- 1Meuhedet Health Services, Tel Aviv-Yafo, Israel
- 2Department of Medicine, European University Cyprus, Nicosia, Cyprus
- 3Centro Médico Pere Grau, Barcelona, Spain
- 4Pediatria, Childcare Worldwide, Padova, Italy
- 5Department of Pediatrics, Medical University Graz, Graz, Austria
- 6Department of Paediatrics, University Hospital Ghent, Ghent, Belgium
- 7Department of Paediatrics, Regional Hospital AZ Damiaan, Ostend, Belgium
- 8Department of Hygiene and Epidemiology, Faculty of Public Health, Medical University of Varna, Varna, Bulgaria
- 9Andrija Štampar School of Public Health, School of Medicine, Univeristy of Zagreb, Zagreb, Croatia
- 10Department of Pediatrics, School of Medicine, National and Kapodistrian University of Athens, Athens, Greece
- 11Institute of Clinical Medicine, Medical Faculty, Vilnius University, Vilnius, Lithuania
- 12Department of Pediatrics and Pediatric Endocrinology and Diabetes, Medical College, University of Rzeszow, Rzeszow, Poland
- 13Department of Pediatrics, Hospital Beatriz Ângelo, Loures, Portugal
- 14Health Center Domžale, Domžale, Slovenia
- 15Department of Pediatrics, Shupyk National Medical Academy of Post-graduate Education, Kyiv, Ukraine
- 16Pediatria di Famiglia, Federazione Italiana Medici Pediatri FIMP, Naples, Italy
- 17Paediatric Clinic, Prague, Czechia
- 18Paediatric Clinic, Hagen, Germany
- 19Kinderaerzte Kurwerk, Burgdorf, Switzerland
- 20Paediatric Clinic, Budapest, Hungary
- 21Biostatistics Unit, Cyprus Institute of Neurology and Genetics, Nicosia, Cyprus
- 22Adelson School of Medicine, Ariel University, Ariel, Israel
- 23Maccabi Healthcare Services, Tel Aviv-Yafo, Israel
Background: During the COVID-19 pandemic, telemedicine use has increased within community pediatrics. This trend runs counter to reluctance to adaptation of the new mode of healthcare that existed prior to the pandemic. Little is known about what we can expect after the pandemic: if physicians will opt for telemedicine modalities and if tele-pediatrics will continue to be a significant mode of community pediatric care.
Objective: The goal of this study was to survey primary pediatric care providers as to their experiences and clinical decision making with telemedicine modalities prior to and during the COVID-19 pandemic, as well as their projected use after the pandemic ends.
Material and methods: Using the EAPRASnet database we surveyed pediatricians throughout Europe, using a web-based questionnaire. The survey was performed during the COVID-19 pandemic (June–July 2020), assessed telemedicine use for several modalities, prior to and during the pandemic as well as predicted use after the pandemic will have resolved. Participants were also surveyed regarding clinical decision making in two hypothetical clinical scenarios managed by telemedicine.
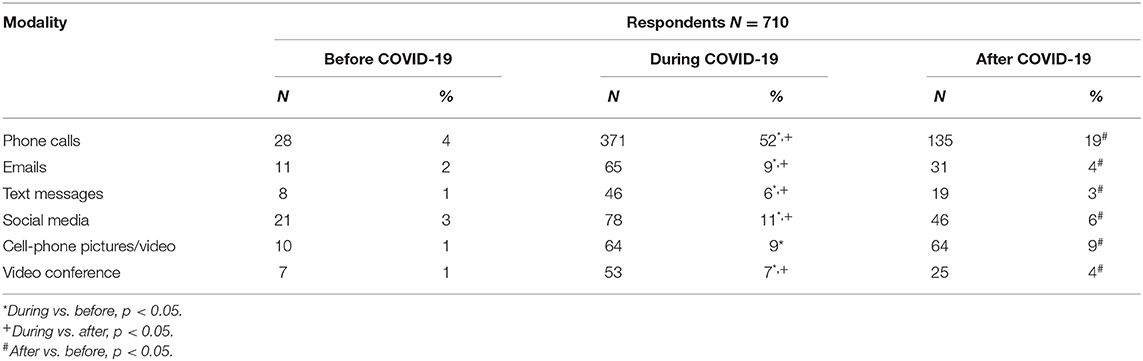
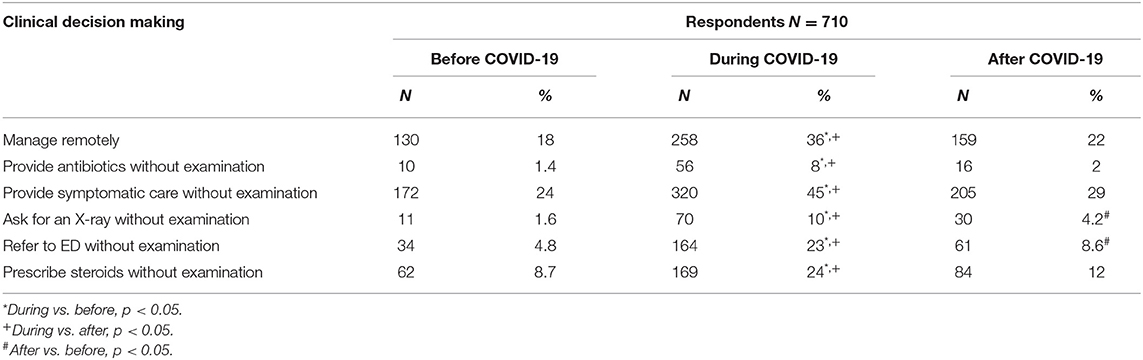
Results: A total of 710 physicians participated, 76% were pediatricians. The percentage of respondents who reported daily use for at least 50% of all encounters via telemedicine modalities increased during the pandemic: phone calls (4% prior to the pandemic to 52% during the pandemic), emails (2–9%), text messages (1–6%), social media (3–11%), cell-phone pictures/video (1–9%), and video conferencing (1–7%) (p < 0.005). The predicted post-pandemic use of these modalities partially declined to 19, 4, 3, 6, 9, and 4%, respectively (p < 0.005), yet demonstrating a prospectively sustained use of pictures/videos after the pandemic. Reported high likelihood of remotely treating suspected pneumonia and acute otitis media with antibiotics decreased from 8 to 16% during the pandemic to an assumed 2 and 4% after the pandemic, respectively (p < 0.005).
