- Neonatal Intensive Care Unit, Guangdong Women‘s and Children‘s Hospital, Guangzhou, China
Background and Aim: Guidelines recommended that cardiac index (CI) of term infants with septic shock should reach the target level of 3.3–6.0L/(min⋅m2). However, there are still no standard values for preterm infants with septic shock. Herein, we investigated the functional echocardiographic baseline values of left ventricular (LV) systolic functional parameters at the onset of septic shock in preterm infants and possible correlations between baseline values and poor outcomes.
Materials and Methods: This was a prospective, observational, and longitudinal single-center study. Eligible infants were monitored for LV systolic functional parameters using functional echocardiography at the onset of septic shock. The primary study outcome was the difference in the baseline value of LV systolic functional parameters in preterm infants with septic shock with different gestational age (GA) and birth weight (BW). The secondary outcome was septic shock-associated death or severe brain injury (including grade 3–4 intraventricular hemorrhage or periventricular leukomalacia).
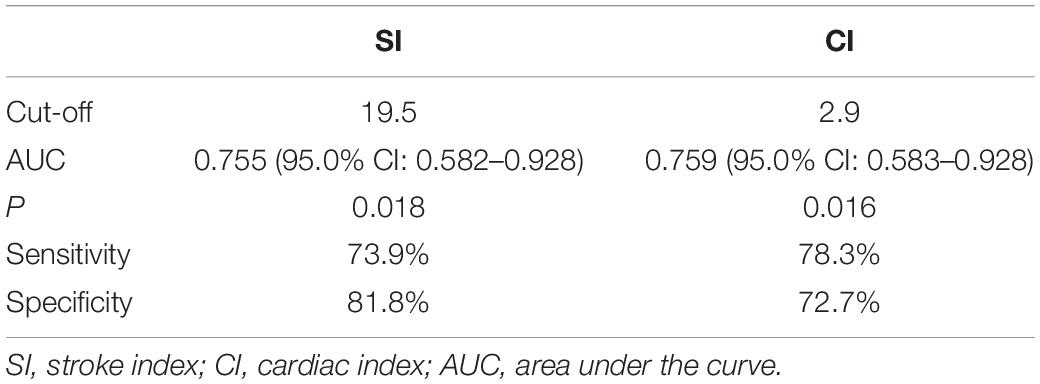
Results: In total, 43 subjects met the criteria, with a median GA of 321/7 weeks and BW of 1800 grams. No difference was observed in baseline values of LV systolic functional parameters among infants with different GA and BW. Infants were assigned to good and poor outcomes groups based on septic shock-associated death or severe brain injury. Out of 43 infants, 29 (67.4%) had good outcomes vs. 14 (32.6%) with poor outcomes. Stroke index (SI) [18.2 (11.1, 18.9) mL/m2 vs. 23.5 (18.9, 25.8) mL/m2, p = 0.017] and cardiac index (CI)[2.7 (1.6, 3.5) L/(min⋅m2) vs. 3.4 (3.0, 4.8) L/(min⋅m2), p = 0.015] in infants with poor outcomes were significantly lower (P < 0.05). Receiver operating characteristic (ROC) curve analysis showed that the cut-off values of SI and CI for predicting poor outcomes in preterm infants with septic shock were 19.5 mL/m2 (sensitivity, 73.9%; specificity, 81.8%) and 2.9L/(min⋅m2) (sensitivity, 78.3%; specificity, 72.7%), with area under the ROC curve (AUC) value of 0.755 and 0.759, respectively.
Conclusion: There were no differences in baseline LV systolic functional values among preterm infants with septic shock with different GA and BW. However, preterm infants with SI<19.5mL/m2 and/or CI<2.9L/(min⋅m2) at the onset of septic shock were at high risk of having poor outcomes.
Introduction
Sepsis is the leading cause of death for hospitalized infants, accounting for 45% of deaths in the neonatal intensive care unit (NICU) (1). Moreover, the sepsis-related mortality rate was reported to be twice as high among patients who developed cardiovascular dysfunction and septic shock (2). Hence, a precise assessment of cardiovascular compromise is essential for the appropriate management of infants with shock.
