- 1Neonatal Intensive Care Unit, S.Orsola-Malpighi University Hospital, Bologna, Italy
- 2Department of Medical and Surgical Sciences (DIMEC), University of Bologna, Bologna, Italy
- 3Obstetric Unit, Department of Medical and Surgical Sciences, Policlinico Sant'Orsola-Malpighi, University of Bologna, Bologna, Italy
- 4University of Bologna, Bologna, Italy
The perspective proposed by this article will focus on perinatal palliative care as a strategy for improving the quality of life of neonates with life-limiting conditions when extending the patient's life is no longer the goal of care. This manuscript reports the creation of an innovative program of perinatal palliative care called “Percorso Giacomo” (Giacomo's Pathway) at Sant'Orsola Hospital in Bologna, Italy in 2013. Key features include interdisciplinary collaboration between professionals from obstetrics, neonatology and other specialties aiming to reach the most detailed fetal and neonatal diagnosis and prognosis; communication and engagement with the family to discuss goals of care and prepare a birthing plan that follows the family's desires and expectations; and personalized care to achieve comfort for each newborn and support for families according to their social, cultural, and religious backgrounds.
Introduction
Perinatal palliative care (PPC) is offered in the settings of fetal or neonatal diagnoses of life-limiting conditions (LLCs) as a plan to achieve comfort of the neonate and to support the family. Given the complexity of the medical and non-medical needs of these neonates and the emotional challenges for parents, PPC is a necessarily holistic and interdisciplinary approach to care. PPC is a journey with families that begins at the moment of diagnosis, whether prenatal or postnatal, and involves a collaboration among maternal-fetal medicine specialists, neonatologists, and other professionals with the goal of establishing an individualized plan of care for the mother-baby dyad.
The American College of Obstetricians and Gynecologists (ACOG) considers PPC one of the options of care that should be offered to patients facing pregnancies complicated by fetal LLC (1). Yet, PPC is not yet routinely integrated in prenatal counseling in the United States (2, 3). This also holds true for Italy. A recent Italian national survey of neonatal intensive care unit (NICU) practitioners demonstrated that only 30% of the institutions represented offer a structured PPC program. Of these, 34% have only one program coordinator, and fewer than 30% organize PPC training for health care providers (4).
Despite technological advances in the ability to detect severe fetal anomalies, infants with LLCs are occasionally diagnosed only after birth. Moreover, critically ill neonates admitted to the NICU can face a potentially adverse prognosis or reach the end-of-life stage, at which point a redirection of goals of care is required. According to the World Health Organization (WHO), palliative care and intensive care should be provided concurrently to critically ill infants with potentially adverse prognoses (5). The American Academy of Pediatrics (AAP) and the Italian Society of Neonatology (SIN) provide recommendations for achieving comfort of terminally ill neonates and of those affected by an LLC (6–9).
The urgent need to provide the option of PPC to families with neonates prenatally or postnatally diagnosed with an LLC prompted the creation and implementation of an innovative PPC program at Sant'Orsola Hospital (SOH) in Bologna in 2013. The program was named “Percorso Giacomo” (Giacomo's Pathway) in honor of the first infant to whom SOH provided such care. This paper describes the origin and the development of the program over its first 7 years.
Clinical Case
Giacomo was prenatally diagnosed with anencephaly. His parents, although aware of his short life expectancy, chose to carry the pregnancy to term. The mother was a G4 P3 woman with two healthy children and another baby with anencephaly whose delivery was complicated by failure to progress and stillbirth. As she again received an anencephaly diagnosis, she asked her provider to manage her care with the goal of having some precious time with her baby after birth. At that time there were no guidelines for PPC at SOH, so the obstetrician involved a neonatologist and a midwife to plan the delivery and the infant's postnatal care according to the mother's desire. Giacomo was delivered by cesarean section (transverse position) with Apgar scores of 9 and 9. After his scalp wound was carefully dressed, he was given to his family to hold. Per parental wish, he was baptized by the hospital chaplain. Following the family desire for bonding, Giacomo was allowed to room-in with his mother in a private postpartum room. At SOH, this was the first time that a baby with LLC was not admitted to the NICU. Comfort measures, including skin-to-skin care and holding to facilitate bonding and warmth, were offered. The infant had no sucking reflex; thus, he was given small feeds via an orogastric tube to relieve hunger and thirst. Discomfort and pain were assessed but Giacomo had no signs of distress and did not need any pharmacological treatment. Giacomo lived for only 19 hours, but he had the opportunity to meet his parents, siblings, and relatives, and he was comfortable throughout his entire life.
