- Institute of Biomedical Ethics and History of Medicine, University of Zurich, Zurich, Switzerland
Background: The provision of psychotherapy over distance using technology is a growing market reaching many patients and therefore the risks and benefits need to be known by all psychotherapists whether they themselves practice online or not. This comprehensive review of the main ethical arguments for and against different forms of online psychotherapy aims to enhance discussion of ethical issues in this growing area.
Methods: A search of three databases (PubMed, PsycINFO, Web of Science) was conducted in August 2019 using a specific search protocol yielding 249 publications.
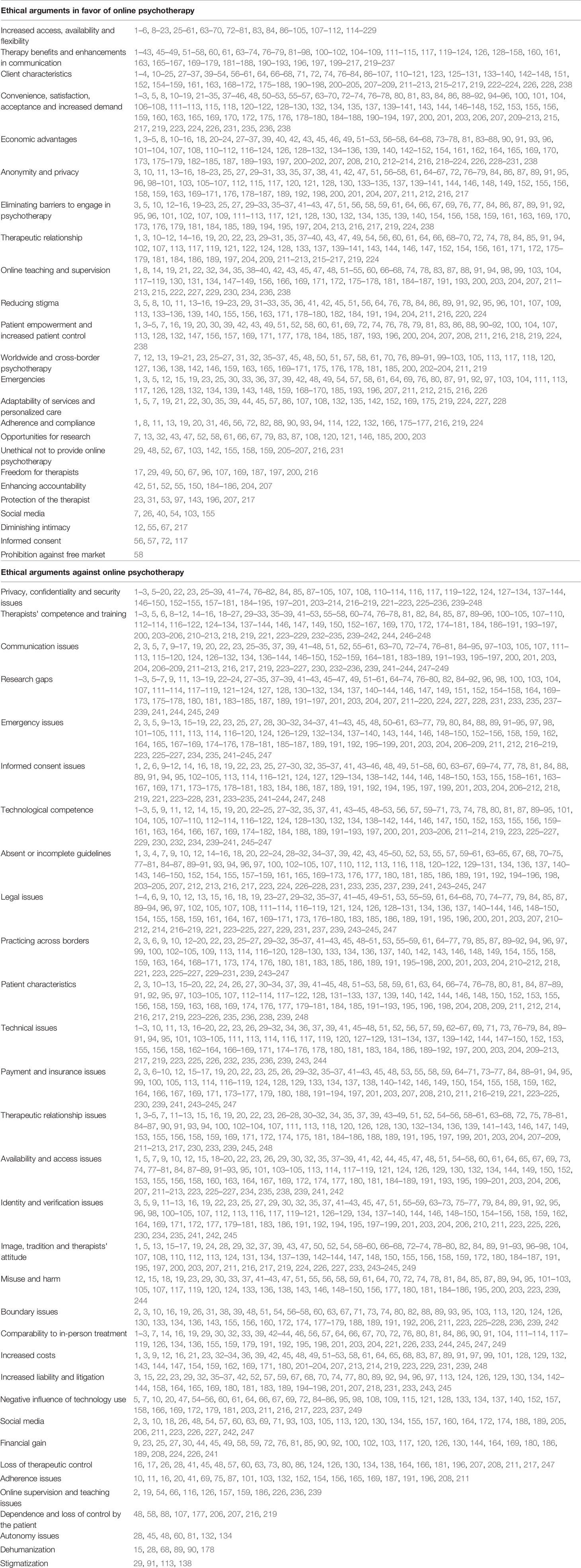
Results: Of 24 ethical arguments in favor of online psychotherapy and 32 against, the top five ethical arguments in favor of online psychotherapy were (1) increased access to psychotherapy and service availability and flexibility; (2) therapy benefits and enhanced communication; (3) advantages related to specific client characteristics (e.g. remote location); (4) convenience, satisfaction, acceptance, and increased demand; and (5) economic advantages. The top five ethical arguments against engagement in online psychotherapy were (1) privacy, confidentiality, and security issues; (2) therapist competence and need for special training; (3) communication issues specific to technology; (4) research gaps; and (5) emergency issues.
Conclusions: The findings may be of help to practitioners in deciding whether to engage in online psychotherapy, and in informing patients about risks and benefits, improving ethical guidelines, and stimulating further ethical discussion. The findings are argumentative and qualitative in nature, and further quantitative research is needed.
Introduction
Technological innovation has led to rapid change in many professions, bringing both benefits and challenges. Since the late 1990s, a growing body of research has addressed issues related to online psychotherapy. To begin, that research focused mainly on the usefulness of online psychotherapy before shifting in emphasis to situations in which online psychotherapy might be used, with a view to evaluating the strengths and shortcomings of this approach (1).
The Joint Task Force for the Development of Telepsychology Guidelines for Psychologists (2) define telepsychology as “[…] the provision of psychological services using telecommunication technologies […]” (p. 792), which may be synchronous (real-time) or asynchronous, including “[…] telephone, mobile devices, interactive videoconferencing, e-mail, chat, text, and Internet […]” (p. 792). The service can be standalone or an adjunct to traditional psychotherapy. The various terms used to describe such services generally refer to psychotherapy delivered remotely using some form of communication technology. In this review, the term online psychotherapy encompasses all such terminological variants, including telepsychology [see (2)], telepsychiatry [see (1)], online counseling [see (3)], behavioral telehealth, telemental health [see (4)], internet therapy [see (5)], internet counseling, online practice, online therapy, e-therapy, cyber-counseling, cyberpsychology, e-social work [see (6)], and e-mental health [see (7)]. These terms may differ slightly according to professional context or technological modality.
The practice of online psychotherapy reflects the rapid evolution of technology and may include the use of “virtual reality, augmented reality, intelligent wearable devices, and artificial intelligence applications” [(8), p. 125]. As these technologies are still in the early stages of development, they are not included in this review. The present review includes online psychotherapy conducted by psychiatrists, psychologist, and social workers. Nurses are not included because of differences in their education and legal restrictions on the scope of their work.
As a growing number of patients seek online psychotherapy, therapists must consider the related ethical issues (3) and should be able to participate in this ethical discussion (9). For example, one important feature of a thorough process of informed consent is knowledge of risks and benefits in making a fully informed decision (10). One of the main barriers to further implementation of online psychotherapy is the uncertainty around ethical and legal issues (1), which are increasingly addressed in ethical codes of conduct (11).
The aim of this review is to summarize the main ethical arguments for and against the provision of online psychotherapy to further ethical discussion within the relevant professions, and to facilitate the development of comprehensive ethical guidelines to underpin the practice of online psychotherapy. This in turn will help practitioners in deciding to offer this form of psychotherapy and in helping their patients to make a truly informed decision about engaging in online psychotherapy. The present review is not about the quantity or volume of publications in which specific ethical arguments are discussed; rather, our concern was to identify the main ethical arguments to date as a sound basis for future discussion.
