- 1Guanganmen Hospital, China Academy of Chinese Medical Sciences, Beijing, China
- 2Graduate school, Beijing University of Chinese Medicine, Beijing, China
- 3School of Pharmacy, Peking University Health Science Center, Beijing, China
- 4Traditional Chinese Medicine Department, Cancer Hospital Chinese Academy of Medical Sciences, Beijing, China
Background: Kanglaite injection (KLTI) is a traditional Chinese medicine (TCM) preparation with anti-tumor activity, which has been used to treat malignant tumors in China. The purpose of this study was to evaluate the efficacy and safety of intrapleural infusion with KLTI in the treatment of malignant pleural effusion (MPE).
Methods: Randomized controlled trials (RCTs) on the efficacy and safety of intrathoracic infusion with KLTI in the treatment of MPE were searched from the PubMed, EMBASE, the Cochrane Library, CNKI, VIP, Wanfang and CBM databases. The primary outcome was objective remission rate (ORR). Secondary outcomes included quality of life (QOL) and incidence of adverse events (AEs). The Stata15.1 software and RevMan5.3 software were used to calculate risk ratios (RR) at 95% confidence intervals (CI) and conduct the meta-analysis.
Results: This meta-analysis included 20 RCTs, involving 1,291 patients. The ORR of intrapleural infusion with KLTI + chemotherapy drugs in the treatment of MPE was higher than that of chemotherapy alone (RR) 1.23; 95%CI; 1.11–1.36, I2 = 0%, z = 3.876, p = 0.000]. When KLTI is combined with cisplatin or KLTI 200 ml is used in every time, it is more advantageous to improve ORR. Moreover, compared with intrapleural infusion of chemotherapy drugs alone, KLTI combined with chemotherapy drugs significantly improved the QOL of patients with MPE (RR 1.28; 95%CI; 1.70–1.53, I2 = 0%, z = 2.70, p = 0.007). In addition, the participation of KLTI reduced the gastrointestinal reaction (RR 0.79; 95% CI; 0.66–0.96; I2 = 0%, z = 2.37, p = 0.018) and renal damage (RR 0.468; 95% CI; 0.23–0.945, I2 = 0%, z = 2.11, p = 0.035) caused by chemotherapy drugs, but did not increase other adverse reactions (p > 0.05).
Conclusion: The efficacy and safety of traditional chemotherapy drugs plus KLTI was superior to traditional chemotherapy drugs alone via intrapleural injection in controlling MPE, which suggested that KLTI can be used to treat MPE. However, a more rigorous RCT should be designed and completed before it is widely recommended.
Introduction
Malignant pleural effusion (MPE), a common complication of advanced malignant tumor, is made by malignant tumor involving pleura or pleural primary tumor. (Heffner, 2008). The aggravation of MPE will lead to obvious dyspnea, which will affect the quality of life (QOL) of patients, and even shorten the survival time. With the prolongation of survival time of patients with malignant tumor, the incidence of MPE gradually increased (Zarogoulidis et al., 2013). Although anti-tumor therapy continues to develop, the preventive and therapeutic effect of MPE is not satisfactory. Some studies have shown that MPE is closely related to shorter survival time. Lung cancer patients with MPE have a survival time of only 5.5 months (Porcel et al., 2015), and patients with other types of cancer with MPE have an overall survival time of 3–12 months (Roberts et al., 2010).
In China, traditional Chinese medicine (TCM) has been used for thousands of years. Supported by modern evidence-based evaluation methods and basic research evidence, it shows that TCM has obvious advantages in anti-tumor and reducing side effects, which is widely used as an alternative or combined treatment of cancer (Wang et al., 2021; Zhang et al., 2021). Kanglaite injection (KLTI), extracted from Coix seed, is one of the most popular anti-cancer TCM injections in China (NCI Dictionary, 2019). In 1995, KLTI was approved by China’s State Food and Drug Administration (drug approval number: Z10970091) for cancer treatment and widely used in anti-tumor therapy (China Food and Drug Administration, 2019; Liu et al., 2019; Li et al., 2020). Since 2002, a series of KLTI clinical studies (NCT00733850, NCT00031031) for cancer patients have been approved and carried out in the United States (Clinicaltrials.gov., 2019). KLTI has been approved by the Ministry of Health of the Russian Federal government as a prescription drug for the treatment of cancer in Russia. Clinical trials have showed that KLTI combined with chemotherapy can better delay the progression of tumor patients, improve disease control rate, prolong survival time and reduce toxicity (Schwartzberg et al., 2017; Lian et al., 2006). Basic studies have also shown that KLTI has a variety of anticancer-related activities, such as promoting apoptosis, destroying the mitotic process, anti-multidrug resistance of tumor cells and improving cellular immunity (Yang et al., 2018; Chen et al., 2021).
Intrapleural perfusion is still one of the main methods for the treatment of MPE, which can increase local drug concentration, cause chemical inflammatory reaction between visceral pleura and mural pleura, stimulate pleural cells to produce mesothelial fibrosis, promote pleural adhesion, reduce pleural permeability and reduce pleural effusion exudation, so as to achieve the purpose of controlling pleural effusion (Scherpereel et al., 2010). However, the adverse reactions caused by intrapleural perfusion of chemotherapeutic drugs are difficult for patients to tolerate, affecting their QOL, so not all MPE patients can benefit from it (Biaoxue et al., 2016). At present, some studies have found that KLTI combined with chemotherapy drugs for intrapleural perfusion has better efficacy than chemotherapy drugs alone, and the incidence of adverse reactions is low. However, the sample sizes of those most clinical studies were small and their quality were low. There was no systematic evaluation method for the efficacy of this therapy to do further evidence-based medicine support. In this study, meta-analysis was used to integrate the clinical research literature of intrapleural perfusion with chemotherapy drugs plus KLTI in the treatment of MPE, in order to provide evidence-based medical evidence for enriching the clinical application of MPE. No similar research topics were found in the PROSPERO website based on the search strategy “(Malignant Pleural Effusion) AND (Kanglaite).”
Methods
This study was conducted in accordance with the Cochrane Handbook on Systematic Review of Interventions and presented in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) Guidelines (Liberati et al., 2009) (Supplementary Table S1).
Identification of Literature
We searched and identified the relevant RCTs from the PubMed, EMBASE, the Cochrane Library, CNKI, VIP, Wanfang, and CBM databases (from the establishment of the database to January 2021). The keywords used in the search were as follows: (((“Pleural Effusion, Malignant” (Mesh)) OR (Malignant Pleural Effusion*(Title/Abstract])) OR (MPE (Title/Abstract))) AND ((Kanglaite (Title/Abstract)) OR (Coix Seed Oil (Title/Abstract))) (Supplementary Table S2). In addition, if we found that the references included in the study were closely related to intrapleural perfusion with KLTI, we should further search and identify them. The retrieved research was considered as a potential source and is reviewed manually. Only Chinese and English documents were included.
Data Variables of Studies
The data we extracted from the original literature are as follows: 1) the year of publication, first author, country of publication; 2) the design type, random mode and implementation method of the study; 3) the number of cases studied and their age, sex and pathological type of tumor and 4) drugs, dosage, course of treatment and treatment time. According to Response Evaluation Criteria in Solid Tumors (RECIST), the outcome data in this meta-analysis included objective remission rate (ORR), Karnofsky score (KPS) and incidence of adverse reactions. The changes of tumor condition include complete response (CR), partial response (PR), stable disease (SD) and progressive disease (PD). ORR was defined as CR + PR.
Inclusion Criteria of the Study
1) The study design is limited to RCTs comparing traditional chemotherapy drugs plus KLTI (Treatment group) with chemotherapy alone (Control group) in the treatment of MPE; 2) the subjects of MPE must be diagnosed pathologically and/or cytologically and 3) the outcomes must be determined according to RECIST, and the QOL changes must be assessed by KPS.
Exclusion Criteria of the Study
1) Animal experiments, reviews and other unrelated studies; 2) patients also receiving treatment drugs outside the regimen; 3) no detailed data on ORR, QOL and adverse reactions, or no indicators for them; 4) lack of comparable control groups and 7) single-arm study.
Supervision of the Implementation Process
The test design must meet the following rules: 1) RCTs of traditional chemotherapy drugs plus KLTI versus traditional chemotherapy drugs alone via intrapleural injection for controlling MPE; 2) the dosage of KLTI was determined by the suggestions of producers, usually 100 ml or 200 ml; 3) number of times of administration: more than or equal to 2 times and 4) observations on efficacy and safety: The main efficacy index was ORR. Subgroup analysis was conducted according to whether combined with cisplatin and the dose of KLTI, in order to clarify the different efficacy of KLTI in each subgroup. Secondary measures included QOL and incidence of adverse events (AEs). AEs included gastrointestinal reactions, myelosuppression, chest pain, fever and renal damage.