Heart rate, acid-base state, and lactate levels are the most common traditional indicators for the prediction of poor outcomes in infants with shock. However, recent studies on using color Doppler ultrasonography and near-infrared spectroscopy found that these indicators are relatively insensitive to tissue perfusion and oxygen delivery (3). In infants with shock, the imbalance between oxygen delivery and oxygen consumption can lead to metabolic disorders, organ dysfunction, and death (4). Functional echocardiographic analysis can be used to assess hemodynamics in neonates, provide a better understanding of the pathophysiological processes, and help monitor the effectiveness of and response to treatment decisions (5). In addition, left ventricular (LV) systolic functional parameters, such as stroke volume (SV) and cardiac output (CO), are essential for organs perfusion and oxygen delivery in critically ill infants with cardiovascular compromise (6, 7). Therefore, determining whether LV systolic function is normal or reduced is valuable in assessing perfusion, elucidating the mechanisms underlying hemodynamic instability, and helping target therapeutic strategies.
Guidelines recommended that cardiac index (CI) of in term infants with septic shock should reach the target level of 3.3–6.0L/(min⋅m2) (8). However, there are still no standard values for preterm infants with septic shock. Moreover, the diagnosis and treatment of septic shock in preterm infants need to be further improved.
We hypothesized that LVCO is reduced in preterm infants with poor outcomes compared to those with good outcomes at the onset of septic shock. We performed a prospective observational study to assess the baseline value of LV systolic functional parameters at the onset of septic shock in preterm infants using functional echocardiography and analyze the association with baseline value and poor outcomes.
Methodology
This prospective observational study was conducted in an 80-bed tertiary level NICU, Guangdong Women‘s and Children‘s Hospital, Guangzhou, China, from 1 June 2019 to 30 November 2020. The study was approved by the Ethics Committee of the hospital, and informed consent was provided by all parents/guardians.
Clinical data were extracted from the electronic medical record. The first co-author performed all functional echocardiograms, after which all data were instantaneously revised by the second co-author, using an M9 ultrasound scanner with a 12-MHz transducer (Mindray, Shenzhen, China).
Left ventricular systolic functional parameters were measured by functional echocardiography during the infusion of saline bolus but before giving vasoactive drugs for all enrolled preterm infants. This period of time was considered as the onset of septic shock. All infants were clinically followed until 28 days of age. Infants were categorized in two cohorts based on septic shock-associated death or severe brain injury [(including grade 3–4 intraventricular hemorrhage (IVH) or periventricular leukomalacia (PVL)]: good and poor outcomes.
We included preterm infants with septic shock who were admitted to the NICU and underwent functional echocardiographic measurements at the onset of septic shock. Neonatal septic shock was defined based on the American College of Critical Care Medicine and International Pediatric Sepsis Consensus (8, 9). Exclusion criteria included multiple congenital anomalies, chromosomal abnormalities, congenital cardiac malformation (except non-hemodynamically significant patent ductus arteriosus and patent foramen ovale), persistent pulmonary hypertension, and suspected metabolic disorders.
Left ventricular systolic function was assessed by SV, stroke index (SI), CO, CI, and LV ejection fraction (LVEF) (10). All enrolled infants were placed in the left lateral decubitus position for the examination. Echocardiographic measurements were the average of three to five consecutive cardiac cycles. SV was calculated by multiplying the velocity-time integral (VTI) with the area of the LV outflow tract (LVOT), using the following formula: π × (LVOT diameter/2)2 × VTI.
SI, CO, and CI were calculated using the following formula: SI = SV/body surface area, CO = SV × hear rate, CI = (SV × hear rate)/body surface area.
LV ejection fraction was calculated using the Teichholz method. In addition, data regarding infants‘s gestational age (GA), birth weight (BW), gender, mode of delivery, 1 and 5 min Apgar scores, and clinical hemodynamic parameters [including blood pressure (BP) and heart rate (HR)] at the onset of septic shock were collected.
Sample size estimation was done according to the previous literature. The mortality rate of very low birth weight infants with septic shock was 71% (11). The required sample size was 42 infants in two groups (good and poor outcomes) with a power of 80% and a level of significance of 5% (two-sided). Continuous variables were expressed as median (IQR), and categorical variables as a number of cases and percentages. Kruskal Wallis Test was used to evaluate differences in LV systolic function measures in the three gestational age-stratified groups and birth weight-stratified groups at the onset of septic shock, respectively. The Mann-Whitney U test was used to evaluate differences in LV systolic function measures in infants with good and poor outcomes. Receiver operating characteristic (ROC) curve analysis was conducted to examine the ability of SI and CI to identify septic shock-associated death or severe brain injury, after which the sensitivity and specificity of optimal cut-offs were described. Data were analyzed using SPSS v. 23 (IBM, Armonk, NY). A p value<0.05 was considered statistically significant.