Methods
Publications were collected in August 2019 from three databases: PubMed, PsycINFO, and Web of Science. These were selected on the basis that the topic relates to medical, psychological, and ethical issues.
To construct the search protocol, the research question was structured in terms of three topics: ethics, psychotherapy, and online. Synonyms and main terms for these three fields were selected, and a search code was constructed for each database (including MeSH terms for PubMed and Thesaurus of Psychological Index Terms for PsycINFO); for details, see Full Search Code in Supplemental Material). The search code was validated by an expert librarian at the University of Zurich.
Publication titles and abstracts were screened according to defined selection criteria (for details, see Publication Selection Criteria in Supplemental Material).
The main ethical arguments were extracted from the selected publications by JS, clustering text passages according to main topics. JM read the selected publications independently and clustered the publications under these main categories (Table 1). Disagreements were discussed and resolved.
Results
The collection of publications in August 2019 in the three databases PubMed, PsycINFO, and Web of Science and selection according to the selection criteria resulted in a final sample of 249 publications.
The final sample (n = 249) included 179 articles, 6 books, 55 book chapters, 2 doctoral theses, 5 book reviews, 1 brief communication, and 1 item of correspondence. Among these, there were 32 literature reviews, 2 systematic reviews (regarding the socioeconomic impact of telehealth and guidelines in videoconferencing), 6 editorials or introductions, 5 book reviews, and 6 books (including 4 practice guides). Additionally, there was one case study, one correspondence, one research digest, one discussion, and one paper on ethical reasoning. In total, 30 of the selected publications were empirical studies, including 14 surveys and 6 website analyses. Six related to specific mental illnesses, one was a comparison of in-person and online psychotherapy, two included practitioner interviews, one was a study protocol for a meta-analysis, and one related to a practitioner discussion forum. Among other notable features of the final sample, 18 included guidelines, and 25 focused on specific countries.
The selected publications ranged across disciplines that included psychology (70), psychiatry (33), psychology and psychiatry (2), social work (12), and telemedicine (6). The remaining publications (125) related to psychotherapy in general, with no specific disciplinary focus. In terms of technological modality, these included email (13), telephone (5), videoconferencing (28), text-based methods including email and chat (14), email and text messages via cellphone (3), mobile phones (3), text messages (1), email and social media (2), and videoconferencing and mobile phones (6). The remaining 173 related to communication technologies in general rather than any specific technology or mode of communication.
Table 1 summarizes the main ethical arguments (24 pro and 32 contra) extracted from the final 249 publications, organized by number of mentions. The next section describes the various categories. For clarity, the summary does not include all discussion points, and reference is made to only one publication for each ethical argument. For further information about the arguments, readers are referred to the source (Table 1).
Ethical Arguments in Favor of Online Psychotherapy
Increased Access, Availability, and Flexibility
Online psychotherapy can improve and enhance access to health care services and evidence-based care, especially for those living in rural or remote areas and populations that are underserved for other reasons [see (12)]. Services can be accessed anywhere and at any time, allowing greater flexibility [see (13)]. This is advantageous for both therapist and patient, enabling immediate and timely care [see (3)]. Online psychotherapy may also facilitate more frequent contact between patient and therapist [see (14)], and as more therapists are available to the patient, specialist care is easier to access, and the range of services is wider [see (1)].
Therapy Benefits and Enhancements in Communication
According to a growing number of favorable research findings, online psychotherapy can be as efficient, effective, and efficacious as traditional therapy (or more so) [see (1)]. Multiple therapeutic orientations and modalities are translated into online communication, but cognitive behavioral approaches seem to be most appropriate or the easiest to transfer [see (15)]. For example, during an in vivo exposure, the therapist could be virtually present [see (16)]. However, also other psychotherapeutic orientations such as psychoanalysis assess and discuss ethical issues of practicing online [see (17)]. Online psychotherapy offers a viable alternative to in-person treatment but can also be used as a supplement or adjunct [see (18)]. This affords new opportunities for creative approaches involving different models of therapy and technological modalities, and additional online material (websites, videos, etc.) are easily integrated into therapy [see (19)]. Data recording and documentation of the online therapeutic process is also easier, allowing treatment, treatment stages, and therapeutic techniques used by therapist and patient to be revisited [see (20)].
Client Characteristics
Online psychotherapy can be especially useful for clients living in geographically remote, rural, or otherwise underserved areas where few or no therapists are available [see (21)], as well as for homebound or mobility-impaired patients [see (22)]. Access to traditional in-person services may be limited by the psychiatric condition itself, as in cases of agoraphobia, anxiety, or other illnesses that restrict physical encounter, and online psychotherapy again offers a possible solution [see (23)]. Online psychotherapy seems especially appropriate for patients with mild or moderate symptoms [see (24)], but might also be a viable tool for patient in acute crisis with no possibility for immediate in-person care [see (25)].
Convenience, Satisfaction, Acceptance, and Increased Demand
Online psychotherapy is perceived as convenient and comfortable by patients and therapists alike [see (26)], not least because of the greater flexibility it offers in terms of location and time [see (27)]. Online services have gained increasing acceptance among patients and therapists [see (28)], who express satisfaction with this approach [see (15)]. Unsurprisingly, then, demand and interest is on the increase among both patients and practitioners [see (29)].
Economic Advantages
Online psychotherapy is reported to be more cost-efficient [see (30)], with the potential to reduce healthcare costs for patients, therapists, and society as a whole [see (31)]. As a single therapist can reach more patients, especially in underserved populations [see (32)], long waiting lists for face-to-face treatment can be reduced [see (33)], offering a possible solution to the workforce shortage in mental health provision [see (34)]. Online psychotherapy might pose a solution to an undersupply in mental health care in various regions of the world, especially in low- and middle income or developing countries, for example, in India [see (34)].
Anonymity and Privacy
Because online psychotherapy can be provided anonymously and one is not seen entering the therapist's office [see (20)], it can enhance the patient's sense of anonymity and privacy [see (13)]. Perceived or actual anonymity may lead in turn to reduced inhibition and greater openness in discussing emotional topics [see (35)].
Eliminating Barriers to Engagement
By reducing or eliminating barriers such as fear of social stigma, online psychotherapy can reach patients who might never have sought traditional in-person therapy [see (36)]. This might serve as an entry point to the mental health system, including traditional in-person therapy as a possible next step [see (37)].
Therapeutic Relationship
The therapeutic relationship established in online psychotherapy is commonly perceived as equal to or better than in-person therapy, and an established therapeutic relationship can be enhanced using online communication [see (38)].
Online Teaching and Supervision
Technology-mediated communication can contribute positively to teaching and supervision and facilitates inter-professional and inter-collegial exchange worldwide [see (39)]. Online psychotherapy conducted by email or other text-based communication automatically generates a record of the sessions [see (32)], and a videoconferencing approach enables sessions to be videotaped [see (40)] for later supervision.
