- 1Department of Cardiological, Thoracic and Vascular Sciences, and Public Health, University of Padova, Padova, Italy
- 2Surgical Oncology Unit, Veneto Institute of Oncology IOV-IRCCS, Padova, Italy
- 3Affidea Poliambulatorio Morgagni, Padova, Italy
Objective: The Mediterranean diet (MD) contributes to preventing numerous chronic diseases and has benefits on cognitive development. Adherence to the MD is associated with sleep quality and duration in adults and adolescents, but this association seems to have been little investigated in primary-school children. The aim of this cross-sectional study was to verify whether good sleep duration was associated with adherence to the MD.
Design: The study enrolled a sample of Italian primary school children. Their mothers were asked to answer an anonymous, self-administered questionnaire investigating the children's adherence to the MD (using the KidMed score) and variables related to their lifestyles, behavioral traits and socio-economic factors. Logistic regression models were developed to analyze the association between adherence to the MD, entered as the dependent variable, and adequacy of sleep duration.
Setting: Primary schools in Padova, Italy.
Subjects: 267 Italian 6-year-olds in their first year of primary school.
Results: The multivariate analysis showed an association between adherence to the MD and hours of sleep: for children with a good sleep duration, the odds ratio of a poor-to-moderate adherence to the MD was 0.282 (95% CI, 0.109–0.681, p < 0.05).
Conclusion: Ensuring an adequate sleep duration may be an important strategy for enhancing adherence to the MD. Sleep and dietary education should be included in future health promotion programs.
Statement of significance
Long sleep duration (≥10 h/day) is associated with lower odds of poor-to-moderate adherence to the Mediterranean diet (MD) in 6-year-olds children. These results suggest the importance to include sleep and dietary education in future health promotion programs.
Introduction
The Mediterranean diet (MD) is characterized by large amounts of vegetables, whole grains, fish and dairy products, the daily consumption of olive oil, and small amounts of refined carbohydrates and animal proteins (1). It is considered one of the healthiest in the world (2). In association with other prevention measures, the MD contributes over the lifespan to reducing the risk of chronic diseases and disabilities, and premature death (3–6). A healthy diet is associated with a better cognitive and academic performance in children and adolescents (7–9). Some studies have also suggested an association between adherence to the MD and sleeping habits, in terms of sleep quality and duration (10–13). A study conducted in UK women showed that fruit and vegetable intakes differed between sleep duration categories with women sleeping the recommended 7–9 h/day having the highest intake, in cross-sectional and prospective analyses (14). Using an experimental sleep restriction protocol among adolescents, Beebe et al. found that consumption of foods with a high glycemic index (GI) and glycemic load (GL) was higher in a sleep restriction condition (<6.5 h) compared to a healthy sleep condition (∼9 h) (15), subsequently diets with a high GI, high GL, or both, increase the risk of chronic lifestyle-related diseases, such as type 2 diabetes, coronary heart disease and gallbladder disease (16). A short sleep duration has often been found related to an unbalanced diet and unhealthy lifestyle in adults and adolescents (17), but this association has not been thoroughly investigated in children. The American National Sleep Foundation recommends that school-age children sleep 9–11 h a night (18), and this amount of sleep has also been associated with better cognition in children (19). Sleep deficiency in childhood might become increasingly important as there has been a rapid, marked decline in children's average sleep duration in recent decades (20). Several studies on children have also found screen-time negatively associated with sleep quality and sleep duration (21). Meanwhile, there has been a clear tendency worldwide in recent years to move away from the MD, especially among young people (22).
Unhealthy lifestyle factors make an important contribution to an individual's modifiable disease burden, and are consequently a major public health concern (23). Understanding which factors are associated with a poor adherence to the MD may therefore be crucial to addressing the issue of unhealthy lifestyles. The aim of this study was to verify whether adherence to the MD is associated with good sleep duration in a sample of 6-year-old children.
Materials and methods
Participants
A project named “Le Buone Abitudini [Healthy Habits]” was developed to promote a varied, healthy and nutritionally-balanced diet among primary-school children in the province of Padova (north-east Italy) in the academic year 2018–2019. Of the province's 69 state primary schools, 38 were invited to take part, and 14 agreed, participating with at least one class. The present cross-sectional study derives from a survey of the mothers of children in both the participating classes and other classes at the schools involved, before the Healthy Habits project started.
