- 1Department of Woman's and Child's Health, University Hospital of Padua, Padua, Italy
- 2Pediatric Intensive Care Unit, Department of Woman's and Child's Health, University Hospital of Padua, Padua, Italy
Ventilation is one of the most common procedures in critically ill children admitted to the pediatric intensive care units (PICUs) and is associated with potential severe side effects. The longer the mechanical ventilation, the higher the risk of infections, mortality, morbidity and length of stay. Protocol-based approaches to ventilation weaning could have potential benefit in assisting the physicians in the weaning process but, in pediatrics, clear significant outcome difference related to their use has yet to be shown. Extubation failure occurs in up to 20% of patients in PICU with evidences demonstrating its occurrence related to a worse patient outcome including higher mortality. Various clinical approaches have been described to decide the best timing for extubation which can usually be achieved by performing a spontaneous breathing trial before the extubation. No clear evidence is available over which technique best predicts extubation failure. Within this review we summarize the current strategies of ventilation weaning and extubation readiness evaluation employed in the pediatric setting in order to provide an updated view on the topic to guide intensive care physicians in daily clinical practice. We performed a thorough literature search of main online scientific databases to identify principal studies evaluating different strategies of ventilation weaning and extubation readiness including pediatric patients receiving mechanical ventilation. Various strategies are available in the literature both for ventilation weaning and extubation readiness assessment with unclear clear data supporting the superiority of any approach over the others.
Introduction
Mechanical ventilation (MV) is a common procedure for patients admitted to the pediatric intensive care units (PICUs). Although MV is necessary and life-saving, it can be associated with complications such as ventilator associated pneumonia, cardiovascular disfunction, airway injury and patient's immobility (1, 2). The longer the MV, the higher the risk of morbidity, length of stay and mortality (3–5). To reduce the risks associated with a prolonged MV, the clinicians should aim to constantly optimize the ventilation weaning (VWe) process, thus increasing the
likelihood of a successful extubation. VWe is defined as “the gradual reduction of mechanical ventilatory support and the transfer of the respiratory control and the work of breathing back to the patient” (6). Traditionally, VWe was achieved by clinical judgement on a personal decision. Only in the last few years, protocol-based approaches have been implemented, with conflicting results. Extubation is defined as “the removal of the endotracheal tube” and extubation failure occurs when a patient needs a re-intubation within hours or days following a planned extubation. A failed extubation may be secondary to the incapacity to maintain oxygenation, alveolar ventilation, airway patency and protection, secretion management, or any combination of them (7). Extubation failure occurs in 3–22% of patients, independently from the underlying illness severity, with evidence that its occurrence can directly worsen patient outcomes including an increased mortality rate (8). Various clinical approaches are used to decide the best timing for extubation but no clear evidence is available over which technique is the best in children (9). The purpose of this review is to describe the most common strategies of VWe and extubation readiness tests, providing an updated view for the intensive care physicians in daily clinical practice.
Methods
We performed a thorough literature search of Medline, Embase, Scopus, Web of Science and Cinahl to identify studies on different strategies of VWe and extubation readiness tests assessing strengths and weaknesses of each procedure. The keywords used for the research were “mechanical ventilation” AND (“extubation” OR “weaning”) AND (“infants” OR “child” OR “children” OR “pediatric”). All potentially relevant titles and abstracts were retrieved and assessed for eligibility.
Results
Weaning From Mechanical Ventilation
