- 1Department of Social Medicine and Health Management, School of Public Health, Huazhong University of Science and Technology, Wuhan, China
- 2School of Nursing, Wuchang University of Technology, Wuhan, China
- 3Department of Infection Control, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 4Department of Public Health, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 5Department of Nuclear Medicine, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Background: Currently, there is no comprehensive evaluation of the quality of antibiotic prescribing in China’s primary care facilities based on longitudinal data.
Methods: We randomly selected 11 community health centers in Shenzhen, China, and collected all outpatient prescriptions of these centers from 2010 to 2015. To evaluate the quality of antibiotic prescribing, we used six quality indicators for analysis, including number of antibiotics per 100 consultations, ratio between broad-spectrum and narrow-spectrum antibiotics (B/N ratio), percentage of first-line antibiotics recommended by guidelines, percentage of oral antibiotics with a duration exceeding the guideline recommendation, and new pediatric-specific indicators such as percentage of antibiotics with amoxicillin (A index) and ratio between amoxicillin and broad-spectrum antibiotics (A/B ratio).
Results: During the study period, 571,362 outpatient consultations resulted in antibiotic prescriptions, which contained 706,411 antibiotics. The overall number of antibiotics per 100 consultations decreased significantly from 93.50 in 2010 to 19.98 in 2015 (p = 0.004), but the B/N ratio showed an upward trend over time (p = 0.009). In different populations and different common infections, the number of antibiotics used decreased to varying degrees, while the B/N ratio increased to varying degrees, with the most obvious change in children <5 years. The percentage of first-line antibiotics for common infections was not high, ranging from 3.45 to 44.25% during 2014–2015. The percentage of oral antibiotics with an exceeded duration ranged from 0.70 to 19.39%. Moreover, the A index and A/B ratio in children remained low for a long time, which was 0.76% and 0.01 in 2015.
Conclusion: A review of antibiotic prescribing in Shenzhen, China, showed a substantial reduction in antibiotic use in primary care. However, problems such as widespread use of broad-spectrum antibiotics, insufficient use of first-line antibiotics and low use of amoxicillin were prevalent. Improving and optimizing the quality of antibiotic prescribing, particularly in children prescriptions, will be the focus of future antibiotic stewardship in China.
Introduction
Excessive and inappropriate use of antibiotics not only caused a huge economic burden to global health systems, but also rapidly increased the risk of antimicrobial resistance (AMR). Many countries, including China, are trying to tackle global AMR by reducing unnecessary or inappropriate prescribing (Sabuncu et al., 2009; Smieszek et al., 2018; Xiao, 2018). Crucially, identifying these antibiotic prescribing is a necessary precondition for the implementation of national policy interventions and an important feedback for the evaluation of intervention effects.
Reliable quality indicators are needed to identify the quality of antibiotic prescribing. A common methodology for collecting and reporting national antimicrobial consumption data developed by the WHO program of surveillance provided information on the level of use and types of antimicrobials to prescribers (World Health Organization, 2016). The quality indicators developed by the European Surveillance of Antimicrobial Consumption to assess outpatient antibiotic use provided a basis for policy-makers to formulate interventions to address identified problems (World Health Organization Regional Office for Europe, 2017). Furthermore, the use of European quality indicators in Belgium, the Netherlands, Sweden, and the United Kingdom (UK) was feasible and won opportunities for quality improvement of antibiotic prescribing in primary care (de Bie et al., 2016; Tyrstrup et al., 2017; Robertson et al., 2018). These studies on quality evaluation in these countries provided an effective reference for China.
Abuse of antibiotic prescribing in China remains serious, particularly in primary care facilities (Yin et al., 2013; Wang et al., 2014; Liu et al., 2019). The medical visits to primary care facilities accounted for more than half of the total medical visits nationwide in 2017 (China National Health Commission, 2018). However, around 70% of outpatients attending these facilities were reported inappropriate antibiotic prescribing practices, such as overuse of antibiotics, widespread use of broad-spectrum antibiotics, and unnecessary prolonged treatment (Wang et al., 2014; Wei et al., 2017). In the past 2 decades, the Chinese government has made great efforts to promote the appropriate use of antibiotics (Xiao, 2018; National Health Commission of the People’s Republic of China, 2005; Xiao et al., 2013). In 2004, the Chinese Ministry of Health issued the Guidelines for Clinical Application of Antimicrobial Agents in China. In 2011, a long-term national antimicrobial stewardship campaign was launched nationwide. In 2012, China also implemented the strictest regulation yet for antibiotic stewardship, the Administrative Measures for Clinical Use of Antimicrobial Agents. Previous studies showed that overuse of antibiotics in China’s medical institutions at all levels have been significantly controlled (Lin et al., 2016; Li et al., 2019; Li et al., 2020). However, these studies mainly focused on the change of the frequency or amount of antibiotics. For the conformity of drug type and the appropriateness of treatment time, such evaluation report on prescription quality is currently blank. Moreover, it is noteworthy that the greatest source of antibiotic prescribing for outpatients in primary care is common infections, such as acute respiratory tract infections, acute otitis media, and gastroenteritis, etc. (Pouwels et al., 2019). And one-fourth of the outpatients receiving antibiotics for common infections are children (Dong et al., 2008). A comprehensive evaluation is also urgently needed to identify the quality of antibiotic prescribing for specific diseases and specific populations in these facilities.