Results
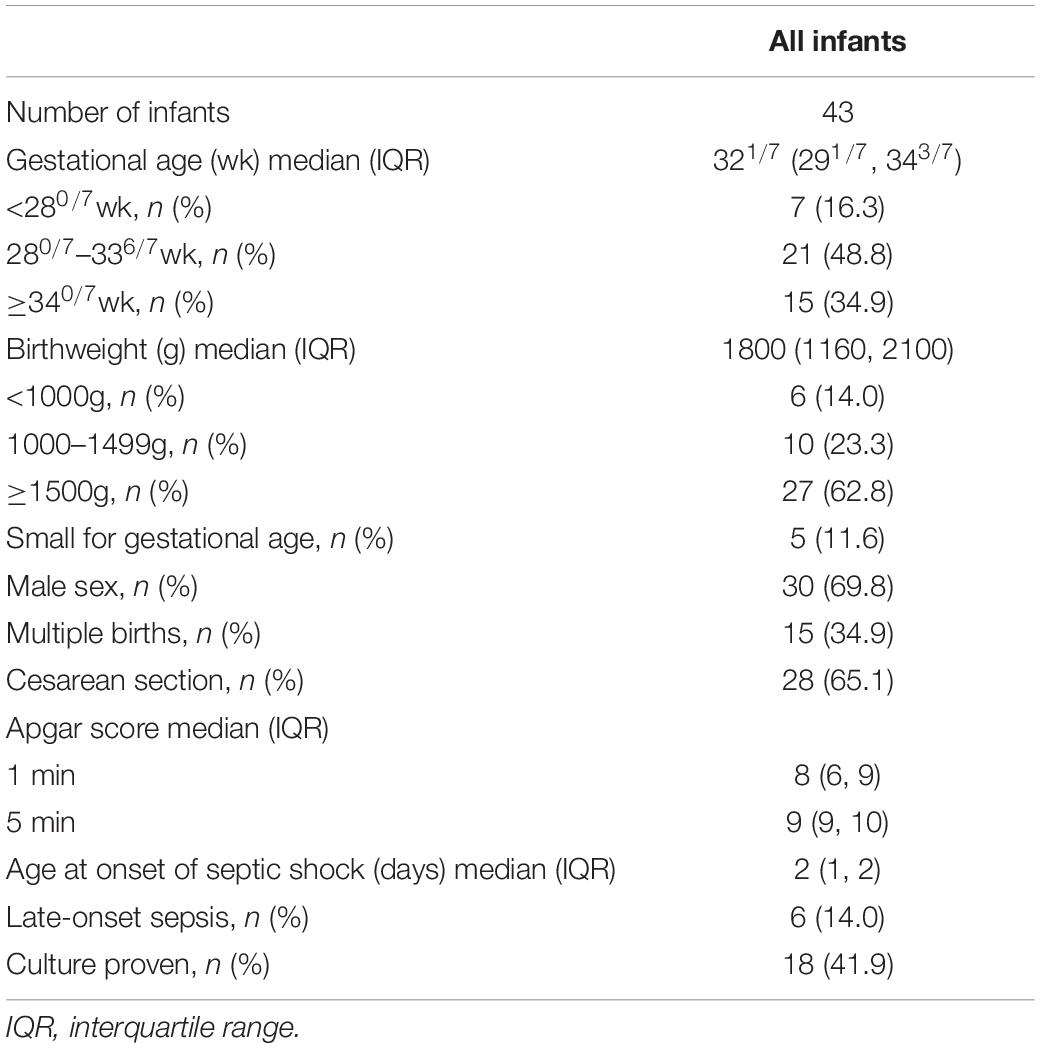
A total of 77 preterm infants were diagnosed with septic shock. According to the inclusion and exclusion criteria, 43 infants were included in the final analysis. Table 1 presents demographic data for the study population. Infants had median GA of 321/7 weeks, and the median BW of 1800 g. There were more infants with GA in the range of 280/7–336/7 weeks (48.8%) and BW ≥ 1500 g (62.8%). The majority of the sample is appropriate for GA (small GA [n = 5], 11.6%). In addition, 30 out of 43 infants were male (69.8%).
Subgroup analyses were performed based on GA (<280/7 weeks, 280/7–336/7 weeks, ≥ 340/7 weeks) and BW (<1000g, 1000–1499g, ≥ 1500g). The baseline values of LV systolic functional parameters in preterm infants with septic shock at different GA- and BW-stratified distributions are reported as the median (IQR) in Tables 2, 3, respectively. The median of SI and CI at the onset of septic shock in these subgroups were below normal ranges (8). Yet, the baseline values of LV systolic functional parameters of these subgroups were not significantly different (P > 0.05).
