Abstract
Background:
Coronary heart disease (CHD) is a leading global cause of mortality, contributing to angina, arrhythmia, myocardial infarction, heart failure, and sudden death. Traditional treatments, including antiplatelet drugs, statins, β-blockers, and coronary stents, have notable side effects such as gastrointestinal bleeding and liver or muscle dysfunction, with post-operative stent complications. Recent studies have identified bioactive substances in leeches, particularly the natural anticoagulant hirudin, which inhibits thrombin and may help mitigate complications of coronary artery disease. Hirudin inhibits thrombin, reduces platelet aggregation, and lowers thrombosis risk. This meta-analysis evaluates the clinical efficacy and safety of Chinese herbal medicines containing leech in treating CHD, focusing on cardiovascular outcomes and adverse events.
Methods:
A systematic search of databases including PubMed, EMBASE, Web of Science, Cochrane Library, China National Knowledge Infrastructure (CNKI), WanFang Data (Wanfang), and VIP China Science and Technology Journal Database (VIP) was conducted to identify randomized controlled trials (RCTs) involving leech-containing Chinese herbal medicines for CHD patients up until February 2025. Key efficacy outcomes analyzed were total effective rate, ECG efficacy, and hemorheological parameters, while adverse event rates assessed treatment safety. The meta-analysis used Standardized Mean Difference (SMD) and 95% confidence intervals (CI) to assess efficacy, and Odds Ratio (OR) with 95% CI for safety. Subgroup analyses examined the relationship between therapeutic effects and patient characteristics.
Results:
Sixty-five studies involving 7,221 patients were included. The results showed that leech-based treatments significantly improved the total effective rate [OR = 3.70, 95% CI (3.19, 4.31), Z = 17.05, P < 0.00001] and ECG efficacy [OR = 2.58, 95% CI (2.23, 2.99), P < 0.0001], along with significant improvements in hemorheological parameters. Subgroup analysis indicated leech treatments were particularly effective for improving the total effective rate, ECG outcomes, and hemorheological indices. Importantly, adverse event rates did not increase compared to conventional treatments.
Conclusion:
Chinese herbal medicines containing leeches provide significant clinical benefits for CHD, particularly in improving ECG outcomes and blood parameters. These findings suggest that leech-based treatments are both effective and safe, with no increase in adverse events.
Systematic Review Registration:
https://www.crd.york.ac.uk/prospero/, Identifier CRD42024564675.
1 Introduction
Coronary heart disease is primarily caused by atherosclerosis or functional abnormalities in the coronary arteries, leading to myocardial ischemia, hypoxia, and necrosis. The disease’s primary clinical manifestations include angina pectoris, arrhythmia, and myocardial infarction (Pothineni et al., 2017). As one of the leading causes of global mortality, CHD accounts for approximately 9.31 million deaths annually, or nearly half of all cardiovascular disease-related deaths (Katta et al., 2021). The management of CHD typically involves antiplatelet agents, lipid-lowering drugs, β-blockers, and coronary stent implantation. However, these treatments are not without limitations, as prolonged use of these drugs can lead to adverse effects such as gastrointestinal bleeding, muscle and liver dysfunction, and complications from stent implantation (Passacquale et al., 2022; Mao et al., 2021; Zhang et al., 2024; Xin et al., 2023; Shan-Shan and Lu, 2022).
In light of the potential drawbacks of conventional therapies, recent research has focused on alternative treatments derived from traditional Chinese medicine (TCM) (Chunmiao et al., 2024). Substances in leeches, particularly hirudin, have garnered attention for their anticoagulant, anti-inflammatory, and fibrinolytic properties (Wu et al., 2024; Junren et al., 2021; Lemke and Vilcinskas, 2020). Hirudin directly inhibits thrombin activity, reduces platelet aggregation, and improves vascular health. Many randomized controlled trials have examined the efficacy of Chinese patent medicines containing leech components for treating CHD. However, no comprehensive comparison of the efficacy of different leech-containing medicines have been conducted. This study aims to bridge this gap by conducting a meta-analysis of RCTs to compare the efficacy and safety of these treatments.
2 Materials and methods
This meta-analysis was conducted in accordance with the PRISMA guidelines of the Cochrane Handbook and was registered on the PROSPERO website. The registration number (CRD42024564675).
2.1 Search strategy
A systematic search was performed across multiple key medical databases, including PubMed, Embase, Cochrane Library, Web of Science, CNKI, Wanfang, and VIP, covering publications from their inception until February 2025. Keywords such as “Leeches,” “Coronary Disease,” “Angina,” “Heart Disease,” “Acute Coronary Syndromes,” and “Randomized Controlled Trial (RCT)” were used to identify relevant studies. In addition, experts in the field were consulted to gather unpublished data and ensure a comprehensive search. Detailed search formula table is attached as an appendix.
2.2 Study selection
The studies were screened according to the PICOS framework. Eligible studies included RCTs evaluating the efficacy of Chinese herbal medicines containing leech components in CHD patients. Studies were excluded if they did not clearly mention the use of leech components, had incomplete data, or lacked scientific rigor (Table 1).
TABLE 1
| Parameter | Inclusion criteria |
|---|---|
| Population | Patients with a definite diagnosis of coronary heart disease (diagnostic criteria were in accordance with relevant domestic and foreign guidelines) were enrolled |
| Intervention | Chinese herbal medicines containing leech ingredients were used alone or in combination with conventional treatment |
| Comparator | Conventional treatment, placebo or other Chinese medicine; |
| Outcome | The improvement rate of angina symptoms, electrocardiogram improvement rate, hemorheology index, incidence of major cardiovascular events and adverse drug reactions were recorded. |
| Study design | Being an RCT in either parallel or cross-over design |
| Exclusion criteria | Non-RCT studies, those not clearly mentioning the components of leeches, incomplete data or inability to extract valid data, studies with a follow-up period shorter than 4 weeks or lacking scientific evidence, as well as low-quality studies that have been repeatedly published. |
Inclusion and exclusion criteria table.
This meta-analysis aims to evaluate the efficacy and safety of traditional Chinese medicines containing leech in the treatment of CHD by including high-quality RCTs. The inclusion criteria focus on studies with clear diagnostic standards for CHD, encompassing patients of any age or sex with stable or unstable angina. The interventions include the use of leech-containing traditional Chinese medicine, either as monotherapy or combined with conventional western medicine, compared with control groups receiving standard treatments, placebo, or TCM without leech. Key outcomes are categorized into primary outcomes, such as angina relief rate and ECG improvement rate, and secondary outcomes, including hemorheology and cardiac function indexes, incidence of major cardiovascular events, and drug-related adverse reactions. To ensure reliability, included studies must provide a clear description of randomization, control settings, and intervention measures, along with complete baseline data, post-treatment results, and statistical analyses. This comprehensive approach aims to provide robust evidence for the role of leech-containing TCM in CHD management.
Studies were excluded from this analysis if they: (1) Non-rct studies (such as observational studies, case reports, reviews, etc.); (2) The leech component was not explicitly mentioned in the intervention; (3) Incomplete data or unable to extract valid data; (4) The duration of follow-up was less than 4 weeks or the intervention lacked scientific evidence; (5) Duplicate published studies, and only the versions with complete data or higher quality were included.
2.3 Data extraction and quality assessment
Two investigators independently completed data extraction and cross-checked the extracted data. Disagreements were resolved through consultation or the intervention of third-party experts. The study authors; Time of publication; The sample size; Gender of the patient; Mean age; Type of disease; Primary outcome measures. If the data units are different for each parameter, we convert them to the most commonly used units.
The Cochrane Bias risk assessment tool was used to evaluate the quality of the included studies from the following six dimensions: 1. Random sequence generation (selection bias); 2. Allocation concealment (selection bias); 3. Blinded implementation (implementation bias and detection bias); 4. Data integrity (loss of follow-up bias); Selective reporting (reporting bias); 5. 6. Other sources of bias. According to the scoring results, the quality of the studies was divided into “high risk of bias”, “low risk of bias” and “uncertain risk of bias”.
Meta-analysis was performed using RevMan 5.4 software provided by Cochrane Collaboration. Relative risk difference (RD) and Mean difference (MD) were used as effect measures, and the point estimate of each effect size and its 95% confidence interval (95%CI) were reported. The test of heterogeneity was conducted by χ2 test (test level α = 0.1), and the degree of heterogeneity was evaluated by I2 statistic. Considering the possible statistical heterogeneity between studies, a random-effects model was used to integrate the results of various studies more accurately. In addition, funnel plots were used to assess the possibility of publication bias during the analysis of effect measures.
3 Results
3.1 Results of literature search
A total of 1,342 studies were initially retrieved, and after removing duplicates and screening titles and abstracts, 97 studies were shortlisted for full-text review as shown in Figure 1. Ultimately, 65 studies (Wu et al., 2001; Tong et al., 2001; Zhongtian and Rihui, 2001; Jian and Xudong, 2002; Jing et al., 2002; Taojin, 2002; Xianming et al., 2002; Yuxia et al., 2002; Zehong et al., 2002; Chunjian et al., 2003; Haijie and Changshi, 2003; Jinghe, 2003; Linfeng, 2003; Yanhong et al., 2003; Junjiang et al., 2004; Shaohua, 2004; Sujuan and Haijun, 2004; Lifang and Guofeng, 2005; Shougang, 2005; Xiaoyan and Bainian, 2006; Zhi-Min et al., 2006; Chunyan, 2007; Dongsheng and Jimin, 2008; Qingfan and Hezhong, 2008; Tangheng, 2008; Rongxing and Linlin, 2009; Shugang et al., 2009; Weidong and Lihua, 2009; Yunhai, 2009; Changming, 2010; Cuixia and Cunji, 2010; Haiyan, 2010; Shiyao, 2010; Xiaojun, 2010; Yong, 2010; Jun et al., 2011; Leilei, 2011; Quanyou, 2011; Shaofeng and Xinfeng, 2011; Xiao-Mei, 2011; Yongchao et al., 2011; Haiqing, 2012; Jinbao et al., 2012; Tingguo et al., 2012; Xinnian and Lu, 2012; Jinliang and Yunyi, 2013; Wei et al., 2013; Yu, 2013; Zongsheng, 2013; Cailiang et al., 2014; Sujuan et al., 2014; Yanbo, 2014; Youjun, 2014; Xuexu et al., 2014; Hongying et al., 2015; Zhaomei and Lian, 2015; Zhijing et al., 2016; Hongying et al., 2016; Jianmin et al., 2016; Mao and Qiang, 2017; Zhixue et al., 2017; Wenhui and Shiliang, 2019; Wenhua et al., 2020; Fei, 2021; Laiqiang, 2021), involving 7,221 patients, met the inclusion criteria.
FIGURE 1
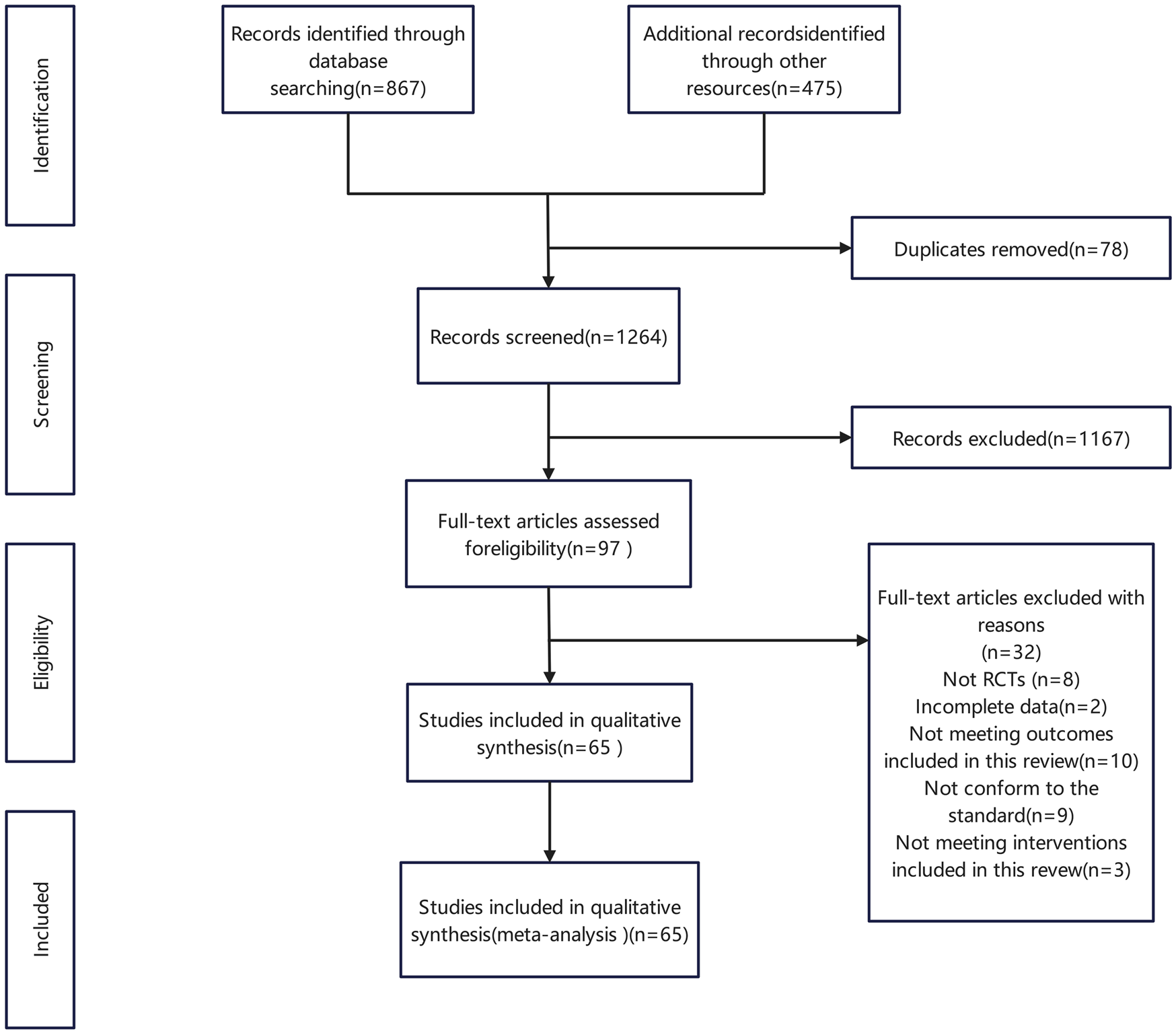
Flow chart of literature screening.
3.2 Basic characteristics of the included literature
After systematic screening and evaluation, a total of 7,221 patients were enrolled in this study, including 3,795 patients in the experimental group and 3,426 patients in the control group. All studies were RCTS.
The studies included patients with stable or unstable angina, with a mean age of 50–70 years in most studies. Of the 65 studies, 31 primarily focused on coronary heart disease (Wu et al., 2001; Jian and Xudong, 2002; Taojin, 2002; Yuxia et al., 2002; Zehong et al., 2002; Linfeng, 2003; Sujuan and Haijun, 2004; Xiaoyan and Bainian, 2006; Zhi-Min et al., 2006; Chunyan, 2007; Dongsheng and Jimin, 2008; Tangheng, 2008; Weidong and Lihua, 2009; Yunhai, 2009; Changming, 2010; Haiyan, 2010; Shiyao, 2010; Jun et al., 2011; Leilei, 2011; Xiao-Mei, 2011; Yongchao et al., 2011; Haiqing, 2012; Tingguo et al., 2012; Xinnian and Lu, 2012; Jinliang and Yunyi, 2013; Wei et al., 2013; Sujuan et al., 2014; Yanbo, 2014; Youjun, 2014; Hongying et al., 2016; Jianmin et al., 2016), 23 on unstable angina (Tong et al., 2001; Zhongtian and Rihui, 2001; Jing et al., 2002; Chunjian et al., 2003; Haijie and Changshi, 2003; Yanhong et al., 2003; Junjiang et al., 2004; Shaohua, 2004; Lifang and Guofeng, 2005; Shougang, 2005; Qingfan and Hezhong, 2008; Rongxing and Linlin, 2009; Shugang et al., 2009; Cuixia and Cunji, 2010; Xiaojun, 2010; Yong, 2010; Quanyou, 2011; Jinbao et al., 2012; Yu, 2013; Zongsheng, 2013; Hongying et al., 2015; Mao and Qiang, 2017; Wenhua et al., 2020), 9 on stable angina pectoris (Xianming et al., 2002; Jinghe, 2003; Shaofeng and Xinfeng, 2011; Cailiang et al., 2014; Xuexu et al., 2014; Zhaomei and Lian, 2015; Wenhui and Shiliang, 2019; Fei, 2021; Laiqiang, 2021) and 2 on general angina symptoms (Zhijing et al., 2016; Zhixue et al., 2017). The detailed basic characteristics of the included studies are shown in Table 2.
