- 1Nephrology and Dialysis Unit, Department of Pediatrics, IRCCS Azienda Ospedaliero-Universitaria of Bologna, Bologna, Italy
- 2Nephrology, Dialysis and Transplantation Unit, Department of Experimental, Diagnostic and Specialty Medicine, IRCCS Azienda Ospedaliero-Universitaria of Bologna, Bologna, Italy
In the field of medical care, successful transition from pediatric-centered to adult-oriented healthcare can provide a sense of continuity in the development of youth, and prepare them to accept responsibility for and manage their own chronic kidney condition in complete autonomy. The so-called transition process requires the presence of some basic aspects: a multidisciplinary team, which acts as a bridge between child and adult services; a comprehensive clinical, cognitive, psychological, and social change for the young people; the involvement of family and caregivers. Within the framework of transition and chronicity during the developmental age, we selected international papers explaining models which agreed on some important steps in the transition process, although many differences can be observed between different countries. In fact, in Europe, the situation appears to be heterogeneous as regards certain aspects: the written transition plan, the educational programmes, the timing of transfer to adult services, the presence of a transition coordinator, a dedicated off-site transition clinic. We then analyzed some studies focusing on patients with renal diseases, including the first to contain a standardized protocol for transition which was launched recently in the USA, and which seems to have already achieved important positive, although limited, results. In Italy, the issue of transition is still in its infancy, however important efforts in the management of chronic kidney disease have already been initiated in some regions, including Emila Romagna, which gives us hope for the future of many young people.
Introduction
An Overview of Transitional Care
The term transitional care is a heterogeneous concept which incorporates a series of steps aimed at ensuring the coordination and continuity of care for patients who are transferred from one centre to another or between different levels of intensity of care (1–3). The starting point is the integration of the various professional roles, settings, and healthcare pathways involved. Therefore, the model of “intermediate care” provides a bridge, for example between the hospital and the home, or between pediatric and adult services, within which two very different settings synergistically create a process of total patient care (1, 4, 5). Transition, therefore, implicates the passage from a child-centered to an adult-centered health system, with the aim of preparing adolescents to take responsibility for and manage their own health problems (6–8). Due to the progressive increase in the number of adolescents suffering from chronic diseases and the higher survival rates of a large number of children and adolescents affected by chronic diseases necessitating special care (SiQuAs-VRQ, 2014), the concept of transitional care has become ever more emergent over the last few years. In Italy, it is estimated that around 15–18% of adolescents suffer from a chronic illness; of these, ~8-900,000 have only one disease, while circa 100-150,000 have at least two (9). Among these, according to the National Plan for Chronicity (PNC) elaborated by the Italian Ministry of Health (10), per year, there are ~30–50 new cases requiring dialysis, with the prospect of rapid access to transplantation. Since the concept of transitional care was creating terminological confusion in the scientific literature, the Italian Society for Quality Healthcare (SiQuAs-VRQ) organized a project-event called “Transitional Care” in 2014, which was aimed at defining a precise topic of interest, namely the transition of healthcare for patients with chronic diseases from the pediatric to the adult age.
In order to have a better understanding of the current state of transitional care, we searched the PubMed database for articles relevant to the topic: the transition of adolescents and young adults with chronic diseases to adult services; we then created a subgroup of articles related specifically to adolescents and young adults with chronic or end-stage renal disease, with or without a transplant, who were “in transition” to adult services. As numerous articles related to chronic diseases were available, we narrowed our selection criteria by including only the articles which considered the following: studies which had applied the existing guidelines in the planning and implementation of their transition process (more specifically, if there was a written/verbal protocol to follow, a specialized transition team, dedicated transition clinics, involvement of specific roles i.e., a psychologist/psychotherapist, a coordinator etc.); studies representative of the main countries where the international transition guidelines for pediatric patients have been applied; studies which evaluated the efficacy of transition from a medical (adherence, transplant success, reduced hospitalization), psycho-social (readiness, degree of satisfaction, quality of life) and logistic (dedicated structures, costs, feasibility) point of view; studies which considered participation in “camps” as a measure of effectiveness of the transition process; previous reviews of retrospective studies which included the abovementioned criteria. We excluded the articles which did not contain pertinent information: studies which evaluated the outcomes of pediatric patients after their transition to adult services, not during the process; studies which were similar in terms of authors, results and country of origin; studies which had not applied the international guidelines for the transition of pediatric patients; studies with only one outcome (graft loss or hospitalization or medical adherence) without considering psycho-social factors (readiness, degree of satisfaction, quality of life), costs or feasibility; retrospective studies which provided scanty information (data collection, sample size, outcomes, etc.). We selected 37 articles based on the abovementioned criteria and excluded nine.
