- 1Department of General Surgery, Pancreatic Disease Center, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2Shanghai Key Laboratory of Pancreatic Neoplasms Translational Medicine, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 3Research Institute of Pancreatic Diseases, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 4Clinical Research Center, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 5Division of Noncommunicable Diseases and Injury, Shanghai Municipal Center for Disease Control and Prevention, Shanghai, China
- 6Department of Vital Statistics, Division of Health Information, Shanghai Municipal Center for Disease Control and Prevention, Shanghai, China
- 7Shanghai Institute of Microsystem and information Technology, Chinese Academy of Sciences, Shanghai, China
- 8Shanghai Institute of Endocrine and Metabolic Diseases, Department of Endocrinology and Metabolism, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
Background: Shanghai has become a modern and international metropolis. A more comprehensive understanding of cancer incidence and mortality rates and socioenvironmental factors is explored to develop effective cancer control policies in Shanghai.
Methods: Cancer registration data are currently collected in Shanghai from 1973 to 2017, and socioenvironmental factors were obtained from the Shanghai statistical yearbook. Multivariate ridge regression analysis explored the contributions of socioenvironmental factors to cancer incidence and mortality, and the estimated annual percentage change (EAPC) was calculated for each cancer type by gender and district.
Results: Multivariate ridge regression analysis indicated that the number of divorces, total waste gas from industry, areas of buildings completed, and number of computers probably drove the increase in cancer incidence, and health expenditure and medical insurance cost probably contributed to the decrease in cancer mortality in Shanghai. Age-standardized cancer incidences of the lung in female patients, prostate, thyroid, and cervix increased most, and the incidence and mortality of esophagus, liver, and stomach cancers decreased most in Shanghai from 2002 to 2017. The most common cancer sites diagnosed were lung, colorectal, female breast, and male prostate in Shanghai in 2017, similar to the pattern in high-income countries. Stricter air control strategies, lower divorce rates, healthier lifestyles, and more effective HPV vaccination campaigns may be useful actionable measures of cancer prevention.
Conclusions: The longitudinal cancer data from the real world, which span decades, reported here and Shanghai’s experience in cancer prevention and control can be a reference for government guidelines in preventing population-level cancer incidence during city development.
Introduction
Cancer has been the leading cause of death and a significant public health issue in China (1). Shanghai is a significant economic and cultural center in China, and its rapid metropolitanization may cause population growth or aging or sociodemographic changes (2), which may impact cancer burden. Earlier studies have documented cancer burden in Shanghai, highlighting trends in cancer incidence in urban Shanghai from 1973 to 2010 (3) and urban–rural disparities in cancer incidence and mortality from 2002 to 2015 (4). However, it is rarely known whether socioenvironmental factors impact cancer incidence and cancer mortality in the process of the metropolitanization of Shanghai.
A more comprehensive understanding of cancer incidence and mortality and socioenvironmental factors is crucial to formulate effective cancer control policies. Therefore, this study presented cancer incidence and mortality trends in Shanghai, potential socioenvironmental factors probably attributing to these trends, cancer incidence and mortality pattern, and their implications for cancer control in Shanghai.
Methods
Data source
To comprehensively investigate and interpret the change of cancer trends, cancer registration data are currently collected in urban Shanghai from 1973 to 2017 and in rural Shanghai from 2002 to 2017. Factors associated with society and environment were collected from the Shanghai statistical yearbook, including population, population density, GDP per capita, total waste gas from industry, computers per hundred families, areas of buildings completed, divorce, total health expenditure, and medical insurance cost. Cancer registration utilizes internationally recognized ICD-10 codes for classification. Single cancer site and site groups comprising multiple sites were analyzed as the predominant causes of cancer incidence and death. Cancer sites in this study included nasopharynx (C11), esophagus (C15), stomach (C16), bowel (C18-20), liver (C22), gallbladder (C23-24), pancreas (C25), lung (C33-34), breast (C50), cervix (C53), uterus (C54), ovary (C56), prostate (C61), kidney (C64), bladder (C67), brain and central nervous system (C70-72), thyroid (C73), lymphoma (C81-86, C96), and leukemia (C91-C95). This study has been reviewed and approved by the Ethics Committee of Shanghai Municipal Center for Disease Control and Prevention.
Statistical analysis
EAPC values were calculated using a reported method of a generalized linear regression model with quasi-Poisson link function (5, 6). The study measured age-standardized cancer incidence and mortality rates per 100,000 as the outcome, with time from 2002 to 2017 serving as the independent variable. EAPC was estimated using the formula (exp (β^−1)’ 100, where β^ represented the estimated slope of the period variable. The 95% confidence interval (CI) is calculated from the fitted quasi-poison regression model (7). Trend analysis was based on the methodology outlined in the published paper (5). In brief, the criteria were followed: firstly, an increasing trend was identified when the EAPC value exceeds zero and the corresponding p-value was less than 0.05, indicating a notable upward trend with statistical significance. Secondly, a statistically significant decline trend was observed when the EAPC value was below 0 and the corresponding p-value was less than 0.05. Ultimately, when these conditions were unmet, cancer trends were determined to have remained stable. Univariate linear regression and multivariate ridge regression are used to quantify the contribution of each factor on cancer incidence and mortality trends. R version 4.4.2 was used for statistical analysis (8).