TABLE 2
| Author | Year | Cases | Male/Female | Age (mean+SD) | Variety of disease | Outcome | ||
|---|---|---|---|---|---|---|---|---|
| T | C | |||||||
| Xue fei | 2021 | T:30 C:30 | 17/13 | 16/14 | T:65.21±4.42 | C:65.21±4.46 | Stable angina pectoris | [1] [4] [5] [6] |
| Wang lai qiang | 2021 | T:50 C:50 | 27/23 | 25/25 | T:63.47±5.89 | C:62.56±6.57 | Stable angina pectoris | [1] [2] [4] [7] |
| Liang wen hua | 2020 | T:49 C:53 | 57/45 | T+C:56.15±9.24 | Unstable angina | [1] [4] [5] [6] [7] [12] | ||
| Fan wen hui | 2019 | T:60 C:60 | 30/30 | 32/28 | T:58.50±4.73 | C:57.40 ±5.03 | Stable angina pectoris | [1] [2] [4] [14] [15] [16] [17] |
| Ye mao | 2017 | T:60 C:60 | 34/26 | 33/27 | T:61.7±15.5 | C:61.5±15.3 | Unstable angina | [1] [2] [12] [13] [14] [15] [16] [17] [5] [6] |
| Tian zhi xue | 2017 | T:40 C:40 | 28/12 | 27/13 | T:60.3±5.4 | C:60.8±5.7 | Angina | [1] [4] [5] [6] [7] [8] |
| Yao hong ying | 2016 | T:30 C:30 | 17/13 | 15/15 | T:52.78±2.56 | C:53.69±3.23 | Coronary heart disease | [1] [14] [15] [17] |
| Liin zhi jing | 2016 | T:150 C:150 | 79/71 | 76/74 | T:65.2 | C:64.1 | Angina | [1] [12] [13] [20] |
| Dai jian min | 2016 | T:37 C:36 | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Coronary heart disease | [1] [2] [4] [14] [15] [16] [17] |
| Li hong ying | 2015 | T:52 C:54 | 31/21 | 33/21 | Not mentioned | Not mentioned | Unstable angina | [1] [2] [4] |
| Deng zhao mei | 2015 | T:30 C:30 | 35/25 | T+C:57.7±5.91 | Stable angina pectoris | [1] [2] | ||
| Zhang you jun | 2014 | T:56 C:50 | 35/21 | 32/18 | T:62 | C:61 | Coronary heart disease | [1] [2] [3] |
| Yang su juan | 2014 | T:96 C:104 | 44/52 | 49/55 | Not mentioned | Not mentioned | Coronary heart disease | [1] [12] [13] |
| Su xue xu | 2014 | T:30 C:30 | 16/14 | 15/15 | T:64.4±12.2 | C:67.8±12.4 | Stable angina pectoris | [1] [2] |
| Peng cai liang | 2014 | T:40 C:40 | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Stable angina pectoris | [1] [12] [13] [20] |
| Li yan bo | 2014 | T:50 C:50 | 28/22 | 24/26 | T:64.5 | C:66.5 | Coronary heart disease | [1] |
| Wu jin liang | 2013 | T:156 C:98 | 90/66 | 58/40 | T:70 | C:69.5 | Coronary heart disease | [1] [5] [6] [7] [8] [14] [15] [16] |
| Shang yu | 2013 | T:66 C:56 | 42/24 | 36/20 | T:67±4.9 | C:68±3.8 | Unstable angina | [1] [5] [6] [10] [11] [7] |
| Huang wei | 2013 | T:72 C:36 | 40/32 | 20/16 | T:57±7 | C:57±8 | Coronary heart disease | [1] [2] |
| Du zong sheng | 2013 | T:30 C:30 | 18/12 | 17/13 | T:51.8±15.4 | C:49.8 ±14.7 | Unstable angina | [1] [12] [13] [20] [23] |
| Yu hai qing | 2012 | T:103 C:48 | 68/35 | 32/16 | T+C:59.2 | Coronary heart disease | [1] [2] [5] [6] | |
| Shi jin bao | 2012 | T:35 C:32 | 20/15 | 18/14 | T:58.1 | C:60.2 | Unstable angina | [1] [2] [4] |
| Lu ting guo | 2012 | T:80 C:80 | 45/35 | 43/37 | T:48.3 | C:47.5 | Coronary heart disease | [1] [2] [12] [13] |
| Liu xin nian | 2012 | T:31 C:30 | 17/14 | 16/14 | T:58.15±5.13 | C:56.45±5.65 | Coronary heart disease | [20] [21] [22] [23] |
| Zhu lei lei | 2011 | T:23 C:23 | 15/8 | 14/9 | T:58 ±3.23 | C:56 ±3.29 | Coronary heart disease | [1] [2] |
| Zhang yong chao | 2011 | T:40 C:40 | 19/21 | 20/20 | T:62.25±10.72 | C:61.78±11.32 | Coronary heart disease | [2] [12] |
| Ma xiao mei | 2011 | T:60 C:60 | 36/24 | 38/22 | T:58 | C:59 | Coronary heart disease | [1] [2] |
| Li jun | 2011 | T:36 C:36 | 21/15 | 20/16 | T:68±9 | C:67±8 | Coronary heart disease | [1] [24] [25] |
| Gong quan you | 2011 | T:70 C:70 | 42/28 | 40/30 | Not mentioned | Not mentioned | Unstable angina | [1] [2] |
| Cai shao feng | 2011 | T:52 C:50 | 37/15 | 33/17 | Not mentioned | Not mentioned | Stable angina pectoris | [1] [2] |
| Lu shi yao | 2010 | T:43 C:42 | 28/15 | 24/18 | T:62.6 | C:64.1 | Coronary heart disease | [1] |
| Liu chang ming | 2010 | T:60 C:60 | 42/18 | 38/22 | Not mentioned | Not mentioned | Coronary heart disease | [1] |
| Liu cui xia | 2010 | T:40 C:38 | 28/12 | 29/9 | T:57±8 | C:56±9 | Unstable angina | [1] |
| Li xiao jun | 2010 | T:30 C:30 | 42/18 | T+C:52±7 | Unstable angina | [1] | ||
| Jin yong | 2010 | T:62 C:50 | 40/22 | 36/14 | T:80 | C:79 | Unstable angina | [1] [2] |
| Huang hai yan | 2010 | T:42 C:40 | 22/20 | 21/19 | T:58.2 | C:56.2 | Coronary heart disease | [1] [2] |
| Yuan shu gang | 2009 | T:60 C:60 | 38/22 | 40/20 | T:67.15 | C:68.12 | Unstable angina | [1] |
| Ni wei dong | 2009 | T:36 C:32 | 42/26 | T+C:52±7.5 | Coronary heart disease | [1] | ||
| Chen rong xing | 2009 | T:60 C:58 | 40/20 | 39/19 | Not mentioned | Not mentioned | Unstable angina | [2] [12] [13] |
| Cai yun hai | 2009 | T:69 C:66 | 35/34 | 31/35 | T:46.39±10.17 | C:45.12±8.97 | Coronary heart disease | [1] |
| Zhou tang heng | 2008 | T:48 C:42 | 30/18 | 29/13 | T:64 | C:61 | Coronary heart disease | [1] [2] |
| Zhang qing fan | 2008 | T:57 C:56 | 31/26 | 30/26 | Not mentioned | Not mentioned | Unstable angina | [1] [2] |
| Chen dong sheng | 2008 | T:60 C:40 | 44/16 | 30/10 | T:56±1.56 | C:56±1.53 | Coronary heart disease | [1] [2] |
| Yan chun yan | 2007 | T:60 C:60 | 81/39 | Not mentioned | Not mentioned | Coronary heart disease | [1] [23] | |
| Zhang zhi min | 2006 | T:250 C:250 | 163/87 | 166/84 | T:55.6±20.4 | C:54.3±17.7 | Coronary heart disease | [14] [15] [16] [17] |
| Yang xiao yan | 2006 | T:40 C:40 | 24/16 | 23/17 | T:55.7±4.3 | C:54.9±4.9 | Coronary heart disease | [1] [24] [25] |
| Jiao shou gang | 2005 | T:50 C:42 | 28/22 | 24/18 | T:58.6 | C:56.7 | Unstable angina | [1] [2] [12] [14] [15] [17] |
| Chen li fang | 2005 | T:31 C:30 | 18/13 | 19/11 | T:65.5 | C:63.61 | Unstable angina | [1] [2] |
| Zhang shao hua | 2004 | T:21 C:18 | 17/4 | 15/3 | T:68.7 | C:68.1 | Unstable angina | [1] [20] [21] [22] [23] |
| Zhang jun jiang | 2004 | T:42 C:42 | 32/10 | 36/6 | Not mentioned | Not mentioned | Unstable angina | [1] [6] [10] |
| Yang su juan | 2004 | T:120 C:80 | 86/34 | 58/22 | Not mentioned | Not mentioned | Coronary heart disease | [1] [2] |
| Yu hai jie | 2003 | T:22 C:22 | 19/3 | 17/5 | T:59.2 | C:61.4 | Unstable angina | [1] [2] |
| Wang yan hong | 2003 | T:60 C:40 | 41/19 | 28/12 | T:68.3±6.4 | C:67.4±6.9 | Unstable angina | [1] [2] [5] [6] [8] |
| Shang jing he | 2003 | T:66 C:60 | 40/26 | 40/20 | T:56.3 | C:60.5 | Stable angina pectoris | [1] [2] [5] [6] [7] [14] [15] [16] |
| Niu chun jian | 2003 | T:30 C:30 | 16/14 | 15/15 | T:60.7 | C:61.4 | Unstable angina | [1] [12] [7] [14] [15] [10] |
| Liao lin feng | 2003 | T:40 C:25 | 27/13 | 14/11 | T:62.43 | C:61.56 | Coronary heart disease | [1] [2] [5] [6] [7] [8] |
| Zhao ze hong | 2002 | T:175 C:121 | 195/101 | T+C:63.2±9.7 | Coronary heart disease | [1] [2] [12] | ||
| Zhao yu xia | 2002 | T:31 C:31 | 18/13 | 28/3 | T:57±12 | C:54±11 | Coronary heart disease | [14] [15] [16] |
| Xue jing | 2002 | T:29 C:29 | 16/13 | 15/14 | T:61.2 | C:60.5 | Unstable angina | [1] [2] [14] [15] [7] [19] |
| Li tao jin | 2002 | T:36 C:36 | 20/16 | 18/18 | T:60.2±6.56 | C:59.61±7.26 | Coronary heart disease | [1] [2] [4] [18] |
| Fu jian | 2002 | T:45 C:40 | 26/19 | 24/16 | T:61±7.2 | C:59±6.2 | Coronary heart disease | [1] [2] [3] |
| Fang xian ming | 2002 | T:30 C:30 | 23/7 | 24/6 | T:56.8 | C:57.2 | Stable angina pectoris | [1] [2] [3] |
| Xu zhong tian | 2001 | T:52 C:52 | 38/14 | 34/18 | Not mentioned | Not mentioned | Unstable angina | [1] [5] [6] [20] [9] [11] |
| Wang tong | 2001 | T:82 C:80 | 60/22 | 60/20 | T+C:51.5±3.2 | Unstable angina | [1] [2] [5] [6] [10] [9] | |
| Wang ling yun | 2001 | T:100 C:100 | 107/93 | T+C:56.3 | Coronary heart disease | [1] [2] | ||
Evaluation table of literature quality.
T, experimental group, C, control group; A, Chinese patent medicine containing leech ingredients; B, conventional treatment; Efficacy evaluation indexes include; [1] Effective; [2] ECG efficacy; [3] Efficacy of main symptoms; [4] TCM symptom points; [5] Whole blood viscosity; [6] plasma viscosity (high + low); [7] Fibrinogen; [8] Hematocrit; [9] Sedimentation rate equation; [10] Platelet adhesion rate; [11] hematocrit; [12] frequency of angina attacks; [13] Duration of angina; [14] Total cholesterol; [15] Triglycerides; [16] High-density lipoprotein; [17] Low-density lipoprotein; [18] Blood glucose; [19] Prothrombin time; [20] ST-T changes; [21] Sum of ST changes; [22] systolic blood pressure; [23] heart rate; [24] Cardiac ejection fraction; [25] Left ventricular end-diastolic diameter.
3.3 Quality evaluation of included studies
Among the 65 included studies, 56 studies were low-risk, 6 studies only mentioned randomization, but did not specify the random allocation method, rated as unclear risk, and 3 studies did not mention it. In terms of allocation concealment, 38 studies were rated as low risk, 6 studies did not give clear allocation as high risk, and the remaining 23 studies did not mention allocation concealment as unclear risk. In terms of research blinding, 25 studies mentioned it, 36 studies did not mention it, and 4 studies were rated as high risk because they could not be blinded due to different types of interventions included in the studies. In terms of completeness of outcome indicators, 17 items clearly stated that there was no loss of follow-up and were rated as low risk. Six items mentioned loss of follow-up, which was rated as high risk. The remaining 42 did not mention loss to follow-up and were rated as unclear risk. Data were reported selectively; 24 were low-risk and 41 were high-risk. Other risks of bias were only mentioned in 12 articles, and the rest were unclear. The risk of bias assessment of the included studies is shown in Figures 2, 3.
FIGURE 2
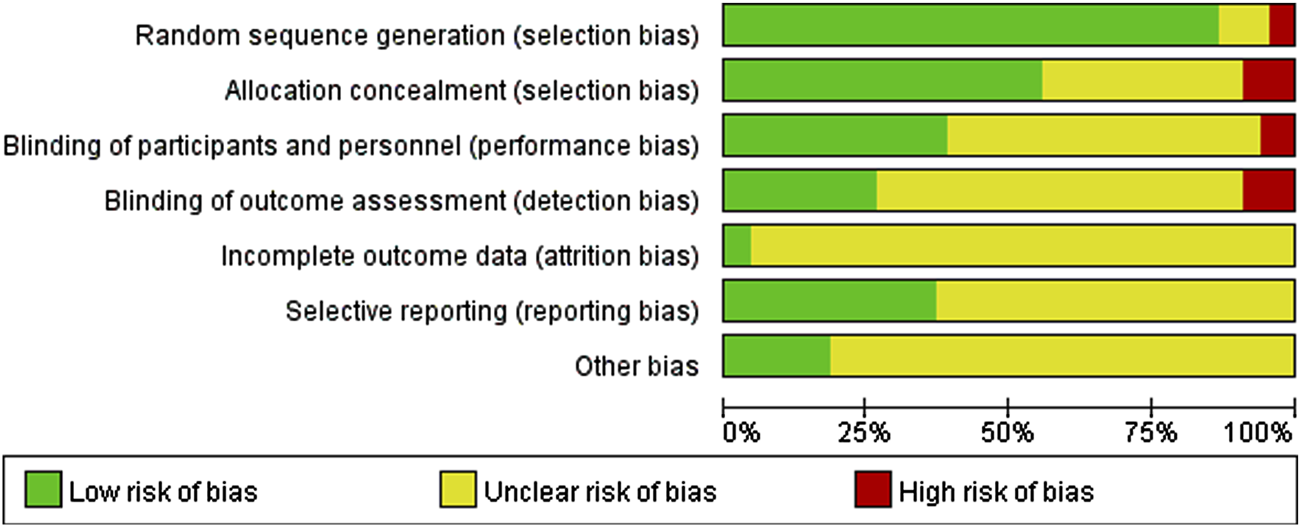
Proportion of items that generated risk of bias in the included literature.
