- Institute of Molecular Biology and Translational Medicine, The Affiliated People's Hospital, Jiangsu University, Zhenjiang, China
Objective: Dazhu hongjingtian [DZHJT, Rhodiola wallichiana var. cholaensis (Praeger) S.H. Fu] preparation as an add-on therapy has been applied to the treatment of angina pectoris. We aimed to evaluate the efficacy and safety of DZHJT as adjuvant therapy for the treatment of unstable angina pectoris (UAP).
Methods: An extensive literature search was conducted on PubMed, Emase, Cochrane Library, Wanfang, CNKI, and VIP databases from inception to January 2019. Randomized controlled trials (RCTs) comparing DZHJT in combination with Western medicine with Western medicine alone were included. Two authors independently performed the literature search, data extraction and risk of bias assessment of included studies, and conducted the statistical analysis.
Results: A total of 18 RCTs involving 1,679 patients were included in the meta-analysis. Adjuvant treatment with DZHJT significantly decreased ≥80% reduction in the frequency of angina attacks [risk ratio (RR) 1.57; 95% CI 1.36–1.81], weekly frequency of angina attacks [mean difference (MD) −1.03 times; 95% confidence interval (CI) −1.51 to −0.55], marked improved abnormal electrocardiogram (RR 1.46; 95% CI 1.23–1.74). In addition, DZHJT significantly reduced the whole-blood viscosity (MD −0.70 mPa.s; 95% CI −0.84 to −0.55), plasma viscosity (MD −0.28 mPa.s; 95% CI −0.38 to −0.19), serum level of fibrinogen (MD −0.67 g/L; 95% CI −0.79 to −0.54), thromboxanes B2 (MD −14.01 ng/L; 95% CI −20.86 to −7.15), and C-reactive protein (MD −1.48 mg/L; 95% CI −2.72 to −0.25). No significant differences in headache/dizziness (RR 0.72; 95% CI 0.31–1.67) were observed between two groups.
Conclusion: Adjuvant treatment with DZHJT has an add-on effect in reducing angina pectoris attacks in patients with UAP. The beneficial effect may be correlated with regulating whole-blood viscosity, plasma viscosity, fibrinogen, thromboxanes B2, and CRP level. However, future well-designed prospective, randomized, double-blind placebo-controlled trials with large sample sizes are required to evaluate the evidence.
Introduction
Angina pectoris is a symptomatic condition characterized by chest pain attacks. It is clinically classified into stable angina pectoris (SAP) and unstable angina pectoris (UAP). UAP is a type of acute coronary syndrome characterized by an attack at rest and severe, prolonged, and frequent or newly developed angina pectoris (Basra et al., 2016). The population weighted prevalence of UAP is 5.7% in men and 6.7% in women (Hemingway et al., 2008). UAP is associated with higher risk of acute myocardial infarction and sudden death. The current therapeutic strategy of angina pectoris mainly includes anti-ischemia, anti-thrombosis, and anti-platelet or revascularization procedures (Parikh and Kadowitz, 2014; Silva et al., 2015).
Dazhu hongjingtian (DZHJT)/Rhodiola wallichiana var. cholaensis [Praeger] S.H. Fu (R. wallichiana var.) has been frequently introduced to patients with angina pectoris in China (Fan et al., 2005). R. wallichiana var. is used for preparing DZHJT injection/capsule preparation, extracted from the root and rhizome. These preparations (detailed information of DZHJT is provided in Supplemental Text S1) have been approved by the Food and Drug Administration of China. Cardiovascular effects of DZHJT have been described in the dilation of cardiac vessels and reduction of myocardial oxygen consumption (Zhang et al., 2005). In addition, DZHJT also has anti-inflammatory activity (Choe et al., 2012), anti-diabetic effect (Gao et al., 2009), and sedative–hypnotic property (Li et al., 2007). Clinically, DZHJT is mainly used to treat angina pectoris (Jiang and Pan, 2012). A previous well-designed meta-analysis (Chu et al., 2014) has demonstrated the beneficial effects of DZHJT in SAP patients. Several clinical studies (Yu et al., 2011; Chen, 2013; Zhang, 2013; Cao et al., 2014; Jia and Wang, 2014; Li and Zhao, 2014; Shen et al., 2014) have investigated the add-on effects of the DZHJT in patients with UAP, but the findings were limited by small sample sizes and varying study quality. Therefore, we conducted this meta-analysis of randomized controlled trials (RCT) to assess the efficacy and safety of DZHJT as adjuvant therapy for patients with UAP.
Materials and Methods
Literature Search
We conducted this meta-analysis following the checklists of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Guidelines (Liberati et al., 2009). This meta-analysis was registered in the PROSPERO international database of prospectively registered systematic reviews (PROSPERO CRD42018111885). Two authors systematically searched PubMed, Embase, Cochrane Library, China Science and Technology Journal Database (VIP), China National Knowledge Infrastructure (CNKI), and Wanfang Database and from inception to January 2019. The searching items for English medical literature were “unstable angina pectoris” OR “angina” OR “acute coronary syndrome” AND “rhodiola” OR “hong jing tian” OR “hongjingtian” AND “randomized controlled trial” OR “randomized” OR “randomized.” Chinese searching terms included “bù wěn dìng xíng xin jiǎo tòng” OR “unstable angina pectoris” AND “hóng jing tiān” OR “rhodiola” AND “suí ji” AND “duìzhào.” A manual search was performed using the reference lists of relevant articles.