Reducing Stigma
Any stigma, stigmatization, or perceived stigma associated with seeking mental help services or concerns about being stereotyped can be reduced or eliminated by online psychotherapy. This may in turn help to address barriers to traditional psychotherapy such as concerns about anonymity and privacy [see (41)].
Patient Empowerment and Increased Patient Control
Online psychotherapy empowers the patient because, for example, it is much easier to move to another therapist [see (42)], giving the patient more control over their therapy [see (43)]. This reconfigures the balance of power between therapist and patient, making the interaction more collaborative [see (20)].
Worldwide and Cross-Border Psychotherapy
Online psychotherapy can be provided from anywhere, without regard to geographical boundaries, state lines, national borders, or time-zones, allowing therapists to reach patients who are, for instance, temporarily abroad [see (19)].
Emergencies
Online psychotherapy can be useful for emergencies and crisis interventions. As compared to traditional in-person therapy, it may provide more immediate access to services, and disclosure of suicidal or homicidal tendencies may be easier online [see (19)]. In the context of crisis and suicide prevention, suicide hotlines and other forms of telephone emergency care are long established and proven practices [see (37)].
Adaptability of Services and Personalized Care
Online psychotherapy can offer services that specifically match patients' needs [see (19)], facilitating genuinely patient-centered care [see (44)] and individualized treatment and technology options [see (45)].
Adherence and Compliance
Levels of adherence, attendance, and compliance as good as or better than in-person treatment can be achieved using online psychotherapy [see (46)].
Opportunities for Research
Online psychotherapy offers unique opportunities for research [see (32)]; for example, email-based therapy automatically creates a written record, which can be used for research purposes [see (47)].
Unethical Not to Provide Online Psychotherapy
Failure to provide online psychotherapy to vulnerable people who need it can be seen as unethical—for example, patients living in rural or remote areas with few or occasional local options [see (48)].
Freedom for Therapists
Online psychotherapy can afford the therapist greater freedom [see (49)], including more professional opportunities and a better balance between professional and private life [see (50)].
Enhancing Accountability
Online psychotherapy increases the accountability of both therapist and patient, not least because it is easier to keep records and to make transcripts available to both parties [see (51)], reducing the potential for malpractice and litigation [see (52)].
Protection of the Therapist
Security issues raised by risky environments or when communicating with potentially dangerous patients can be reduced by online service provision [see (53)].
Social Media
Offering unprecedented opportunities for access and connecting with patients and other therapists, social media can be a useful therapeutic tool [see (54)].
Diminishing Intimacy
As the distance provided by technology inhibits physical proximity, online psychotherapy can help to reduce the risk of patient-therapist (sexual) intimacy [see (55)].
Informed Consent
The informed consent process can be enhanced by online communication—for example, web pages can be revisited (56), with links to additional information resources or technical material and translation into different languages [see (57)].
Prohibition Against Free Market
The view that one should not engage in online psychotherapy is legally problematic because it restricts trade and the ethical right to a free market (58).
Ethical Arguments Against Online Psychotherapy
Privacy, Confidentiality, and Security Issues
Among concerns about privacy, confidentiality, security, and safety in online psychotherapy [see (59)], one relates to the use of unsecured websites or unencrypted communication tools, like commercially available software [see (60)] that is easily hacked [see (61)]. Data security may also be compromised when technology fails [see (62)], with potential breaches of confidentiality that might extend beyond the therapist's control [see (63)].
Therapist Competence and Training
To provide online psychotherapy, training is needed to ensure appropriate technology-related competences, as well as clinical and therapeutic competences specific to the online setting. In particular, the therapist would require knowledge of ethical approaches and guidelines, as well as specific legal requirements and policies [see (18)]. In general, therapeutic skills in in-person contact do not automatically translate into online therapeutic skills [see (32)]. At present, standards are not well defined, and there are few training or education programs for online psychotherapy, which is not included in most traditional curricula [see (64)]. In relation to working remotely with patients in other countries, the therapist would need to be familiar with international laws and legal requirements in the patient's jurisdiction, and additional cultural competences might also be required [see (65)].
Communication Issues
Among negative issues, one of the most widely discussed is the absence of non-verbal cues in the therapeutic interaction, especially when using text-based media but also when using telephone or videoconferencing, which may lead to misunderstandings and miscommunication [see (20)]. If a therapist were to miss some important item of clinical information, the whole diagnostic process and psychological assessment could be impaired [see (28)]. The use of e-mail in this context can undermine the conversation in terms of time lag and lack of spontaneity, and it may prove difficult to express empathy, warmth, and feelings [see (64)]. For these reasons, online psychotherapy may not be appropriate for all therapeutic approaches and modalities [see (66)].
Research Gaps
Many authors claim that there is insufficient research in support of online psychotherapy or that there are too many knowledge gaps, especially with regard to effectiveness, efficacy, and long-term outcomes and as compared to in-person treatment [see (30)].
Emergency Issues
Questions also arise as to whether an emergency or crisis situation involving threat to self or others can be detected and addressed where patient and therapist are at different locations [see (67)]. Other ethical issues regarding emergency or crisis situations include verification of patient identity and location [see (68)], technological difficulties [see (69)], and cross-border practice [see (70)].
Informed Consent Issues
In light of the many differences from in-person therapy (e.g. technical, legal), online psychotherapy requires a particular form of informed consent [see (71)]. However, it might be difficult to determine whether the patient is legally able to give consent or to assess their mental capacity to do so [see (72)].
Technological Competence
A therapist's lack of technological competence and patient and therapist awareness of their respective skills are important issues in this context, as discomfort or fear of using technology is not uncommon [see (73)].
Absent or Incomplete Guidelines
Regulatory guidelines and standards of practice or care in this area are considered incomplete or absent. Guidance by legal or regulatory bodies is also lacking, especially in terms of global or international regulation of cross-border practice, and the absence of specific ethical guidelines or codes of conduct for online psychotherapy leaves many ethical questions unanswered [see (42)].
Legal Issues
Unresolved jurisdiction and few or no specific laws governing licensing, certification, training and education, informed consent, and cross-border practice are problematic issues for online psychotherapy [see (74)].
Practicing Across Borders
Many issues arise in relation to online psychotherapy conducted across state or national borders, including legislative, licensing, and cultural differences [see (30)]. For instance, it may be unclear whether the therapy is seen to take place at the patient's or the therapist's location, raising such questions as which jurisdiction is responsible when a problem arises or which regulates professional practice in the event of a violation [see (75)]. The therapist may not even know or cannot be sure where the patient is located, especially if they choose to remain anonymous [see (76)]. Cultural differences between patient and therapist might influence the communication itself by different cultural behaviors or language use resulting in different interpretations of the behavior and potential misunderstandings [see (30)].
