- 1Department of Hematology, Oncology and Stem Cell Transplantation, Bambino Gesù Children's Hospital (IRCCS), Rome, Italy
- 2Neuroradiology Unit, Department of Imaging, Bambino Gesù Children's Hospital (IRCCS), Rome, Italy
- 3Department of Pathology, Bambino Gesù Children's Hospital (IRCCS), Rome, Italy
- 4Neuro-oncology Unit, Department of Hematology, Oncology and Stem Cell Transplantation, Bambino Gesù Children's Hospital (IRCCS), Rome, Italy
- 5Neurosurgery Unit, Department of Neuroscience and Neurorehabilitation, Bambino Gesù Children's Hospital (IRCCS), Rome, Italy
Extraventricular neurocytoma (EVN) is an extremely rare tumor of neuroglial origin with a tendency toward ganglionic or glial differentiation. In the 2016 World Health Organization Classification, EVN was classified as a grade II tumor and described as a neoplasm with good outcome. However, the presence of cellular atypia is an important unfavorable prognostic factor. Here, we describe the first case of a patient with a congenital EVN localized in the brainstem. After a sub-total resection, his disease rapidly progressed despite several chemotherapies, including molecular targeting approaches. He died 13 months after diagnosis. In conclusion, we report an atypical case of EVN presenting an extremely aggressive behavior, despite the absence of cellular atypia. The brainstem origin and the age of the patient may have represented two important prognostic factors for our patient.
Introduction
Brain tumors are extremely rare in the first year of life, accounting for less than 2% of brain neoplasms at all pediatric ages [1]. The definition of “congenital brain tumor” (CBT) is subject to debate, with several classifications described in the literature [2]. However, the 2 main criteria taken into account for the diagnosis of a CBT are the age of the child at the onset of symptoms (first 3 months of age) [3] and the histology of the tumor which differs from the one observed for older patients [2].
Neurocytomas are rare brain tumors associated with neuronal differentiation, which develop mainly in young adults aged 25–35 years old and rarely in children with no case, to our knowledge, being reported as congenital [4]. Neurocytomas are located within the ventricular system (CN, “central neurocytomas”) or, less commonly, within the extra-ventricular region (EVN, “extra-ventricular neurocytoma”) of the central nervous system. EVN differs from CN by having a more heterogeneous and complex histological appearance. When compared to CN, EVN is less cellularized, and shows a pronounced tendency toward glial or ganglionic differentiation in part of the tumor, hence providing the name of extra-ventricular (ganglio)neurocytoma [5].
EVNs are defined as grade II tumors according to the WHO classification [6]. However, EVNs can be divided into typical and atypical sub-groups, depending on their histological features and aggressiveness. The typical EVNs represent the less-aggressive variants of the disease. In contrast, the atypical EVNs are aggressive tumors characterized by an elevated mitotic and proliferative index and/or high vascularization and necrosis [7]. Another factor indicative of unfavorable prognosis for EVNs is cellular atypia [8], although there are reports on EVNs with atypia characteristics for patients who have excellent disease control, and, on the other hand, EVNs without sign of atypia, for patients who present a poor overall outcome [9].
We report the first case of congenital EVN localized in the brainstem of a 3-month-old patient. The patient presented a dismal outcome despite multimodal therapy and absence of cellular atypia.
Case Description
History
A 3-month-old male was referred to our hospital for the management of a congenital intracranial mass and infective endocarditis in the bicuspid aortic valve.
