- 1Department of Pediatric Surgery, Nagoya University Graduate School of Medicine, Nagoya, Japan
- 2Department of Rare/Intractable Cancer Analysis Research, Nagoya University Graduate School of Medicine, Nagoya, Japan
Congenital duodenal atresia with situs inversus is occasionally accompanied by a preduodenal portal vein (PDPV), which is incidentally diagnosed during surgery. Duodenoduodenostomy is the most common and effective treatment. However, some patients require other anastomoses. Here, we present two cases of laparoscopic gastrojejunostomy for congenital duodenal atresia with situs inversus and PDPV and describe the reason for selecting gastrojejunostomy. The optimal surgical strategy is patient specific and should be determined based on the patient's general and physical condition.
1. Introduction
Duodenal obstruction causes bilious vomiting and requires early diagnosis and treatment. It consists of duodenal atresia and stenosis, which occur in 1 in 5,000–10,000 live births (1). Duodenoduodenostomy or duodenojejunostomy is performed in such cases to connect the intestines. Since Bax et al. originally reported performing a laparoscopic duodenoduodenostomy in 2001 (2), laparoscopic surgery for duodenal atresia has been further developed. A recent systematic review revealed that laparoscopic surgery for duodenal atresia is safe and yields outcomes equivalent to those of open surgery (3).
An appropriate strategy for the safe performance of duodenal atresia surgery is important, as more than 50% of patients with duodenal atresia have associated congenital anomalies (4). We encountered two cases of duodenal atresia with situs inversus and a preduodenal portal vein (PDPV). Reports of laparoscopic management of such cases are rare. Therefore, we present our surgical strategy for duodenal atresia to prevent postoperative complications.
2. Case presentation
Case 1: A 2-day-old boy with a gestational age of 38 weeks and weighing 3,200 g was transferred to our hospital with suspected duodenal atresia. The patient was prenatally diagnosed with situs inversus. Abdominal radiography revealed a double-bubble sign with situs inversus (Figure 1A). Upper gastrointestinal contrast imaging revealed duodenal atresia and a minor duodenal papilla in the oral duodenum (Figure 1B). Ultrasonography revealed situs inversus without any apparent cardiac anomalies or malrotation. The patient was diagnosed with duodenal atresia, and laparoscopic surgery was performed. Laparoscopy revealed situs inversus and duodenal atresia with a PDPV (Figures 2A,B). A laparoscopic gastrojejunostomy was performed using a 5 mm stapling instrument (Figure 2C). The postoperative course was uneventful, and the patient showed no apparent symptoms four years after surgery.
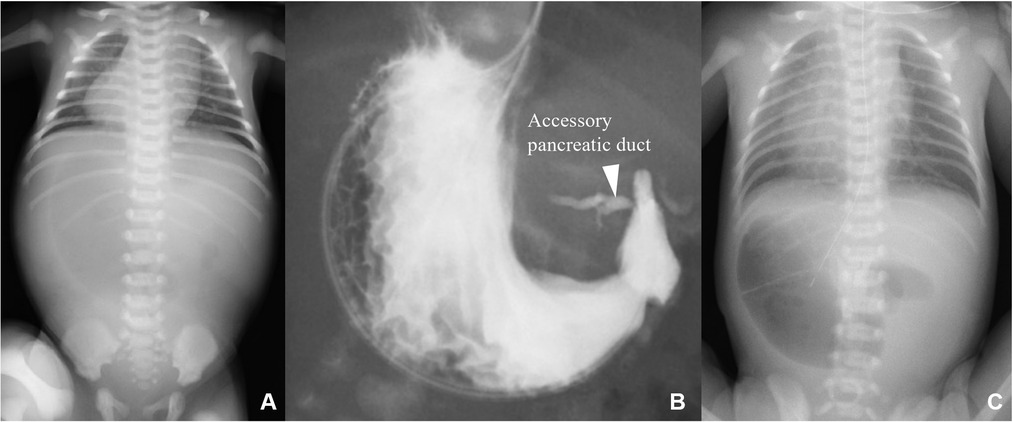
Figure 1. Preoperative imaging studies. (A) Chest radiograph showing the double-bubble sign with situs inversus. (B) Upper gastrointestinal contrast-enhanced imaging revealing duodenal atresia. The distal duodenum was enhanced through the accessory pancreatic duct. (C) Abdominal radiograph showing the double-bubble sign with situs inversus.