The study sample concerned 379 children in their first year of primary school (6–7 years old) in 21 classes at 14 different schools. For all children in the classes involved in the project, the parents were asked to give their written informed consent to their participation. The parents of 32 children refused, and their mothers were not asked to complete the questionnaire. Of the 347 questionnaires distributed, 299 were completed and returned to the study authors, but 32 were not included in our analysis because they had been answered by a person other than the mother. In all, 267 questionnaires were thus included in this study (Figure 1).
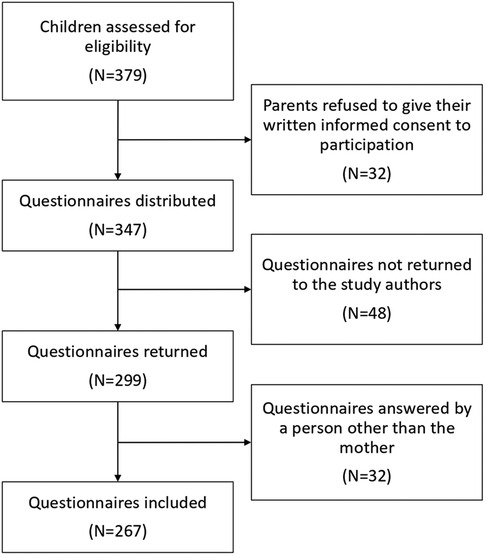
Figure 1. Flowchart diagram representing children lost to follow-up and included in the final analysis and the reasons for a drop-out.
Materials
The children's mothers were asked to anonymously answer a self-administered questionnaire investigating several variables relating to their children's lifestyles and behavioral traits, and the family's socio-economic situation. The questionnaire contained 34 multiple-choice items and touched on all the factors potentially associated with the risk of a poor adherence to the MD, i.e., demographics, family setting, and lifestyles (24).
Children's weight and height were collected by means of the questionnaire and their body mass index (BMI) was computed using the standard formula [weight(kg)/height(m)2], classifying the children according to the International Obesity Task Force cut-offs, as suggested by Cole et al. (25).
The “adherence to the MD” variable was derived from the Italian version of the KidMed index (26), developed to assess the factors that sustain or undermine the adoption of Mediterranean dietary patterns. The scores range from 0 to 12, based on a test containing 16 questions (those with a negative connotation vis-à-vis the MD are assigned a value of −1, and those with a positive connotation score +1). We classified KidMed scores of 8 or more as “good”, and scores of 7 or less as “poor-to-moderate”. The validity of the measures used in this study had been tested previously, and the KidMed index has demonstrated reliable psychometric properties (27).
The “hours of sleep” variable included sleep at night and naps during the day.
Children's behavioral traits were measured on the basis of the answers their mothers gave in the Italian version of the Strengths and Difficulties Questionnaire (SDQ) (28). The SDQ uses a 3-point Likert scale (from 0 = not true to 2 = very true), and consists of five sub-scales investigating: internalizing problems, externalizing problems, hyperactivity/inattention, peer relationship problems, and prosocial behavior. Risk tertiles are identified for each behavioral trait; the first tertile identifies children showing a given behavioral trait less, and the third those who showed it more.
For lifestyle factors other than eating habits, the questionnaire investigated whether the children engaged in any competitive sports (yes or no).
The questionnaire also covered socio-economic aspects regarding the children's mothers and their family environments, including: whether they had siblings (yes or no); the mother's marital status (married or unmarried, separated, divorced or widowed); and the family's disposable income, measured with the question “How do you make ends meet with your finances?” (very/quite easily or with some/great difficulty). The mother's health literacy was tested as well, using the Italian version of the Newest Vital Sign (NVS) (29), and scoring it as “adequate” (NVS scores 4 or 5) or “marginal/limited” (NVS scores 0–3).
Statistical methods
The proportions and 95% confidence intervals of children with a low adherence to the MD were calculated using binomial exact distribution. The associations between the adequacy of children's sleep duration (poor: <10 h, good: ≥10 h) and the observed categorical variables were tested with Pearson's chi-squared test.