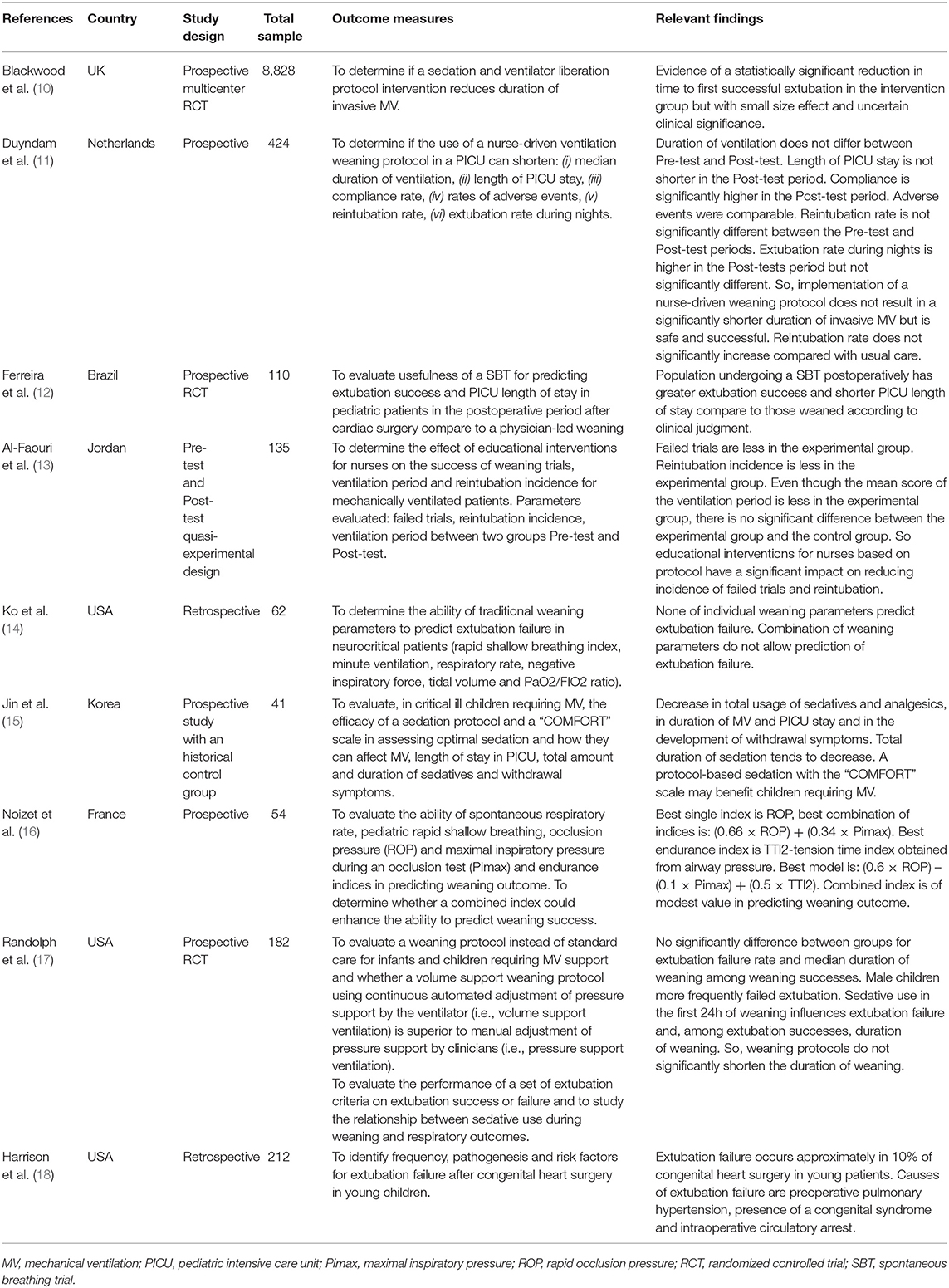
MV is divided into two phases: the maintenance phase and the weaning process. During the maintenance phase patients are usually ventilated with a synchronized modality or, if deeper sedation is required, with a controlled mode. The weaning phase usually starts when the patient is recovering from the disease which caused the intubation allowing him/her to start an inspiratory effort. The weaning process implies a transition from a full ventilatory support to a spontaneous breathing work, by gradually decreasing ventilatory parameters such as respiratory rate, positive end-expiratory pressure (PEEP) and pressure support (PS). In children, the synchronized intermittent mandatory ventilation (SIMV) with PS option is used during the weaning phase, allowing the gradual reduction of such parameters until the child is able to breath on his/her own. The weaning process is not standardized and may vary depending on different factors such as duration of MV, ventilatory muscle strength, endurance of ventilatory muscles, depth of sedation which can affect the neuromuscular conduction, and the underlying disease (16). In PICU, VWe should be a collaborative process and depends on interrelated components including clinical experience, professional judgment and autonomy, multidisciplinary team working and organizational structure (11, 13) (Table 1).
Monitoring During Weaning From MV
During ventilation, it is mandatory to constantly assess the correct timing for the transition between the two abovementioned phases: clinical factors such as the level of consciousness and sedation, the ability to clear the airways with effective cough and the absence of excessive secretions should guide any decision. Patients can also be considered eligible for the weaning phase when hemodynamically stable, with adequate oxygenation and gas exchange within acceptable parameters: usually FiO2 <50%, PaO2 >60 mmHg, PEEP <5–8 cm H2O, pH >7.25 (19, 20). After every ventilation parameter change, it is pivotal to monitor the patient's response in term of work of breathing, level of oxygenation, both clinically and with the aid of blood-gases.
Weaning Protocols and Techniques
While in adults, protocol-based weaning approaches are well established (20, 21), in pediatrics no protocol-based approach over a physician individualized decision has demonstrated a clear superiority. Schultz and colleagues found a reduction in the time spent in the weaning phase in the ”protocol-driven” patients compared to the ”clinician-driven” ones, even if no difference in the total duration of MV and number of complications were observed between the two groups (22). Randolph and colleagues found that weaning protocols did not significantly shorten duration of weaning in pediatric patients who had already failed one extubation (17). Nevertheless, the implementation of a sedation protocol was associated with a significant decrease in the total dose of sedatives, incidence of withdrawal symptoms, length of MV and ICU stay (15, 23). Ferreira and colleagues reduced the length of MV using a strict weaning protocol evaluating daily respiratory function coupled with echocardiographic assessment of the heart function on minimal ventilatory support (12). Minimal sedation is often feasible in adults mainly due to patient's cooperation and the early transition to tracheostomy, which is usually postponed in children. Children need to be maintained with a deeper level of sedation because of possible agitation and less tolerance to intubation. Blackwood et al. recently published a multicenter study comparing the use of a sedation and weaning protocol to the standard care including many centers (28 PICUs) and a significant number of patients (8,843 children) (10). The use of the protocol showed a significant reduction in the duration of MV to first successful extubation compared to usual care. Nonetheless, effect size was small and clinical significance uncertain considering that this approach seemed to require a huge economical and organizational investment. Despite that, the implementation of such a protocol may offer several advantages: greater involvement of nurses in ventilation, weaning and sedation assessment, a more standardized approach to ventilation and weaning and overall, a closer attention to the patient's needs.