Therefore, based on the longitudinal prescription data from community health centers in Shenzhen, China and referring to Chinese guidelines, this study evaluated the quality of antibiotic prescribing in primary care facilities from various aspects to provide a clear reference for antibiotic policy interventions in China.
Materials and Methods
Ethical Approval
This study was approved by the Research Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology. Waiver for informed consent was granted by the ethics committees as no patients were involved in developing the research design or measurement of the outcome indicators.
Study Design and Data Source
We retrospectively analyzed the consultation prescriptions of outpatients in primary care facilities in Shenzhen, China, from January 2010 to December 2015. Shenzhen, a metropolis with 13 million permanent populations, is located in southern China and has relatively developed primary care facilities, named as community health centers (CHCs).
The data were obtained from electronic information systems of CHCs in Xixiang Subdistrict, Shenzhen. Over the study period, there were 33 CHCs in Xixiang Subdistrict. We selected 11 from the 33 CHCs through a simple random sampling method to cover approximately 30% of patients (Li et al., 2020). Then we collected all outpatient prescription data for six consecutive years from their electronic information systems. In this database, each prescription included information on patient sex and age, disease diagnoses, medication costs, and details of prescribed medications (generic name; unit cost; numbers, dosage, and route of administration; treatment days). The International Statistical Classification of Diseases, Tenth Revision (ICD-10) codes was used to classify and code disease diagnoses (World Health Organization, 2014). The antibiotics were identified using the Anatomic Treatment and Chemical (ATC) classification, code J01 (World Health Organization, 2018).
Indicators and Definition
We first adopted four quality indicators including number of antibiotics per 100 consultations, ratio between broad-spectrum and narrow-spectrum antibiotics (B/N ratio), percentage of first-line antibiotics recommended by guidelines and percentage of oral antibiotics with a duration exceeding the guideline recommendation to evaluate the quality of antibiotic prescribing in the overall populations (World Health Organization Regional Office for Europe, 2017; Pouwels et al., 2019). Then, taking into account differences in the prevalence of infection and drug use between children and adults, we used two child-specific indicators including percentage of antibiotics with amoxicillin (A index) and ratio between amoxicillin and broad-spectrum antibiotics (A/B ratio) to further evaluate the use of amoxicillin in children (de Bie et al., 2016). In this study, the broad-spectrum antibiotics included broad-spectrum penicillins, second- and third-generation cephalosporins and macrolides [J01CR, J01DC, J01DD and J01F (without erythromycin)]; the narrow-spectrum antibiotics included narrow-spectrum penicillins, first-generation cephalosporins and erythromycin (J01CE, J01DB and J01FA01) (de Bie et al., 2016). Our reference guideline was the Guidelines for Clinical Application of Antimicrobial Agents in China (2004 edition).
In China, a patient is typically prescribed one prescription per outpatient consultation. A single prescription contains one or more drugs. The number of antibiotics (J01) per 100 consultations was used to reflect the amount of antibiotics consumed by outpatients. The B/N ratio was expressed as the ratio between the number of broad-spectrum antibiotics used and that of narrow-spectrum antibiotics. The smaller the B/N ratio, the most appropriate the prescribing. The percentage of first-line antibiotics recommended by guidelines was expressed as the percentage of the number of first-line antibiotics used over the total number of antibiotics. The percentage of oral antibiotics with a duration exceeding the guideline recommendation was expressed as the percentage of the number of oral antibiotics with an exceeded duration over the total number of oral antibiotics. So the higher the percentage of first-line antibiotics or the lower the percentage of oral antibiotics with an exceeded duration, the most appropriate the prescribing. Furthermore, the A index was defined as the percentage of the number of amoxicillin (J01CA04) used over the total number of antibiotics. The A/B ratio was defined as the ratio between the number of amoxicillin used and those of broad-spectrum antibiotics. Thus, the greater the A index or A/B ratio, the most appropriate the amoxicillin prescribing for children.
Data Analysis
In calculating percentage of first-line antibiotics and percentage of oral antibiotics with an exceeded duration, we included the 12 common infections in Chinese guidelines, including acute sinusitis, acute sore throat, acute cough and bronchitis, community-acquired pneumonia, acute otitis media, gastroenteritis, pericoronitis, acute periapical abscess, pelvic inflammatory disease, bacterial vaginosis, acute prostatitis, cellulitis (Supplementary Table S1). These infections came from the body systems of respiratory, digestive, genitourinary, or skin, and were common primary diagnoses for which antibiotics were generally prescribed in outpatients. The Chinese guidelines had been used for a long time since issued in 2004, and recommended the types of first-line antibiotics for common infections and the duration of antibiotic treatment, so as to regulate the rational use of antibiotics by clinicians. We further evaluated the quality of antibiotic prescribing for each of 12 common infections. Due to the lack of first-line antibiotics recommended and duration of treatment for four common infections (acute cough and bronchitis, community-acquired pneumonia, gastroenteritis, cellulitis) in the Chinese guidelines, we referred to relevant contents from the Public Health England guidance during 2013–2015 which was widely used (Pouwels, et al., 2019). For the analysis of treatment days, we included only oral antibiotics.
