- Department of Oncology, Guang’anmen Hospital, China Academy of Chinese Medical Sciences, Beijing, China
Background: Depression is one of the common complications in patients with postoperative breast cancer (BC). Conventional therapies for postoperative depression of BC always have modest treatment outcomes and undesirable side effects. Clinical practice and many studies have shown that traditional Chinese medicine (TCM) has a good effect on postoperative depression of BC. This meta-analysis aimed to assess the clinical effect of TCM as an add-on treatment for postoperative depression of BC.
Methods: A systematic and thorough search was conducted on eight online electronic databases up to 20 July 2022. The control group received conventional therapies, and intervention groups received what control groups received plus TCM treatment. Review Manager 5.4.1 was used for statistical analysis.
Results: Nine RCTs involved 789 participants who met the inclusion standards. The results showed the intervention group was better at decreasing the score of the Hamilton rating scale for depression (HAMD) (mean difference, MD = −4.21, 95% CI −5.54 to −2.88) and the self-rating depression scale (SDS) (MD = −12.03, 95% CI −15.94 to −8.13), improving clinical efficacy (RR = 1.25, 95% CI 1.14–1.37), increasing the levels of 5-hydroxytryptamine (5-HT) (MD = 0.27, 95% CI 0.20–0.34), dopamine (DA) (MD = 26.28, 95% CI 24.18–28.77), and norepinephrine (NE) (MD = 11.05, 95% CI 8.07–14.04), and influencing the immune index, including the levels of CD3+ (MD = 15.18, 95% CI 13.61–16.75), CD4+ (MD = 8.37, 95% CI 6.00–10.74), and CD4+/CD8+ (MD = 0.33, 95% CI 0.27–0.39). The level of CD8+ (MD = −4.04, 95% CI −11.98 to 3.99) had no obvious difference between the two groups.
Conclusion: The meta-analysis stated that a therapeutic regimen involving TCM could better improve the depression status in postoperative BC.
Introduction
According to the global cancer statistics data in 2020, breast cancer (BC) has replaced lung cancer as the most common cancer globally, and its incidence and mortality are the first in female individuals (Sung et al., 2021). Currently, the primary treatment of BC is a comprehensive treatment based on surgery (Miller et al., 2009; Gradishar et al., 2022). Due to the absence of breasts, damaged appearance, and weakened femininity, BC patients will have a sense of shame, which increases the psychological burden of patients and is more likely to cause negative emotions of depression and pessimism after surgery (Xie and He, 2017). In addition, sexual dysfunction, side-effects of radiotherapy and chemotherapy, endocrine disorders, economic burden, and the disease itself will affect the mood of patients, leading to postoperative depression and even suicidal tendencies (Abdollahzadeh et al., 2014; Wang et al., 2015; Grusdat et al., 2022). Many studies have shown that patients suffering from BC have a significantly higher incidence of depression than other cancer populations (Shang et al., 2019; Padmalatha et al., 2021). A systematic review showed that the prevalence of long-term symptoms of depression after BC treatment ranged from 9.4% to 66.1%, and the overall percentage was 39.9% (Maass et al., 2015). There was a study report that the prevalence of depression after mastectomy in BC patients is 64% (Kamińska et al., 2015). An estimate of 51.4% of BC patients after mastectomy exhibited symptoms of depression in the first year (de Raaff et al., 2016).
Depression and these accompanying symptoms not only directly reduce the quality of life of patients but also negatively affect the immune function of patients (Abu-Helalah et al., 2014; Kim et al., 2018; Zhu et al., 2022). The immune system may also play a key role in the link between depression and cancer, although this relationship is currently unclear (Fraile-Martinez et al., 2022). In addition, patients with poor psychological status will decline treatment compliance and survival time (Kim et al., 2022). Current research showed that monoamine neurotransmitters, including 5-hydroxytryptamine (5-HT), dopamine (DA), and norepinephrine (NE), are decreased in patients with depression (Yang et al., 2020). Therefore, selective serotonin reuptake inhibitors, selective serotonin–norepinephrine reuptake inhibitors, and selective serotonin–norepinephrine dopamine reuptake inhibitors were commonly used in increasing the levels of 5-HT, DA, and NE to treat depression (Davies et al., 2019). However, conventional therapies for postoperative depression of BC always have modest treatment outcomes and are often accompanied by autonomic nervous system, gastrointestinal, and nervous system side effects (Carvalho et al., 2014; Tian et al., 2020). A growing body of research showed that the use of syndrome differentiation and treatment under the guidance of traditional Chinese medicine (TCM) theory has achieved good clinical efficacy in the postoperative depression of BC and can improve the depression status, increasing the levels of 5-HT, DA, and NE in the serum, and influence the immune index (Liu and Xiao, 2011; Xiong et al., 2021; Chen et al., 2022).
However, there is no systematic review of TCM efficacy in treating postoperative depression of BC. This study conducted a meta-analysis of the RCTs evaluating the clinical efficacy of TCM in the treatment of patients with postoperative depression of BC and synthesized evidence from the perspective of evidence-based medicine.
Methods
Search strategy
We searched the following databases comprehensively from the inception of databases to 20 July 2022: PubMed, Cochrane Library, Embase, Web of Science, China National Knowledge Infrastructure, Wanfang database, VIP database, and Chinese BioMedical Literature database. Medical subject headings (MeSH) terms and free text terms were used to obtain more comprehensive studies. The MeSH terms of “medicine, Chinese traditional,” “botanical drugs,” “breast neoplasms,” “postoperative period,” “depression,” and “depressive disorder” were used to construct search strategies. The search strategy of PubMed is shown in Supplementary Material S2.
Eligibility criteria
Inclusion criteria
1. Patients who were diagnosed with BC by histopathology and underwent surgical treatment; whether or not combined with other adjuvant therapy such as chemotherapy.
2. Only RCTs were included.
3. All patients included were diagnosed with depression diagnostic criteria, including Chinese Classification and Diagnostic Criteria for Mental Disorders Version 3 (CCMD-3); and Diagnostic and Statistical Manual of Mental Disorders, United States.
4. The control group received conventional therapies (e.g., chemoradiotherapy, endocrine therapy, antidepressant drugs, and psychological counseling), and intervention groups received what control groups received plus TCM treatment, including Chinese medicine decoction and Chinese patent medicine.
5. The outcomes included Hamilton’s depression scale (HAMD), depression self-rating score values (SDS), clinical efficacy, and levels of laboratory tests: 5-HT, DA, and NE in the serum, and immune function index (CD3+, CD4+, CD8+, and CD4+/CD8+).
Exclusion criteria
1. Repeated publication;
2. Outcome of interest not included;
3. Original data cannot be obtained by contacting the original author;
4. The language of publication was neither English nor Chinese.
Study selection and data extraction
EndNote 20 was used to manage the literature. Two researchers (YW and SYL) independently retrieved the titles and abstracts of all articles. Any disagreement in the screening process was consulted with another researcher (YZ) to make a decision. The relevant information was independently extracted and cross-checked by two researchers (YW and SYL) independently, which included: 1) basic information on the article: author’s name, year of publication, study type, and sample size; 2) patient characteristics: age, disease course, operation types, pathologic types, and stage; and 3) treatment outcomes: clinical intervention, intervention time, and outcomes. Disagreements were solved by discussion or consulting a third-party opinion (YZ), imputing a change-from-baseline standard deviation (SD) and mean using a correlation coefficient. A SD of the change from baseline for the experimental intervention was input using the following formula:
SD E, change = √[SD2 E, baseline + SD2 E, final - (2 × Corr × SD E, baseline × SD E, final)]; Corr = 0.75 (Zhang and Han, 2009).
The mean value of the change from baseline for the experimental intervention was input using the following formula:
Mean E, change = Mean E, final−Mean E, baseline (Higgins et al., 2022).
All data were rounded to two decimal places.