FIGURE 3
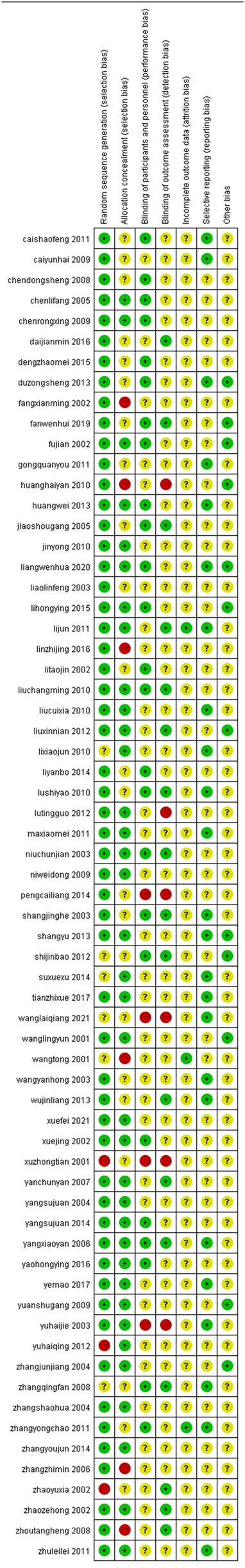
The proportion of items with bias risks in each literature work.
3.4 Results
3.4.1 Total clinical effective rate
A total of 58 studies (Wu et al., 2001; Tong et al., 2001; Zhongtian and Rihui, 2001; Jian and Xudong, 2002; Jing et al., 2002; Taojin, 2002; Xianming et al., 2002; Zehong et al., 2002; Chunjian et al., 2003; Haijie and Changshi, 2003; Jinghe, 2003; Linfeng, 2003; Yanhong et al., 2003; Junjiang et al., 2004; Shaohua, 2004; Sujuan and Haijun, 2004; Lifang and Guofeng, 2005; Shougang, 2005; Xiaoyan and Bainian, 2006; Chunyan, 2007; Dongsheng and Jimin, 2008; Qingfan and Hezhong, 2008; Tangheng, 2008; Shugang et al., 2009; Weidong and Lihua, 2009; Changming, 2010; Cuixia and Cunji, 2010; Haiyan, 2010; Shiyao, 2010; Xiaojun, 2010; Yong, 2010; Jun et al., 2011; Leilei, 2011; Quanyou, 2011; Shaofeng and Xinfeng, 2011; Xiao-Mei, 2011; Haiqing, 2012; Jinbao et al., 2012; Tingguo et al., 2012; Jinliang and Yunyi, 2013; Wei et al., 2013; Yu, 2013; Zongsheng, 2013; Cailiang et al., 2014; Yanbo, 2014; Youjun, 2014; Xuexu et al., 2014; Hongying et al., 2015; Zhaomei and Lian, 2015; Zhijing et al., 2016; Hongying et al., 2016; Jianmin et al., 2016; Mao and Qiang, 2017; Zhixue et al., 2017; Wenhui and Shiliang, 2019; Wenhua et al., 2020; Fei, 2021; Laiqiang, 2021) with total clinical response rate as the outcome index, a total of 6,065 patients were included. The total response rate of 58 studies was homogeneous (P = 0.68, I2 = 0%), and a fixed effect model was set. Meta-analysis results showed that: The total effective rate of the treatment group was higher than that of the control group, and the difference was statistically significant [OR = 3.70, 95%CI (3.19, 4.31), Z = 17.05, P < 0.00001], indicating that in terms of improving the total effective rate of coronary heart disease, the combination of conventional western medicine with leech Chinese patent medicine was significantly better than the simple conventional western medicine (Figure 4).
FIGURE 4
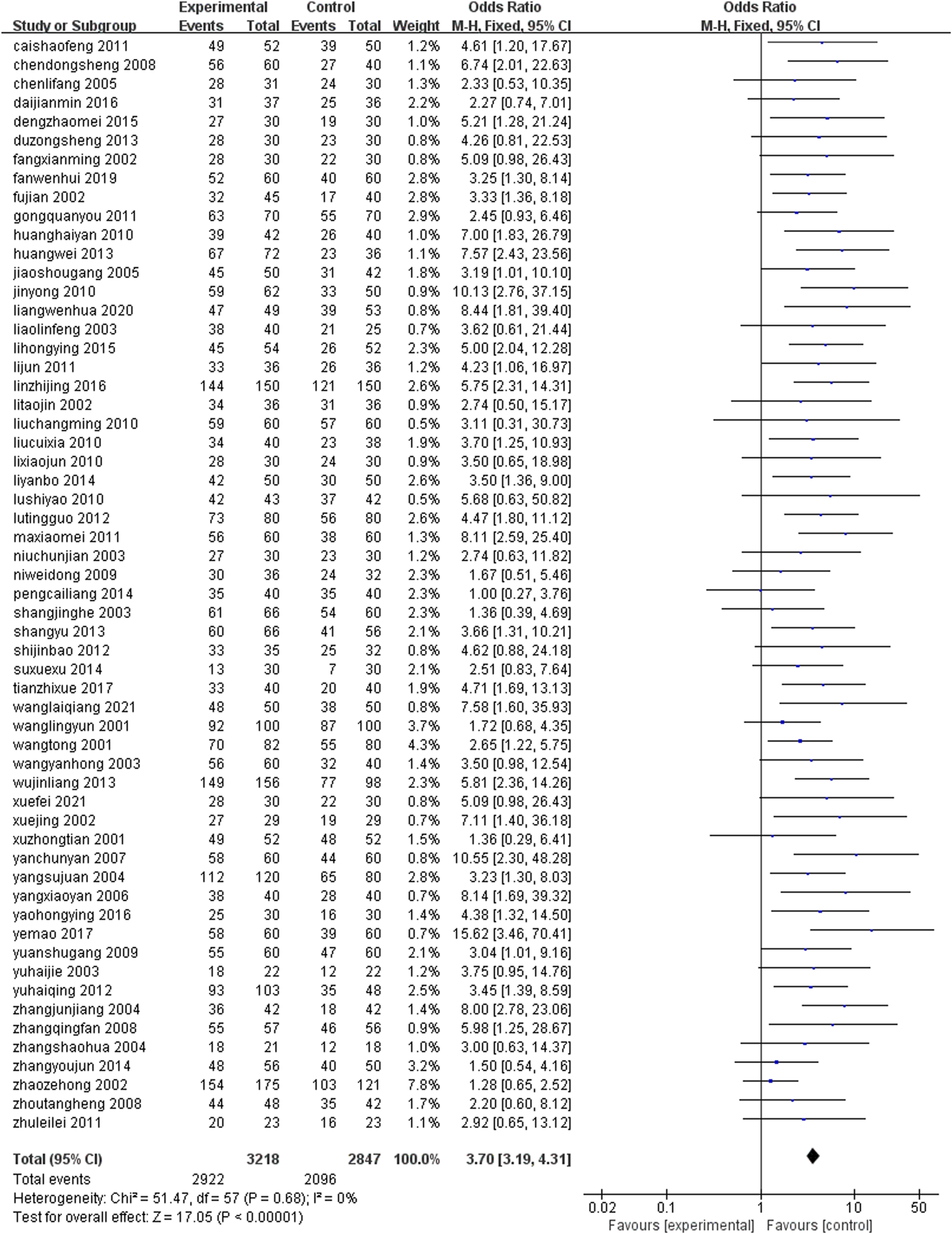
Total effective rate.
3.4.2 ECG efficacy
Thirty eight studies (Wu et al., 2001; Tong et al., 2001; Jian and Xudong, 2002; Jing et al., 2002; Taojin, 2002; Xianming et al., 2002; Zehong et al., 2002; Haijie and Changshi, 2003; Jinghe, 2003; Linfeng, 2003; Sujuan and Haijun, 2004; Lifang and Guofeng, 2005; Shougang, 2005; Dongsheng and Jimin, 2008; Qingfan and Hezhong, 2008; Tangheng, 2008; Rongxing and Linlin, 2009; Yunhai, 2009; Haiyan, 2010; Yong, 2010; Leilei, 2011; Quanyou, 2011; Shaofeng and Xinfeng, 2011; Xiao-Mei, 2011; Yongchao et al., 2011; Haiqing, 2012; Jinbao et al., 2012; Tingguo et al., 2012; Wei et al., 2013; Sujuan et al., 2014; Youjun, 2014; Xuexu et al., 2014; Hongying et al., 2015; Zhaomei and Lian, 2015; Jianmin et al., 2016; Mao and Qiang, 2017; Wenhui and Shiliang, 2019; Laiqiang, 2021) (n = 4,190) reported the ECG efficacy after treatment. The results of meta-analysis under fixed effects model (I2 = 2%, P < 0.0001) showed that the group containing leech Chinese medicine combined with conventional treatment had better ECG efficacy after treatment, and the difference was statistically significant [OR = 2.58, 95%CI (2.23, 2.99), P < 0.0001] (Figure 5).
FIGURE 5
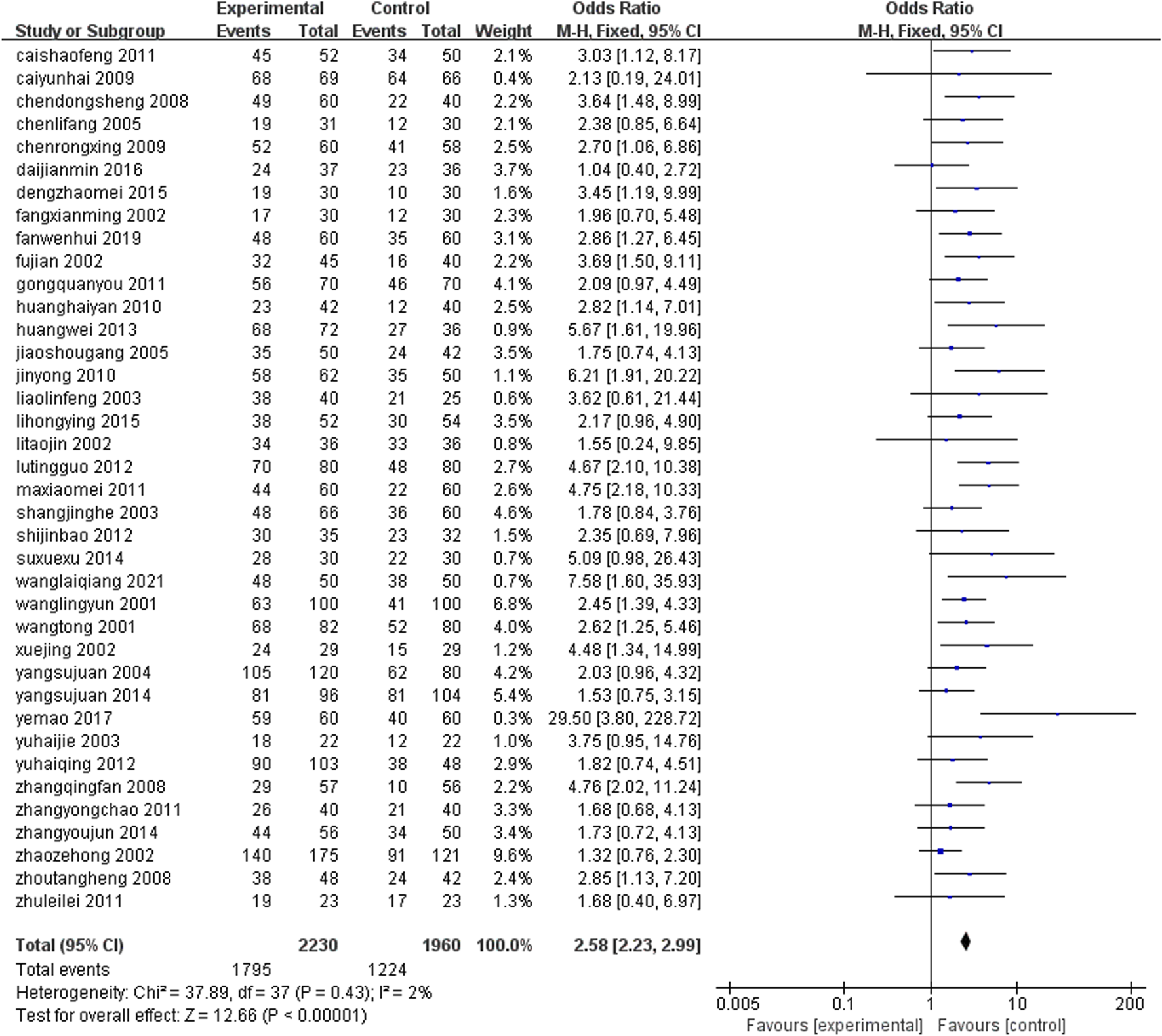
Comparison of ECG efficacy between leech combined with conventional treatment and conventional treatment alone.
3.4.3 TCM symptoms and efficacy
Three studies (Jinbao et al., 2012; Hongying et al., 2015; Wenhui and Shiliang, 2019) (n = 293) reported the efficacy of TCM symptoms after treatment, and the difference between the two groups was statistically significant [OR = 3.75, 95%CI (1.81, 7.73), Z = 3.57, P = 0.0004]. The Chinese patent medicine containing leech combined with conventional medicine in the treatment of CHD could improve the efficacy of TCM symptoms than conventional western medicine alone (Figure 6).
FIGURE 6
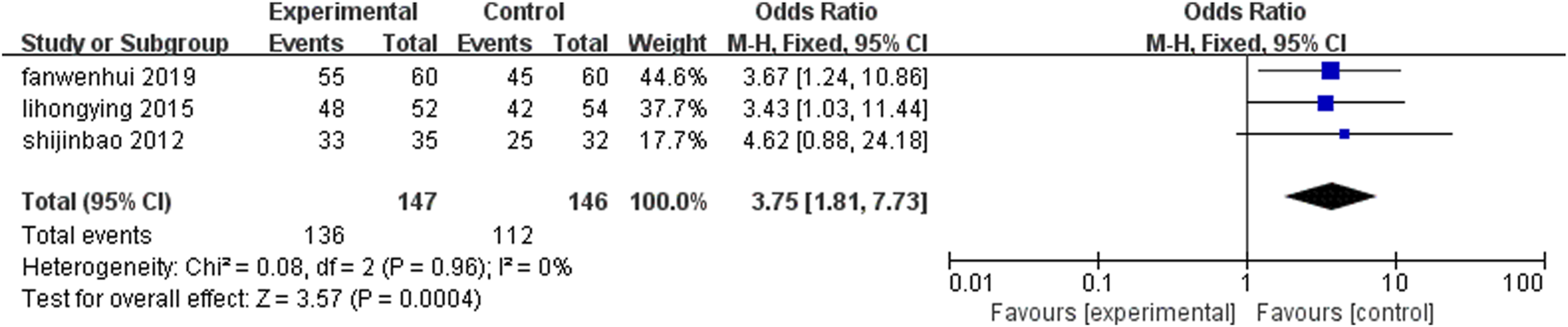
Comparison of the efficacy of leech combined with conventional treatment and conventional treatment alone for TCM symptoms.
3.4.4 Frequency of angina pectoris
Nine studies (Shougang, 2005; Rongxing and Linlin, 2009; Yongchao et al., 2011; Tingguo et al., 2012; Zongsheng, 2013; Cailiang et al., 2014; Zhijing et al., 2016; Mao and Qiang, 2017; Wenhua et al., 2020) (n = 1,112) reported the frequency of angina pectoris in each group after treatment. The results of Meta-analysis showed that the frequency of angina pectoris attack after treatment with leech Chinese medicine combined with conventional medication was lower than that of conventional treatment alone, and the incidence of angina pectoris was significantly reduced. The difference between the two groups was statistically significant [SMD = −1.13, 95%CI (-1.52, −0.75), Z = 5.75, P ≤ 0.00001] (Figure 7).