Study Selection
Inclusion criteria were as follows: (1) study design was RCT; (2) patients diagnosed with UAP according to the guideline of the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) (Braunwald et al., 2000), World Health Organization (Organization, 1979), European Society of Cardiology (ESC) (Fox et al., 2006) or Chinese Society of Cardiology (CSC) (Cardiology, 2000); (3) DZHJT in combination with conventional Western medicine vs. Western medicine alone; and (4) primary outcomes were ≥80% reduction in frequency of angina attacks weekly and marked improvement of abnormal electrocardiogram (restore normal or nearly normal defined by at least 0.05 mv restoration at ST segment). The secondary outcomes were the whole-blood viscosity, plasma viscosity, fibrinogen, thromboxanes B2, or C-reactive protein (CRP) and adverse events. Articles were excluded when: (1) diagnostic criteria for UAP were not specified; (2) patients have SAP; (3) combined application of DZHJT with other Chinese herbs as intervention.
Data Extraction and Quality Assessment
For the included trials, two authors independently extracted the data and assessed the methodological quality. Any disagreements in this process were resolved by discussion. The extracted data included the last name of the first author, year of publication, sample size, patients' age, diagnostic criteria, interventions (dose of DZHJT and course of treatment), outcome measures, and methodological information. We evaluated the methodological quality of the included trials according to the Cochrane risk of bias tool, which included selection bias, performance bias, detection bias, attrition bias, reporting bias, and other sources of bias. Each trial was categorized by “high,” “unclear,” or “low” risk of bias.
Statistical Analysis
The RevMan 5.2 software was used for the meta-analysis. We summarized as the risk ratio (RR) with 95% confidence intervals (CI) for dichotomous outcomes or mean difference (MD) with 95% CI for continuous outcomes. The Cochrane Q statistic and I2 index were applied to the analysis of heterogeneity across the studies. A random effect meta-analysis was conducted when the p-value of Cochrane Q statistic test is <0.10 and I2 >50%. Otherwise, we pooled the data by using a fixed-effect model. We used a funnel plot to examine the possible publication bias when the number of trials was sufficient. Leave-one-out sensitivity analysis was conducted to test the stability of the pooling results.
Results
Search Results and Study Characteristics
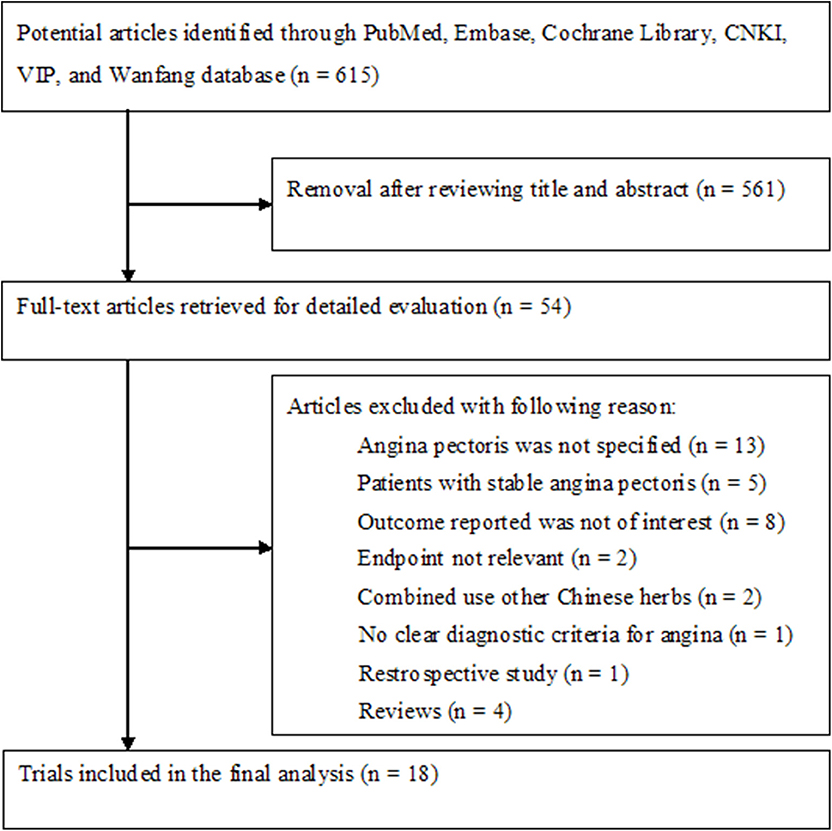
In brief, our initial literature search yielded 615 potentially relevant articles. After screening the titles and abstracts, we retrieved 54 full-text articles for detailed evaluation. We further removed 36 articles on the basis of our predefined inclusion criteria. Thus, 18 articles (Yu et al., 2011; Chen, 2013; Zhang, 2013; Cao et al., 2014; Jia and Wang, 2014; Li and Zhao, 2014; Shen et al., 2014; Liu and Jiang, 2015; Wang et al., 2015; Weng et al., 2015; Zhai et al., 2015; Qin and Gao, 2016; Zhang and Lu, 2016; Du, 2017; Li, 2017; Li and Cheng, 2018; Wang and Yang, 2018; Zhang et al., 2018) were finally included in the meta-analysis (Figure 1).