Written informed consent was obtained from Giacomo's parents for the publication of any potentially identifiable images or data included in this article.
Percorso Giacomo
Origin
The experience with Giacomo made our perinatal team aware of the urgency to formalize a systematic approach to families who received a fetal or neonatal diagnosis of LLC, and a collaborative journey began. Another key factor that triggered the initiation of a PPC program, was that the neonatologist who provided care to Giacomo received training in PPC in 2009–2011 by participating in the Neonatal Comfort Care Program (NCCP) (10) at Columbia University Medical Center (CUMC) in New York, NY, US. Upon her return to Italy she began to investigate the feasibility of a similar program at SOH, and the meeting with Giacomo's family was the occasion to start the project.
During the debreafing of Giacomo's case, each of the professionals involved in the care expressed interest in developing a service for similar cases and the planning began. The group decided to name the program “Percorso Giacomo” (PG) in honor of Baby Giacomo.
The experience with this family was not only the trigger for the planning of a new service, but also a milestone in the understanding of the complex medical and non-medical needs of these infants and their families.
The group then opened to other professionals interested in the same goal, and a working group of champions called the “Percorso Giacomo Team” (PGT) was established. Two main objectives were identified: (1) assemble an interdisciplinary team, and (2) define guidelines and eventually establish a new hospital policy for PPC.
Gathering an Interdisciplinary Team
SOH is a large academic institution with a busy maternal-fetal medicine service that has approximately 3,500 deliveries each year. The level 3 NICU takes care of some 300 critically ill neonates annually, including infants prenatally or postnatally diagnosed with an LLC. The two services work collaboratively, but until 2013 there was limited knowledge and no direct experience of PPC.
The PGT is an interdisciplinary team that includes nine clinicians from obstetrics and neonatology who identify themselves as champions for the care of mothers and infants with a fetal or neonatal diagnosis of LLC. The program is not funded, and the team members make themselves available as primary providers for the mother-baby dyad and facilitate the execution of the plan of care in collaboration with medical staff involved in the care. Professionals from a variety of other specialties (cardiology, neurology, surgey, nephrology, genetics, etc.) are also available for consultation.
Establishing Guidelines
After carefully reviewing PPC literature, including recommendation from the ACOG (11), the AAP (6), and the SIN (8), and through networking with other national and international academic centers, local guidelines were created and implemented to standardize interventions. The essential elements are summarized in Tables 1, 2.
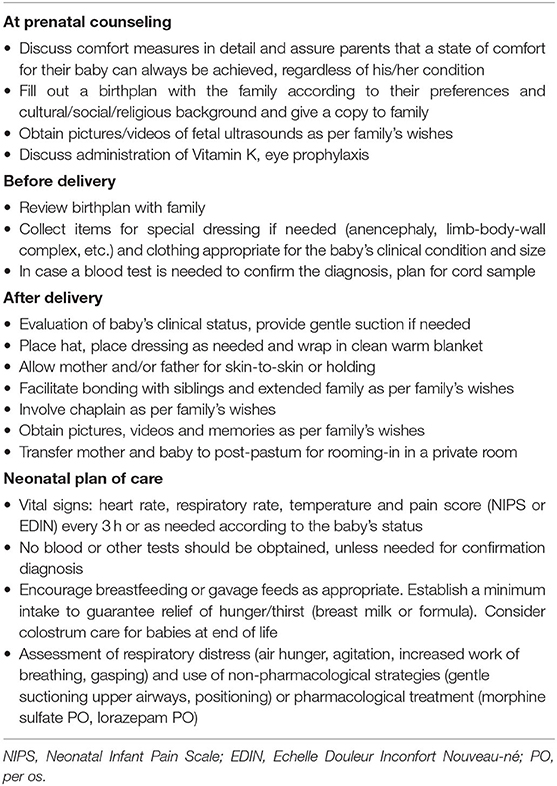
Table 1. Guidelines to provide comfort to neonates prenatally diagnosed with life-limiting conditions.