Patient Characteristics
Online psychotherapy may not be suitable for all patients, clinical conditions, psychiatric disorders, and problems; it may sometimes be contraindicated, especially in the case of severe mental disorder, or for patients who are highly dysfunctional and/or pose a threat to themselves or others [see (16)]. A patient's inability, diminished competence, or discomfort when using technology might also be considered a barrier [see (15)].
Technical Issues
Technical difficulties and failures are major concerns in this context, possibly leading to frustration and anger, which may be distracting or disturbing [see (73)].
Payment and Insurance Issues
Payment, reimbursement, fee structure, and billing for online psychotherapy raise many questions, such as how interruption or technical failure will be handled [see (77)]. Another important issue is whether insurers will cover online psychotherapy in general, as well as instances of malpractice or liability, which may become especially complicated across state or national borders [see (68)].
Therapeutic Relationship Issues
Many authors have questioned whether an effective and successful therapeutic alliance can be developed solely through technology [see (78)] and whether the well-known benefits of the therapeutic relationship might disappear or diminish in online psychotherapy [see (79)]. Other issues raised in this include absence of non-verbal cues and lack of intimacy [see (51)].
Availability and Access Issues
Because technology often creates a sense of permanent access, this may become a problem, as the therapist cannot and will not guarantee this [see (60)]. Response time and delays are also an important issue, especially in emergency situations [see (80)]. Additionally, accessibility (for instance, in terms of technology, devices, connectivity, and applications) may be restricted for people of lower socioeconomic status or for those unable to use the equipment [see (32)].
Identity and Verification Issues
As it may be difficult to verify the identity of the patient (or the therapist) online, deception or fraud is a possibility—for example, a therapist might inadvertently treat a minor without parental consent [see (64)].
Image, Tradition, and Therapist Attitude
Many therapists have a negative view of online psychotherapy and are clearly concerned or strictly against it, with poor reported satisfaction and acceptance among therapists [see (1)] and concerns that online psychotherapy might damage the profession's image [see (58)].
Misuse and Harm
Unethical, malign, or abusive behavior may be easier online [see (81)]—for instance, practicing without a license or without appropriate training, or even pretending to be a therapist [see (23)].
Boundary Issues
Online psychotherapy may make it more difficult to maintain professional boundaries, posing a threat to the professional relationship—for example, an interaction mediated by technology might seem social, conversational, or less formal, and the flexibility of location and time might lead to communication in inappropriate locations or at odd times, as the therapist might be tempted to communicate while on holidays, traveling, or while ill [see (26)]. As another potential threat to boundaries, therapists and/or patients might use search engines to explore private information [see (82)].
Comparability to In-Person Treatment
One important open question is whether online psychotherapy is truly comparable to in-person treatment, and whether it can replace traditional in-person therapy. Many authors have expressed doubts in this regard, to the extent that some believe online services may prevent patients from seeking more suitable traditional therapy [see (56)].
Costs
Online psychotherapy entails some initial costs for the therapist, which may make access to online psychotherapy services too expensive for some patients [see (68)]. These initial costs could make it difficult to implement online psychotherapy in some low-income and developing countries [see (83)].
Increased Liability and Litigation
Therapists who provide an online service may be more exposed to litigation and increased liability, as for example in cross-border cases [see (29)].
Negative Influence of Technology Use
Online psychotherapy may contribute to internet overuse and ultimately internet addiction [see (47)], potentially increasing social isolation [see (84)] and exposure to unregulated and misleading health-related or other information [see (85)].
Social Media
The use of social networking sites poses new ethical challenges and invites potentially unethical interactions in the context of online psychotherapy, such as friend requests from patients [see (57)] or problematic self-disclosure [see (18)].
Financial Gain
There is a danger that online psychotherapy might be conducted for financial gain without due regard to the best interests of the patient [see (27)].
Loss of Therapeutic Control
Online psychotherapy may risk loss of therapeutic control [see (86)]—for example, in relation to the patient's location [see (57)].
Adherence Issues
Compliance and adherence to therapy may be undermined in an online setting, given the ease of dropping out, logging off, hanging up the phone, or terminating the connection [see (87)].
Online Supervision and Teaching Issues
Supervising and teaching online raises a number of specific ethical issues and questions [see (66)].
Patient Dependence and Loss of Control
In online psychotherapy, the patient may experience less control (58), and the process may foster dependence [see (88)].
Autonomy Issues
Online psychotherapy may hamper patient autonomy [see (28)]—for example, a patient may experience a sense of intrusion when receiving online psychotherapy at home [see (81)].
Dehumanization
Online psychotherapy may lead to dehumanization of the therapeutic environment [see (89)] or of the patient if experienced as intrusive by someone who is already vulnerable [see (90)].
Stigmatization
An online setting may promote inadvertent discrimination or cultural insensitivity by masking important cues [see (91)].
Discussion
Online psychotherapy offers many advantages like benefits for the therapeutic process and the therapeutic communication itself, also by being more convenient than traditional settings of psychotherapy. Both many patients and therapists seem to be satisfied with the use of online psychotherapy. Not surprisingly, this kind of psychotherapy is increasingly being used. Online psychotherapy promises to solve economic pressures by being more cost-effective, offering a solution for workforce shortage problems and increasing access to necessary psychotherapy for many different populations suffering from mental health problems who might be difficult to reach such as patients living in rural areas. Reducing barriers to engaging in psychotherapy by reducing stigma, being able to attend online sessions anonymously thus enhancing a sense of privacy, reaching patients worldwide and across borders are other advantages of online psychotherapy. Conducting psychotherapy online gives the possibility to adapt services to specific patients offering more personalized care, enhancing patient control, and empowering the patient resulting in more adherence to and compliance with the treatment itself. The specific setting of online psychotherapy gives the therapist more freedom and offers physical protection, but might also protect the patient from breaches of intimacy boundaries and enhance the accountability of both patient and therapist. Additionally, online psychotherapy offers new opportunities for research, teaching, and supervision, enhancing the informed consent process, offering new opportunities through the use of social media and might give good assistance in emergency situations. Online psychotherapy might even improve and extend the therapeutic relationship.
One of the biggest and most discussed disadvantages of using psychotherapy is the risks with regard to privacy, confidentiality, and data security. Online psychotherapy creates new challenges to therapist competences which brings about the need for new forms of training and education, especially technological competences regarding many technical issues that might occur. Technological competence is not only needed by the therapist, but also by the patient. New communication skills are needed and particular attention must be paid to the development of the therapeutic relationship regarding the many boundary issues that might occur. Difficulties herein are put up by new access and availability issues and the loss of therapeutic control. Broader research, new guidelines, and a consideration of legal issues in general are needed especially regarding the practice across borders of nations, new payment and insurance issues, challenges to the informed consent process, dealing with emergency situations, enhancing the identification process of the therapist and the patient, and selecting patients that are suitable for online psychotherapy. The comparability to in-person treatment might be questioned and some fear danger to the image of psychotherapy. Therapists might fear increased liability and litigation. Online, new forms of misuse are possible and charlatans might utilize this kind of psychotherapy to achieve financial gains. Other feared disadvantages of online psychotherapy are the dehumanization and stigmatization of patients, patient dependence, and loss of patients' autonomy. New adherence issues might occur regarding the ease of ending an online session. Online supervision and teaching and the use of social media raise further ethical questions. Extensive costs might be faced by patient and therapists, when using online psychotherapy, for example, to set up the new technologies. Last but not least, the negative influence of technology itself might endanger its users.