Outcomes of interest
The primary outcome of this study was depression status, evaluated with HAMD or SDS. HAMD was developed in 1960 and is the most commonly used scale in the clinical evaluation of depression. The SDS was developed in 1965, and it is one of the scales recommended by the United States Department of Education, Health, and Welfare for psychopharmacological research. The secondary outcomes included clinical efficacy, levels of laboratory tests (5-HT, DA, and NE) in the serum, and the immune function index of CD3+, CD4+, CD8+, and CD4+/CD8+. Clinical efficacy evaluation criteria: HAMD or SDS reduction rate = [(pre-treatment score−post-treatment score)/pre-treatment score × 100%]. The HAMD or SDS score reduction rate ≥ 75% was considered as recovery, 50% ∼ 74% as a significant improvement, 25% ∼ 49% as improvement, and <25% as no improvement. Clinical efficacy rate = (recovery + significant effect + improvement)/n × 100% (Zhang, 1998).
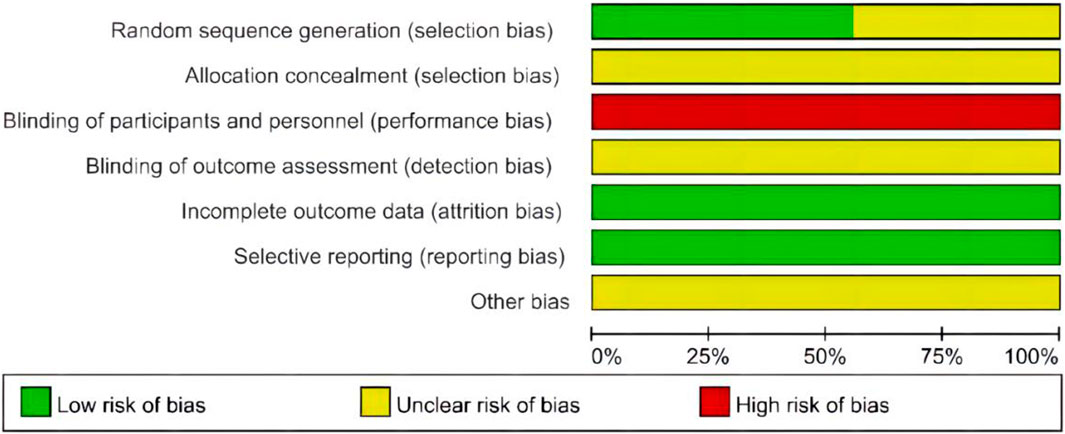
Quality assessment
Two researchers (YW and SYL) used the Cochrane Risk of Bias Tool (RoB) (Higgins et al., 2011) to evaluate the methodological quality of all included RCTs independently. The following seven domains were assessed: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. The included RCTs were assessed as low, uncertain, or high risk of bias. The results are shown in the RoB graph.
Statistical analysis
Review Manager software (version 5.4.1) was used to perform the meta-analysis. The random-effect model was used to synthesize evidence. Sensitivity or subgroup analysis was conducted to determine the cause of heterogeneity if it exists. The method of deleting studies one by one needed to be used to perform a sensitivity analysis of the results to ensure stability. The subgroup analysis of the meta-analysis results for each outcome was required. The subgroup only includes items related to the comparison. Subgroup analysis was performed based on whether to receive chemotherapy. For continuous variables, effect estimates were calculated as mean difference (MD); and for dichotomous variables, the risk ratio (RR) was calculated. The effect estimates with their 95% confidence intervals (CI) were presented in the forest plots. If meta-analysis was not suitable, descriptive analysis was performed. A funnel plot was used to analyze potential publication bias. p < 0.05 was considered statistically significant.
Results
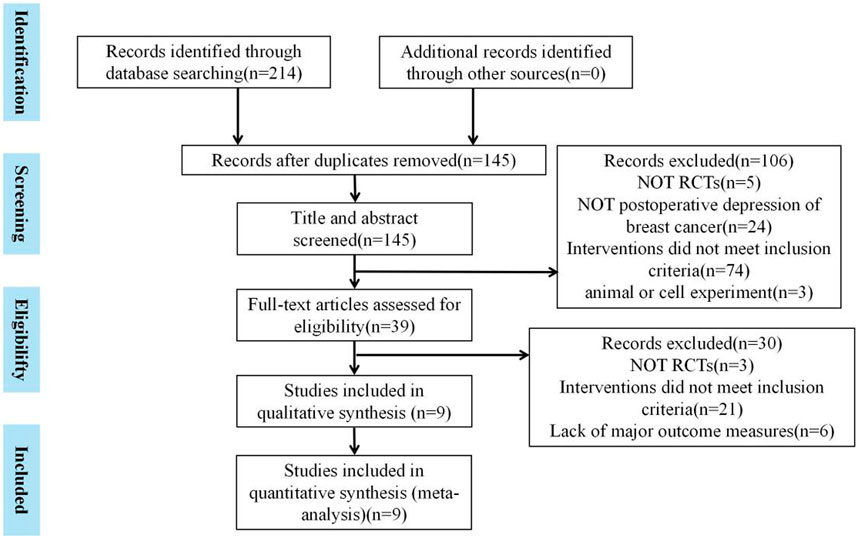
A total of 214 articles were obtained by searching the database. In total, 69 duplicate literature reports were found. After reading the title and abstract, 106 articles were excluded. Then, after strict literature screening and reading the full-text articles according to the inclusion and exclusion criteria, 30 articles were eliminated for the following reasons: 3 did not have RCTs, 21 did not meet the inclusion criteria, and 6 studies lacked outcome measures. Finally, a total of nine eligible trials were included. The specific retrieval process is shown in Figure 1.
Study characteristics
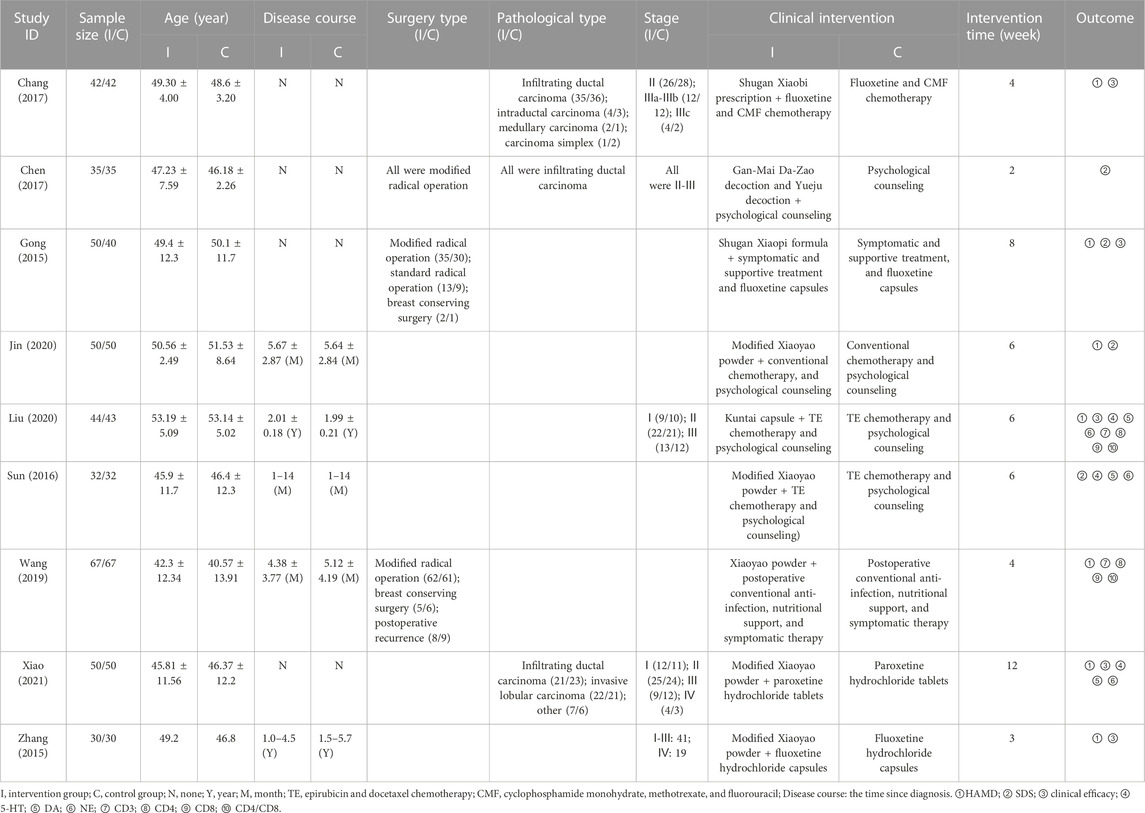
Nine RCTs were included with 789 participants that were divided into two groups; the control group received conventional therapies (n = 389), and intervention groups received what control groups received plus TCM treatment (n = 400) (Gong and Jiang, 2015; Zhang et al., 2015; Sun et al., 2016; Chang et al., 2017; Chen, 2017; Wang et al., 2019; Jin et al., 2020; Liu et al., 2020; Xiao, 2021). Study characteristics of included studies are shown in Table 1. Among participants, the average age of patients in the nine studies was between 45 and 54 years old, and the average course of disease ranged from 1 month to more than 5 