Conclusions: This study demonstrates an increased utilization of telemedicine by pediatric providers during the COVID-19 pandemic, as well as a partially sustained effect that will promote telemedicine use as part of a hybrid care provision after the pandemic will have resolved.
Introduction
Telehealth is the delivery of medical care by remote technology. Telemedicine refers particularly to the patient-physician clinical encounter via remote technology (1). Prior to 2020, these modalities of medical care have been slowly developing, with limited application and use in community pediatrics (2).
During the COVID-19 pandemic, unprecedented changes were made in the delivery of care in the ambulatory setting. Telehealth has proven its utility, as the use of telemedicine modalities increased during times of social distancing (3). In-person visits to the physician's office declined due to social distancing measures, and as such, telehealth practiced increased. Cautious of in-person interactions, many physicians and patients gravitated to the burgeoning telemedicine options as an alternative to in-office visits (4–6). National guidelines supported this trend, promoting telehealth to mitigate the pandemic while maintaining medical services (7–9).
The European Pediatric Association, Union of National European Pediatric Societies and Associations, demonstrated that pediatric care was sustained during the pandemic through the compensatory use of telemedicine. However, periodic health screening visits and screening programs were significantly reduced (10).
Telemedicine modalities, such as telephone calls, text messages, image or video transfers, video conferencing, or tele-diagnostic devices, are not identical to the traditional “hands-on” approach that physicians were trained to practice. Resistance to change is prevalent among physicians, as is controversy regarding the accuracy of telediagnosis. Previous reports describe overmedication with remote prescribing and raise concern of the deterioration of the physician-patient relationship and the service-oriented nature of medicine that may ensue (11–14).
Prior to the COVID-19 pandemic, telehealth has been promoted globally, at the very least, to provide care to improve accessibility to medical care, and at the most, to ultimately usher in a new model for ideal medical care (15). However, during 2020, telehealth has nevertheless “thrown down the gauntlet,” as it may, challenging today's physicians to accept new technology here and now, in providing primary care.
This change may alter physician's attitudes toward these new modalities to provide medical care and lead to greater utilization of telemedicine modalities in the future (16). Published results of a survey among Israeli physicians demonstrate a limited, albeit significant change in physician's willingness to adapt to telemedicine (17). Previous reports state that clinicians' acceptance of change is the pivotal factor to adaptation (18). The question remains, what lasting effect will the telemedicine experience during this pandemic have on physician behavior and the way care is delivered.
In this study we ascertain physician's impression of telemedicine, inquiring as to their use of telemedicine prior to and during the pandemic, as well as to what extent they expect telemedicine to remain part of their medical practice in the future, after the pandemic.