To explore the quality of antibiotic prescribing in different populations, particularly in children, we performed a stratified analysis by age group (<5, 5–17, and ≥18 years). To analyze trends in the quality of antibiotic prescribing, we combined all available annual data into three 2-year time periods (2010–2011, 2012–2013, and 2014–2015) and reported the absolute changes in quality indicators during 2010–2011 vs. 2014–2015. Moreover, we also calculated the total number of excess antibiotic days for 12 common infections, defined as the cumulative number of days beyond the recommended duration in the guidelines. We used linear regression analysis to test linear trends of indicators over time. The confidence interval (CI) was calculated using a logit transformation based on the estimated standard error. All statistical tests were two sided, and p values <0.05 were considered significant. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, United States).
Results
Characteristics of Antibiotic Prescribing
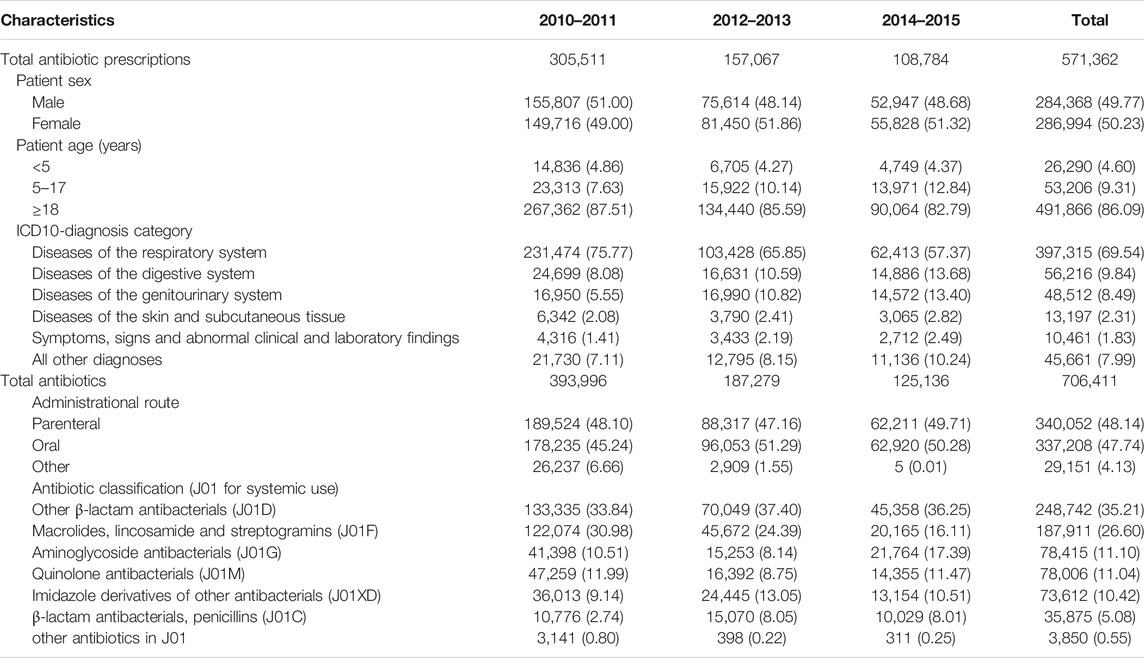
Between 2010 and 2015, 1,482,223 outpatient consultations were conducted from 11 participating CHCs. Of these, 571,362 (38.55%) consultations led to antibiotic prescriptions, which contained 706,411 antibiotics. Among all antibiotic prescriptions, 79,496 (13.91%) antibiotic prescriptions were issued in young children <18 years. And the top three systematic diagnoses for antibiotic prescriptions were the diseases of respiratory, digestive, and genitourinary systems, accounting for 69.54, 9.84, and 8.49%, respectively. Among all antibiotics, the frequencies of oral antibiotics used were 337,208 (47.74%). A total of 90% of antibiotics were in turn covered by cephalosporins, macrolides, aminoglycosides, quinolones, imidazoles, and penicillins, involving 23 antibiotic classes. See Table 1 for details.