Four different logistic regression models were developed to analyze the association between poor-to-moderate adherence to the MD, entered as the dependent variable, and adequacy of sleep duration. A simple univariate model was run first (Model 1). Then multivariate logistic regressions were implemented incrementally, adjusting the effect for different covariates: the children's sex and age (Model 2); the mothers' disposable income, marital status and health literacy (Model 3); and the children's ratings in the SDQ domains (prosocial behavior, peer or conduct problems, hyperactivity, emotional symptoms), sporting activity, body mass index (BMI) and siblings (Model 4). RStudio software was used for these analyses.
Ethical approval and consent to participation
The study was approved by the Padova Teaching Hospital's Ethical Committee (No. 4526/U6/18). The children's participation in the study was subject to the consent of the directors at the schools involved. If approved, the intervention program then became part of the school's teaching plan, which always has to be signed by parents at the start of each academic year. All parents of the children ultimately participating in the study then signed an informed consent form. All procedures also complied with the ethical standards of the Italian National Research Committee, and the 1964 Helsinki Declaration and subsequent revisions thereof, or comparable ethical standards.
Results
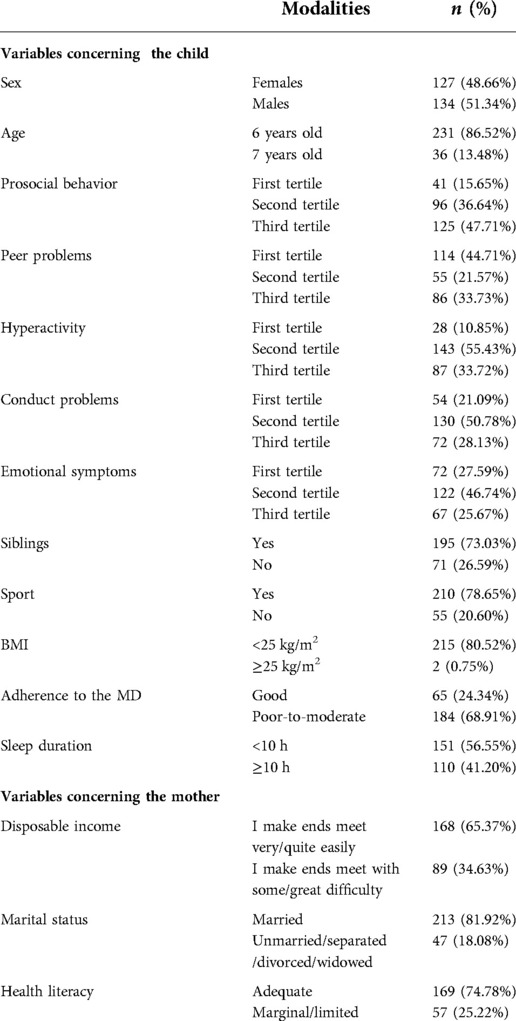
Our final sample included 267 children aged 6.13 ± 0.34 years (mean ± SD), with both sexes equally represented (48.7% females) (Table 1). Only one in four children (24.3%; 95% CI, 19.32–29.95) had a good adherence to the MD, and the proportion was similar in both sexes (25.2%; 95% CI, 17.92–33.67 in females vs. 24.6%; 95% CI, 17.60–32.81 in males). The mean hours of sleep were 9.52 h per day (95% CI, 9.43–9.61), and were much the same in both sexes (9.60; 95% CI, 9.46–9.74 in females vs. 9.44; 95% CI, 9.31–9.56 in males). The bivariate distribution of the children's sleep duration by good vs. poor-to-moderate adherence to the MD showed a significant difference (p 0.015) in the hours of sleep between the two KidMed groups (Table 2).