Assessment for Quality of Randomized Controlled Trials
For each included study, two investigators (XMW and RKG) completed the Jadad scale used specifically for the quality of the evaluation method. A third-party researcher (XXZ) was consulted whenever there was a disagreement between the two investigators. The evaluation criteria provided in the Cochrane manual were used to evaluate the quality of the included studies. It includes the following items: 1) random sequence generation (selection bias); 2) blinding of participants and personnel (performance bias); 3) allocation concealment (selection bias); 4) incomplete outcome data (attrition bias); 5) selective reporting (reporting bias) and 6) other bias. According to the above criteria, the quality of the trial is divided into three levels: low bias risk, unclear bias risk, and high bias risk (Xu et al., 2016).
Statistical Methods and Analysis
Stata 15.1 software was used for this meta-analysis. The risk ratios (RR) was used to analyze the binary variables. By calculating the Z value of chi-square test, p < 0.05 is considered to have significant difference. Chi-square (X2) test was used for heterogeneity test, and heterogeneity was quantitatively estimated with I-squared (I2). If I2 ≤ 50% and p ≥ 0.1, the homogeneity is good; if heterogeneity exists, the random-effects model would be used to address it. If the heterogeneity test is obvious (I2 > 75%), meta regression and subgroup analysis should be considered to explore the source of heterogeneity. p values less than 0.05 were considered statistically significant. We use funnel chart to determine publication bias.
Results
Literature Retrieval Process
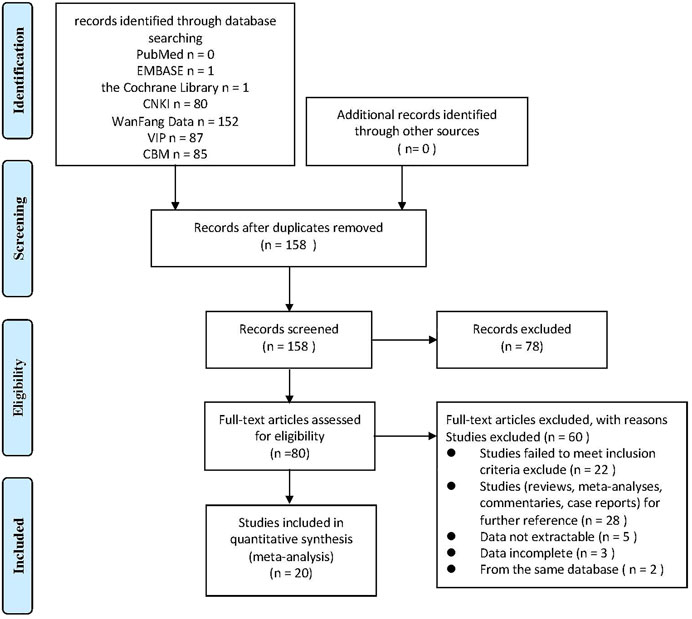
We conducted a systematic search from the database and obtained a total of 406 potential related original studies. 248 repetitive literatures were selected and deleted, the titles and abstracts of the remaining 158 literatures were browsed. 78 of the studies were deleted because the design and implementation of them did not conform to our research theme. After reading the full text of the literature for further screening and evaluation, 60 articles were excluded, including studies that did not meet the inclusion criteria, not belong to clinical studies, the data being incomplete or not be extracted, and from the same database. Finally, a total of 20 original studies were included in the meta-analysis. The flow chart showing the selection process was presented in Figure 1.
General Characteristics of Included Studies
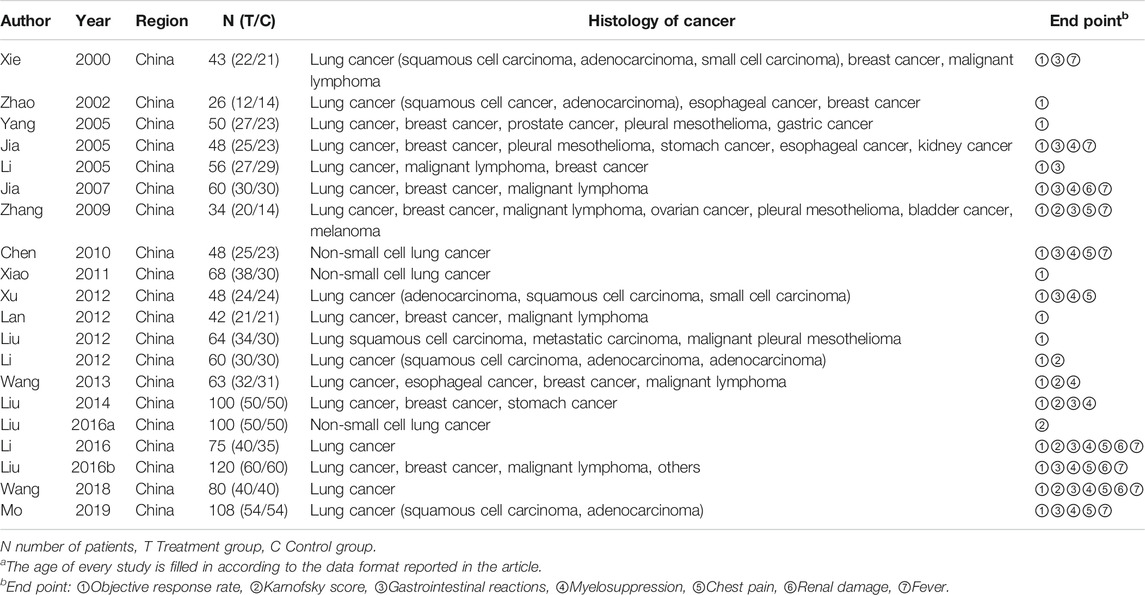
The 20 original studies (Xie and Zhou, 2000; Zhao et al., 2002; Yang et al., 2005; Jia et al., 2005; Li and Cai, 2005; Jia et al., 2007; Zhang et al., 2009; Chen et al., 2010; Xiao et al., 2011; Xu et al., 2012; Lan et al., 2012; Liu and Zhang, 2012; Li et al., 2012; Wang et al., 2013; Liu et al., 2014; Liu et al., 2016a; Li et al., 2016; Liu et al., 2016b; Wang et al., 2018; Mo et al., 2019) included were all RCTs, all of which were conducted in China, including a total of 1,291 patients. The sample size of the study ranges from 26 (Zhao et al., 2002) to 120 (Liu et al., 2016b). One of the studies did not report the sex and age distribution of the patients (Yang et al., 2005). Patients in other studies were between 21 (Xu et al., 2012) and 87 (Jia et al., 2005) years old, and there were more male (733) than female (520). In all studies, malignant tumors were diagnosed by pathology or pleural effusion cytology. Lung and breast cancer were the most common causes of MPE in the included studies. Table 1 lists the basic information in 20 studies.
There were 14 studies (Xie and Zhou, 2000; Jia et al., 2005; Li and Cai, 2005; Yang et al., 2005; Jia et al., 2007; Zhang et al., 2009; Chen et al., 2010; Lan et al., 2012; Li et al., 2012; Liu and Zhang, 2012; Xu et al., 2012; Wang et al., 2013; Li et al., 2016; Mo et al., 2019) of intrapleural infusion of platinum chemotherapeutic drugs and KLTI in the treatment of MPE, of which 10 studies (Xie and Zhou, 2000; Yang et al., 2005; Jia et al., 2005; Li and Cai, 2005; Jia et al., 2007; Zhang et al., 2009; Chen et al., 2010; Lan et al., 2012; Liu and Zhang, 2012; Li et al., 2012; Li et al., 2016) used cisplatin, two studies (Xu et al., 2012; Wang et al., 2013) used carboplatin, and two studies used lobaplatin (Mo et al., 2019) and oxaliplatin (Li et al., 2016) respectively. In addition, four studies used cisplatin + doxorubicin (Zhao et al., 2002), hydroxycamptothecin (Xiao et al., 2011), docetaxel (Liu et al., 2014) or recombinant human interleukin-2 (Mo et al., 2019), and arsenite was used in two studies (Liu et al., 2016a; Liu et al., 2016b). The dosage of KLTI was 100 ml or 200 ml each time, and at least once. Pleural perfusion was performed after pleural effusion drainage. There was no significant difference in baseline data between the two groups (p > 0.05), indicating that they were comparable. Table 2 lists the treatments in 20 studies.