Special Populations
Critically ill children affected by cardiac and neurological disorders may need special attention in the weaning process, carrying some specific features compared to the general pediatric population. Children after cardiac surgery have Pre-existing co-morbidities which may increase the severity of their conditions. Moreover, this subset of patients usually undergoes a thoracotomy/sternotomy, which alters chest wall integrity, or a cardiopulmonary bypass, that triggers a systemic inflammatory response which may result in end-organ dysfunction. Furthermore, MV itself, altering the labile equilibrium of the intrathoracic pressures may have adverse effects on hemodynamic. Also, the presence of pulmonary hypertension, a coexisting congenital syndrome or deep hypothermic circulatory arrest were all described as independent predictors of extubation failure (18).
In neurocritical care patients the success of weaning from MV depends on the underlying neurological condition: patients affected by acute syndromes/illnesses could have spontaneous recovery, while those affected by neurodegenerative diseases are predictably difficult to wean, and may require tracheostomy and possibly subsequent home ventilation. Furthermore, positive fluid balance, secondary to high amounts of intravenous fluids administered to maintain an adequate cerebral perfusion may complicate the weaning process (14).
Nurse-Driven Protocols
The role of nurses may be pivotal for an effective decision-making in VWe due to their active presence at the patients' bedside 24 h per day. The introduction of protocol-based weaning parameters associated with a strong training of the nurses on ventilatory management are the basis for the hypothesis that a VWe nurse-driven protocol could optimize this process. Until now, however, the application of a nurse-driven weaning protocol has not demonstrated a clear association with a reduction of weaning time and did not lead to a shorter length of MV (13). Nevertheless, the use of a nurse-driven weaning protocol is considered safe and showed a reduction of the incidence of reintubation rate compared with usual care (11). Further studies are still needed but it seems that nurse-driven protocol could upgrade the performance of PICU's nurses, improve quality of care and reduce risks for patients.
Extubation Readiness/Failure
Clinical Practice and Monitoring
Readiness for extubation implies that the VWe process is almost completed; the patient should be assessed for the ability to produce effective respiratory breaths, protect the airways with intact and valid reflexes, and have a stable hemodynamic (19).
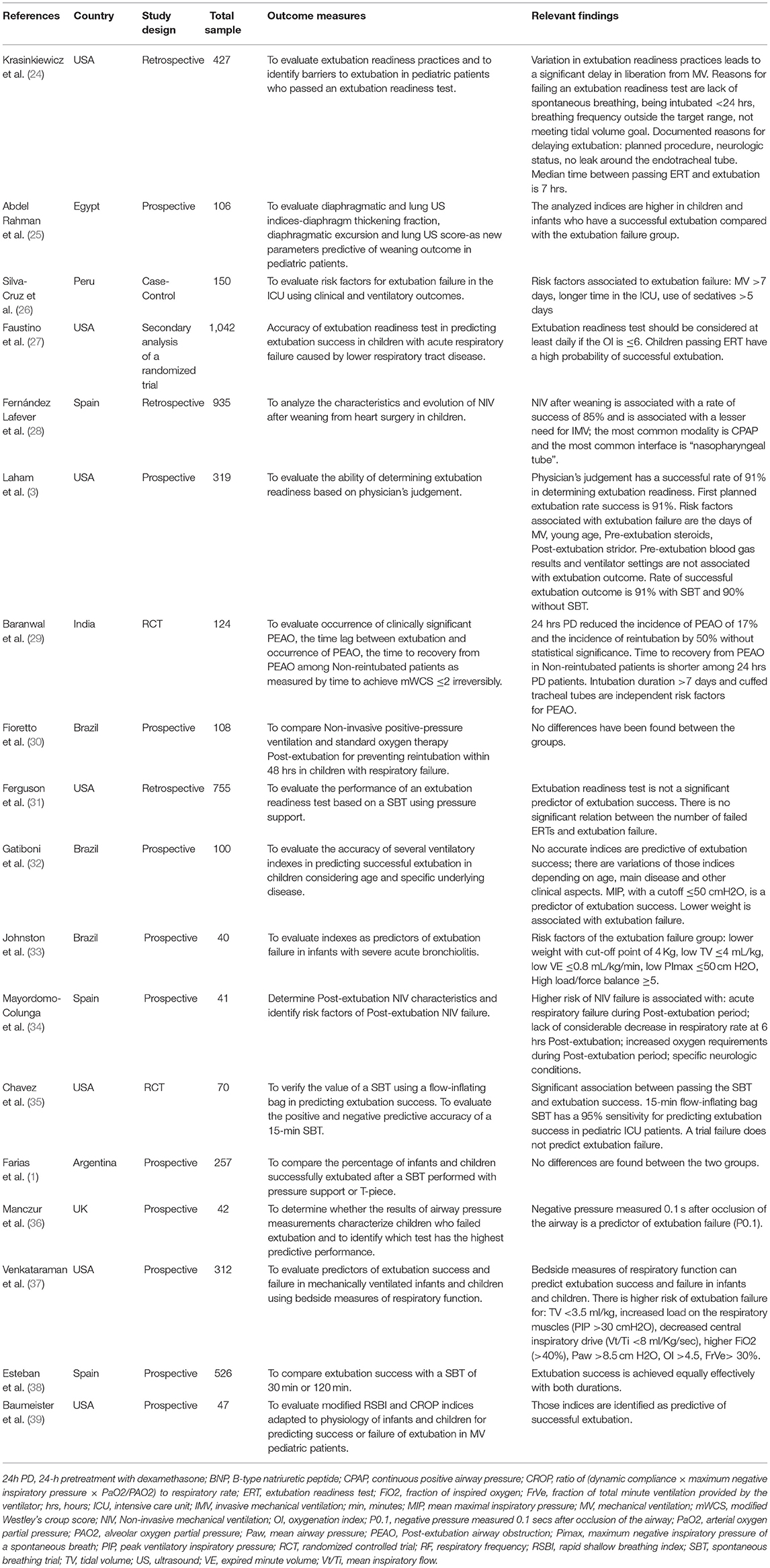
Multiple tests and indices are available, but a consensus on the best practice is still lacking (Table 2). In a work of Faustino et al., an Extubation Readiness Test (ERT) was applied to more than 1,000 children intubated for acute respiratory failure. The chances of successful extubation were greater if patients maintained the following parameters for 2 h: oxygen saturation >95%, exhaled tidal volume (VT) >5 ml/Kg and normal respiratory rate for age (27). Post extubation upper airway obstruction due to subglottic edema and stenosis could be a complication, not so rare in the pediatric population, often requiring reintubation.
Pre-extubation variables and weaning parameters easily obtained at patient's bedside can potentially predict the relative risk of extubation failure but evidences are still controversial. Venketaram et al. showed that an increased work of breathing resulting in higher peak inspiratory pressures, a lower tidal volume or a decreased central inspiratory drive, as shown by a VT/Ti <8 mL/kg/s, may predict a higher risk of failure (37); in other studies, though, easily measured parameters such as ventilator settings, VT, respiratory rate, Pimax and arterial blood gases were not considered reliable factors for extubation readiness because of their possible correlation with other clinical aspects such as the patients' age or the underlying disease (1, 3, 32).