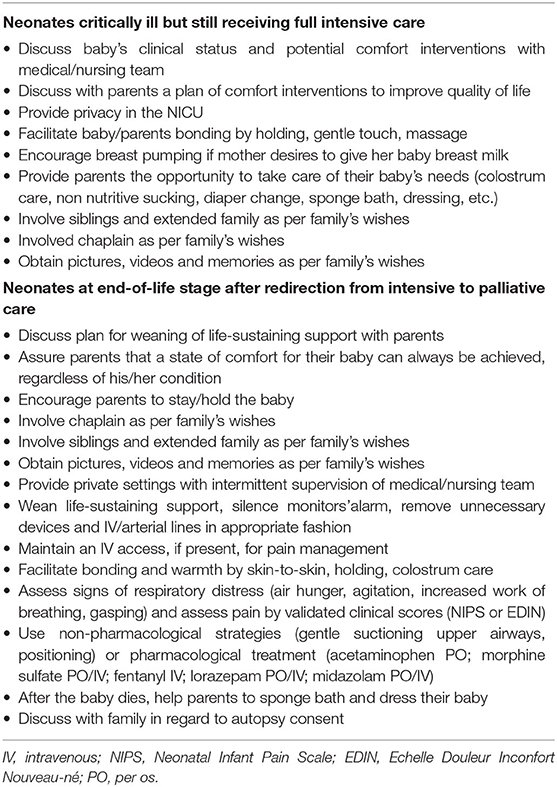
Table 2. Guidelines to provide comfort to neonates with life-threatening or terminal conditions in the NICU.
As the focus of care is the satisfaction of neonates' basic needs for bonding, maintanance of body temperature, and relief of hunger and thirst, our guidelines reflected these recommendations. Pain and distress are assessed and treated with pharmacological interventions (12). The Neonatal Infant Pain Scale (NIPS) (13) and Echelle Douleur Inconfort Nouveau-ne' (EDIN) (14) are the preferred pain assessment tools because they are based on the infant's behavior and do not require vital signs detection, which could disrupt the bonding experience. Each neonate has unique medical and non-medical needs; thus, we personalized the care plan in consideration of diagnosis, prognosis, gestational age, and family preferences. Additionally, as a result of a policy change in our hospital, when a neonate, prenatally diagnosed with an LLC, is not admitted to the NICU, is directly transitioned from delivery room to a post-partum for rooming-in with the mother in private setting. The midwife in charge of the mother-baby dyad provides support and care in collaboration with NICU nurses and neonatologist is available for medical evaluation and interventions.
Criteria for Enrollment
PG offers PPC to neonates prenatally or postnatally diagnosed with an LLC that is expected to render their life brief, such as renal agenesis, anencephaly or extreme prematurity. PPC is also offered to neonates diagnosed with severe genetic, metabolic, skeletal, cardiac, neurological or oncological conditions and life-limiting syndromes. The provision of intensive care can prolong the life of these neonates, but when the burden of invasive and aggressive treatment might exceed the benefit in terms of length of life, an option of PPC is offered.
Perinatal Counseling
The PGT can be accessed in different ways. If a mother receives a diagnosis of fetal LLC at SOH, the obstetric provider offers available options, including consultation with the PGT. Patients might also be referred by outside institutions. After consultation, the mother has the option to transfer her care to SOH, or to continue care with her current provider, with the PGT functioning as consultant.
Members of the PGT—including a neonatologist, an obstetrician, and a midwife—are involved in the encounter with the family. Before meeting the family, team members meet to review available information about the fetal diagnosis, discuss the need to obtain further tests and/or to involve more specialists, and identify care options to be presented to the family. It is essential that the family receives clear and honest information from both obstetricians and neonatologists.