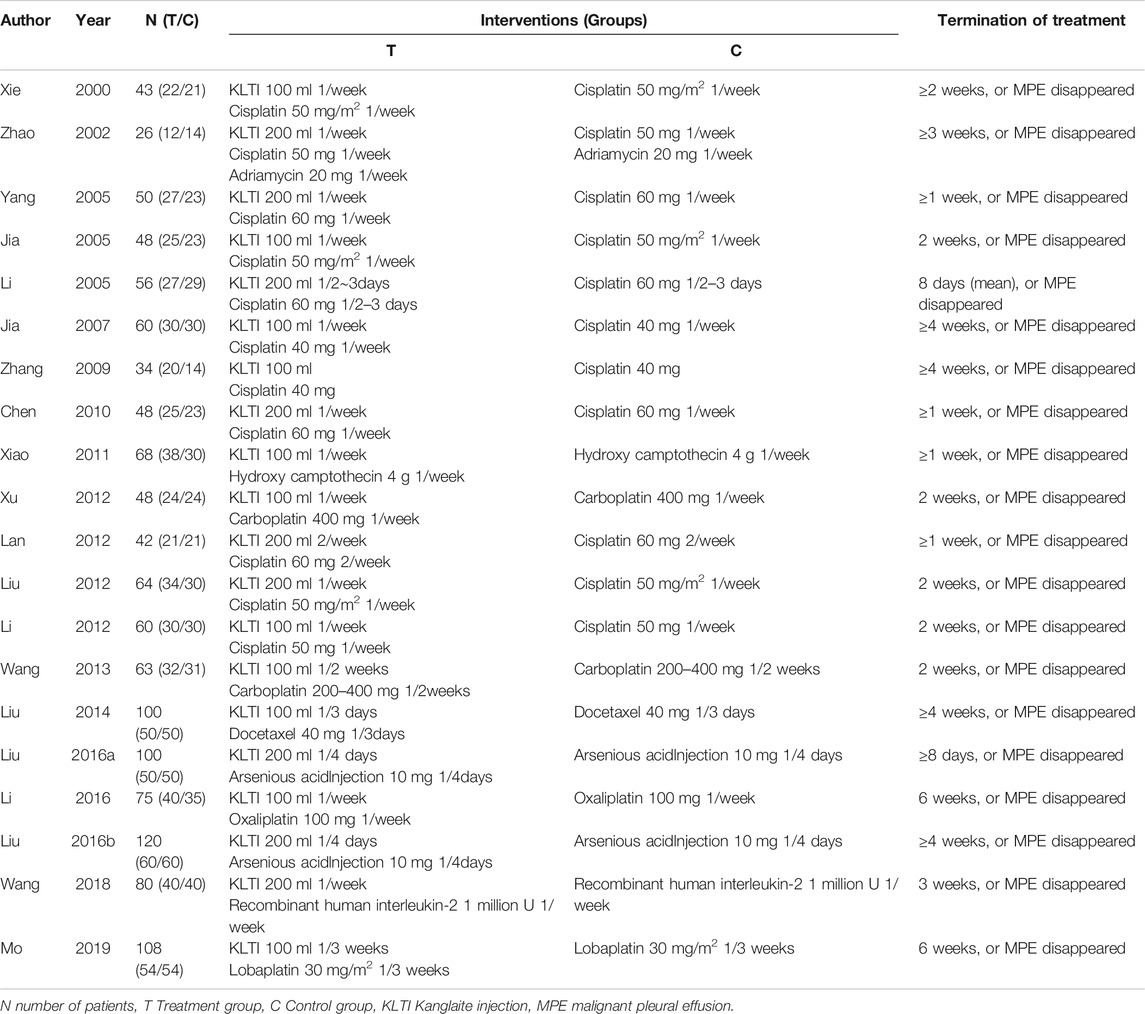
The Assessment of Heterogeneity
16 (Xie and Zhou, 2000; Zhao et al., 2002; Yang et al., 2005; Jia et al., 2005; Li and Cai, 2005; Jia et al., 2007; Chen et al., 2010; Xiao et al., 2011; Xu et al., 2012; Liu and Zhang, 2012; Li et al., 2012; Liu et al., 2014; Liu et al., 2016a; Li et al., 2016; Liu et al., 2016b; Mo et al., 2019) of the 20 studies only mentioned the word “random”, so their risk was rated as uncertain. Three studies (Lan et al., 2012; Wang et al., 2013; Wang et al., 2018) were assessed as low risk by using random number table method. One study (Zhang et al., 2009) was randomly assigned according to the time of the patient’s visit, and was assigned alternately, so it was rated as a high risk. No allocation concealment and blind methods were reported in all studies, so the risk was assessed as uncertain. No shedding cases were reported in all studies, and the observation indicators mentioned in the study program were reported in the results. The data of the results are complete and are not selectively reported, so the risk is classified as low. Due to the insufficient information in the literature, other bias risks are classified as uncertainty. (see Figure 2).
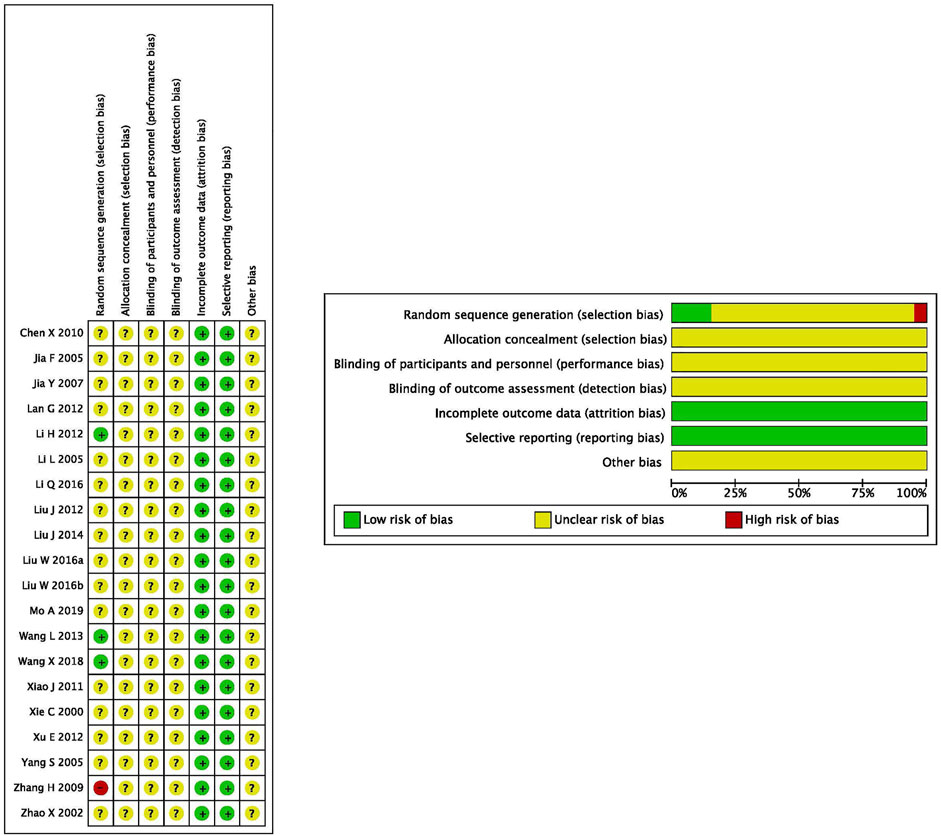
FIGURE 2. Quality evaluation of included studies: according to the criteria made by the Cochrane Handbook (Version 5.0.1), no heterogeneity existed in eligible RCTs; Overall, these studies had moderate to higher quality.
Primary Outcome
Comparison of Objective Remission Rate Between Traditional Chemotherapy Drugs Plus Kanglaite Injection Versus Traditional Chemotherapy Drugs Alone via Intrapleural Injection for Controlling Malignant Pleural Effusion
Of the 20 studies included, 19 RCTs (Xie and Zhou, 2000; Zhao et al., 2002; Yang et al., 2005; Jia et al., 2005; Li and Cai, 2005; Jia et al., 2007; Zhang et al., 2009; Chen et al., 2010; Xiao et al., 2011; Xu et al., 2012; Lan et al., 2012; Liu and Zhang, 2012; Li et al., 2012; Wang et al., 2013; Liu et al., 2014; Li et al., 2016; Liu et al., 2016b; Wang et al., 2018; Mo et al., 2019) reported ORR data that controlled MPE. The results showed that X2 was 3.00 (Degrees of freedom = 18; p = 1.000) and that the value of I2 (variation in RR attributable to heterogeneity) showed as 0.0%. The results showed that the RR was 1.23 (95%CI; 1.11–1.36, I2 = 0%, z = 3.876, p = 0.000), which showed that the ORR of traditional chemotherapeutic drugs plus KLTI was a little better than that treated with traditional chemotherapeutic drugs alone (see Figures 3A,B).