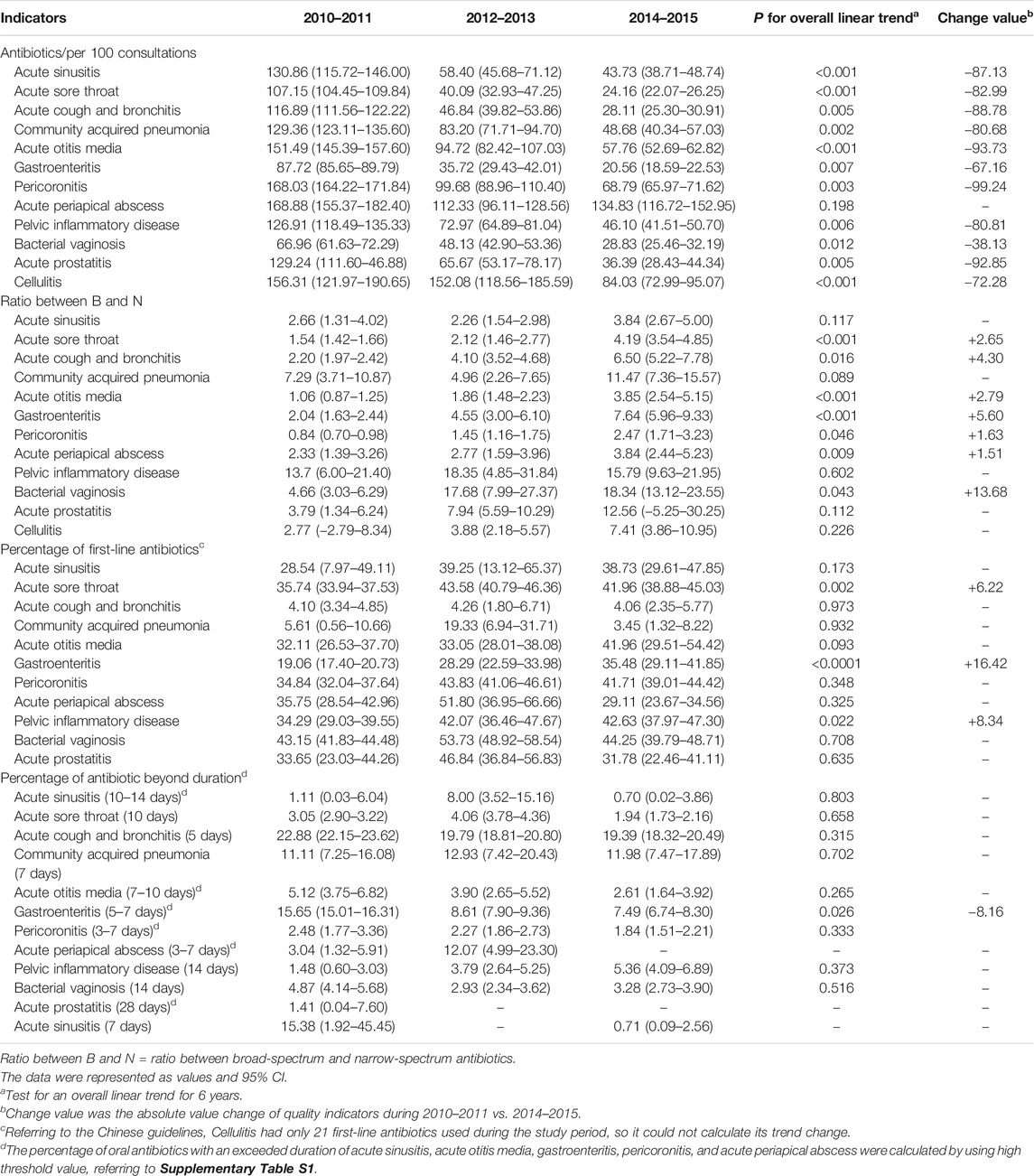
Evaluation of the Quality of Overall Antibiotic Prescribing
The analysis of overall antibiotic prescribing showed that the number of antibiotics per 100 consultations decreased significantly from 93.50 in 2010 to 19.98 in 2015 (p = 0.004). The number of antibiotics used in different age groups decreased to different degrees, and the decrease was most evident in children aged <5 years, from 85.47 in 2010 to 10.37 in 2015 (p = 0.009) (Figure 1A). The overall B/N ratio showed an increasing trend over time (p = 0.009), and the increase was also most evident in children aged <5 years (p = 0.020) (Figure 1B). Referring to the Chinese guidelines, the overall percentage of first-line antibiotics for 12 common infections increased from 26.42% in 2010 to 34.91% in 2015, but the trend change was not statistically significant (p = 0.054) (Figure 1C). The percentage of first-line antibiotic used in different age groups first increased and then decreased, and the trend change was not obvious. In addition, the overall percentage of oral antibiotics with an exceeded duration for 12 common infections increased from 11.99% in 2010 to 13.38% in 2015. However, the trend change was not statistically significant (p = 0.181) (Figure 1D). Detailed data were shown in Supplementary Table S2.
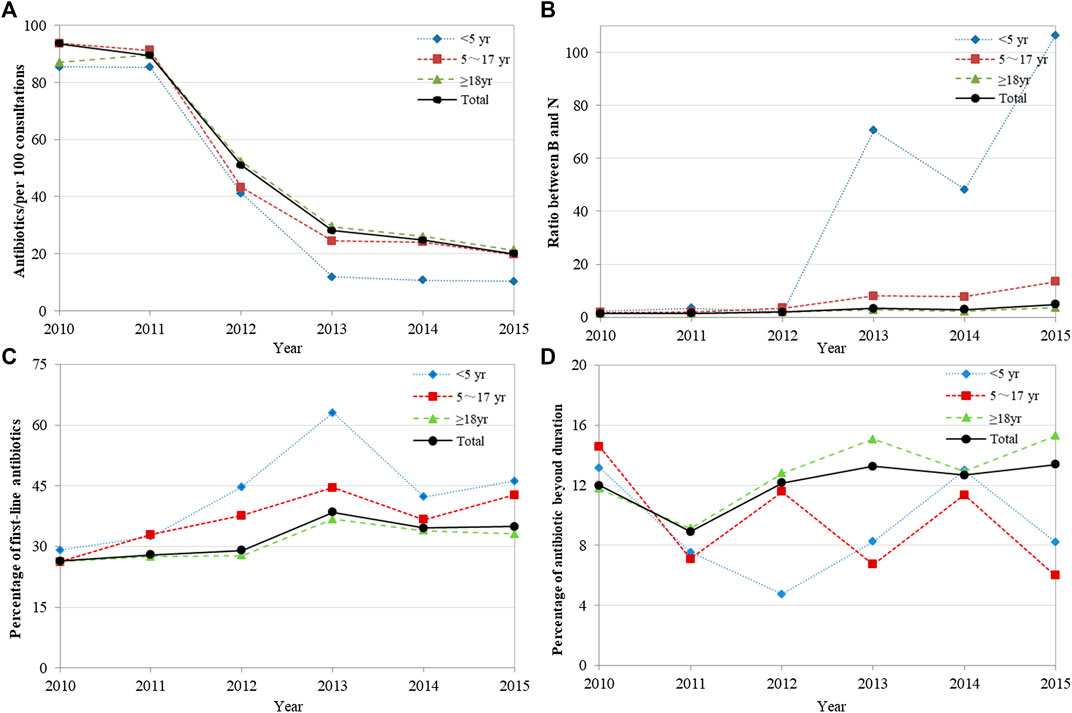
FIGURE 1. Changes in the quality of overall antibiotic prescribing, 2010–2015. (A) Antibiotics/per 100 consultations; (B) Ratio between B and N; (C) Percentage of first-line antibiotics recommended by guidelines; (D) Percentage of oral antibiotics with a duration exceeding the guideline recommendation. Ratio between B and N = Ratio between broad-spectrum and narrow-spectrum antibiotics.