Chronicity During the Developmental Age
The management of chronic illnesses differs greatly between adolescent and adult patients. Primarily, the constantly changing needs of patients as they develop creates healthcare complexities requiring medical care and social welfare interventions, possibly long-term, which are organized on the basis of personalized plans and a combination of primary and hospital care. Furthermore, it is possible that the disease and/or disability can cause oftentimes irreversible developmental delay, which needs to be prevented. Finally, the need to facilitate the inclusion of youth with chronic diseases in academic, recreational, and social situations constitutes an important component of welfare interventions (10). For this reason, the PNC supports the empowerment of all of the parties involved, in such a way as to help patients and their families through the acquisition of competences and trust, so that the patient as a “person” becomes expert in navigating their personal history of “coexistence” with chronicity (10). The presence of a multi-professional team comprising doctors, nurses, dieticians, social workers, play therapists, psychologists, and educators has been seen to be the most efficacious way of minimizing their disability and maximizing their potential. The support that children and their families receive from a multi-professional team, rather than from a single treating physician, is the main difference between pediatric and adult healthcare (11).
Transition: A Challenge for the Adolescent
For youth with chronic diseases, the transition pathway toward adulthood represents an additional complexity. The difficulty in treating adolescent patients with chronic diseases lies in the series of their physical, psychological, and emotional changes, which complicate the management of the transition as a process of care. In fact, for many children and their families, this developmental transition, which begins at around 13 to 14 years of age and continues until late adolescence or early adulthood, can be an especially stressful process, particularly because the illness makes the adolescents more dependent on their parents and healthcare staff, which hinders their physiological individuation. Consequently, one of the first reactions we see in clinical practice is oppositional behavior accompanied by outbursts of anger and the resulting lack of treatment adherence from patients (12, 13).
Guidelines and Assessment Tools
What the Literature Tells Us About the Transition of Patients With Chronic Diseases
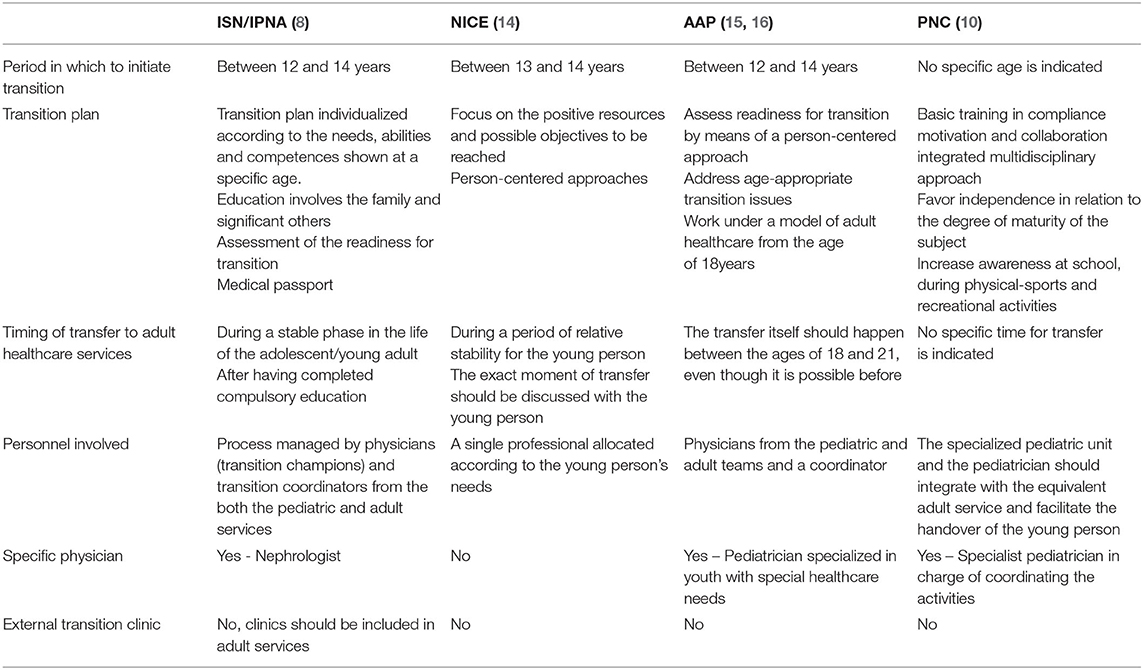
In its most desirable form, the transfer of a pediatric patient from a model of pediatric care initially managed by the caregiver to the self-management of the disease in an adult context is an event which occurs at the end of a process (7). We compared the different guidelines available for the management of the care pathway during the transition of chronic patients in general (Table 1), namely those from the American Academy of Pediatrics (AAP) (15, 16) and the United Kingdom National Institute for Health and Care Excellence (NICE) (14), which include recommendations concerning both the preceding and successive phases of the transfer itself. In particular, the AAP (16) has developed an approach known as “Six Core Elements of Health Care Transition,” which can be applied to different care models. The six elements include:
