- 1PediatricNeurology, Pediatric University Department, Azienda Ospedaliero Universitaria Pisana, University of Pisa, Pisa, Italy
- 2Pediatric Clinic, Pediatric University Department, Azienda Ospedaliero Universitaria Pisana, University of Pisa, Pisa, Italy
- 3Department of Pediatrics, Child Neurology Division, Sapienza University Rome, Roma, Italy
- 4Psychiatric Clinic, Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy
- 5Division of Statistical Support to Clinical Studies, Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy
- 6“IRCCS Istituto Giannina Gaslini” member of ERN-Epicare, Genova, Italy
- 7Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health, University of Genova, Genova, Italy
Introduction: Essential headache is one of the main causes of pain in children, and has an important impact on their quality of life. In children with essential headaches play an important role in both triggers like stress, excessive use of video terminals, or physical fatigue but also comorbidities like anxiety, depression, and sleep disturbances. CoViD-19 Pandemic was very stressful, especially for children, and amplified all headache triggers and comorbidities.
Study objective: In this work, we studied the aspects concerning the headache,lifestyle, habits, and mental health of children before, during, and after the lockdown and the differences between some categories (selected by age, gender, and headache status before the lockdown).
Methods: This study was conducted on 90 patients with primary headaches followed at the AOUP Neuropediatrics Clinic from January 2018 to March 2022. Participants answered a questionnaire of 21 questions. For every question, the answer was divided into three periods: before, during, or after the lockdown. All dates have been converted and inserted into a database and we used SPSS technology for statistical analysis.
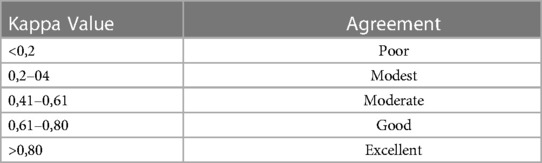
Results: In our study, 51,1% were females and 48,9% were males and there was a prevalence of adolescents (56,7%) compared to children from 5 to 11 years (43,3%). Regarding the headache onset, 77,7% of patients started to suffer from headaches before 10 years, moreover, 68,9% had familiarity with the headache. Using Cohen's K- Concordance Test, we performed a Concordance Analysis, studying the questions in the three periods above mentioned: considering headache characteristics there is poor concordance about the trend of headache; modest concordance (K: 0,2–0,4) about the frequency and the type (migraine or tension headache); moderate concordance (K: 0,41–0,61) about the acute use of analgesic. Analyzing lifestyle the lockdown had a significant impact on sports (practiced much less) and on the use of video terminals (used much more).
Conclusion: The pandemic and lockdown aren't events that led to strong and unidirectional responses in patients, there is great variability in the answers about headache, lifestyle, and psychology, and each patient had individualized reactions. However, these considerations are not applied to physical activity and the use of video terminals, because both have been inevitably modified by the pandemic situations and so were not affected by subjective influence.
Introduction
Headache is defined as a limited or diffuse, continuous or sporadic painful sensation affecting the head. The International Classification of Headache Disorders (ICHD), now in its 3rd edition, divided headaches into three principal categories: Primary headaches, Secondary Headaches, Painful cranial neuropathies, and facial pain (1). Primary Headache (PH) is a paroxysmal multifactorial and complex disorder, characterized by the recurrence of symptoms interspersed with physical and mental well-being (2). ICHD-3 divides Primary Headaches into four principal types: Migraine, Tension-type headache, Trigeminal autonomic cephalalgia, and Other primary headache disorders (1).
The diagnosis is clinical, based on accurate anamnesis and the general and neurological physical examination (3, 4). It's one of the three main causes of pediatric pain after muscular-skeletal and abdominal pain. Primary Headache is also the first reason for absenteeism from school and the most frequent neurological cause of access to the pediatric emergency room. Due to her debilitating nature and the repercussions on the family and school, headache has a significant social impact in this life period.
