- 1Psychiatry Department, School of Medicine, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
- 2Psychiatry Department, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
- 3College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- 4Department of Psychiatry, College of Medicine and Health Sciences, Dilla University, Dilla, Dilla, Ethiopia
Background: Post-traumatic stress disorder (PTSD) occurs after exposure to actual or threatened death, serious injury, or sexual violence. Road traffic accident (RTA) is one of the traumatic experiences, which may result in PTSD. But treatment is mainly concentrated on physical health. This may be due to a lack of evidence in low-income countries.
Aim: To determine the incidence level and identify risk factors of PTSD after RTA.
Methods: Longitudinal panel study was done to assess the incidence of PTSD after RTA. The study was conducted in three orthopedic settings of Bahir Dar town Northwest, Ethiopia. The study was on 299 adult car accident survivors. PTSD Checklist (PCL) civilian version, Sheehan disability assessment scale, Patient Health Question (PHQ-2), and Alcohol Use Disorder Identification Test (AUDIT) were instruments to assess the outcome and associated factors. The generalized linear model with Poisson log-linear method was applied to identify associated factors. Ethical clearance was obtained from Bahir Dar University. Individuals with PTSD symptoms were linked to the psychiatric clinic.
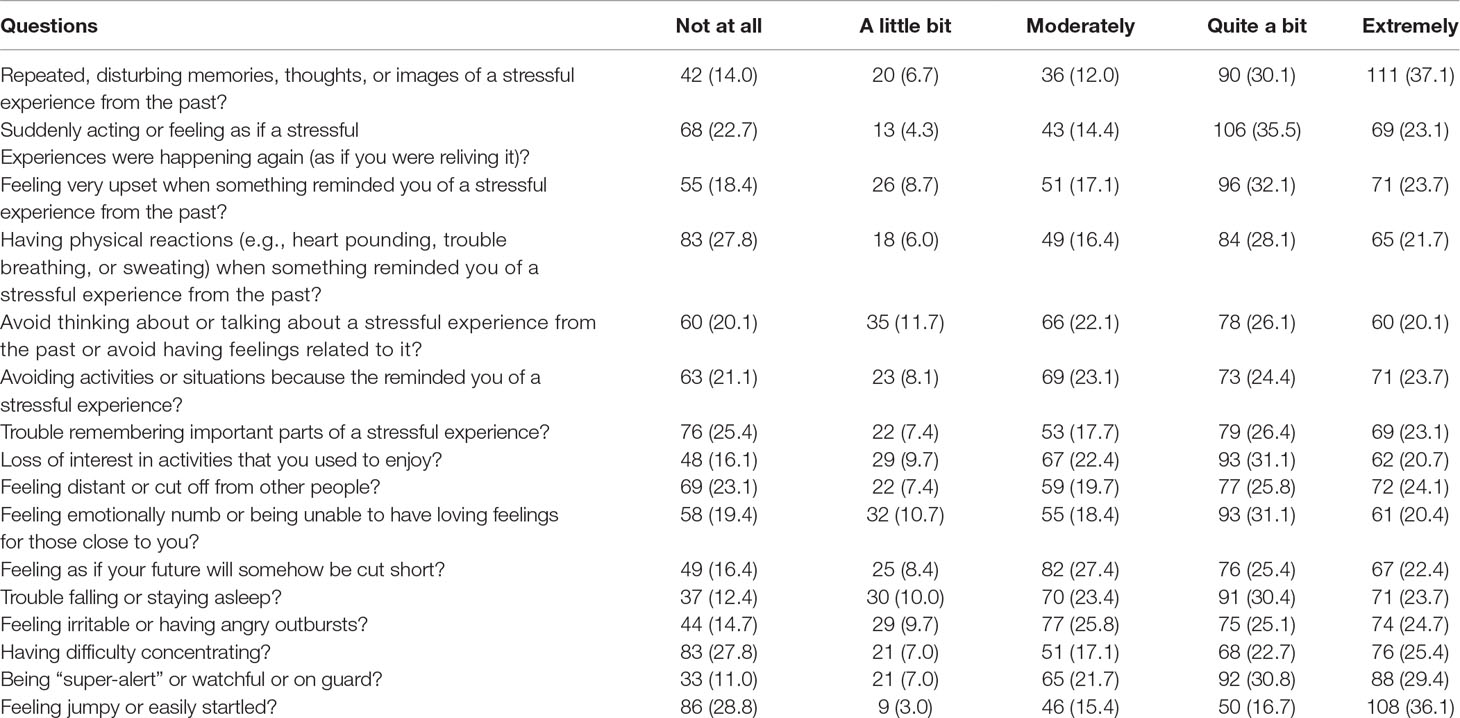
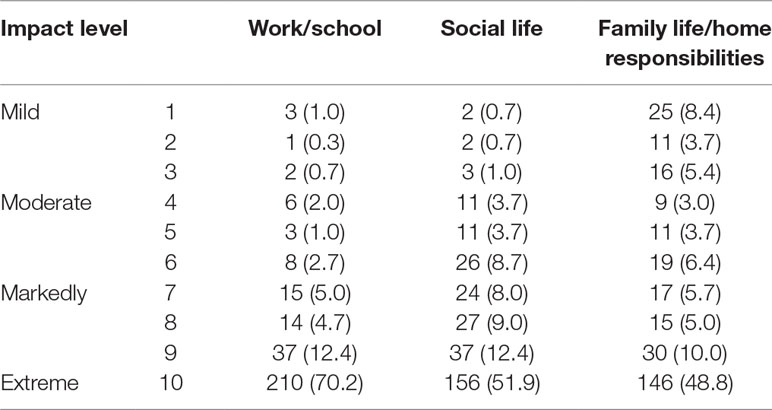
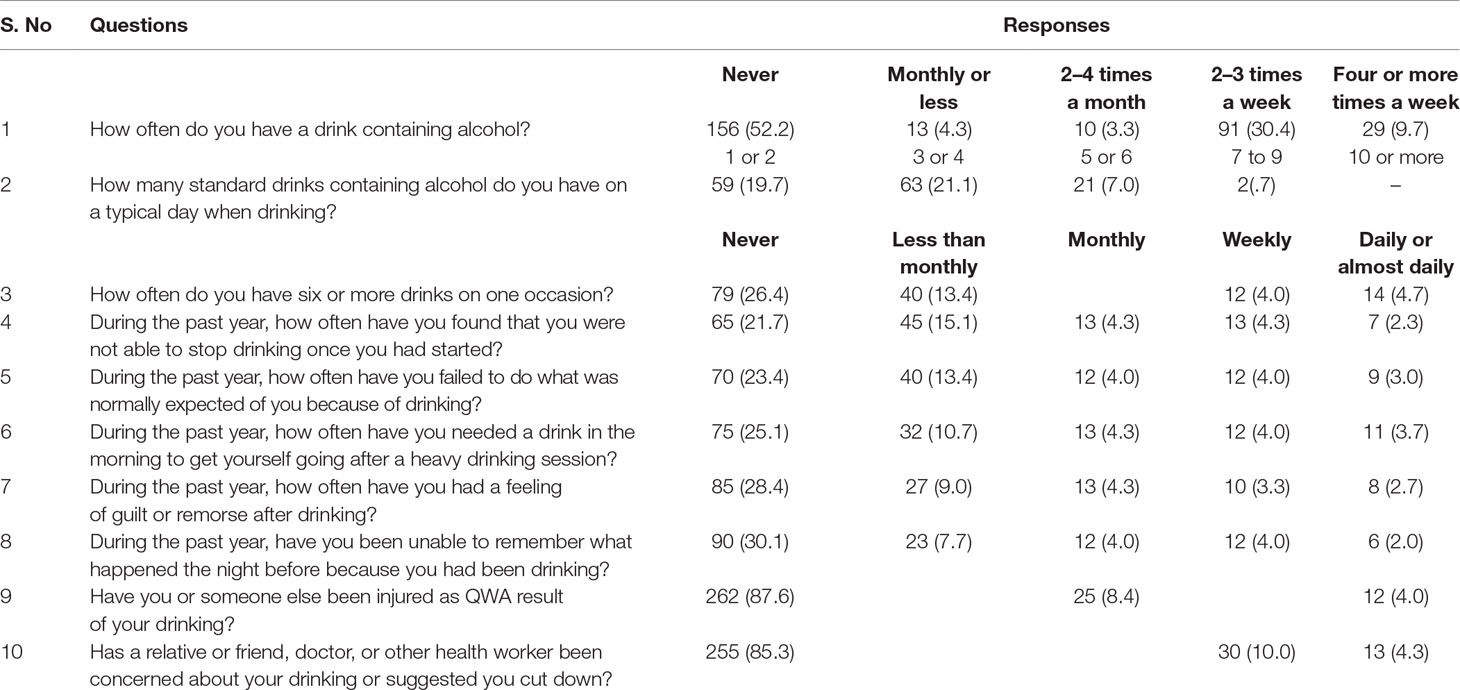
Result: One hundred thirty-nine (46.5%) participants had at least three extremely severe symptoms that fulfil criteria B, C, and D of Diagnostic Statistical Manual IV of PTSD. The most frequent severe symptoms were having repeated, disturbing memories, thoughts, or images. Two hundred ten (70.2%) participants reported the extreme impact of the accident on work or schooling and 156 (51.9%) reported extreme problems in social functioning. Alcohol dependence, hazardous alcohol consumption, and harmful use were reported by 7.9%, 15.1%, and 4.7% of the participants, respectively. In the final model witnessing death, severe sleep problem and severe impairment in family functioning were significantly associated with PTSD.