1. Transition policy;
2. Transition tracking and monitoring;
3. Transition readiness;
4. Transition planning;
5. Transfer and/or integration into adult-centered care;
6. Transition completion and ongoing care with adult clinician.
Furthermore, the PNC highlights the “lack of clear indications regarding the process of ‘transition’ from the pediatric to the adult age or the age at which said transition should occur. On the other hand, there are no shared indications concerning the fact that all pediatric patients should be followed exclusively by pediatric centers and not by adult services.” Nevertheless, the lines of intervention for the management of pediatric chronicity must consider the peculiar characteristics related to childhood. Thus, the PNC envisages the identification of four macro activities:
(1) continuity of care for children with chronic health conditions;
(2) the role of the family;
(3) age-specific relational environments (school, sport, social);
(4) the passage from pediatric to adult management (10).
The different guidelines contain some common characteristics pertaining to the nature and phases of the transition process, which can be considered useful in the approach to nephrological patients too: start planning the transition process (14–17), transfer to the adult service (17). All the recommendations focus on the importance of the presence of a transition coordinator: the AAP guidelines, NICE, and PNC (10) refer to social workers, but make no specifications for the inclusion of psychologists and/or psychotherapists in the transition team. Furthermore, it is estimated that only around half of the European centres have a formalized transition care unit (18). Although programmes envisage high resource intensity, the development and running costs of a multidisciplinary transition programme can be compensated for by the positive outcomes of the patients involved (19).Transition should begin as soon as possible, with gradual processes of support, education, and preparation (14).
Multidisciplinary teams within dedicated clinics are able to help youth deal with the situations connected to transition (20). However, only a few of the guidelines make reference to this (8).
The lack of communication between hospital healthcare teams, patients, and primary care providers (usually pediatricians) is still a cause for concern (21). As regards transplanted children, who generally have a lifelong care plan to follow, dedicated transition appears inevitable. The medical passport represents an attempt to solve such problems by permitting the identification of individuals at risk, preventing premature transition, and improving long-term results (20).
What the Literature Tells Us About the Transition of Patients With Renal Disease
In nephropathic patients, some particular forms of treatment, such as dialysis, transplantation, and the risk of acute rejection and graft loss (22, 23) require long periods of hospitalization, isolation from peers, and interrupted schooling, which prolong the form of attachment to reference figures characterized by dependence on adults. In some cases, advanced renal disease can be associated with reduced cognitive capacity and increased psychological distress (24, 25). Of note is the increased risk of graft failure associated with older age (26); in fact, renal transplantation in adolescents and young adults has a poorer outcome compared to younger age groups (27). Transition plays an important role during this developmental period (28, 29). A child with kidney disease should therefore be treated by a multidisciplinary clinical and surgical team with specific pediatric competences, able to create a treatment plan comprehensive of conservative and nutritional requirements and corrective actions for associated anomalies and, at a later stage, dialysis and transplantation in an adequate setting (10).