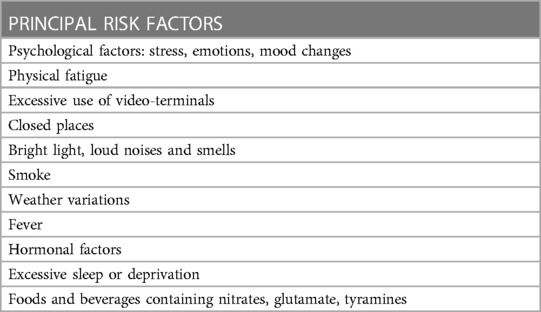
The prevalence of Primary headaches in childhood varies from 5.9% to 82%, increasing progressively with age and reaching a peak around 13 years (5). Moreover, the prevalence of headaches increases more in girls (ratio of 3: 1) during puberty (6). Specific triggers such as stress, sleep deprivation, fever, loud noises, starvation, abuse of technological devices, etc. can cause or aggravate headache episodes going to act as a stimulus for the activation of pathogenetic mechanisms. Recognizing and preventing them is essential to reduce the frequency of attacks and improve the patient's quality of life (Table 1). Avoiding these triggers should reduce their frequency and improve the patient's quality of life (7–9). The Covid-19 pandemic has been a stressful event that has disrupted everyone's life with different psychological reactions. this event can be taken as an example to understand how stressful and psychological factors can influence headaches in a specific age group (10). In particular, regarding childhood primary headaches, some studies have evaluated the short and long-term effects of the lockdown; the short-term effects seem to be beneficial for headaches and patients improve activating coping mechanisms (11, 12).
In the long term, patients report a worsening of headaches, related to sleep disturbances, dietary changes, increased stress, anxiety, and depression, with the potential to evolve into a chronic form. This information clarifies how lifestyle changes can affect headaches (13, 14).
The objective of the study: This is a retrospective study to value the clinical differences of primary headaches in a pediatric population concerning the Covid-19 pandemic.
The primary outcomes of this study were to evaluate the variations of primary headache frequency and medication use in three periods: before, during, and after lockdown; furthermore, if these changes are statistically correlated with lifestyle changes due to restrictive measures of the Covid-19 emergency. A secondary outcome was to value the differences in these parameters in school-age children and adolescents.
Materials and methods
Population