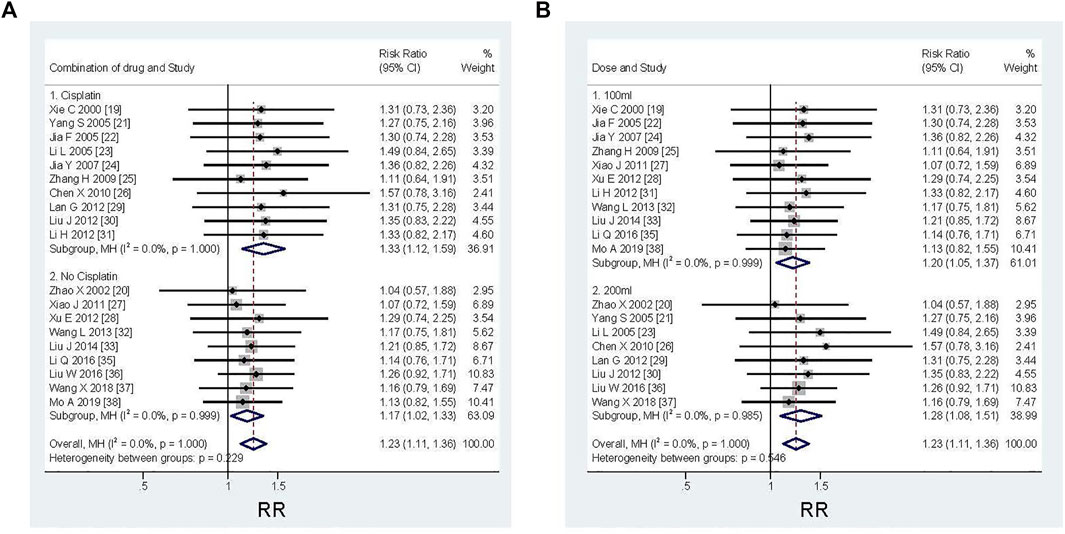
FIGURE 3. Efficacy comparison of KLTI combined with another agent versus another agent alone by thoracic perfusion for controlling MPE. Subgroup analysis of different types of chemotherapeutic drugs: when combined with cisplatin, the improvement of ORR is more advantageous; Subgroup analysis of different KLTI dosage: the ORR was more advantageous when using KLTI 200 ml each time. RR, Risk ratio; ORR, Objective response rate; KLTI, Kanglaite injection.
In order to explore the efficacy of KLTI combined with different types of chemotherapy drugs in the treatment of MPE, the subgroup analysis showed that ORR could be improved when KLTI combined with cisplatin or non-cisplatin. However, when combined with cisplatin, the improvement is more advantageous (cisplatin versus non-cisplatin: RR 1.33; 95%CI; 1.12–1.59, I2 = 0%, z = 3.26, p = 0.001 versus RR 1.17; 95%CI; 1.02–1.33, I2 = 0%, z = 2.33, p = 0.020) (see Figure 3A). According to the subgroup analysis of the dosage of KLTI, it was found that KLTI could both improve ORR, when using 100 ml or 200 ml. But it was more advantageous when using KLTI 200 ml each time (100 versus 200 ml: RR 1.20; 95%CI; 1.05–1.37, I2 = 0%, z = 2.64, p = 0.008 versus RR 1.28; 95%CI; 1.08–1.51, I2 = 0%, z = 2.89, p = 0.004) (see Figure 3B).
Secondary Outcome
Comparison of Quality of Life Between Traditional Chemotherapy Drugs Plus Kanglaite Injection Versus Traditional Chemotherapy Drugs Alone via Intrapleural Injection for Controlling Malignant Pleural Effusion
QOL improvement was evaluated by the patient’s KPS score. As shown in Table 1, a total of 7 RCTs (Zhang et al., 2009; Li et al., 2012; Wang et al., 2013; Liu et al., 2014; Liu et al., 2016a; Li et al., 2016; Wang et al., 2018) provided KPS data, comparing the QOL between conventional chemotherapy plus KLTI and conventional chemotherapy alone via intrathoracic injection for controlling MPE. After treatment, an increase in KPS score ≥10 was defined as QOL improvement. We found that the improvement rate in the KLTI combined perfusion group (190/262, 72.52%) was higher than that in the simple chemotherapy group (122/250, 48.80%). The heterogeneity analysis showed that X2 was 0.99 (Degrees of freedom = 6, p = 0.986), I2 = 0.0%. The results of meta-analysis showed that the combined RR was 1.28 (95%CI; 1.70–1.53, I2 = 0%, z = 2.70, p = 0.007), which indicated that intrapleural infusion of KLTI combined with chemical drugs could significantly improve the QOL of patients with MPE compared with chemical drugs alone (see Figure 4).
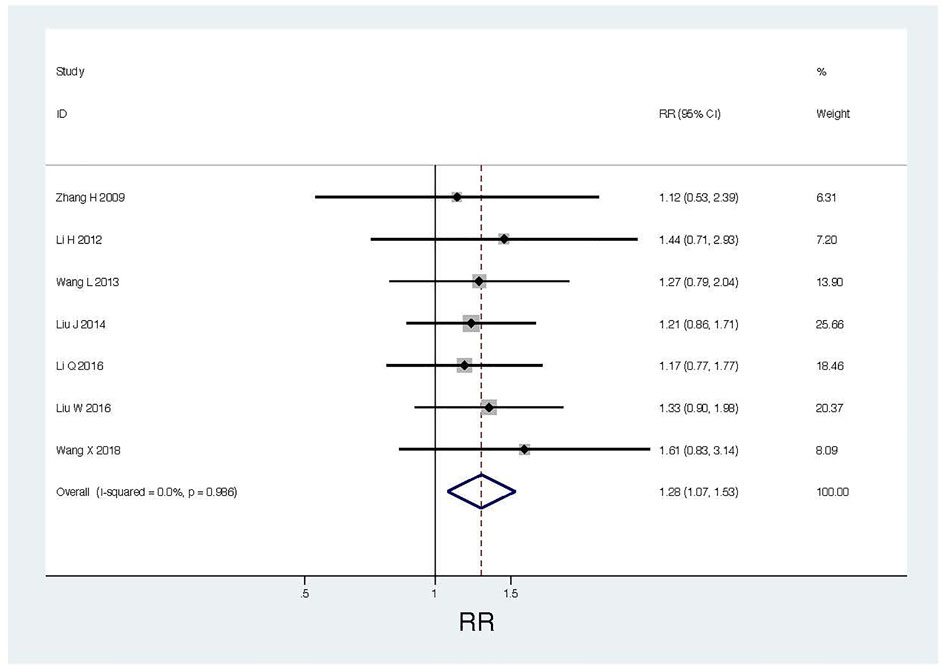
FIGURE 4. Thoracic perfusion of KLTI combined with other agents improved the QOL of patients with MPE compared with other agents alone. RR, Risk ratio; QOL, Quality of life; KLTI, Kanglaite injection.
Composition Ratio of Adverse Events on Traditional Chemotherapy Drugs Plus Kanglaite Injection Versus Traditional Chemotherapy Drugs Alone via Intrapleural Injection for Controlling Malignant Pleural Effusion
The AEs reported in 12 items of RCTs (Xie and Zhou, 2000; Jia et al., 2005; Li and Cai, 2005; Jia et al., 2007; Zhang et al., 2009; Chen et al., 2010; Xu et al., 2012; Liu et al., 2014; Li et al., 2016; Liu et al., 2016b; Wang et al., 2018; Mo et al., 2019) were gastrointestinal reactions (such as nausea or/and vomiting) (Combined group versus Single drug group: 132/417, 31.65% versus 179/401, 44.64%). 10 items of RCTs (Jia et al., 2005; Jia et al., 2007; Chen et al., 2010; Xu et al., 2012; Wang et al., 2013; Liu et al., 2014; Li et al., 2016; Liu et al., 2016b; Wang et al., 2018; Mo et al., 2019) reported myelosuppression (such as leukopenia, hemoglobin or/and thrombocytopenia) (68/380, 17.89% versus 78/373, 20.91%). Seven RCTs (Zhang et al., 2009; Chen et al., 2010; Xu et al., 2012; Li et al., 2016; Liu et al., 2016b; Wang et al., 2018; Mo et al., 2019) reported chest pain (68/263, 25.86% versus 72/248, 29.03%). Nine RCTs (Xie and Zhou, 2000; Jia et al., 2005; Jia et al., 2007; Zhang et al., 2009; Chen et al., 2010; Li et al., 2016; Liu et al., 2016b; Wang et al., 2018; Mo et al., 2019) reported fever (42/316, 13.29% vs 35/300, 11.67%). Four items of RCTs (Jia et al., 2007; Liu et al., 2016b; Li et al., 2016; Wang et al., 2018) reported renal damage (10/170, 5.88% vs 24/165, 14.55%) (see Table 3).