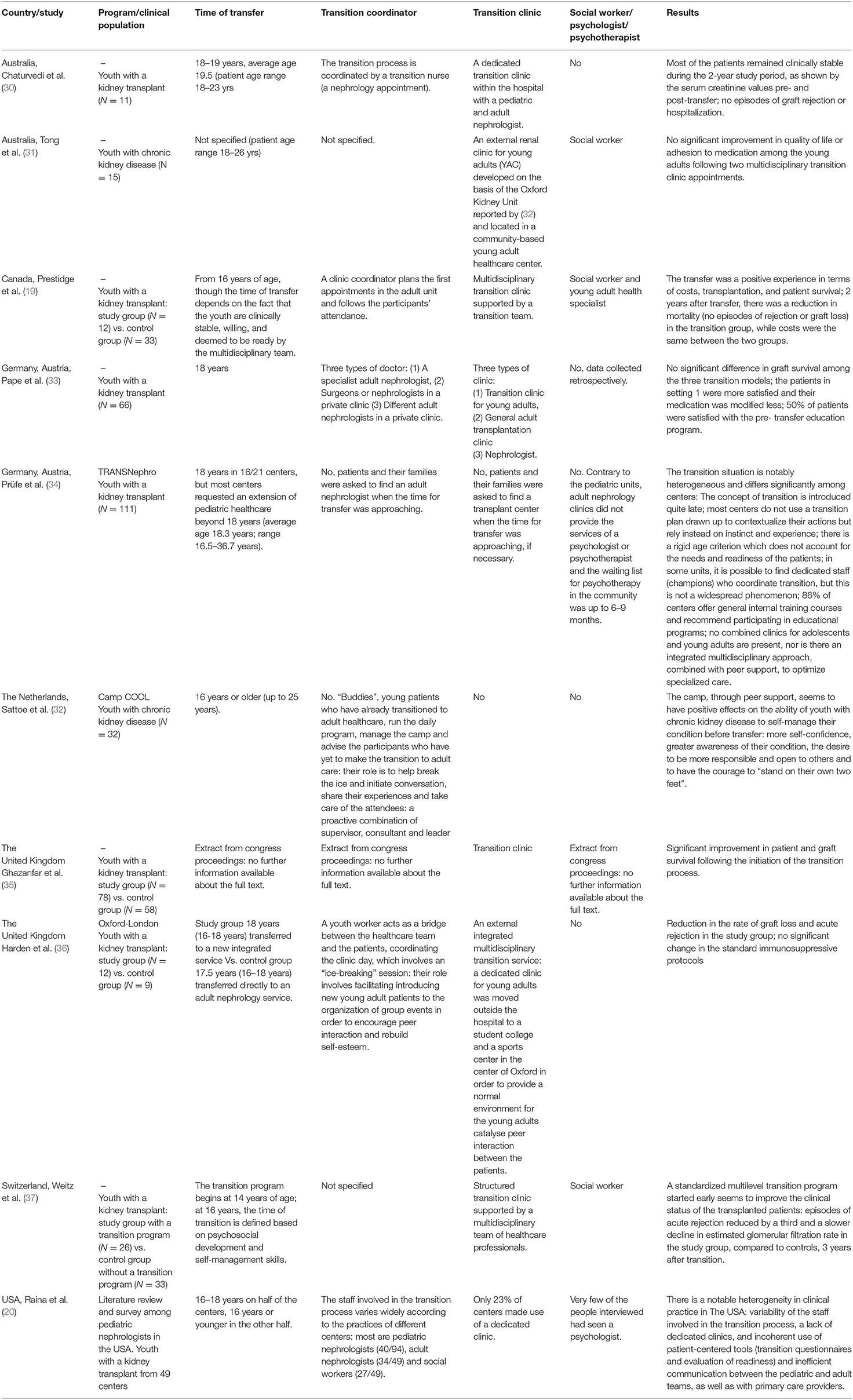
Until well into 2016, the published articles on transitional care were subdivided according to their field of application: diabetes, arthritis, cystic fibrosis. Only over the last decade, have research efforts focused on analyzing the phenomenon of transition in the pediatric populations affected by kidney diseases, as described in the selected papers summarized in Table 2. In The UK, Harden et al. (36) performed a study aimed at evaluating the efficacy of the transition process involving youth and young adults with kidney disease; in Canada, Prestidge et al. (19) described a positive transition experience in terms of costs, transplantation, and survival of patients with a kidney transplant. Tong and collaborators (31) tried to develop a new transition clinic (YAC), based on the Oxford Kidney Unit model (36). The qualitative results suggest that the learning of self-management strategies through peer groups, encouragement, and a sense of responsibility can strongly motivate the patient toward autonomy. The possibility to conduct group activities in locations outside the clinical setting can also reduce the young person's health anxiety. Other studies included the degree of patient satisfaction in their indices of outcome (30, 33), concluding that in order to achieve a good transition result, planning must begin as soon as possible and monitoring must continue after transition is complete (30, 37). In particular, Chaturvedi et al. (30) suggest involving young patients in the planning phase of their transition. In Germany, the same result was obtained with pediatric renal transplant populations (34, 38). The abovementioned study was part of the TRANSNephro trial, the first randomized controlled trial in Germany and Austria to focus on transitional care. The objectives of the transition process for children were centered on self-care, autonomy, and treatment adherence (38). Although the majority of the centres involved offered educational programmes, none of them utilized tools for assessing their transition readiness (35). In the TRANSNephro study, age at transition was 18 years, yet most centres requested a special dispensation to extend pediatric care beyond that age; the reasons were medical in nature (transplant) and/or psychosocial (family, school, professional training). The aspects considered as fundamental for transition suitability included: autonomy, a sense of responsibility, emotional stability, cognitive maturity, knowledge of the disease and adherence to treatment. The role of emotional stability was defined as a prerequisite for acting responsibly and maturely, the lack of which was considered a risk factor. The key question should not be “How old is the patient?” but “How ready is the patient to transfer to adult healthcare?” (39).