Newth et al. described the use of the cuff leak test, which was used to predict the occurrence of post extubation stridor, especially in patients who underwent prolonged intubation or with high amounts of secretions. During the test, a cuff deflation is applied maintaining a peak inspiratory pressure in a range between 20 and 25 cm H2O; usually an audible air flow from the patient is expected to be heard. Various studies showed a good specificity but low sensibility of this test, so its presence may be reassuring for the physician, but a negative test -i.e., the absence of audible leak- should not delay the extubation attempt. The serial repetition of leak tests, instead, seemed to be a good predictor for extubation readiness (4).
Ultrasound (US) is also used as a Non-invasive tool for testing patients' readiness for extubation. Rahman et al. firstly introduced diaphragm thickening fraction, diaphragmatic excursion and lung US score as possible new indices for the evaluation of diaphragmatic and pulmonary status. All parameters were significantly higher in children who underwent a successful extubation. In the future US may be used with good sensitivity and specificity as an additional predictive tool and may be considered to be integrated in an ideal protocol (25).
Spontaneous Breathing Trials
New techniques for assessing readiness for weaning and predicting extubation success are being developed. In adult ICU the most used technique is the SBT which consists of a period of time usually between 30 and 120 min during which the patient is examined for cardiovascular and respiratory stability while ventilated on zero to minimal respiratory support, thus permitting to test the patients' ability to tolerate clinical conditions similar to that after extubation. SBT can be performed with continuous positive airway pressure (CPAP), T-piece or PS modalities (9).
During such time, patients are strictly monitored for possible signs of poor tolerance to the trial through different methods: vital signs (e.g., increase respiratory rate and heart rate), clinical signs of increased respiratory work (e.g., apnea, decreased air entry, severe retractions, tachypnea, nasal flaring), mechanical respiratory parameters (e.g., VT, minute volume, respiratory rate, dynamic compliance and muscle strength), changes in arterial blood gases, oxygen saturation and capnography. This strategy is still not routinely used in PICU and which option is the best to predict extubation success is still under debate. Farias et al. compared SBT with the use of a T-piece vs. PS of 10 cm H2O before extubation in children. The study was not able to demonstrate a difference in reducing the work of breathing between SBT with T-piece and SBT with PS and both strategies had controversial aspects such as the higher cost of a T-piece system, or the air leakage of uncuffed tubes when PS was applied (1). Ferguson et al. underlined the possible negative role of PS which could mask the respiratory insufficiency due to diaphragmatic disfunction and reduce the work of breathing during the test, by overcoming the resistance of small diameter tubes (31). Chavez et al. analyzed an SBT using a T-piece/CPAP system (with an anesthesia bag) to maintain functional residual capacity during the trial. In this way continuous positive pressure prevented the development of atelectasis. Ninety-two percent of patients were successfully extubated after a positive SBT, the specificity of the SBT was 37% with a negative predictive value of 50% (35).