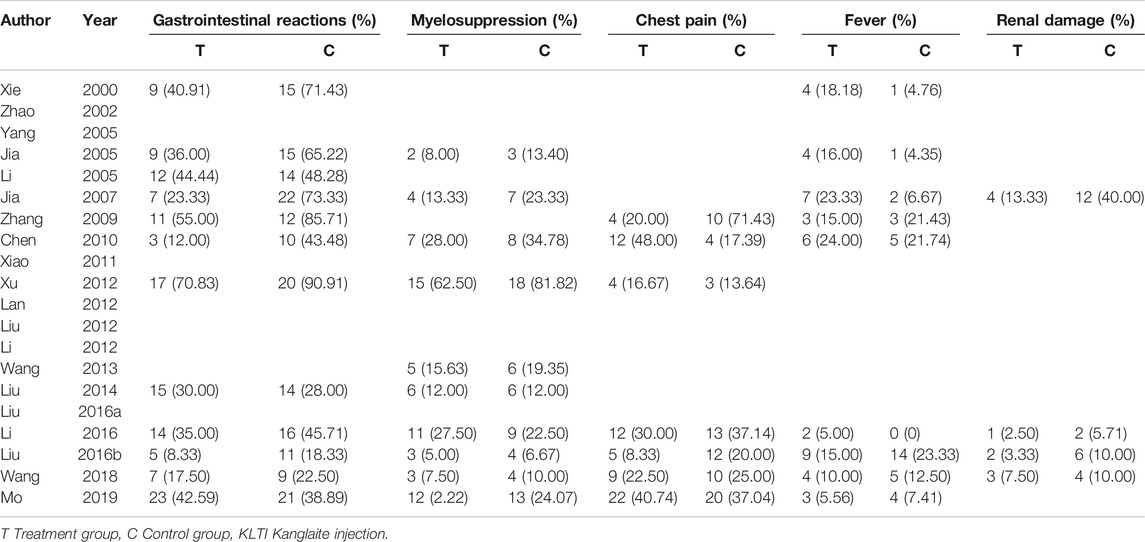
TABLE 3. Comparison of adverse events between KLTI combined with chemotherapeutic agents versus chemotherapeutic agents alone.
Comparison of Adverse Events Between Traditional Chemotherapy Drugs Plus Kanglaite Injection Versus Traditional Chemotherapy Drugs Alone via Intrapleural Injection for Controlling Malignant Pleural Effusion
Heterogeneity test found that I2 ≤ 50% and p ≥ 0.1, indicating that homogeneity is good. By comparing the results of AEs, it was found that the incidence of AEs in the treatment group was significantly lower than that in the control group (RR 0.84; 95%CI; 0.73–0.96, I2 = 0%, z = 2.64, p = 0.008). Among them, the incidence of gastrointestinal reactions (nausea or/and vomiting) in the treatment group was significantly lower than that in the control group (RR 0.79; 95% CI; 0.66–0.96; I2 = 0%, z = 2.37, p = 0.018). The incidence of renal damage in the treatment group was significantly lower than that in the control group (RR 0.468; 95% CI; 0.23–0.945, I2 = 0%, z = 2.11, p = 0.035).
In addition, there was no significant difference in the incidence of myelosuppression (RR 0.88; 95% CI; 0.66–1.17, I2 = 0%, z = 0.88, p = 0.377), chest pain (RR 0.91; 95% CI; 0.67–1.23, I2 = 22.8%, z = 0.63, p = 0.532) and fever (RR 1.047; 95% CI; 0.674–1.628, I2 = 0%, z = 0.20, p = 0.838) between the two groups (see Figure 5).
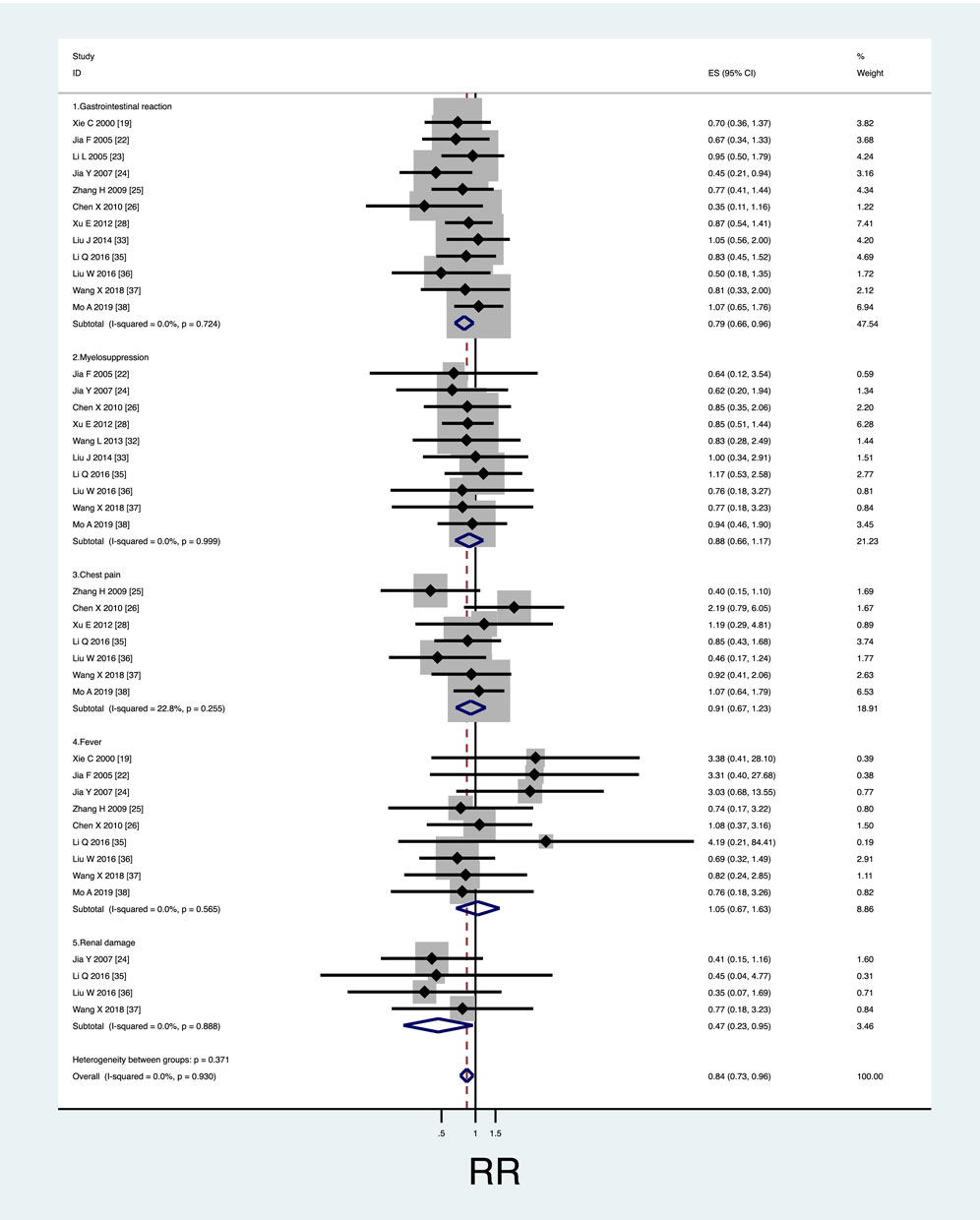
FIGURE 5. Safety evaluation of KLTI combined with another agent versus another agent alone by thoracic perfusion for controlling MPE. (A) The KLTI combination therapy displayed a lower incidence rate of gastrointestinal reactions than the project of other agents alone; (B) No difference in incidence rate of myelosuppression was testified between KLTI combined with other agents and other agents alone; (C) No difference in incidence rate of chest pain was testified between KLTI combined with other agents and other agents alone; (D) No difference in incidence rate of fever was testified between KLTI combined with other agents and other agents alone; (E) No difference in incidence rate of renal damage was testified between KLTI combined with other agents and other agents alone. RR, Risk ratio; KLTI, Kanglaite injection.
Assessment of Publication Bias
We drew a funnel chart and noticed that the included study was symmetrically distributed on both sides of the funnel chart (see Figures 6A–C), indicating that there was no significant publication bias in the meta-analysis.
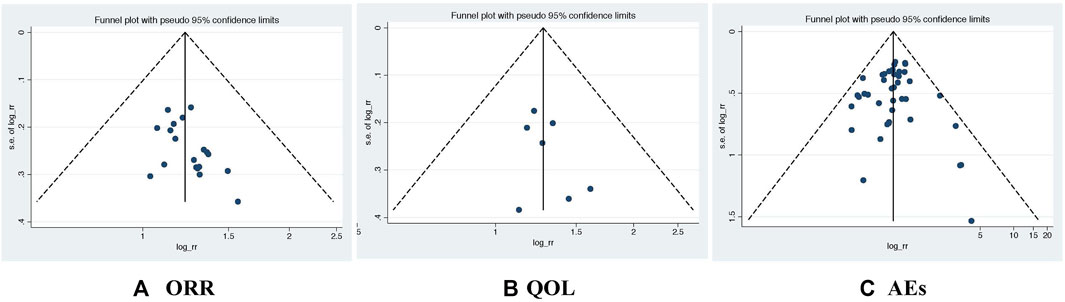
FIGURE 6. The shape of the funnelplot appeared to be approximately symmetrical. ORR, Objective response rate; QOL, Quality of life; AEs, Adverse events.