Methods
Study Sample
During the early phases of the pandemic, we utilized the EAPRAS network to conduct a survey of primary care pediatric care providers throughout the continent. The European Academy of Pediatrics Research in Ambulatory Settings Network (EAPRASnet), established in 2009, is a practice-based research network of primary care pediatricians affiliated with the European Academy of Pediatrics. The network has previously been involved in studies performed in primary care (19–22).
Data Collection
Data were collected using a web-based questionnaire that was posted on the home page of the EAPRASnet during June-July 2020. Only registered physicians were permitted to participate. Respondents were invited to participate via email using a mailing list that had been created for previous EAPRASnet projects. Pediatric care providers not belonging to the network were invited by national EAPRASnet coordinators to complete the questionnaire. Three reminders were sent out via email, and data were collected till the end of July 2020.
Socio-Demographic Details
Participants were asked for their gender, age, years in practice, medical specialty, and place of work.
Use of Telemedicine Modalities
The first part of the survey inquired about frequency of use of various telemedicine modalities prior to and during the epidemic, as well-expected use after the epidemic. Participants were asked specifically regarding phone calls, text messages, photo/video, email, and video conferencing.
Clinical Scenarios
The latter part of the survey consisted of two hypothetical scenarios and evaluated the decision to manage remotely.
Case 1, a suspected pneumonia, was presented as:
“The parents of a 7-year-old girl contact you and report that the child has had 4 days of high fever, cough, and nasal congestion. The child is not in distress, has mild anorexia, no vomiting and passed two loose stools today.”
Respondents were asked to rate the likelihood of making an empiric diagnosis, prescribing antibiotic treatment, prescribing symptomatic treatment, referring for a chest X-ray, referring to an emergency room, and in the case of wheezing, prescribing corticosteroids.
Case 2, a suspected otitis media, was presented as:
“The parents of a 2-year-old boy contact you and report that the child has had fever for 2 days, mild upper respiratory symptoms and left ear pain. The child is vigorous, eating well, had one loose stool, but slept poorly last night.”
Respondents were asked to rate the likelihood of making an empiric diagnosis, prescribing antibiotic treatment, and prescribing symptomatic treatment.