Another open issue is the optimal duration of SBT. In most studies the length of the test is set up to 2 h but the ideal duration is still under debate with some authors suggesting a shorter time, up to 30 min (38). Despite everything, the physician's evaluation coupled with the routine use of a suitable SBT are essential to assess the correct timing of extubation readiness. It is important to notice that, most of the abovementioned signs of failure usually develop within the initial few minutes of the SBT; the patient should be closely monitored mostly in the first phases of the trial to confirm if they are able to complete it.
Prognostic Factors for Extubation Failure
Several factors, related to the patient or to MV, are associated with a high risk of extubation failure. Silva-Cruz et al. enrolled 150 pediatric patients in a case-control study for the detection of risk factors associated with extubation failure. The failure group presented with a longer duration of MV, PICU length of stay and number of sedatives (26). Johnston et al. analyzed 40 infants with severe acute bronchiolitis who underwent a planned extubation; patient's weight was lower in the extubation failure group (33). Krasinkiewicz et al. reported that compromised neurological status can cause delaying in extubation. In fact, these patients either received higher doses of medication for sedation and management of pain or were unable to protect their airway for neurologic causes (24). This trend was confirmed in a similar study by Mayordomo-Colunga et al., which concluded that neurological disorders may influence extubation due to pharyngeal hypotonia and inability to properly protect airway (34).
Corticosteroids: Adjuncts to Extubation
Upper airway obstruction is the primary cause of extubation failure in most pediatric studies, therefore efforts should be focused on avoiding tracheal inflammation and subglottic edema before extubation. With these assumptions it is not surprising that numerous studies have focused on the use of steroids. Neonatal and pediatric studies showed mixed results. A Cochrane review concluded that the use of corticosteroids to either prevent or treat stridor after extubation has not proven effective, but “consistent trends toward benefit” were noted. Intravenous dexamethasone, administered at least once prior to extubation, was the most common steroid regimen used; in the literature, however, no evidence exists over which steroid is the most effective (29, 40). In conclusion, corticosteroids seem to be beneficial for infants and children, but definitive evidence of efficacy is lacking. Moreover, the use of multiple steroid doses and administration timing before extubation are still unclear and deserve further studies.
Role of Non-invasive Ventilation
Use of elective-NIV in high-risk children immediately after extubation is associated with a reduced risk of reintubation compared with rescue-NIV administered when the patient is already presenting with respiratory failure (41, 42).
In children the literature is scarce, even if the number of publications is increasing, with results comparable to adults (30, 34). Similar results were found also in children after heart surgery (28).
Furthermore, studies underline the importance of monitoring parameters such as the increase of respiratory rate (RR), blood pressure and/or oxygen demand as possible risk factors of NIV failure (34). Nevertheless, Post-extubation NIV is not yet the standard of care and still need to be clarified the need for implementation in daily clinical practice.
Indexes to Evaluate Extubation Readiness
In adults several integrated variables and indexes have been studied to predict extubation readiness but none of them is fully integrated in pediatric clinical practice.
Rapid shallow breathing test (RSBI) (43) is defined as the ratio between respiratory rate and tidal volume (RR/VT) when the patient breaths unassisted. This test is predictive of extubation success if <105 breaths/min/L. The test was also proposed in the pediatric population, with a modified RSBI based on patient's weight (39). However, clear-cut cut-offs are still lacking and the ones proposed showed a low sensibility and specificity (19, 44).
Maximum-inspiratory-pressure (MIP) consists in a maximal voluntary inspiratory effort against an occluded airway. Data are measured using an external manometer with a unidirectional valve or the “Negative-Inspiratory-Force” function available on most ventilators with a value to predict extubation failure of <30 cm H2O (45). Both these methods require full patient cooperation which is challenging to obtain in children. Finally, occlusion pressure P0.1 is the value of airway pressure 0.1 sec after initiation of an inspiratory effort against an occluded airway, reflecting patient's respiratory drive. Normal values in adults are 1–2 cm H2O, whereas 3–4 cm H2O may reflect the need for a high respiratory drive to maintain adequate alveolar ventilation. Children who fail extubation, on the contrary, were found to have a lower median P0.1, probably secondary to a reduced respiratory drive (36). Adult guidelines on weaning consider these indexes as possible ancillary tests, even if often unnecessary and redundant (20). At present, they are not sufficiently accurate in pediatrics, probably due to the wide ranges of age and weights (1, 3, 32, 46).
Conclusions
The science of ventilator weaning and extubation readiness is still an art to be refined. No definitive data are available supporting the superiority of one approach over the others. Lack of guidelines makes the weaning from ventilation a controversial process in pediatric patients with a fundamental role still played by clinical judgment. Further studies are needed to build strong literature and standardized protocols.