FIGURE 7
![Forest plot showing a meta-analysis of studies comparing experimental and control groups. Each study is listed with mean, standard deviation, and weight percentage. The plot includes standard mean differences with 95% confidence intervals. The overall effect size is -1.13 with a confidence interval of [-1.52, -0.75]. The heterogeneity measures are tau squared equals 0.30, chi squared equals 67.18, degrees of freedom equals 8, p-value less than 0.00001, and I squared equals 88%. The overall effect test is significant with Z equals 5.75 and p less than 0.00001.](https://www.frontiersin.org/files/Articles/1643611/xml-images/fphar-16-1643611-g007.webp)
Comparison of frequency of angina episodes between leech combined with conventional treatment and conventional treatment alone.
3.4.5 Whole blood viscosity
Twelve studies (Tong et al., 2001; Zhongtian and Rihui, 2001; Jinghe, 2003; Linfeng, 2003; Yanhong et al., 2003; Haiqing, 2012; Jinliang and Yunyi, 2013; Yu, 2013; Mao and Qiang, 2017; Zhixue et al., 2017; Wenhua et al., 2020; Fei, 2021) (n = 1,446) reported on post-treatment whole blood viscosity levels in each group. Meta-analysis results showed that: The whole blood viscosity level was lower after the treatment of Chinese patent medicine containing leech ingredients combined with conventional medication than that of conventional treatment alone, and the difference between the two groups was statistically significant [SMD = −1.35, 95%CI (−2.10, −0.60), Z = 3.53, P = 0.0004] (Figure 8).
FIGURE 8
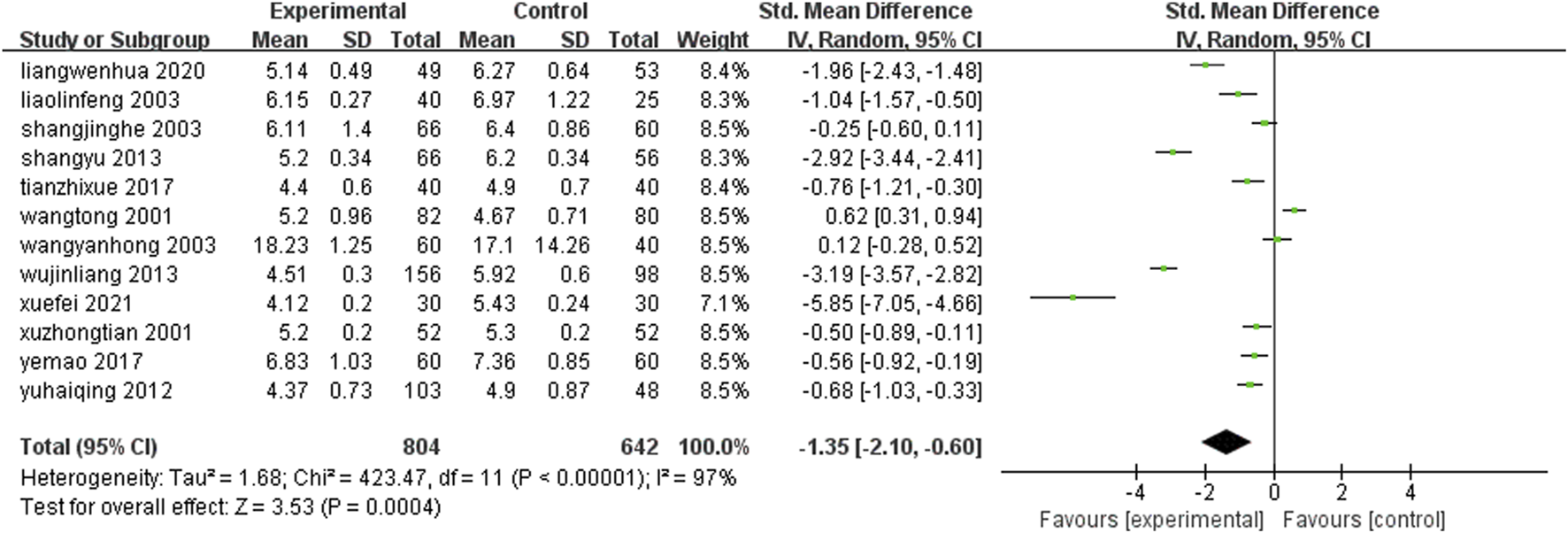
Comparison of whole blood viscosity between leech combined with conventional treatment and conventional treatment alone.
3.4.6 Plasma viscosity
Blood urea nitrogen levels 12 studies (Tong et al., 2001; Zhongtian and Rihui, 2001; Jinghe, 2003; Linfeng, 2003; Yanhong et al., 2003; Haiqing, 2012; Jinliang and Yunyi, 2013; Yu, 2013; Mao and Qiang, 2017; Zhixue et al., 2017; Wenhua et al., 2020; Fei, 2021) (n = 1,446) reported changes in plasma viscosity after treatment in each group. Meta-analysis results showed that: The plasma viscosity level after treatment with leech Chinese proprietary medicine combined with conventional medication was lower than that of conventional treatment alone, and the difference was statistically significant [SMD = −0.81, 95%CI(-1.24, −0.37), Z = 3.66, P = 0.0003] (Figure 9).
FIGURE 9
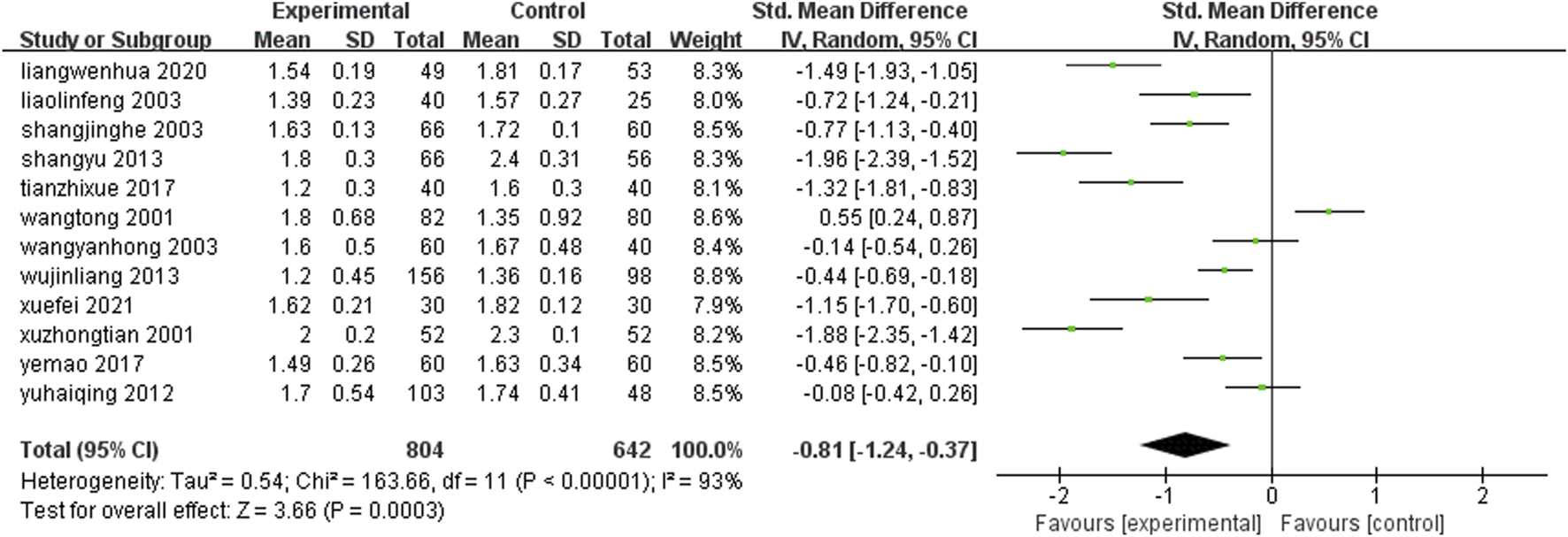
Comparison of plasma viscosity between leech combined with conventional treatment and conventional treatment alone.
3.4.7 Fibrinogen
Eight studies (Chunjian et al., 2003; Jinghe, 2003; Linfeng, 2003; Jinliang and Yunyi, 2013; Yu, 2013; Zhixue et al., 2017; Wenhua et al., 2020; Laiqiang, 2021) (n = 909) reported fibrinogen levels in each group after treatment. Meta-analysis results showed that: The level of fibrinogen in the treatment group was lower than that in the control group [SMD = −0.99, 95%CI (−1.52, −0.47), Z = 3.69, P = 0.0002] (Figure 10).
FIGURE 10
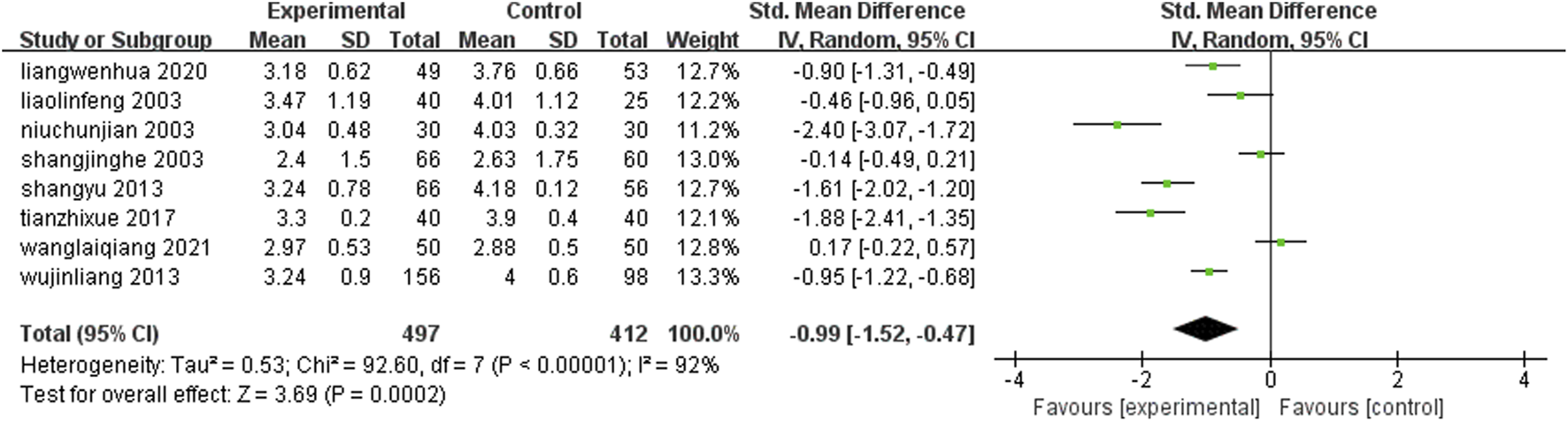
Comparison of leech combined with conventional treatment and conventional treatment alone for fibrinogen.
3.4.8 Total cholesterol
Fifteen studies (Jing et al., 2002; Taojin, 2002; Yuxia et al., 2002; Chunjian et al., 2003; Jinghe, 2003; Lifang and Guofeng, 2005; Shougang, 2005; Zhi-Min et al., 2006; Xiao-Mei, 2011; Yongchao et al., 2011; Jinliang and Yunyi, 2013; Hongying et al., 2016; Jianmin et al., 2016; Mao and Qiang, 2017; Wenhui and Shiliang, 2019) (n = 1858) reported the serum total cholesterol levels of each group after treatment. The results of Meta-analysis showed that the serum total cholesterol level after treatment with leech Chinese medicine combined with conventional treatment was lower than that of conventional treatment alone. The difference between the two groups was statistically significant [SMD = −1.55, 95%CI (−2.11, −0.99), Z = 5.41, P ≤ 0.00001] (Figure 11).
FIGURE 11
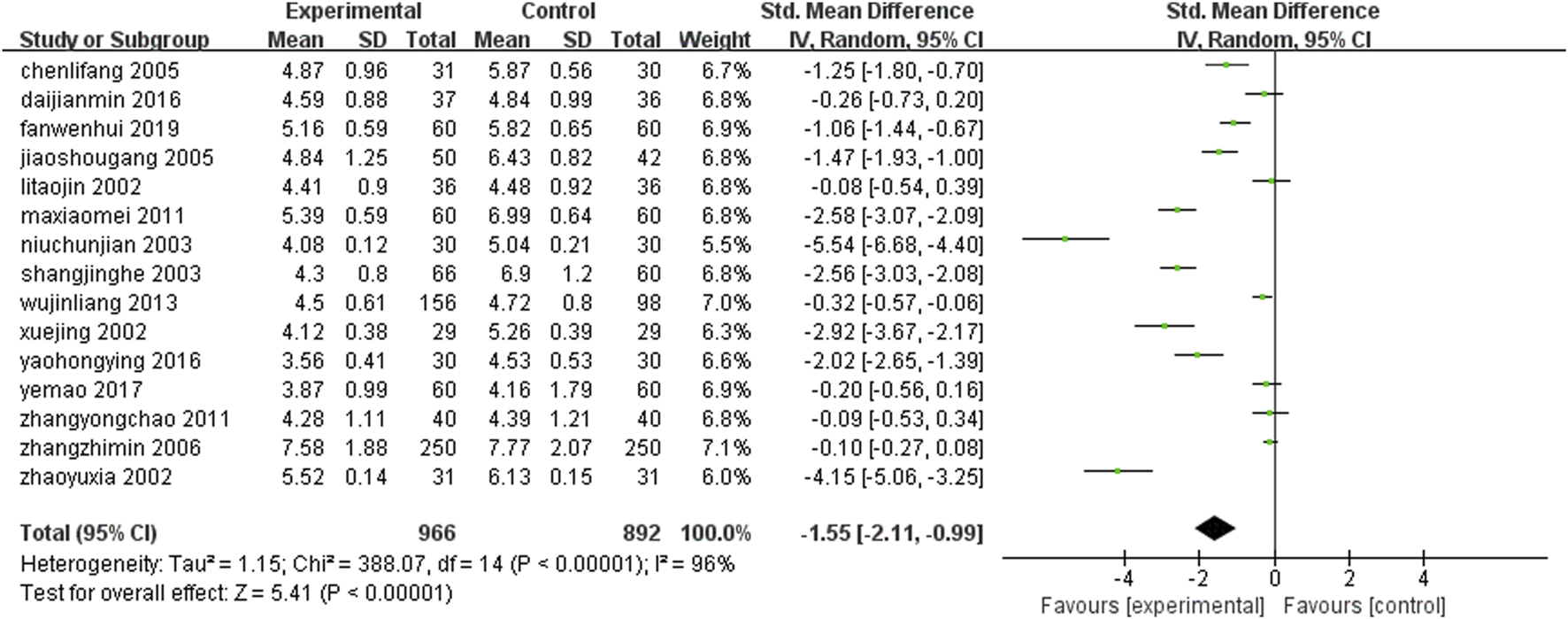
Comparison of total cholesterol between leech combined with conventional treatment and conventional treatment alone.
3.4.9 Triglycerides
Fifteen studies (Jing et al., 2002; Taojin, 2002; Yuxia et al., 2002; Chunjian et al., 2003; Jinghe, 2003; Lifang and Guofeng, 2005; Shougang, 2005; Zhi-Min et al., 2006; Xiao-Mei, 2011; Yongchao et al., 2011; Jinliang and Yunyi, 2013; Hongying et al., 2016; Jianmin et al., 2016; Mao and Qiang, 2017; Wenhui and Shiliang, 2019) (n = 1858) reported the serum triglyceride levels of each group after treatment. The results of Meta-analysis showed that the serum triglyceride level of the treatment with leech Chinese medicine combined with conventional treatment was lower than that of conventional treatment alone. The difference between the two groups was statistically significant [SMD = −1.12, 95%CI (−1.55, −0.69), Z = 5.10, P ≤ 0.00001] (Figure 12).