We included n° 90 patients from 5 to 18 years old with a diagnosis of headache (migraine, migraine with aura, TTH) followed in Neuropediatric of the University Hospital of Pisa from January 2018 to March 2022.
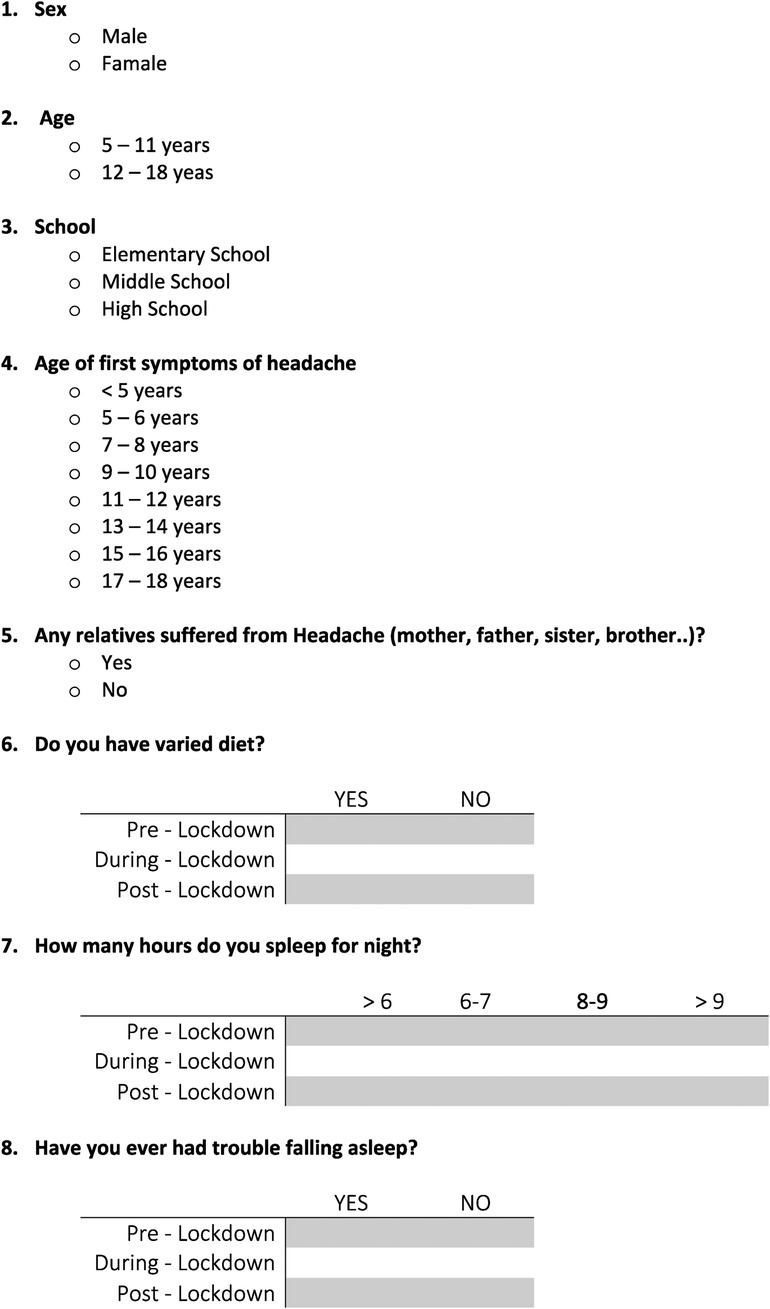
The patients were divided into different categories based on: (1) Age: children (5–11 years old) and adolescents (12–18 years old); (2) Sex: female and male; (3) School attended: elementary school, middle school or high school; (4) Age of the primary headache onset: before 10 years old and after 10 years old; (5) Familiarity: present or absent.
Analysis tools
A questionnaire with 21 questions, made ad hoc by the authors, was sent by e-mail. All the 90 patients included in the study completed the questionnaire, responding to all questions. Parents helped children (5–8 years) answer the questionnaire, reading the questions together and evaluating the best answer together.
The first three questions related to demographic data: age, sex, and school attended. The next two inquired about the age of onset of primary headache and familiarity. The last 16 questions investigated different elements: characteristics of the primary headache, lifestyle, and psychological status of the patients. Each question was asked for the three periods: before, during, or after the lockdown. All patients signed informed consent to the study (Figure 1).
Statistical analysis
Categorical data were described by absolute and relative (%) frequency. To analyze the concordance between categorical repeated measures Cohen's test was performed. All analyzes were carried out with SPSS v.28 technology (Table 2).
Results
Population characteristics
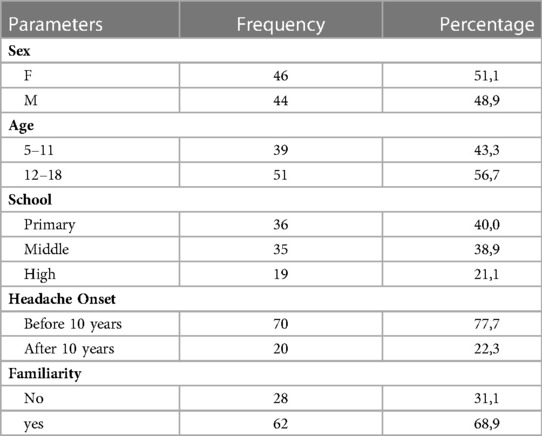
In our study 51.1% of the population was female. Regarding age, we found a prevalence of adolescents (56.7%) compared to children aged 5 to 11 (43.3%). 40% of patients attended Primary school, 38,9% Middle school, and 21,1% High School. The children with primary headache onset before 10 years were 77.7%, and those with onset after 10 years were 22.3%. Finally, 68.9% of patients had at least one family member who suffers or had suffered from a headache (Table 3).