In both scenarios, respondents were to assume that the patient is known to the respondent and that there is no suspicion of COVID-19 for the case. Participants were asked to answer each question as if they would have practiced prior to the pandemic, currently practice during the pandemic and how they foresee themselves practicing after the pandemic. Responses were evaluated using a 5-point Likert scale ranging from “certainly not” to “certainly will.”
Data Analysis
Demographic data were presented as percentages of the total responses. Evaluation of the answers to the use of telemedicine technologies and responses to the two clinical scenarios between pre-, during and post-COVID-19 periods were compared using chi-square tests. Statistical significance was considered if the p-value was <0.05. Analyses were performed using R statistical software. The raw data is available in the Supplementary Material.
Results
Demographic Data
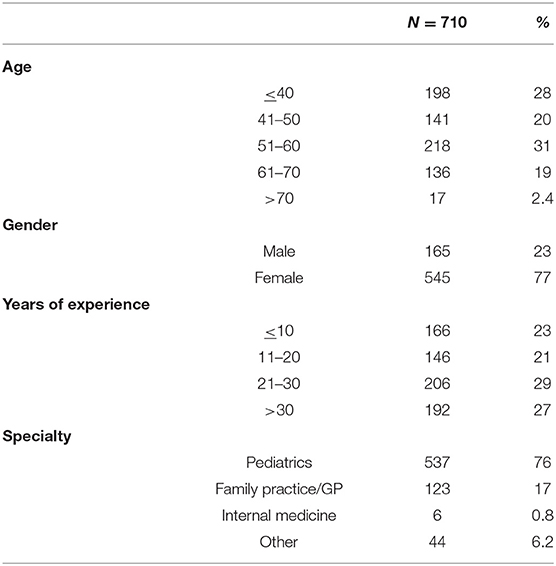
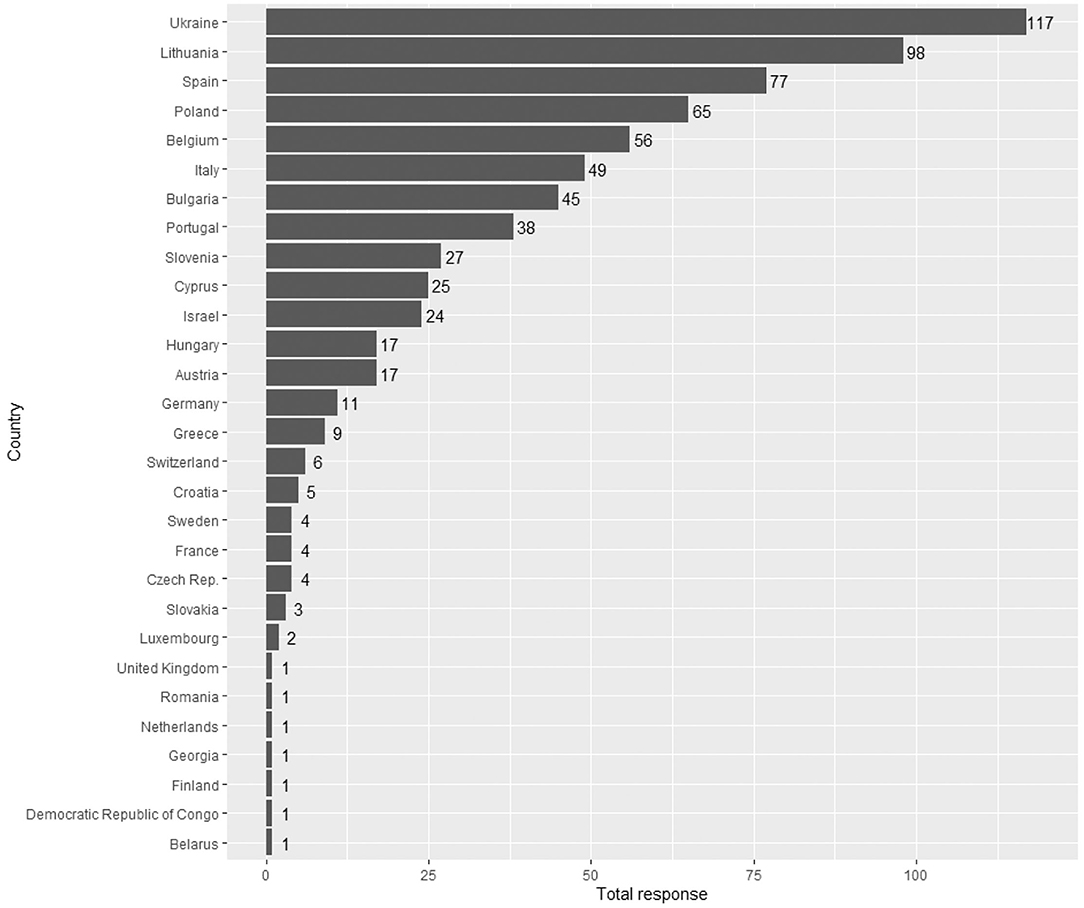
A total of 710 physicians responded to the survey, 77% were female, 76% were pediatricians, and 17% were family or general practitioners. Details regarding age, specialty and years of experience are presented on Table 1. Geographic distribution of respondents is presented on Figure 1.
Use of Telemedicine Modalities
Table 2 represents the use of telemedicine modalities for at least 50% of all daily encounters, including phone calls, emails, text messages, social media, cell-phone picture/video, and video conferencing. Usage is reported for prior to the pandemic and during the pandemic, as well as projected use after the pandemic.
Reported use of all telemedicine modalities increased significantly during the pandemic. For all modalities except for pictures/video, the degree of use is predicted to decrease after the pandemic yet remain significantly greater than prior to the pandemic. Post-pandemic predicted picture/video use is not only higher than pre-pandemic use but is predicted to remain at the same level as pandemic era use.
Scenario 1
Table 3 demonstrates clinical decision-making patterns for Scenario 1, the high-likelihood (likely to or certainly will) to manage remotely, and more specifically, to provide antibiotics, provide symptomatic care, refer for chest X-ray, refer to the ED, or prescribe steroids, all without having seen the patient in-person. All management options via telemedicine increased in frequency during the pandemic and yet all are predicted to reduce in frequency after the pandemic. The option to manage remotely is predicted to return to near pre-pandemic frequency, as are most management options. Only referrals to X-ray and the ED are predicted to have any increase in frequency sustained after the pandemic, when compared to pre-pandemic levels.