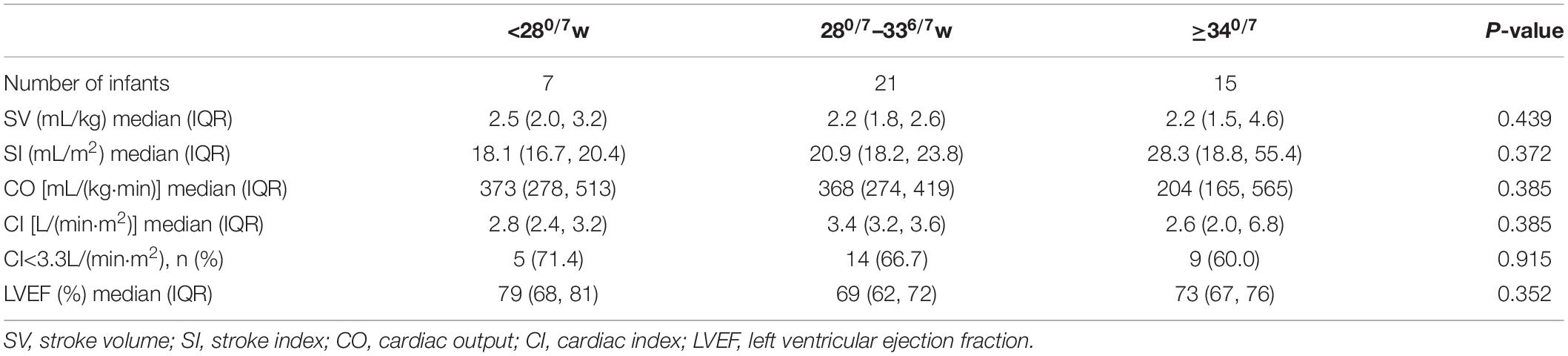
Table 2. The baseline values of LV systolic functional parameters in preterm infants with septic shock at the different gestational age-stratified distribution.
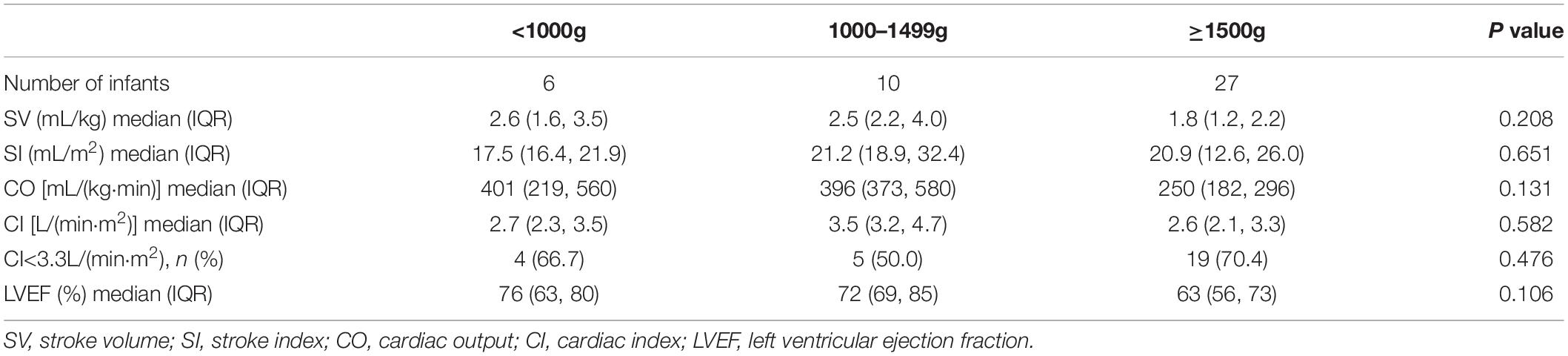
Table 3. The baseline values of LV systolic functional parameters in preterm infants with septic shock at the different birth weight-stratified distribution.