FIGURE 12
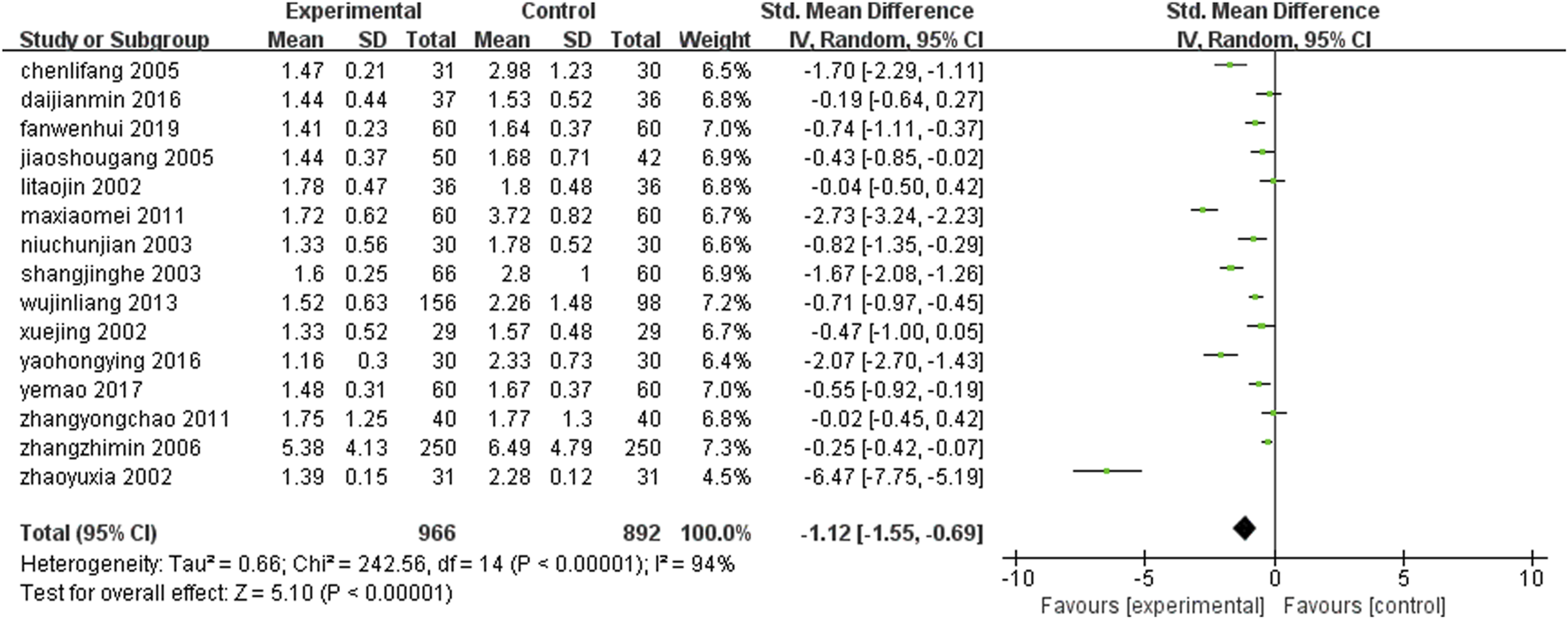
Comparison of leeches combined with conventional treatment and conventional treatment alone triglyceride.
3.4.10 High density lipoprotein
Eleven studies (Taojin, 2002; Yuxia et al., 2002; Jinghe, 2003; Lifang and Guofeng, 2005; Shougang, 2005; Zhi-Min et al., 2006; Xiao-Mei, 2011; Jinliang and Yunyi, 2013; Jianmin et al., 2016; Mao and Qiang, 2017; Wenhui and Shiliang, 2019) (n = 1,600) reported changes in HDL after treatment in each group. Meta-analysis results showed that: The level of high-density lipoprotein after leech combined with conventional medication was higher than that of conventional treatment alone, but there was no statistical significance [SMD = 0.37, 95%CI (0.05, 0.69), Z = 2.25, P = 0.02] (Figure 13).
FIGURE 13
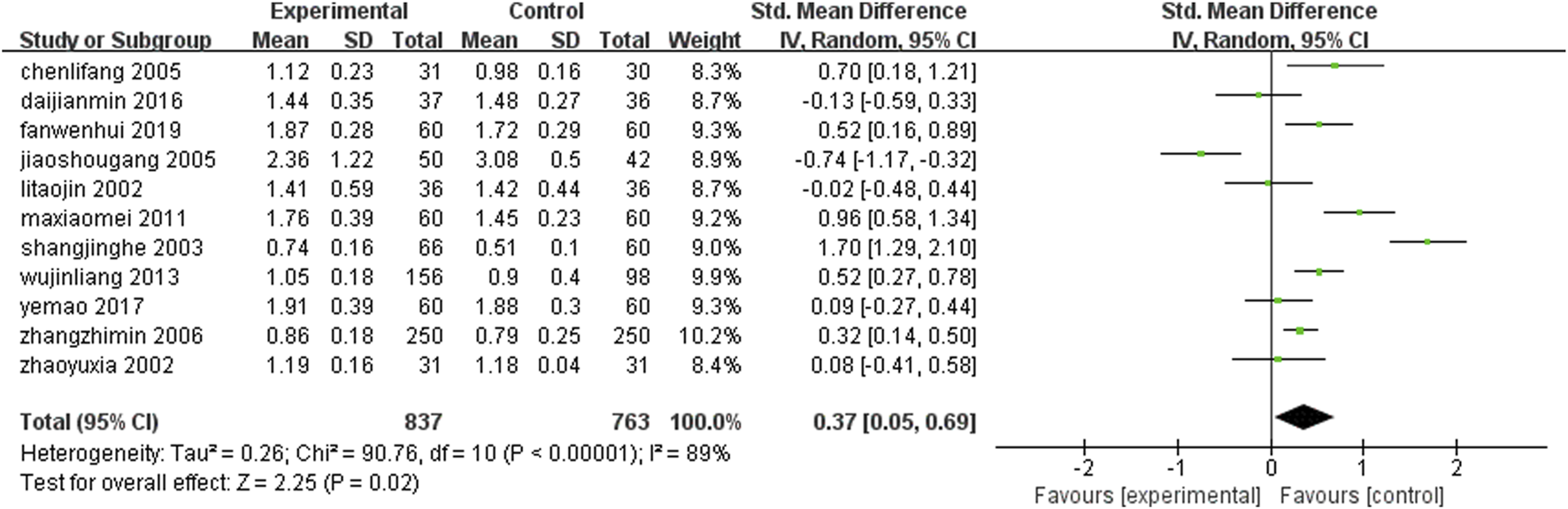
Comparison of leech combined with conventional treatment and conventional treatment alone for HDL.
3.4.11 Low density lipoprotein
Nine studies (Taojin, 2002; Lifang and Guofeng, 2005; Shougang, 2005; Zhi-Min et al., 2006; Xiao-Mei, 2011; Hongying et al., 2016; Jianmin et al., 2016; Mao and Qiang, 2017; Wenhui and Shiliang, 2019) (n = 1,218) reported the levels of low-density lipoprotein in each group after treatment. The results of Meta-analysis showed that the level of low-density lipoprotein after treatment with leech Chinese medicine combined with conventional treatment was lower than that of conventional treatment alone. The difference between the two groups was statistically significant [SMD = −0.75, 95%CI (−1.29, −0.21), Z = 2.74, P < 0.006] (Figure 14).
FIGURE 14
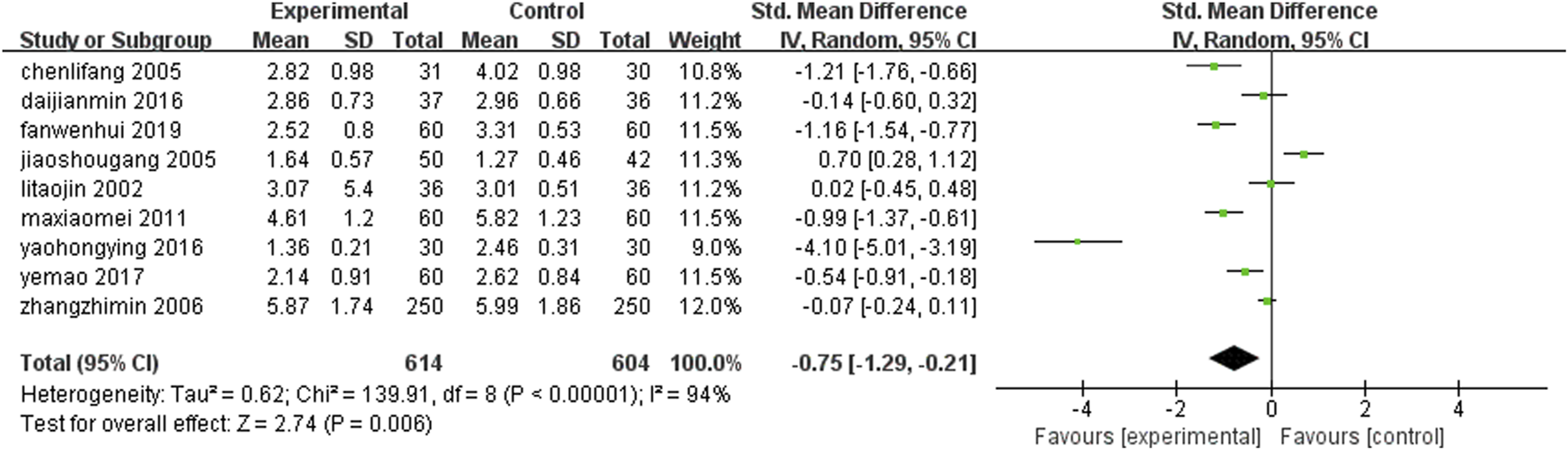
Leech combined with conventional treatment compared with conventional treatment alone for LDL.
3.4.12 Adverse reactions
Twenty six studies (Wu et al., 2001; Jian and Xudong, 2002; Taojin, 2002; Xianming et al., 2002; Haijie and Changshi, 2003; Junjiang et al., 2004; Shaohua, 2004; Lifang and Guofeng, 2005; Shougang, 2005; Xiaoyan and Bainian, 2006; Dongsheng and Jimin, 2008; Qingfan and Hezhong, 2008; Rongxing and Linlin, 2009; Shugang et al., 2009; Weidong and Lihua, 2009; Jun et al., 2011; Shaofeng and Xinfeng, 2011; Xiao-Mei, 2011; Jinbao et al., 2012; Wei et al., 2013; Yu, 2013; Hongying et al., 2015; Hongying et al., 2016; Jianmin et al., 2016; Mao and Qiang, 2017; Wenhui and Shiliang, 2019) (n = 2,406) reported the adverse reactions that occurred in the patients of each group after treatment. The number of adverse reactions and their symptoms are presented in Table 3. All adverse reactions were mild and resolved spontaneously after treatment. All adverse reactions were effectively managed through regular monitoring and appropriate intervention. The study found that compared with the group that only received conventional treatment, the incidence of adverse events in the group that received combined treatment with herbal medicine from earthworms did not significantly increase. The results of the meta-analysis showed that there was no statistically significant difference in the incidence of adverse reactions between the two groups [RD = 0.00, 95%CI (−0.01, 0.01), P = 0.90] (Figure 15).
TABLE 3
| Adverse reaction | |||
|---|---|---|---|
| Author | Year | Number | Symptoms |
| Yao hong ying | 2016 | 1 | Mild vomiting |
| Li hong ying | 2015 | 1 | Mild thirst |
| Ma xiao mei | 2011 | 3 | Slight headache |
| Liu cui xia | 2010 | 2 | Minor bleeding on the skin |
| Yuan shu gang | 2009 | 1 | Slight headache |
| Chen rong xing | 2009 | 1 | Gastric discomfort, relieved by eating |
| Yang xiao yan | 2006 | 1 | Gastric discomfort, relieved by eating |
| Fu jian | 2002 | 3 | Gastric discomfort, relieved by eating |
| Wang ling yun | 2001 | 1 | Gastrointestinal discomfort |
Adverse reaction symptom.
FIGURE 15
![Forest plot showing the risk difference with 95% confidence intervals for multiple studies. Each line represents a study, with a point estimate and horizontal line indicating the confidence interval. All studies except one favor neither the experimental nor control group significantly. The overall risk difference is -0.00 with a confidence interval of [-0.01, 0.01]. Total events are 1 for experimental and 9 for control. Heterogeneity statistics show no significant variation between studies.](https://www.frontiersin.org/files/Articles/1643611/xml-images/fphar-16-1643611-g015.webp)
Adverse reactions.
3.5 Subgroup analysis
Subgroup analyses were performed on specific outcomes based on two primary intervention factors: drug type and treatment duration. The results consistently demonstrated that the experimental treatment outperformed the control group. The overall pooled odds ratio for all treatment combinations across subgroups classified by drug type was 3.76 (95% CI: 3.08–4.60), indicating a robust and consistent effect of the experimental treatment across all subgroups. Similarly, the overall effect across all treatment durations in the subgroups stratified by treatment duration was 3.51 (95% CI: 3.02–4.08), suggesting that treatment duration did not significantly impact the results, with the experimental treatment remaining effective across various timeframes. Statistical significance was observed in all subgroups. The forest plots of the results are presented in Figures 16, 17.
FIGURE 16
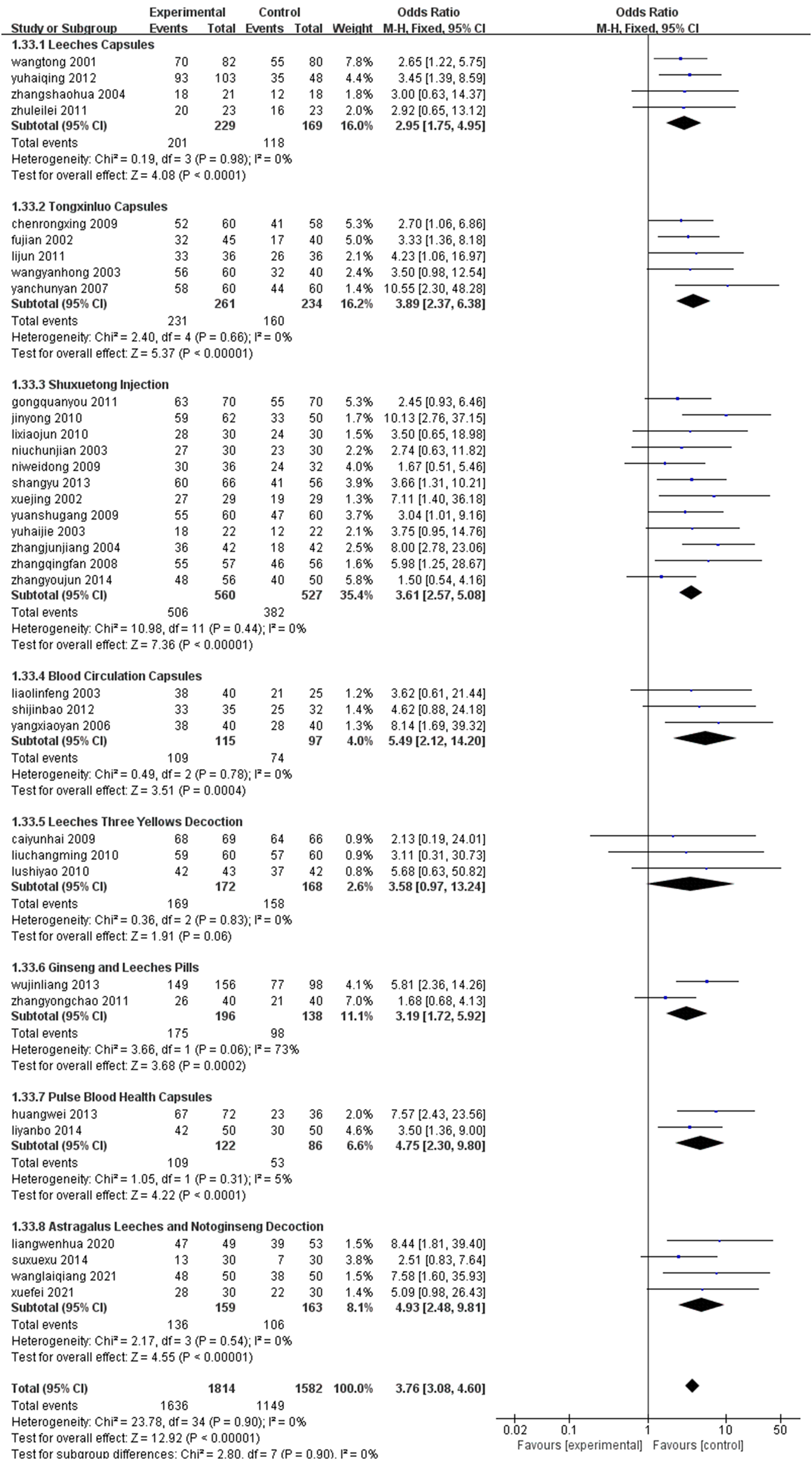
Drug classification grouping.