The conversation with the family focuses on communicating of detailed information about the presumed or certain diagnosis and prognosis and, if needed, any further medical investigations. Team members listen attentively to the family to identify concerns, hopes, and expectations that will help them prepare a comprehensive plan for the reminder of the pregnancy, labor and delivery, and postnatal birthing plan. At the end of the meeting the parents are also given the option to meet a psychologist to assess mental health and to provide grief support, resources, and referrals for the family at large. Depending on the complexity of the diagnosis and the gestational age, one or more meetings are needed to complete a comprehensive plan.
The outcome of the conversation/s is documented on the mother's health record to facilitate communication with all clinicians involved in mother-baby care. Moreover, providers and family complete a document -the “birthing plain”- that is kept by the family and presented upon hospital admission.
Members of the PGT follow labor and delivery, and the neonatologist present at birth either confirms the neonate's diagnosis or obtains further tests for confirmation. The team ensures that the birth plan formulated during prenatal counseling is included in the overall management care plan.
When neonates admitted to the NICU are postnatally diagnosed with an LLC or a potentially adverse prognosis, the medical team attentively evaluates each case and may involve the PGT as an extra layer of support to families. Different options can be proposed including the continuation of intensive care with focus on quality of life, or the redirection of goals of care with transition to palliative care.
Pregnancy and Neonatal Outcomes
The PGT cared for 24 cases in its first 7 years. The team followed 20 pregnancies, the outcome of which included two intrauterine fetal deaths, two second trimester spontaneous abortions, and 16 live births. Three of these infants are currently alive and stable, and PPC was not considered medically appropriate for these infants because their postnatal diagnoses were more favorable than had been expected. The PGT also facilitated palliative care plans for four neonates admitted to the NICU with severe brain injury secondary to severe metabolic conditions or hypoxic-ischemic insults, all of whom died.
Education and Program Development
Teaching and training are essential to fostering a mindset that includes palliative care as an essential component of medical practice in perinatology. Over time the PGT built several initiatives for PPC training at SOH. Formal teaching, including a curriculum of six lessons for pediatric residents and fellows, was established in 2017. Bedside training and clinical case discussion for physicians, midwives, and nurses also have been introduced over the past 7 years.
In 2014, the concern for education and program development inspired the PGT to organize a National Workshop featuring national and international experts in PPC. The workshop goals included presentation of cutting-edge experiences of PPC and network development. The workshop was attended by some 300 clinicians from all across Italy and laid the foundation for collaboration with several academic institutions. The meeting was also attended by the Maternal Infant Department leadership and administrators. They expressed their interest and encouraged development of a PPC service at SOH. The PGT then worked tirelessly with administrators and leadership to establish a new hospital policy for PPC, which was approved in 2019.
In our region of Italy, Emilia-Romagna, a new project for the organization of a regional palliative care network has begun (15). This pediatric hospice network offers inpatient care and home care for children with complex medical conditions and chronic health problems. PG has been included in this network by the project committee. This is an essential step to build a continuity of care for neonates born with LLC or for those with complex diseases and potentially adverse prognoses. After hospital discharge, infants can be supported either at home or in a rehabilitation facility by specialists in palliative care. This project is also an opportunity to promote the palliative care mindset in our region and, hopefully, in the entire nation.
Discussion
Over the past years, PPC has been gaining interest in Italy, and clinicians involved in perinatology have been working to define the best care practice (16) and to establish adequate pathways to care for neonates diagnosed with LLCs (17). Moreover, the SIN has offered suggestions for PPC in a document focused on guidelines for prevention and treatment of neonatal pain (8, 9) and Italy has enacted legislation promoting the use of palliative care (18).
PG has positioned itself as an innovative pathway for PPC origins and guidelines.
What triggered the actualization of this program was the desire of a family (Giacomo's parents) to be accompanied along the perinatal journey. The professionals involved in the care were inspired to create a standardized program for families with similar needs. The experience of PG show that a strong motivation is pivotal to the birth of a new program.