Results
Socioenvironmental factors could influence cancer incidence and mortality trends in Shanghai
Between 1978 and 2017, Shanghai transformed into a modern international metropolis, experiencing significant growth in population, population density, and GDP per capita (Figures 1A–C). The economic growth and increasingly urbanized and westernized lifestyle resulted in increasing environmental pollution (9). During the metropolitanization of Shanghai, outdoor and indoor environmental pollution (increases in waste gas from industry and buildings completed, Figures 1D, E), westernized lifestyles reflected by the increasing number of computers (Figure 1F), and mental stress (more divorce cases and higher price of real estate, Figure 1G)—all of these socioenvironmental factors were positively correlated with cancer incidence (Table 1), probably driving the increase in new cancer cases by 189.9% from 12,008 in 1973 to 34,810 in 2017 and an increase in crude cancer incidence by 170.6% from 213.4 in 1973 to 577.5 per 100–000 in 2017 in urban Shanghai, respectively (Figure 1H). Even though we adjusted the impact of age using Segi’s world population in 1960, an increase in age-standardized cancer incidence was observed in urban Shanghai from 1973 to 2017. In addition, screening projects and advanced early-stage diagnosis technology may contribute to the upward trend in cancer incidence. Facing the severe cancer burden, Shanghai made more efforts to improve the prognosis of cancer patients. Increasing health expenditure and medical insurance cost were negatively correlated with cancer mortality (Figures 1I, J, Table 1), probably attributing to the decline of age-standardized cancer mortality in urban Shanghai between 1973 and 2017 (Figure 1H). The increasing crude mortality may be the result of aging and population increase over time (Figure 1H).
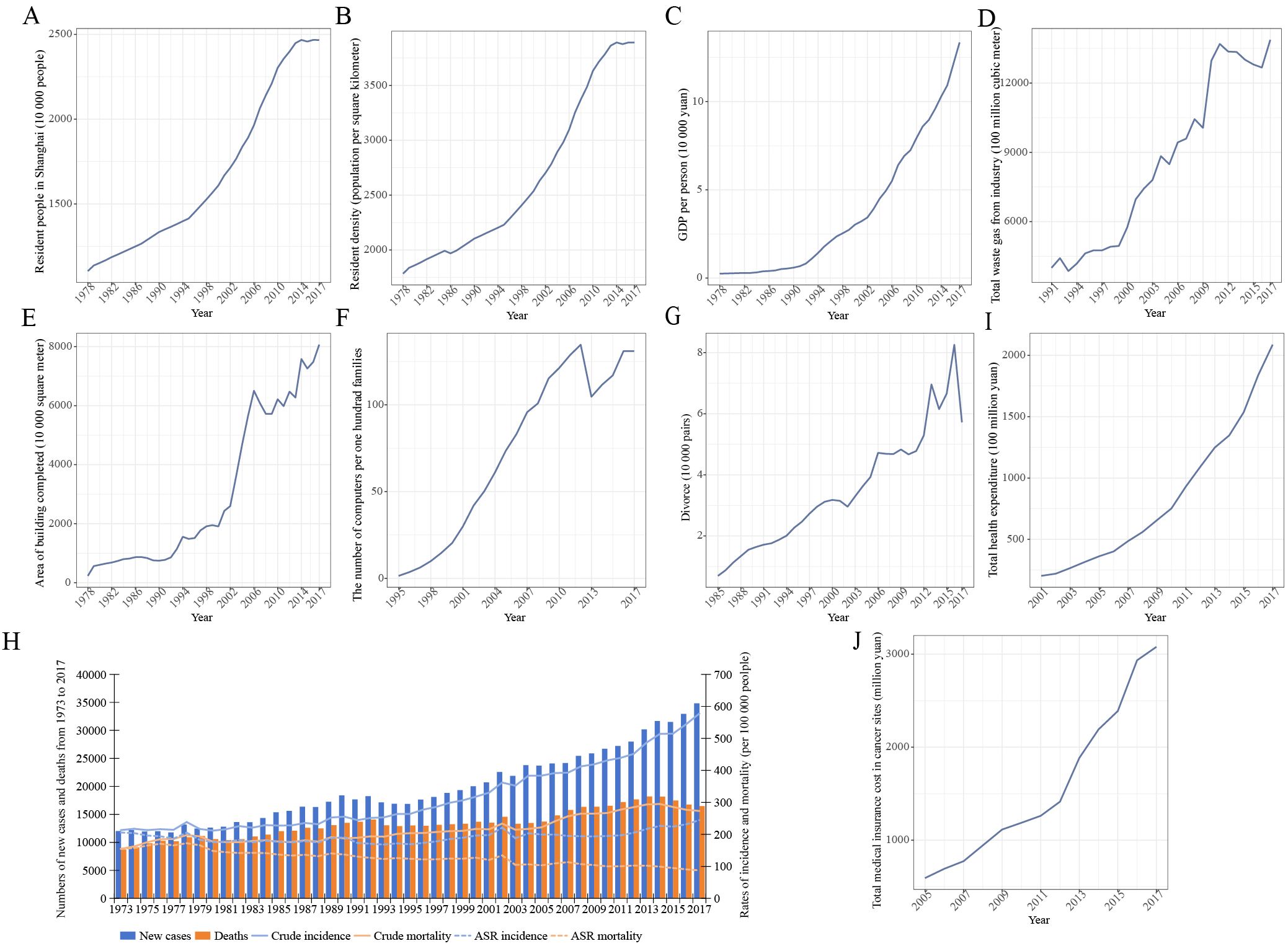
Figure 1. Analysis of socioenvironmental trends alongside cancer incidence and mortality rates over time in Shanghai. (A–C) Trends in population, population density, and GDP per capita in Shanghai from 1978 to 2017. (D–G) Trends in total waste gas from industry, area of building completed, the number of computers per hundred families, and the number of divorces over time in Shanghai. (H) Analysis of crude and age-standardized cancer incidence and mortality in urban Shanghai from 1973 to 2017. (I, J) Trends in total health expenditure and medical insurance cost for all cancers over time in Shanghai.