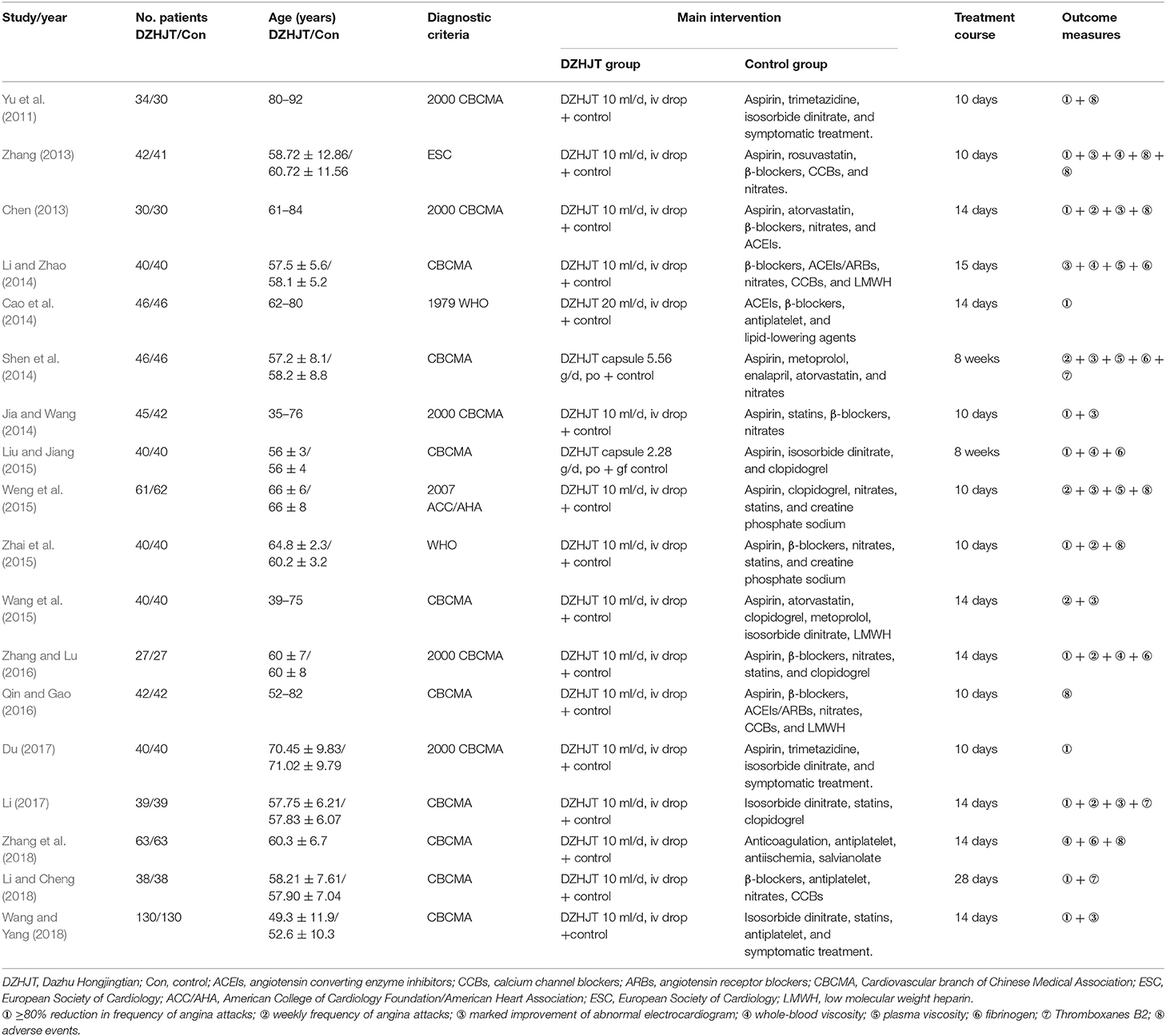
The main characteristics of the included trials are summarized in Table 1. A total of 1,679 patients with UAP were identified with eligible trials. All of the selected trials were published in Chinese medical databases from 2011 to 2019. Two trials (Shen et al., 2014; Liu and Jiang, 2015) used DZHJT capsule as intervention, and the others used DZHJT injection. The duration of intervention ranged from 10 days to 8 weeks. Main conventional Western medicines referred to treatment included aspirin, nitrates, β-blockers, calcium channel blockers, angiotensin converting enzyme inhibitors, angiotensin receptor blockers, low molecular weight heparin, and lipid-lowering agents. All of the 18 trials indicated randomization, but only 4 trials (Chen, 2013; Liu and Jiang, 2015; Zhai et al., 2015; Zhang and Lu, 2016) described the detailed method of randomization. None of the trials reported the allocation concealment, dropout or withdrawal. Figure S1 shows the detailed methodological quality of the included trials.
Frequency of Angina Attacks
A total of 13 trials (Yu et al., 2011; Chen, 2013; Zhang, 2013; Cao et al., 2014; Jia and Wang, 2014; Liu and Jiang, 2015; Wang et al., 2015; Zhai et al., 2015; Zhang and Lu, 2016; Du, 2017; Li, 2017; Li and Cheng, 2018; Wang and Yang, 2018) selected ≥80% reduction in frequency of angina attacks as an outcome. As shown in Figure 2A, a fixed-effect model was applied because no heterogeneity was observed across trials (I2 = 0%, p = 0.63). Meta-analysis showed that adjuvant treatment with DZHJT significantly reduced the ≥80% reduction in frequency of angina attacks (RR 1.57; 95% CI 1.36–1.81). When we removed one trial (Yu et al., 2011) enrolling patients with age of more than 80 years, the pooled RR of ≥80% reduction in frequency of angina attacks was 1.52 (95% CI 1.31–1.76) in a fixed-effect model. Visual inspection of the funnel plot showed no evidence of publication bias (Figure S2). Five trials (Chen, 2013; Shen et al., 2014; Weng et al., 2015; Zhang and Lu, 2016; Li, 2017) reported the weekly frequency of angina attacks as an outcome measure. As shown in Figure 2B, a random effect model meta-analysis showed that adjuvant treatment with DZHJT was associated with a reduced weekly frequency of angina attacks [MD −1.03 times; 95% confidence interval (CI) −1.51 to −0.88; I2 = 84%, p < 0.001].