The International Society of Nephrology together with the International Pediatric Nephrology Association (ISN/IPNA) elaborated specific guidelines for the transition of pediatric patients with kidney disease, approved for implementation in the United Kingdom, The USA, Australia, and Egypt. In Italy, the PNC elaborated by the Ministry of Health (10) compiled an initial list of chronic diseases, for the majority of which, at present, there are no specific national plans of action.
Recently, a group of American researchers (20) conducted a literature review and a survey among pediatric nephrologists in The USA, with the objective of analyzing the current state of transitional care (Table 2). This led to the creation of the transition protocol “RISE to transition,” for patients with a kidney transplant. The protocol is aimed at improving: graft survival, compliance to treatment, and quality of life. It comprises four areas of competency that the patient must reach before the moment of transition:
1. Recognition - awareness of their disease process, the healthcare system and the reason for transplant;
2. Insight - awareness of their own emotional needs;
3. Self-reliance - autonomous treatment planning and participation;
4. Establishment - healthy lifestyle choices, life-long adherence to medications and follow-up, the acquisition of psychosocial skills.
Competency in these areas forms the basis for effective transition. The key players are: the patient and family; the pediatric team; the transition team; the adult team; the primary care provider. The protocol also refers to:
1. The medical passport.
2. Complete medical records.
3. Medical records relating to the transplant.
4. Transition readiness assessment, performed every 6 months.
The transition process is divided into three stages, depending on patient age:
1. Pre-transition stage (14–18 years): dedicated to the education of the family.
2. Active transition stage (18–21 years): the pediatric team initiates the transition process, assessing the needs and competences of the patient and family in order to personalize the process. The transition team assesses patient progress in terms of the four areas of competency and acts as a bridge between the pediatric and adult services. During this period, assessments are carried out every 6 months until the patient is deemed autonomous.
3. Post-transition stage (21–26 years): the adult team becomes the primary team. Six months after transition, a meeting between the two teams is planned to discuss the patient's progress, and this is repeated until the patient is 26 years of age (20). As this is a complex phenomenon, the current national transitional care project (SIQuAS-VRQ, 2014) was created with the objective of delivering homogeneous care during the passage from the pediatric to the adult age and was developed according to the best practice guidelines proposed by Donabedian (40): active listening, the ability to work in a team, organizational quality, and relational quality. The typology of care must also take into consideration the long history of the disease and the considerable experience each patient has in dealing with healthcare services and professionals (SIQuAS-VRQ, 2014). The project, which is consistent with the PNC guidelines, is articulated in three phases which proceed in parallel:
1. The establishment of a “Control Group” and a Technical Advisory Committee, comprising various medical scientific societies and health charities, whose duty it is to construct hypotheses regarding the functional and quality requirements of a “transition service”;
2. The mapping of the experiences present on the territory by means of a questionnaire aimed at gathering information regarding the current management of transitional care;
3. The collection of the experimentations of the regional realities (Piedmont, Marche and Apulia) which have been instrumental in defining concrete organizational models.
Currently, there are four nosological areas of interest (oncology, diabetology, rare diseases and respiratory diseases), which are the subject of experimentation in the three aforementioned Italian regions. To these, cystic fibrosis, nephrology, and rheumatology have been added.
The most frequently studied aspect concerns the “taking charge” of the patients, using multiprofessional and interdisciplinary modalities, with the aim of building a real “transition group” which plans the “transition service.”
In this phase, the investigative activities involve:
(1) The centrality of the subjects;
(2) The concept of transition viewed as a long-term process;
(3) The relevance of the temporal dimension of the illness experience;
(4) The co-construction of therapeutic relationships and diagnostic and care pathways.
If transition is to be successful, it is important to evaluate the readiness of the young person and their family. Different tools exist for use in the pediatric populations affected by kidney disease:TRxANSITION Scale (41); Youth Quiz from the On Trac programme (42); Transition Readiness Assessment Questionnaire (TRAQ) (43); Readiness for Transition Questionnaire (RTQ) (43). In agreement with the general principles of the ISN/IPNA guidelines (2011), the TRxANSITION Scale (41) has been considered suitable for the evaluation and monitoring of patient and caregivers' progress in terms of reaching the objectives of transition through 10 domains (Type of illness, Medications, Adherence, Nutrition, Self-management, Informed-reproduction, Trade/school issues, Insurance issues, Ongoing support, New health providers). Based on the patient and caregivers' responses on the TRxANSITION Scale, the multidisciplinary team decides the most suitable time for transition.