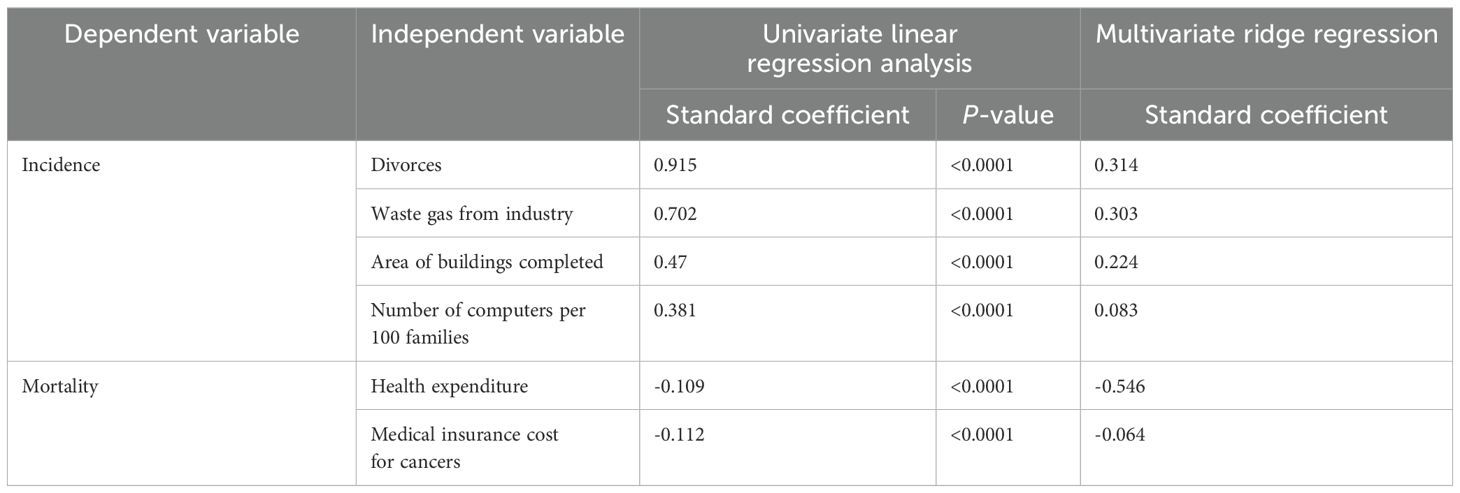
Table 1. Correlation analysis between cancer incidence and mortality and socioenvironmental factors.
Individual cancer incidence and mortality trends during Shanghai’s metropolitanization
We further calculated the EAPC for each cancer type by gender and district from 2002 to 2017. The EAPCs based on crude rates for most cancer sites except liver, esophagus, and stomach are more than 0, indicating upward trends both in crude cancer incidence and cancer mortality from 2002 to 2017 (Figure 2A). However, the EAPC values based on age-standardized cancer incidence and mortality for most cancer sites (esophagus, liver, stomach, etc.) sharply decreased, especially for cancer mortality (Figure 2B). Population growth and aging probably led to the opposite results.