Evaluation of the Quality of Antibiotic Prescribing for Common Infections
During the study period, the total number of antibiotics used for the 12 included infections was 337,859. The results of different infections showed that except for acute periapical abscess (p = 0.198), the number of antibiotics used for other infections decreased to varying degrees. Acute otitis media decreased the most, with the number of absolute antibiotic changes per 100 consultations being −93.73 between 2010–2011 and 2014–2015 (p < 0.001) (Table 2). The B/N ratio of seven infections involving the systems of respiratory, digestive, and genitourinary showed different degrees of increase, and the B/N ratio of bacterial vaginosis in women was the highest by 2014–2015 at 18.34 (95% CI: 13.12 to 23.55) (Table 2). Moreover, the total number of first-line antibiotics recommended for 12 included infections was 103,787 (30.72% of total). The results of different infections showed that the percentages of first-line antibiotics recommended by guidelines ranged from 3.45 to 44.25% by 2014–2015. Although the percentages of first-line antibiotics used in acute sore throat, gastroenteritis, and pelvic inflammatory disease in women increased significantly by 6.22, 16.42, and 8.34%, respectively, the percentages of first-line antibiotics in these infections were still less than 50% (Table 2). The total number of oral antibiotics used for these 12 infections was 154,917, and 17,939 (11.58%) were oral antibiotics with an exceeded duration. The percentages of oral antibiotics with an exceeded duration for different infections ranged from 0.70 to 19.39% by 2014–2015, and this translated into 51,051 excess antibiotic days for these 12 infections. Despite a significant decline of 8.16% in this percentage of gastroenteritis (p = 0.026), 19.39% (95% CI: 18.32–20.49%) was still found in this percentage of acute cough and bronchitis (Table 2).
Evaluation of the Quality of Child-Specific Antibiotic Prescribing
Analysis of the quality of child-specific antibiotic prescribing showed that the A index and the A/B ratio first increased and then decreased overall, with no statistical difference in trend change (p = 0.262 and p = 0.539) (Figures 2A,B). These two indicators have been at low levels for a long time, 0.76% and 0.01 by 2015, respectively. Furthermore, amoxicillin use was lower in children aged <5 years than in those aged 5–17 years. Detailed data were shown in Supplementary Table S2.
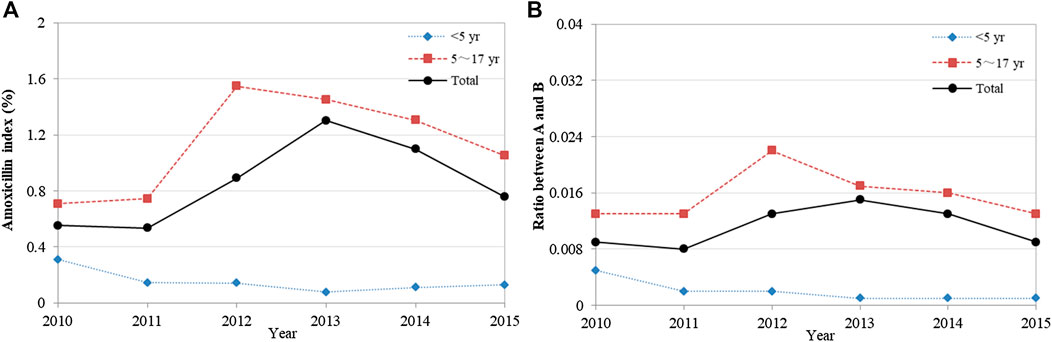
FIGURE 2. Changes in the quality of child-specific antibiotic prescribing, 2010–2015. (A) Amoxicillin index (%); (B) Ratio between A and B. Amoxicillin index (%) = Percentage of antibiotics with amoxicillin; Ratio between A and B = Ratio between amoxicillin and broad-spectrum antibiotic.
Discussion
This study comprehensively evaluated the quality of antibiotic prescribing in primary care facilities in Shenzhen, China. We found that, despite a significant decline in the number of antibiotic used, the B/N ratio increased over time, and the percentages of first-line antibiotics used for most infections and the use of amoxicillin in children were low. These inappropriate antibiotic prescribing might be an important aspect of future antibiotic stewardship in primary care facilities.