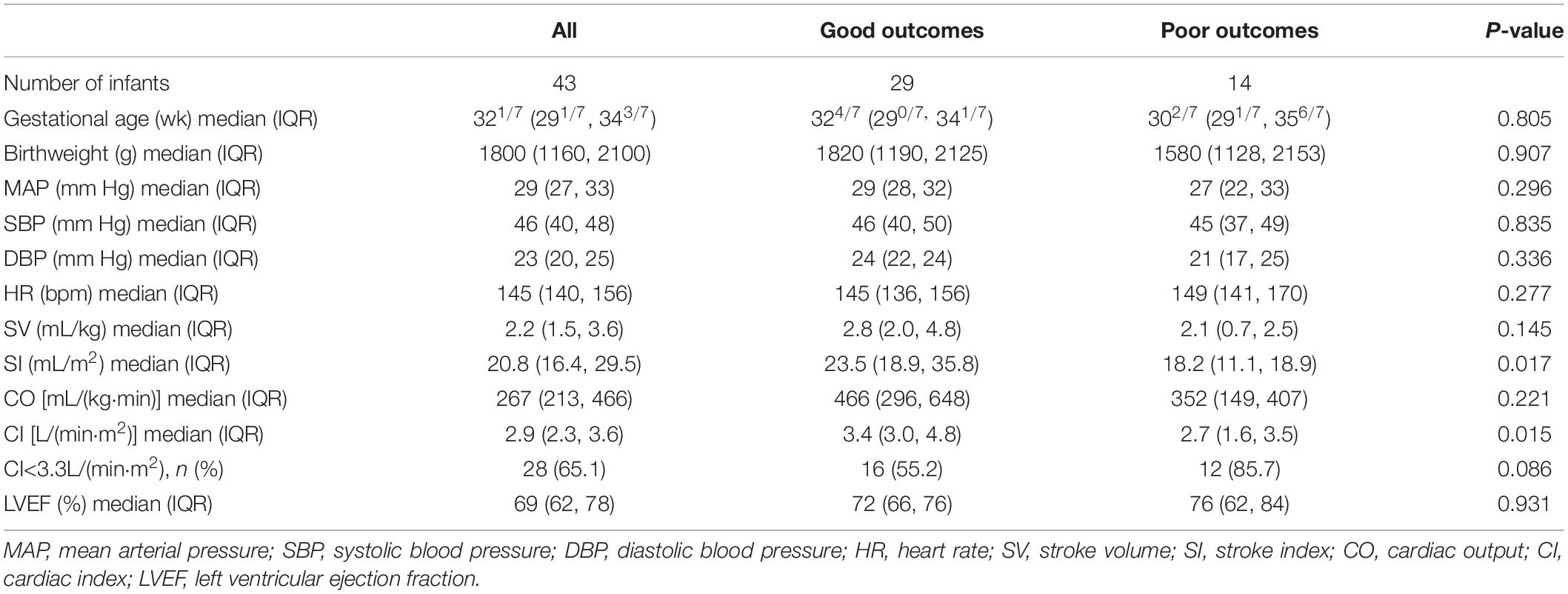
The baseline values of LV systolic functional parameters of all included infants are summarized in Table 4. Twenty-nine infants (67.4%) had good outcomes, and 14 (32.6%) had poor outcomes. Among infants with poor outcomes, severe brain injury was found in 9 (20.9%), septic shock-associated death in 7 (16.3%) cases, and all-cause death within 28 days in 13 (30.2%) patients. Infants with poor outcomes had lower SI [18.2 (11.1, 18.9) mL/m2 vs. 23.5 (18.9, 25.8) mL/m2, p = 0.017] and lower CI [2.7 (1.6, 3.5) L/(min⋅m2) vs. 3.4 (3.0, 4.8) L/(min⋅m2), p = 0.015]. There were no differences in other baseline parameters between infants with good and poor outcomes, including BP, HR, SV, CO, and LVEF (P > 0.05).
The area under the curve (AUC) for SI to identify poor outcomes was 0.755 (95% CI 0.582, 0.928), and for CI was 0.759 (95% CI 0.583, 0.928) (Figure 1). The sensitivity and specificity of optimal cut-offs for SI and CI for poor outcomes are summarized in Table 5.