Scenario 2
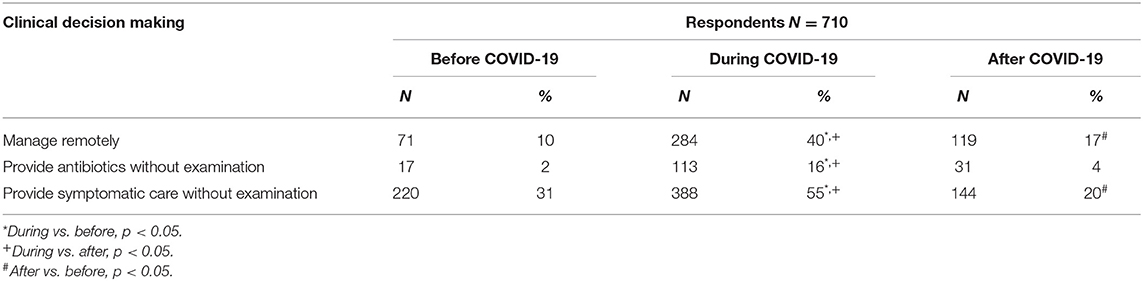
Table 4 demonstrates clinical decision-making patterns for Scenario 2, the high-likelihood (likely to or certainly will) to manage remotely, and more specifically, to provide antibiotics or symptomatic care without an in-person visit. Managing and treating via telemedicine increased significantly during the pandemic when compared to the pre-pandemic rates. Predicted use of telemedicine to manage and provide symptomatic care after the pandemic dropped significantly; however, when compared to pre-pandemic patterns, a significant increase in frequency is still sustained. Yet, post-pandemic antibiotic prescribing via telemedicine is predicted to return to near pre-pandemic levels, with no significant change predicted for the time after the pandemic, when compared to the pre-pandemic period.
Discussion
Our study demonstrates increased utilization of telemedicine for outpatient pediatric care during the COVID-19 pandemic. This increase was reported for all modalities considered: telephone calls, text messages, photo/video clips, and video calls, both when considering overall use, as well as when applied to specific clinical scenarios. These findings are consistent with other studies demonstrating physician's willingness to quickly adapt to telemedicine practices during the pandemic (3–6). However, for the first time, according to our knowledge, we could demonstrate that the use of all telemedicine modalities was predicted to remain in increased use after the pandemic, when compared to pre-pandemic levels. Experience during the pandemic has brought primary pediatric care to the forefront of telemedicine use.
A similar survey was previously used in a study of Israeli participants demonstrating a similar adaptation to telemedicine during the pandemic, yet it could not demonstrate similar willingness to adopt such practices after the pandemic (17). The difference between the studies may be the result of population variances. Additionally, the smaller sample size of the Israeli study (170 pediatricians) may not have had the power to detect significant changes for the post-pandemic phase. However, there may be more at hand. This European study was performed in June and July 2020, immediately after the completion of the Israeli study (May 2020). Though only 2 months following, we surmise that as physicians continued to use telemedicine, they became more comfortable with the modality thereby increasing their willingness to use it under “normal” circumstances.
As medical care advances during the twenty-first century, a hybrid of physician-patient interactions is developing, consisting of both in-person and telemedicine visits. However, whereas previous goals may have been created to utilize telemedicine to access hard to reach patients, crossing distances or physical barriers, current COVID-19 era use has forged a new ideal. Current telemedicine use has demonstrated that a significant percentage of physician-patient encounters does not require an in-person visit. The convenience of interacting remotely may increase efficiency for certain aspects of primary pediatric care.
Prior to the COVID-19 pandemic, strides in telemedicine were lagging for community pediatrics. Previous studies demonstrate physician's resistance to telemedicine utilization for reasons that include: lack of reimbursement, lack of infrastructure, non-familiarity with new modalities, discomfort with adopting new technologies, lack of confidence in the accuracy of tele-diagnosis, ease of missing or delaying critical diagnoses (such as medical emergencies or cancer), predisposition to ancillary testing and antibiotic prescribing with telemedicine use, lack of human interaction and impaired interpersonal dialogue that is critical to the physician-patient relationship (23–26).
The current COVID-19 pandemic has forced the primary care pediatrician's hand in utilization of telemedicine for a lack of a better alternative. We predict that this recent use will engender favorable attitudes toward the modality and lead to sustained use after the pandemic resolves.
We suggest that increased use during this era has increased familiarity, reduced “techno-phobia,” allowed for the learning of meaningful use, as well as demonstrated telemedicine's opportunities for efficiency and convenience. Experience during the pandemic allows for the development of meaningful use both on the individual and on the institutional level with the development of protocols and guidelines (27, 28).
Clinical scenarios that require the elucidation of physical findings for diagnostic accuracy pose a unique challenge to telemedicine. In the clinical scenarios we presented, physicians were willing to diagnose and prescribe empirically and without a physical exam only during the pandemic era and expect to return to in-patient visits after the pandemic. However, as new technologies offer “telediagnostics,” whereby part of the physical exam may be performed remotely, expectations are likely to change. New devices allow for auscultation, otoscopy, and visualization of the oropharynx via a remote device. Such devices have recently proven to provide high quality sound and images, on par with traditional medical devices (29, 30).