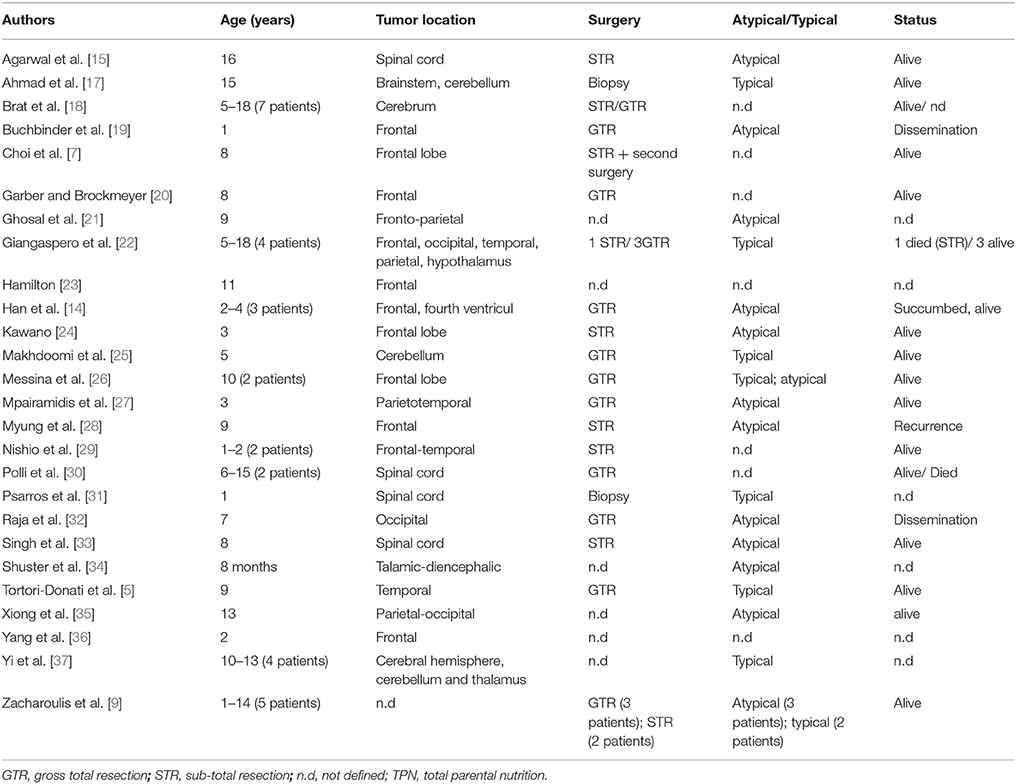
At birth, the child presented lower limb weakness, left seventh nerve palsy and left neck swelling, due to his cardiac problem, associated with a head turning difficulty. A magnetic resonance imaging of the brain showed a left pontine-bulbar lesion extended upward into the cerebellum. The fourth ventricle and the cerebellar vermis was dislocated (Figure 1). A few days after the diagnosis, he presented fever associated to Staphylococcus aureus bacteremia. An echocardiogram showed a vegetative endocarditis in the bicuspid aortic valve with an ejection fraction of 45%. The patient received antibiotic therapy for this infection.
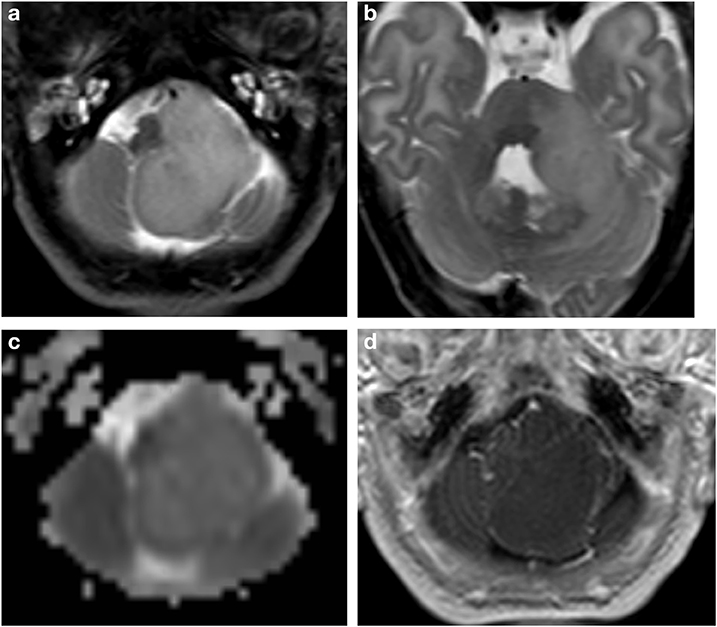
Figure 1. Brain MRI. Axial T2w (a,b) ADC map (c) and Gd T1w (d) images. Extensive hyperintense mass in the left cerebellopontine angle extended upward into the cerebellum with lower peripheral ADC values and subtle peripheral linear irregular enhancement after gadolinium injection. The fourth ventricle, medulla oblongata and the cerebellum are dislocated and compressed.
After transfer to our center, he underwent aortic valve replacement via Ross Procedure with no complications. He presented a neurological deterioration with a left sided hemiparesis, dysphagia and recurrent episodes of apnea.