years. Three studies mentioned the type of surgery (Gong and Jiang, 2015; Chen, 2017; Wang et al., 2019) and the pathological type (Chang et al., 2017; Chen, 2017; Xiao, 2021), but only one study showed that all patients included underwent modified radical operation and had infiltrating ductal carcinoma (Chen, 2017). Five studies involved the stage of disease [(Chang et al., 2017; Chen, 2017), (Liu et al., 2020), (Zhang, 1998; Higgins et al., 2011; Gong and Jiang, 2015; Sun et al., 2016; Chang et al., 2017; Chen, 2017; Wang et al., 2019; Jin et al., 2020; Liu et al., 2020; Xiao, 2021)], in which two RCTs indicated that all patients were in stage II–III (Chang et al., 2017; Chen, 2017). In clinical intervention, four studies mentioned combined chemotherapy (Sun et al., 2016; Chang et al., 2017; Jin et al., 2020; Liu et al., 2020), three studies combined psychological counseling (Chang et al., 2017; Jin et al., 2020; Liu et al., 2020), three studies combined fluoxetine hydrochloride capsules (Gong and Jiang, 2015; Zhang et al., 2015; Chang et al., 2017), and one study combined paroxetine capsules (Xiao, 2021) in two groups. TCM treatments included Xiaoyao powder/pill (Zhang et al., 2015; Sun et al., 2016; Wang et al., 2019; Jin et al., 2020; Xiao, 2021), Shugan Xiaopi formula (31), Shugan Xiaobi prescription (Chang et al., 2017), Kuntai capsule (Liu et al., 2020), Gan-Mai Da-Zao decoction, and Yueju pill (Chen, 2017). The composition and source of the formulations are described in detail in Supplementary Material S3.
Methodological quality of included studies
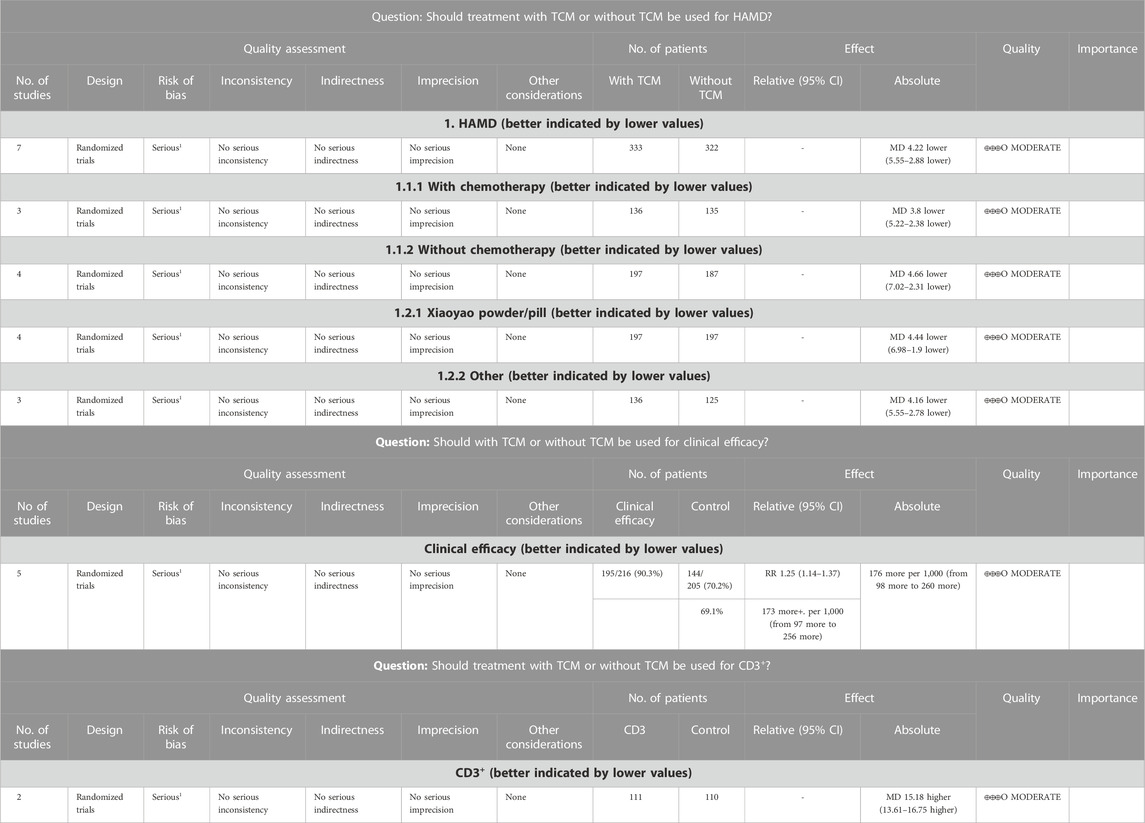
Five RCTs used the random number tables method and were assessed as low risk of random sequence generation (Sun et al., 2016; Chang et al., 2017; Wang et al., 2019; Liu et al., 2020; Xiao, 2021), and the other four RCTs did not elaborate on specific methods of randomization, and the risks were unclear (Gong and Jiang, 2015; Zhang et al., 2015; Chen, 2017; Jin et al., 2020). None of the included studies explicitly mentioned the use of allocation concealment and the blind method, which led to a high or unclear risk of bias in the relative domain. None of the nine studies had data missing or missing data that were comparable in each intervention group, and the reasons for missing data were similar, so they were rated as having a low risk of attrition bias. Nine studies were all at low risk of reporting bias (Figure 2). The GRADE method to rate the quality of evidence across studies was applied, and the quality of HAMD, clinical efficacy, and CD3+ was moderate. The quality of evidence of included studies is shown in Table 2.
Depression status
HAMD
A total of seven RCTs with 655 patients evaluated depression status with HAMD (Gong and Jiang, 2015; Zhang et al., 2015; Chang et al., 2017; Wang et al., 2019; Jin et al., 2020; Liu et al., 2020; Xiao, 2021). The meta-analysis showed that the effect of the intervention group was significantly better than that of the control group in reducing the HAMD score (MD = −4.21, 95% CI −5.54 to −2.88). Further subgroup analysis was conducted according to whether combined chemotherapy was used or not and whether Xiaoyao powder/pill or other traditional Chinese medicines were used. Subgroup analysis showed no statistical difference in whether chemotherapy (p = 0.54) and Xiaoyao Powder were used. (p = 0.85) In the sensitivity analysis, the results showed that one study was the main source of heterogeneity, which may be related to the fact that this RCT (Wang et al., 2019) only received postoperative anti-infective therapy and did not receive psychological treatment (including antidepressant therapy or psychological counseling). The forest plot is shown in Figure 3.