External physical findings, such as dermatologic exams have demonstrated increased utility for telemedicine use. Of all modalities surveyed in our study, images/video clips is the only modality to have predicted future use to remain sustained at pandemic levels. Advanced cell-phone camera technology has made it easy for taking and sending quality photographs. Studies have demonstrated that most skin lesions in pediatric primary care attention could be managed by tele-dermatology (31, 32).
However, increased utilization of telemedicine during COVID-19 for the clinical scenarios presented elucidate a particular need for caution with telemedicine: over-prescription. Previous studies have shown an increased frequency in antibiotic prescribing via telemedicine as compared to in-person visits (26). This tendency was confirmed by our presented case scenarios, with an increase in tele-prescribing during the pandemic. One may counter-argue, however, that our study of pandemic era practices presents a unique phenomenon during necessary social distancing, one that would not necessarily hold true during “normal” circumstances.
Our study has several limitations. Subjective and predictive reporting of use does not reflect the same accuracy as objective measures. Those who responded may not actually represent the opinions of all physicians in pediatric primary care. Participation was not proportional across all countries, and this may alter the study's ability to represent all of Europe. However, the limitation of the sample representativeness should be considered in the context of a first study of its kind, bringing data originating from primary care pediatricians. The pandemic spread varied in different countries, which may have influenced survey results. Future use are predictions made in the earlier part of the pandemic. Predictions may not be entirely accurate as attitudes may change as the pandemic persists and use of telemedicine (now for almost 2 years) is prolonged.
Our study did not explore chronic care, preventive care, or behavioral and developmental pediatrics. Unlike the clinical acute care scenarios presented, chronic care, preventive care and behavioral and developmental management may have greater utility for telemedicine (33, 34).
Our study did not explore the “other side of the examination table,” or how patients feel about telemedicine. Initial studies in pediatric telemedicine are optimistic, demonstrating significant patient satisfaction (35). This may drive pressure on physicians to provide a service that patients demand. Health maintenance organizations and other healthcare organizations may require such practice from their providers to save costs, improve quality of care, increase patient compliance or simply as a means to attract patients. The ethics of utilization must also be explored.
We suggest further studies that (1) assess via objective measures (2), differentiate between visits that focus more on a physical exam vs. those that relate to preventive, behavioral, developmental, or administrative issues, as well as chronic care (3), assess the use of pediatric telediagnostics, and (4) reassess over time.
Additional studies will be needed to assess the cost of telemedicine as well as physician and patient satisfaction with its use. Ethical use, the quality of its care and liability issues must be further explored, so that evidence-based guidelines and protocols can be developed to guide further telemedicine use (36, 37).
In conclusion, our study demonstrates an increased use of telemedicine in primary care pediatrics during the COVID-19 epidemic, as well as its predicted effect of greater telemedicine use in the future after the pandemic, compared to the pre-pandemic situation.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
SR and ZG conceived of and designed the study and composed the manuscript. KM performed statistical analysis. AH, DE, ST, and HD provided analytical and editorial review. AG, RP, AMu, GS, AV, AMa, JR, MS, MM, AD'A, GK, KG, CW, and PA coordinated data collection. All authors have discussed the results and contributed to the final manuscript.
Conflict of Interest
SR is a paid consultant of Tytocare.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2021.713930/full#supplementary-material
References
2. Harvey JB, Valenta S, Simpson K, Lyles M, McElligott J. Utilization of outpatient telehealth services in parity and nonparity states 2010–2015. Telemed J E Health. (2019) 25:132–6. doi: 10.1089/tmj.2017.0265
3. Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. (2020) 27:957–62. doi: 10.1093/jamia/ocaa067
4. Ting DSW, Carin L, Dzau V, Wong TY. Digital technology and COVID-19. Nat Med. (2020) 26:458–64. doi: 10.1038/s41591-020-0824-5
5. Elkbuli A, Ehrlich H, McKenney M. The effective use of telemedicine to save lives and maintain structure in a healthcare system: current response to COVID-19. Am J Emerg Med. (2020) 44:468–9. doi: 10.1016/j.ajem.2020.04.003
6. Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed J E Health. (2020) 26:571–3. doi: 10.1089/tmj.2020.29040.rb
7. Coronavirus Disease. Center for Medicare and Medicaid Services. (2020). Available online at: http://www.cms.gov (accessed January 7, 2021).
8. Israel Pediatric Association. Guidance for Community Pediatricians. (2020). Available online at: https://www.pediatrics.org.il/clinical-guidelines (accessed Jan 7, 2021).
9. Royal College of Paediatrics and Child Health (RCPCH). COVID-19 - Guidance for Community Settings. (2020). Available online at: https://www.rcpch.ac.uk/resources/covid-19-guidance-community-settings (accessed June 4, 2020).