This review has a number of limitations. First, only articles in English and German were included. However, only fourteen of the articles that were found to meet the search criteria were in a different language and therefore excluded. Among the emerging research topics not included in this review are online training and supervision, social media, avatar, second life, robots and bots, artificial intelligence, computer-mediated (self-help) therapy, psychology-related smartphone apps, internet-based group therapy and telecare, online forums, open chat, therapy for older adults, therapy for children and adolescents, and marriage and family therapy.
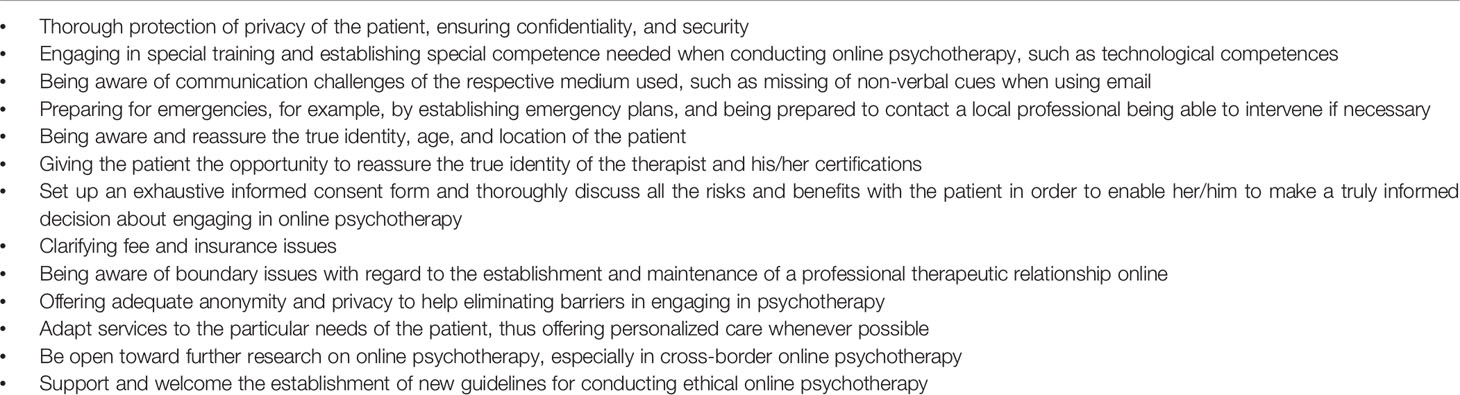
It is beyond the scope of the present review to offer exhaustive recommendations for clinical practice or how these ethical risks might be resolved in practice, and further systematic research should more fully address this topic. For some recommendations directly deducted from the results of this review, see Table 2.
Counting the frequency of arguments does not clarify their relative importance; to evaluate their true weight, a more quantitative survey of experts' ratings is needed. Without that deeper understanding, the risks and benefits reviewed here remain anecdotal and qualitative, with only limited validity (92).
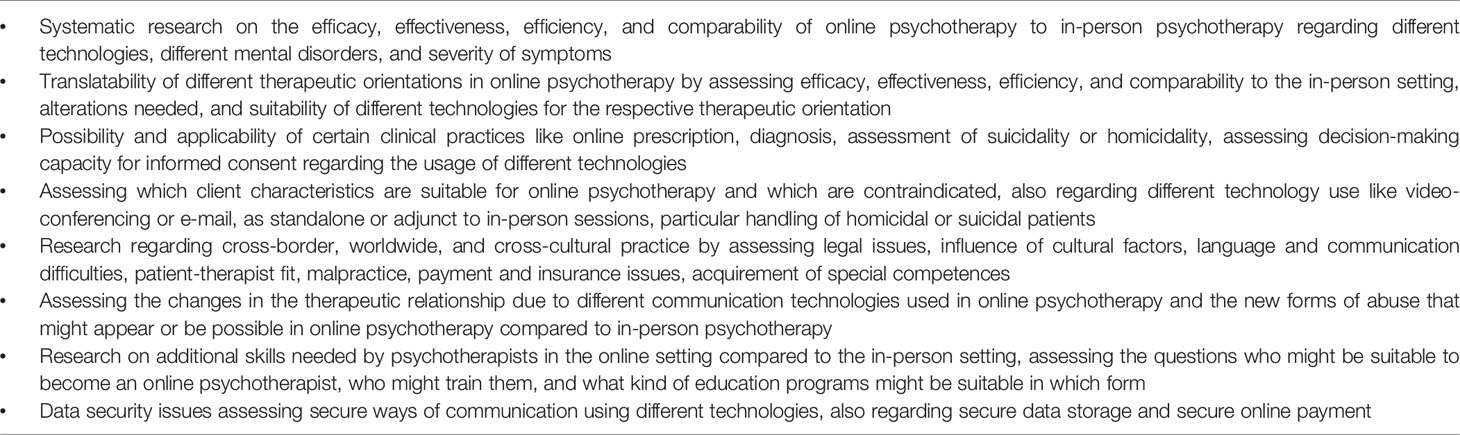
In future systematic research on efficacy, effectiveness, and efficiency of online psychotherapy is needed and practice guidelines, legal and ethical frameworks need to be developed. Further research in the fast growing field of online psychotherapy seems vital. Some important topics requiring further investigation are summarized in Table 3.
Conclusion
If trained psychotherapists choose not to participate in the new and emerging field of online psychotherapy, it seems likely that charlatans will emerge to meet the ever-growing demand, perhaps driving professional psychotherapists out of the market (37). For that reason, psychotherapists from all professional backgrounds must be properly informed about the risks and benefits of online psychotherapy if they are to make well-informed decisions and act in the best interests of their patients. Even if they decide not to offer such services themselves, they should be equipped to provide information about online psychotherapy that enables patients to make a well-considered decision about using such services.