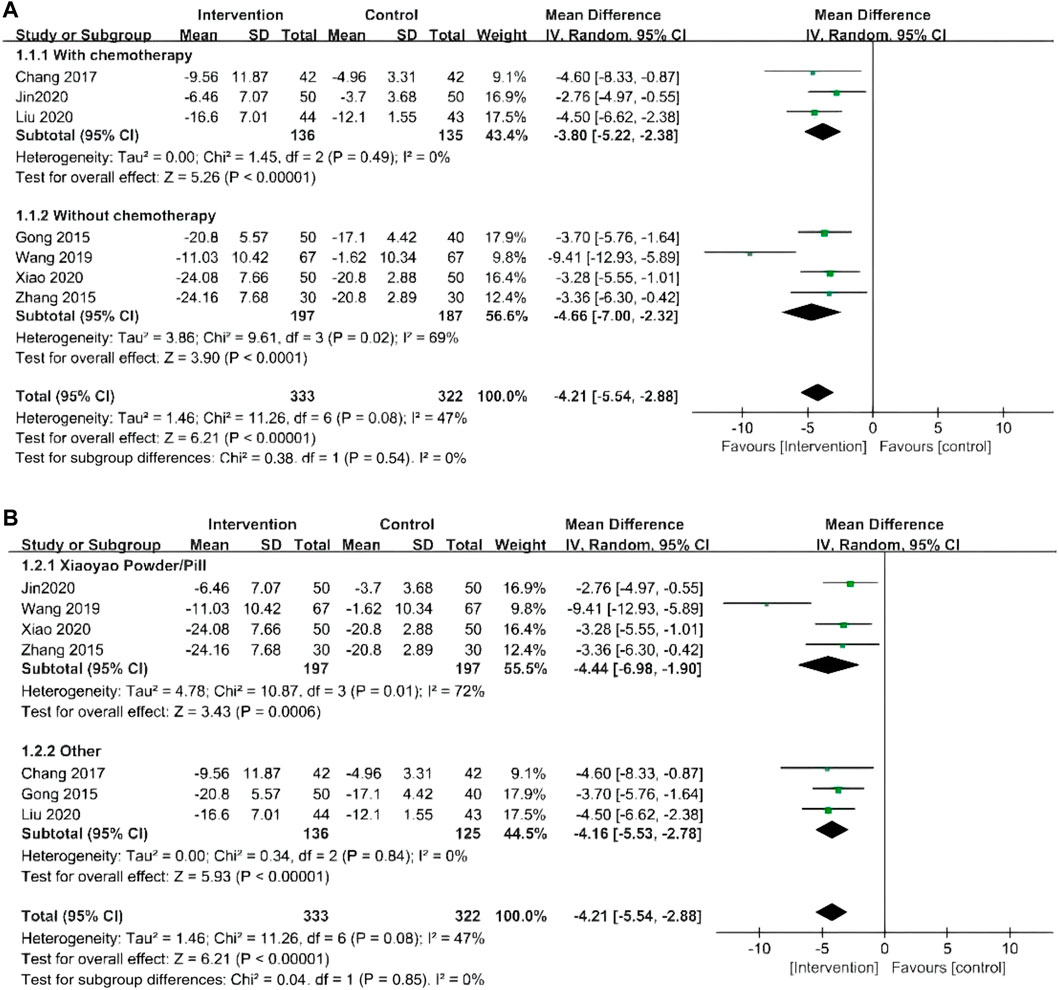
FIGURE 3. (A) Forest plots of HAMD by whether combined chemotherapy or not; (B) Forest plots of HAMD by whether to use Xiaoyao Powder/Pill or other traditional Chinese medicines.
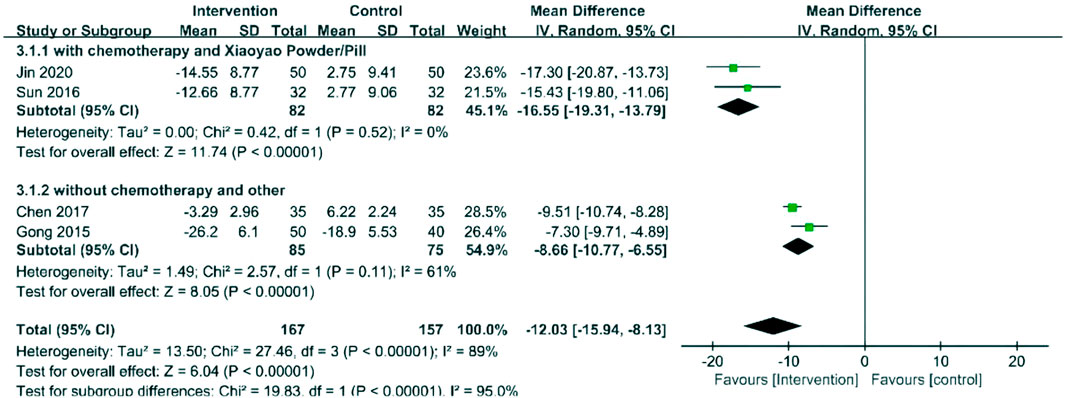
SDS
Four RCTs with 324 patients evaluated depression status with SDS (Gong and Jiang, 2015; Chen, 2017; Jin et al., 2020; Liu et al., 2020). The results showed that the intervention group had a more significant effect on decreasing the SDS score (MD = −12.03, 95% CI −15.94 to −8.13). Xiaoyao powder/pill was used in two studies that combined chemotherapy, and other traditional Chinese medicines were used in two studies without combined chemotherapy. Subgroup analysis was conducted according to whether chemotherapy was received and whether Xiaoyao powder/pill or other medicines were used. The result of the subgroup analysis suggested that the SDS score of patients treated with Xiaoyao powder/pill at the chemotherapy stage decreased more significantly than that of those treated with other traditional Chinese medicines at the non-chemotherapy stage (p < 0.00001). The forest plot is shown in Figure 4.
Clinical efficacy
Five RCTs reported clinical efficacy in outcome indicators (Gong and Jiang, 2015; Zhang et al., 2015; Chang et al., 2017; Liu et al., 2020; Xiao, 2021). The results showed that compared to the patients who received conventional therapies, those who received TCM plus conventional therapies have a significantly better clinical efficacy (RR = 1.25, 95% CI 1.14–1.37). The forest plot is shown in Figure 5.
Levels of laboratory tests
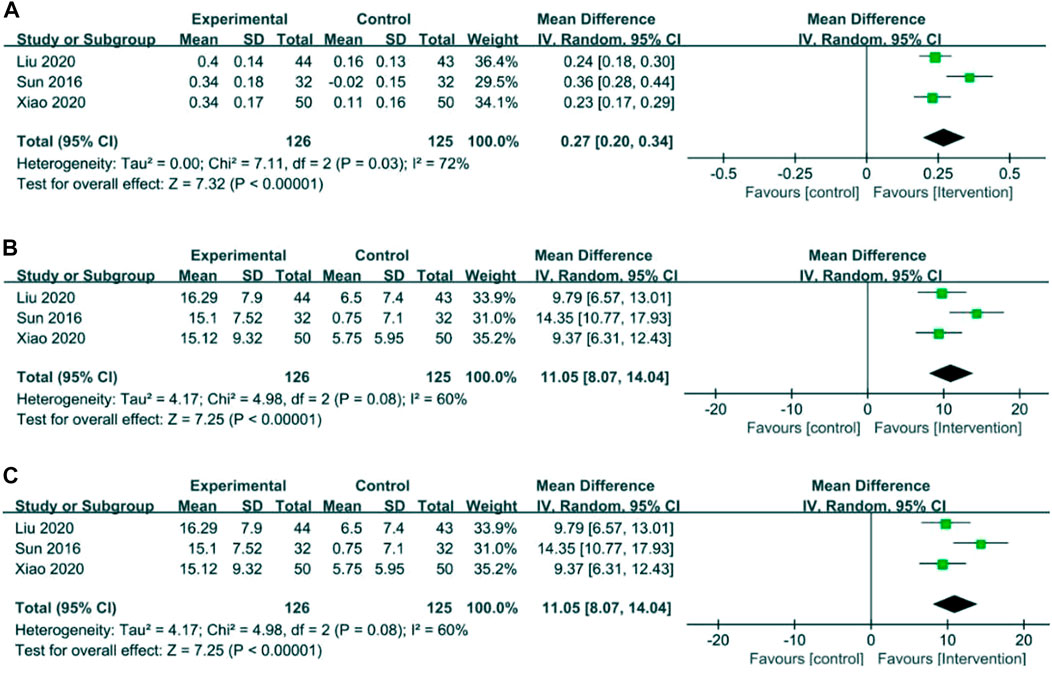
5-HT, DA, and NE
Three RCTs involving 126 cases in the intervention group and 125 cases in the control group reported 5-HT, DA, and NE in the outcome indicators (Sun et al., 2016; Xiao, 2021). Meta-analysis showed that compared to control groups, intervention groups were significantly better in increasing 5-HT (MD = 0.27, 95% CI 0.20–0.34), DA (MD = 26.48, 95% CI 24.18–28.77), and NE (MD = 11.05, 95% CI 8.07–14.04). The results are presented in Figure 6.