In this study, both the overall antibiotic usage and the use of antibiotics for common infections showed a significant downward trend. This was consistent with those reported in previous studies in China (Lin et al., 2016; Li et al., 2019; Li et al., 2020), suggesting that the implementation of antibiotic policies had dramatically reduced the use of antibiotics in primary care facilities. Although the use of antibiotic had declined to a low level, the quality of outpatient antibiotic prescribing was still worth improving in several aspects. First, the use of broad-spectrum antibiotics in most infections of the respiratory, digestive, and genitourinary systems was several times that of narrow-spectrum antibiotics, and this gap had been increasing over time, with bacterial vaginosis in women reaching 18.34 times. This was consistent with the results reported in previous studies that Chinese prescribers tended to favor broad-spectrum antibiotics (Wang et al., 2014; Xiao et al., 2016). Second, the results based on the Chinese guidelines showed that the percentages of first-line antibiotics for 12 common infections were not high, with no more than 50%. And the percentage of oral antibiotics with an exceeded duration for acute cough and bronchitis was still 19.39%. Promoting the appropriate use of antibiotics can be achieved by choosing first-line antibiotics recommended by guidelines when a disease is clearly diagnosed, or avoiding unnecessarily long durations of treatment (Lode, 2014; Spellberg, 2016; Smieszek et al., 2018). Obviously, there is a substantial scope for improving the quality of antibiotic prescribing if prescribers in our study are better adherent to recommended durations of antibiotic treatment. At least, 51,051 days of unnecessary antibiotic could be reduced. Third, for Children’s prescriptions in primary care, although the number of antibiotic used in children aged <5 years declined the most, the B/N ratio was the greatest. Moreover, the use of amoxicillin in children was extremely low, with the A index at 0.76% by 2015. However, this indicator ranged from 30 to 60% in the Netherlands, United Kingdom and Italy (de Bie et al., 2016). Acute respiratory tract infections remained by far the most common indications for children antibiotic prescribing in community practice. Many guidelines recommend amoxicillin as the first-line choice for suspected bacterial respiratory infections, including pneumonia and otitis media (Bradley et al., 2011; Harris et al., 2011; World Health Organization, 2012). For example, amoxicillin became the most highly prescribed antibiotic in pediatric emergency departments and by private practice pediatricians after publication of the new French national guidelines (Ouldali et al., 2017). Appropriate selection of narrow-spectrum antibiotics and encouraging the use of amoxicillin should be an important content of improving the quality of children antibiotic prescribing in China.
Our study suggested that the quality of antibiotic prescribing in Shenzhen’s primary care was not high. This might be due to the following reasons. First, the contents of China’s antibiotic policies were not perfect. The primary objective of these interventions, whether the national antimicrobial stewardship campaign in 2011 or the Administrative Measures for Clinical Use of Antimicrobial Agents in 2012, was to control the quantity of antibiotic use. For example, the stewardship campaign required that the percentage of outpatient prescriptions with antibiotics not exceed 20% by the end of 2013. However, there was no strict control requirement for the appropriate type of antibiotic use, such as broad-spectrum antibiotics. Second, although China formulated the Guidelines for Clinical Application of Antimicrobial Agents in China, insufficient attention had been paid to the implementation of this guidelines in prescribing behaviors. Because there was basically no research on evaluating the type conformity and time appropriateness of antibiotic prescribing based on Chinese guidelines. Therefore, improving the contents of the antibiotic policy and paying more attention to the practice guidelines, so as to guide the prescriber to prescribe antibiotics correctly, are also the work that cannot be ignored in the antibiotic stewardship.
This study was the first to evaluate in detail the quality of antibiotic prescribing for common infections in primary care facilities in China. Our study selected rich quality indicators, involved many common infections, and carried out the specific evaluations of children. This comprehensive report provided clues to the future antibiotic stewardship from various aspects in China. Second, we used the published Chinese guidelines to evaluate the quality of antibiotic prescribing. This kind of guideline-based evaluation study was of great significance to identify the compliance of prescribers with the guidelines and the rationality of prescribing behaviors. Third, the data of our study were based on the entire prescriptions rather than sampling data, which avoided sampling bias and provided more realistic and reliable assessment. Furthermore, this electronic information system was regularly checked by data inspectors, which ensured the accuracy of the data in this study.
However, our study had several limitations when interpreting the findings. First, this study only carried out the evaluation of prescription quality in primary care facilities in Shenzhen. Further studies with wider coverage and larger sample sizes are needed to evaluate the quality of antibiotic prescribing in China’s primary care. Nevertheless, this study serves as a practical case to provide policy makers and researchers with valuable information on prescription quality. Second, only one primary diagnosis, which was determined by the physician based on a patient’s chief complaint, was documented on our prescription records. It was not clear whether the prescriber decided to replace antibiotics or longer the duration of treatment because of the patient’s other diseases or conditions. Thus, the magnitude of irrational antibiotic use in this regard might be overestimated. Third, we did not get records for culture of infecting pathogens in patients. Therefore, we could not identify whether the antibiotic usage was based on empirical or definitive therapy. We also could not combine patients’ prescription records with laboratory results to determine the objective medication regimen developed by the prescribers. This is difficult because we have limited access to outpatient information. This implied the need to strengthen the standardization and integrity of prescription records in primary care facilities in order to provide more reliable data for prescription evaluation. Fourth, there is a time lag in this study. However, considering that inappropriate use of antibiotics in China’s medical institutions is a long-standing problem, the poor quality of these antibiotic prescriptions is unlikely to be improved significantly. Thus, our results should be still applicable. Furthermore, the comprehensive evaluation model of the quality of antibiotic prescribing in this study can optimize antibiotic stewardship and is worthy of reference in other regions.
