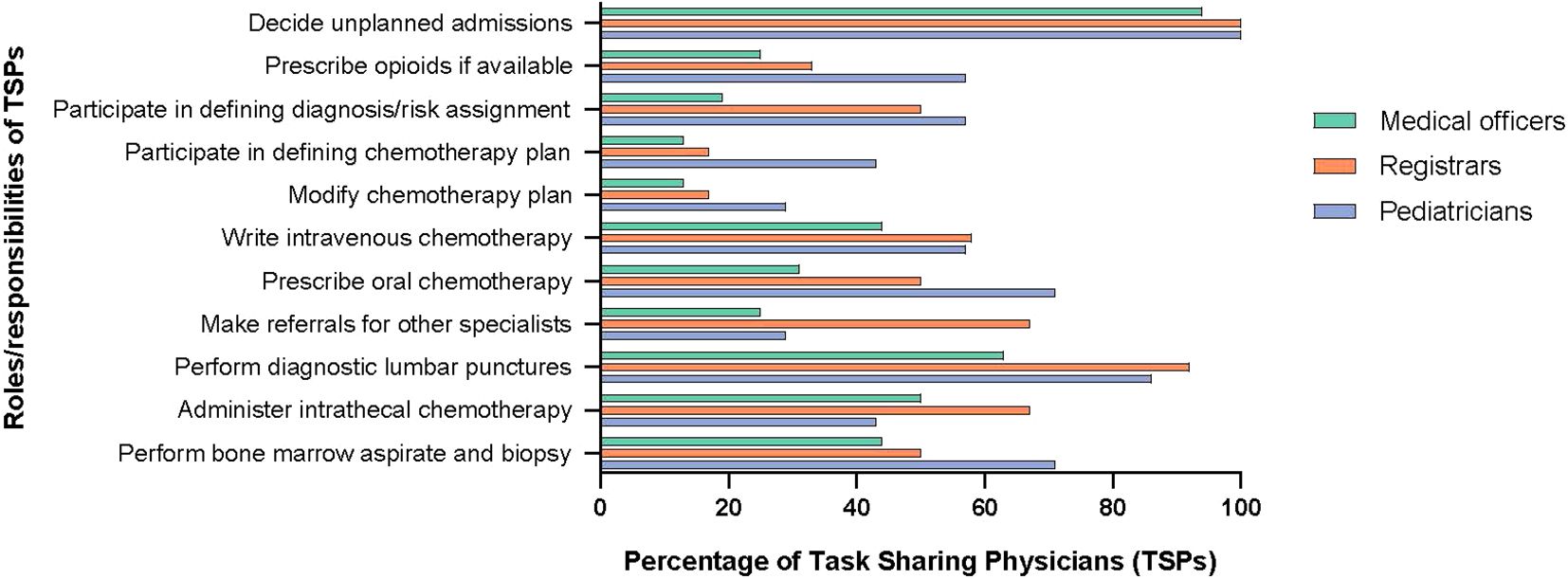
In terms of the scope of work, TSPs decided on unplanned admissions, such as those for febrile neutropenia, at all hospitals. At several hospitals, they could participate in defining cancer diagnosis and risk-stratification (n = 9; 56%), selecting initial chemotherapy plans for patients with newly diagnosed cancer (n = 6; 38%) and modifying chemotherapy on the basis of toxicities (n = 6; 38%) under supervision of a pediatric oncologist. In addition, TSPs could write intravenous chemotherapy orders (n = 10; 63%) and prescribe oral chemotherapy (n = 10; 63%). Furthermore, they could independently perform common procedures in pediatric oncology, such as lumbar punctures (n = 15; 94%), intrathecal chemotherapy administration (n = 11; 69%), and bone marrow aspirates and biopsies (n = 11; 69%). At five centers (31%), TSPs were also involved in the preparation and administration of intravenous chemotherapy.
In the inpatient and outpatient setting, patients seen by TSPs were discussed with a pediatric oncologist at most centers (n = 12; 75%), however, direct examination of every patient by a pediatric oncologist occurred at fewer centers (n = 6; 38%). Among peripheral hospitals that were staffed by a TSP without a pediatric oncologist on site, new patients were referred to the hub center. Subsequently, communication about other patients with pediatric oncologists was done through telemedicine to provide support for decision making (Supplementary Table S2).
Discussion
Although anecdotal reports on task sharing exist in pediatric oncology, the different strategies used have not been formally evaluated and reported. In this study, we have comprehensively described the roles and tasks assigned to non-specialists caring for children with cancer in an LMIC, Pakistan. TSPs are engaged in all hospital settings where pediatric cancer patients are cared for and participate in the key elements of the cancer care continuum.