Concordance analysis
Headache
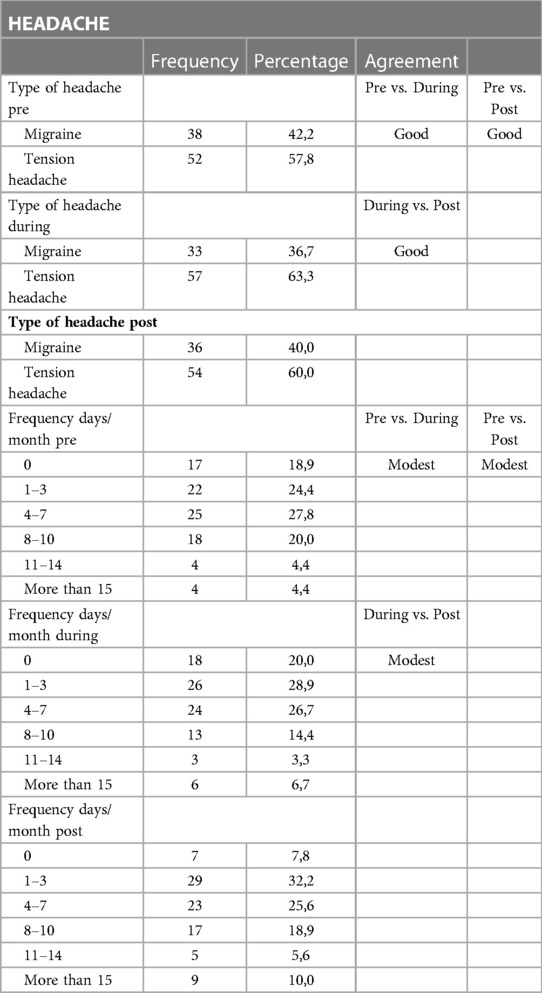
We found a good concordance for migraine with or without aura or tension-type headaches in the three periods. Children with migraine were 42.2% pre-lookdown, 36.7% during the lockdown, and 40% post-lookdown. We concluded that there wasn't a significant variation in the type of primary headache in the three periods and tensive-type headache remained the most widespread type of headache (Table 4).
Regarding the frequency of primary headaches, we have identified six categories (shown in Table 2), without finding statistically significant differences before, during, and after the lockdown. The biggest difference regards the category of those who have never had a headache in the two periods “during and post-lockdown”. The percentage of this response goes from 20% to 7.8%, highlighting a trend of increasing headache attendance when activities resume. We supposed that the cause could be attributable to the increased environmental demands that were triggered in some subjects.
Drugs
We analyzed the use of drugs for primary headache both in acute, during headache attack, and for prophylaxis, to prevent the exacerbation; we found a moderate concordance between the periods “pre” and “during” lockdown and a modest concordance comparing “pre” and “post” lockdown or “during” and “post” lockdown. Furthermore, in the questionnaire, we asked those who used prophylactic drugs to list the type of drug used. We also evaluated whether the lookdown had increased the need for psychotherapy but the concordance between the three periods was moderate. 10 patients used psychotherapy before the lockdown and only 2 were added in the post-period. These 10 patients didn't have any certified psychiatric pathology (Table 5).
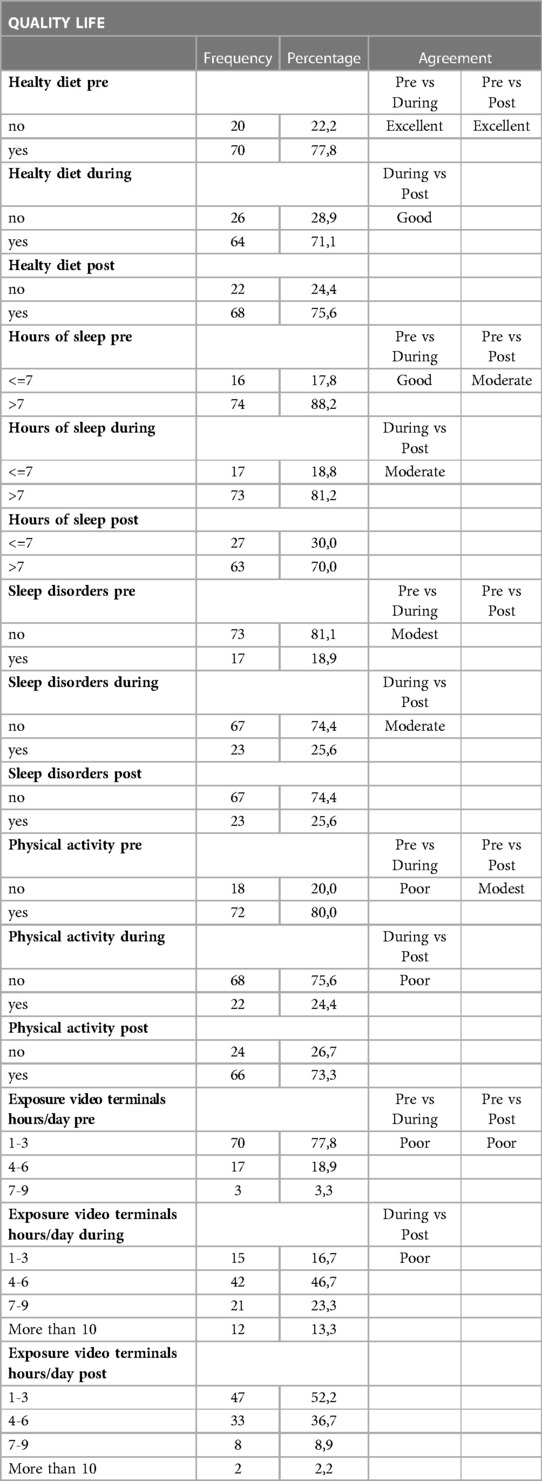
Quality life
We found excellent concordance between the periods “pre” and “during” lockdown and “pre” and “post” lockdown and good concordance comparing the periods “during” and “post” lockdown. There was a trend towards a less healthy diet during the lockdown, but the change was not significant (Table 6).
The hours of sleep were distinguished in less or more than 7 h per night and we found a good concordance between “pre” and “during” lockdown, while a moderate concordance was found between “pre” and “post” lockdown or “ during” and “post” lockdown. Overall, there is a progressive increase in patients who sleep less, going from 17.8% to 30% in the activity recovery phase.