Summary
Transitional care is an essential step for patients with kidney disease. In Europe, there are numerous heterogeneous general models for approaching transitional care for patients with chronic diseases, so we decided to evaluate them in terms of their healthcare-related and organizational aspects, and how these aspects could be better integrated in the field of nephrology. The most evident differences include the timing of transfer, the presence of a coordinator, and the logistics. The greatest limitation, which reduces their applicability, is the absence of written guidelines. The American experience can be seen as one of the first good examples of transition for patients suffering from kidney disease and although there are inevitable differences born from specific context-related cultural characteristics, it must be considered a milestone. In Italy, the situation appears to be considerably heterogeneous and, in many respects, disorganized. However, the transition process has already been activated in at least three regions, including Emila-Romagna, and has been applied to various chronic diseases of the developmental age, with the same objectives: the inclusion and empowerment of the patient, and the same multidisciplinary structure.
It is evident that, to date, transitional care is not only an objective to reach, but a process still in its developmental stages that has to deal with the restrictions and limits imposed by the different legislative procedures and organization of healthcare services seen in different countries, as well as within individual territories. Nonetheless, we agree on the four areas of competency that the patient must reach before the moment of transition: awareness of their disease process, awareness of their own emotional needs, autonomous treatment planning and participation, healthy lifestyle choices.
We know with certainty that when the guidelines are applied it is possible to increase the effectiveness criteria: quality of life, survival, compliance and reduce drop-out. Furthermore, the degree of patient satisfaction in their indices of outcome rises.
Within this reference framework, the healthcare objectives of patients with chronic diseases, which cannot include recovery, concern the overall definition of the clinical picture, functional state, control of symptoms, prevention of disability and improvement in quality of life. In order to achieve this, it is necessary to redefine the care pathways able to take charge of the patient in the long term, guaranteeing continuity of care and the integration of social and health interventions by both the pediatric and adult services.
Author Contributions
DS and VC contributed to the conception and design of the work, perfomed the literature search, and wrote the first draft of the manuscript. APa, GL, and APe contributed to the conception and design of the work, and critically reviewed the manuscript. CB, CL, FM, and MB critically reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank Alexandra Teff for providing the English version of the article.
Abbreviations
SiQuAs-VRQ, Società Italiana per la Qualità dell'Assistenza Sanitaria; UNICEF, United Nations International Children's Emergency Fund; PNC, Piano Nazionale della Cronicità; AAP, American Academy of Pediatrics; NICE, United Kingdom National Institute for Health and Care Excellence; ISN, International Society of Nephrology; IPNA, International Pediatric Nephrology Association; USA, United States of America; ONU, Organizzazione delle Nazioni Unite; TRAQ, Transition Readiness Assessment Questionnaire; RTQ, Readiness for Transition Questionnaire; YAC, Young Adult Clinic; COOL, Communicatie (Communication), Ontplooiing (Self-development), Ontmoeting (Meeting), Lol (Fun).
References
2. Somme D, Hébert R, Bravo G, Blanchard F, Saint-Jean O. The individualized service plan as a clinical integration tool: qualitative analysis in the Quebec PRISMA experiment. Int J Integr Care. (2007) 7:e52. doi: 10.5334/ijic.215
3. Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. (2003) 51:549–55. doi: 10.1046/j.1532-5415.2003.51185.x
4. Compagni A, Tediosi F, Tozzi V. L'integrazione tra ospedale e territorio nelle Aziende Sanitarie. In: Anessi Pessina E, Cantù E, editors. Rapporto OASI 2010. Milano: L'aziendalizzazione della sanità in Italia (2011).
5. Melis RJ, Olde Rikkert MG, Parker SG, van Eijken MI. What is intermediate care? BMJ. (2004) 329:360–1. doi: 10.1007/s11739-007-0025-y
6. Bell LE, Bartosh SM, Davis CL, Dobbels F, Al-Uzri A, Lotstein D, et al. Adolescent transition to adult care in solid organ transplantation: a consensus conference report. Am J Transplant. (2008) 8:2230–42. doi: 10.1111/j.1600-6143.2008.02415.x
7. Blum RW, Garell D, Hodgman CH, Jorissen TW, Okinow NA, Orr DP, et al. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health. (1993) 14:570–6. doi: 10.1016/1054-139X(93)90143-D
8. Watson AR, Harden P, Ferris M, Kerr PG, Mahan J, Ramzy MF. Transition from pediatric to adult renal services: a consensus statement by the international society of nephrology (ISN) and the international pediatric nephrology association (IPNA). Pediatr Nephrol. (2011) 26:1753–7. doi: 10.1007/s00467-011-1981-z
9. UNICEF. La condizione dell'infanzia nel mondo. (2012). Available online at: https://www.unicef.it/Allegati/SOWC_2012_ITA.pdf (accessed January, 2020).