Author Contributions
EP reviewed the literature, contributed to the acquisition, interpretation of the data, and drafted the manuscript. FC, MP, DV, LZ, and FZ contributed to the acquisition and interpretation of the data, drafted the manuscript, and reviewed the literature. AP critically revised the manuscript. MD drafted and critically revised the manuscript. CM conceived the idea for this review, drafted, and critically reviewed the manuscript. All the authors finally approved the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CPAP, continuous positive airway pressure; ERT, extubation readiness test; MIP, maximum-inspiratory-pressure; MV, mechanical ventilation; NIV, Non-invasive ventilation; PEEP, positive end-expiratory pressure; PICU, pediatric intensive care unit; PS, pressure support; RR, respiratory rate; RSBI, rapid shallow breathing test; SBT, spontaneous breathing trials; SIMV, synchronized intermittent mandatory ventilation; VT, tidal volume; VWe, ventilation weaning.
References
1. Farias J, Retta A, Alía I, Olazarri F, Esteban A, Golubicki A, et al. A comparison of two methods to perform a breathing trial before extubation in pediatric intensive care patients. Intensive Care Med. (2001) 27:1649–54. doi: 10.1007/s001340101035
2. Principi T, Fraser DD, Morrison GC, Farsi S al, Carrelas JF, Maurice EA, et al. Complications of mechanical ventilation in the pediatric population. Pediatr Pulmonol. (2011) 46:452–7. doi: 10.1002/ppul.21389
3. Laham JL, Breheny PJ, Rush A. Do clinical parameters predict first planned extubation outcome in the pediatric intensive care unit? J Intensive Care Med. (2015) 30:89–96. doi: 10.1177/0885066613494338
4. Newth CJL, Venkataraman S, Willson DF, Meert KL, Harrison R, Dean JM, et al. Weaning and extubation readiness in pediatric patients. Pediatr Crit Care Med. (2009) 10:1–11. doi: 10.1097/PCC.0b013e318193724d
5. Monteverde E, Fernández A, Poterala R, Vidal N, Siaba Serrate A, Castelani P, et al. Characterization of pediatric patients receiving prolonged mechanical ventilation. Pediatr Crit Care Med. (2011) 12: e287–91. doi: 10.1097/PCC.0b013e3182191c0b
6. Blackwood B, Murray M, Chisakuta A, Cardwell CR, O'Halloran P. Protocolized vs. non-protocolized weaning for reducing the duration of invasive mechanical ventilation in critically ill paediatric patients. Cochrane Database Syst Rev. (2013) 7:CD009082. doi: 10.1002/14651858.CD009082.pub2
7. Parotto M, Cooper RM, Behringer EC. Extubation of the challenging or difficult airway. Curr Anesthesiol Rep. (2020) 10:334–40. doi: 10.1007/s40140-020-00416-3
8. Kurachek SC, Newth CJ, Quasney MW, Rice T, Sachdeva RC, Patel NR, et al. Extubation failure in pediatric intensive care: a multiple-center study of risk factors and outcomes. Crit Care Med. (2003) 31:2657–64. doi: 10.1097/01.CCM.0000094228.90557.85
9. Burns KEA, Soliman I, Adhikari NKJ, Zwein A, Wong JTY, Gomez-Builes C, et al. Trials directly comparing alternative spontaneous breathing trial techniques: a systematic review and meta-analysis. Crit Care. (2017) 21:27. doi: 10.1186/s13054-017-1698-x
10. Blackwood B, Tume LN, Morris KP, Clarke M, McDowell C, Hemming K, et al. Effect of a sedation and ventilator liberation protocol vs. usual care on duration of invasive mechanical ventilation in pediatric intensive care units: a randomized clinical trial. JAMA. (2021) 326:401–10. doi: 10.1001/jama.2021.17731
11. Duyndam A, Houmes RJ, van Rosmalen J, Tibboel D, van Dijk M, Ista E. Implementation of a nurse-driven ventilation weaning protocol in critically ill children: can it improve patient outcome? Aust Crit Care. (2020) 33:80–8. doi: 10.1016/j.aucc.2019.01.005
12. Ferreira FV, Sugo EK, Aragon DC, Carmona F, Carlotti APCP. Spontaneous breathing trial for prediction of extubation success in pediatric patients following congenital heart surgery: a randomized controlled trial. Pediatr Crit Care Med. (2019) 20:940–6. doi: 10.1097/PCC.0000000000002006
13. Al-Faouri IG, Abualrub RF, Jumah DM. The impact of educational interventions for nurses on mechanically ventilated patients' outcomes in a Jordanian university hospital. J Clin Nurs. (2014) 23:2205–14. doi: 10.1111/jocn.12497
14. Ko R, Ramos L, Chalela JA. Conventional weaning parameters do not predict extubation failure in neurocritical care patients. Neurocrit Care. (2009) 10:269–73. doi: 10.1007/s12028-008-9181-9
15. Jin HS, Yum MS, Kim SL, Shin HY, Lee EH, Ha EJ, et al. The efficacy of the COMFORT scale in assessing optimal sedation in critically ill children requiring mechanical ventilation. J Korean Med Sci. (2007) 22:693–7. doi: 10.3346/jkms.2007.22.4.693