Conclusion: Nearly half of RTA survivors develop PTSD. Clinicians need to link these patients to the psychiatry clinic. Special attention should be given to patients who witnessed death, with a serious disability, and previous psychiatric history.
Introduction
Post-traumatic stress disorder (PTSD) occurs after exposure to actual or threatened death, serious injury, or sexual violence. It is characterized by recurrent, involuntary, and intrusive distressing memories of the traumatic event and dissociative reactions (1). PTSD symptoms are higher in traumatic events compared to non-traumatic events (2).
Road traffic accident (RTA) is one of the traumatic experiences, which may results in PTSD (3, 4). Globally, road traffic injuries result in more than 1.25 million deaths and 50 million injuries per year (5). More than 90% of road traffic deaths occur in low- and middle-income countries (5). In Ethiopia, though the number of vehicles is one of the lowest in the world, morbidity, disability, and mortality are high. In the region, where the current study is conducted, at least one person is killed each day and 1,884 people are injured or disabled per year due to RTA (6).
The incidence, prevalence, and severity of PTSD in peoples who witnessed or survived from RTA depend on sex, age, place of injury, perceived life treat, and responsibility for the injury (7, 8). Santiago et al. (9) have reported a prevalence of 30.1% at month 1 and 14.0% at month 12 in non-intentional injuries from a systematic review of 58 articles. A study in Sweden reported prevalence of 19.7% in women and 13.2% in men PTSD (10). In a follow-up study, 18.4% of survivors fulfill the criteria for PTSD within 6 months after the accident in Germany (11). In Nigeria, PTSD was higher in RTA survivors (26.7%) than two matched controls (8% and 8.7%) (12). Pervanidou et al. (13) in Greece have reported a higher (nearly half) incidence of PTSD in children who survived from motor vehicle accident.
The important predictor about the level of PTSD across studies was severity of injury. Most articles reported higher magnitude of PTSD in severe cases while some report insignificant association. Keppel et al. (14) and Mayou et al. (15) have reported higher level of PTSD in severe injuries while Stallard et al. (16) reported no association between the two.
Though PTSD was common in victims of RTA, the treatment options are mainly focused in restoring physical activity. The stress is either left undiagnosed or left untreated. If PTSD is left untreated, it will reduce quality of life, limit physical rehabilitation, and increase hospital stay (11, 17). This may be due to lack of evidences especially from low-income countries. The aim of this study was to determine the incidence level and identify factors associated with PTSD in individuals who survived from RTA.
Methods
The study is reported based on STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement, which guides reporting of Observational Studies (18). This is an incidence report from individuals surviving RTA. The study was conducted in three orthopedic settings of Bahir Dar town Northwest, Ethiopia. One of the hospitals (Felegehiwote referral hospital) is a public regional referral hospital while the other two (Gambi and Addinas hospitals) are private hospitals.
Participants
Adults who survived from RTA within 1 month who
1. Have no major trauma before the RTA
2. Can communicate and with no major cognitive impairment which limits verbal report of the symptoms
3. Are admitted to one of the hospitals for orthopedic or other medical care. This is done because we believe that the accident may be enough to result in PTSD if the patient is admitted to a hospital.