One month after the cardiac surgery, he underwent suboccipital craniotomy in the prone position with intraoperative neuronavigation and neurophysiologic monitoring. The surgery was interrupted during resection of the infiltrating bulbar component because of sustained bradycardia and arterial hypertension and only a sub-total resection (STR) was performed. He presented a stable neurological status after surgery but received a tracheostomy for a mild pulmonary insufficiency.
Pathological Findings
Histology showed proliferation of small/medium-size round cells with a central round nucleus, finely speckled chromatin, and small nucleolus. Ganglioid cells, intermediates between neurocytes and ganglion cells, were evenly distributed and differentiation toward fully mature ganglion cells was observed. Neoplastic cells were strongly positive for synaptophysin and neurofilaments, mildly positive for Neu-N, and negative for GFAP and CD34, indicating a neuronal nature of the tumor. Additional immunohistochemistry revealed weak positivity for p53 (< 5%), mTor, phospho-mTor and EGFR. Ki67 was low (1% with some areas up to 3–4%). Mitoses were 3–4/10 HPF. BRAFv600E mutation was assessed by DNA sequencing and resulted positive. A diagnosis of extra-ventricular (ganglio)neurocytoma was then formulated and the tumor was classified as grade II according to WHO 2016, with a particular mention of the focal higher proliferation index (Figure 2).
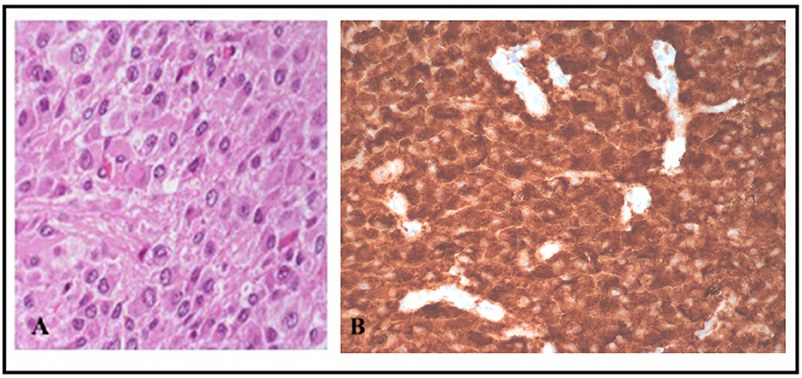
Figure 2. (A) Hematoxylin&Eosin staining shows a diffused, monomorphic, round cell proliferation with various degrees of ganglioid differentiation. (B) Strong positivity for synaptophysin immunostain.
Postoperative Course
Considering the young age of the patient and the sub-total resection, we decided to perform an adjuvant therapy. After two cycles with high-dose carboplatin and etoposide, Magnetic Resonance Imaging (MRI) showed a local disease progression. A treatment with the mTOR inhibitor, Everolimus, as single agent was started but no tumor response was observed. Despite further treatments with irinotecan, temozolomide and then the BRAFV600E inhibitor Vemurafenib, the MRI showed a gradual increase of tumor size associated with hydrocephalus. The patient underwent a ventriculo-peritoneal shunt. The number and duration of desaturation episodes increased due to the involvement of the medullary respiratory center. Intermittent mechanical ventilation and total parenteral nutrition were necessary.
The child died of a cardiorespiratory arrest thirteen months after diagnosis.
Discussion
EVN is included in the 2016 “WHO classification of tumors of the central nervous system” in the “Neuronal and mixed neuronal-glial tumors” group and classified as grade II [6]. Most of EVNs are supratentorial with few cases reported as cerebellar or spinal, and only 3 described in the pons [10]. EVN incidence is unknown but it is certainly a rare disease with just over 100 cases found in the literature. EVN arises predominantly in young adults (median age of 25 years old) [11], and there are only 43 cases of pediatric EVNs reported so far and summarized in Table 1.
To our knowledge, we describe here the first case of a congenital EVN. Therefore, EVN could be added to the list of other known CBTs, including teratomas, choroid plexus papillomas, embryonal tumors, infantile desmoplastic astrocytomas/gangliogliomas and craniopharyngiomas [2]. The EVN described here presented characteristics of (ganglio)neurocytomas suggested by the presence of ganglioid intermediates and fully differentiated ganglion cells. The disease did not show a detectable sign of cellular atypia, a factor normally considered as an unfavorable prognosis for EVN [9]. However, we defined it as atypical because of the high proliferation index (Ki67>2%) observed in some tumor areas, a feature associated with a high recurrence rate [12]. Our case also presented a mutation in the BRAF gene never described before for EVN and rarely detected in pediatric brain tumors [13].