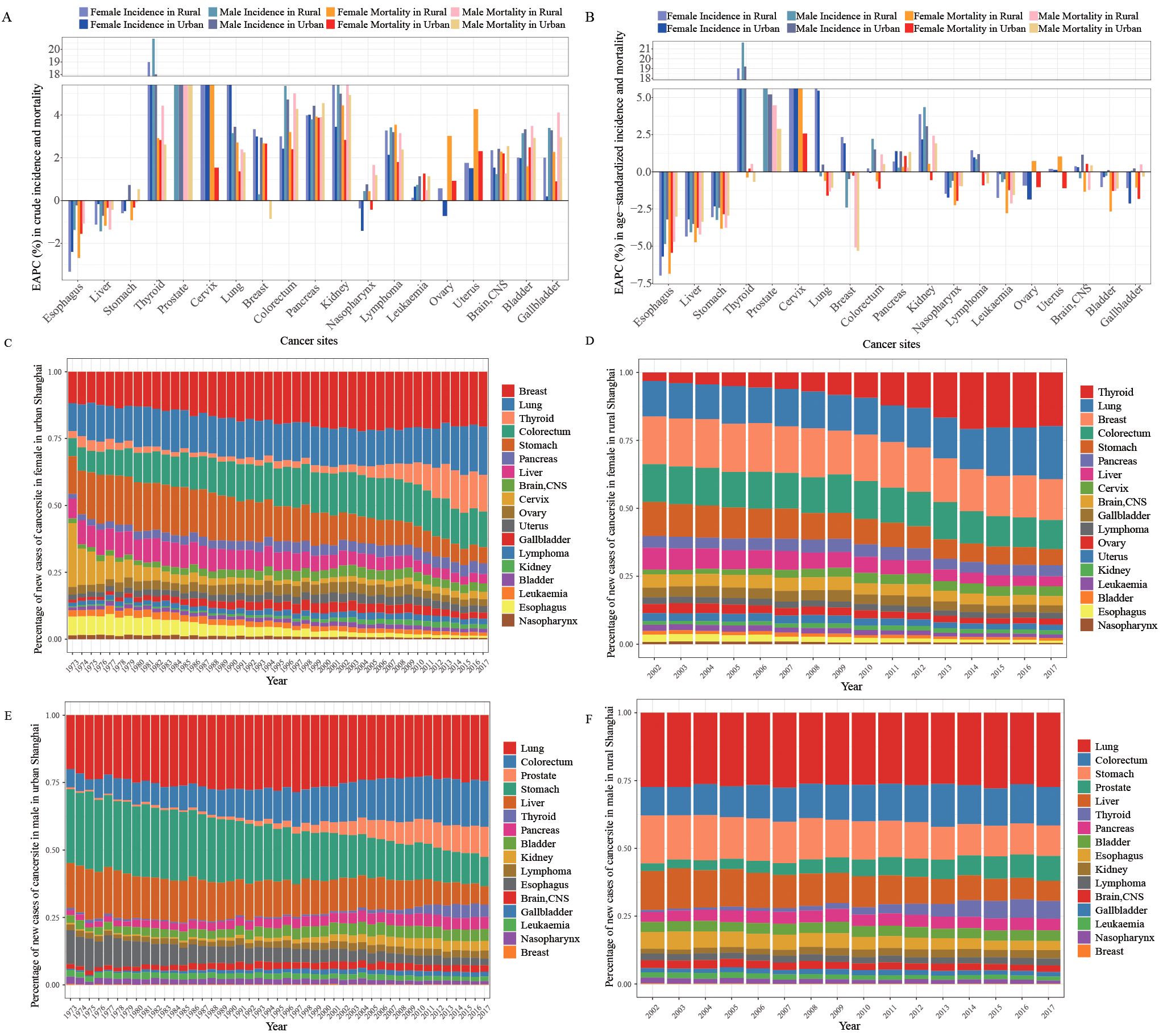
Figure 2. Incidence and mortality trends of each cancer type and cancer patterns in Shanghai, 2002–2017. (A, B) Estimated annual percentage change (EAPC) of crude and age-standardized cancer incidence and mortality categorized by gender and district in Shanghai from 2002 to 2017. (C, D) Stacked bar plots depict the cancer patterns of new cases in women in urban, 1973–2017, and in rural, 2002–2017. (E, F) Stacked bar plots depict the cancer patterns of new cases in men in urban, 1973–2017, and in rural, 2002–2017.
The incidence and mortality trends of specific cancer sites differed by gender and district over time (Figures 2B, 3). The incidence and mortality of esophagus, liver, and stomach cancers decreased by more than 2% per year both in rural and urban locations from 2002 to 2017. The top-four increase in age-standardized incidence was observed in cancers of the lung in females, prostate, thyroid, and cervix, with more than 5.0% increase per year (Figure 2B). In contrast to the upward incidence trend, the mortality of thyroid cancer remained very low and stable at less than 1.5% (Figure 2B). However, trends in mortality of prostate and cervix cancer increased by more than 2% per year, especially in rural areas. Lung cancer incidence in female patients sharply increased at 5.4% and 6.0% per year in urban and rural areas, respectively, while incidences in male patients hardly remained stable from 2002 to 2017 (urban EAPC of 0.46%, 95% CI (-0.30, 0.23); rural EAPC of -0.29%, 95% CI (-0.71, 0.14)). The age-standardized mortality of lung cancer slightly decreased in all populations. The age-standardized incidences of breast and colorectal cancer rose over time. Female breast cancer incidence, both in urban and rural areas, increased by more than 1.5% per year, while mortality in both rural and urban areas remained stable. The incidence and mortality of male colorectal cancer increased, especially in rural incidence, while the female colorectal cancer rates remained stable. Pancreas and kidney cancer incidence and mortality rates all slightly increased in all population, except in female mortality in urban areas.