Author Contributions
JS and MT designed the review and developed the search strategy. JS and JM were involved in search, exclusion, and argument extraction processes. JS and MT wrote and edited the final article, which was reviewed and approved by JM.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Special thanks to Sabine Klein, expert librarian at the University of Zurich, who reviewed the final search code and provided many useful inputs, and to Jörg Zemp, librarian at the Institute of Biomedical Ethics and History of Medicine, University of Zurich, who assisted us in locating the full-text publications that were not directly available.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2019.00993/full#supplementary-material
References
1. Chakrabarti S. Usefulness of telepsychiatry: A critical evaluation of videoconferencing-based approaches. World J Psychiatry (2015) 5(3):286–304. doi: 10.5498/wjp.v5.i3.286
2. Joint Task Force for the Development of Telepsychology Guidelines for Psychologists (2013). Guidelines for the practice of telepsychology. Am Psychol 68(9):791–800. doi: 10.1037/a0035001
3. Cipolletta S, Mocellin D. Online counseling: An exploratory survey of Italian psychologists' attitudes towards new ways of interaction. Psychother Res (2017) 28:1–16. doi: 10.1080/10503307.2016.1259533
4. Comer JS. Introduction to the special series: Applying new technologies to extend the scope and accessibility of mental health care. Cogn Behav Pract (2015) 22(3):253–7. doi: 10.1016/j.cbpra.2015.04.002
5. Coyle D, Doherty G, Matthews M, Sharry J. Computers in talk-based mental health interventions. Interact Comput (2007) 19(4):545–62. doi: 10.1016/j.intcom.2007.02.001
6. Finn J, Schoech D. Introduction. J Technol In Hum Serv (2008) 26(2/4):105–8. doi: 10.1080/15228830802061428
7. Jorm AF, Morgan AJ, Malhi GS. The future of e-mental health. Aust New Z J Psychiatry (2013) 47(2):104–6. doi: 10.1177/0004867412474076
8. Luxton DD, Nelson E-L, Maheu MM. Conclusion. In: Luxton DD, Nelson E-L, Maheu MM, editors. A practitioner"s guide to telemental health: How to conduct legal, ethical, and evidence-based telepractice. Washington, DC, US: American Psychological Association (2016b). p. 121–6.
9. Fisher CB, Fried AL. Internet-mediated psychological services and the American Psychological Association Ethics Code. Psychother: Theory Res Pract Training (2003) 40(1/2):103–11. doi: 10.1037/0033-3204.40.1-2.103
10. Wells SY, Williams K, Walter KH, Moreno L, Butler E, Glassman LH, et al. The informed consent process for therapeutic communication in clinical videoconferencing. In: Tuerk PW, Shore P, editors. Clinical videoconferencing in telehealth: Program development and practice. Cham, Switzerland: Springer International Publishing (2015). p. 133–66.
11. Abbott J-AM, Klein B, Ciechomski L. Best practices in online therapy. J Technol In Hum Serv (2008) 26(2/4):360–75. doi: 10.1080/15228830802097257
12. Zur O. Telehealth and the technology for delivering care. In: Zur O, editor. Boundaries in psychotherapy: Ethical and clinical explorations. Washington, DC, US; American Psychological Association (2007). p. 133–46.
13. Chester A, Glass CA. Online counselling: A descriptive analysis of therapy services on the Internet. Br J Guid Couns (2006) 34(2):145–60. doi: 10.1080/03069880600583170
14. Wodarski J, Frimpong J. Application of e-therapy programs to the social work practice. J Hum Behav In Soc Environ (2013) 23(1):29–36. doi: 10.1080/10911359.2013.737290
15. Perle JG, Langsam LC, Nierenberg B. Controversy clarified: An updated review of clinical psychology and tele-health. Clin Psychol Rev (2011) 31(8):1247–58. doi: 10.1016/j.cpr.2011.08.003
16. Brenes GA, Ingram CW, Danhauer SC. Benefits and challenges of conducting psychotherapy by telephone. Prof Psychol: Res Pract (2011) 42(6):543–9. doi: 10.1037/a0026135
17. Scharff JS. Technology-assisted psychoanalysis. J Am Psychoanal Assoc (2013) 61(3):491–509. doi: 10.1177/0003065113485423
18. Johnson GR. Toward uniform competency standards in telepsychology: A proposed framework for Canadian psychologists. Can Psychol/Psychol Can (2014) 55(4):291–302. doi: 10.1037/a0038002
19. Fenichel M, Suler J, Barak A, Zelvin E, Jones G, Munro K, et al. Myths and realities of online clinical work. CyberPsychol Behav (2002) 5(5):481–97. doi: 10.1089/109493102761022904
21. Luxton DD, Nelson E-L, Maheu MM. Concepts, principles, and benefits of telemental health. In: Luxton DD, Nelson E-L, Maheu MM, editors. A practitioner"s guide to telemental health: How to conduct legal, ethical, and evidence-based telepractice. Washington, DC, US: American Psychological Association (2016a). p. 9–16.
22. Godine N, Barnett JE. The use of telepsychology in clinical practice: Benefits, effectiveness, and issues to consider. Int J Cyber Behav Psychol Learn (2013) 3(4):70–83. doi: 10.4018/ijcbpl.2013100105
23. Fitzgerald TD, Hunter PV, Hadjistavropoulos T, Koocher GP. Ethical and legal considerations for Internet-based psychotherapy. Cogn Behav Ther (2010) 39(3):173–87. doi: 10.1080/16506071003636046
24. Gun SY, Titov N, Andrews G. Acceptability of Internet treatment of anxiety and depression. Australas Psychiatry (2011) 19(3):259–64. doi: 10.3109/10398562.2011.562295
25. Haas LJ, Malouf JL. Keeping up the good work: A practitioner"s guide to mental health ethics. Sarasota, FL, US; Professional Resource Press/Professional Resource Exchange (2002).
26. Drum KB, Littleton HL. Therapeutic boundaries in telepsychology: Unique issues and best practice recommendations. Prof Psychol: Res Pract (2014) 45(5):309–15. doi: 10.1037/a0036127
27. Montalto M. The ethical implications of using technology in psychological testing and treatment. Ethical Hum Psychol Psychiatry: Int J Crit Inq (2014) 16(2):127–36. doi: 10.1891/1559-4343.16.2.127
28. Van Wynsberghe A, Gastmans C. Telepsychiatry and the meaning of in-person contact: A preliminary ethical appraisal. Med Health Care Philos (2009) 12(4):469–76. doi: 10.1007/s11019-009-9214-y
29. Holmes K. Ethical practice online: An exploration of provider liability risk among practitioners in the emerging field of online therapy. Doctor of Philosophy: Capella University (2008a).