10. Ministero della Salute. Direzione Generale Della Programmazione Sanitaria. Piano Nazionale Della Cronicità. Accordo tra lo Stato, le Regioni e le Province Autonome di Trento e di Bolzano del 15 Settembre. (Rome) (2016).
11. Watson AR. Problems and pitfalls of transition from pediatric to adult renal care. Pediatr Nephrol. (2005) 20:113–7. doi: 10.1007/s00467-004-1763-y
12. Durston S, Casey BJ. What have we learned about cognitive development from neuroimaging? Neuropsychologia. (2005) 44:2149–57. doi: 10.1016/j.neuropsychologia.2005.10.010
13. Giedd JN. The teen brain: insights from neuroimaging. J Adolesc Health. (2008) 42:335–43. doi: 10.1016/j.jadohealth.2008.01.007
14. National Institute for Health and Care Excellence. Transition From Children's to Adults' Services for Young People Using Health or Social Care Services (NICE guideline NG43) (London) (2016).
15. Cooley WC, Sagerman PJ, American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians; Transitions Clinical Report Authoring Group. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. (2011) 128:182–200. doi: 10.1542/peds.2011-0969
16. White PH, Cooley WC, Transitions Clinical Report Authoring Group; American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. (2018) 142:e20182587. doi: 10.1542/peds.2018-3610
17. Francis A, Johnson DW, Craig JC, Wong G. Moving on: transitioning young people with chronic kidney disease to adult care. Pediatr Nephrol. (2017) 33:973–83. doi: 10.1007/s00467-017-3728-y
18. Forbes TA, Watson AR, Zurowska A, Shroff R, Bakkaloglu S, Vondrak K, et al. European paediatric dialysis working group adherence to transition guidelines in European paediatric nephrology units. Pediatr Nephrol. (2014) 29:1617–24. doi: 10.1007/s00467-014-2809-4
19. Prestidge C, Romann A, Djurdjev O, Matsuda-Abedini M. Utility and cost of a renal transplant transition clinic. Pediatr Nephrol. (2012) 27:295–302. doi: 10.1007/s00467-011-1980-0
20. Raina R, Wang J, Krishnappa V. Structured transition protocol for children with cystinosis. Front Pediatr. (2017) 5:191. doi: 10.3389/fped.2017.00191
21. Raina R, Wang J, Krishnappa V, Ferris M. Pediatric renal transplantation: focus on current transition care and proposal of the “RISE to transition” protocol. Ann Transplant. (2018) 23:45–60. doi: 10.12659/AOT.906279
22. Annunziato RA, Kim SK. Assessment in transition: options, challenges, and future directions. Pediatr Transplant. (2015) 19:446–8. doi: 10.1111/petr.12521
23. Watson AR. Non-compliance and transfer from paediatric to adult transplant unit. Pediatr Nephrol. (2000) 14:469–72. doi: 10.1007/s004670050794
24. Johnson RJ, Warady BA. Long-term neurocognitive outcomes of patients with end-stage renal disease during infancy. Pediatr Nephrol. (2013) 28:1283–91. doi: 10.1007/s00467-013-2458-z
25. Wong CJ, Moxey-Mims M, Jerry-Fluker J, Warady BA, Furth SL. CKiD (CKD in children) prospective cohort study: a review of current findings. Am J Kidney Dis. (2012) 60:1002–11. doi: 10.1053/j.ajkd.2012.07.018
26. Foster BJ. Heightened graft failure risk during emerging adulthood and transition to adult care. Pediatr Nephrol. (2015) 30:567–76. doi: 10.1007/s00467-014-2859-7
27. Smith JM, Ho PL, McDonald RA. North American pediatric renal transplant cooperative S. Renal transplant outcomes in adolescents: a report of the North American pediatric renal transplant cooperative study. Pediatr Transplant. (2002) 6:493–9. doi: 10.1034/j.1399-3046.2002.02042.x
28. Samuel SM, Nettel-Aguirre A, Hemmelgarn BR, Tonelli MA, Soo A, Clark C, et al. Graft failure and adaptation period to adult healthcare centers in pediatric renal transplant patients. Transplantation. (2011) 91:1380–5. doi: 10.1097/TP.0b013e31821b2f4b
29. Samuel SM, Nettel-Aguirre A, Soo A, Hemmelgarn B, Tonelli M, Foster B. Avoidable hospitalizations in youth with kidney failure after transfer to or with only adult care. Pediatrics. (2014) 133:e993–1000. doi: 10.1542/peds.2013-2345