Discussion
KLTI is a kind of TCM preparation with bi-directional broad-spectrum anticancer effect, which is the extract of coix seed. Its main chemical component coixenolide has been proved to be an effective anticancer ingredient. Basic research found that KLTI can inhibit tumor cell proliferation and induce its apoptosis. Jiang Y et al. (Jiang et al., 2015) found that for A549 and H1975 NSCLC cell lines, KLTI mainly blocked cells in G2-M phase and combined with pemetrexed in S phase to enhance the cytotoxicity of chemotherapy. In addition, KLTI also plays a role in inhibiting cancer cell migration and intratumoral angiogenesis (Woo et al., 2007; Jiang and Fang, 2019). KLTI can regulate immune function. Pan et al. (Pan et al., 2012) found that KLTI can increase the level of serum IL-2 and stimulate T cell proliferation in Lewis lung cancer-bearing mice. In the study of Kunming lung cancer mice by Duan (Duan, 2018), it was found that compared with cisplatin alone, KLTI combined with cisplatin could significantly increase the spleen index and enhance the immune function of mice by reducing the level of TAM. A large number of clinical studies have shown that KLTI is effective in enhancing anti-tumor efficacy, improving patients’ quality of life and reducing adverse reactions (Huang et al., 2020; Li et al., 2020).
Through systematic search and screening, we finally included 20 items of RCTs for this meta-analysis to compare the efficacy and safety of KLTI combined with chemotherapy and chemotherapy alone in the treatment of MPE in the form of thoracic perfusion. Through statistical verification and combined with the clinical information of those studies, we found that those included RCTs have good homogeneity and comparability. This meta-analysis showed that compared with intrathoracic infusion of traditional chemotherapeutic drugs in the treatment of MPE, KLTI combined with chemotherapeutic drugs could benefit ORR (RR = 1.229, p = 0.000). The ORR of patients with MPE treated by intrapleural infusion of KLTI + chemotherapeutic drugs was 1.229 times higher than that of chemotherapeutic drugs alone. The results showed that KLTI played an important role in the thoracic perfusion treatment of MPE, indicating that KLTI could be used as an alternative drug to control MPE in clinical application. Network pharmacological study (Wang, 2019) showed that three main active components were screened from KLTI: triglyceride, coixenin and coixenolide. There are 25 potential anticancer targets of the three components, which can treat 22 kinds of cancer through different pathways. After KEGG analysis, 7 pathways were found to be closely related to the anticancer effect, mainly related to the regulation of cell proliferation, protein kinase B, cyclooxygenase pathway and so on. It can promote the secretion of TNF- α, inhibit the expression of COX-2 and regulate the activity of transcription factor FOX3a. Therefore, KLTI can control the tumor from multi-target and multi-angle.
With the emergence of anti-tumor measures, the survival time of tumor patients is longer than before, so the QOL of patients has been widely concerned by patients, society and doctors. Nowadays, more and more clinical studies use QOL improvement in patients to evaluate the effectiveness of treatment (Anota et al., 2015). According to this meta-analysis, it was found that the improvement of QOL in patients with MPE treated by intrathoracic infusion of KLTI combined with chemotherapeutic drugs was better than that of chemotherapy drugs alone (RR = 1.281, 0.007). The quality of life of patients with intrathoracic infusion of KLTI was 0.281 times higher than that of patients with intrapleural infusion of chemotherapeutic drugs. Previous studies have shown that coix seed can affect energy synthesis by regulating glucose and lipid metabolism, which may be the mechanism of improving the QOL of patients. Kim et al. (Kim et al., 2007) fed the obese rats with the water extract of Coix seed. It was found that the leptin level, fat content and body weight in the experimental group were lower than those in the control group. The expression of neuropeptide Y and leptin receptor was also decreased. The aqueous extract of Coix seed can control the energy balance by regulating the expression of neuropeptide Y and leptin receptor in hypothalamus. Chen et al. (Chen et al., 2019) isolated a water-soluble polysaccharide PAS from coix seed. After using it to treat type 2 diabetic mice, it was found that the content of insulin in mice increased. Oxidative stress and fat accumulation caused by hyperglycemia were also improved. In addition, the immune enhancement function of KLTI can also affect the QOL. Huang Ting et al. (Huang and Li, 2018) believed that KLTI could promote the activity and proliferation of NK cells, and not affect the immune function of normal mice, which may be related to PI3K/AKT pathway. However, it can enhance the immune function of mice at the cellular level and promote the ability of antibody production in mice (Zhou et al., 2018).
At present, chemotherapy is still one of the main anti-tumor measures. However, the adverse reactions caused by chemotherapeutic drugs, such as digestive tract reactions, myelosuppression and renal damage, affect patients’ tolerance to treatment, reduce patients’ quality of life, and may also lead to insufficient treatment cycle. it has become one of the important issues of clinicians. The results of meta-analysis showed that intrapleural infusion of KLTI could significantly reduce the incidence of chemotherapeutic drug-related adverse reactions (RR = 0.838, p = 0.008). In the study included in this meta-analysis, it was found that gastrointestinal reactions and myelosuppression were the most common adverse reactions. The results showed that intrathoracic infusion of KLTI could significantly reduce the incidence of digestive tract reactions (RR = 0.79, p = 0.018), and did not increase the incidence of myelosuppression (RR = 0.878, p = 0.377). In addition, intrathoracic infusion of KLTI reduced the incidence of renal damage (RR = 0.468, p = 0.035), but did not increase the burden of chest pain and fever (RR = 0.908, p = 0.532; RR = 1.047, p = 0.838). It is suggested that intrathoracic infusion of KLTI is safe in the treatment of MPE and can reduce the occurrence of some adverse reactions. Li et al. (Li et al., 2019) found that compared with other traditional Chinese medicine injections, there was no significant statistical difference in the effective rate of intrathoracic infusion of KLTI + cisplatin in the treatment of MPE. However, according to the probability ranking results, the incidence of nausea and vomiting in KLTI + cisplatin regimen was the lowest.
After the heterogeneity test of the results, it is found that the included studies have excellent homogeneity and comparability in the merger of the results. According to the symmetry of funnel chart, no obvious publication bias was found.
However, this meta-analysis still has some limitations:
①most of the samples included in the study are very small, which reduces the efficiency of the test.
②The blind method was not implemented in the study, and whether to implement distributive concealment was not described. The lax research process may exaggerate the efficacy.
③Because KLTI has been approved by China’s State Food and Drug Administration, most of the patients are from China, which may lead to geographical and ethnic differences.
④This study is designed for simple meta-analysis, not reticular meta-analysis, so there is no difference in efficacy between KLTI and other TCM injections.
⑤All the original literatures included were MPE caused by lung cancer. First, because MPE is most common in patients with lung cancer (Penz et al., 2017). In addition, KLTI was registered in China for use in lung and liver cancer. In the future, high-quality RCTs should be designed to evaluate the efficacy of KLTI in the treatment of MPE caused by other cancers. Nevertheless, our results provide an important recommendation that KLTI is effective and safe and can be used in combination with chemotherapeutic drugs for pleural perfusion in the treatment of MPE.
Conclusion
Compared with chemotherapy alone, intrathoracic infusion of KLTI + chemotherapy drugs can more effectively improve ORR of patients with MPE, and can also improve the QOL of patients. When combined with cisplatin and each use of KLTI 200ml, the effect is more significant. In addition, the participation of KLTI can also reduce the toxicity caused by chemotherapeutic drugs. However, a more rigorous RCT should be designed and completed before it is widely recommended.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
Conceptualization and study design: GZ, XW, JL, YZ, RG, XZ, BX, JH, MD, JC; Writing an original draft: GZ; Project administration: JL, YZ; Review and editing: XW, RG, XZ, BX, JH, MD, JC; Formal analysis: XW, RG; Supervision: JL, YZ; Investigation of data: BX, JH, MD, JC; and All authors read and approved the final manuscript.
Funding
National Key Research and Development Program of China, No.2018YFC1707405.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2021.694129/full#supplementary-material
Abbreviations
KLTI, Kanglaite injection; TCM, Traditional Chinese medicine; MPE, malignant pleural effusion; RCTs, Randomized controlled trials; ORR, Objective remission rate; QOL, quality of life; WHO, World Health Organization; RECIST, Response Evaluation Criteria in Solid Tumors; KPS, Karnofsky score; CR, complete response; PR, Partial response; SD, stable disease; PD, Progressive disease; AEs, Adverse events; RR, risk ratios; X2, Chi-square; I2, I-squared.