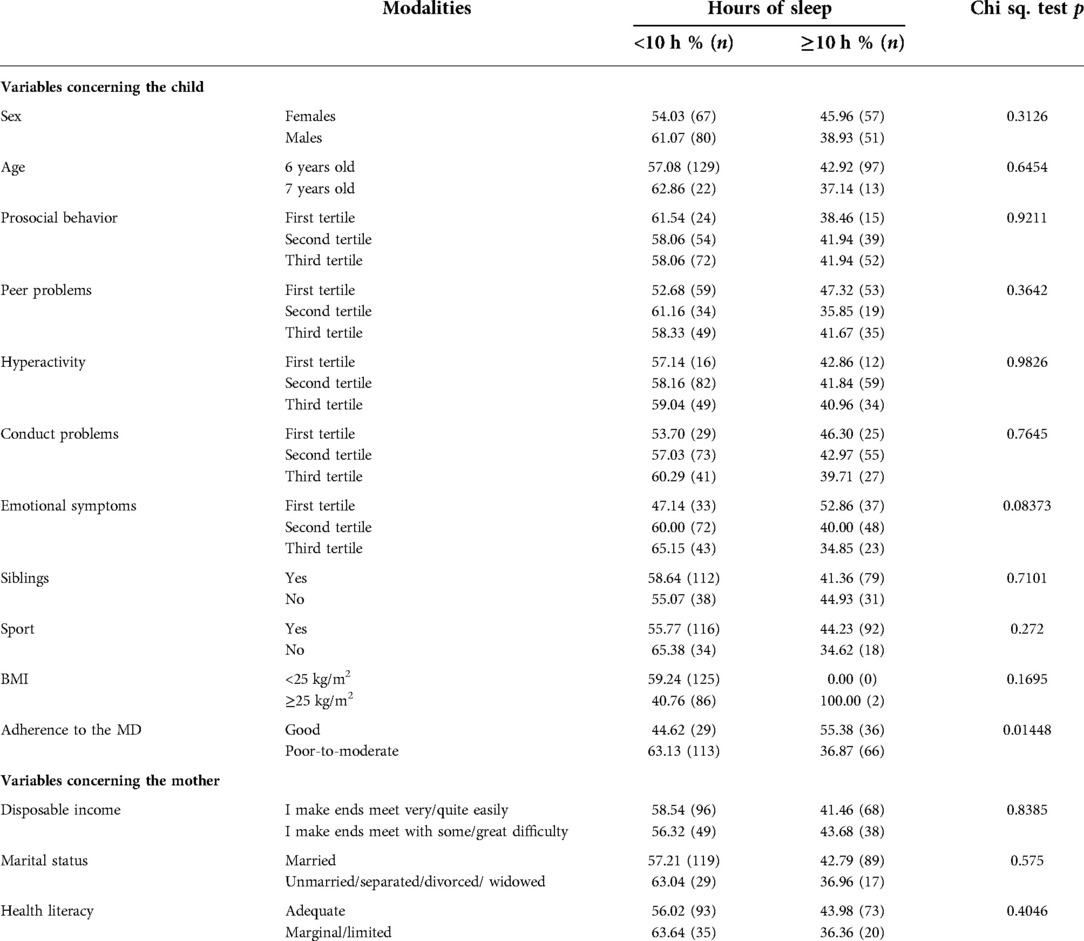
Table 2. Bivariate analysis. Distribution of hours of sleep among primary-school children by socio-demographic and lifestyle variables.
The multivariate analyses always showed an association between adherence to the MD and daily hours of sleep (Table 3): Model 1, unadjusted (OR 0.471; 95% CI, 0.263–0.834, p < 0.05); Model 2, adjusted for children's sex and age (OR 0.456; 95% CI, 0.253–0.816, p < 0.001); Model 3, adjusted for children's sex and age, and by mothers' disposable income, marital status, and health literacy (OR 0.456; 95% CI, 0.242–0.849, p < 0.05); Model 4, adjusted for children's sex, age, sport, BMI, siblings, and ratings in the SDQ domains, and for mothers' disposable income, marital status and health literacy (OR 0.282; 95% CI, 0.109–0.681, p < 0.05).
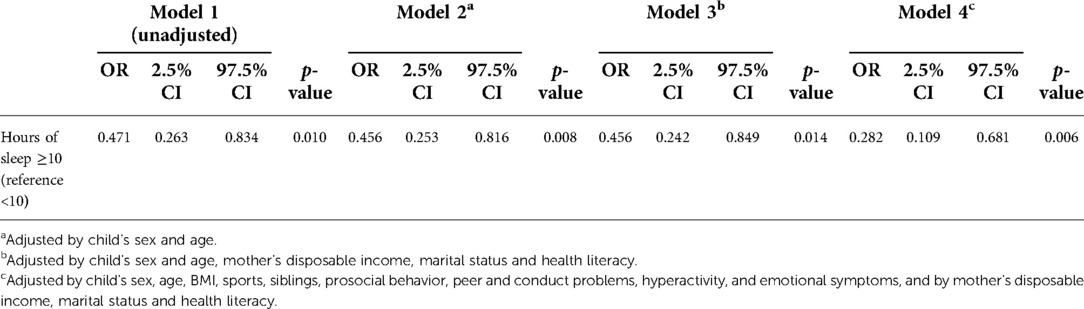
Table 3. Logistic multivariate models: dependent variable poor-to-moderate adherence to Mediterranean diet (KidMed score ≤7); independent variable (sleep ≥10 h/day); adjusted for different sets of covariates.