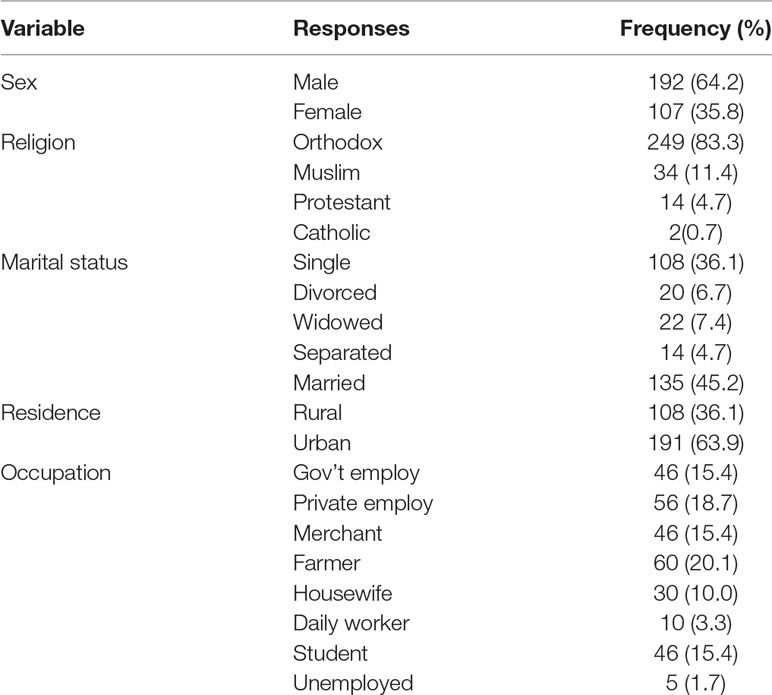
Three hundred thirteen adult RTA survivors who had been admitted in one of orthopedic setting of Bahir Dar town were approached for interview, and 299 (95.53%) accepted to participate. One hundred ninety-two (64.2%) were males, and the median age was 31 with Inter Quartile Range (IQR) of 25–42. One hundred thirty-five (45.2%) of the participants were married, and 28.1% are illiterate. The median household income was 1,000 birr with average family members of 3.46 (Table 1). Two hundred sixteen (72.2%) of the survivors were travelers during the accident, and the remaining were pedestrians. One hundred twenty-eight (42.8%) of the participants witnessed a death in the accident, and 22.4% had other family member in the accident.
Instruments
1. PTSD Checklist (PCL) civilian version, a self-report scale with 17 items having five-point severity scale, was used to assess symptoms of PTSD. It had good psychometric properties including test–retest reliability value of 96% (19). The tool had been developed based on the Diagnostic Statistical Manual symptoms of PTSD (1). The tool was not validated in Ethiopia, but we have done pre-test and confirmatory factor analysis (21) to see the performance of the tool. In the confirmatory factor analysis, the first two items were highly correlated (82.2%) and one of the items was deleted to avoid multicollinearity. The final 16-item instrument had Cronbach’s alpha (22) of 96.2% (Supplementary File). PTSD was reported if an individual report:
● At least one response of extremely severe symptom in questions 1–5 and
● At least one response of extremely severe symptom in questions 6–12 and
● At least one response of extremely severe symptom in questions 13–17
2. Sheehan disability assessment scale (23) was used to screen disability related with the trauma.
3. Patient Health Questionnaire (PHQ-2) was used to assess core symptoms of depression. PHQ-2 was validated in Ethiopia to screen depression (24). The other instruments were Oslo social support scale (25), Alcohol Use Disorders Identification Test (AUDIT) (26), and 8-item PROMIS Sleep Disturbance Short Form (27).
Data were collected with trained nurses, and mental health professionals closely supervised the data collection. The interview was done with Amharic (local language). Data entry was done with Epi Info-7 (28), and SPSS (29) was used to analyze the data. Generalized linear model with Poisson log-linear method (30) was applied to identify factors associated. The presence of association was presented with risk ratio (31) and 95% confidence interval where p-value ≤ 0.05 is considered as statistically significant.
Results
Incidence of PTSD
One hundred thirty-nine (46.5%) participants had at least three extremely severe symptoms of PTSD, which fulfills criteria B, C, nd D of DSM IVRT criteria of PTSD (1). The most frequent severe symptoms were having repeated, disturbing memories, thoughts, or images of a stressful experience from the past and feeling jumpy or easily startled, while feeling emotionally numb or being unable to have loving feelings for closed ones and avoiding thinking about or talking about a stressful experience from the past or avoid having feelings related to it are rare severe symptoms (Table 2).
Impact of the Trauma (Sheehan Disability Assessment Scale)
Two hundred ten (70.2%) participants report extreme impact of accident on work or schooling, and 156 (51.9%) report extreme problems in social functioning (Table 3).