PG was modeled after the NCCP in New York. In the planning process the PGT utilized evidence-based recommendations (6, 8, 9, 11); however, the innovative aspects of the PG guidelines came largely from direct experience and ongoing collaboration with the NCCP. An important step for “culture change” at SOH is the transition of neonates with LLC from delivery room directly to post-partum to room-in with the mother, instead of admission to the NICU (Table 1).
Another innovative element includes the introduction of early palliative care interventions to improve quality of life of babies still receiving full intensive care (Table 2). Both innovations have been supported by studies of parental satisfaction (19) and stress evaluation (20) published by the NCCP.
In pregnancy care, two patients are at stake. Thus, tight collaboration of specialists in obstetrics and neonatology is essential to propose available options (1), to plan a safe pregnancy and delivery, and to provide a personalized care for each neonate in accord with the family's preference (21). Pregnancy is a time of hope and expectation, but with the discovery of severe anomalies, fear can quickly overcome hope as expectations are no longer the norm. The option of PPC supports the family and helps in the decision-making process (22, 23). Moreover, the 7-years experience of PG shows that families felt welcomed and embraced along the perinatal journey. Parents expressed of PG gratitude and praise for the program, as clearly illustrated by parental feed-back messages. “PG was the light at the end of the tunnel, PG was the hope that our baby would have been able to be embraced by mom, dad an her siblings”; “PG taught us that our life cannot be measured by its lenght, rather by the mark we leave”; “The program filled somehow the void we experienced and we felt serene.”
The greatest desire of parents of neonates with LLC is not wanting them to suffer. Thus, pain and distress must be attentively assessed and treated (12). In the population we served any degree of discomfort was successfully managed with the use of non-pharmacological strategies, such as skin-to-skin holding, and colostrum care (24) or proper medications. This observation has been validated by studies of parental perception of their infants' state of comfort, when infants were treated with standardized comfort measures (19).
PPC not only addresses the population of neonates expected to have early perinatal demise, but also can be integrated with the intensive care of critically ill neonates at any stage of the illness (20, 25). In its first years, PG focuses largely on the care of mothers with fetal life-limiting diagnoses and followed neonates with short life expectancy however, in time the PGT began to be consulted regarding the plan of care of critically ill neonates with unexpected life-threatening diagnoses. Thus the PGT developed guidelines to facilitate quality of life during the NICU admission and/or to redirect goals of care at end of life (Table 2).
Future Direction
PG has been offering perinatologists the opportunity to improve their confidence in this growing field in medicine. Within 1 year of the program's establishment, the PGT organized a national conference. Since that time many other educational initiatives have been proposed to guide and educate providers. When PPC knowledge is lacking, clinicians are uncomfortable and reluctant to offer this much-needed care (26). Thus, PG is planning to continue to offer training courses for medical and nursing professionals built on the knowledge and experience acquired over the past 7 years.
Throughout the years, PG has followed infants with a variety of severe life-threatening conditions, including rare and complex diseases. Collaboration with other academic centers has been essential to share experiences, to discuss challenging cases, and to provide the best possible care to each infant. Further networking opportunities will support the implementation of new programs in tertiary NICUs and will provide the necessary tools to professionals working in small institutions where programs cannot be implemented.
PG intends to facilitate the spreading of a mindset that integrates palliative care in the medical plan for neonates with LLC or critically ill. Being aware that further studies measuring outcomes and quality of care are needed, our group is in the process of analyzing the efficacy of this program.
As recommended by national and international organizations (1, 6, 27), PPC is a crucial option to be offered to families facing a fetal or neonatal diagnosis of LLC. Essential components include early involvement with families at the time of diagnosis, interdisciplinary collaboration of perinatologists, and promotion of education to facilitate a culture change.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Written informed consent was obtained from the participant's parents for the publication of any potentially identifiable images or data included in this article.
Author Contributions
CL conceptualized and designed the report. MB, LC, GF, LP, and GS drafted the initial manuscript and approved the final manuscript as submitted. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors express their profound gratitude to the members of the Percorso Giacomo Team (Patrizio Calderoni, Santo Merlini, Maria Antonietta Graziano, Silvia Savini, Marika Friguglietti, Caterina Voli, Marta Bucchi) and to the babies and their families, from whom they have learned so much about perinatal palliative care.