Immune function index
CD3+, CD4+, CD8+, and CD4+/CD8+
Two RCTs with 221 patients reported an immune function index (Wang et al., 2019; Liu et al., 2020). Meta-analysis showed that the intervention group was greatly improved compared with the control group in increasing CD3+ (MD = 15.18, 95% CI 13.61–16.75), CD4+ (MD = 8.37, 95% CI 6.00–10.74), and CD4+/CD8+ (MD = 0.33, 95% CI 0.27–0.39). The results showed that there was no statistical difference between the intervention group and the control group in CD8+ (MD = −4.00, 95% CI −11.98 to 3.99). The results are presented in Figure 7.
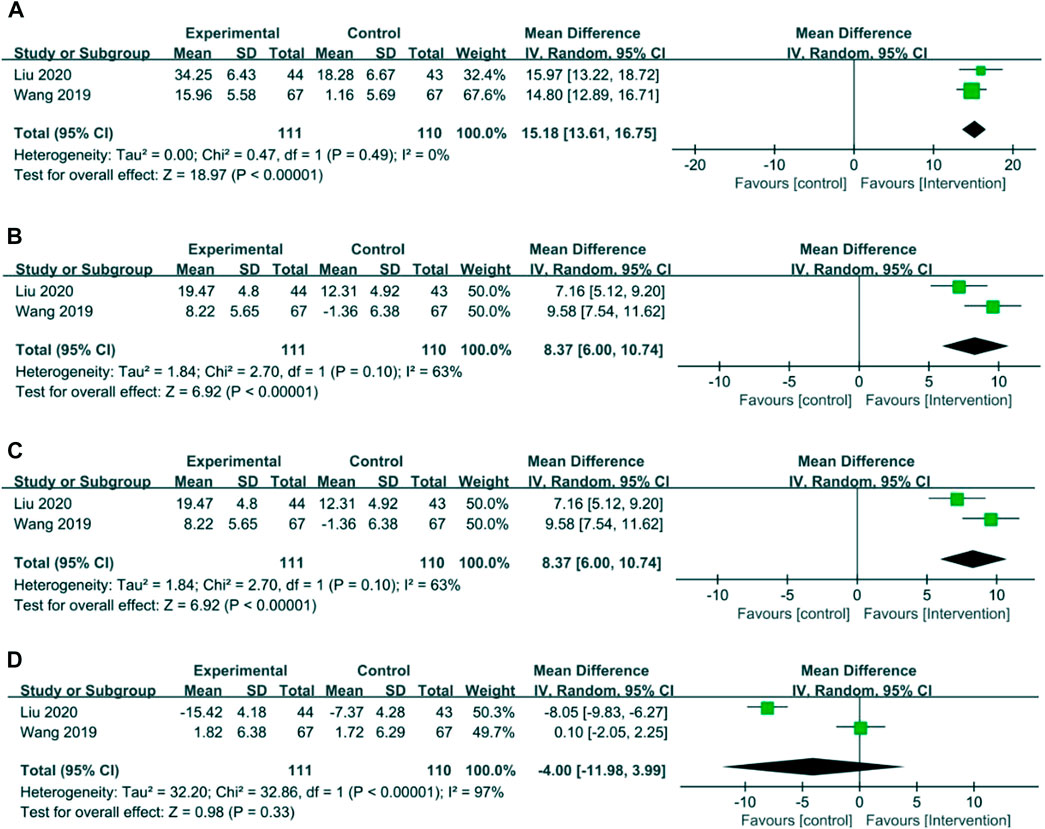
FIGURE 7. Forest plots of the immune function index. (A) CD3+, (B) CD4+, (C) CD4+/CD8+, and (D) CD8+.
Safety outcomes
A study showed that no adverse events, side effects, or TCM treatment-related toxic side effects were reported in the intervention group in the nine RCTs (Wang et al., 2019). Some RCTs showed that the incidence of adverse reactions such as nausea and vomiting, cardiotoxicity, liver and kidney function injury, bone marrow suppression, and alopecia in the intervention group was lower than that in the control group (Sun et al., 2016; Jin et al., 2020; Liu et al., 2020; Xiao, 2021). This indicates that TCM was safe for the treatment of postoperative depression of BC.
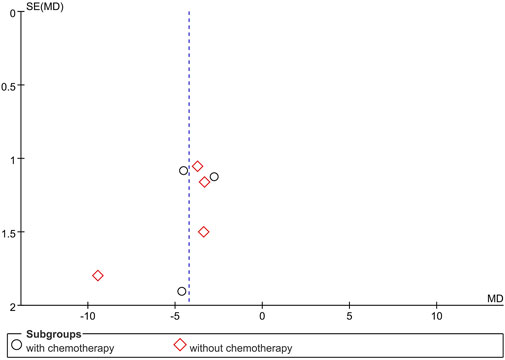
Publication bias
The funnel plot of the primary outcome (HAMD) showed no complete symmetry and indicated the existence of publication bias. The result is presented in Figure 8. Publication bias may be associated with negative results not being published.
Discussion
In this systematic review and meta-analysis of nine RCTs in the postoperative depression of BC, we have used the GRADE method to rate the quality of evidence across studies and have moderate certainty that application of TCM may lead to a better effect on improving the HAMD score. At the same time, the SDS score is reduced to some extent. It also increased the levels of 5-HT, DA, and NE in the serum and improved the immune index of CD3+, CD4+, and CD4+/CD8+.
The immune ability of the patients directly affects the development of tumors, and T lymphocytes play an indispensable role in the fight against tumors. CD4+ T lymphocytes can activate CD8+ T lymphocytes through a variety of pathways to kill tumor cells, and CD3+-induced lymphocyte proliferation plays a central role in the immune response cascade (McGregor et al., 2004; Yuan et al., 2023). One study showed that higher levels of CD3+, CD4+, and CD8+ were associated with longer survival (Castaneda et al., 2016).
The literature on the immune index and depression appears inconclusive. Most studies have indicated that CD3+ and CD4+ are negatively correlated with depression, and the increased CD3+ and CD4+ levels may improve the depression status of patients (Laumet et al., 2020; Lu et al., 2021). However, some studies have shown that the higher levels of CD4+ and CD8+ among active treatment BC patients may cause the poorer quality of life and sleep quality (Boivin et al., 2020). There was considerable controversy regarding the relationship between CD8+ and depression. Some studies have indicated that a higher CD8+ and CD4+/CD8+ ratio in people with depression may lead to worse depressive symptoms (Zorrilla et al., 2001; Boivin et al., 2020). However, another research has shown that the CD4+/CD8+ ratio was negatively associated with depression (Laumet et al., 2020). The relationship between the immune index and depression may weaken after treatment and may relate to the type of depression (Yang Shengliang et al., 2021; Lu et al., 2021). Although the relationship between the CD+ marker and depression is still controversial, it can be concluded in this meta-analysis that TCM can significantly reduce the depression status of patients. Current antidepressants that are used in Western medicine usually have a single pathway of action, significant side effects, and modest curative effects. However, TCM has the characteristics of multiple targets, high safety, and good clinical efficacy, which may offer new options for the treatment of cancer-related depression (Lin et al., 2017).