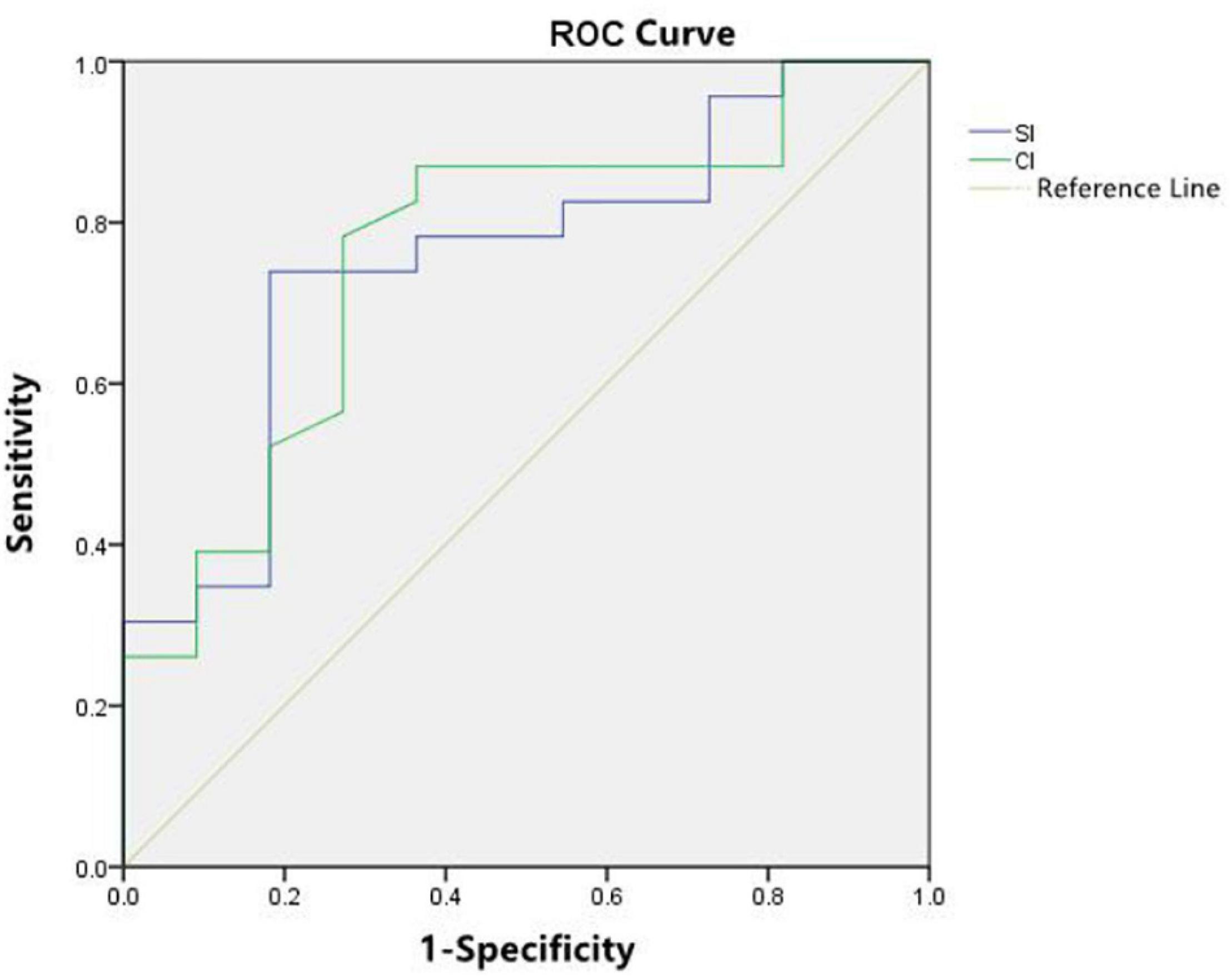
Figure 1. Receiver operating characteristic (ROC) curve analysis showed good performance of stroke index (SI) and cardiac index (CI) as predictors of subsequent septic shock-related death and severe brain injury.
Discussion
To the best of our knowledge, this is the first study that described echocardiographic LV systolic functional measurements at the onset of septic shock in preterm infants. This study also explored the value of baseline parameters in predicting the prognosis of preterm infants with septic shock. The key findings of this study are follo wing: (a) low SI and/or low CI at the onset of septic shock were correlated with the risk of poor prognosis in preterm infants, and the predicting value of SI and CI was similar; (b) isolated low BP, low SV, low CO or high HR values at the onset of septic shock cannot clearly identify the risk of poor outcomes; (c) there was no significant difference of baseline value of LV systolic functional parameters among preterm infants with different GA and BW. Using ROC analyses, we determined that the recorded baseline SI and CI were associated with septic shock-associated death and/or severe brain injury in preterm infants. SI ≥ 19.5mL/m2 and/or CI ≥ 2.9L/(min⋅m2) was correlated with the lowest rates of septic shock-associated death and/or severe brain injury.
The mortality rate of preterm infants with septic shock in our study (16.3% [7/43]) was significantly lower than that reported in the previous study (40–71%) (12), which is probably related to the use of functional echocardiographic techniques in assessment of LV cardiac output that can better guide management regimes for preterm infants with septic shock. LVCO is an important hemodynamic parameter that aids in targeting organ perfusion and oxygen delivery in infants with cardiovascular compromise. The latest guideline recommends using both transthoracic echocardiography and/or transesophageal echocardiography for the assessment of LVCO in evaluating responses to treatment (13). Thus, the reliability of subjective assessment of LVCO is questionable.