Regarding the quality of sleep, we asked if the patients had difficulty falling asleep or if they were subject to nocturnal awakenings. From “pre” to “during” lockdown, patients with sleep problems increased from 18.9% to 25.6% and this situation remained unchanged even in the “post”. About video terminals, there was a significant increase in hours of exposure during the lockdown, attributable both to online lessons and to the absence of alternative activities. We divided the exposure to video terminals into four categories: 1–3 h a day, 4–6 h a day, 7–9 h per day, and more than 10 h a day. Patients who used electronic devices for 7–9 h per day increased from 3,3% in “pre” lockdown to 13,3% during the lockdown and decreased again to 2,2% in post-lockdown.
Finally, we stratified the subjects according to gender (males and females) and age group (5–11 and 12–18) and performed a stratified analysis considering the responses given by the patients to the question on headache self-rating. The variability in this response is greater in females and adolescents, probably due to the different sensitivity of females and adolescents towards an event such as leading to a radical change in habits and sociability.
Discussion
Data analysis has highlighted some significant aspects of headaches in the periods evaluated. First, the large variability of many of the categories analyzed in the absence of a unidirectional trend.
In absolute terms, in the post-lockdown period, there was a slightly worsening trend in headaches compared to the pre-lockdown period, although in the absence of statistical significance, there are some subjects whose headaches improved during the lockdown period and others whose headaches got worse, according to the study by Dellavalle G. et al.l (15). The cases which presented a worsening headache go from 22.2% to 35.6%, compared to subjects who have an improvement in headache, who instead increased from 31.1% to 35.6%, even if there is no statistical significance. Probably the first group is subjects who suffered from a situation of environmental stress (school, sport, friendships, etc.), which failed with the lockdown. Conversely, the second group probably suffered more than the others from the discomfort caused by the restrictions resulting in the worsening of their headaches.
Considering the specific categories, adolescents and women were more affected by the influence of the lockdown, probably due to a greater sensitivity of these categories to the changes induced by the pandemic period (16, 17).
The only aspects that have undergone a statistically significant change are physical activity and hours of use of video terminals (18).
For the other lifestyle elements examined, such as nutrition, sleep, etc. no statistically significant changes were found (19, 20).