FIGURE 17
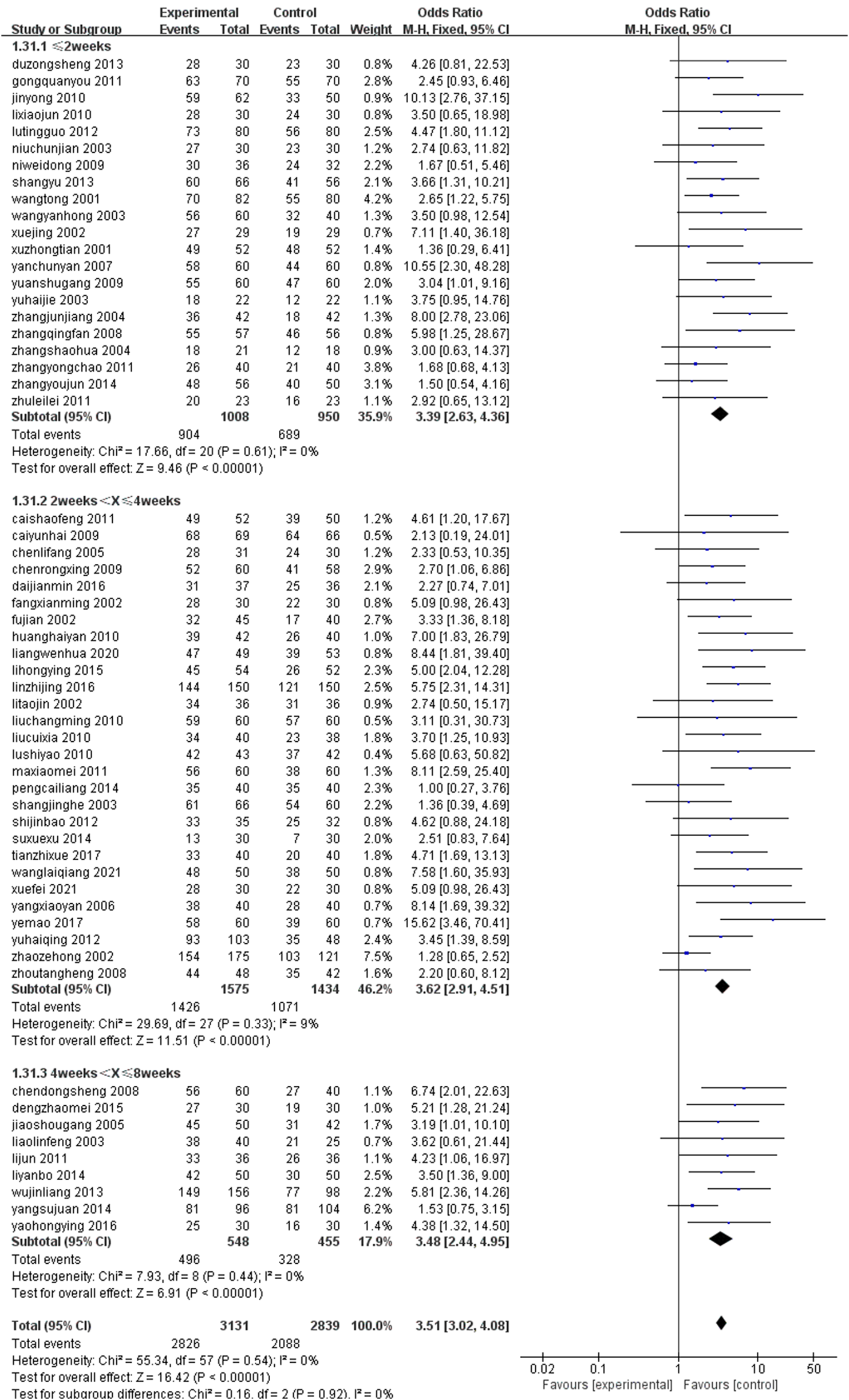
Treatment time grouping.
3.6 Publication bias analysis
The risk of publication bias was evaluated using funnel plots for the total effective rate and ECG efficacy of the primary outcome indicators, as shown in Figures 18, 19, respectively. It was observed that the scatter points of the funnel plot of the two outcome indicators were distributed above the horizontal axis, but the distribution was basically symmetrical, suggesting that there was no risk of publication bias.
FIGURE 18
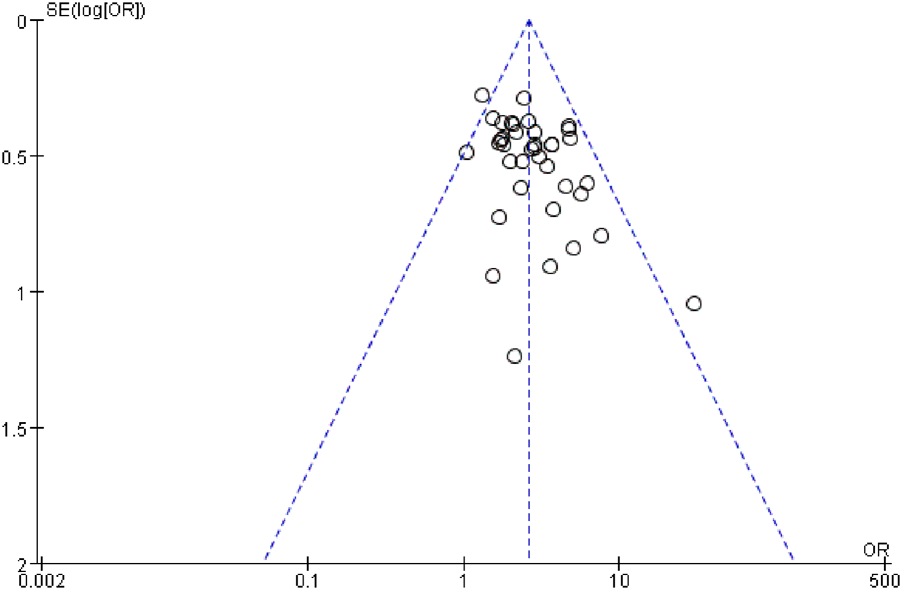
Funnel plot of total clinical response rate.
FIGURE 19
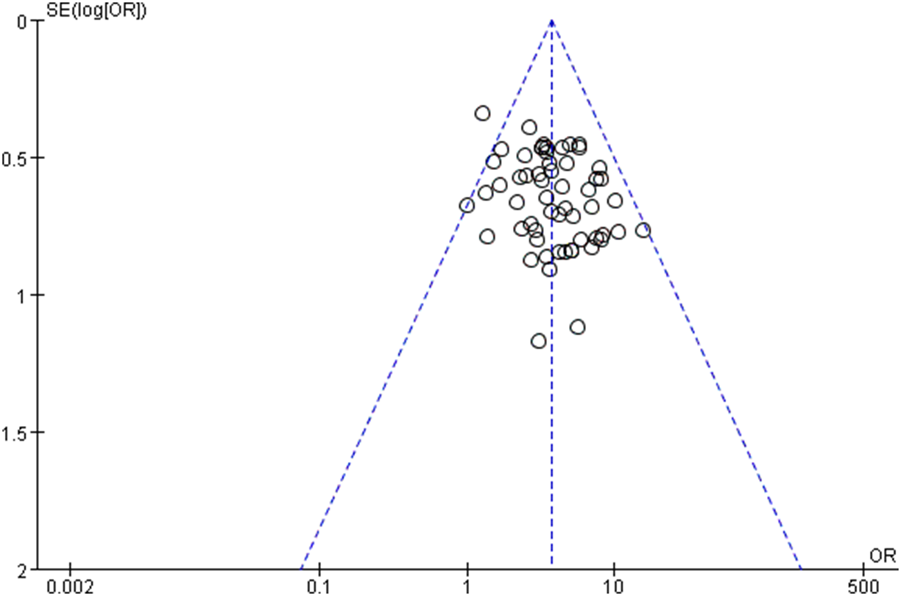
Funnel plot of ECG efficacy.
3.7 GRADE assessment
Using the GRADE approach, we conducted a certainty assessment for the primary outcome measures. For effective and ECG efficacy, the evidence was downgraded by one level due to serious concerns about risk of bias, resulting in moderate certainty of evidence (Table 4). For traditional Chinese medicine symptom efficacy, the evidence was rated as moderate certainty due to a high risk of bias. For the frequency of angina pectoris, the evidence was downgraded by two levels due to both a high risk of bias and publication bias, leading to low-certainty evidence (Table 5). For whole blood viscosity, plasma viscosity, and fibrinogen, some studies had limitations in clinical applicability, high uncertainty in results, and uncontrolled confounding factors, resulting in low-certainty evidence (Table 6). Regarding the biochemical indicator total cholesterol, although there were significant inconsistencies and precision issues, the risk of bias was low, and the evidence was rated as moderate certainty. For triglycerides, considering the substantial inconsistencies, precision issues, and the potential impact of residual confounding factors, the evidence was downgraded by two levels, ultimately rated as low certainty. For high-density lipoprotein (HDL), despite some inconsistencies and precision issues, the risk of bias was low, and the evidence was rated as moderate certainty. For low-density lipoprotein (LDL), due to severe inconsistencies, precision issues, and substantial publication bias, the evidence was downgraded by two levels, resulting in very low-certainty evidence (Table 7).
TABLE 4
| Certainty assessment | No. of patients | Effect | Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | New comparison | Placebo | Relative (95% CI) | Absolute (95% CI) | ||
| Effective | ||||||||||||
| 58 | Randomised trials | Serious | Not serious | Not serious | Not serious | None | 2922/3218 (90.8%) | 2096/2847 (73.6%) | OR 3.70 (3.19 to 4.31) | 175 more per 1,000 (from 163 more to 187 more) | ⨁⨁⨁○ Moderate | CRITICAL |
| Electrocardiogram efficacy | ||||||||||||
| 38 | Randomised trials | Serious | Not serious | Not serious | Not serious | None | 1795/2230 (80.5%) | 1224/1960 (62.4%) | OR 2.58 (2.23 to 2.99) | 186 more per 1,000 (from 163 more to 208 more) | ⨁⨁⨁○ Moderate | CRITICAL |
Effective and ECG efficacy assessment.
CI, confidence interval; MD, mean difference; OR, odds ratio.
TABLE 5
| Certainty assessment | No. of patients | Effect | Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | New comparison | Placebo | Relative (95% CI) | Absolute (95% CI) | ||
| Traditional Chinese medicine, Symptom, Efficacy (二) | ||||||||||||
| 3 | Randomised trials | Serious | Not serious | Not serious | Not serious | None | 136/147 (92.5%) | 112/146 (76.7%) | OR 3.75 (1.81 to 7.73) | 158 more per 1,000 (from 89 more to 195 more) | ⨁⨁⨁○ Moderate | IMPORTANT |
| Frequency of angina pectoris | ||||||||||||
| 9 | Randomised trials | Serious | Very serious | Not serious | Not serious | All plausible residual confounding would reduce the demonstrated effect | 559 | 553 | - | MD 1.14 lower (1.25 lower to 1.04 lower) | ⨁⨁○○ Low | IMPORTANT |
TCM symptoms and frequency of angina pectoris.
CI, confidence interval; MD, mean difference; OR, odds ratio
TABLE 6
| Certainty assessment | No. of patients | Effect | Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | New comparison | Placebo | Relative (95% CI) | Absolute (95% CI) | ||
| Whole blood viscosity | ||||||||||||
| 12 | Randomised trials | Not serious | Serious | Serious | Serious | All plausible residual confounding would reduce the demonstrated effect | 804 | 642 | - | MD 0.69 lower (0.73 lower to 0.64 lower) | ⨁⨁○○ Low | IMPORTANT |
| Plasma viscosity | ||||||||||||
| 12 | Randomised trials | Not serious | Serious | Not serious | Serious | None | 804 | 642 | - | MD 0.19 lower (0.22 lower to 0.17 lower) | ⨁⨁○○ Low | IMPORTANT |
| Fibrinogen | ||||||||||||
| 8 | Randomised trials | Not serious | Serious | Not serious | Serious | None | 497 | 412 | - | MD 0.63 lower (0.7 lower to 0.55 lower) | ⨁⨁○○ Low | IMPORTANT |
Whole blood viscosity, plasma viscosity, and fibrinogen.
CI, confidence interval; MD, mean difference; OR, odds ratio.
TABLE 7
| Certainty assessment | No. of patients | Effect | Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | New comparison | Placebo | Relative (95% CI) | Absolute (95% CI) | ||
| Total cholesterol | ||||||||||||
| 15 | Randomised trials | Not serious | Serious | Not serious | Serious | All plausible residual confounding would reduce the demonstrated effect | 966 | 892 | - | MD 0.79 lower (0.84 lower to 0.75 lower) | ⨁⨁⨁○ Moderate | IMPORTANT |
| Triglycerides | ||||||||||||
| 15 | randomised trials | not serious | very serious | not serious | serious | all plausible residual confounding would reduce the demonstrated effect | 966 | 892 | - | MD 0.62 lower (0.67 lower to 0.58 lower) | ⨁⨁○○ Low | IMPORTANT |
| High density lipoprotein | ||||||||||||
| 11 | Randomised trials | Not serious | Serious | Serious | Not serious | All plausible residual confounding would reduce the demonstrated effect | 837 | 763 | - | MD 0.11 higher (0.09 higher to 0.14 higher) | ⨁⨁⨁○ Moderate | IMPORTANT |
| Low density lipoprotein | ||||||||||||
| 9 | Randomised trials | Not serious | Very serious | Not serious | Serious | Publication bias strongly suspected all plausible residual confounding would reduce the demonstrated effect | 614 | 604 | - | MD 0.63 lower (0.71 lower to 0.54 lower) | ⨁○○○ Very low | IMPORTANT |
Total cholesterol triglycerides HDL and LDL.
4 Discussion
According to the results of this meta-analysis, Chinese patent medicine containing leech has shown clinical efficacy in the treatment of coronary heart disease, especially in improving the overall cure rate, abnormal electrocardiogram, hemorheology indexes and TCM symptom scores. The treatment group was superior to conventional western medicine in reducing the frequency of angina pectoris, improving the ischemic changes of electrocardiogram and regulating blood lipid levels. This may elucidate the effective effects of leech components on relieving angina pectoris and improving myocardial ischemia can be clarified.
The results of this meta-analysis show that leech-based treatments significantly improved the total effective rate and ECG outcomes in CHD patients. Specifically, the treatment group exhibited better clinical responses compared to those receiving only conventional treatments. This is crucial, as CHD patients typically suffer from ischemic changes reflected in abnormal ECG results (Albus et al., 2017; Su et al., 2023). The improvement in ECG outcomes suggests that hirudin play a role in mitigating myocardial ischemia. Hirudin, by inhibiting thrombin, directly reduces thrombosis and platelet aggregation, thereby enhancing coronary blood flow (Junren et al., 2021). This improvement likely contributes to the observed reduction in ischemic changes on the ECG.