In this meta-analysis, there was no significant difference in HAMD scores between the two groups reported by two RCTs, but significant differences were observed in SDS scores in the same RCTs (Gong and Jiang, 2015; Jin et al., 2020). There are possible reasons for this result: HAMD score is a professional tool for doctors to assess the degree of depression and objectively evaluate the overall condition of patients through other rating methods. In the SDS score, patients were scored according to the frequency and degree of their symptoms to avoid evaluation errors caused by unclear expression, and the score can reflect the severity of symptoms. Some of the negative feelings were also evident in normal people in times of adversity, which may lead to SDS scores higher than in the normal population. Both of them could reflect the severity of depression from subjective and objective perspectives, respectively. HAMD is more accurate than SDS in distinguishing the severity of depression. Some studies showed there were significant differences in SDS and HAMD scores between different severity depression groups, and the consistency between the severity of symptoms derived from SDS and the severity level derived from the existing severity classification criteria is not high. The evaluation value of the HAMD score is generally higher than that of SDS (Liu Baoyan et al., 2021). Another study showed that the SDS grade was not consistent with the severity of symptoms obtained by HAMD. The sensitivity and specificity of SDS were not satisfactory. Therefore, the depression scale should be used rationally in clinical practice to enhance the accuracy of evaluation (Duan and Sheng, 2012).
It is believed that the pathogenesis of depression is related to the hypothalamic–pituitary–adrenal (HPA) axis, the gut–brain–microbiome axis, brain-derived neurotrophic factor (BDNF), monoamine neurotransmitters, and cytokines (Kubera et al., 2011; Dooley et al., 2016; Zhao J. et al., 2022; Flores et al., 2022; Maybee et al., 2022). Studies have shown that Gan-Mai Da-Zao decoction can increase the content of monoamine neurotransmitters in patients with depression, regulate the function of the monoamine system, reduce central and peripheral pro-inflammatory factors, and inhibit HPA axis hyperactivity. It can increase the mRNA and protein expression of BDNF, thereby exerting the clinical effect of antidepressants (Yang Xuejing et al., 2021). Xiaoyao power can also improve gastrointestinal function and depression by affecting the gut–brain–microbiome axis and the neuro–endocrine–immune axis (RenQi et al., 2021; Zhao D. et al., 2022). The present study suggests that albiflorin and paeoniflorin may treat cancer-related depression by modulating the neuroendocrine-immune networks and aberrant metabolic pathways (Wang et al., 2021). TCM may increase the content of 5-HT, DA, and NE in blood and affect immunity through the aforementioned ways to play an anti-depressant effect.
At present, there are few relevant clinical studies and a lack of data on the treatment of depression after BC surgery with TCM, almost no double-blinded studies, and the literature quality is poor. More high-quality RCTs should be conducted in the future. Most of the nine RCTs in this meta-analysis were treated with TCM combined with chemotherapy. More RCTs can be conducted on postoperative depression of BC after chemoradiotherapy or without chemoradiotherapy to avoid distractions from other treatments. Most of the original studies included in this meta-analysis did not mention the surgical method and clinical stage of the included patients, although some studies showed that there was no significant relationship between the surgical method and clinical stage in the postoperative depression of BC (Xu et al., 2015) which needed more studies to verify this conclusion in the future.
Studies have shown that psychosocial factors are closely related to the incidence of BC-related depression. Depression is one of the adverse factors in the recurrence and unfavorable evolution of BC (Wang et al., 2020; Schenker et al., 2022; Xu et al., 2022). The incidence of postoperative depression in BC is closely related to physiology, society, and psychology. The contemporary medical model has gradually changed to the bio–psycho–social medical model. TCM maintains physical and mental health through the combination of psychological intervention, emotional adjustment, and TCM treatment, showing the advantages of TCM clinical treatment and providing patients with more reasonable and efficient treatment plans (Liu Xue et al., 2021). However, most of the clinical studies on the treatment of postoperative depression of BC have no quality control and chemical report in the treatments. This is a shortcoming of this article and a limitation of current common assessment tools in TCM. TCM plays an increasingly important role in treating postoperative depression of BC. Therefore, it is necessary to increase further the exploration and conduct more high-quality research on depression after BC surgery with TCM to better apply it in clinical practice.
Conclusion
Overall, TCM can be an add-on therapy for postoperative depression of BC for improving symptoms of depression, increasing the 5-HT, DA, and NE levels in the blood, and raising the immune index of patients with a significant and safe effect. More randomized clinical trials and extended follow-ups are needed to evaluate the effect of TCM on postoperative depression of BC.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author.
Author contributions
YZ, as the corresponding author, designed the study. YW and SYL wrote the first draft and were responsible for the literature searching, carrying out data extraction and conducting the quality assessment. YW and SYL contributed equally to this work and share first authorship. YX and SHY provided statistical support for the meta-analysis. GHZ, HPW, and BWX played an important role in the process of revising. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by National Traditional Chinese Medicine Inheritance and Innovation team sub-project-the clinical study on the intervention of Brucea javanica oil Emulsion Injection on survival of advanced colon cancer patients who failed multi-line treatment (No: ZYYCXTD-C-202205) and the China Evidence-based Medicine Center of Traditional Chinese Medicine “Director Special of Business Research Office”. Project Name: Integration innovation and application of traditional Chinese medicine trial and real-world data research under the environment of integrated traditional Chinese and western medicine (No: 2020YSJZX-3).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1019049/full#supplementary-material
References
Abdollahzadeh, F., Moradi, N., Pakpour, V., Rahmani, A., Zamanzadeh, V., Mohammadpoorasl, A., et al. (2014). Un-met supportive care needs of Iranian breast cancer patients. Asian Pac J. Cancer Prev. 15 (9), 3933–3938. doi:10.7314/apjcp.2014.15.9.3933
Abu-Helalah, M., Al-Hanaqta, M., Alshraideh, H., Abdulbaqi, N., and Hijazeen, J. (2014). Quality of life and psychological well-being of breast cancer survivors in Jordan. Asian Pac. J. Cancer Prev. 15 (14), 5927–5936. doi:10.7314/apjcp.2014.15.14.5927
Boivin, M. J., Aaron, G. P., Felt, N. G., and Shamoun, L. (2020). Preliminary study on the effects of treatment for breast cancer: Immunological markers as they relate to quality of life and neuropsychological performance. BMC Womens Health 20 (1), 109. doi:10.1186/s12905-020-00971-1
Carvalho, A. F., Hyphantis, T., Sales, P. M., Soeiro-de-Souza, M. G., Macêdo, D. S., Cha, D. S., et al. (2014). Major depressive disorder in breast cancer: A critical systematic review of pharmacological and psychotherapeutic clinical trials. Cancer Treat. Rev. 40 (3), 349–355. doi:10.1016/j.ctrv.2013.09.009
Castaneda, C. A., Mittendorf, E., Casavilca, S., Wu, Y., Castillo, M., Arboleda, P., et al. (2016). Tumor infiltrating lymphocytes in triple negative breast cancer receiving neoadjuvant chemotherapy. World J. Clin. Oncol. 7 (5), 387–394. doi:10.5306/wjco.v7.i5.387
Chang, Jiye, Wang, Ting, and Zhang, Weidong, (2017). Liver disappear bi party combined fluoxetine treatment the curative effect of breast cancer to merge depression. Int. J. Psychiatry 44 (01), 116–118. doi:10.13479/j.carol.carroll.nki.jip.2017.01.029
Chen, Guifen (2017). Effect of Ganmai Dazao decoction and Yueju decoction on depression state and quality of life after mastectomy. Strait Pharm. 29 (11), 107–109. doi:10.3969/j.issn.1006-3765.2017.11.044
Chen, J., Lei, C., Li, X., Wu, Q., Liu, C., Ma, Q., et al. (2022). Research progress on classical traditional Chinese medicine formula xiaoyaosan in the treatment of depression. Front. Pharmacol. 13, 925514. doi:10.3389/fphar.2022.925514
Davies, P., Ijaz, S., Williams, C. J., Kessler, D., Lewis, G., and Wiles, N. (2019). Pharmacological interventions for treatment-resistant depression in adults. Cochrane Database Syst. Rev. 12 (12), CD010557. doi:10.1002/14651858.CD010557.pub2
de Raaff, C. A., Derks, E. A., Torensma, B., Honig, A., and Vrouenraets, B. C. (2016). Breast reconstruction after mastectomy: Does it decrease depression at the long-term? Gland. Surg. 5 (4), 377–384. doi:10.21037/gs.2016.05.02
Dooley, L. N., Ganz, P. A., Cole, S. W., Crespi, C. M., and Bower, J. E. (2016). Val66Met BDNF polymorphism as a vulnerability factor for inflammation-associated depressive symptoms in women with breast cancer. J. Affect Disord. 197, 43–50. doi:10.1016/j.jad.2016.02.059
Duan, Q., and Sheng, L. (2012). Clinical validity of self-rating Anxiety and Depression scales. Chin. J. Ment. Health 26, 676–679.