References
Anota, A., Hamidou, Z., Paget-Bailly, S., Chibaudel, B., Bascoul-Mollevi, C., Auquier, P., et al. (2015). Time to Health-Related Quality of Life Score Deterioration as a Modality of Longitudinal Analysis for Health-Related Quality of Life Studies in Oncology: Do We Need RECIST for Quality of Life to Achieve Standardization. Qual. Life Res. 24 (1), 5–18. doi:10.1007/s11136-013-0583-6
Biaoxue, R., Hui, P., Wenlong, G., and Shuanying, Y. (2016). Evaluation of Efficacy and Safety for Recombinant Human Adenovirus-P53 in the Control of the Malignant Pleural Effusions via Thoracic Perfusion. Sci. Rep. 6, 39355. doi:10.1038/srep39355
Chen, C., Ai, Q. D., and Wei, Y. H. (2021). Kanglaite Enhances the Efficacy of Cisplatin in Suppression of Hepatocellular Carcinoma via Inhibiting CKLF1 Mediated NF-Κb Pathway and Regulating Transporter Mediated Drug Efflux. J. Ethnopharmacol 264, 113388. doi:10.1016/j.jep.2020.113388
Chen, L. C., Jiang, B. K., Zheng, W. H., Zhang, S. Y., Li, J. J., and Fan, Z. Y. (2019). Preparation, Characterization and Anti-diabetic Activity of Polysaccharides from Adlay Seed. Int. J. Biol. Macromol 139, 605–613. doi:10.1016/j.ijbiomac.2019.08.018
Chen, X., He, M., and Zhu, H. (2010). Observation on the Efficacy of Cisplatin Combined with Kanglaite Injection in the Treatment of Malignant Pleural Effusion (In Chinese). Shandong Med. J. 50 (06), 71–72.
China Food and Drug Administration (2019). China Food and Drug Administration (CFDA). Available at: http://app1.sfda.gov.cn/datasearch/face3/base.jsp?tableId=25&tableName=TABLE25&title=%E5%9B%BD%E4%BA%A7%E8%8D%AF%E5%93%81&bcId=124356560303886909015737447882 (Accessed July 28, 2019).
Clinicaltrials.gov (2019). Kanglaite Injection Phase I Study. Available at: https://www.clinicaltrials.gov/ct2/show/NCT00031031?cond=Kanglaite+injection&rank=5 (Accessed July 28, 2019).
Duan, G. C. (2018). The Effects of Combination of Coix Seed Extract and Cisplatin on TAM and Expression of HIF-1α In Vivo in Lewis Lung Carcinoma. Iran J. Public Health 47 (6), 838–843.
Heffner, J. E., and Klein, J. S. (2008). Recent Advances in the Diagnosis and Management of Malignant Pleural Effusions. Mayo Clin. Proc. 83 (1), 235–250. doi:10.4065/83.2.235
Huang, T., and Li, X. Y. (2018). Study on the Effect of Kanglaite Injection on the Function of Human NK Cells (In Chinese). Jiangxi J. Traditional Chin. Med. 49 (4), 35–12.
Huang, X., Wang, J., Lin, W., Zhang, N., Du, J., Long, Z., et al. (2020). Kanglaite Injection Plus Platinum-Based Chemotherapy for Stage III/IV Non-small Cell Lung Cancer: A Meta-Analysis of 27 RCTs. Phytomedicine 67, 153154. doi:10.1016/j.phymed.2019.153154
Jia, F., Hou, M. Y., Hou, M. H., Liu, Y. J., Cao, C. J., and Li, T. S. (2005). Observation on the Efficacy of Kanglaite Combined with Cisplatin in the Treatment of Malignant Pleural Effusion (In Chinese). J. Mod. Oncol. 13 (02), 249–250. doi:10.3969/j.issn.1672-4992.2005.02.046
Jia, Y. J., Chen, L. W., Chen, J., and Sun, Y. Y. (2007). Clinical Observation of Pleural Injection of Kanglaite and Cisplatin Combined with Local Hyperthermia in the Treatment of Malignant Pleural Effusion (In Chinese). Liaoning J. Traditional Chin. Med. 34 (05), 607–608. doi:10.3969/j.issn.1000-1719.2007.05.039
Jiang, G. Q., and Fang, F. (2019). Effects of Erlotinib Combined with Kanglaite on Proliferation, Invasion and JAK2/STAT3 Signal Pathway of Lung Cancer Cell Line A549 (In Chinese). J. Zhengzhou University(Medical Sciences) 54 (3), 418–422.
Jiang, Y., Yuan, Q., Huang, A., and Fang, Q. (2015). The Synergistic Mechanism of Pemetrexed Followed by Kanglaite Was Due to KLT Subsequently Inhibiting the Pemetrexed-Activated MAPK Signaling Pathway. Clin. Lab. 61 (10), 1353–1363. doi:10.7754/clin.lab.2015.150134
Kim, S. O., Yun, S. J., and Lee, E. H. (2007). The Water Extract of Adlay Seed (Coix Lachrymajobi Var. Mayuen) Exhibits Anti-obesity Effects through Neuroendocrine Modulation. Am. J. Chin. Med. 35 (2), 297–308. doi:10.1142/S0192415X07004825
Lan, G. C., Su, Q. Y., Hong, R. L., and Li, Z. F. (2012). Intracavitary Injection of Kanglaite Combined with Cisplatin in the Treatment of Malignant Pleural Effusion (In Chinese). Mod. Traditional Chin. Med. 32 (5), 39–40.
Li, B., Yuan, Q. Z., Wang, Y., Shi, M. J., Ren, X., and Dong, Y. L. (2019). Reticular Meta-Analysis of 8 Kinds of Traditional Chinese Medicine Injection Combined with Cisplatin in the Treatment of Malignant Pleural Effusion (In Chinese). Chin. J. Hosp. Pharm. 39 (10), 1052–1057.
Li, H. H., Liu, L., Zhang, C., and Liu, H. (2012). Clinical Observation of Kanglaite in the Treatment of Malignant Pleural Effusion in Patients with Non-small Cell Lung Cancer (In Chinese). Guide China Med. 10 (21), 438–439.
Li, J., Li, H. Z., Zhu, G. H., Gao, R. K., Zhang, Y., Hou, W., et al. (2020). Efficacy and Safety of Kanglaite Injection Combined with First-Line Platinum-Based Chemotherapy in Patients with Advanced NSCLC: a Systematic Review and Meta-Analysis of 32 RCTs. Ann. Palliat. Med. 9 (4), 1518–1535. doi:10.21037/apm-20-616
Li, L., and Cai, H. (2005). Clinical Observation of 56 Cases of Malignant Pleural Effusion Treated with Kanglaite Combined with Microcatheter (In Chinese). Chin. Remedies Clin. 5 (5), 387–388.
Li, Q., Xiao, G. H., and Cheng, C. H. (2016). Pleural Infusion of Kanglaite Combined with Oxaliplatin in the Treatment of Malignant Pleural Effusion and its Effect on the Expression of RCAS1 and VEGF (In Chinese). J. Mod. Oncol. 24 (11), 1736–1739.
Lian, Z., Lu, Y., Hou, E., and Wang, X. (2006). Combination of GP Regimen and Kanglaite in the Treatment of Advanced Non-small Cell Lung Cancer. Zhongguo Fei Ai Za Zhi 9 (1), 74–77. doi:10.3779/j.issn.1009-3419.2006.01.19
Liu, J., Liu, X., Ma, J., Li, K., and Xu, C. (2019). The Clinical Efficacy and Safety of Kanglaite Adjuvant Therapy in the Treatment of Advanced Hepatocellular Carcinoma: A PRISMA-Compliant Meta-Analysis. Biosci. Rep. 39 (11), BSR20193319. doi:10.1042/BSR20193319
Liu, J., and Zhang, T. H. (2012). Clinical Observation and Nursing of Kanglaite Combined with Cisplatin Pleural Perfusion to Improve the Quality of Life of Patients with Malignant Pleural Effusion (In Chinese). Int. J. Nurs. 31 (9), 1758–1759.
Liu, J. T., Hao, Z. F., and Sun, S. G. (2014). Observation on the Efficacy of Docetaxel and Kanglaite Sequential Pleural Perfusion Combined with Hyperthermia in the Treatment of Malignant Pleural Effusion (In Chinese). Jilin Med. J. 35 (31), 6993–6995.
Liu, W., Zhang, Y. X., Kang, G. Q., Zhao, X. J., Li, Y., Feng, H. Y., et al. (2016b). Clinical Study of Pleural Injection of Kanglaite and Arsenite Combined with Hyperthermia in the Treatment of Malignant Pleural Effusion (In Chinese). J. Clin. Res. 33 (5), 967–969.