30. Barnett JE, Scheetz K. Technological advances and telehealth: Ethics, law, and the practice of psychotherapy. Psychother: Theory Res Pract Training (2003) 40(1/2):86–93. doi: 10.1037/0033-3204.40.1-2.86
31. Morland LA, Poizner JM, Williams KE, Masino TT, Thorp SR. Home-based clinical video teleconferencing care: Clinical considerations and future directions. Int Rev Psychiatry (2015) 27(6):504–12. doi: 10.3109/09540261.2015.1082986
32. Mallen MJ, Vogel DL, Rochlen AB. The practical aspects of online counseling: Ethics, training, technology, and competency. Couns Psychol (2005) 33(6):776–818. doi: 10.1177/0011000005278625
33. Proudfoot JG. Computer-based treatment for anxiety and depression: Is it feasible? Is it effective? Neurosci Biobehav Rev (2004) 28(3):353–63. doi: 10.1016/j.neubiorev.2004.03.008
34. Malhotra S, Chakrabarti S, Shah R. Telepsychiatry: Promise, potential, and challenges. Indian J Psychiatry (2013) 55(1):3–11. doi: 10.4103/0019-5545.105499
35. Fraser L. Etherapy: Ethical and clinical considerations for Version 7 of the World Professional Association for Transgender Health's Standards of Care. Int J Transgenderism (2009) 11(4):247–63. doi: 10.1080/15532730903439492
36. Kramer GM, Mishkind MC, Luxton DD, Shore JH. Managing risk and protecting privacy in telemental health: An overview of legal, regulatory, and risk-management issues. In: Myers K, Turvey CL, editors. Telemental health: Clinical, technical, and administrative foundations for evidence-based practice. Elsevier: Amsterdam, Netherlands (2013). p. 83–107.
37. Rummell CM, Joyce NR. “So wat do u want to wrk on 2day?”: The ethical implications of online counseling. Ethics Behav (2010) 20(6):482–96. doi: 10.1080/10508422.2010.521450
38. Mishna F, Fantus S, McInroy LB. Informal use of information and communication technology: Adjunct to traditional face-to-face social work practice. Clin Soc Work J (2017) 45(1):49–55. doi: 10.1007/s10615-016-0576-3
39. Craig SL, Lorenzo MVC. Can information and communication technologies support patient engagement? A review of opportunities and challenges in health social work. Soc Work In Health Care (2014) 53(9):845–64. doi: 10.1080/00981389.2014.936991
40. Simpson S, Richardson LK, Pelling N. Introduction to the special issue “Telepsychology: Research and practice”. Aust Psychol (2015) 50(4):249–51. doi: 10.1111/ap.12146
41. Smiley PA, VandeCreek L. Problems and solutions with online therapy. In: VandeCreek L, Allen JB, editors. Innovations in clinical practice: Focus on health & wellness. Sarasota, FL, US: Professional Resource Press/Professional Resource Exchange (2005). p. 187–97.
42. Finfgeld DL. Psychotherapy in cyberspace. J Am Psychiatr Nurses Assoc (1999) 5(4):105–10. doi: 10.1016/S1078-3903(99)90008-3
43. Alleman JR. Online counseling: The Internet and mental health treatment. Psychother: Theory Res Pract Training (2002) 39(2):199–209. doi: 10.1037/0033-3204.39.2.199
44. Chaet D, Clearfield R, Sabin JE, Skimming K. Ethical practice in telehealth and telemedicine. J Gen Internal Med (2017) 32(10):1136–40. doi: 10.1007/s11606-017-4082-2
45. Nelson E-L, Davis K, Velasquez SE. Ethical considerations in providing mental health services over videoteleconferencing. In: Myers K, Turvey CL, editors. Telemental health: Clinical, technical, and administrative foundations for evidence-based practice. Amsterdam, Netherlands: Elsevier (2013). p. 47–62.
46. Valdagno M, Goracci A, di Volo S, Fagiolini A. Telepsychiatry: New perspectives and open issues. CNS Spectrums (2014) 19(6):479–81. doi: 10.1017/s1092852913000916
47. Barak A. Psychological applications on the Internet: A discipline on the threshold of a new millennium. Appl Prev Psychol (1999) 8(4):231–45. doi: 10.1016/s0962-1849(05)80038-1
48. Gupta K, Sinha A, Bhola P. Intersections between ethics and technology: Online client-therapist interactions. In: Bhola P, Raguram A, editors. Ethical issues in counselling and psychotherapy practice: Walking the line. New York, NY, US: Springer Science + Business Media (2016). p. 169–86.
49. Reed GM, McLaughlin CJ, Milholland K. Ten interdisciplinary principles for professional practice in telehealth: Implications for psychology. Prof Psychol: Res Pract (2000) 31(2):170–8. doi: 10.1037//0735-7028.31.2.170
50. Barnwell SS. The accidental telepsychologist: Creating opportunities in a burgeoning field. In: Maheu MM, Drude KP, Wright SD, editors. Career paths in telemental health. Cham, Switzerland: Springer International Publishing (2017). p. 131–8.
51. Lau PL, Aga Mohd Jaladin R, Abdullah HS. Understanding the two sides of online counseling and their ethical and legal ramifications. Proc Soc Behav Sci (2013) 103:1243–51. doi: 10.1016/j.sbspro.2013.10.453
52. Norman S. The use of telemedicine in psychiatry. J Psychiatr Ment Health Nurs (2006) 13(6):771–7. doi: 10.1111/j.1365-2850.2006.01033.x
53. Frueh BC, Deitsch SE, Santos AB, Gold PB, Johnson MR, Meisler N, et al. Procedural and methodological issues in telepsychiatry research and program development. Psychiatr Serv (2000) 51(12):1522–7. doi: 10.1176/appi.ps.51.12.1522
54. Frankish K, Ryan C, Harris A. Psychiatry and online social media: Potential, pitfalls and ethical guidelines for psychiatrists and trainees. Australas Psychiatry (2012) 20(3):181–7. doi: 10.1177/1039856212447881
55. Koocher GP. Twenty-first century ethical challenges for psychology. Am Psychol (2007) 62(5):375–84. doi: 10.1037/0003-066X.62.5.375
56. Childress CA. Ethical issues in providing online psychotherapeutic interventions. J Med Internet Res (2000) 2(1):e5. doi: 10.2196/jmir.2.1.e5
57. Gamble N, Boyle C, Morris ZA. Ethical practice in telepsychology. Aust Psychol (2015) 50(4):292–8. doi: 10.1111/ap.12133
58. Haas LJ, Benedict JG, Kobos JC. Psychotherapy by telephone: Risks and benefits for psychologists and consumers. Prof Psychol: Res Pract (1996) 27(2):154–60. doi: 10.1037/0735-7028.27.2.154
59. Heinlen KT, Welfel ER, Richmond EN, Rak CF. The scope of WebCounseling: A survey of services and compliance with NBCC Standards for the ethical practice of WebCounseling. J Couns Dev (2003b) 81(1):61–9. doi: 10.1002/j.1556-6678.2003.tb00226.x
60. Fantus S, Mishna F. The ethical and clinical implications of utilizing cybercommunication in face-to-face therapy. Smith Coll Stud In Soc Work (2013) 83(4):466–80. doi: 10.1080/00377317.2013.833049
61. Childress CA, Asamen JK. The emerging relationship of psychology and the Internet: Proposed guidelines for conducting Internet intervention research. Ethics Behav (1998) 8(1):19–35. doi: 10.1207/s15327019eb0801_2
62. Palomares RS, Miller TW. Security and transmission of data and information. In: Campbell LF, Millán F, Martin JN, editors. A telepsychology casebook: Using technology ethically and effectively in your professional practice. Washington, DC, US: American Psychological Association (2018). p. 83–98.