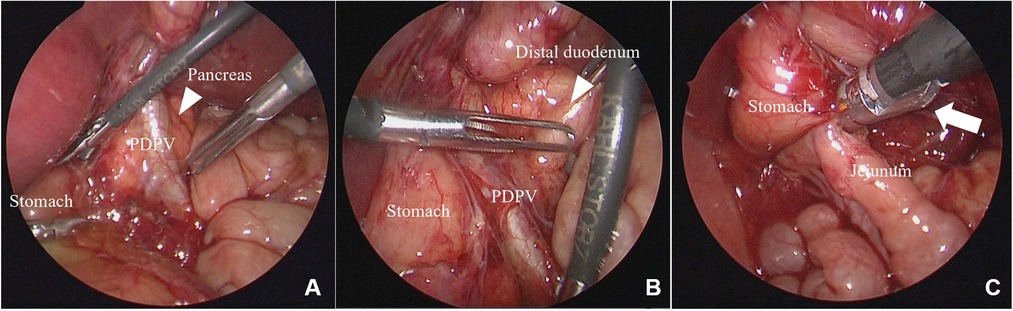
Figure 2. Laparoscopic findings for case 1. (A) The PDPV is confirmed. (B) The duodenum was obliterated near the pyloric end. (C) Gastrojejunostomy is performed using a 5 mm stapler (white arrow). PDPV, preduodenal portal vein.
Case 2: A 1-day-old girl with a gestational age of 37 weeks and weighing 2,278 g was born via cesarean section. The patient was prenatally diagnosed with situs inversus, polysplenia, and cardiac anomalies. Abdominal radiography revealed a double-bubble sign with situs inversus (Figure 1C). Duodenal atresia was suspected, and laparoscopic surgery was performed. Laparoscopy revealed situs inversus, annular pancreas, malrotation, and duodenal atresia with a PDPV (Figures 3A,B). A laparoscopic gastrojejunostomy was performed using a 5 mm stapling instrument (Figure 3C). The postoperative course was uneventful, and the patient remained under follow-up for two years after surgery with no apparent symptoms.
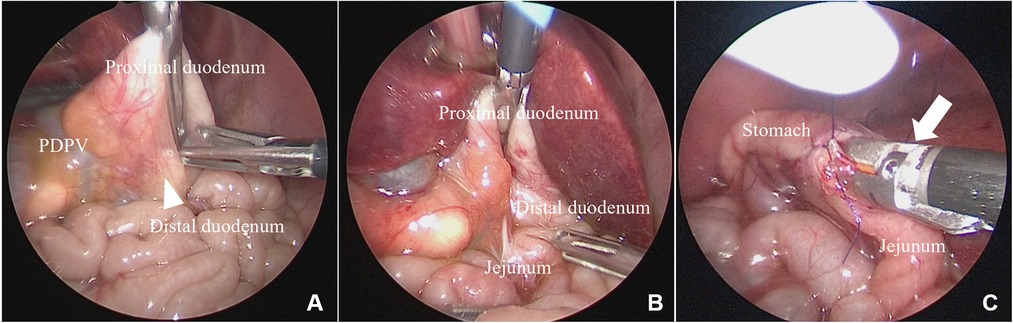
Figure 3. Laparoscopic findings for case 2. (A,B) A PDPV and duodenal atresia with an annular pancreas were diagnosed. (C) Gastrojejunostomy was performed using a 5 mm stapler (white arrow). PDPV, preduodenal portal vein.
2.1. Surgical technique
2.1.1. Port placement
A circumumbilical incision was made and a 5 mm balloon port was placed. The insufflation pressure was 8 mmHg with irrigation at 5 L/min. A 5 mm 30 degree laparoscope was inserted. Three 3 mm trocars were placed on the right flank, left flank, and left upper abdomen (Figure 4A).