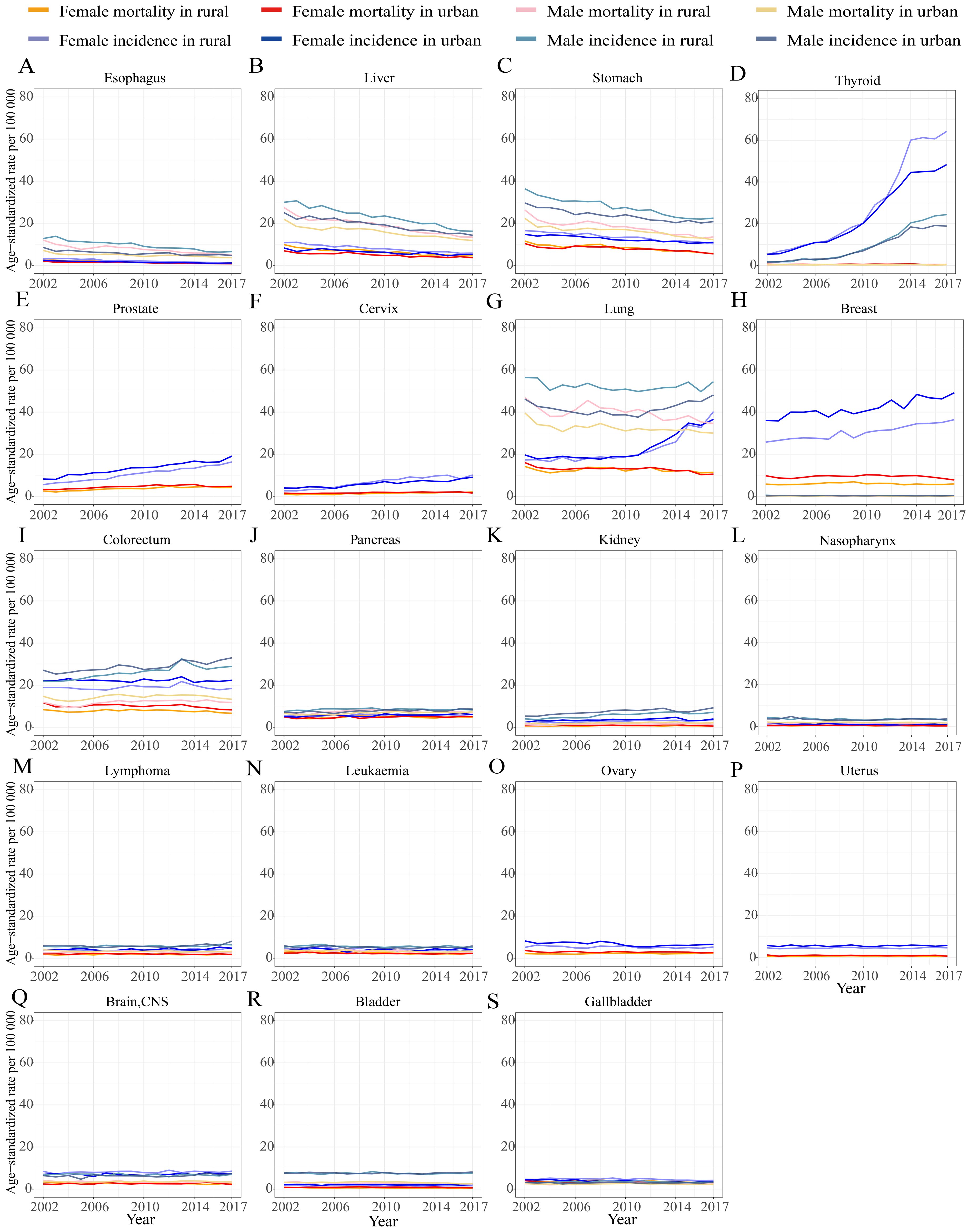
Figure 3. Trends in individual cancer incidence and mortality standardized by Segi’s world population in 1960, categorized by gender and district in Shanghai from 2002 to 2017. (A) esophagus; (B) liver; (C) stomach; (D) thyroid; (E) prostate; (F) cervix; (G) lung; (H) breast; (I) colorectum; (J) pancreas; (K) kidney; (L) nasopharynx; (M) lymphoma; (N) leukaemia; (O) ovary; (P) uterus; (Q) brain and central nervous system (brain, CNS); (R) bladder; (S) gallbladder.
Furthermore, we made a sensitivity analysis to present the cancer trends in urban (1973–2017) and in rural (2002–2017) areas (Supplementary Figures S1A, B). The results showed similar trends except cancer sites in cervix and gallbladder. Supplementary Figure S1C shows that the upward trend in cervix cancer in urban areas from 2002 to 2017 is consistent with that in rural Shanghai from 2002 to 2017, while the downward trend in cervix cancer in urban areas from 1973 to 2002 resulted in the opposite trends in urban areas, between Supplementary Figures S2A, B and Supplementary Figures S1A, B, contributed by the widespread application of human papillomavirus (HPV) vaccines. Similarly, the upward trends in gallbladder cancer incidence and mortality in urban Shanghai in 1973 to 2002 are opposite to the downward trend in gallbladder cancer in rural and urban Shanghai in 2003–2017 (Supplementary Figure S1D).
Cancer incidence and mortality patterns in Shanghai
During the metropolitanization of Shanghai, the cancer incidence profile seemed to be increasingly similar to the patterns of high-income countries (10), such as United States (11) and Japan (12). For women, the mostly frequently diagnosed cancer sites were cervix, stomach, and breast in urban Shanghai in 1973, which had been breast, colorectal, and lung cancers in urban and rural Shanghai since 2002, similar to the patterns of highly developed countries (Figures 2C, D). The proportion of new cases of breast cancer in urban Shanghai increased from 11.77% to 20.53% from 1973 to 2017, higher than 15.01% in rural areas in 2017. For men, the most frequently diagnosed cancer sites were lung, stomach, colorectal, and liver in rural and urban Shanghai in 2002. By 2017, the prevalent cancer sites had shifted to lung, colorectal, prostate, and stomach (Figures 2E, F). Specially the proportion of new cases of stomach cancer in male patients in urban Shanghai decreased from 27.31% to 10.91% from 1973 to 2017, only a little lower than 11.21% in men in rural Shanghai in 2017. The cancer types of lung, colorectal, male prostate, and female breast may be the universal cancer incidence patterns in metropolitanized cities. Westernized lifestyles, environmental pollution, effective prevention, and healthcare awareness promotion may be the reason for these pattern transformations in the process of metropolitanization.