Because of the rarity of the EVNs, few data are available regarding the therapeutic strategies used to treat patients [14]. The use of radiotherapy in children is subject to debate because of the poor survival benefit [15] and the undesirable effects observed in the developing brain, such as stroke and neurocognitive deficits [16]. For this patient the radiotherapy option was not considered because of the young age and the presence of recurrent episodes of apnea. Gross total resection (GTR), which represents the mainstay of treatment for EVN [14], was not possible because of the brainstem localization of the tumor, so only an STR was performed. The main chemotherapeutic regimens used to date for EVNs treatment include cisplatin/etoposide/cyclophosphamide, procarbazine/CCNU/vincristine and ifosfamide/carboplatin/etoposide [9]. In our case, following an STR, two cycles of high dose of carboplatin and cisplatin, and the use of targeted therapies including topoisomerase, mTOR and BRAFV600E inhibitors, the disease progressed and the young patient died 13 months after diagnosis.
Conclusions
To our knowledge, this is the first report of a congenital EVN. The disease, localized in the brainstem, presented an aggressive behavior and progressed rapidly, leading to death despite the absence of unfavorable histology with the exception of a focal high proliferation index. The impossibility to achieve a GTR and the critical localization of the tumor are two potentially significant factors for the prognosis of patients who develop an EVN.
Ethics Statement
This study was carried out in accordance with the recommendations of the Internal Review Board of the Bambino Gesù Ospedale Pediatrico with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the Internal Review Board of the Bambino Gesù Ospedale Pediatrico.
Informed Consent
The authors declare that written informed consent was obtained from the patient's parents for publication of this case report.
Authors Contributions
MP: design of the work, structuration, interpretation of the data, writing; AM: conception (ideation), structuration, acquisition of the data, structuration, revision, final approval to be published; EM: acquisition of the data, structuration, revision; EdB and AD: revision; MV: acquisition of the data, elaboration of the data; GC: acquisition of the data, acquisition and elaboration of the images; FD-C: pathological findings; AC: conception, structuration, acquisition of the data, revision.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Manoranjan B, Provias JP. Congenital brain tumors: diagnostic pitfalls and therapeutic interventions. J Child Neurol. (2011) 26:599–614. doi: 10.1177/0883073810394848
2. Severino M. Schwartz ES, Thurnher MM, Rydland J, Nikas I, Rossi A. Congenital tumors of the central nervous system. Neuroradiology (2010) 52:531–48. doi: 10.1007/s00234-010-0699-0
3. Alamo L, Beck-Popovic M, Gudinchet F, Meuli R. Congenital tumors: imaging when life just begins. Insights Imaging (2011) 2:297–308. doi: 10.1007/s13244-011-0073-8
4. Phi JH, Kim DG. Rare pediatric central neurocytomas. Neurosurg Clin N Am. (2015) 26:105–8. doi: 10.1016/j.nec.2014.09.015
5. Tortori-Donati P, Fondelli MP, Rossi A, Cama A, Brisigotti M, Pellicanò G. Extraventricular neurocytoma with ganglionic differentiation associated with complex partial seizures. Am J Neuroradiol. (1999) 20:724–7.
6. Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization Classification of tumors of the central nervous system: a summary. Acta Neuropathol. (2016) 131:803–20. doi: 10.1007/s00401-016-1545-1
7. Choi H, Park SH, Kim DG, Paek SH. Atypical extraventricular neurocytoma. J Korean Neurosurg Soc. (2011) 50:381–4. doi: 10.3340/jkns.2011.50.4.381
8. Kane AJ, Sughrue ME, Rutkowski MJ, Aranda D, Mills SA, Lehil M, et al. Atypia predicting prognosis for intracranial extraventricular neurocytomas. J Neurosurg. (2012) 116:349–54. doi: 10.3171/2011.9.JNS10783
9. Zacharoulis S, Morales La Madrid A, Bandopadhayay P, Chi SN, Manley P, Ullrich NN, et al. Central versus extraventricular neurocytoma in children : a clinicopathologic comparison and review of the literature. J Pediatr Hematol Oncol. (2016) 38:479–85. doi: 10.1097/MPH.0000000000000627
10. Hawasli AH, Haydon DH, Dahiya S, Smyth MD. Pontine extraventricular neurocytoma in a child. Pediatr Neurosurg. (2014) 48:319–23. doi: 10.1159/000351576
11. Huang WY, Zhang BY, Geng DY, Zhang J. Computed tomography and magnetic resonance features of extraventricular neurocytoma: a study of eight cases. Clin Radiol. (2013) 68:e206–12. doi: 10.1016/j.crad.2012.11.009
12. Xu L, Ouyang Z, Wang J, Liu Z, Fang J, Du J, et al. A clinicopathologic study of extraventricular neurocytoma. J Neurooncol. (2016) 132:75–82. doi: 10.1007/s11060-016-2336-1
13. Kieran, MW. Targeting BRAF in pediatric brain tumors. Am Soc Clin Oncol Educ Book (2014) e436–440. doi: 10.14694/EdBook_AM.2014.34.e436
14. Han L, Niu H, Wang J, Wan F, Shu K, Ke C, et al. Extraventricular neurocytoma in pediatric populations: a case report and review of the literature. Oncol Lett. (2013) 6:1397–405. doi: 10.3892/ol.2013.1583
15. Agarwal S, Sharma MC, Sarkar C, Suri V, Jain A, Sharma MS, et al. Extraventricular neurocytomas: a morphological and histogenetic consideration. A study of six cases. Pathology (2011) 43:327–34. doi: 10.1097/PAT.0b013e3283463f97
16. Roddy E, Mueller S. Late effects of treatment of pediatric central nervous system tumors. J Child Neurol. (2016) 31:237–54. doi: 10.1177/0883073815587944
17. Ahmad F, Rosenblum MK, Chamyan G, Sandberg DI. Infiltrative brainstem and cerebellar neurocytoma. J Neurosurg Pediatr. (2012) 10:418–22. doi: 10.3171/2012.8.PEDS08286
18. Brat DJ, Scheithauer BW, Eberhart CG, Burger PC. Extraventricular neurocytomas: pathologic features and clinical outcome. Am J Surg Pathol. (2001) 25:1252–60. doi: 10.1097/00000478-200110000-00005
19. Buchbinder D, Danielpour M, Yong WH, Salamon N, Lasky J. Treatment of atypical central neurocytoma in a child with high dose chemotherapy and autologous stem cell rescue. J Neurooncol. (2010) 97:429–37. doi: 10.1007/s11060-009-0029-8
20. Garber ST, Brockmeyer DL. A rare case of a pediatric extraventricular neurocytoma: case report and review of the literature. Childs Nerv Syst. (2012) 28:321–6. doi: 10.1007/s00381-011-1649-9
21. Ghosal N, Dadlani R, Somorendra Singh S, Hegde AS. Atypical extraventricular neurocytoma: a rare and challenging case diagnosed on intraoperative cytology. Cytopathology (2012) 23:270–3. doi: 10.1111/j.1365-2303.2011.00861.x
22. Giangaspero F, Cenacchi G, Losi L, Cerasoli S, Bisceglia M, Burger PC, et al. Extraventricular neoplasms with neurocytoma features. A clinicopathological study of 11 cases. Am J Surg Pathol. (1997) 21:206–12. doi: 10.1097/00000478-199702000-00011
23. Hamilton R. Case of the month. August 1996–frontal lobe tumor in 11 year old girl. Brain Pathol. (1997) 7:713–4. doi: 10.1111/j.1750-3639.1997.tb01086.x
24. Kawano H, Kimura T, Iwata K, Furukawa M, Nomura S, Ishii A, et al. Atypical extraventricular neurocytoma in a 3-year-old girl: case report with radiological-pathological correlation. Childs Nerv Syst. (2015) 31:1189–93. doi: 10.1007/s00381-015-2706-6