Conclusion
In summary, a practice study in Shenzhen, China, found a significant decrease in the use of antibiotics in primary care facilities. However, the prevalence of broad-spectrum antibiotics in most common infections, the low use of first-line antibiotics, and the poor quality of antibiotic prescribing in children were serious problems. China’s future antibiotic stewardship campaign should be devoted to improving the rationality of antibiotic types and treatment time, and standardizing the content of antibiotic use in children, so as to comprehensively improve the quality of antibiotic prescribing.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available from the corresponding author on reasonable request.
Ethics Statement
Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author Contributions
Conception and design: YG, HL, and XY. Data acquisition: HY, KT, and WL. Analysis and interpretation of data: YG, HL, XL, and JW. Drafting or revising the article critically for important intellectual content: YG, HL, GZ, and XY. Supervision: GZ and XY. Funding obtain: XY. Final approval of the version to be submitted: YG, HL, HY, KT, WL, XL, JW, GZ, and XY.
Funding
This work was supported by National Natural Science Foundation of China “Research on Intervention of Self-medication of Antibiotics Based on the Knowledge Translation Theory” (No. 71874060) and “Empirical and Methodological Research on the Evaluation of Antibiotic Management Policies” (No. 71403091). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2020.617260/full#supplementary-material.
Abbreviation
A index, percentage of antibiotics with amoxicillin; A/B ratio, ratio between amoxicillin and broad-spectrum antibiotics; AMR, antimicrobial resistance; B/N ratio, ratio between broad-spectrum and narrow-spectrum antibiotics; CHCs, community health centers; CI, confidence interval, UK, United Kingdom; WHO, World Health Organization.
References
Bradley, J. S., Byington, C. L., Shah, S. S., Alverson, B., Carter, E. R., Harrison, C., et al. (2011). Executive summary: the management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin. Infect. Dis. 53 (7), 617–630. doi:10.1093/cid/cir625
China National Health Commission (2018). China Health Statistics Yearbook 2018. (Beijing, China: Chinese Peking Union Medical College Press).
de Bie, S., Kaguelidou, F., Verhamme, K. M., De Ridder, M., Picelli, G., Straus, S. M., et al. (2016). Using prescription patterns in primary care to derive new quality indicators for childhood community antibiotic prescribing. Pediatr. Infect. Dis. J. 35 (12), 1317–1323. doi:10.1097/INF.0000000000001324
Dong, L., Yan, H., and Wang, D. (2008). Antibiotic prescribing patterns in village health clinics across 10 provinces of Western China. J. Antimicrob. Chemother. 62 (62), 410–415. doi:10.1093/jac/dkn153
Harris, M., Clark, J., Coote, N., Fletcher, P., Harnden, A., McKean, M., et al. (2011). British Thoracic Society guidelines for the management of community acquired pneumonia in children: update 2011. Thorax. 66 (Suppl 2), ii1–ii23. doi:10.1136/thoraxjnl-2011-200598
Li, H., Gong, Y., Han, J., Zhang, S., Chen, S., Xu, X., et al. (2020). Interrupted time-series analysis to evaluate the impact of a national antimicrobial stewardship campaign on antibiotic prescribing: a typical practice in China’s primary care. Clin. Infect. Dis. [Online ahead of print]. doi:10.1093/cid/ciaa962
Li, H., Yan, S., Li, D., Gong, Y., Lu, Z., and Yin, X. (2019). Trends and patterns of outpatient and inpatient antibiotic use in China’s hospitals: data from the Center for Antibacterial Surveillance, 2012-16. J. Antimicrob. Chemother. 74 (6), 1731–1740. doi:10.1093/jac/dkz062
Lin, H., Dyar, O. J., Rosales-Klintz, S., Zhang, J., Tomson, G., Hao, M., et al. (2016). Trends and patterns of antibiotic consumption in Shanghai municipality, China: a 6 year surveillance with sales records, 2009-14. J. Antimicrob. Chemother. 71 (6), 1723–1729. doi:10.1093/jac/dkw013
Liu, C., Liu, C., Wang, D., Deng, Z., Tang, Y., and Zhang, X. (2019). Determinants of antibiotic prescribing behaviors of primary care physicians in Hubei of China: a structural equation model based on the theory of planned behavior. Antimicrob. Resist. Infect. Contr. 8, 23. doi:10.1186/s13756-019-0478-6
Lode, H. M. (2014). Preserving the efficacy of front-line fluoroquinolones through selective use to optimise clinical outcomes. Int. J. Antimicrob. Agents. 43 (6), 497–507. doi:10.1016/j.ijantimicag.2014.02.014
National Health Commission of the People’s Republic of China (2005). Guidelines on the clinical application of antibiotics. Available at: http://www.nhc.gov.cn/wjw/zcjd/201304/2da63e01325e4df8a235590112321403.shtml (Accessed July 10, 2020).