16. Noizet O, Leclerc F, Sadik A, Grandbastien B, Riou Y, Dorkenoo A, et al. Does taking endurance into account improve the prediction of weaning outcome in mechanically ventilated children? Crit care. (2005) 9:R798–807. doi: 10.1186/cc3898
17. Randolph AG, Wypij D, Venkataraman ST, Hanson JH, Gedeit RG, Meert KL, et al. Effect of mechanical ventilator weaning protocols on respiratory outcomes in infants and children a randomized controlled trial. JAMA. (2002) 288:2561–8. doi: 10.1001/jama.288.20.2561
18. Harrison AM, Cox AC, Davis S, Piedmonte M, Drummond-Webb JJ, Mee RBB. Failed extubation after cardiac surgery in young children: prevalence, pathogenesis, and risk factors. Pediatr Crit Care Med. (2002) 3:148–52. doi: 10.1097/00130478-200204000-00011
19. Johnston C, da Silva PSL. Weaning and extubation in pediatrics. Curr Respir Med Rev. (2012) 8:68–78. doi: 10.2174/157339812798868852
20. MacIntyre NR, Cook DJ, Ely EW Jr, Epstein SK, Fink JB, Heffner JE, et al. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American college of chest physicians; the American association for respiratory care; and the American college of critical medicine. Chest. (2001) 120:375S−95S. doi: 10.1378/chest.120.6_suppl.375S
21. Kollef MH, Shapiro SD, Silver P, St John RE, Prentice D, Sauer S, et al. A randomized, controlled trial of protocol-directed vs. physician-directed weaning from mechanical ventilation. Crit Care Med. (1997) 25:567–74. doi: 10.1097/00003246-199704000-00004
22. Schultz TR, Lin RJ, Watzman HM, Durning SM, Hales R, Woodson A, et al. Weaning children from mechanical ventilation: a prospective randomized trial of protocol-directed vs. physician-directed weaning. Respir Care. (2001) 46:772–82.
23. Kress JP, Pohlman AS, O' Connor MF, Hall J. Daily interruption of sedative infusion in critically ill patients undergoing mechanical ventilation. N Engl J Med. (2000) 342:1471–7. doi: 10.1056/NEJM200005183422002
24. Krasinkiewicz JM, Friedman ML, Slaven JE, Lutfi R, Abu-Sultaneh S, Tori AJ. Extubation readiness practices and barriers to extubation in pediatric subjects. Respir Care. (2021) 66:582–90. doi: 10.4187/respcare.08332
25. Abdel Rahman DA, Saber S, El-Maghraby A. Diaphragm and lung ultrasound indices in prediction of outcome of weaning from mechanical ventilation in pediatric intensive care unit. Indian J Pediatr. (2020) 87:413–20. doi: 10.1007/s12098-019-03177-y
26. Silva-Cruz AL, Velarde-Jacay K, Carreazo NY, Escalante-Kanashiro R. Risk factors for extubation failure in the intensive care unit. Rev Bras Ter Intensiva. (2018) 30:294–300. doi: 10.5935/0103-507X.20180046
27. Faustino EV, Gedeit R, Schwarz AJ, Asaro LA, Wypij D, Curley MA. Accuracy of an extubation readiness test in predicting successful extubation in children with acute respiratory failure from lower respiratory tract disease. Crit Care Med. (2017) 45:94–102. doi: 10.1097/CCM.0000000000002024
28. Fernández Lafever S, Toledo B, Leiva M, Padrón M, Balseiro M, Carrillo A, et al. Non-invasive mechanical ventilation after heart surgery in children. BMC Pulm Med. (2016) 16:167. doi: 10.1186/s12890-016-0334-x
29. Baranwal AK, Meena JP, Singhi SC, Muralidharan J. Dexamethasone pretreatment for 24 h vs. 6 h for prevention of postextubation airway obstruction in children: a randomized double-blind trial. Intensive Care Med. (2014) 40:1285–94. doi: 10.1007/s00134-014-3358-9
30. Fioretto JR, Ribeiro CF, Carpi MF, Bonatto RC, Moraes MA, Fioretto EB, et al. Comparison between noninvasive mechanical ventilation and standard oxygen therapy in children up to 3 years old with respiratory failure after extubation: a pilot prospective randomized clinical study. Pediatr Crit Care Med. (2015) 16:124–30. doi: 10.1097/PCC.0000000000000309
31. Ferguson LP, Walsh BK, Munhall D, Arnold JH. A spontaneous breathing trial with pressure support overestimates readiness for extubation in children. Pediatr Crit Care Med. (2011) 12:e330–5. doi: 10.1097/PCC.0b013e3182231220
32. Gatiboni S, Piva JP, Garcia PCR, Jonhston C, Hommerding P, Franz F, et al. Lack of accuracy of ventilatory indexes in predicting extubation success in children submitted to mechanical ventilation. Rev Bras Ter Intensiva. (2011) 23:199–206. doi: 10.1590/S0103-507X2011000200013
33. Johnston C, de Carvalho W, Piva J, Celiny P, Garcia R, Fonseca M. Risk factors for extubation failure in infants with severe acute bronchiolitis. Respir Care. (2010) 55:328−33.