Alcohol and Sleep-Related Problems
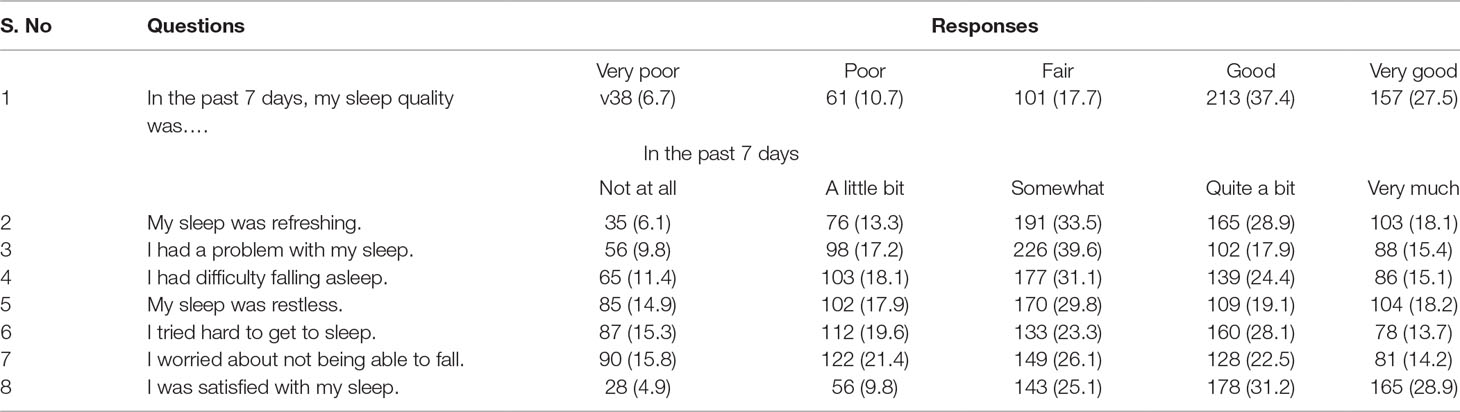
Alcohol dependence, hazardous alcohol consumption, and harmful use were reported by 7.9%, 15.1%, and 4.7% of the participants, respectively (Table 4). Thirty-three (11%) participants reported moderate sleep disturbance. One hundred twenty-four (41.5%) accident survivors report mild sleep disturbance, and the remaining 47.5% had none to slight sleep disturbance (Table 5).
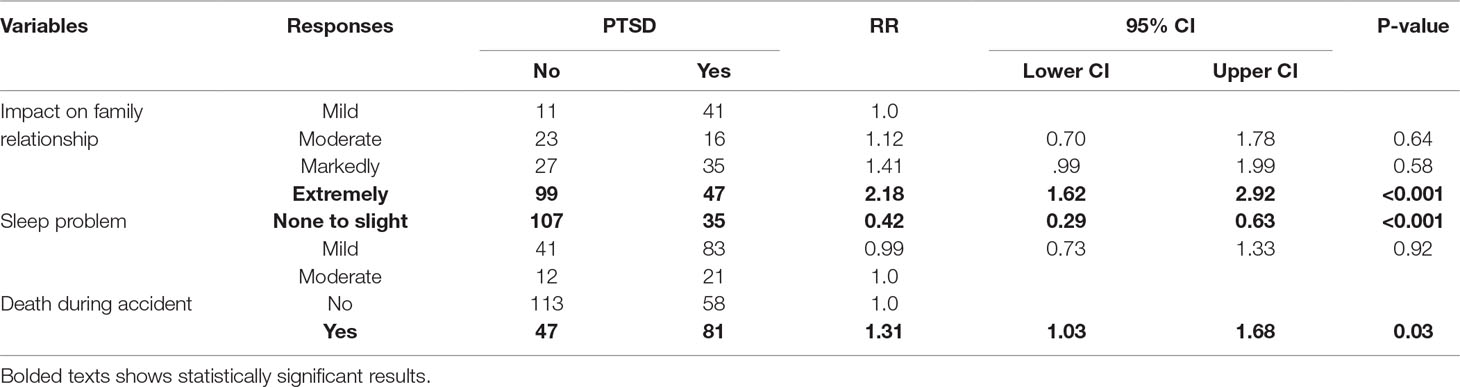
Factors Associated With PTSD
In bivariate analysis, sum score of Alcohol Use Disorder Identification Test (AUDIT), severe impact on social relationship and family functioning, severity of sleep problems, accident on other family members, witnessing death during the accident, and previous reported psychiatric illness was significantly associated with the incidence of PTSD. In the final model (multivariable analysis) witnessing death, severe sleep problem and severe impairment in family functioning were significantly associated with PTSD (Table 6).