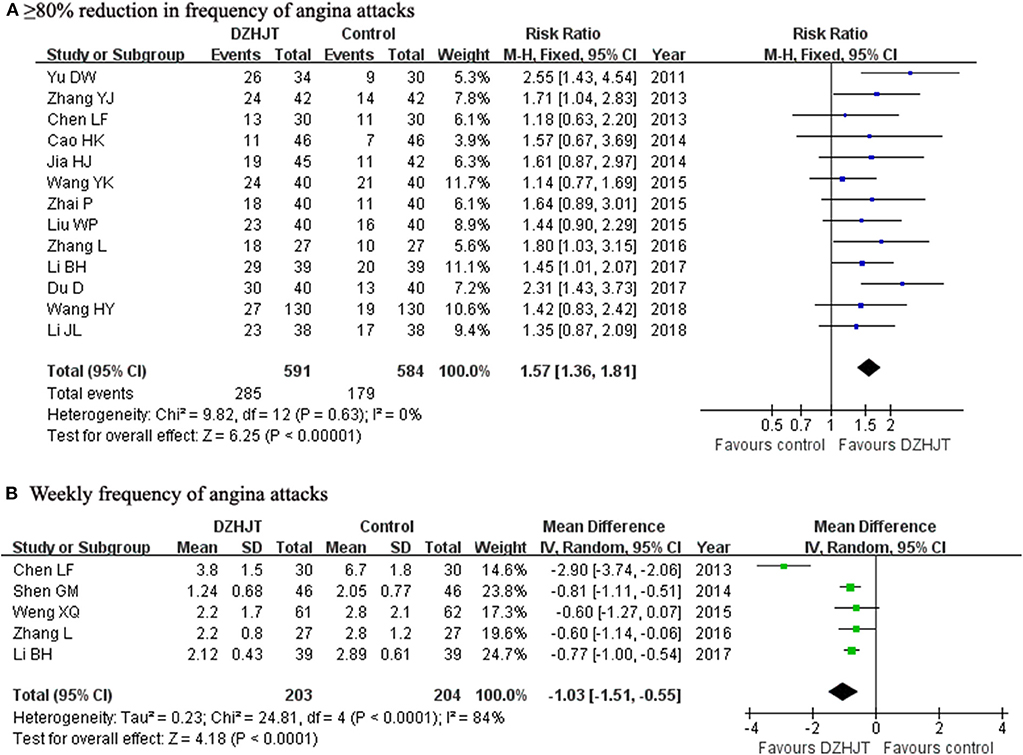
Figure 2. Forest plots showing comparison of ≥80% reduction in frequency of angina attacks (A) and weekly frequency of angina attacks (B) in patients with or without DZHJT treatment.
Abnormal Electrocardiogram
Nine trials (Chen, 2013; Zhang, 2013; Jia and Wang, 2014; Li and Zhao, 2014; Shen et al., 2014; Wang et al., 2015; Weng et al., 2015; Li, 2017; Wang and Yang, 2018) reported marked improvement of abnormal electrocardiogram as an outcome. As shown in Figure 3, a fixed-effect model meta-analysis indicated that adjuvant treatment with DZHJT was associated with marked improvement of abnormal electrocardiogram (RR 1.46; 95% CI 1.23–1.74; I2 = 0%, p = 0.93). No evidence of publication bias was observed based on the visual inspection of the funnel plot (Figure S3).
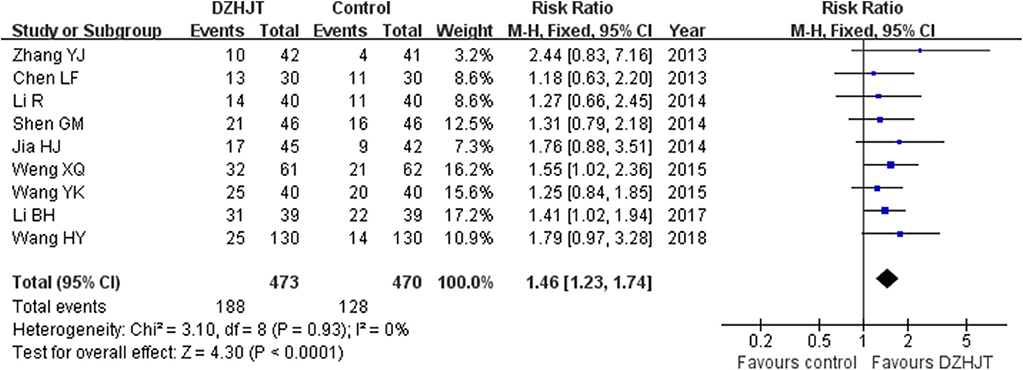
Figure 3. Forest plots showing comparison of marked improvement of abnormal electrocardiogram in patients with or without DZHJT treatment.
Serum Fibrinogen, Whole-Blood Viscosity, and Plasma Viscosity
As shown in Figure 4A, a fixed-effect model meta-analysis of five trials (Zhang, 2013; Li and Zhao, 2014; Liu and Jiang, 2015; Zhang and Lu, 2016; Zhang et al., 2018) indicated that adjuvant treatment with DZHJT significantly reduced serum fibrinogen level (MD −0.67 g/L; 95% CI −0.79 to−0.54; I2 = 26%, p = 0.25). As shown in Figures 4B,C, a random effect model meta-analysis showed that whole-blood viscosity (MD −0.78 mPa.s; 95% CI −1.14 to −0.41; I2 = 76%, p = 0.006); four trials (Zhang, 2013; Li and Zhao, 2014; Liu and Jiang, 2015; Zhang et al., 2018) and plasma viscosity (MD −0.28 mPa.s; 95% CI −0.38 to −0.19; I2 = 80%, p = 0.002); four trials (Zhang, 2013; Li and Zhao, 2014; Shen et al., 2014; Weng et al., 2015) were significantly reduced in the DZHJT combined with Western medicine group.