However, the cancer mortality profiles did not seem to change from 2002 to 2017. For cancer deaths, lung, colorectal, stomach, liver, and pancreas had been the top five cancer sites in men, similar to that of lung, colorectal, stomach, breast, and pancreas in women in urban and rural Shanghai in 2017 (Supplementary Figure S2). The proportion of deaths due to colorectal cancer rose from 1973 to 2017 in urban Shanghai, which became the second leading cause of cancer deaths (Supplementary Figures S2A, B).
Cancer prevention and control in Shanghai
Lung cancer and colorectal cancer were the top two causes of new cancer cases and cancer deaths in Shanghai in 2017, highlighting the need for more efforts on enhanced prevention and control strategies, such as stricter air quality controls and healthier lifestyles. In 2002, the Shanghai Municipal Government initiated a colorectal cancer screening program in communities. Great progress was archived on the initial screening completion, with colorectal cancer detection rates of 201.35/100,000 in 2013 (13). Next, screening programs for cancers of the lung, stomach, esophagus, liver, breast, and cervix have been initiated in Shanghai since 2013. In addition, “Healthy Shanghai 2030” and “Healthy Shanghai Action (2019–2030)” projects were initiated in 2019, both emphasizing more effective tobacco control strategies, healthy lifestyles, and control measures of environment pollution. Notably, lung and breast cancer incidences and mortality among women have increased significantly. The corresponding prevention and control measures should be taken, such as healthier lifestyles and reduction of indoor pollution and divorce rates. Even though the trend in cervix cancer incidence sharply dropped before 2002 due to the widespread uptake of HPV vaccines, the upward trend since 2002 indicated the need for more effective HPV vaccination campaigns.
We believe that the longitudinal cancer data from the real world, which span decades, reported here and Shanghai’s experience in cancer prevention and control can be a reference for government guidelines in preventing population-level cancer incidence during city development.
Discussion
During the recent decades, the rapid metropolitanization of Shanghai brought dramatic changes due to socioenvironmental factors (14). A multivariate ridge regression analysis indicated that some socioenvironmental factors probably contributed to cancer incidence, including number of divorces, total waste gas from industry, buildings completed, and number of computers per 100 families (minimum contribution). The dramatic increase in total waste gas from industry and the areas of building completed may increase the outdoor air pollution, especially particulars (PM2.5), and indoor air pollution (formaldehyde and benzene), respectively, which are attributed to lung cancer incidence (15) and cancer burden (16). The rising number of computers per 100 families reflected the increasingly westernized lifestyles, and more and more divorces triggered stronger mental stress, both of which cancer incidence is attributed to (17, 18). More health expenditure and medical insurance cost are probably attributed to the decline of age-standardized cancer mortality in urban Shanghai, which were consistent with the published results (19, 20). Even though correlations between socioenvironmental factors and cancer incidence and mortality are observed, causal relationships remain unproven. In addition, the impacts of genetic predisposition, diagnostic advancements, aging population effects, and migration effects on cancer burden were not estimated, which probably influence the current results. Therefore, it is necessary for prospective robust studies to validate these causal relations.
During Shanghai’s metropolitanization, the cancer incidence patterns shifted to lung, colorectal, and female breast and male prostate cancers, which were also close to our many efforts on fighting against cancers. Primary prevention actions have been implemented since the 1990s, such as free hepatitis B vaccinations, Helicobacter pylori infection screening, and health education regarding cancer risk behavior, causing the decline in hepatitis B virus infection, Helicobacter pylori infection, and reflux esophagitis, all cancer risk factors (21, 22). The advanced treatment therapies and increases over time in fruit and vegetable consumption may result in a decline in mortality due to liver, stomach, and esophagus cancers (23). The dramatic increase in thyroid cancer was also observed in other countries, which may reflect “over-diagnosis” through the increasing use of new imaging diagnostic technologies, such as ultrasound and computed tomography (24). Herein thyroid cancer was not listed in the estimation of cancer incidence patterns. Prostate-specific antigen screening may drive the increase in prostate cancer (25). The increase in cervix cancer incidence and mortality may be attributed to the limitations of current HPV screening methods and vaccines (26). The implementation of strict smoking control laws in Shanghai since 1994 may have contributed to stabilizing the rising trend in male incidence (27). The increase in female lung cancer cases is probably due to indoor air pollution caused by cooking and heating using fuel gas and coals, along with soil and water contamination. The implementation of one-child policy since the 1970s and more divorces, along with mammography screening program, may contribute to the increasing trend in female breast cancer incidence. The adoption of westernized lifestyles, characterized by higher obesity rates and physical inactivity, may have an impact on the increase in incidences of breast and colorectal cancers.
The current study have some limitations. Firstly, this study is an ecological study. The trends of cancer burden and socioenvironmental factors were only correlated, resulting in no robust causal relations. Secondly, the distribution of age in cancer was not further explored. Thirdly, cancer data in rural Shanghai from 1973 to 2001 was not obtained.