Discussion
The incidence of PTSD among RTA survivors was 46.5%. PTSD was associated with witnessing death during the accident, severe impact of the trauma on family relationship, and previous psychiatric illness.
The incidence of PTSD was higher in the current study than studies conducted elsewhere (9–12). The possible reason for this discrepancy may be:
1) In the current study, we include admitted survivors only. Individuals with severe injuries are more likely to be admitted, and PTSD was predicted by the severity of injuries in other studies (7, 8).
2) We exclude injuries who lasted for more than a month. Since, the level of stress decreases over time the high incidence may be explained by short duration (32). However, the level of PTSD is comparable with other studies in United Kingdom, Spain, and Greece (33, 34).
The most consistent associated factors with PTSD in previous studies include: gender, age, severity of injuries, premorbid psychological health, and perceived life threat (11, 32, 35, 36). In the current study, PTSD was associated with previous psychiatric illness, which was also reported in the study from UK (32, 33, 37).
There is 31% increased risk of developing PTSD in peoples who witnessed death than who don’t. This is also reported in other studies (2, 38). Impairment in family relationship and PTSD were significantly associated with PTSD (RR = 2.18, 95% CI [1.62, 2.92]). Severe impairment in family relationship results in serious psychological burden which results in worsening of PTSD symptoms (39, 40). Maintaining family relation especially in traditional society is important. If an individual fails to maintain this responsibility, it will worsen the psychological trauma (41, 42).
Some important variables such as sex and severity of injury were not associated with the incidence of PTSD. The result was mixed in previous evidences where some report higher level of PTSD symptoms among females and people with severe injuries while others report no significant association (14–16).
Limitation
The study had some limitations. The first limitation is related with the validity of instruments, but we have done pretest and factor analysis to familiarize the tool, and the final version of the tools had excellent psychometric properties. The second limitation which may affect the result was we didn’t consider the injury type in the analysis which may limit application. We also excluded people with major cognitive impairment, and the result may be underestimated because these people have higher chance of having PTSD symptoms. We may also miss important biological predictors.
Conclusion
Nearly half of RTA survivors develop PTSD after a month, but the treatment is merely focused on physical rehabilitation. This indicates that clinicians need to link these patients to the psychiatry clinic as it is also helpful for better physical rehabilitation. Special attention should be given to patients who witnessed death, with serious disability, and have previous psychiatric history.
Data Availability
The original data will be made available by placing a reasonable request with the corresponding author.
Ethics Statement
Ethical clearance was obtained from Bahir Dar University. The code was given to every participant and their address was kept private. Participants were informed about the aim of the study, the advantages of the study, confidentiality, and their rights even to stop in the middle of the interview. Written consent was taken before data collection. Individuals with PTSD were linked to the psychiatric clinic.
Author Contributions
WF and TM conceived the research. They framed the methods, did the analysis, and wrote the final paper. HB participated in framing the method, data collection, and write-up. KY and AB conceived the research idea and approved the final manuscript. All the authors read and agreed on the final manuscript.
Funding
The research was funded by Bahir Dar University. WF was supported through the DELTAS Africa Initiative [DEL-15-01]. The DELTAS Africa Initiative is an independent funding scheme of the African Academy of Sciences (AAS)’s Alliance for Accelerating Excellence in Science in Africa (AESA) and supported by the New Partnership for Africa’s Development Planning and Coordinating Agency (NEPAD Agency) with funding from the Wellcome Trust [DEL-15-01] and the UK government. The views expressed in this publication are those of the author(s) and not necessarily those of AAS, NEPAD Agency, WellcomeTrust, or the UK government.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2019.00519/full#supplementary-material
References
1. Association AP. Diagnostic and statistical manual of mental disorders (DSM-5®). USA: American Psychiatric Pub (2013).
2. Boals A, Schuettler D. PTSD symptoms in response to traumatic and non-traumatic events: the role of respondent perception and A2 criterion. J Anxiety Disord (2009) 23(4):458–62. doi: 10.1016/j.janxdis.2008.09.003
3. Butler DJ, Moffic HS, Turkal NW. Post-traumatic stress reactions following motor vehicle accidents. Am Fam Physician (1999) 60(2):524–31.