Another critical finding is the significant reduction in the frequency of angina pectoris attacks in the treatment group, alongside improvements in hemorheological parameters whole blood and plasma viscosity. These results suggest that leech-based treatments contribute to better blood flow, particularly in coronary microcirculation. The reduction in blood viscosity, facilitated by hirudin’s anticoagulant properties, enhances tissue perfusion, ensuring that oxygen and nutrients reach ischemic myocardial tissue more efficiently. This is consistent with the known mechanisms of hirudin, which improves blood fluidity and prevents clot formation (Junren et al., 2021; Qiu et al., 2022), thus reducing the incidence of angina attacks and alleviating myocardial ischemia.
The meta-analysis also demonstrated significant improvements in lipid profiles, including reductions in total cholesterol, LDL, and triglycerides, along with a modest increase in HDL. These lipid changes are important for the long-term management of CHD, as they help slow the progression of atherosclerosis (Kamstrup, 2021; Shaya et al., 2022; Alloubani et al., 2021; Humm et al., 2023; Ueki et al., 2024) By improving lipid metabolism, substances in leeches may help stabilize atherosclerotic plaques, reducing the risk of plaque rupture and subsequent cardiovascular events. The observed lipid improvements may be attributed to the anti-inflammatory effects of leech components, which can reduce lipid oxidation and promote healthier vascular function.
The clinical benefits observed in this study are closely tied to the pharmacological properties ofsubstances in leeches. Hirudin, as a potent anticoagulant, plays a central role in preventing thrombus formation and improving blood flow (Junren et al., 2021). Its ability to reduce fibrinogen levels and enhance blood fluidity is crucial in alleviating myocardial ischemia. Moreover, the reduction in blood viscosity enhances coronary microcirculation, leading to better tissue perfusion and a reduction in ischemic damage to the heart (Del Buono et al., 2021).
Additionally, the improvement in lipid metabolism, evidenced by the decrease in LDL and increase in HDL, is likely due to the anti-inflammatory and antioxidant properties of leech components (Junren et al., 2021). These effects help reduce oxidative stress and inflammation, which are key factors in the progression of atherosclerosis (Kong et al., 2022; Attiq et al., 2024; Violi et al., 2024; Guo et al., 2024). Moreover, leech components’ ability to promote nitric oxide (NO) release by up-regulating endothelial nitric oxide synthase (eNOS) enhances vascular relaxation, improves coronary perfusion, and contributes to better endothelial function, all of which are essential for managing CHD (Junren et al., 2021; Jaishankar et al., 2023; Sun et al., 2025).
5 Limitation
This study has several limitations. Firstly, the quality of some of the included studies was relatively low, particularly regarding randomization, allocation concealment, and blinding, where descriptions were unclear, potentially compromising the reliability of the results. Secondly, some studies had small sample sizes and short follow-up durations, making it difficult to assess the long-term efficacy and safety of the treatment comprehensively. Additionally, there was heterogeneity in the treatment protocols and traditional Chinese medicine formulas used, which could contribute to variations in the results and limit the ability to assess the efficacy of individual treatment plans clearly. Moreover, most of the studies included in this analysis were conducted in China, with the majority of the literature being in Chinese, which may introduce regional and cultural biases, thereby limiting the generalizability of the findings. Despite conducting a thorough literature search, there is still the possibility of publication bias, particularly with respect to the underreporting of negative results. Finally, the existing studies do not provide an in-depth exploration of the specific mechanisms of action of the leech-derived components, the mechanism by which hirudin exerts its effects through improving endothelial function, nitric oxide production, and regulating inflammatory responses is primarily based on existing pharmacological research and theoretical speculation, rather than being directly supported by the clinical data from this study, preventing a full understanding of their precise role in treating coronary heart disease. Special attention must be given to the potential interaction between bioactive components extracted from leeches and conventional anticoagulant or cardiovascular medications. While the therapeutic benefits of leech extracts are evident, combining these extracts with other medications requires careful monitoring of bleeding risks in patients. Some patients may have a history of prior medications or multiple comorbidities, which could influence treatment outcomes. Due to the design and scope of the current study, these factors were not fully accounted for. Although we evaluated several alternative biomarkers in this study, which provide valuable insights into biological effects, it is important to emphasize that these biomarkers cannot directly demonstrate clinical benefit. While they may reflect underlying biological mechanisms or the impact of therapeutic interventions, they are not equivalent to clinical endpoints, such as myocardial infarction, mortality, or quality of life, which are the critical measures for determining the clinical significance of a treatment. Therefore, although alternative biomarkers can serve as useful early predictors, they cannot fully substitute for definitive clinical outcomes. Future research should focus on further exploring these mechanisms, prioritizing clinical endpoints, validating the relationship between alternative biomarkers and actual clinical benefits, and assessing treatment efficacy across diverse patient populations and coronary artery disease subtypes to provide more precise clinical guidance.
6 Conclusion
The results of this meta-analysis show that the Chinese patent medicine containing leech has good clinical efficacy in the treatment of coronary heart disease, which can significantly improve the symptoms, electrocardiogram performance and hemorheological indicators of patients, and has high safety. Its multi-target and synergistic mechanism provide a potentially effective TCM treatment for CHD.
Although this study has a certain clinical guiding significance, due to the low quality of some included studies, more high-quality, large sample and long-term follow-up randomized controlled trials are still needed to further verify its efficacy and safety, and clarify its mechanism of action, optimal treatment regimen and applicable population. In general, the potential of Chinese patent medicine containing leech in the comprehensive treatment of coronary heart disease is worthy of further research and application.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
ZZ: Data curation, Software, Writing – original draft, Writing – review and editing, Formal Analysis. DY: Investigation, Writing – review and editing, Formal Analysis, Data curation, Writing – original draft. ML: Validation, Writing – review and editing, Data curation, Investigation. YJ: Investigation, Writing – review and editing, Formal Analysis. JZ: Supervision, Funding acquisition, Resources, Writing – review and editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was funded by the National Natural Science Foundation of China (grant number 82160875), District Natural Science Research Fund (2022JJD140107), Zheng Jinghui - Academic Affairs Office - Fifth Batch of National Outstanding Traditional Chinese Medicine Clinical Talent Cultivation Program (grant number 06F24006) and Guangxi First-Class Discipline Construction Project (Gui Jiao Ke Yan [2022] No. 1).
Acknowledgments
Thanks to all authors for their valuable contributions to this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2025.1643611/full#supplementary-material
Abbreviations
CHD, Coronary heart disease; CNKI, China National Knowledge Infrastructure; VIP, VIP China Science and Technology Journal Database; RCTs, Randomized controlled trials; SMD, Standardized Mean Difference; CI, Confidence intervals; OR, Odds Ratio; TCM, Traditional Chinese medicine; RD, Relative risk difference; MD, Mean difference.
References
1
Albus C. Barkhausen J. Fleck E. Haasenritter J. Lindner O. Silber S. (2017). The diagnosis of chronic coronary heart disease. Dtsch. Arzteblatt Int.114 (42), 712–719. 10.3238/arztebl.2017.0712
2
Alloubani A. Nimer R. Samara R. (2021). Relationship between hyperlipidemia, cardiovascular disease and stroke: a Systematic Review. Curr. Cardiol. Rev.17 (6), e051121189015. 10.2174/1573403x16999201210200342
3
Attiq A. Afzal S. Ahmad W. Kandeel M. (2024). Hegemony of inflammation in atherosclerosis and coronary artery disease. Eur. J. Pharmacol.966, 176338. 10.1016/j.ejphar.2024.176338
4
Cailiang P. Songshan G. Ning J. (2014). Clinical observation on the treatment of stable angina pectoris with astragalus capsule. Heilongjiang J. Traditional Chin. Med.43 (5), 19–20.
5
Changming L. (2010). 120 cases of coronary heart disease treated with leech and sanhuang tang. Guangming J. Chin. Med.25 (09), 1625–1626. 10.3969/j.issn.1003-8914.2010.09.045
6
Chunjian N. Xiaobing W. Tianyu G. (2003). Clinical observation on the treatment of unstable angina pectoris with blood-sparing injection solution. Nei Mongol J. Traditional Chin. Med. (S1), 4. 10.16040/j.cnki.cn15-1101.2003.s1.003
7
Chunmiao Y. Yuan L. Yongqing Z. Qiu J. Lingna W. (2024). Herbal textual research on hirudo. Chin. J. Mod. Appl. Pharm.41 (19), 2648–2657. 10.13748/j.cnki.issn1007-7693.20230875
8
Chunyan Y. (2007). Clinical observation of Tongxinluo in the treatment of angina pectoris of coronary heart disease. Pract. J. Cardiac Cereb. Pneumal Vasc. Dis.15 (3), 217–218. 10.3969/j.issn.1008-5971.2007.03.020
9
Cuixia L. Cunji F. (2010). Therapeutic efficacy of leech and blood stasis-expelling soup in the treatment of unstable angina pectoris. China Pract. Med.5 (05), 137–138. 10.14163/j.cnki.11-5547/r.2010.05.019
10
Del Buono M. G. Montone R. A. Camilli M. Carbone S. Narula J. Lavie C. J. et al (2021). Coronary microvascular dysfunction across the spectrum of cardiovascular diseases: JACC State-of-the-Art Review. J. Am. Coll. Cardiol.78 (13), 1352–1371. 10.1016/j.jacc.2021.07.042
11
Dongsheng C. Jimin M. (2008). Clinical observation on the treatment of angina pectoris in coronary heart disease by Long Hirudan. Hubei J. Traditional Chin. Med.30 (11), 27–28. 10.3969/j.issn.1000-0704.2008.11.015
12
Fei X. (2021). Effect of Qizhi Sanqi Decoction on the treatment of stable angina pectoris due to coronary heart disease with Qi-deficiency and blood-stasis syndrome. China Pract. Med.16 (30), 142–144. 10.14163/j.cnki.11-5547/r.2021.30.056
13
Guo Z. Yang Z. Song Z. Li Z. Xiao Y. Zhang Y. et al (2024). Inflammation and coronary microvascular disease: relationship, mechanism and treatment. Front. Cardiovasc. Med.11, 1280734. 10.3389/fcvm.2024.1280734
14
Haijie Y. Changshi L. (2003). Observations on the efficacy of blood-sparing in the treatment of unstable angina pectoris. Pract. J. Rural Dr.10 (04), 30. 10.3969/j.issn.1672-7185.2003.04.026
15
Haiqing Y. (2012). Compound leech capsule in the treatment of angina pectoris of coronary heart disease in 112 cases. Guangming J. Chin. Med.27 (11), 2228–2229. 10.3969/j.issn.1003-8914.2012.11.038
16
Haiyan H. (2010). Clinical observation on the treatment of angina pectoris of coronary heart disease with self-proposed ginseng and leech soup. J. Liaoning Universtity Traditional Chin. Med.12 (04), 154–155. 10.13194/j.jlunivtcm.2010.04.156.huanghy.064
17
Hongying L. Shaojun C. Jing Y. Yong C. Youhe M. (2015). Observation on the efficacy of Astragalus Ginseng and Dan Hirudin Tang in the treatment of unstable angina pectoris. J. Emerg. Traditional Chin. Med.24 (3), 509–511. 10.3969/j.issn.1004-745X.2015.03.050
18
Hongying Y. Zhaoping W. Hongmin S. Fang L. Wei L. (2016). Study on the efficacy and safety of Vermicelli and Snake Tongluo Capsules in the treatment of coronary heart disease. Word Latest Med. Inf.16 (79), 174–74. 10.3969/j.issn.1671-3141.2016.79.145
19
Hummelgaard S. Vilstrup J. P. Gustafsen C. Glerup S. Weyer K. (2023). Targeting PCSK9 to tackle cardiovascular disease. Pharmacol. Ther.249, 108480. 10.1016/j.pharmthera.2023.108480
20
Jaishankar T. Shivasekar M. Vinodhini V. M. (2023). Endothelial nitric oxide synthase T-786C and G-894T gene polymorphisms: a risk assessment of coronary heart disease. J. Assoc. Physicians India71 (9), 45–50. 10.59556/japi.71.0294
21
Jian F. Xudong L. (2002). Observation on the efficacy of Tongxinluo capsule in the treatment of angina pectoris of coronary heart disease. Acta Acad. Med. Jiangxi42 (6), 55. 10.3969/j.issn.1000-2294.2002.06.033
22
Jianmin D. Rong Y. F. Yurong X. Jinghua F. Sui X. Zhe Y. (2016). Effect analysis of Qizhi Tongmai granule in the treatment of coronary heart disease in a multicenter trail. World Clin. Drugs37 (5), 324–327. 10.13683/j.wph.2016.05.008
23
Jinbao S. Fang L. Huikang H. (2012). Clinical efficacy observation on the treatment of unstable angina pectoris by blood circulation and pulse circulation capsule. Chin. J. Geriatric Care10 (4), 23–25. 10.3969/j.issn.1672-4860.2012.04.009
24
Jing X. Ming G. Dan C. Xin L. (2002). Clinical observation on the treatment of unstable angina pectoris with blood-sparing injection solution. Clin. Focus17 (06), 338–339. 10.3969/j.issn.1004-583X.2002.06.022
25
Jinghe S. (2003). Clinical observations on effect of Qishen Capsules on angina pectoris. Chin. Tradit. Pat. Med.25 (4), 303–304. 10.3969/j.issn.1001-1528.2003.04.014
26
Jinliang W. Yunyi Z. (2013). Observations on the clinical application of Ginseng Hirudo Pill in the treatment of 156 cases of coronary heart disease angina pectoris of the silt-blood paralysis-obstruction type. Chin. Foreign Med. Res.11 (3), 39. 10.14033/j.cnki.cfmr.2013.03.008
27
Jun L. Xiangyun L. Lei Z. (2011). Analysis of the efficacy of Tongxinluo capsule in the treatment of coronary heart disease chronic heart failure. Hebei Med. J.33 (12), 1892–1893. 10.3969/j.issn.1002-7386.2011.12.085
28
Junjiang Z. Qingxiang D. Aiqing L. (2004). Clinical observation of coronary heart disease unstable angina pectoris treated by Shu-xue-tong Injection. Pract. Clin. J. Integr. Traditional Chin. West. Med.04 (06), 15–16. 10.3969/j.issn.1671-4040.2004.06.010
29
Junren C. Xiaofang X. Huiqiong Z. Gangmin L. Yanpeng Y. Xiaoyu C. et al (2021). Pharmacological activities and mechanisms of hirudin and its derivatives - a Review. Front. Pharmacol.12, 660757. 10.3389/fphar.2021.660757
30
Kamstrup P. R. (2021). Lipoprotein(a) and cardiovascular disease. Clin. Chem.67 (1), 154–166. 10.1093/clinchem/hvaa247
31
Katta N. Loethen T. Lavie C. J. Alpert M. A. (2021). Obesity and coronary heart disease: epidemiology, pathology, and coronary artery imaging. Curr. Problems Cardiol.46 (3), 100655. 10.1016/j.cpcardiol.2020.100655
32
Kong P. Cui Z. Y. Huang X. F. Zhang D. D. Guo R. J. Han M. (2022). Inflammation and atherosclerosis: signaling pathways and therapeutic intervention. Signal Transduct. Target. Ther.7 (1), 131. 10.1038/s41392-022-00955-7
33
Laiqiang W. (2021). Efficacy of astragalus vermicularis and panax ginseng soup in the treatment of qi deficiency and blood stasis in stable angina pectoris of coronary heart disease. Psychol. Mag.16 (12), 80–176. 10.19738/j.cnki.psy.2021.12.039
34
Leilei Z. (2011). Clinical observation on the treatment of angina pectoris of coronary heart disease by compound hirudin essence capsule. J. Guiyang Coll. Traditional Chin. Med.33 (06), 86–87. 10.3969/j.issn.1002-1108.2011.06.44
35
Lemke S. Vilcinskas A. (2020). European medicinal leeches-new roles in modern medicine. Biomedicines8 (5), 99. 10.3390/biomedicines8050099
36
Lifang C. Guofeng J. (2005). Clinical observation on the treatment of unstable angina pectoris by leech Ding Yu Si Shen San. J. Emerg. Traditional Chin. Med.14 (09), 817–818. 10.3969/j.issn.1004-745X.2005.09.005
37
Linfeng L. (2003). Observation on the efficacy of blood circulation and blood circulation capsule in the treatment of angina pectoris of coronary heart disease. J. Emerg. Traditional Chin. Med.12 (04), 298–299. 10.3969/j.issn.1004-745X.2003.04.006
38
Mao Y. Qiang Z. (2017). Clinical analysis of red hirudin in the treatment of unstable angina pectoris. J. Pract. Traditional Chin. Med.33 (10), 1116–1118. 10.3969/j.issn.1004-2814.2017.10.002
39
Mao P. Liu X. Weng Y. Tang L. Tang Y. (2021). Clinical efficacy of aspirin combination treatment in the treatment of coronary heart disease and its effect on inflammatory factors: a systematic review and meta-analysis. Ann. Palliat. Med.10 (8), 8858–8868. 10.21037/apm-21-1648
40
Passacquale G. Sharma P. Perera D. Ferro A. (2022). Antiplatelet therapy in cardiovascular disease: current status and future directions. Br. J. Clin. Pharmacol.88 (6), 2686–2699. 10.1111/bcp.15221
41
Pothineni N. V. K. Subramany S. Kuriakose K. Shirazi L. F. Romeo F. Shah P. K. et al (2017). Infections, atherosclerosis, and coronary heart disease. Eur. heart J.38 (43), 3195–3201. 10.1093/eurheartj/ehx362
42
Qingfan Z. Hezhong X. (2008). Therapeutic efficacy of blood-sparing in the treatment of unstable angina pectoris observed. J. Med. Forum29 (11), 74–75. 10.3969/j.issn.1672-3422.2008.11.045
43
Qiu J. Ling-Na W. Qian L. Chun-Miao Y. Yong-Qing Z. (2022). Research progress on processing history evolution, chemical constituents, and pharmacological effects of hirudo. China J. Chin. Materia Medica47 (21), 5806–5816. 10.19540/j.cnki.cjcmm.20220411.201
44
Quanyou G. (2011). Observations on the clinical effect of blood-sparing in the treatment of unstable angina pectoris. Contemp. Med.17 (06), 61–62. 10.3969/j.issn.1009-4393.2011.6.044
45
Rongxing C. Linlin L. (2009). Interventional effect of Tongxinluo capsule on unstable angina pectoris. Guizhou Med. J.33 (10), 923–924. 10.3969/j.issn.1000-744X.2009.10.030
46
Shan-Shan L. Lu H. (2022). Pharmaceutical care for a patient with statin intolerant familial hypercholesterolemia by lipid-lowering strategy. Cent. South Pharm.20 (01), 209–213.