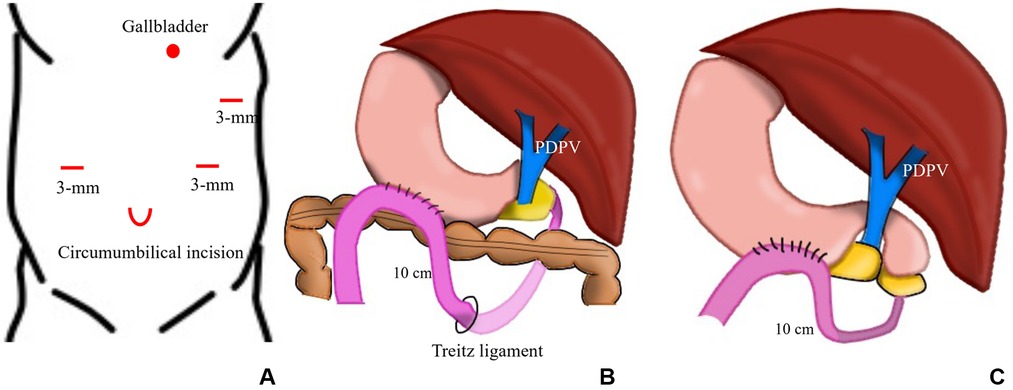
Figure 4. Schema of port placement and anastomosis. (A) A 5 mm balloon port for the laparoscope and three 3 mm trocars for the working port were placed at the umbilicus, right and left flanks, and left upper abdomen, respectively. (B) A laparoscopic gastrojejunostomy was performed about 10 cm from the ligament of Treitz in case 1. (C) Laparoscopic gastrojejunostomy was performed 10 cm from the duodenal atresia site in case 2.
2.1.2. Laparoscopic manipulation
The gallbladder was pulled with 5-0 suture to the left upper abdomen to secure a field of view. The duodenal lumen was obliterated near the pyloric end and a PDPV was diagnosed. The anal portion of the duodenum was identified on the left side of the portal vein. Considering the anatomical position of the PDPV and the oral/anal side of the duodenum, duodenoduodenostomy might have obstructed the PDPV and kinked the pancreatic duct. Therefore, a laparoscopic gastrojejunostomy was performed. The posterior gastric wall and jejunum were anastomosed side to side with a 5 mm stapler, 10 cm from the ligament and 10 cm from the distal duodenum in cases 1 and 2, respectively. The anastomosis was performed via the antecolic route and antiperistalsis (Figures 4B,C).
3. Discussion
In this study, we selected laparoscopic gastrojejunostomy for cases of duodenal atresia with a PDPV and situs inversus, which resulted in good short- and long-term outcomes. A PDPV is a rare anomaly associated with situs inversus (5), which is often incidentally diagnosed during surgery.
A PDPV can cause extrinsic obstruction; however, less than 50% of PDPVs cause obvious obstruction (6). When a PDPV causes obstructive symptoms, a duodenoduodenostomy is performed to bypass the obstruction. In our two cases, the obstructive symptoms were apparently caused by duodenal atresia rather than the PDPV. Duodenoduodenostomy or jejunostomy is performed for duodenal atresia, even when accompanied by a PDPV. Gastrojejunostomy was selected by a process of elimination.
Gastrojejunostomies have several disadvantages. Although our literature search for reports on patients with duodenal atresia who underwent gastrojejunostomy failed to reveal detailed descriptions of long-term complications. Complications in adults with almost the same anatomical condition, that is, Billroth-II or Roux-en-Y reconstruction, have been reported. One such complication is afferent limb syndrome or blind loop syndrome, which occurs in approximately 1% of patients who undergo Billroth-II reconstruction (7) and 0.2% who undergo Roux-en-Y reconstruction (8) among patients who undergo distal gastrectomy. Braun anastomosis can prevent afferent limb syndrome; however, routine Braun anastomosis is controversial because of the relatively low incidence of afferent limb syndrome (7). We decided not to perform Braun anastomosis in our two cases because it would require an additional anastomosis. We will perform this procedure if the patients show symptoms of afferent limb syndrome in the future. Other complications include gastritis and bile reflux. Billroth-II reconstruction is more likely to cause gastritis and bile reflux than Roux-en-Y reconstruction (9). However, Roux-en-Y reconstruction requires two anastomotic sites, which results in a longer operation time and increase in anastomotic site complications. In addition, it causes Roux stasis syndrome in 7%–30% of cases (10–12). Considering the aforementioned factors, we believe that Billroth-II reconstruction was an appropriate reconstruction method for gastrojejunostomy in our cases. Another complication of gastrojejunostomy is marginal ulceration, which can be prevented with postoperative antacids (13).