From all this, it can be concluded that the pandemic cannot be considered an event that induces a one-way and unambiguous variation toward the worsening of the headache. There are subjective factors that influence the response variably even in the presence of the same environmental stress factor.
Another interesting element that emerges is the failure to return to pre-pandemic values of headaches in the period following the lockdown. We can hypothesize that the population examined not only felt the effects of an extreme condition such as the lockdown but also that the psychological and social consequences persist even after the end of the lockdown.
Conclusions
The Covid-19 pandemic was a dramatic event that radically changed people's lifestyles. In this context of sudden and prolonged restrictions, we have evaluated how sudden changes in routine habits ve affected the course of headaches.
Although lifestyle changes were common for all, there is not a single direction from the course of the headaches. The answers provided in the questionnaire are characterized by wide variability and only a slight variation in absolute value can be observed.
The pre-pandemic state of the headache also depended on the context so the improvement or worsening during the lockdown varied according to the presence of other stress and subjective psychological factors. The only exceptions are physical activity and abuse of video terminals which can be taken as examples of aspects whose variation is unidirectional and guided by the circumstance of confinement and not by the subjective response.
What emerges is the importance of evaluating the patient in all its complexity, since the treatment of any comorbidities, such as psychological problems and the correction of some lifestyles, are essential to obtain an appropriate clinical response.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
AB and IR: conceptualized and designed the study, drafted the initial manuscript, and contributed to data collection. AO, GD, and TB reviewed and critically revised the final manuscript. GM and RM performed the statistical analysis. AO, DP, and AB: study design, data interpretation, and manuscript revision. PS and AS: study design, supervision, and manuscript revision. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors thank the Italian Ministry of Health-Ricerca Corrente 2023.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at https://www.frontiersin.org/articles/10.3389/fped.2023.1166984/full#supplementary-material
References
1. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition. Cephalalgia. (2018) 38(1):1–211. doi: 10.1177/0333102417738202
2. Schor LI, Pearson MS, Shapiro RE, Zhang W, Miao H, Burish MJ, et al. Cluster headache epidemiology including pediatric onset, sex, and ICHD criteria: results from the international cluster headache questionnaire. Headache. (2021) 61(10):1511–20. doi: 10.1111/head.14237
3. Panda PK, Ramachandran A, Sharawat IK, Bhat NK Feasibility, utility, and interrater reliability of the cluster headache severity scale, cluster headache quality of life, cluster headache Index, and 6-item headache impact test in pediatric cluster headache. J Child Neurol. (2022) 37(10–11):825–32. doi: 10.1177/08830738221114220
4. Park EG, Yoo IH. The diagnostic values of red flags in pediatric patients with headache. Brain Dev. (2022) 44(8):512–9. doi: 10.1016/j.braindev.2022.04.008
5. Papetti L, Di Loro PA, Tarantino S, Grazzi L, Guidetti V, Parisi P, et al. I stay at home with a headache. A survey to investigate how the lockdown for COVID-19 impacted headaches in Italian children. Cephalalgia. (2020) 40(13):1459–73. doi: 10.1177/0333102420965139
6. Babineau SE, Green MW. Headaches in children. Continuum (Minneap Minn). (2012) 18(4):853–68. doi: 10.1212/01.CON.0000418647.77773.4e
7. Roth-Isigkeit A, Thyen U, Stöven H, Schwarzenberger J, Schmucker P. Pain among children and adolescents: restrictions in daily living and triggering factors. Pediatrics. (2005) 115(2):e152–62. doi: 10.1542/peds.2004-0682