Discussion
This study aimed to assess the association between adherence to the MD and sleep duration in a sample of primary-school children, an age group in which this association has been under-investigated. We found that children who slept more had lower odds of poor-to-moderate adherence to the Mediterranean diet.
Two previous studies support the theory of a positive association between adherence to the MD and sleep duration: one performed in 2020 on 891 Portuguese children attending elementary school (30); and another conducted in Italy in 2017 on 690 greater children from 9 to 11 years old (17). In contrast, a Spanish study on 309 children aged 8–13 years found no such correlation between adherence to the MD and sleep duration (31).
Our findings suggest that the promotion of a healthy diet should also consider sleeping habits. Some dietary patterns and foods have revealed a sleep-modulating role due to the effect of certain nutrients on sleep regulation (32). Sleep has also been shown to influence eating behavior (33). Changes in sleeping habits and lack of sleep reportedly facilitate the ingestion of calories through several potential mechanisms, including: more time and opportunities for eating; psychological distress (prompting a preference for energy-dense foods); greater sensitivity to food reward; disinhibited eating; more energy needed to stay awake (34). Moreover, from a biological point of view, previous studies indicate that sleep deprivation results in changes in levels of several hormones, including leptin, ghrelin, insulin, cortisol, and growth hormone (35–37), and hormonal changes may contribute to selection of calorie-dense food, excessive food intake and changes in energy expenditure (38).
Encouraging healthy habits in children is a cost-effective strategy for promoting their cognitive development and keeping them healthy in later life—and sleep is known to have positive effects in developmental age. Magnetic resonance images of the brain of healthy 5- to 18-year-olds revealed a positive correlation between sleep duration on weekdays and the bilateral volume of the hippocampal body (39). In adolescents, sleep has shown an important role in cognitive development and mental well-being (40). A Canadian study found that children aged 7–11 who participated in a sleep education program called “Sleep for Success” extended their sleep duration and enhanced their sleep efficiency (41), with a significant improvement in their daytime functioning and academic performance (42, 43).
In conclusion, ensuring an adequate sleep duration may be an important strategy for enhancing adherence to the MD, and sleep education should be included in comprehensive healthy lifestyle promotion programs in future, alongside a healthy diet and adequate physical activity, as a relatively low-cost strategy to keep people healthy. Both healthy diet and adequate sleep could be promoted during childhood, for example through health promotion interventions in primary schools. The school setting can be an appropriate environment for assessing lifestyle, modifying misconducts, and educating students, while maintaining a stable contact with them. When aiming to improve children's sleeping and eating habits, interventions not only at school, but also in family settings have a greater likelihood of inducing behavioral changes, such as a longer sleep duration. Within this framework, schools and families are both optimal settings for programs aimed at improving children's lifestyle habits (44).