Clinical research on outcomes in neonates with septic shock has been mainly focusing on blood pressure, while the utility of hemodynamic parameters as clinical surrogates of hemodynamic status is not fully understood. The present study showed no significant difference in baseline blood pressure at the onset of septic shock between infants with good and poor outcomes. Therefore, the use of blood pressure to assess hemodynamic status remains controversial. A recent study found that by using third percentile cut-off for systolic BP, which is a common practice in the NICU, a large majority of infants with low CO fail to be detected (14). This evidently shows that BP values and LVCO are weakly correlated regardless of GA and underlying etiology. Moreover, some studies failed to show an improved prognosis after the treatment of hypotension based on mean arterial BP thresholds (15). The uncertainty about the lower limit of normal BP range in preterm infants is even more challenging. Our results further confirmed previous observations suggesting that BP should not be used as an isolated surrogate of hemodynamic status in preterm infants, irrespective of the underlying pathology, gestational age, and postnatal age.
Our study found that low SI and/or low CI at the onset of septic shock were correlated with the risk of poor prognosis in preterm infants, which is inconsistent with prior study results (16, 17). Previous studies reported high cardiac output in those with early onset of septic shock, especially in non-surviving infants, which may be related to particularities of our subjects sample with early age of onset. In this study, the median age at onset was 2 days, while the study above reported an onset of sepsis at 4 days after birth. Also, low SI and/or CI at the onset of septic shock in preterm infants could be caused by different factors (18). First, the myocardium of the preterm infant possesses an inefficient contractile mechanism and a preponderance of non-contractile, poorly compliant collagen, leading to impaired diastolic performance, particularly during the early transitional period. Furthermore, preterm infants exhibit a high resting peripheral vascular tone owing to the relatively higher concentration of vasoconstrictive receptors at the expense of vasodilatory. Additionally, the myocardium, on the other hand, lacks adequate adrenergic innervation limiting its ability to increase contractility. Therefore, our results are credible and aligned with our expectations.
Study Limitation
Our study has several limitations. First, we did not include a control group, which may lead to some bias. Nevertheless, hyper-metabolic diseases like shock require higher CO to satisfy the enhanced metabolic demand of the body. Therefore, comparisons of CO between normal and ill infants may not be significant. Second, our observations are limited to a relatively small sample size despite the apparent plausibility of low SI and low CI at the onset of septic shock in preterm infants with poor outcomes. Third, we assessed the single value of baseline parameters as predictors of poor outcomes without considering the duration of low SI and low CI or subsequent course of the preterm infants.
Conclusion
Low SI and/or low CI at the onset of septic shock were associated with death and/or severe brain injury in preterm infants. Functional echocardiographic parameters used to determine the hemodynamic status of shock may be used to understand the pathophysiology and predict poor outcomes in preterm infants with septic shock to inform decision-making regarding indications, timing, and approach to therapy. Our results provided support for our hypothesis that the baseline value of LV systolic functional parameters could be used to predict poor outcomes in preterm infants with septic shock. Therefore, these findings deserve further investigation in larger samples and future studies to further verify their clinical significance.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethical Committee (No. 202101188) in the Guangdong Women‘s and Children‘s Hospital. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
XY, CS, YW, and JM conceptualized and designed the study, organized the acquisition of data, and reviewed and revised both the analyses and manuscript. JZo, JZa, DM, and YL drafted and critically evaluated the article. JY corrected the final version of the manuscript. All authors approved the final manuscript to be published.
Funding
This work was supported by the Guangzhou Planned Project of Science and Technology (No. 202102080378) and the National Key R&D Program of China (No. 2021YFC2701700).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Meadow W, Frain L, Ren Y, Lee G, Soneji S, Lantos J. Serial assessment of mortality in the neonatal intensive care unit by algorithm and intuition: certainty, uncertainty, and informed consent. Pediatrics. (2002) 109:878–86. doi: 10.1542/peds.109.5.878
2. Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, et al. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med. (2006) 34:344–53. doi: 10.1097/01.ccm.0000194725.48928.3a
3. Seri I, Markovitz B. Cardiovascular compromise in the newborn infant. 9th ed. In: Gleason CA, Devaskar SU editors. Avery’s Diseases of the Newborn. Philadelphia, PA: Elsevier Saunders (2012). p. 714–31.