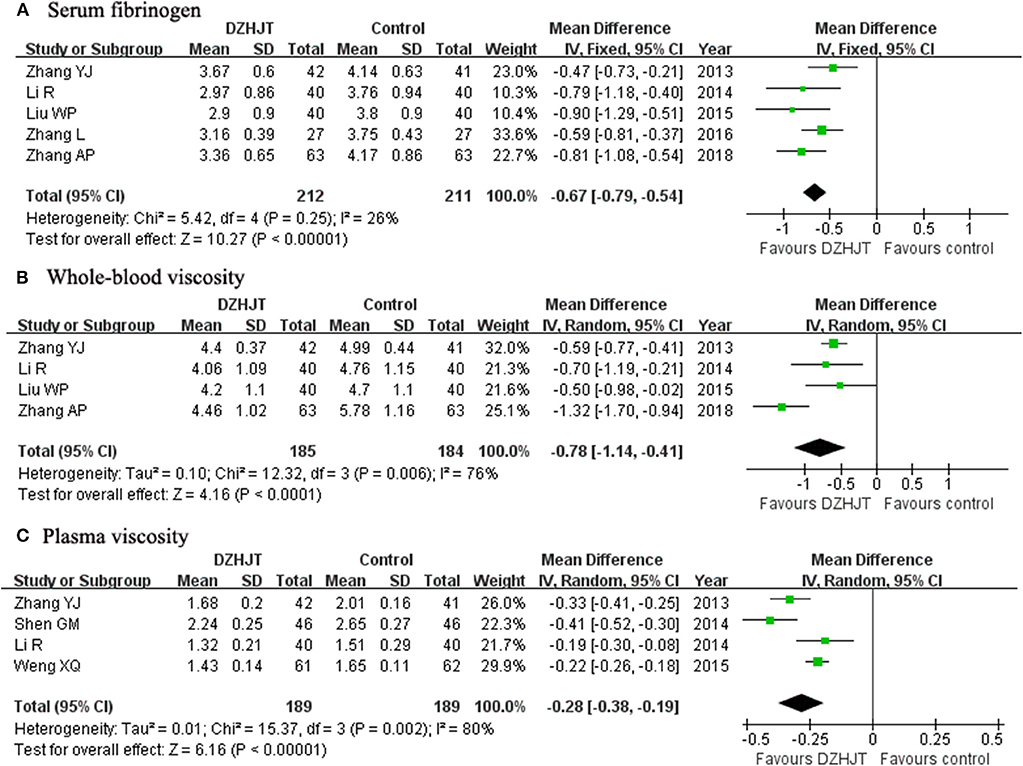
Figure 4. Forest plots showing comparison of the serum fibrinogen (A), whole-blood viscosity (B), and plasma viscosity (C) in patients with or without DZHJT treatment.
Serum Thromboxanes B2 and CRP Level
As shown in Figure 5A, a random effect model meta-analysis of three trials showed that DZHJT in combination with conventional Western medicine significantly decreased serum thromboxanes B2 level (MD −14.01 ng/L; 95% CI −20.86 to −7.15; I2 = 74%, p = 0.02); 3 trials (Shen et al., 2014; Li, 2017; Li and Cheng, 2018) compared with Western medicine alone. Moreover, Figure 5B shows that adjuvant treatment with DZHJT also significantly reduced serum CRP level (MD −1.48 mg/L; 95% CI −2.72 to −0.25; I2 = 94%, p < 0.001); three trials (Wang et al., 2015; Weng et al., 2015; Li, 2017) in a random effect model.
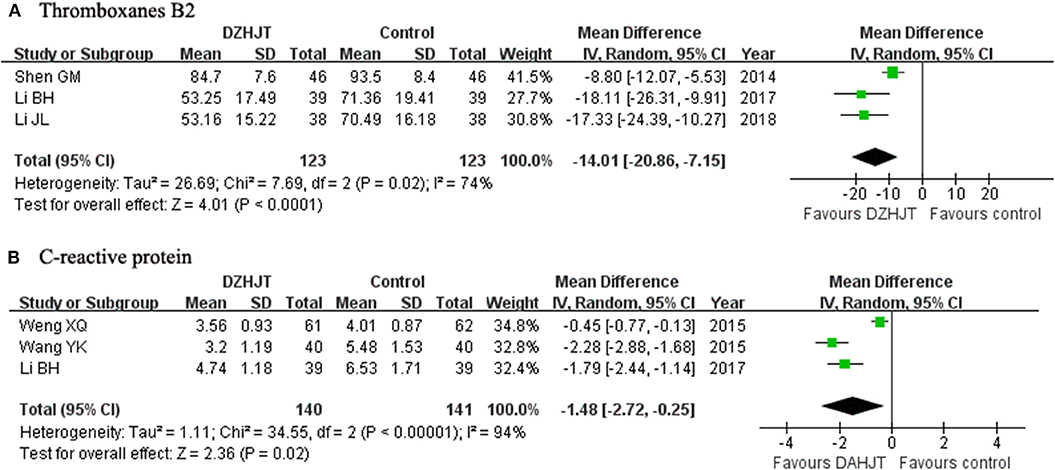
Figure 5. Forest plots showing comparison of the serum thromboxanes B2 (A) and C-reactive protein (B) level in patients with or without DZHJT treatment.
Adverse Events
Five trials (Yu et al., 2011; Weng et al., 2015; Zhai et al., 2015; Qin and Gao, 2016; Zhang et al., 2018) described the adverse events. The common adverse events were headache and dizziness. No severe adverse events were reported. The incidences of headache and dizziness was 3.75 and 5.06%, respectively. As shown in Figure 6, no significant differences were found in headache and dizziness (RR 0.72; 95% CI 0.31–1.67; I2 = 0%, p = 0.60) between two groups. When we excluded one trial (Yu et al., 2011) enrolling patients with age of more than 80 years old, the pooled RR of headache and dizziness was 0.56 (95% CI 0.19–1.63) in a fixed-effect model.