34. Mayordomo-Colunga J, Medina A, Rey C, Concha A, Menéndez S, Arcos ML, et al. Non invasive ventilation after extubation in paediatric patients: a preliminary study. BMC Pediatr. (2010) 10:29. doi: 10.1186/1471-2431-10-29
35. Chavez A, dela Cruz R, Zaritsky A. Spontaneous breathing trial predicts successful extubation in infants and children. Pediatr Crit Care Med. (2006) 7:324–8. doi: 10.1097/01.PCC.0000225001.92994.29
36. Manczur TI, Greenough A, Pryor D, Rafferty GF. Assessment of respiratory drive and muscle function in the pediatric intensive care unit and prediction of extubation failure. Pediatr Crit Care Med. (2000) 1:124–6. doi: 10.1097/00130478-200010000-00006
37. Venkataraman ST, Khan N, Brown A. Validation of predictors of extubation success and failure in mechanically ventilated infants and children. Crit Care Med. (2000) 28:2991–6. doi: 10.1097/00003246-200008000-00051
38. Esteban A, Alía I, Tobin MJ, Gil A, Gordo F, Vallverdú I, et al. Effect of spontaneous breathing trial duration on outcome of attempts to discontinue mechanical ventilation. Am J Respir Crit Care Med. (1999) 159:512–8. doi: 10.1164/ajrccm.159.2.9803106
39. Baumeister BL, El-Khatib M, Smith PG, Blumer JL. Evaluation of predictors of weaning from mechanical ventilation in pediatric patients. Pediatr Pulmonol. (1997) 24:344–52. doi: 10.1002/(sici)1099-0496(199711)24:5<344::aid-ppul7>3.0.co;2-i
40. Khemani RG, Randolph A, Markovitz B. Corticosteroids for the prevention and treatment of post-extubation stridor in neonates, children and adults. Cochrane Database Syst Rev. (2008) 2:CD001000. doi: 10.1002/14651858.CD001000.pub3
41. Ouellette DR, Patel S, Girard TD, Morris PE, Schmidt GA, Truwit JD, et al. Liberation from mechanical ventilation in critically ill adults: an official American college of chest physicians/American thoracic society clinical practice guideline: inspiratory pressure augmentation during spontaneous breathing trials, protocols minimizing sedation, and noninvasive ventilation immediately after extubation. Chest. (2017) 151:166–80. doi: 10.1016/j.chest.2016.10.036
42. Esteban A, Frutos-Vivar F, Ferguson ND, Arabi Y, Apezteguía C, González M, et al. Noninvasive positive-pressure ventilation for respiratory failure after extubation. N Engl J Med. (2004) 350:2452–60. doi: 10.1056/NEJMoa032736
43. Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med. (1991) 324:1445–50. doi: 10.1056/NEJM199105233242101
44. Khemani RG, Sekayan T, Hotz J, Flink RC, Rafferty GF, Iyer N, et al. Risk factors for pediatric extubation failure: The importance of respiratory muscle strength. Crit Care Med. (2017) 45:e798–805. doi: 10.1097/CCM.0000000000002433
45. Moxham J, Goldstone J. Assessment of respiratory muscle strength in the intensive care unit. Eur Respir J. (1994) 7:2057–61.
Keywords: weaning, mechanical ventilation, extubation, pediatric, children, pediatric intensive care unit
Citation: Poletto E, Cavagnero F, Pettenazzo M, Visentin D, Zanatta L, Zoppelletto F, Pettenazzo A, Daverio M and Bonardi CM (2022) Ventilation Weaning and Extubation Readiness in Children in Pediatric Intensive Care Unit: A Review. Front. Pediatr. 10:867739. doi: 10.3389/fped.2022.867739
Received: 01 February 2022; Accepted: 04 March 2022;
Published: 01 April 2022.
Edited by:
Alfonso Galderisi, Hôpital Necker-Enfants Malades, FranceReviewed by:
Warwick Wolf Butt, Royal Children's Hospital, AustraliaCopyright © 2022 Poletto, Cavagnero, Pettenazzo, Visentin, Zanatta, Zoppelletto, Pettenazzo, Daverio and Bonardi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elisa Poletto, ZWxpc2Fwb2xldHRvODlAZ21haWwuY29t
†Elisa Poletto orcid.org/0000-0002-6609-9432
Francesca Cavagnero orcid.org/0000-0003-3480-8860
Marco Pettenazzo orcid.org/0000-0002-2588-3888
Davide Visentin orcid.org/0000-0002-7939-3729
Laura Zanatta orcid.org/0000-0002-4912-4827
Fabrizio Zoppelletto orcid.org/0000-0001-8095-7045
Andrea Pettenazzo orcid.org/0000-0001-8378-8961
Marco Daverio orcid.org/0000-0002-3127-8836
Claudia Maria Bonardi orcid.org/0000-0002-6266-3665
‡These authors have contributed equally to this work and share last authorship
 Elisa Poletto
Elisa Poletto Francesca Cavagnero
Francesca Cavagnero Marco Pettenazzo
Marco Pettenazzo Davide Visentin
Davide Visentin Laura Zanatta
Laura Zanatta Fabrizio Zoppelletto
Fabrizio Zoppelletto Andrea Pettenazzo
Andrea Pettenazzo Marco Daverio
Marco Daverio Claudia Maria Bonardi
Claudia Maria Bonardi