8. Bigal ME, Lipton RB. The epidemiology, burden, and comorbidities of migraine. Neurol Clin. (2009) 27(2):321–34. doi: 10.1016/j.ncl.2008.11.011
9. Ackley E, Clementi MA, Yonker ME. Headache and sleep disturbances in the pediatric population. Semin Pediatr Neurol. (2021) 40:100924. doi: 10.1016/j.spen.2021.100924
10. Orsini A, Corsi M, Pedrinelli V, Santangelo A, Bertelloni C, Dell'Oste V, et al. Post-traumatic stress, anxiety, and depressive symptoms in caregivers of children tested for COVID-19 in the acute phase of the Italian outbreak. J Psychiatr Res. (2021) 135:256–63. doi: 10.1016/j.jpsychires.2021.01.024
11. Webster KM, Sun M, Crack P, O'Brien TJ, Shultz SR, Semple BD, et al. Inflammation in epileptogenesis after traumatic brain injury. J Neuroinflammation. (2017) 14(1):10. doi: 10.1186/s12974-016-0786-1
12. Verhagen IE, van Casteren DS, Lentsch SdV, Terwindt GM, et al. Effect of lockdown during COVID-19 on migraine: a longitudinal cohort study. Cephalalgia. (2021) 41(7):865–70. doi: 10.1177/0333102420981739
13. Daniunaite I, Truskauskaite-Kuneviciene I, Thoresen S, Zelviene P, Kazlauskas E, et al. Adolescents amid the COVID-19 pandemic: a prospective study of psychological functioning. Child Adolesc Psychiatry Ment Health. (2021) 15(1):45. doi: 10.1186/s13034-021-00397-z
14. Gonzalez-Martinez A, Planchuelo-Gómez Á, Guerrero ÁL, García-Azorín D, Santos-Lasaosa S, Navarro-Pérez MP, et al. Evaluation of the impact of the COVID-19 lockdown in the clinical course of migraine. Pain Med. (2021) 22(9):2079–91. doi: 10.1093/pm/pnaa449
15. Dallavalle G, Pezzotti E, Provenzi L, Toni F, Carpani A, Borgatti R, et al. Migraine symptoms improvement during the COVID-19 lockdown in a cohort of children and adolescents. Front Neurol. (2020) 11:579047. doi: 10.3389/fneur.2020.579047
16. Magson NR, Freeman JYA, Rapee RM, Richardson CE, Oar EL, Fardouly J, et al. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J Youth Adolesc. (2021) 50(1):44–57. doi: 10.1007/s10964-020-01332-9
17. Jones EAK, Mitra AK, Bhuiyan AR. Impact of COVID-19 on mental health in adolescents: a systematic review. Int J Environ Res Public Health. (2021) 18(5):48–60. doi: 10.3390/ijerph18052470
18. Schmidt SCE, Anedda B, Burchartz A, Eichsteller A, Kolb S. Physical activity and screen time of children and adolescents before and during the COVID-19 lockdown in Germany: a natural experiment. Sci Rep. (2020) 10(1):21780. doi: 10.1038/s41598-020-78438-4
19. Di Renzo L, Gualtieri P, Pivari F, Soldati L, Attinà A, Cinelli G, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. (2020) 18(1):229. doi: 10.1186/s12967-020-02399-5
Keywords: headaches, COVID-19, lockDown, pandemic, video-terminal
Citation: Bonuccelli A, Depietri G, Baldaccini T, Ricciutelli I, Peroni D, Spalice A, Massimetti G, Morganti R, Orsini A and Striano P (2023) Essential headaches in developmental age: What is changed before, during and after the lockdown for COVID-19 pandemic. Clinical study. Front. Pediatr. 11:1166984. doi: 10.3389/fped.2023.1166984
Received: 15 February 2023; Accepted: 31 March 2023;
Published: 25 April 2023.
Edited by:
Kette D. Valente, University of São Paulo, BrazilReviewed by:
Silvia Vincentiis, University of São Paulo, BrazilSebastian Ortiz, Filadelfia, Denmark
Jaime Carrizosa, University of Antioquia, Colombia
© 2023 Bonuccelli, Depietri, Baldaccini, Ricciutelli, Peroni, Spalice, Massimetti, Morganti, Orsini and Striano. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alessandro Orsini YW9yc2luaS5tZEBnbWFpbC5jb20=
Specialty Section: This article was submitted to Pediatric Neurology, a section of the journal Frontiers in Pediatrics
 Alice Bonuccelli
Alice Bonuccelli Greta Depietri
Greta Depietri Tommaso Baldaccini
Tommaso Baldaccini Irene Ricciutelli2
Irene Ricciutelli2 Diego Peroni
Diego Peroni Riccardo Morganti
Riccardo Morganti Alessandro Orsini
Alessandro Orsini Pasquale Striano
Pasquale Striano