10. Somekh I, Somech R, Pettoello-Mantovani M, Somekh E. Changes in routine pediatric practice in light of coronavirus 2019 (COVID-19). J Peds. (2020) 224:190–3. doi: 10.1016/j.jpeds.2020.05.053
11. Ehrich J, Namazova-Baranova L, Pettoello-Mantovani M. Introduction to “diversity of child health care in Europe: a study of the European paediatric association/union of national European paediatric societies and associations.” J Pediatr. (2016) 177S:S1–10. doi: 10.1016/j.jpeds.2016.04.036
12. Haimi M, Brammly Greenberg S, Baron Epel O, Waisman Y. Assessing patient safety in a pediatric telemedicine setting: a multi-methods study. BMC Med Inform Decis Mak. (2020) 20:63. doi: 10.1186/s12911-020-1074-7
13. Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. (2018) 24:4–12. doi: 10.1177/1357633X16674087
14. European Commission. Market Study on Telemedicine. (2018). Available online at: https://ec.europa.eu/health/sites/health/files/ehealth/docs/2018_provision_marketstudy_telemedicine_en.pdf (accessed January 18, 2021).
15. World Health Organization. Global Health Observatory (GHO) Data. (2016). https://www.who.int/gho/goe/telehealth/en/ (accessed January 7, 2021).
16. Gamus A, Chodick G. Telemedicine after COVID-19: the Israeli perspective. Isr Med Assoc J. (2020) 22:467–9.
17. Grossman Z, Chodick G, Reingold SM, Chapnick G, Ashkenazi S. The future of telemedicine visits after COVID-19: perceptions of primary care pediatricians. Isr J Health Policy Res. (2020) 9:53. doi: 10.1186/s13584-020-00414-0
18. Wade VA, Eliott JA, Hiller JE. Clinician acceptance is the key factor for sustainable telehealth services. Qual Health Res. (2014) 24:682–94. doi: 10.1177/1049732314528809
19. Del Torso S, Van Esso D, Gerber A, Drabik A, Hadjipanayis A, Nicholson A, et al. European academy of paediatrics research in ambulatory setting network (EAPRASnet): a multi-national general paediatric research network for better child health. Child Care Health Dev. (2010) 36:385–91. doi: 10.1111/j.1365-2214.2010.01086.x
20. Grossman Z, van Esso D, Del Torso S, Hadjipanayis A, Drabik A, Gerber A, et al. Primary care pediatricians' perceptions of vaccine refusal in Europe. Pediatr Infect Dis J. (2011) 30:255–6. doi: 10.1097/INF.0b013e3181faaaa3
21. Grossman Z, del Torso S, Hadjipanayis A, van Esso D, Drabik A, Sharland M. Antibiotic prescribing for upper respiratory infections: European primary paediatricians' knowledge, attitudes and practice. Acta Paediatr. (2012) 101:935–40. doi: 10.1111/j.1651-2227.2012.02754.x
22. van Esso D, del Torso S, Hadjipanayis A, Biver A, Jaeger-Roman E, Wettergren B, Nicholson A. Primary-secondary working group (PSWG) of European academy of paediatrics (EAP). Paediatric primary care in Europe: variation between countries. Arch Dis Child. (2010) 95:791–5. doi: 10.1136/adc.2009.178459
23. Sisk B, Alexander J, Bodnar C, Curfman A, Garber K, McSwain SD, et al. Pediatrician attitudes toward and experiences with telehealth use: results from a national survey. Acad Pediatr. (2020) 20:628–35. doi: 10.1016/j.acap.2020.05.004
24. Kane CK, Gillis K. The use of telemedicine by physicians: still the exception rather than the rule. Health Aff. (2018) 37:1923–30. doi: 10.1377/hlthaff.2018.05077
25. Olson CA, McSwain SD, Curfman AL. The current pediatric telehealth landscape. Pediatrics. (2018) 141:3. doi: 10.1542/peds.2017-2334
26. Ray KN, Shi Z, Gidengil CA, Poon SJ, Uscher-Pines L, Mehrotra A. Antibiotic prescribing during pediatric direct-to-consumer telemedicine visits. Pediatrics. (2019) 143:5. doi: 10.1542/peds.2018-2491
27. Pedrotti CHS, Accorsi TAD, De Amicis Lima K, Serpa Neto A, Lira MTSS, Morbeck RA, et al. Antibiotic stewardship in direct-to-consumer telemedicine consultations leads to high adherence to best practice guidelines and a low prescription rate. Int J Infect Dis. (2021) 105:130–4. doi: 10.1016/j.ijid.2021.02.020