Conclusion
The longitudinal cancer data from the real world, which span decades, reported here and Shanghai’s experience in cancer prevention and control can be a reference for government guidelines in preventing population-level cancer incidence during city development.
Data availability statement
Due to the grounds of our ethics approval, data from this study are unable to be shared. Most of the data supporting the conclusions of this study are available in the Cancer Incidence in Five Continents (CI5) series: Cancer Incidence in Five Continents Volumes I to X by IARC (http://ci5.iarc.fr/CI5I-X/Default.aspx).
Ethics statement
The studies involving humans were approved by the Ethics Committee of Shanghai Municipal Center for Disease Control and Prevention. The studies were conducted in accordance with the local legislation and institutional requirements.
Author contributions
JQ: Writing – original draft, Investigation, Funding acquisition, Writing – review & editing, Formal Analysis, Methodology, Software, Data curation, Resources, Visualization, Validation, Conceptualization. MW: Funding acquisition, Investigation, Writing – review & editing, Data curation, Validation, Methodology. SZ: Validation, Data curation, Writing – review & editing, Investigation. KG: Data curation, Writing – review & editing, Investigation. RC: Writing – review & editing, Investigation, Data curation. ZT: Data curation, Formal Analysis, Writing – review & editing. DZ: Formal Analysis, Writing – review & editing. JT: Writing – review & editing. WY: Formal Analysis, Conceptualization, Project administration, Writing – review & editing, Supervision, Software. BS: Resources, Funding acquisition, Writing – review & editing, Project administration, Conceptualization, Methodology, Software, Supervision, Data curation, Investigation. YS: Funding acquisition, Resources, Writing – review & editing, Formal Analysis, Project administration, Conceptualization, Software, Methodology, Data curation, Validation, Supervision, Investigation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the National Natural Science Foundation of China (grant number: 82304212(J.Q.), and 82273356 (B.S.)) and 2024 Shanghai Oriental Talents - Technology Platform Program (M. W).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2025.1615492/full#supplementary-material
Supplementary Figure 1 | Sensitivity analysis of incidence and mortality trends of each cancer type in rural Shanghai, 2002–2017, and in urban Shanghai, 1973–2017. (A, B) Estimated annual percentage change (EAPC) of crude and age-standardized cancer incidence and mortality categorized by gender and district in rural 2002 to 2017 and urban 1973 to 2017. (C, D) Trends in cervix and gallbladder incidence and mortality standardized by Segi’s world population in 1960, categorized by gender and district in rural 2002 to 2017 and urban 1973 to 2017.
Supplementary Figure 2 | Stacked bar plots depict the cancer patterns of deaths by genders in rural, 2002–2017, and urban, 1973–2017.
References
1. Chen W, Zheng R, Zhang S, Zeng H, Xia C, Zuo T, et al. Cancer incidence and mortality in China, 2013. Cancer Lett. (2017) 401:63–71. doi: 10.1016/j.canlet.2017.04.024
2. Wu H, Yang C, Liang A, Qin Y, Dunchev D, Ivanova B, et al. Urbanization and carbon storage dynamics: spatiotemporal patterns and socioeconomic drivers in shanghai. Land. (2024) 13:2098. doi: 10.3390/land13122098
3. Bao P-P, Zheng Y, Wu C-X, Huang Z-Z, Gao Y-T, Jin F, et al. Cancer incidence in urban Shanghai, 1973-2010: an updated trend and age-period-cohort effects. BMC Cancer. (2016) 16:284. doi: 10.1186/s12885-016-2313-2
4. Li X, Deng Y, Tang W, Sun Q, Chen Y, Yang C, et al. Urban-rural disparity in cancer incidence, mortality, and survivals in shanghai, China, during 2002 and 2015. Front Oncol. (2018) 8:579. doi: 10.3389/fonc.2018.00579
5. Shelton J, Zotow E, Smith L, Johnson SA, Thomson CS, Ahmad A, et al. 25 year trends in cancer incidence and mortality among adults aged 35–69 years in the UK, 1993-2018: retrospective secondary analysis. BMJ. (2024) 384:e076962. doi: 10.1136/bmj-2023-076962
6. Gardner W, Mulvey EP, and Shaw EC. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychol Bull. (1995) 118:392–404. doi: 10.1037/0033-2909.118.3.392
7. Hankey BF, Ries LA, Kosary CL, Feuer EJ, Merrill RM, Clegg LX, et al. Partitioning linear trends in age-adjusted rates. Cancer Causes Control CCC. (2000) 11:31–5. doi: 10.1023/a:1008953201688
8. R Core Team. A language and environment for statistical computing version 4.4.2 (2024). Available online at: https://www.r-project.org/ (Accessed October 31, 2024).