Flores, A. D., Yu, W. S., Fung, M. L., and Lim, L. W. (2022). Neuromodulation and hippocampal neurogenesis in depression: A scoping review. Brain Res. Bull. 188, 92–107. doi:10.1016/j.brainresbull.2022.07.009
Fraile-Martinez, O., Alvarez-Mon, M. A., Garcia-Montero, C., Pekarek, L., Guijarro, L. G., Lahera, G., et al. (2022). Understanding the basis of major depressive disorder in oncological patients: Biological links, clinical management, challenges, and lifestyle medicine. Front. Oncol. 12, 956923. doi:10.3389/fonc.2022.956923
Gong, P., and Jiang, G. (2015). Effect of integrated traditional Chinese and Western medicine therapy on anxiety, depression and quality of life after breast cancer surgery. New Tradit. Chin. Med. 47 (2), 178–180. doi:10.13457/j.carol.carroll.nki.JNCM.2015.02.084
Gradishar, W. J., Moran, M. S., Abraham, J., Aft, R., Agnese, D., Allison, K. H., et al. (2022). Breast cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Canc Netw. 20 (6), 691–722. doi:10.6004/jnccn.2022.0030
Grusdat, N. P., Stäuber, A., Tolkmitt, M., Schnabel, J., Schubotz, B., Wright, P. R., et al. (2022). Routine cancer treatments and their impact on physical function, symptoms of cancer-related fatigue, anxiety, and depression. Support Care Cancer 30 (5), 3733–3744. doi:10.1007/s00520-021-06787-5
Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343, d5928. doi:10.1136/bmj.d5928
Higgins, J., and James, T., (2022). Cochrane handbook for systematic reviews of interventions. https://training.cochrane.org/handbook/current/chapter-06.
Jin, Y., Zheng, C., Liu, L., et al. (2020). Effect of modified Xiaoyao SAN on depression syndrome of liver stagnation and spleen deficiency in patients with breast cancer undergoing chemotherapy and its influence on SDS and HAMD scores. Maternal Child World (34), 116.
Kamińska, M., Kubiatowski, T., Ciszewski, T., Czarnocki, K. J., Makara-Studzińska, M., Bojar, I., et al. (2015). Evaluation of symptoms of anxiety and depression in women with breast cancer after breast amputation or conservation treated with adjuvant chemotherapy. Ann. Agric. Environ. Med. 22 (1), 185–189. doi:10.5604/12321966.1141392
Kim, S. H., Choe, Y. H., Cho, Y. U., Park, S., and Lee, M. H. (2022). Effects of a partnership-based, needs-tailored self-management support intervention for post-treatment breast cancer survivors: A randomized controlled trial. Psychooncology 31 (3), 460–469. doi:10.1002/pon.5828
Kim, S. Y., Kim, S. W., Shin, I. S., Park, M. H., Yoon, J. H., Yoon, J. S., et al. (2018). Changes in depression status during the year after breast cancer surgery and impact on quality of life and functioning. Gen. Hosp. Psychiatry 50, 33–37. doi:10.1016/j.genhosppsych.2017.09.009
Kubera, M., Obuchowicz, E., Goehler, L., Brzeszcz, J., and Maes, M. (2011). In animal models, psychosocial stress-induced (neuro)inflammation, apoptosis and reduced neurogenesis are associated to the onset of depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 35 (3), 744–759. doi:10.1016/j.pnpbp.2010.08.026
Laumet, G., Edralin, J. D., Dantzer, R., Heijnen, C. J., and Kavelaars, A. (2020). CD3+ T cells are critical for the resolution of comorbid inflammatory pain and depression-like behavior. Neurobiol. Pain 7, 100043. doi:10.1016/j.ynpai.2020.100043
Lin, Y., Wu, S., and Zhengzheng, X., (2017). Effects of modified Xiaoyao SAN on the expression of brain-gut peptide SS and GAS in depressed rats with gastrointestinal dysfunction. Shizhen Natl. Med. 28 (6), 1290–1292.
Liu, B., Jin, Z., and Zheng, D. (2021a). Study on accuracy of distinguishing the severity of depression between HAMD and SDS. Chongqing Med. 50 (18), 3174–3177. doi:10.3969/j.issn.1671-8348.2021.18.025
Liu, H., Fan, Y., and Guo, Q., (2020). Effects of Kuntai capsule on anxiety, depression and immune function in patients with depression after breast cancer surgery. Int. J. Psychiatry 47 (02), 370–372. doi:10.13479/j.carol.carroll.nki.jip.2020.02.051
Liu, X., Li, H., and Li, X. (2021b). TCM understanding and research progress of breast cancer related depression. Chin. J. Traditional Chin. Med. 36 (4), 2219–2221.
Liu, Z., and Xiao, B. (2011). Chinese medicine diagnosis and treatment for breast cancer clinical observation of 30 cases of depression. Guide Chin. Med. 17 (8), 13–15.
Lu, X., Zhu, P., and Chen, Y., (2021). Risk factors of depression and its correlation with immune status in breast cancer patients undergoing postoperative chemotherapy and their correlation with immune statys. Zhejiang Med. 43 (21), 2341–23442348.
Maass, S. W., Roorda, C., Berendsen, A. J., Verhaak, P. F. M., and de Bock, G. H. (2015). The prevalence of long-term symptoms of depression and anxiety after breast cancer treatment: A systematic review. Maturitas 82 (1), 100–108. doi:10.1016/j.maturitas.2015.04.010
Maybee, J., Pearson, T., and Elliott, L. (2022). The gut-brain-microbiome connection: Can probiotics decrease anxiety and depression? Issues Ment. Health Nurs. 43, 996–1003. doi:10.1080/01612840.2022.2106525
McGregor, B. A., Antoni, M. H., Boyers, A., Alferi, S. M., Blomberg, B. B., and Carver, C. S. (2004). Cognitive-behavioral stress management increases benefit finding and immune function among women with early-stage breast cancer. J. Psychosom. Res. 56 (1), 1–8. doi:10.1016/S0022-3999(03)00036-9
Miller, A. M., Steiner, C. A., and Barrett, M. L., (2009). “Breast reconstruction surgery for mastectomy in hospital inpatient and ambulatory settings,” in Healthcare cost and utilization project (HCUP) statistical briefs (Rockville, MD, United States: Agency for Healthcare Research and Quality US.