The presented data includes institutions that vary in terms of the type of hospital, pediatric oncology infrastructure, and trained pediatric oncologists, as well as the volume of patients with pediatric cancer. In Pakistan, TSPs contributed to pediatric oncology coverage across all areas of the hospital and were expected to possess a variety of decision-making and procedural skills necessary for the comprehensive care of a child with cancer. This is consistent with the description of tasks distribution in adult oncology and plans to use non-oncologists as primary oncology providers in some settings (11, 15, 21).
Medical officers were the most common TSPs in our study. They are general physicians and have often gained several years of on-the-job experience. Although they have no formal training in oncology, they were considered instrumental by pediatric oncologists in running inpatient and outpatient services, where they were providing direct patient care and doing the bulk of medical record charting, including updating chemotherapy treatment roadmaps. Notably, initial diagnosis, risk-stratification, and defining a treatment plan are arguably the most complex tasks of pediatric oncology in which TSPs were participating. In most instances here, these responsibilities were directly overseen by pediatric oncologists. This dynamic optimizes the time of pediatric oncologists, consistent with the very nature of task sharing (12, 13). Nonetheless, collection of prospective clinical outcomes and patient satisfaction evaluations would be needed to confirm that the quality of provided care is not negatively impacted by TSPs.
In addition to addressing the problem of limited numbers of trained specialists, TSPs become available to institutions in a more cost-effective way due to their salaries being lower than those of consultants. We did not obtain data on cost savings in our survey, however, anecdotally, the salary of a medical officer can be ten times lower than that of a consultant in Pakistan. Cost saving through task shifting or sharing has been reported for other diseases in LMICs (22, 23). Additional studies evaluating the cost effectiveness of task sharing in pediatric cancer units are needed.
To optimize the use of task sharing, professionals must have the necessary competencies to provide quality care for children with cancer. To facilitate this, an effective course based on a structured and systematic design, starting with a targeted needs assessment, is one key element. Our findings contribute to the targeted needs assessment for a course that is being designed for TSPs that will cover the most relevant elements necessary for working with pediatric oncology patients. We are following the 6-step approach described by Kern et al., which is a systematic method that links curriculum development to health care needs and competencies required of the target audience (24). The authors have previously implemented a course using this approach with success (25).
Our study has several limitations. First, our findings reflect task-sharing practices in one LMIC, limiting broader generalizability of our results to other countries. Nonetheless, the varied characteristics of the institutions included in our study could mitigate this limitation. Second, the validity of the assessment tools can be disputed because a preexisting, validated assessment does not exist, and the surveys used were created de novo. To mitigate the risk of poor validity and reliability of data, the surveys were created by a pediatric oncologist, reviewed by content experts, and piloted at 2 sites that were not included in the final dataset.
In conclusion, our findings illustrate that TSPs are responsible for many essential steps in the pediatric cancer care continuum, spanning from initial diagnosis and risk stratification to the prescription of chemotherapy. Tiered training initiatives are being planned to support this critical workforce in their roles, which we anticipate will be applicable in other limited-resource settings as well. Future studies will focus on the impact of these initiatives.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author contributions
SKH: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. MRR: Conceptualization, Investigation, Methodology, Resources, Supervision, Writing – review & editing. MA: Investigation, Writing – review & editing. GQ: Investigation, Writing – review & editing. UI: Investigation, Writing – review & editing. ZF: Investigation, Writing – review & editing. AlA: Investigation, Writing – review & editing. HS: Investigation, Writing – review & editing. TG: Investigation, Writing – review & editing. NY: Investigation, Writing – review & editing. ZR: Investigation, Writing – review & editing. MH: Investigation, Writing – review & editing. MFR: Investigation, Writing – review & editing. AmA: Investigation, Writing – review & editing. RI: Investigation, Writing – review & editing. JS: Investigation, Writing – review & editing. SH: Investigation, Writing – review & editing. WF: Project administration, Writing – review & editing. CR: Conceptualization, Resources, Writing – review & editing. SJ: Conceptualization, Writing – review & editing. AB: Conceptualization, Methodology, Supervision, Writing – review & editing. DM: Conceptualization, Formal Analysis, Funding acquisition, Methodology, Resources, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported in part by the American Lebanese Syrian Associated Charities (ALSAC) and the Conquer Cancer Foundation (Global Oncology Young Investigator Award, awarded to author DCM). The work is also supported by the St. Jude Children’s Research Hospital NCI Cancer Center Support CORE Grant CA21765. The funders had no specific role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
The authors thank Cherise Guess, PhD, ELS, for scientific editing of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2025.1560208/full#supplementary-material
Supplementary Figure 1 | Map of Pakistan showing participating institutions.