Liu, W., Zhang, Y. X., Kang, G. Q., Zhao, X. J., Li, Y., Feng, H. Y., et al. (2016a). Effect of Kanglaite on Quality of Life and Immune Function in Patients with Pleural Effusion of Lung Cancer (In Chinese). J. Clin. Res. 33 (3), 577–578.
Mo, A. W., Mai, Z. F., Wang, Y. Y., and Ji, X. Z. (2019). Clinical Study of Kanglaite Injection Combined with Carboplatin in the Treatment of Malignant Pleural Effusion in Patients with Non-small Cell Lung Cancer (In Chinese). Drugs & Clinic 34 (4), 1080–1083.
NCI Dictionary (2019). NCI Dictionary. Available at: https://www.cancer.gov/publications/dictionaries/cancer-drug/def/kanglaite (Accessed July 28, 2019).
Pan, P., Wu, Y., Guo, Z. Y., Wang, R., Wang, Y. J., and Yuan, Y. F. (2012). Antitumor Activity and Immunomodulatory Effects of the Intraperitoneal Administration of Kanglaite In Vivo in Lewis Lung Carcinoma. J. Ethnopharmacol 143 (2), 680–685. doi:10.1016/j.jep.2012.07.025
Penz, E., Watt, K. N., Hergott, C. A., Rahman, N. M., and Psallidas, I. (2017). Management of Malignant Pleural Effusion: Challenges and Solutions. Cancer Manag. Res. 9, 229–241. doi:10.2147/CMAR.S95663
Porcel, J. M., Gasol, A., Bielsa, S., Civit, C., Light, R. W., and Salud, A. (2015). Clinical Features and Survival of Lung Cancer Patients with Pleural Effusions. Respirology 20 (4), 654–659. doi:10.1111/resp.12496
Roberts, M. E., Neville, E., Berrisford, R. G., Antunes, G., and Ali, N. J. (2010). Management of a Malignant Pleural Effusion: British Thoracic Society Pleural Disease Guideline 2010. Thorax 65 (2), ii32–40. doi:10.1136/thx.2010.136994
Scherpereel, A., Astoul, P., Baas, P., Berghmans, T., Clayson, H., de Vuyst, P., et al. (2010). Guidelines of the European Respiratory Society and the European Society of Thoracic Surgeons for the Management of Malignant Pleural Mesothelioma. Eur. Respir. J. 35 (3), 479–495. doi:10.1183/09031936.00063109
Schwartzberg, L. S., Arena, F. P., Bienvenu, B. J., Kaplan, E. H., Camacho, L. H., Campos, L. T., et al. (2017). A Randomized, Open-Label, Safety and Exploratory Efficacy Study of Kanglaite Injection (KLTi) Plus Gemcitabine versus Gemcitabine in Patients with Advanced Pancreatic Cancer. J. Cancer 8 (10), 1872–1883. doi:10.7150/jca.15407
Wang, B. L. (2019). Study on Anti-tumor Mechanism of Three Main Components of Kanglaite Injection Based on Network Pharmacology (In Chinese). Chin. Mod. Appl. Pharm. 36 (01), 58–63.
Wang, K., Chen, Q., Shao, Y., Yin, S., Liu, C., Liu, Y., et al. (2021). Anticancer Activities of TCM and Their Active Components against Tumor Metastasis. Biomed. Pharmacother. 133, 111044. doi:10.1016/j.biopha.2020.111044
Wang, L. F., Huang, C. P., and Yu, Z. H. (2013). Observation on the Efficacy of Carboplatin Combined with Kanglaite Hyperthermic Perfusion Chemotherapy in the Treatment of Malignant Abdominal Pleural Effusion (In Chinese). Strait Pharm. J. 25 (03), 266–267.
Wang, X. M., Guo, S. J., and Zeng, C. S. (2018). Clinical Observation of Kanglaite Combined with Recombinant Human Interleukin-2 Infusion in the Treatment of Malignant Pleural Effusion (In Chinese). Med. Innovation China 15 (28), 22–25.
Woo, J. H., Li, D., Wilsbach, K., Orita, H., Coulter, J., Tully, E., et al. (2007). Coix Seed Extract, a Commonly Used Treatment for Cancer in China, Inhibits NFkappaB and Protein Kinase C Signaling. Cancer Biol. Ther. 6 (12), 2005–2011. doi:10.4161/cbt.6.12.5168
Xiao, J., Wang, Y. Z., Zhen, Y. J., and Lu, P. T. (2011). Efficacy and Mechanism of Coix Seed Injection Combined with Hydroxycamptothecin in the Treatment of Malignant Pleural Effusion in Elderly Patients with Advanced Non-small Cell Lung Cancer (In Chinese). Chin. J. Gerontol. 31 (21), 4092–4094.
Xie, C. Q., and Zhou, W. (2000). Combination of Cisplatin and Kanglaite in the Treatment of 43 Cases of Malignant Pleural Effusion (In Chinese). J. Pract. Oncol. 15 (2), 130–131.
Xu, E. Y., Jiang, B., and Wang, L. (2012). Clinical Observation of Kanglaite Combined with Carboplatin in the Treatment of Malignant Pleural Effusion in Patients with Advanced Lung Cancer (In Chinese). World Health Dig. 09 (26), 239.
Xu, W., Jiang, X., Xu, Z., Ye, T., and Shi, Q. (2016). The Efficacy of Brucea Javanica Oil Emulsion Injection as Adjunctive Therapy for Advanced Non-small-cell Lung Cancer: a Meta-Analysis. Evid. Based Complement. Alternat Med. 2016, 5928562. doi:10.1155/2016/5928562
Yang, C., Hou, A., Yu, C., Dai, L., Wang, W., Zhang, K., et al. (2018). Kanglaite Reverses Multidrug Resistance of HCC by Inducing Apoptosis and Cell Cycle Arrest via PI3K/AKT Pathway. Onco Targets Ther. 11, 983–996. doi:10.2147/OTT.S153814
Yang, S. F., Wu, X. L., Zhang, Y. P., and Tian, H. W. (2005). Clinical Observation of Kanglaite Combined with Cisplatin in the Treatment of Malignant Pleural Effusion (In Chinese). Pract. Oncol. J. 19 (04), 291–292. doi:10.3969/j.issn.1002-3070.2005.04.019
Zarogoulidis, K., Zarogoulidis, P., Darwiche, K., Tsakiridis, K., Machairiotis, N., Kougioumtzi, I., et al. (2013). Malignant Pleural Effusion and Algorithm Management. J. Thorac. Dis. 5 (4), S413–S419. doi:10.3978/j.issn.2072-1439.2013.09.04
Zhang, H., Wang, J. P., Feng, J. H., Sun, Z. T., and Li, Y. C. (2009). Study on the Efficacy and Safety of Kanglaite Combined with Cisplatin Pleural Perfusion in the Treatment of Malignant Pleural Effusion (In Chinese). Traditional Chin. Drug Res. Clin. Pharmacol. 20 (03), 278–280.
Zhang, Y., Lou, Y., Wang, J., Yu, C., and Shen, W. (2020). Research Status and Molecular Mechanism of the Traditional Chinese Medicine and Antitumor Therapy Combined Strategy Based on Tumor Microenvironment. Front. Immunol. 11, 609705. doi:10.3389/fimmu.2020.609705
Zhao, X. H., Zhao, X. H., Zhang, L., Cui, X. M., and Bai, X. (2002). Curative Effect Observation and Nursing of Treatment of Malignant Hy Drothorax with KLTI and ADM, DDP (In Chinese). Chin. J. Cancer Prev. Treat. 9 (06), 636–637. doi:10.3969/j.issn.1673-5269.2002.06.034
Keywords: kanglaite injection, malignant pleural effusion, pleural perfusion, chemotherapeutic drugs, meta-analysis
Citation: Zhu G, Wang X, Li J, Zhang Y, Gao R, Zhang X, Xu B, Hu J, Dai M and Chen J (2021) Evaluation of Efficacy and Safety for Kanglaite Injection in the Control of the Malignant Pleural Effusions via Thoracic Perfusion: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Pharmacol. 12:694129. doi: 10.3389/fphar.2021.694129
Received: 12 April 2021; Accepted: 19 October 2021;
Published: 03 November 2021.
Edited by:
Elaine Leung, Macau University of Science and Technology, Macau SAR, ChinaCopyright © 2021 Zhu, Wang, Li, Zhang, Gao, Zhang, Xu, Hu, Dai and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Li, cWZtMjAyMGppZWxpQHllYWgubmV0
†These authors have contributed equally to this work
 Guanghui Zhu
Guanghui Zhu Xinmiao Wang
Xinmiao Wang Jie Li1*
Jie Li1* Bowen Xu
Bowen Xu Jiaqi Hu
Jiaqi Hu