References
1. Perinatal Palliative Care. Committee Opinion No. 786. American College of Obstetricians and Gynecologists Committee on Obstetric Practice, Committee on Ethics. Obstet Gynecol. (2019) 134:e84–9. doi: 10.1097/AOG.0000000000003425
2. Tosello B, Haddad G, Gire C, Einaudi M. Lethal fetal abnormalities: how to approach perinatal palliative care? J Matern Fetal Neonatal Med. (2017) 30:755–8. doi: 10.1080/14767058.2016.1186633
3. Kukora S, Gollehon N, Laventhal N. Antenatal palliative care consultation: implications for decision-making and perinatal outcomes in a single-centre experience. Arch Dis Child Fetal Neonatal Ed. (2017) 102:F12–16. doi: 10.1136/archdischild-2016-311027
4. Cavicchiolo ME, Rusalen F, Benini F, Baraldi E, Lago P. Perinatal palliative care: a national survey in Italy. Arch Dis Child Fetal Neonatal Ed. (2019) 104:F567–8. doi: 10.1136/archdischild-2018-316327
5. World Health Organization. WHO Definition of Palliative Care. (2018). Available online at: https://www.who.int/health-topics/palliative-care
6. Section on Hospice and Palliative Medicine and Committee on Hospital Care. Pediatric palliative care and hospice care commitments, guidelines, and recommendations. Pediatrics. (2013) 132:966–72. doi: 10.1542/peds.2013-2731
7. Committee on Fetus Newborn, Section on Anesthesiology Pain Medicine, Keels E, Sethna N, Watterberg KL, Cummings JJ, et al. Prevention and management of procedural pain in the neonate: an update. Pediatrics. (2016) 137:e20154271. doi: 10.1542/peds.2015-4271
8. Società Italiana di Neonatologia Gruppo di Studio di Analgesia e Sedazione. Linee guida per la prevenzione ed il Trattamento del Dolore nel neonato. Padova: Cooperativa Libraria Editrice Università di Padova (2008).
9. Società Italiana di Neonatologia Gruppo di Studio di Analgesia e Sedazione nel Neonato. Linee guida per la prevenzione ed il Trattamento del Dolore nel neonato. Milano: Biomedia (2016).
10. Neonatal Comfort Care Program. Available online at: www.neonatalcomfortcare.com (accessed 21 July 2020).
11. American College of Obstetrician and Gynecologists Committee on Ethics American Academy of Pediatrics Committe on Bioethics. Maternal-fetal intervention and fetal care centers. Pediatrics. (2011) 128:e473–8. doi: 10.1542/peds.2011-1570
12. Carter BS, Jones PM. Evidence-based comfort care for neonates towards the end of life. Semin Fetal Neonatal Med. (2013) 18:88–92. doi: 10.1016/j.siny.2012.10.012
13. Lawrence J, Alcock D, McGrath P, Kay J, MacMurray SB, Dulberg C. The development of a tool to assess neonatal pain. Neonatal Netw. (1993) 12:59–66.
14. Debillion T, Zupan V, Ravault N, Magny JF, Dehan M. Development and initial validation of the EDIN scale, a new tool for assessing prolonged pain preterm infants. Arch Dis Child Fetal Neonatal Ed. (2001) 85:F36–41. doi: 10.1136/fn.85.1.F36
15. DRG 1131/2015. Recepimento dell'accordo tra Governo, Regioni e Province autonome del documento ‘Individuazione delle figure professionali competenti nel campo delle cure palliative e della terapia del dolore, nonchè delle strutture sanitarie, ospedaliere e territoriali, coinvolte nelle reti delle cure palliative. Bologna: Atti della Giunta della Regione Emilia Romagna. (2015).