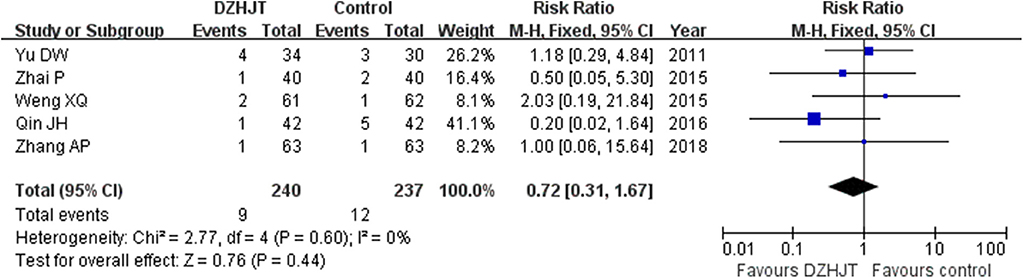
Figure 6. Forest plots showing comparison of incidence of headache/dizziness in patients with or without DZHJT treatment.
Discussion
The main findings of this meta-analysis suggested that adjuvant treatment with DZHJT significantly reduced the frequency of angina attacks and restored the abnormal electrocardiogram. Moreover, whole-blood viscosity, plasma viscosity, fibrinogen, thromboxanes B2, and CRP levels were significantly lower after DZHJT in combination with Western medicine treatment compared with conventional Western medicine alone.
Haemostatic parameters mainly include fibrinogen level, whole-blood viscosity, plasma viscosity, and hematocrit. These haemostatic parameters are elevated in patients with UAP (Neumann et al., 1991). Whole-blood viscosity represents the frictional resistance of blood flow on the intimal wall of blood vessels. Fibrinogen plays a major determinant in platelet aggregation and blood viscosity, whereas increased whole-blood viscosity may lead to high shear forces at the vascular endothelium, contributing to plaque instability (Cowan et al., 2012). Elevated haemorheological parameters correlate with the increased risk of cardiovascular events (Di Minno and Mancini, 1990; Lowe et al., 1997; Marton et al., 2003). DZHJT has the action of removing stasis and stopping bleeding. Therefore, it can reduce the high blood viscosity associated with blood stagnation. Our meta-analysis indicated that adjuvant treatment with DZHJT significantly decreased the whole-blood viscosity, plasma viscosity, fibrinogen, and thromboxanes B2 level. DZHJT significantly reduced serum CRP level. In summary, the beneficial effect of DZHJT in patients with UAP may correlate with the capability to normalize blood rheology and reduce the inflammatory reaction. However, whether DZHJT can decrease the development of coronary artery disease requires further investigation.
Most of the included trials did not select adverse events as outcome measures. None of the included trials reported severe adverse events. Headache and dizziness were the most frequently reported adverse events among these included trials. Headache may be more closely correlated with the use of nitrates (Thadani and Rodgers, 2006). Nevertheless, our pooled results revealed no significant differences in headache and dizziness between two groups. The possible adverse events associated with DZHJT use require further monitoring.
Several limitations in this meta-analysis must be noted. Firstly, the overall methodological quality of the included trials was suboptimal. All the included trials were generally of small sample size and none of the trials mentioned the sample size calculation, allocation concealment, and withdrawal/dropout or adopted the blinded, placebo controlled designs. Secondly, Traditional Chinese Medicine (TCM) is a holistic system of medicine. However, most of the included trials did not consider syndrome differentiation in patient selection. TCM syndrome differentiation must be incorporated into the diagnostic process and DZHJT is suitable for blood stagnation syndrome. Thirdly, generalizing the current findings to patients with SAP must be with caution. Finally, the included trials did not report the long-term follow-up results, and whether adjuvant treatment with DZHJT can reduce the risk of future cardiovascular events is unknown.
Conclusions
This meta-analysis suggests that adjuvant treatment with DZHJT has an add-on effect in reducing the frequency of angina pectoris attacks among patients with UAP. The beneficial effect of DZHJT may be correlated with its function to regulate whole-blood viscosity, plasma viscosity, fibrinogen, thromboxanes B2 and CRP level. However, based on the existing evidence, no conclusion about the therapeutic benefits, limitations of use and potential risks can be drawn. Future well-designed prospective, randomized, double-blind placebo-controlled trials with large sample sizes are required to evaluate the evidence.
Author Contributions
CM and ZD made the literature search, extracted data, evaluated the study quality, and performed the statistical analysis. CM drafted the manuscript. YF designed the study, interpreted the results, and revised the manuscript.
Funding
This work was supported by Jiangsu Provincial Key&D Special Fund (BE2015666).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2020.00213/full#supplementary-material
Supplemental Text S1. The detailed information of DZHJT.
Figure S1. Risk of bias graph (A) and risk of bias summary (B).
Figure S2. Funnel plots of trial reporting ≥80% reduction in frequency of angina attacks.
Figure S3. Funnel plots of trial reporting marked improvement of abnormal electrocardiogram.