Despite the disadvantages of gastrojejunostomy, we considered it a better option than duodenoduodenostomy or duodenojejunostomy in our cases, mainly because of the preservation of blood flow in the portal vein. Ohno et al. reported that the repeated passage of food over the anastomosis site, which overbridges the vessel, can induce thickening of the duodenal wall (14); therefore, they recommended loose overbridging duodenoduodenostomy to maintain portal blood flow. Loose overbridging duodenoduodenostomy was deemed difficult to perform in these two cases because the proximal duodenum was relatively short. We also considered that duodenoduodenostomy could cause kinking of the pancreatic duct as we have experienced four cases of pancreatitis in patients who had undergone duodenoduodenostomy for duodenal atresia/stenosis (15).
Importantly, gastrojejunostomy is not the best treatment option for other congenital duodenal obstructions. Moreover, long-term follow-up is essential for patients undergoing gastrojejunostomy, with routine check-ups for gastritis.
4. Conclusion
We encountered two cases of duodenal atresia with situs inversus and a PDPV. Although gastritis and bile reflux are risk factors, laparoscopic gastrojejunostomy was selected to preserve the portal vein blood flow. The appropriate surgical strategy is different for each patient and should be determined based on the patient's general and physical condition.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the patient’s legal guardian for the publication of this case report.
Author contributions
YN: investigation, writing–original draft, writing—review and editing. WS and SM: patient treatment and validation. HU: supervision, validation, writing—review, and editing. AH, CS, KY, HA, AY, AA, DK, TM, and YG: validation. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors thank all patients and their parents. YN was supported by the Nagoya University CIBoG WISE program from MEXT.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kimura K, Loening-Baucke V. Bilious vomiting in the newborn: rapid diagnosis of intestinal obstruction. Am Fam Physician. (2000) 61:2791–8.10821158
2. Bax NM, Ure BM, van der Zee DC, van Tuijl I. Laparoscopic duodenoduodenostomy for duodenal atresia. Surg Endosc. (2001) 15:217. doi: 10.1007/BF03036283
3. Zhang J, Xu X, Wang X, Zhao L, Lv Y, Chen K. Laparoscopic versus open repair of congenital duodenal obstruction: a systematic review and meta-analysis. Pediatr Surg Int. (2022) 38:1507–15. doi: 10.1007/s00383-022-05209-9
4. Choudhry MS, Rahman N, Boyd P, Lakhoo K. Duodenal atresia: associated anomalies, prenatal diagnosis and outcome. Pediatr Surg Int. (2009) 25:727–30. doi: 10.1007/s00383-009-2406-y
5. Ruben GD, Templeton JM, Ziegler MM. Situs inversus: the complex inducing neonatal intestinal obstruction. J Pediatr Surg. (1983) 18:751–6. doi: 10.1016/s0022-3468(83)80018-9
6. Mordehai J, Cohen Z, Kurzbart E, Mares AJ. Preduodenal portal vein causing duodenal obstruction associated with situs inversus, intestinal malrotation, and polysplenia: a case report. J Pediatr Surg. (2002) 37:1–3. doi: 10.1053/jpsu.2002.31643
7. Kim DJ, Lee JH, Kim W. Afferent loop obstruction following laparoscopic distal gastrectomy with Billroth-II gastrojejunostomy. J Korean Surg Soc. (2013) 84:281–6. doi: 10.4174/jkss.2013.84.5.281