Some limitations need to be considered when interpreting the findings of the present study. For a start, the cross-sectional study design prevented us from establishing any causality for the significant association examined. It would be well worth seeking potential causal relationships and mechanisms, using appropriate study designs. Future randomized intervention trials are needed to test the effectiveness of extending children's hours of sleep in promoting their adoption of a healthier lifestyle and greater adherence to the MD. Second, our data on adherence to the MD and other variables were obtained by means of questionnaires, as we lacked the opportunity to obtain more objective evidence of the children's eating habits (such as biochemical markers). Our findings consequently suffer from the inherent limitations of self-reported data, such as the influence of social desirability. Third, the questionnaires did not aim to define a clinical diagnosis of sleep disorders or did not investigate comorbidities which can interrupt sleep duration (as rheumatoid arthritis or diabetes). Finally, another limitation of this study lies in the relatively small sample size, however it was calculated allowing to detect difference in diet adherence among sleep groups.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Padova Teaching Hospital's Ethical Committee (No. 4526/U6/18). The children's participation in the study was subject to the consent of the directors at the schools involved. If approved, the intervention program then became part of the school's teaching plan, which always has to be signed by parents at the start of each academic year. All parents of the children ultimately participating in the study then signed an informed consent form. All procedures also complied with the ethical standards of the Italian National Research Committee, and the 1964 Helsinki Declaration and subsequent revisions thereof, or comparable ethical standards. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
AB obtained funding, conceptualized the study, interpreted the data, drafted the manuscript, and approved the final manuscript as submitted. GG, CZ and SFM drafted the manuscript, and approved the final manuscript as submitted. CC performed the statistical analysis. FB and TB supervised the study, and approved the final manuscript as submitted. VB critically reviewed and revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by Despar Nordest.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Villani A, Sultana J, Doecke J, Mantzioris E. Differences in the interpretation of a modernized Mediterranean diet prescribed in intervention studies for the management of type 2 diabetes: how closely does this align with a traditional Mediterranean diet? Eur J Nutr. (2018) 58(4):1369–80. doi: 10.1007/s00394-018-1757-3
2. Willet WC, Sacks F, Trichopoulou A, Drescher G, Ferro-luzzi A, Helsing E, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. (1995) 61(6):1402S–6S. doi: 10.1093/ajcn/61.6.1402S
3. WHO. Diet, nutrition and the prevention of chronic disease: report of a joint WHO/FAO expert consultation. WHO Technical Report Series 916 (2003).
4. Tuttolomondo A, Casuccio A, Buttà C, Pecoraro R, Di Raimondo D, Della Corte V, et al. Mediterranean diet in patients with acute ischemic stroke: relationships between Mediterranean Diet score, diagnostic subtype, and stroke severity index. Atherosclerosis. (2015) 243(1):260–7. doi: 10.1016/j.atherosclerosis.2015.09.017
5. Tuttolomondo A, Di Raimondo D, Casuccio A, Velardo M, Salamone G, Cataldi M, et al. Mediterranean diet adherence and congestive heart failure: relationship with clinical severity and ischemic pathogenesis. Nutrition. (2020) 70:110584. doi: 10.1016/j.nut.2019.110584
6. Tuttolomondo A, Di Raimondo D, Casuccio A, Velardo M, Salamone G, Arnao V, et al. Relationship between adherence to the Mediterranean Diet, intracerebral hemorrhage, and its location. Nutr Metab Cardiovasc Dis. (2019) 29(10):1118–25. doi: 10.1016/j.numecd.2019.06.010