Supplementary Figure 2 | Schema of post-graduate medical training in Pakistan.
Supplementary Table 1 | The infrastructure of individual institutions and details of their pediatric oncology physician workforce.
Supplementary Table 2 | Participants’ comments on oversight of task-sharing physicians.
Supplementary File | Study questionnaire.
Abbreviations
HICs, High-income countries; LMICs, Low- and middle-income countries; TSPs, Task-sharing physicians; IQR, Interquartile range; PHO, Pediatric Hematology Oncology.
References
1. Ward ZJ, Yeh JM, Bhakta N, Frazier AL, Atun R. Estimating the total incidence of global childhood cancer: a simulation-based analysis. Lancet Oncol. (2019) 20:483–93. doi: 10.1016/S1470-2045(18)30909-4
2. Ward ZJ, Yeh JM, Bhakta N, Frazier AL, Girardi F, Atun R. Global childhood cancer survival estimates and priority-setting: a simulation-based analysis. Lancet Oncol. (2019) 20:972–83. doi: 10.1016/S1470-2045(19)30273-6
3. Chen L, Evans T, Anand S, Boufford JI, Brown H, Chowdhury M, et al. Human resources for health: overcoming the crisis. Lancet. (2004) 364(9449):1984–90. doi: 10.1016/S0140-6736(04)17482-5
4. Lassi ZS, Musavi NB, Maliqi B, Mansoor N, de Francisco A, Toure K, et al. Systematic review on human resources for health interventions to improve maternal health outcomes: evidence from low- and middle-income countries. Hum Resour Health. (2016) 14:10. doi: 10.1186/s12960-016-0106-y
5. Ribeiro RC, Antillon F, Pedrosa F, Pui CH. Global pediatric oncology: lessons from partnerships between high-income countries and low- to mid-income countries. J Clin Oncol. (2016) 34:53–61. doi: 10.1200/JCO.2015.61.9148
6. Atun R, Bhakta N, Denburg A, Frazier AL, Friedrich P, Gupta S, et al. Sustainable care for children with cancer: a Lancet Oncology Commission. Lancet Oncol. (2020) 21(4):e185–224. doi: 10.1016/S1470-2045(20)30022-X
7. Cappellano A, Gorostegui M, Gonzalez-Ramella O, Filho NPC, Valencia D, Chantada L, et al. International Society of Paediatric Oncology (SIOP) Global Mapping Programme: Latin American Society of Pediatric Oncology (SLAOP) country-level report. Pediatr Blood Cancer. (2024) 71(6):e30973. doi: 10.1002/pbc.30973
8. Orkin AM, Rao S, Venugopal J, Kithulegoda N, Wegier P, Ritchie SD, et al. Conceptual framework for task shifting and task sharing: an international Delphi study. Hum Resour Health. (2021) 19(1):61. doi: 10.1186/s12960-021-00605-z
9. WHO. Health workforce requirements for universal health coverage and the Sustainable Development Goals. Geneva: World Health Organisation (2016).
10. Guilbert JJ. The World Health Report 2006: working together for health. Educ Health (Abingdon). (2006) 19(3):385–7. doi: 10.1080/13576280600937911
11. Rubagumya F, Greenberg L, Manirakiza A, DeBoer R, Park PH, Mpunga T, et al. Increasing global access to cancer care: models of care with non-oncologists as primary providers. Lancet Oncol. (2017) 18(8):1000–2. doi: 10.1016/S1470-2045(17)30519-3
12. Ashengo T, Skeels A, Hurwitz EJH, Thuo E, Sanghvi H. Bridging the human resource gap in surgical and anesthesia care in low-resource countries: a review of the task sharing literature. Hum Resour Health. (2017) 15:77. doi: 10.1186/s12960-017-0248-6
13. Falk R, Taylor R, Kornelsen J, Virk R. Surgical task-sharing to non-specialist physicians in low-resource settings globally: A systematic review of the literature. World J Surg. (2020) 44:1368–86. doi: 10.1007/s00268-019-05363-7
14. Zhao Y, Hagel C, Tweheyo R, Sirili N, Gathara D, English M. Task-sharing to support paediatric and child health service delivery in low- and middle-income countries: current practice and a scoping review of emerging opportunities. Hum Resour Health. (2021) 19:95. doi: 10.1186/s12960-021-00637-5
15. Gyawali B, Carson LM, Shuel S, Wilkinson AN, Ostic H, Savage C, et al. Training general practitioners in oncology: lessons learned from a cross-sectional survey of GPOs in Canada. JCO Glob Oncol. (2023) 9:e2200421. doi: 10.1200/GO.22.00421
16. Kisker CT, Fethke CC, Tannous R. Shared management of children with cancer. Arch Pediatr Adolesc Med. (1997) 151:1008–13. doi: 10.1001/archpedi.1997.02170470042008
17. World Population Dashboard -Pakistan . United Nations Population Fund. Available online at: https://www.unfpa.org/data/world-population/PK (Accessed December 1, 2023).