30. Chaturvedi S, Jones CL, Walker RG, Sawyer SM. The transition of kidney transplant recipients: a work in progress. Pediatr Nephrol. (2009) 24:1055–60. doi: 10.1007/s00467-009-1124-y
31. Tong A, Gow K, Wong G, Henning P, Carroll R. Patient perspectives of a young adult renal clinic: a mixed-methods evaluation. Nephrology. (2015) 20:352–59. doi: 10.1111/nep.12396
32. Sattoe JN, Jedeloo S, van Staa A. Effective peer-to-peer support for young people with end-stage renal disease: a mixed methods evaluation of camp COOL. BMC Nephrol, (2013) 14:279
33. Pape L, Lammermuhle J, Oldhafer M, Blume C, Weiss R, Ahlenstiel T. Different models of transition to adult care after pediatric kidney transplantation: a comparative study. Pediatr Transplant. (2013) 17:518–24. doi: 10.1111/petr.12102
34. Prüfe J, Dierks ML, Bethe D, Oldhafer M, Müther S, Thumfart J, et al. Transition structures and timing of transfer from paediatric to adult-based care after kidney transplantation in Germany: a qualitative study. BMJ Open. (2017) 7:e015593. doi: 10.1136/bmjopen-2016-015593
35. Ghazanfar A, Roberts D, Palmer A, Shenoy M, Riad HN. Transfer vs transition in paediatric renal allograft recipients; experience over two decades. Pediatr Transplant, (2011) 15:41–439.
36. Harden PN, Walsh G, Bandler N, Bradley S, Lonsdale D, Taylor J, et al. Bridging the gap: an integrated paediatric to adult clinical service for young adults with kidney failure. BMJ. (2012) 344:e3718. doi: 10.1136/bmj.e3718
37. Weitz M, Heeringa S, Neuhaus TJ, Fehr T, Laube GF. Standardized multilevel transition program: does it affect renal transplant outcome? Pediatr Transplant. (2015) 19:691–7.
38. Kreuzer M, Prüffe J, Bethe D, Vogel C, Grosshennig A, Koch A, et al. Study group of the German society for pediatric N. The TRANSNephro-study examining a new transition model for post-kidney transplant adolescents and an analysis of the present health care: study protocol for a randomized controlled trial. Trials. (2014) 15:505. doi: 10.1186/1745-6215-15-505
39. Zhang LF, Ho JS, Kennedy SE. A systematic review of the psychometric properties of transition readiness assessment tools in adolescents with chronic disease. BMC Pediatr. (2014) 14:4. doi: 10.1186/1471-2431-14-4
40. Donabedian A. Evaluating the quality of medical care. 1996. Milbank Q. (2005) 83:691–729. doi: 10.1111/j.1468-0009.2005.00397.x
41. Ferris ME, Harward DH, Bickford K, Layton JB, Ferris MT, Hogan SL, et al. A clinical tool to measure the components of health-care transition from pediatric care to adult care: The UNC TRxANSITION scale. Ren Fail. (2012) 34:744–53. doi: 10.3109/0886022X.2012.678171
42. Paone MC, Wigle M, Saewyc E. The ON TRAC model for transitional care of adolescents. Prog Transplant. (2006) 16:291–302. doi: 10.1177/152692480601600403
Keywords: transition, kidney, chronic, multidisciplinary, pediatric
Citation: Scarponi D, Cammaroto V, Pasini A, La Scola C, Mencarelli F, Bertulli C, Busutti M, La Manna G and Pession A (2021) Multidisciplinarity in Transition Pathways for Patients With Kidney Disease: The Current State of Play. Front. Pediatr. 9:689758. doi: 10.3389/fped.2021.689758
Received: 01 April 2021; Accepted: 10 August 2021;
Published: 20 September 2021.
Edited by:
Corrado Romano, Oasi Research Institute (IRCCS), ItalyReviewed by:
Dhurata Ivziku, Campus Bio-Medico University, ItalyYuko Ishizaki, Kansai Medical University, Japan
Copyright © 2021 Scarponi, Cammaroto, Pasini, La Scola, Mencarelli, Bertulli, Busutti, La Manna and Pession. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrea Pasini, YW5kcmVhLnBhc2luaUBhb3NwLmJvLml0
 Dorella Scarponi1
Dorella Scarponi1 Andrea Pasini
Andrea Pasini Claudio La Scola
Claudio La Scola Gaetano La Manna
Gaetano La Manna Andrea Pession
Andrea Pession