8. Aoki M, Saka M, Morita S, Fukagawa T, Katai H. Afferent loop obstruction after distal gastrectomy with roux-en-Y reconstruction. World J Surg. (2010) 34:2389–92. doi: 10.1007/s00268-010-0602-5
9. Choi C I, Baek DH, Lee SH, Hwang SH, Kim DH, Kim KH, et al. Comparison between Billroth-II with Braun and Roux-en-Y reconstruction after laparoscopic distal gastrectomy. J Gastrointest Surg. (2016) 20:1083–90. doi: 10.1007/s11605-016-3138-7
10. Gustavsson S, Ilstrup DM, Morrison P, Kelly KA. Roux-Y stasis syndrome after gastrectomy. Am J Surg. (1988) 155:490–4. doi: 10.1016/S0002-9610(88)80120-X
11. Nakamura M, Nakamori M, Ojima T, Iwahashi M, Horiuchi T, Kobayashi Y, et al. Randomized clinical trial comparing long-term quality of life for Billroth I versus Roux-en-Y reconstruction after distal gastrectomy for gastric cancer. Br J Surg. (2016) 103:337–47. doi: 10.1002/bjs.10060
12. Imamura H, Takiguchi S, Yamamoto K, Hirao M, Fujita J, Miyashiro I, et al. Morbidity and mortality results from a prospective randomized controlled trial comparing Billroth I and Roux-en-Y reconstructive procedures after distal gastrectomy for gastric cancer. World J Surg. (2012) 36:632–7. doi: 10.1007/s00268-011-1408-9
13. De Ugarte DA, Dutson EP, Hiyama DT. Annular pancreas in the adult: management with laparoscopic gastrojejunostomy. Am Surg. (2006) 72:71–3. doi: 10.1177/000313480607200117
14. Ohno K, Nakamura T, Azuma T, Yoshida T, Hayashi H, Nakahira M, et al. Evaluation of the portal vein after duodenoduodenostomy for congenital duodenal stenosis associated with the preduodenal superior mesenteric vein, situs inversus, polysplenia, and malrotation. J Pediatr Surg. (2007) 42:436–9. doi: 10.1016/j.jpedsurg.2006.10.019
Keywords: duodenal atresia, preduodenal portal vein, situs inversus, gastrojejunostomy, laparoscopy
Citation: Nakagawa Y, Sumida W, Makita S, Uchida H, Hinoki A, Shirota C, Tainaka T, Yokota K, Amano H, Yasui A, Takimoto A, Kato D, Maeda T and Gohda Y (2023) Case report: Laparoscopic gastrojejunostomy for duodenal atresia with situs inversus and preduodenal portal vein: a report of two cases. Front. Pediatr. 11:1220393. doi: 10.3389/fped.2023.1220393
Received: 10 May 2023; Accepted: 12 June 2023;
Published: 27 June 2023.
Edited by:
Juan A. Tovar, University Hospital La Paz, SpainReviewed by:
Tutku Soyer, Hacettepe University, TürkiyeTetsuya Ishimaru, National Center for Child Health and Development (NCCHD), Japan
© 2023 Nakagawa, Sumida, Makita, Uchida, Hinoki, Shirota, Tainaka, Yokota, Amano, Yasui, Takimoto, Kato, Maeda and Gohda. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hiroo Uchida aGlybzIwMTNAbWVkLm5hZ295YS11LmFjLmpw
†ORCID Yoichi Nakagawa orcid.org/0000-0003-1570-8661 Satoshi Makita orcid.org/0000-0002-8461-5998 Hiroo Uchida orcid.org/0000-0002-1818-6697 Akinari Hinoki orcid.org/0000-0001-6878-2043 Takahisa Tainaka orcid.org/0000-0002-3965-2087
 Yoichi Nakagawa
Yoichi Nakagawa Wataru Sumida
Wataru Sumida Satoshi Makita1,†
Satoshi Makita1,† Hiroo Uchida
Hiroo Uchida Chiyoe Shirota
Chiyoe Shirota Takahisa Tainaka
Takahisa Tainaka Kazuki Yokota
Kazuki Yokota Hizuru Amano
Hizuru Amano Yousuke Gohda
Yousuke Gohda