References
Basra, S. S., Virani, S. S., Paniagua, D., Kar, B., and Jneid, H. (2016). Acute coronary syndromes: unstable angina and non-ST elevation myocardial infarction. Heart Fail. Clin. 12, 31–48. doi: 10.1016/j.hfc.2015.08.004
Braunwald, E., Antman, E. M., Beasley, J. W., Califf, R. M., Cheitlin, M. D., Hochman, J. S., et al. (2000). ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: executive summary and recommendations. A report of the American college of cardiology/American heart association task force on practice guidelines (committee on the management of patients with unstable angina). Circulation 102, 1193–1209. doi: 10.1161/01.CIR.102.10.1193
Cao, H. K., Zhang, Y. K., Fu, W., and Yang, K. (2014). Effect of Dazhu hongjingtian Injection on unstable angina pectoris in the elderly patients. Med. Infor. 27, 272–273. doi: 10.3969/j.issn.1006-1959.2014.30.423
Cardiology, C. S. O. (2000). Recommendations for the diagnosis and treatment of unstable angina pectoris. Chin. J. Cardiol. 28, 409–412. doi: 10.3321/j.issn:1000-3614.2001.03.033
Chen, L. F. (2013). Treatment of 30 cases of elderly unstable angina pectoris by integrated traditional Chinese and Western medicine. Fujian J. TCM 44, 27–28. doi: 10.13260/j.cnki.jfjtcm.011391
Choe, K. I., Kwon, J. H., Park, K. H., Oh, M. H., Kim, M. H., Kim, H. H., et al. (2012). The antioxidant and anti-inflammatory effects of phenolic compounds isolated from the root of Rhodiola sachalinensis A. BOR. Mol. 17, 11484–11494. doi: 10.3390/molecules171011484
Chu, J. F., Wu, G. W., Zheng, G. H., Zheng, F., Xu, J. F., Peng, J., et al. (2014). A systematic review of randomized controlled trials on treating chronic stable angina pectoris by Rhodiola. Chin. J. Integr. Trad. West Med. 34, 940–946. doi: 10.7661/CJIM.2014.08.0940
Cowan, A. Q., Cho, D. J., and Rosenson, R. S. (2012). Importance of blood rheology in the pathophysiology of atherothrombosis. Cardiovasc. Drugs Ther. 26, 339–348. doi: 10.1007/s10557-012-6402-4
Di Minno, G., and Mancini, M. (1990). Measuring plasma fibrinogen to predict stroke and myocardial infarction. Arteriosclerosis 10, 1–7. doi: 10.1161/01.ATV.10.1.1
Du, D. (2017). Effects of dazhu hongjingtian injection on QT dispersion and heart rate variability in elderly patients with unstable angina pectoris. Mod. J. Int. Trad. Chin. Western Med. 26, 723–725. doi: 10.3969/j.issn.1008-8849.2017.07.013
Fan, J. M., Wang, S. F., Qing, H., Zhai, L. H., Mao, J. Y., and Sun, L. J. (2005). Efficacy of rhodiola injection treatment for 233 cases of coronary heart disease associated with angina pectoris (blood-stasis syndrome): a multicenter randomized, double- blind, positive controlled trial. TCM Res. 18, 26–28. doi: 10.3969/j.issn.1001-6910.2005.10.017
Fox, K., Garcia, M. A., Ardissino, D., Buszman, P., Camici, P. G., Crea, F., et al. (2006). Guidelines on the management of stable angina pectoris: executive summary: the task force on the management of stable angina pectoris of the European society of cardiology. Eur. Heart J. 27, 1341–1381. doi: 10.1093/eurheartj/ehl001
Gao, D., Li, Q., Liu, Z., Feng, J., Li, J., Han, Z., et al. (2009). Antidiabetic potential of Rhodiola sachalinensis root extract in streptozotocin-induced diabetic rats. Methods Find. Exp. Clin. Pharmacol. 31, 375–381. doi: 10.1358/mf.2009.31.6.1380457
Hemingway, H., Langenberg, C., Damant, J., Frost, C., Pyorala, K., and Barrett-Connor, E. (2008). Prevalence of angina in women versus men: a systematic review and meta-analysis of international variations across 31 countries. Circulation 117, 1526–1536. doi: 10.1161/CIRCULATIONAHA.107.720953
Jia, H. J., and Wang, G. T. (2014). Effect of dazhu hongjingtian injection on the treatment of unstable angina pectoris and serum level of SOD and MDA. Heilongjiang Med. J. 38, 640–641. doi: 10.3969/j.issn.1004-5775.2014.06.012
Jiang, H., and Pan, T. (2012). Research progress of Rhodiola in prevention and treatment of cardiovascular diseases. Chin. J. Int. Med. Cardio-/Cerebrovascular Dis. 10, 341–342. doi: 10.3969/j.issn.1672-1349.2012.03.045
Li, B. H. (2017). Therapeutic effect of dazhu hongjingtian injection combined with clopidogrel on unstable angina pectoris and its effect on platelet function. Clin. Med. 37, 99–100. doi: 10.19528/j.issn.1003-3548.2017.10.050
Li, J. L., and Cheng, H. T. (2018). Curative effect of sofren injection on unstable angina pectoris and its influence on platelet function. Chin J. Heart. Heart Rhythm 6, 65–67. doi: 10.1016/j.hrthm.2017.09.007
Li, R., and Zhao, L. (2014). Sofren injection for the treatment of unstable angina pectoris and its influence on hemorheology. Mod. Dist. Educ. Chin. Med. 12, 50–51. doi: 10.3969/j.issn.1672-2779.2014.21.028
Li, T., Xu, G., Wu, L., and Sun, C. (2007). Pharmacological studies on the sedative and hypnotic effect of salidroside from the Chinese medicinal plant rhodiola sachalinensis. Phytomedicine 14, 601–604. doi: 10.1016/j.phymed.2006.12.016
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gotzsche, P. C., Ioannidis, J. P., et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 62, e1–34. doi: 10.1016/j.jclinepi.2009.06.006
Liu, W. P., and Jiang, C. H. (2015). Rhodiola crenulate capsule on thrombus formation in patients with unstable angina pectoris. China J. Pharmaceutical Econ. 10, 36–37.