7. Nyaradi A, Li J, Hickling S, Whitehouse AJO, Foster JK, Oddy WH. Diet in the early years of life influences cognitive outcomes at 10 years: a prospective cohort study. Acta Paediatr. (2013) 102:1165–73. doi: 10.1111/apa.12363
8. Burrows T, Goldman S, Pursey K, Lim R. Is there an association between dietary intake and academic achievement: a systematic review. J Hum Nutr Diet. (2017) 30:117–40. doi: 10.1111/jhn.12407
9. Adelantado-Renau M, Beltran-Valls MR, Esteban-Cornejo I, Martinez-Vizcaino V, Santaliestra-Pasias AM, Moliner-Urdiales D. The influence of adherence to the Mediterranean diet on academic performance is mediated by sleep quality in adolescents. Acta Paediatr. (2019) 108(2):339–46. doi: 10.1111/apa.14472
10. Muscogiuri G, Barrea L, Aprano S, Framondi L, Di Matteo R, Laudisio D, et al. Sleep quality in obesity: does adherence to the Mediterranean diet matter? Nutrients. (2020) 12(5):1364. doi: 10.3390/nu12051364
11. Godos J, Ferri R, Caraci F, Cosentino FII, Castellano S, Galvano F, et al. Adherence to the Mediterranean Diet is associated with better sleep quality in Italian adults. Nutrients. (2019) 11(5):976. doi: 10.3390/nu11050976
12. Rosi A, Giopp F, Milioli G, Melegari G, Goldoni M, Parrino L, et al. Weight status, adherence to the Mediterranean diet, physical activity level, and sleep behaviour of Italian junior high school adolescents. Nutrients. (2020) 12(2):478. doi: 10.3390/nu12020478
13. Gianfreddi V, Nucci D, Tonzani Amodeo R, Benvenuti AL, Villarini M, Moretti M. Sleep disorder, Mediterranean diet and learning performance among nursing students: inSOMNIA, a cross-sectional study. Ann Ig. (2018) 30(6):470–81. doi: 10.7416/ai.2018.224730614496
14. Noorwali EA, Hardie LJ, Cade JE. Recommended sleep duration is associated with higher consumption of fruits and vegetables; cross-sectional and prospective analyses from the UK Women’s Cohort Study. Sleep Sci Pract. (2018) 2:13. doi: 10.1186/s41606-018-0032-0
15. Beebe DW, Simon S, Summer S, Hemmer S, Strotman D, Dolan LM. Dietary intake following experimentally restricted sleep in adolescents. Sleep. (2013) 36(6):827–34. doi: 10.5665/sleep.2704
16. Barclay AW, Petocz P, McMillan-Price J, Flood VM, Prvan T, Mitchell P, et al. Glycemic index, glycemic load, and chronic disease risk–a meta-analysis of observational studies. Am J Clin Nutr. (2008) 87(3):627–37. doi: 10.1093/ajcn/87.3.627
17. Rosi A, Calestani MV, Parrino L, Milioli G, Palla L, Volta E, et al. Weight status is related with gender and sleep duration but not with dietary habits and physical activity in primary school Italian children. Nutrients. (2017) 9(6):579. doi: 10.3390/nu9060579
18. Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep foundation's updated sleep duration recommendations: final report. Sleep Health. (2015) 1:233–43. doi: 10.1016/j.sleh.2015.10.004
19. Walsh J, Barnes JD, Cameron JD, Goldfield GS, Chaput JP, Gunnell KE, et al. Associations between 24 hour movement behaviours and global cognition in US children: a cross-sectional observational study. Lancet Child Adolesc Health. (2018) 2(11):783–91. doi: doi: 10.1016/S2352-4642(18)30278-5
20. Matricciani L, Olds T, Petkov J. In search of lost sleep: secular trends in the sleep time of school-aged children and adolescents. Sleep Med Rev. (2012) 16(3):203–11. doi: 10.1016/j.smrv.2011.03.005
21. Tambalis KD, Panagiotakos DB, Psarra G, Sidossis LS. Screen time and its effect on dietary habits and lifestyle among schoolchildren. Cent Eur J Public Health. (2020) 28(4):260–6. doi: 10.21101/cejph.a6097
22. Nylund Sørensen LM, Aamodt G, Brantsæter AL, Meltzer HM, Papadopoulou E. Diet quality of Norwegian children at 3 and 7 years: changes, predictors and longitudinal association with weight. Int J Obes. (2022) 46(1):10–20. doi: 10.1038/s41366-021-00951-x