Padmalatha, S., Tsai, Y. T., Ku, H. C., Wu, Y. L., Yu, T., Fang, S. Y., et al. (2021). Higher risk of depression after total mastectomy versus breast reconstruction among adult women with breast cancer: A systematic review and metaregression. Clin. Breast Cancer 21 (5), e526–e538. doi:10.1016/j.clbc.2021.01.003
RenQi, S., Zhao, F., and Yu, H. (2021). Research progress of xiaoyao SAN in the treatment of depression. J. Traditional Chin. Med. 49 (4), 112–116. doi:10.19664/j.cnki.1002-2392.210099
Schenker, R. A., Marinescu, I., Stovicek, P. O., Lukács, E., Pauna-Cristian, L., Nica-Badea, D., et al. (2022). The clinical, biological, psychological and psychiatric impact of the diagnosis of breast cancer in women. Curr. Health Sci. J. 48 (1), 29–38. doi:10.12865/CHSJ.48.01.04
Shang, Z. M., Wu, J., and Zhou, J. (2019). A trajectory study of sleep and related symptoms in breast cancer patients based on ecological momentary assessment. Chin. J. Nurs. 54 (10), 1456–1462.
Sun, S., Yang, L., and Zhang, H., (2016). Effect of modified xiaoyao powder on depression in breast cancer patients with postoperative chemotherapy. Chin. J. TCM 31 (04), 1499–1502.
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., et al. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71 (3), 209–249. doi:10.3322/caac.21660
Tian, H., Hu, Z., Xu, J., and Wang, C. (2020). The molecular pathophysiology of depression and the new therapeutics. MedComm 3 (3), e156. doi:10.1002/mco2.156
Wang, Haiming, Sun, Huan, and Chen, Gege (2019). Xiaoyao powder for breast cancer patients with postoperative depressive state of random parallel control study. J. Traditional Chin. Med. Rev. 25 (4), 67–70. doi:10.13862/j.carol.carroll.nki.cn43-1446/r.2019.04.018
Wang, L. Y., Pierdomenico, A., Lefkowitz, A., and Brandt, R. (2015). Female sexual health training for oncology providers: New applications. Sex. Med. 3 (3), 189–197. doi:10.1002/sm2.66
Wang, P., Gao, X., Liang, M., Fang, Y., Jia, J., Tian, J., et al. (2021). Dose-effect/toxicity of bupleuri radix on chronic unpredictable mild stress and normal rats based on liver metabolomics. Front. Pharmacol. 12, 627451. doi:10.3389/fphar.2021.627451
Wang, X., Wang, N., Zhong, L., Wang, S., Zheng, Y., Yang, B., et al. (2020). Prognostic value of depression and anxiety on breast cancer recurrence and mortality: A systematic review and meta-analysis of 282,203 patients. Mol. Psychiatry 25 (12), 3186–3197. doi:10.1038/s41380-020-00865-6
Xiao, F. (2021). Clinical effect of modified Xiaoyao powder combined with paroxetine in the treatment of depression after breast cancer surgery. Chin. J. Ration. Drug Use 14 (13), 78–80. doi:10.15887/j.cnki.13-1389/r.2021.13.031
Xie, Yalan, and He, Caiyun (2017). Incidence and influencing factors of depression in breast cancer patients. General Nurs. 15 (3), 279–281. doi:10.3969/j.issn.1674-4748.2017.03.008
Xiong, Wei, Wang, Qingxi, and Wang, Xindong (2021). Clinical study of Ganmai Dazao Tang combined with routine Western medicine therapy for depression caused by malignant tumor. New tradit. Chin. Med. does (12), 140–144. doi:10.13457/j.carol.carroll.nki.JNCM.2021.12.036
Xu, C., Ganesan, K., Liu, X., Ye, Q., Cheung, Y., Liu, D., et al. (2022). Prognostic value of negative emotions on the incidence of breast cancer: A systematic review and meta-analysis of 129,621 patients with breast cancer. Cancers (Basel) 14 (3), 475. doi:10.3390/cancers14030475
Xu, N., Zhang, P., and Zhou, D., (2015). Investigation of depression status in postoperative patients with breast cancer and analysis its relationship with risk factors. Chin. J. Mod. Med. 25 (34), 68–72.
Yang, S., Huang, L., and Dai, H., (2021a). Characteristics of T lymphocyte subsets in patients with unipolar depression and bipolar depression. Chin. J. Med. Med. 59 (18), 23–26.
Yang, W., Liu, M., Zhang, Q., Zhang, J., Chen, J., Chen, Q., et al. (2020). Knockdown of miR-124 reduces depression-like behavior by targeting CREB1 and BDNF. Curr. Neurovasc Res. 17 (2), 196–203. doi:10.2174/1567202617666200319141755
Yang, Xuejing, Xu, Erping, and Shang, Lizhi (2021b). Sweet soup of big jujube of wheat and its progress party treat depression study. Chin. J. Exp. Formulas Chin. Med. 27 (24), 55–60. doi:10.13422/j.carol.carroll.nki.syfjx.20210342
Yuan, C., Huang, J., Li, H., Zhai, R., Zhai, J., Fang, X., et al. (2023). Association of clinical outcomes and the predictive value of T lymphocyte subsets within colorectal cancer patients. Front. Surg. 10, 1102545. doi:10.3389/fsurg.2023.1102545
Zhang, L., and Han, K. (2009). “How to analyze change from baseline: Absolute or percentage change,” in D-Level essay in statistics (Dalarna, Sweden: Dalarna University).
Zhang, Li-Hong, Zhi-jiang, Zhuang, and Wang, Ji-cheng (2015). Clinical study of Xiaoyao powder combined with fluoxetine hydrochloride capsule in the treatment of depression after breast cancer surgery. Chin. J. Traditional Chin. Med. 30 (6), 785–787. doi:10.16368/j.issn.1674-8999.2015.06.271
Zhang, Mingyuan (1998). Changsha, Hunan, China: Hunan Science and Technology Press, 121–126. Psychiatric Rating Scale Manual.
Zhao, D., Zhang, J., Zhu, Y., He, C., Fei, W., Yue, N., et al. (2022b). Study of antidepressant-like effects of Albiflorin and Paeoniflorin through metabolomics from the perspective of cancer-related depression. Front. Neurol. 13, 828612. doi:10.3389/fneur.2022.828612
Zhao, J., Shi, W., Lu, Y., Gao, X., Wang, A., Zhang, S., et al. (2022a). Alterations of monoamine neurotransmitters, HPA-axis hormones, and inflammation cytokines in reserpine-induced hyperalgesia and depression comorbidity rat model. BMC Psychiatry 22 (1), 419. doi:10.1186/s12888-022-04065-0
Zhu, Q., Yang, L., Yang, H., Han, Y., Chen, Y., and He, Y. (2022). Quercetin alleviates the progression of breast cancer-related depression via inhibiting the pyroptosis and promoting the immune response. Mediat. Inflamm. 2022, 8011988. doi:10.1155/2022/8011988
Keywords: traditional Chinese medicine, postoperative, depression, breast cancer, meta-analysis
Citation: Wang Y, Liu S, Zhang Y, Zhu G, Wang H, Xu B, Xie Y and Yang S (2023) Effect of traditional Chinese medicine on postoperative depression of breast cancer: a systematic review and meta-analysis. Front. Pharmacol. 14:1019049. doi: 10.3389/fphar.2023.1019049
Received: 14 August 2022; Accepted: 07 June 2023;
Published: 23 June 2023.
Edited by:
Reza Alizadeh-Navaei, Mazandaran University of Medical Sciences, IranReviewed by:
Ka Yui Kum, Life Code Limited, Hong Kong SAR, ChinaDanial Shamshirian, Shahid Beheshti University of Medical Sciences, Iran
Copyright © 2023 Wang, Liu, Zhang, Zhu, Wang, Xu, Xie and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ying Zhang, enlsenk1MDFAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Yan Wang
Yan Wang Suying Liu†
Suying Liu† Ying Zhang
Ying Zhang Yi Xie
Yi Xie