Lowe, G. D., Lee, A. J., Rumley, A., Price, J. F., and Fowkes, F. G. (1997). Blood viscosity and risk of cardiovascular events: the Edinburgh artery study. Br. J. Haematol. 96, 168–173. doi: 10.1046/j.1365-2141.1997.8532481.x
Marton, Z., Horvath, B., Alexy, T., Kesmarky, G., Gyevnar, Z., Czopf, L., et al. (2003). Follow-up of hemorheological parameters and platelet aggregation in patients with acute coronary syndromes. Clin. Hemorheol. Microcirc. 29, 81–94.
Neumann, F. J., Katus, H. A., Hoberg, E., Roebruck, P., Braun, M., Haupt, H. M., et al. (1991). Increased plasma viscosity and erythrocyte aggregation: indicators of an unfavourable clinical outcome in patients with unstable angina pectoris. Br. Heart J. 66, 425–430. doi: 10.1136/hrt.66.6.425
Organization, W. H. (1979). Nomenclature and criteria for diagnosis of ischemic heart disease. Report of the joint international society and federation of cardiology/World Health Organization task force on standardization of clinical nomenclature. Circulation 59, 607–609. doi: 10.1161/01.CIR.59.3.607
Parikh, R., and Kadowitz, P. J. (2014). Angina pectoris: current therapy and future treatment options. Expert Rev. Cardiovasc. Ther. 12, 175–186. doi: 10.1586/14779072.2014.880339
Qin, J. H., and Gao, Y. (2016). Clinical efficacy of dazhu hongjingtian for treatment of unstable angina pectoris. J. Med. Theor. Prac. 29, 3345–3346. doi: 10.19381/j.issn.1001-7585.2016.24.019
Shen, G. M., Fan, S. M., and Tian, X. S. (2014). Influence of big plant rhodiola capsule treat on unstable angina patients. Chin. J. Exp. Trad. Med. Form. 20, 200–203. doi: 10.13422/j.cnki.syfjx.2014160200
Silva, F. M., Pesaro, A. E., Franken, M., and Wajngarten, M. (2015). Acute management of unstable angina and non-ST segment elevation myocardial infarction. Einstein 13, 454–461. doi: 10.1590/S1679-45082015RW3172
Thadani, U., and Rodgers, T. (2006). Side effects of using nitrates to treat angina. Expert Opin. Drug Saf. 5, 667–674. doi: 10.1517/14740338.5.5.667
Wang, H. Y., and Yang, S. Z. (2018). Clinical observation of dazhu hongjingtian injection in the treatment of unstable angina pectoris. Chin. J. Int. Med. Cardio-/Cerebrovascular Dis. 16, 1075–1077. doi: 10.12102/j.issn.1672-1349.2018.08.024
Wang, Y. K., Shang, S. Z., Gu, X., Zhang, Y. J., Ding, Z. X., Li, J. J., et al. (2015). Clinical observation on treating 80 cases of unstable angina with the dazhu hongjingtian injection. Clin. J. Chin. Med. 7, 62–64. doi: 10.3969/j.issn.1674-7860.2015.22.032
Weng, X. Q., Zhuang, C. W., Shi, X. L., Tu, C. L., and Jiang, H. (2015). Clinical analysis of the efficacy of creatine phosphate sodium combined with Dazhu Hongjingtian Injection for the treatment of unstable angina pectoris. Clin. J. Med. Offic. 43, 827–830. doi: 10.16680/j.1671-3826.2015.11.16
Yu, D. W., Su, Y., Yang, Y., Liang, Y., Liu, D., and Hua, P. H. (2011). Clinical analysis of Dazhu Hongjingtian in treatment of unstable angina pectoris in patients with advanced age. Med. J. Nat. Defending Forces Southwest China 21, 1309–1311. doi: 10.3969/j.issn.1004-0188.2011.12.011
Zhai, P., Zhu, G. B., and Liang, J. (2015). Efficacy of dazhu hongjingtian combined with creatine phosphate sodium for the treatment of 80 cases of unstable angina pectoris. Chin. Rem. Clin. 15, 556–557.
Zhang, A. P., Zhang, H. S., and Zhang, C. J. (2018). Clinical study on sofren injection combined with salvianolate in treatment of unstable angina pectoris. Drugs Clin. 33, 1594–1598.
Zhang, L., and Lu, G. X. (2016). Therapeutic effects of dazhu hongjingtian injection combined with clopidogrel on unstable angina pectoris. Hebei Med. J. 38, 2140–2142.
Zhang, Y. J. (2013). Clinical observation of sofren injection in treating patients with unstable angina. Henan Med. Res. 22, 348–350.
Keywords: Dazhu hongjingtian, Rhodiola wallichiana, unstable angina pectoris, angina attacks, blood rheology, meta-analysis
Citation: Man C, Dai Z and Fan Y (2020) Dazhu Hongjingtian Preparation as Adjuvant Therapy for Unstable Angina Pectoris: A Meta-Analysis of Randomized Controlled Trials. Front. Pharmacol. 11:213. doi: 10.3389/fphar.2020.00213
Received: 11 February 2019; Accepted: 14 February 2020;
Published: 10 March 2020.
Edited by:
Jianxun Liu, China Academy of Chinese Medical Sciences, ChinaReviewed by:
Fang Lu, China Academy of Chinese Medical Sciences, ChinaZhong Wang, China Academy of Chinese Medical Sciences, China
Michael Heinrich, UCL School of Pharmacy, United Kingdom
Copyright © 2020 Man, Dai and Fan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu Fan, anN6amZhbnl1QDE2My5jb20=
 Changfeng Man
Changfeng Man Yu Fan
Yu Fan