4. Undavalli C, Das P, Dutt T, Bhoi S, Kashyap R. PTSD in post-road traffic accident patients requiring hospitalization in Indian subcontinent: a review on magnitude of the problem and management guidelines. J Emerg Trauma Shock (2014) 7(4):327. doi: 10.4103/0974-2700.142775
5. Organization WH. Global status report on road safety 2015. Switzerland: World Health Organization (2015).
6. Mekonnen FH, Teshager S. Road traffic accident: the neglected health problem in Amhara National Regional State, Ethiopia. Ethiop J Health Dev (2014) 28(1):3–10.
7. Chossegros L, Hours M, Charnay P, Bernard M, Fort E, Boisson D, et al. Predictive factors of chronic post-traumatic stress disorder 6 months after a road traffic accident. Accid Anal Prev (2011) 43(1):471–7. doi: 10.1016/j.aap.2010.10.004
8. Roitman P, Gilad M, Ankri YL, Shalev AY. Head injury and loss of consciousness raise the likelihood of developing and maintaining PTSD symptoms. J Trauma Stress (2013) 26(6):727–34. doi: 10.1002/jts.21862
9. Santiago PN, Ursano RJ, Gray CL, Pynoos RS, Spiegel D, Lewis-Fernandez R, et al. A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: intentional and non-intentional traumatic events. PloS ONE (2013) 8(4):e59236. doi: 10.1371/journal.pone.0059236
10. Crutebo S, Nilsson C, Skillgate E, Holm LW. The course of symptoms for whiplash-associated disorders in Sweden: 6-month followup study. J Rheumatol (2010) 37(7):1527–33. doi: 10.3899/jrheum.091321
11. Frommberger UH, Stieglitz RD, Nyberg E, Schlickewei W, Kuner E, Berger M. Prediction of posttraumatic stress disorder by immediate reactions to trauma: a prospective study in road traffic accident victims. Eur Arch Psychiatry Clin Neurosci (1998) 248(6):316–21. doi: 10.1007/s004060050057
12. Iteke O, Bakare MO, Agomoh AO, Uwakwe R, Onwukwe JU. Road traffic accidents and posttraumatic stress disorder in an orthopedic setting in south-eastern Nigeria: a controlled study. Scandinavian journal of trauma, resuscitation and emergency medicine. (2011) 19(1):39. doi: 10.1186/1757-7241-19-39
13. Pervanidou P, Kolaitis G, Charitaki S, Lazaropoulou C, Papassotiriou I, Hindmarsh P, et al. The natural history of neuroendocrine changes in pediatric posttraumatic stress disorder (PTSD) after motor vehicle accidents: progressive divergence of noradrenaline and cortisol concentrations over time. Biol Psychiatry (2007) 62(10):1095–102. doi: 10.1016/j.biopsych.2007.02.008
14. Keppel-Benson JM, Ollendick TH, Benson MJ. Post-traumatic stress in children following motor vehicle accidents. J Child Psychol Psychiatry (2002) 43(2):203–12. doi: 10.1111/1469-7610.00013
15. Mayou R, Ehlers A, Bryant B. Posttraumatic stress disorder after motor vehicle accidents: 3-year follow-up of a prospective longitudinal study. Behav Res Ther (2002) 40(6):665–75. doi: 10.1016/S0005-7967(01)00069-9
16. Stallard P, Salter E, Velleman R. Posttraumatic stress disorder following road traffic accidents. Eur Child Adolesc Psychiatry (2004) 13(3):172–8. doi: 10.1007/s00787-004-0399-6
17. Frommberger U, Stieglitz RD, Straub S, Nyberg E, Schlickewei W, Kuner E, et al. The concept of “sense of coherence” and the development of posttraumatic stress disorder in traffic accident victims. J Psychosom Res (1999) 46(4):343–8. doi: 10.1016/S0022-3999(98)00117-2
18. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med (2007) 4(10):e296. doi: 10.1371/journal.pmed.0040296
19. Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther (1996) 34(8):669–73. doi: 10.1016/0005-7967(96)00033-2
21. Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ (2011) 2:53. doi: 10.5116/ijme.4dfb.8dfd
22. Williams J. Mental health status, functioning and disabilities measures. In: Handbook of psychiatric measures, 1st ed. Washington, DC: American Psychiatric Association (2000). p. 96–100.
23. Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, et al. Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res (2013) 210(2):653–61. doi: 10.1016/j.psychres.2013.07.015
24. Abiola T, Udofia O, Zakari M. Psychometric properties of the 3-item oslo social support scale among clinical students of Bayero University Kano, Nigeria. Malays J Psychiatry (2013) 22(2):32–41.