18. Basbous M, Al-Jadiry M, Belgaumi A, Sultan I, Al-Haddad A, Jeha S, et al. Childhood cancer care in the Middle East, North Africa, and West/Central Asia: A snapshot across five countries from the POEM network. Cancer Epidemiol. (2021) 71(Pt B):101727. doi: 10.1016/j.canep.2020.101727
19. Graetz D, Ahmad A, Raza MR, Hameed A, Naheed A, Najmi A, et al. Barriers and facilitators of quality family-centered communication in Pakistan. JCO Glob Oncol. (2023) 9:e2300178. doi: 10.1200/GO.23.00178
20. Ashraf MS. Pediatric oncology in Pakistan. J Pediatr Hematol Oncol. (2012) 34 Suppl 1:S23–5. doi: 10.1097/MPH.0b013e318249abf9
21. Martin AN, Kaneza KM, Kulkarni A, Mugenzi P, Ghebre R, Ntirushwa D, et al. Cancer control at the district hospital level in Sub-Saharan Africa: an educational and resource needs assessment of general practitioners. J Glob Oncol. (2019) 5:1–8. doi: 10.1200/JGO.18.00126
22. Seidman G, Atun R. Does task shifting yield cost savings and improve efficiency for health systems? A systematic review of evidence from low-income and middle-income countries. Hum Resour Health. (2017) 15:29. doi: 10.1186/s12960-017-0200-9
23. Joshi R, Peiris D. Task-sharing for the prevention and control of non-communicable diseases. Lancet Glob Health. (2019) 7:e686–7. doi: 10.1016/S2214-109X(19)30161-5
24. Thomas PA, Kern DE, Hughes MT, Chen BY eds. Curriculum Development for Medical Education: A Six-Step Approach. ed (3). Baltimore, MD: Johns Hopkins University Press (2016).
Keywords: pediatric oncology, workforce, capacity building, training, task sharing, medical officers, pediatricians
Citation: Hashmi SK, Raza MR, Ashraf MS, Qadir G, Imam U, Fadoo Z, Ahmad A, Saeed H, Ghafoor T, Yasmeen N, Rana ZA, Hamid MH, Rehman MFu, Ahmad A, Iqbal R, Syed J, Hashmani S, Farooq W, Rodriguez-Galindo C, Jeha S, Belgaumi AF and Moreira DC (2025) Evaluation of task sharing as a workforce optimization strategy in pediatric oncology. Front. Oncol. 15:1560208. doi: 10.3389/fonc.2025.1560208
Received: 14 January 2025; Accepted: 01 April 2025;
Published: 28 April 2025.
Edited by:
Luca Giacomelli, Polistudium srl, ItalyReviewed by:
Anurag Agrawal, UCSF Benioff Children’s Hospital Oakland, United StatesMuhammad Abdul Rehman, Mayo Clinic, United States
Copyright © 2025 Hashmi, Raza, Ashraf, Qadir, Imam, Fadoo, Ahmad, Saeed, Ghafoor, Yasmeen, Rana, Hamid, Rehman, Ahmad, Iqbal, Syed, Hashmani, Farooq, Rodriguez-Galindo, Jeha, Belgaumi and Moreira. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Saman K. Hashmi, c2FtYW4uaGFzaG1pQHN0anVkZS5vcmc=
†These authors have contributed equally to this work
 Saman K. Hashmi
Saman K. Hashmi Muhammad Rafie Raza3†
Muhammad Rafie Raza3† Ghulam Qadir
Ghulam Qadir Uzma Imam
Uzma Imam Zehra Fadoo
Zehra Fadoo Alia Ahmad
Alia Ahmad Tariq Ghafoor
Tariq Ghafoor Nuzhat Yasmeen
Nuzhat Yasmeen Ameer Ahmad
Ameer Ahmad Carlos Rodriguez-Galindo
Carlos Rodriguez-Galindo Sima Jeha
Sima Jeha Daniel C. Moreira
Daniel C. Moreira