23. WHO. Global health risks: Mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization (2009).
24. Buja A, Grotto G, Brocadello F, Sperotto M, Baldo V. Primary school children and nutrition: lifestyles and behavioral traits associated with a poor-to-moderate adherence to the Mediterranean diet. A cross-sectional study. Eur J Pediatr. (2020) 179:827–34. doi: 10.1007/s00431-020-03577-9
25. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. (2000) 320(7244):1240–3. doi: 10.1136/bmj.320.7244.1240
26. Serra-Majem L, Ribas L, Ngo J, Ortega RM, Garcia A, Perez-Rodrigo C, et al. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality index in children and adolescents. Public Health Nutr. (2004) 7(7):931–5. doi: 10.1079/PHN2004556
27. Zurita-Ortega F, San Román-Mata S, Chacón-Cuberos R, Castro-Sánchez M, Muros JJ. Adherence to the Mediterranean diet is associated with physical activity, self-concept and sociodemographic factors in university students. Nutrients. (2018) 10(8):966. doi: 10.3390/nu10080966
28. Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. (1997) 38:581–6. doi: 10.1111/j.1469-7610.1997.tb01545.x
29. Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. (2005) 3:514–22. doi: 10.1370/afm.405
30. Santos Marques GF, Oliveira Pinto SM, Rodrigues da Silva Reis AC, Barbosa Martins TD, da Conceição AP, Vieira Pinheiro AR. Adherence to the Mediterranean diet in elementary school children (1st cycle). Rev Paul Pediatr. (2021) 39:e2019259. doi: 10.1590/1984-0462/2021/39/2019259
31. Fernández-Iglesias R, Álvarez-Pereira S, Tardón A, Fernández-García B, Iglesias-Gutiérrez E. Adherence to the Mediterranean diet in a school population in the principality of Asturias. Nutrients. (2021) 13(5):1507. doi: 10.3390/nu13051507
32. St-Onge MP, Mikic A, Pietrolungo CE. Effects of diet on sleep quality. Adv Nutr. (2016) 7(5):938–49. doi: 10.3945/an.116.012336
33. Chaput JP, Katzmarzyk PT, LeBlanc AG, Tremblay MS, Barreira TV, Broyles ST, et al. Associations between sleep patterns and lifestyle behaviors in children: an international comparison. Int J Obes Suppl. (2015) 5(Suppl 2):S59–S65. doi: 10.1038/ijosup.2015.21
34. Chaput JP. Sleep patterns, diet quality and energy balance. Physiol Behav. (2014) 134:86–91. doi: 10.1016/j.physbeh.2013.09.006
35. Spiegel K, Leproult R, L’Hermite-Baleriaux M, Copinschi G, Penev PD, Van Cauter E. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab. (2004) 89:5762–71. doi: 10.1210/jc.2004-1003
36. Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. (1999) 354:1435–9. doi: 10.1016/S0140-6736(99)01376-8
37. Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. (2004) 1:e62. doi: 10.1371/journal.pmed.0010062
38. Taheri S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Arch Dis Child. (2006) 91:881–4. doi: 10.1136/adc.2005.093013
39. Taki Y, Hashizume H, Thyreau B, Sassa Y, Takeuchi H, Wu K, et al. Sleep duration during weekdays affects hippocampal gray matter volume in healthy children. NeuroImage. (2012) 60(1):471–5. doi: 10.1016/j.neuroimage.2011.11.072
40. Tarokh L, Saletin JM, Carskadon MA. Sleep in adolescence: physiology, cognition and mental health. Neurosci Biobehav Rev. (2016) 70:182–8. doi: 10.1016/j.neubiorev.2016.08.008
41. Gruber R, Somerville G, Bergmame L, Fontil L, Paquin S. School-based sleep education program improves sleep and academic performance of school-age children. Sleep Med. (2016) 21:93–100. doi: 10.1016/j.sleep.2016.01.012
42. Gruber R, Cassoff J, Frenette S, Wiebe S, Carrier J. Impact of sleep extension and restriction on children's Emotional lability and impulsivity. Pediatrics. (2012) 130:e1155–61. doi: 10.1542/peds.2012-0564
43. Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Dev. (2003) 74(2):444–55. doi: 10.1111/1467-8624.7402008
Keywords: sleep, nutrition, children, lifestyles, Mediterranean diet
Citation: Buja A, Grotto G, Zampieri C, Mafrici SF, Cozzolino C, Baldovin T, Brocadello F and Baldo V (2022) Is adherence to the Mediterranean diet associated with good sleep duration in primary-school children?. Front. Pediatr. 10:959643. doi: 10.3389/fped.2022.959643
Received: 1 June 2022; Accepted: 5 October 2022;
Published: 1 November 2022.
Edited by:
Nicholas P. Hays, Nestle, SwitzerlandReviewed by:
Lovro Štefan, University of Zagreb, CroatiaAntonino Tuttolomondo, University of Palermo, Italy
© 2022 Buja, Grotto, Zampieri, Mafrici, Cozzolino, Baldovin, Brocadello and Baldo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alessandra Buja YWxlc3NhbmRyYS5idWphQHVuaXBkLml0
Specialty Section: This article was submitted to Children and Health, a section of the journal Frontiers in Pediatrics
 Alessandra Buja
Alessandra Buja Giulia Grotto
Giulia Grotto Chiara Zampieri1
Chiara Zampieri1 Tatjana Baldovin
Tatjana Baldovin Filippo Brocadello
Filippo Brocadello Vincenzo Baldo
Vincenzo Baldo