16. Rusalen F, Cavicchiolo ME, Lago P, Salvadori S, Benini F. Perinatal palliative care: is palliative care really available to everyone? Ann Palliat Med. (2018) 7:487–8. doi: 10.21037/apm.2018.07.09
17. Rusalen F, Cavicchiolo ME, Lago P, Salvadori S, Benini F. Perinatal palliative care: a dedicated care pathway. BMJ Support Palliat Care. (2019). doi: 10.1136/bmjspcare-2019-001849. [Epub ahead of print].
18. Legge 15 marzo 2010 n 38. Disposizioni per Garantire L'accesso alle Cure Palliative e alla terapia del Dolore. Roma: Gazzetta Ufficiale della Repubblica Italiana (2010).
19. Parravicini E, Daho M, Foe G, Steinwurtzel R, Byrne M. Parental assessment of comfort in newborns affected by life-limiting conditions treated by a standardized neonatal comfort care program. J Perinatol. (2018) 38:142–7. doi: 10.1038/jp.2017.160
20. Callahan K, Steinwurtzel R, Bruaire L, Schechter S, Parravicini E. Early palliative care reduces stress in parents of neonates with congenital heart disease: validation of the “Baby, Attachment, Comfort Interventions.” J Perinatol. (2019) 39:1640–7. doi: 10.1038/s41372-019-0490-y
21. Carter BS. More than medication: perinatal palliative care. Acta Paediatr. (2016) 105:1255–6. doi: 10.1111/apa.13529
22. Cote-Arsenault D, Denney-Koelsch E. “Have no regrets:” parents' experiences and developmental tasks in pregnancy with a lethal fetal diagnosis. Soc Sci Med. (2016) 154:100–9. doi: 10.1016/j.socscimed.2016.02.033
23. Janvier A, Farlow B, Barrington KJ. Parental hopes, interventions, and survival of neonates with trisomy 13 and trisomy 18. Am J Med Genet C Semin Med Genet. (2016) 172:279–87. doi: 10.1002/ajmg.c.31526
24. Parravicini E, McCarthy F. Comfort in perinatal and neonatal palliative care: an innovative plan of care focused on relational elements. In: Limbo R, Wool C, Carter BS, editors. Handbook of Perinatal and Neonatal Palliative Care: A Guide for Nurses, Physicians, and Other Health Professionals. Chapter 4. New York, NY: Springer Company, LLC (2020).
25. Parravicini E. Neonatal palliative care. Curr Opin Pediatr. (2017) 29:135–40. doi: 10.1097/MOP.0000000000000464
26. Wool C. Clinician confidence and comfort in providing perinatal palliative care. J Obstet Gynecol Neonatal Nurs. (2013) 42:48–58. doi: 10.1111/j.1552-6909.2012.01432.x
27. National Consensus Project for Quality Palliative Care. Clinical practice guidelines for quality palliative care. 4th ed. Richmond, VA: National Coalition for Hospice and Palliative Care (2018). Available online at: https://www.nationalcoalitionhpc.org/ncp
Keywords: perinatal palliative care, neonatal palliative care, life-limiting conditions, comfort care, interdisciplinary team
Citation: Locatelli C, Corvaglia L, Simonazzi G, Bisulli M, Paolini L and Faldella G (2020) “Percorso Giacomo”: An Italian Innovative Service of Perinatal Palliative Care. Front. Pediatr. 8:589559. doi: 10.3389/fped.2020.589559
Received: 31 July 2020; Accepted: 20 October 2020;
Published: 19 November 2020.
Edited by:
Elvira Parravicini, Columbia University, United StatesReviewed by:
Charlotte Wool, York College of Pennsylvania, United StatesEmanuela Ferretti, Children's Hospital of Eastern Ontario (CHEO), Canada
Copyright © 2020 Locatelli, Corvaglia, Simonazzi, Bisulli, Paolini and Faldella. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chiara Locatelli, Y2hpYXJhLmxvY2F0ZWxsaUBhb3NwLmJvLml0
 Chiara Locatelli
Chiara Locatelli Luigi Corvaglia
Luigi Corvaglia Giuliana Simonazzi3
Giuliana Simonazzi3 Lucia Paolini
Lucia Paolini