47
Shaofeng C. Xinfeng Z. (2011). Clinical observation on the treatment of stable angina pectoris with ginseng descending soup. Shanxi Med. J.40 (10), 1012–1013. 10.3969/j.issn.0253-9926-B.2011.10.030
48
Shaohua Z. (2004). Clinical study on the treatment of unstable angina pectoris with leech capsule. J. Sichuan Traditional Chin. Med.22 (04), 34–35. 10.3969/j.issn.1000-3649.2004.04.020
49
Shaya G. E. Leucker T. M. Jones S. R. Martin S. S. Toth P. P. (2022). Coronary heart disease risk: low-density lipoprotein and beyond. Trends Cardiovasc. Med.32 (4), 181–194. 10.1016/j.tcm.2021.04.002
50
Shiyao L. (2010). Treatment of coronary heart disease with leech and sanshuang tang. China Pract. Med.5 (25), 148–149. 10.3969/j.issn.1673-7555.2010.25.118
51
Shougang J. (2005). Clinical observation on the treatment of 50 cases of lability angina pectoris of coronary heart disease with ShenzhiHuoxue Decoction. Guid. J. TCM11 (5), 8–10. 10.3969/j.issn.1672-951X.2005.05.004
52
Shugang Y. Yingxuan G. Guohua Y. (2009). Observation of effect of Shuxuetong Injection in treatment of unstable angina pectoris. Med. World11 (10), 590–591.
53
Su W. Song S. Dong H. Wu H. Meng Z. (2023). Identifying and comparing low-value care recommendations for coronary heart disease prevention, diagnosis, and treatment in the US and China. Int. J. Cardiol.374, 1–5. 10.1016/j.ijcard.2022.12.031
54
Sujuan Y. Haijun G. (2004). 120 cases of coronary heart disease angina pectoris treated with Shu Xin Tong Paralysis Tang. Shaanxi J. Traditional Chin. Med.25 (07), 586–587. 10.3969/j.issn.1000-7369.2004.07.006
55
Sujuan Y. Wang F. Lu H. Guofang D. Yinna W. (2014). Observation on the therapeutic effect of 200 cases of angina pectoris in coronary heart disease treated with cardiac pain relief capsule. Chin. J. Integr. Med. Cardio/Cerebrovascular Dis.2 (13), 190–191. 10.16282/j.cnki.cn11-9336/r.2014.13.005
56
Sun W. T. Du J. Y. Wang J. Wang Y. L. Dong E. D. (2025). Potential preservative mechanisms of cardiac rehabilitation pathways on endothelial function in coronary heart disease. Sci. China. Life Sci.68 (1), 158–175. 10.1007/s11427-024-2656-6
57
Tangheng Z. (2008). Observation on the therapeutic effect of fu zheng resolving phlegm and dispelling blood stasis soup in the treatment of angina pectoris of coronary heart disease. Chin. Med. Mod. Distance Educ. China06 (07), 679–680. 10.3969/j.issn.1672-2779.2008.07.034
58
Taojin L. (2002). Clinical observation on treatment of angina pectoris in coronary heart disease with chrysanthemum and leech soup. Chin. J. Inf. Traditional Chin. Med.9 (08), 7–10. 10.3969/j.issn.1005-5304.2002.08.004
59
Tingguo L. Jun C. Junxiang L. (2012). Observation on the clinical efficacy of Yiqi, Blood-breaking and Vein-passing Soup in the treatment of angina pectoris of coronary heart disease. Chin. Community Dr.14 (18), 245–246. 10.3969/j.issn.1007-614x.2012.18.223
60
Tong W. Ying S. Guojie H. Liyan L. Hua G. Qingkai W. et al (2001). Therapeutic effect of leech capsule with compound danshen and astragalus in the treatment of unstable angina pectoris observed. Bull. Med. Res.30 (03), 56–57. 10.3969/j.issn.1673-548X.2001.03.031
61
Ueki Y. Itagaki T. Kuwahara K. (2024). Lipid-lowering therapy and coronary plaque regression. J. Atheroscler. Thrombosis.31 (11), 1479–1495. 10.5551/jat.RV22024
62
Violi F. Pignatelli P. Valeriani E. (2024). Oxidative stress and atherosclerosis: basic and clinical open issues. Kardiologia Pol.82 (7-8), 689–691. 10.33963/v.phj.100994
63
Wei H. Bihua Z. Suqiang G. (2013). The clinical effects of Maixuekang capsule on coronary heart disease angina pectoris. China Med.8 (8), 1051–1052. 10.3760/cma.j.issn.1673-4777.2013.08.005
64
Weidong N. Lihua G. (2009). Observation of effect of Shuxuetong Injection in treatment of angina pectoris. Med. World11 (12), 790–791.
65
Wenhua L. Wei Z. Gaoqiao S. Shasha X. Yang Z. (2020). Study on the effect and mechanism of Astragalus membranaceus-leech-pseudo ginseng soup on unstable angina pectoris patients with qi deficiency and phlegm stasis type. Prog. Mod. Biomed.20 (12), 2396–2400. 10.13241/j.cnki.pmb.2020.12.043
66
Wenhui F. Shiliang Z. (2019). Clinical efficacy of ginseng vermiculite heart capsule in the adjuvant treatment of stable angina pectoris with qi deficiency and blood stasis and its mechanism. Shandong Med. J.59 (14), 65–68. 10.3969/j.issn.1002-266X.2019.14.019
67
Wu L. Gong Y. Wang X. (2001). Clinical observation on the treatment of angina pectoris in coronary heart disease with thrombus cardiac venous capsule. Heilongjiang Yixue25 (11), 827.
68
Wu S. Zhou Y. Wang Y. Zhang Z. (2024). Therapeutic potentials of medicinal leech in Chinese Medicine. Am. J. Chin. Med.52 (4), 1027–1051. 10.1142/s0192415x24500423
69
Xianming F. Liuhua X. Jianshe Y. (2002). Treatment of coronary heart disease stabilized angina pectoris in 30 cases with Yixinwei granules. Shaanxi J. Traditional Chin. Med.23 (12), 1092–1093. 10.3969/j.issn.1000-7369.2002.12.029
70
Xiao-Mei M. (2011). Efficacy observation of zhidan xiaozhi decoction in 60 cases of coronary heart disease of qi and blood stagnation pattern and internal retention of phlegm damp pattern. World J. Integr. Traditional West. Med.6 (7), 590–597. 10.3969/j.issn.1673-6613.2011.07.014
71
Xiaojun L. (2010). Analysis of 30 cases of unstable angina pectoris treated with blood-sparing injection. Chin. J. Coal Industry Med.13 (03), 423.
72
Xiaoyan Y. Bainian G. (2006). Observation on the therapeutic effect of 40 cases of coronary heart disease treated with blood circulation and blood circulation capsule. Tianjin Med. J.34 (5), 347–348. 10.3969/j.issn.0253-9896.2006.05.028
73
Xin L. Xinyi O. Yanhong W. Yang L. Haoxuan Z. Li Z. et al (2023). Effects of different lipid-lowering treatments on ischemic stroke patients with statin intolerance. J. Med. Res. and Combat Trauma Care36 (05), 473–478. 10.16571/j.cnki.2097-2768.2023.05.005
74
Xinnian L. Lu L. (2012). Treatment of coronary heart disease and angina pectoris with senxiong hirubai granules in 31 cases. Chin. Med. Mod. Distance Educ. China10 (7), 27–28. 10.3969/j.issn.1672-2779.2012.07.015
75
Xuexu S. Li C. Xiuyan Z. (2014). Clinical efficacy of Astragalus Vermiculosus Sanqi Tang in the treatment of stable angina pectoris. China Health Care Nutr. (4), 104–105.
76
Yanbo L. (2014). Observation on the therapeutic effect of Pulse Blood Kang Capsules in treating coronary heart disease angina in middle-aged and old-aged people. Chin. J. Integr. Med. Cardio/Cerebrovascular Dis.12 (03), 302. 10.3969/j.issn.1672-1349.2014.03.025
77
Yanhong W. Huixia J. Xiaodong L. (2003). Coronary heart disease of unstable type treated by Tongxinluo Capsule. Shaanxi J. Traditional Chin. Med.24 (08), 676–678. 10.3969/j.issn.1000-7369.2003.08.002
78
Yong J. (2010). Analysis of therapeutic efficacy of shuoxiantong in treating unstable angina pectoris in the elderly. Chin. J. Misdiagnostics10 (25), 6083–83.
79
Yongchao Z. Chunyi Y. Guoxing G. (2011). Treatment of angina pectoris of coronary heart disease with Shen hirudo pill in 40 cases. Chin. Med. Mod. Distance Educ. China9 (22), 13–14. 10.3969/j.issn.1672-2779.2011.22.007
80
Youjun Z. (2014). Clinical observation of Shu Xue Tong injection in the treatment of 56 patients with coronary heart disease. Chin. Community Dr.30 (32), 82–84. 10.3969/j.issn.1007-614x.2014.32.49
81
Yu S. (2013). Clinical observation on the treatment of unstable angina pectoris in the elderly with blood-sparing injection solution. Contin. Med. Educ.27 (03), 51–52+65. 10.3969/J.ISSN.1004-6763.2013.03.016
82
Yunhai C. (2009). Treatment of coronary heart disease with leech and sanshuang tang. Guangming J. Chin. Med.24 (06), 1081–1083. 10.3969/j.issn.1003-8914.2009.06.054
83
Yuxia Z. Jing Y. Zhonghua C. (2002). Effects of quyu xiaoban Capsule on blood lipid Level and platelet activity in coronary heart disease. J. Guangzhou Univ. Traditional Chin. Med.19 (3), 172–174. 10.3969/j.issn.1007-3213.2002.03.003
84
Zehong Z. Zuyun Z. Linxiang F. Mingxiang H. Jingyuan L. Weidong O. et al (2002). Effect of buxin huoluo capsule for coronary heart disease and its anti-lipid-peroxidation mechanism. J. Guangzhou Univ. Traditional Chin. Med.19 (2), 85–87. 10.3969/j.issn.1007-3213.2002.02.001
85
Zhang X. Yan Q. Jiang J. Luo H. Ren Y. (2024). Safety and efficacy of aspirin and indobufen in the treatment of coronary heart disease: a systematic review and meta-analysis. Front. Cardiovasc. Med.11, 1412944. 10.3389/fcvm.2024.1412944
86
Zhaomei D. Lian X. (2015). Clinical study on the treatment of stable angina pectoris with qi deficiency and blood stasis by astragalus vermicularis and saffron soup. Chin. J. Integr. Med. Cardio/Cerebrovascular Dis.13 (1), 95–96. 10.3969/j.issn.16721349.2015.01.035
87
Zhi-Min Z. Yan-Xia G. Huai-Lin L. Yi-Qiang Y. Li Y. (2006). Wentongjian in prevented coronary restenosis of percutaneous coronary intervention. Chin. J. Arteriosclerosis14 (7), 610–612. 10.3969/j.issn.1007-3949.2006.07.016
88
Zhijing L. Shufeng H. Yingchun L. Xiaojuan S. Ruiling M. Jinchun S. et al (2016). Dialectical treatment of angina pectoris in coronary heart disease by Shandan Guanxin group formulae. Word Latest Med. Inf.16 (41), 152–153. 10.3969/j.issn.1671-3141.2016.41.121
89
Zhixue T. Baicheng Q. Baoliang W. (2017). Clinical study of yiqi huayu decoction in treatment of coronary heart disease angina pectoris with phlegm and blood stasis syndrome China. J. Chin. Med.32 (7), 1251–1253. 10.16368/j.issn.1674-8999.2017.07.329
90
Zhongtian X. Rihui D. (2001). Efficacy observation of 52 cases of unstable angina pectoris treated with self-proposed piper betel vermicompost soup. Clin. J. Traditional Chin. Med.13 (1), 34–35. 10.3969/j.issn.1672-7134.2001.01.018
91
Zongsheng D. (2013). Clinical observation on the treatment of unstable angina pectoris with blood stasis and paralysis closure by leech and safflower soup. Hubei J. Traditional Chin. Med.35 (03), 37–38. 10.3969/j.issn.1000-0704.2013.03.017
Summary
Keywords
coronary heart disease, leech, Chinese herbal medicine, meta-analysis, systematic review
Citation
Ziyuan Z, Di Y, Mei L, Yujing J and Jinghui Z (2025) The clinical efficacy of herbal medicines containing leeches in the treatment of coronary heart disease: a systematic review and meta-analysis. Front. Pharmacol. 16:1643611. doi: 10.3389/fphar.2025.1643611
Received
10 June 2025
Accepted
12 September 2025
Published
17 October 2025
Volume
16 - 2025
Edited by
Javier Echeverria, University of Santiago, Chile
Reviewed by
Mohammed Ahmed Akkaif, QingPu Branch of Zhongshan Hospital Affiliated to Fudan University, China
Sachinkumar Gunjal, Amrutvahini College of Pharmacy, India
Updates
Copyright
© 2025 Ziyuan, Di, Mei, Yujing and Jinghui.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zheng Jinghui, jinghuizheng@yeah.net
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.