Ouldali, N., Bellêttre, X., Milcent, K., Guedj, R., de Pontual, L., Cojocaru, B., et al. (2017). Impact of implementing national guidelines on antibiotic prescriptions for acute respiratory tract infections in pediatric emergency departments: an interrupted time series analysis. Clin. Infect. Dis. 65 (9), 1469–1476. doi:10.1093/cid/cix590
Pouwels, K. B., Hopkins, S., Llewelyn, M. J., Walker, A. S., McNulty, C. A., and Robotham, J. V. (2019). Duration of antibiotic treatment for common infections in English primary care: cross sectional analysis and comparison with guidelines. BMJ. 364, l440. doi:10.1136/bmj.l440
Robertson, J., Iwamoto, K., Hoxha, I., Ghazaryan, L., Abilova, V., Cvijanovic, A., et al. (2018). Antimicrobial medicines consumption in Eastern Europeand Central Asia-an updated cross-national study and assessment of QuantitativeMetrics for policy action. Front. Pharmacol. 9, 1156. doi:10.3389/fphar.2018.01156
Sabuncu, E., David, J., Bernède-Bauduin, C., Pépin, S., Leroy, M., Boëlle, P. Y., et al. (2009). Significant reduction of antibiotic use in the community after a nationwide campaign in France, 2002-2007. PLoS Med. 6 (6), e1000084. doi:10.1371/journal.pmed.1000084
Smieszek, T., Pouwels, K. B., Dolk, F. C. K., Smith, D. R. M., Hopkins, S., Sharland, M., et al. (2018). Potential for reducing inappropriate antibiotic prescribing in English primary care. J. Antimicrob. Chemother. 73 (Suppl 2), ii36–ii43. doi:10.1093/jac/dkx500
Spellberg, B. (2016). The new antibiotic mantra-“shorter is better”. JAMA Intern. Med. 176 (9), 1254–1255. doi:10.1001/jamainternmed.2016.3646
Tyrstrup, M., van der Velden, A., Engstrom, S., Goderis, G., Molstad, S., Verheij, T., et al. (2017). Antibiotic prescribing in relation to diagnoses and consultation rates in Belgium, The Netherlands and Sweden: use of European quality indicators. Scand. J. Prim. Health Care. 35 (1), 10–18. doi:10.1080/02813432.2017.1288680
Wang, J., Wang, P., Wang, X., Zheng, Y., and Xiao, Y. (2014). Use and prescription of antibiotics in primary health care settings in China. JAMA Intern. Med. 174 (12), 1914–1920. doi:10.1001/jamainternmed.2014.5214
Wei, X., Zhang, Z., Walley, J. D., Hicks, J. P., Zeng, J., Deng, S., et al. (2017). Effect of a training and educational intervention for physicians and caregivers on antibiotic prescribing for upper respiratory tract infections in children at primary care facilities in rural China: a cluster-randomised controlled trial. Lancet Glob. Health. 5 (12), e1258–e1267. doi:10.1016/S2214-109X(17)30383-2
World Health Organization (2012). Recommendations for management of common childhood conditions. Available at: https://www.ncbi.nlm.nih.gov/books/NBK138333/ (Accessed July 15, 2020).
World Health Organization (2014). International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10)-2014-WHO Version for 2014. Available at: http://apps.who.int/classifications/icd10/browse/2014/en#/X (Accessed July 12, 2020).
World Health Organization (2016). WHO methodology for a global programme on surveillance of antimicrobial consumption. Available at: https://www.who.int/medicines/areas/rational_use/WHO_AMCsurveillance_1.0.pdf (Accessed July 11, 2020).
World Health Organization (2018). WHO Collaborating Centre for Drug Statistics Methodology. Available at: http://www.whocc.no/atc_ddd_index/.
World Health Organization Regional Office for Europe (2017). Antimicrobial Medicines Consumption (AMC) Network, 2011-2014. Available at: https://www.euro.who.int/__data/assets/pdf_file/0007/337984/51020-WHO-AMC-report-web.pdf.
Xiao, Y. (2018). Antimicrobial stewardship in China: systems, actions and future strategies. Clin. Infect. Dis. 67 (Suppl. l_2), S135–S141. doi:10.1093/cid/ciy641
Xiao, Y., Wang, J., Shen, P., Zheng, B., Zheng, Y., and Li, L. (2016). Retrospective survey of the efficacy of mandatory implementation of the Essential Medicine Policy in the primary healthcare setting in China: failure to promote the rational use of antibiotics in clinics. Int. J. Antimicrob. Agents. 48 (4), 409–414. doi:10.1016/j.ijantimicag.2016.06.017
Xiao, Y., Zhang, J., Zheng, B., Zhao, L., Li, S., and Li, L. (2013). Changes in Chinese policies to promote the rational use of antibiotics. PLoS Med. 10 (11), e1001556. doi:10.1371/journal.pmed.1001556
Keywords: antibiotic prescribing, quality evaluation, primary care, antibiotic stewardship, longitudinal study, China
Citation: Gong Y, Li H, Yang H, Tan K, Liu W, Li X, Wu J, Zhang G and Yin X (2021) Evaluation of the Quality of Antibiotic Prescribing in Primary Care: A Multicenter Longitudinal Study From Shenzhen, China. Front. Pharmacol. 11:617260. doi: 10.3389/fphar.2020.617260
Received: 14 October 2020; Accepted: 30 November 2020;
Published: 19 February 2021.
Edited by:
Maribel Salas, Daiichi Sankyo, United StatesReviewed by:
Muhammad Usman, University of Veterinary and Animal Sciences, PakistanMmamosheledi Elsie Mothibe, Sefako Makgatho Health Sciences University, South Africa
Copyright © 2021 Gong, Li, Yang, Tan, Liu, Li, Wu, Zhang and Yin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoxv Yin, eXh4QGh1c3QuZWR1LmNu
†These authors have contributed equally to this work
 Yanhong Gong1†
Yanhong Gong1† Xiaoxv Yin
Xiaoxv Yin