4. Deshpande SA, Platt MP. Association between blood lactate and acid-base status and mortality in ventilated babies. Arch Dis Child Fetal Neonatal Ed. (1997) 76:F15–20. doi: 10.1136/fn.76.1.f15
5. Beaulieu Y. Bedside echocardiography in the assessment of the critically ill. Crit Care Med. (2007) 35(Suppl. 5):S235–49. doi: 10.1097/01.CCM.0000260673.66681.AF
6. Dinh VA, Ko HS, Rao R, Bansal RC, Smith DD, Kim TE, et al. Measuring cardiac index with a focused cardiac ultrasound examination in the ED. Am J Emerg Med. (2012) 30:1845–51. doi: 10.1016/j.ajem.2012.03.025
7. Gaspar HA, Morhy SS. The role of focused echocardiography in pediatric intensive care: a critical appraisal. Biomed Res Int. (2015) 2015:596451. doi: 10.1155/2015/596451
8. Weiss SL, Peters MJ, Alhazzani W, Agus MSD, Flori HR, Inwald DP, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis–associated organ dysfunction in children. Intensive Care Med. (2020) 46(Suppl. 1):10–67.
9. Davis AL, Carcillo JA, Aneja RK, Deymann AJ, Lin JC, Nguyen TC, et al. American college of critical care medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock. Crit Care Med. (2017) 45:1061–93.
10. Tissot C, Singh Y, Sekarski N. Echocardiographic evaluation of ventricular functional–for neonatologist and pediatric intensivist. Front Pediatr. (2018) 6:79. doi: 10.3389/fped.2018.00079
11. Jennifer B, Cynthia BP, Kenji S, Robert EB, WHO Child Health Epidemiology Reference Group. WHO estimates of the cause of death in children. Lancet. (2005) 365:1147–52. doi: 10.1016/s0140-6736(05)71877-8
12. Duchemin EK, Laborie S, Rabilloud M, Lapillonne A, Claris O. Outcome and prognostic factors in neonates with septic shock. Pediatr Crit Care Med. (2008) 9:186–91. doi: 10.1097/PCC.0b013e31816689a8
13. Porter TR, Shillcutt SK, Adams MS, Desjardins G, Glas KE, Olson JJ, et al. Guidelines for the use of echocardiography as a monitor for therapeutic intervention in adults:a report from the American society of echocardiography. J Am Soc Echocardiogr. (2015) 28:40–56. doi: 10.1016/j.echo.2014.09.009
14. Kharrat A, Rios DI, Weisz DE, Giesinger RE, Groves A, Yang J, et al. The relationship between blood pressure parameters and left ventricular output in neonates. J Perinatol. (2019) 39:619–25. doi: 10.1038/s41372-019-0337-6
15. Dempsey EM, Barrington KJ. Treating hypotension in the preterm infant: when and with what: a critical and systematic review. J Perinatol. (2007) 27:469–78.
16. Shiv SS, Praveen K, Rohit MK. Hemodynamic changes in preterm neonates with septic shock: a prospective observational study. Pediatr Crit Care Med. (2014) 15:443–50. doi: 10.1097/PCC.0000000000000115
17. Koert DW, Nick E. Hemodynamics in preterm infants with late–onset sepsis. J Pediatr. (2010) 156:918–922.e1. doi: 10.1016/j.jpeds.2009.12.026
Keywords: septic shock, preterm infants, stroke index, cardiac index, functional echocardiography
Citation: Zhong J, Shuai C, Wang Y, Mo J, Ma D, Zhang J, Lin Y, Yang J and Ye X (2022) Baseline Values of Left Ventricular Systolic Function in Preterm Infants With Septic Shock: A Prospective Observational Study. Front. Pediatr. 10:839057. doi: 10.3389/fped.2022.839057
Received: 19 December 2021; Accepted: 21 February 2022;
Published: 29 March 2022.
Edited by:
Yogen Singh, Cambridge University Hospitals NHS Foundation Trust, United KingdomReviewed by:
Nilkant Phad, John Hunter Children’s Hospital, AustraliaTanushree Sahoo, All India Institute of Medical Sciences Bhubaneswar, India
Copyright © 2022 Zhong, Shuai, Wang, Mo, Ma, Zhang, Lin, Yang and Ye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiuzhen Ye, eXh6aDMyOEAxMjYuY29t
 Junjuan Zhong
Junjuan Zhong Chun Shuai
Chun Shuai Yue Wang
Yue Wang Jing Mo
Jing Mo Dongju Ma
Dongju Ma Jing Zhang
Jing Zhang Yingyi Lin
Yingyi Lin Xiuzhen Ye
Xiuzhen Ye