28. Hersh WR, Wallace JA, Patterson PK, Shapiro SE, Kraemer DF, Eilers GM, et al. Telemedicine for the medicare population: pediatric, obstetric, and clinician-indirect home interventions. Evid Rep Technol Assess. (2001) 24:1–32. doi: 10.1186/1472-6947-1-5
29. McDaniel NL, Novicoff W, Gunnell B, Cattell Gordon D. Comparison of a novel handheld telehealth device with stand-alone examination tools in a clinic setting. Telemed J E Health. (2019) 25:1225–30. doi: 10.1089/tmj.2018.0214
30. Erkkola-Anttinen N, Irjala H, Laine MK, Tähtinen PA, Löyttyniemi E, Ruohola A. Smartphone otoscopy performed by parents. Telemed J E Health. (2019) 25:477–84. doi: 10.1089/tmj.2018.0062
31. Bianchi MG, Santos AP, Cordioli E. The majority of skin lesions in pediatric primary care attention could be managed by tele-dermatology. PLoS ONE. (2019) 14:12. doi: 10.1371/journal.pone.0225479
32. O'Connor DM, Jew OS, Perman MJ, Castelo-Soccio LA, Winston FK, McMahon PJ. Diagnostic accuracy of pediatric teledermatology using parent-submitted photographs: a randomized clinical trial. J Am Med Assoc Dermatol. (2017) 153:1243–8. doi: 10.1001/jamadermatol.2017.4280
33. Mercuri E, Zampino G, Morsella A, Pane M, Onesimo R, Angioletti C, et al. Contactless: a new personalised telehealth model in chronic pediatric diseases and disability during the COVID-19 era. Ital J Pediatr. (2021) 47:29. doi: 10.1186/s13052-021-00975-z
34. Schweiberger K, Hoberman A, Iagnemma J, Schoemer P, Squire J, Taormina J, et al. Practice-level variation in telemedicine use in a pediatric primary care network during the covid-19 pandemic: retrospective analysis and survey study. J Med Internet Res. (2020) 22:12. doi: 10.2196/24345
35. Shah AC, Badawy SM. Telemedicine in pediatrics: systematic review of randomized controlled trials. JMIR Pediatr Parent. (2021) 4:1. doi: 10.2196/22696
36. Foster C, Martinez KA, Sabella C, Weaver GP, Rothberg MB. Patient satisfaction and antibiotic prescribing for respiratory infections by telemedicine. Pediatrics. (2019) 144:3. doi: 10.1542/peds.2019-0844
Keywords: pediatrics, telemedicine, COVID-19, tele-pediatrics, hybrid medicine
Citation: Reingold SM, Hadjipanayis A, van Esso D, del Torso S, Dornbusch HJ, de Guchtenaere A, Pancheva R, Mujkic A, Syridou G, Valiulis A, Mazur A, Rios J, Spreitzer MV, Mamenko M, D'Avino A, Kubatova G, Geitmann K, Wyder C, Altorjai P, Michailidou K and Grossman Z (2021) COVID-19 Era Effect on Pandemic and Post-pandemic Pediatric Telemedicine Use: A Survey of the European Academy of Pediatrics Research in Ambulatory Settings Network. Front. Pediatr. 9:713930. doi: 10.3389/fped.2021.713930
Received: 24 May 2021; Accepted: 16 September 2021;
Published: 22 October 2021.
Edited by:
Mark Lo, University of Washington, United StatesReviewed by:
Tomasz Szczepanski, Medical University of Silesia, PolandEhrenfried Schindler, University of Bonn, Germany
Copyright © 2021 Reingold, Hadjipanayis, van Esso, del Torso, Dornbusch, de Guchtenaere, Pancheva, Mujkic, Syridou, Valiulis, Mazur, Rios, Spreitzer, Mamenko, D'Avino, Kubatova, Geitmann, Wyder, Altorjai, Michailidou and Grossman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stephen M. Reingold, c3JlaW5nb2xkQGdtYWlsLmNvbQ==
 Stephen M. Reingold
Stephen M. Reingold Adamos Hadjipanayis
Adamos Hadjipanayis Diego van Esso
Diego van Esso Stefano del Torso4
Stefano del Torso4 Ann de Guchtenaere
Ann de Guchtenaere Rouzha Pancheva
Rouzha Pancheva Aida Mujkic
Aida Mujkic Garyfallia Syridou
Garyfallia Syridou Artur Mazur
Artur Mazur Marina Mamenko
Marina Mamenko Peter Altorjai
Peter Altorjai