25. Saunders JB, Aasland OG, Babor TF, De la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction (1993) 88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x
26. Yu L, Buysse DJ, Germain A, Moul DE, Stover A, Dodds NE, et al. Development of short forms from the PROMIS™ sleep disturbance and sleep-related impairment item banks. Behav Sleep Med (2012) 10(1):6–24. doi: 10.1080/15402002.2012.636266
27. Info E. CDC. Centers for Disease Control and Prevention (US): Introducing Epi Info 7. CDC, Atlanta, GA, USA (2012).
28. George D, Mallery P. IBM SPSS Statistics 23 step by step: A simple guide and reference. Routledge (2016). doi: 10.4324/9781315545899
29. McCullagh P. Generalized linear models. Eur J Oper Res (1984) 16(3):285–92. doi: 10.1016/0377-2217(84)90282-0
30. Zhang J, Kai FY. What’s the relative risk?: a method of correcting the odds ratio in cohort studies of common outcomes. Jama (1998) 280(19):1690–1. doi: 10.1001/jama.280.19.1690
31. Heron-Delaney M, Kenardy J, Charlton E, Matsuoka Y. A systematic review of predictors of posttraumatic stress disorder (PTSD) for adult road traffic crash survivors. Injury (2013) 44(11):1413–22. doi: 10.1016/j.injury.2013.07.011
32. Mason S, Wardrope J, Turpin G, Rowlands A. The psychological burden of injury: an 18 month prospective cohort study. Emerg Med J (2002) 19(5):400–4. doi: 10.1136/emj.19.5.400
33. Coronas R, Gallardo O, Moreno M, Suarez D, García-Parés G, Menchon J. Heart rate measured in the acute aftermath of trauma can predict post-traumatic stress disorder: a prospective study in motor vehicle accident survivors. Eur Psychiatry (2011) 26(8):508–12. doi: 10.1016/j.eurpsy.2010.06.006
34. Berna G, Vaiva G, Ducrocq F, Duhem S, Nandrino JL. Categorical and dimensional study of the predictive factors of the development of a psychotrauma in victims of car accidents. J Anxiety Disord (2012) 26(1):239–45. doi: 10.1016/j.janxdis.2011.11.011
35. Jeavons S. Predicting who suffers psychological trauma in the first year after a road accident. Behav Res Ther (2000) 38(5):499–508. doi: 10.1016/S0005-7967(99)00073-X
36. Koren D, Arnon I, Klein E. Acute stress response and posttraumatic stress disorder in traffic accident victims: a one-year prospective, follow-up study. Am J Psychiatry (1999) 156(3):367–73.
37. Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment(2004) 11(4):330–41. doi: 10.1177/1073191104269954
38. McMillan T. Errors in diagnosing post-traumatic stress disorder after traumatic brain injury. Brain Inj (2001) 15(1):39–46. doi: 10.1080/02699050150209110
39. Karam EG, Friedman MJ, Hill ED, Kessler RC, McLaughlin KA, Petukhova M, et al. Cumulative traumas and risk thresholds: 12-month PTSD in the World Mental Health (WMH) surveys. Depress Anxiety (2014) 31(2):130–42. doi: 10.1002/da.22169
40. Evans L, McHugh T, Hopwood M, Watt C. Chronic posttraumatic stress disorder and family functioning of Vietnam veterans and their partners. Aust N Z J Psychiatry (2003) 37(6):765–72. doi: 10.1111/j.1440-1614.2003.01267.x
Keywords: PTSD (post traumatic stress disorder), incidence, car accident, predictors, Ethiopia
Citation: Fekadu W, Mekonen T, Belete H, Belete A and Yohannes K (2019) Incidence of Post-Traumatic Stress Disorder After Road Traffic Accident. Front. Psychiatry 10:519. doi: 10.3389/fpsyt.2019.00519
Received: 14 July 2018; Accepted: 01 July 2019;
Published: 19 July 2019.
Edited by:
Gianluca Serafini, San Martino Hospital (IRCCS), ItalyReviewed by:
Rahul Kashyap, Mayo Clinic, United StatesGeorge P. Chrousos, National and Kapodistrian University of Athens, Greece
Copyright © 2019 Fekadu, Mekonen, Belete, Belete and Yohannes. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wubalem Fekadu, d3ViZmVrQGdtYWlsLmNvbQ==
 Wubalem Fekadu
Wubalem Fekadu Tesfa Mekonen
Tesfa Mekonen Habte Belete
Habte Belete Amsalu Belete3
Amsalu Belete3