25. Makhdoomi R, Malik NK, Wani A, Bhat S, Baba K. Extraventricular neurocytoma of the vermis in a child. J Clin Neurosci. (2010) 17:1469–71. doi: 10.1016/j.jocn.2010.02.027
26. Messina R, Cefalo MG, Secco DE, Cappelletti S, Rebessi E, Carai A, et al. Behavioral disorders as unusual presentation of pediatric extraventricular neurocytoma: report on two cases and review of the literature. BMC Neurol. (2014) 14:242. doi: 10.1186/s12883-014-0242-8
27. Mpairamidis E, Alexiou GA, Stefanaki K, Sfakianos G, Prodromou N. Extraventricular neurocytoma in a child: case report and review of the literature. J Child Neurol. (2009) 24:491–4. doi: 10.1177/0883073808324534
28. Myung JK, Cho HJ, Park CK, Chung CK, Choi SH, Kim SK, et al. Clinicopathological and genetic characteristics of extraventricular neurocytomas. Neuropathology (2013) 33:111–21. doi: 10.1111/j.1440-1789.2012.01330.x
29. Nishio S, Takeshita I, Kaneko Y, Fukui M. Cerebral neurocytoma. A new subset of benign neuronal tumors of the cerebrum. Cancer (1992) 70:529–37. doi: 10.1002/1097-0142(19920715)70:2<529::AID-CNCR2820700225>3.0.CO;2-0
30. Polli FM, Salvati M, Miscusi M, Delfini R, Giangaspero F. Neurocytoma of the spinal cord: report of three cases and review of the literature. Acta Neurochir. (2009) 151:569–74. doi: 10.1007/s00701-009-0305-6
31. Psarros TG, Swift D, Mulne AF, Burns DK. Neurocytoma-like neoplasm of the thoracic spine in a 15-month-old child presenting with diffuse leptomeningeal dissemination and communicating hydrocephalus. Case report. J Neurosurg. (2005) 103:184–90. doi: 10.3171/ped.2005.103.2.0184
32. Raja AI, Yeaney GA, Jakacki RI, Hamilton RL, Pollack IF. Extraventricular neurocytoma in neurofibromatosis type 1: case report. J Neurosurg Pediatr. (2008) 2:63–7. doi: 10.3171/PED/2008/2/7/063
33. Singh A, Chand K, Singh H, Sarkar C, Sharma MC. Atypical neurocytoma of the spinal cord in a young child. Childs Nerv Syst. (2007) 23:207–11. doi: 10.1007/s00381-006-0141-4
34. Shuster A, Midia M. Case of the month #180: atypical thalamic and mesencephalic neurocytoma - a rare neoplasm in children. Can Assoc Radiol J. (2013) 64:74–6. doi: 10.1016/j.carj.2010.09.006
35. Xiong Z, Zhang J, Li Z, Jiang J, Han Q, Sun S, Wu X, et al. A comparative study of intraventricular central neurocytomas and extraventricular neurocytomas. J Neurooncol. (2015) 121:521–9. doi: 10.1007/s11060-014-1659-z
36. Yang GF, Wu SY, Zhang LJ, Lu GM, Tian W, Shah K. Imaging findings of extraventricular neurocytoma: report of 3 cases and review of the literature. AJNR Am J Neuroradiol. (2009) 30:581–5. doi: 10.3174/ajnr.A1279
Keywords: brain tumor, (Ganglio)neurocytoma, extraventricular neurocytoma, pediatric, brainstem
Citation: Piras M, Miele E, Di Giannatale A, Colafati GS, Diomedi-Camassei F, Vinci M, de Billy E, Mastronuzzi A and Carai A (2018) Congenital Extra-Ventricular (Ganglio)Neurocytoma of the Brain Stem: A Case Report. Front. Pediatr. 6:108. doi: 10.3389/fped.2018.00108
Received: 22 December 2017; Accepted: 03 April 2018;
Published: 11 May 2018.
Edited by:
Alberto Spalice, Policlinico Umberto I, ItalyReviewed by:
Satinder Aneja, Lady Hardinge Medical College, IndiaGouri Rao Passi, Choithram Hospital and Research Centre, India
Copyright © 2018 Piras, Miele, Di Giannatale, Colafati, Diomedi-Camassei, Vinci, de Billy, Mastronuzzi and Carai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrea Carai, YW5kcmVhLmNhcmFpQG9wYmcubmV0
 Marta Piras1
Marta Piras1 Evelina Miele
Evelina Miele Emmanuel de Billy
Emmanuel de Billy Angela Mastronuzzi
Angela Mastronuzzi Andrea Carai
Andrea Carai