9. Goss PE, Strasser-Weippl K, Lee-Bychkovsky BL, Fan L, Li J, Chavarri-Guerra Y, et al. Challenges to effective cancer control in China, India, and Russia. Lancet Oncol. (2014) 15:489–538. doi: 10.1016/S1470-2045(14)70029-4
10. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
11. Siegel RL, Miller KD, and Jemal A. Cancer statistics, 2020. CA Cancer J Clin. (2020) 70:7–30. doi: 10.3322/caac.21590
12. Katanoda K, Hori M, Saito E, Shibata A, Ito Y, Minami T, et al. Updated trends in cancer in Japan: incidence in 1985–2015 and mortality in 1958-2018-A sign of decrease in cancer incidence. J Epidemiol. (2021) 31:426–50. doi: 10.2188/jea.JE20200416
13. Gong Y, Peng P, Bao P, Zhong W, Shi Y, Gu K, et al. The implementation and first-round results of a community-based colorectal cancer screening program in shanghai, China. Oncologist. (2018) 23:928–35. doi: 10.1634/theoncologist.2017-0451
14. Cui L and Shu J. Urbanization and its environmental effects in Shanghai, China. Urban Clim. (2012) 2:1–15. doi: 10.1016/j.uclim.2012.10.008
15. Turner MC, Andersen ZJ, Baccarelli A, Diver WR, Gapstur SM, Pope CA, et al. Outdoor air pollution and cancer: An overview of the current evidence and public health recommendations. CA Cancer J Clin. (2020) 10.3322/caac.21632. doi: 10.3322/caac.21632
16. Li N, Zhai Z, Zheng Y, Lin S, Deng Y, Xiang G, et al. Association of 13 occupational carcinogens in patients with cancer, individually and collectively, 1990-2017. JAMA Netw Open. (2021) 4:e2037530. doi: 10.1001/jamanetworkopen.2020.37530
17. Antoni MH, Lutgendorf SK, Cole SW, Dhabhar FS, Sephton SE, McDonald PG, et al. The influence of bio-behavioural factors on tumour biology: pathways and mechanisms. Nat Rev Cancer. (2006) 6:240–8. doi: 10.1038/nrc1820
18. Keum N and Giovannucci E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol. (2019) 16:713–32. doi: 10.1038/s41575-019-0189-8
19. Goss PE, Lee BL, Badovinac-Crnjevic T, Strasser-Weippl K, Chavarri-Guerra Y, St Louis J, et al. Planning cancer control in Latin America and the Caribbean. Lancet Oncol. (2013) 14:391–436. doi: 10.1016/S1470-2045(13)70048-2
20. Zafar SY, Peppercorn JM, Schrag D, Taylor DH, Goetzinger AM, Zhong X, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. (2013) 18:381–90. doi: 10.1634/theoncologist.2012-0279
21. Yu SZ. Facilitating the continuous decline on the incidence rates of hepatitis B and liver cancer through cutting off the mother-to-child viral transmission, based on the “prevention first” strategy, in China. Chin J Epidemiol. (2019) 40:1650–3. doi: 10.3760/cma.j.issn.0254-6450.2019.12.027
22. Yuan JM, Yu MC, Xu WW, Cockburn M, Gao YT, and Ross RK. Helicobacter pylori infection and risk of gastric cancer in Shanghai, China: updated results based upon a locally developed and validated assay and further follow-up of the cohort. Cancer Epidemiol biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. (1999) 8:621–4.
23. Wang J-W, Zhang C-G, Deng Q-L, Chen W-L, Wang X, and Yu J-M. The associations of comorbidities and consumption of fruit and vegetab le with quality of life among stomach cancer survivors. Health Qual Life Outcomes. (2018) 16:62. doi: 10.1186/s12955-018-0886-y
24. Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. (2016) 66:115–32. doi: 10.3322/caac.21338
25. Qi D, Wu C, Liu F, Gu K, Shi Z, Lin X, et al. Trends of prostate cancer incidence and mortality in Shanghai, China from 1973 to 2009: Trends of Prostate Cancer Incidence and Mortality. Prostate. (2015) 75:1662–8. doi: 10.1002/pros.23046
26. Ruan Y, Li H, Liu M, Cao G, Xu X, Han L, et al. A retrospective analysis of human papillomavirus (HPV) prevalence and genotype distribution among 25,238 women in Shanghai, China revealed the limitations of current HPV-based screening and HPV vaccine. Cancer Epidemiol. (2023) 84:102372. doi: 10.1016/j.canep.2023.102372
Keywords: cancer, incidence, mortality, trend, socioenvironment, metropolitanization
Citation: Qin J, Wu M, Zhao S, Gu K, Cai R, Tang Z, Zhu D, Tian J, Yao W, Shen B and Shi Y (2025) Trends in cancer incidence and mortality in the process of metropolitanization of Shanghai, 1973–2017. Front. Oncol. 15:1615492. doi: 10.3389/fonc.2025.1615492
Received: 21 April 2025; Accepted: 08 July 2025;
Published: 01 August 2025.
Edited by:
Jianhua Yin, Second Military Medical University, ChinaReviewed by:
Jaba Tkemaladze, Longevity Clinic Georgia Inc, GeorgiaShujuan Lin, Putian University, China
Copyright © 2025 Qin, Wu, Zhao, Gu, Cai, Tang, Zhu, Tian, Yao, Shen and Shi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Shi, c2hpeWFuY2RjQG91dGxvb2suY29t; Baiyong Shen, c2hlbmJ5QHNoc211LmVkdS5jbg==; Wei Yao, d2VpLnlhb0BtYWlsLnNpbS5hYy5jbg==
†These authors have contributed equally to this work
 Jiejie Qin
Jiejie Qin Mengyin Wu5†
Mengyin Wu5† Jingyan Tian
Jingyan Tian Baiyong Shen
Baiyong Shen Yan Shi
Yan Shi