64. Harris B, Birnbaum R. Ethical and legal implications on the use of technology in counselling. Clin Soc Work J (2015) 43(2):133–41. doi: 10.1007/s10615-014-0515-0
65. Midkiff DM, Wyatt WJ. Ethical issues in the provision of online mental health services (etherapy). J Technol In Hum Serv (2008) 26(2/4):310–32. doi: 10.1080/15228830802096994
66. Gore PA Jr., Leuwerke WC. Technological advances: Implications for counseling psychology research, training, and practice. In: Brown SD, Lent RW, editors. Handbook of counseling psychology, 4th ed. Hoboken, NJ, US: John Wiley & Sons Inc (2008). p. 38–53.
67. Ford GG. Ethical reasoning for mental health professionals. Thousand Oaks, CA, US: Sage Publications, Inc. (2006).
68. Lovejoy TI, Demireva PD, Grayson JL, McNamara JR. Advancing the practice of online psychotherapy: An application of Rogers’ diffusion of innovations theory. Psychother: Theory Res Pract Training (2009) 46(1):112–24. doi: 10.1037/a0015153
69. Ames J. Counselling online in HE: Opportunities and challenges. In: Mair D, editor. Short-term counselling in higher education: Context, theory and practice New York, NY, US: Routledge/Taylor & Francis Group: (2016). p. 179–96.
70. DeMers ST, Harris EA, Baker DC. Interjurisdictional practice. In: Campbell LF, Millán F, Martin JN, editors. A telepsychology casebook: Using technology ethically and effectively in your professional practice. Washington, DC, US: American Psychological Association (2018). p. 141–64.
71. Maheu MM, McMenamin J, Pulier ML. Optimizing the use of technology in psychology with best practice principles. In: Koocher GP, Norcross JC, Greene BA, editors. Psychologists’ desk reference, 3rd ed. New York, NY, US: Oxford University Press (2013). p. 695–9.
72. Derse AR, Miller TE. Net effect: Professional and ethical challenges of medicine online. Cambridge Q Healthc Ethics (2008) 17(4):453–64. doi: 10.1017/s0963180108080572
73. Regueiro V, McMartin J, Schaefer C, Woody JM. Efficacy, efficiency, and ethics in the provision of telepsychology services: Emerging applications for international workers. J Psychol Theol (2016) 44(4):290–302. doi: 10.1177/009164711604400404
74. Mattison M. Social work practice in the digital age: Therapeutic e-mail as a direct practice methodology. Soc Work (2012) 57(3):249–58. doi: 10.1093/sw/sws021
75. Lloyd MG. Have you had a long-distance therapeutic relationship? You will. Ethics Behav (1996) 6(2):170–2. doi: 10.1207/s15327019eb0602_10
76. Finn J, Bruce S. The LivePerson model for delivery of etherapy services: A case study. J Technol In Hum Serv (2008) 26(2/4):282–309. doi: 10.1080/15228830802096820
77. Martin AC. Legal, clinical, and ethical issues in teletherapy. In: Scharff JS, editor. Psychoanalysis online: Mental health, teletherapy, and training. Karnac Books: London, England (2013). p. 75–84.
78. Richards D, Viganó N. Online counseling: A narrative and critical review of the literature. J Clin Psychol (2013) 69(9):994–1011. doi: 10.1002/jclp.21974
79. Baker KD, Ray M. Online counseling: The good, the bad, and the possibilities. Couns Psychol Q (2011) 24(4):341–6. doi: 10.1080/09515070.2011.632875
80. Bhuvaneswar CG, Gutheil TG. E-mail and psychiatry: Some psychotherapeutic and psychoanalytic perspectives. Am J Psychother (2008) 62(3):241–61. doi: 10.1176/appi.psychotherapy.2008.62.3.241
81. Fleming DA, Edison KE, Pak H. Telehealth ethics. Telemed J e-Health (2009) 15(8):797–803. doi: 10.1089/tmj.2009.0035
82. Deen SR, Withers A, Hellerstein DJ. Mental health practitioners' use and attitudes regarding the Internet and social media. J Psychiatr Pract (2013) 19(6):454–63. doi: 10.1097/01.pra.0000438184.74359.88
83. Naskar S, Victor R, Das H, Nath K. Telepsychiatry in India: Where do we stand? A comparative review between global and Indian telepsychiatry programs. Indian J psychol Med (2017) 39(3):223–42. doi: 10.4103/0253-7176.207329
84. Golkaramnay V, Wangemann T, Dogs J, Dogs P, Kordy H. Neue Br¨cken für Lücken in der psychotherapeutischen Versorgung durch das Internet: Hoffnungen, Herausforderungen und ein Lösungsansatz [New bridges for gaps in psychotherapeutic service provision by the Internet: Hopes, challenges and a solution]. Psychother Psychosom Med Psychol (2003) 53(9-10):399–405. doi: 10.1055/s-2003-42175
85. Dyer KA, Thompson CD. Medical Internet ethics: A field in evolution. Stud In Health Technol Inf (2001) 84(Pt 2):1287–91.
86. Andersen AJW, Svensson T. Internet-based mental health services in Norway and Sweden: Characteristics and consequences. Admin Policy In Ment Health Ment Health Serv Res (2013) 40(2):145–53. doi: 10.1007/s10488-011-0388-2
87. Sampson JP, Kolodinsky RW, Greeno BP. Counseling on the information highway: Future possibilities and potential problems. J Couns Dev (1997) 75(3):203–12. doi: 10.1002/j.1556-6676.1997.tb02334.x
88. Yager J. E-mail therapy for anorexia nervosa: Prospects and limitations. Eur Eat Disord Rev (2003) 11(3):198–209. doi: 10.1002/erv.526
89. Satalkar P, Shrivastava S, De Sousa A. Internet-mediated psychotherapy: Are we ready for the ethical challenges? Indian J Med Ethics (2015) 12(4):220–7.
90. Clark PA, Capuzzi K, Harrison J. Telemedicine: Medical, legal and ethical perspectives. Med Sci Monitor (2010) 16(12):RA261–72.
91. Manhal-Baugus M. E-therapy: Practical, ethical, and legal issues. CyberPsychol Behav (2001) 4(5):551–63. doi: 10.1089/109493101753235142
92. Rochlen AB, Zack JS, Speyer C. Online therapy: Review of relevant definitions, debates, and current empirical support. J Clin Psychol (2004) 60(3):269–83. doi: 10.1002/jclp.10263
93. Chin JJ. Medical professionalism in the Internet age. Ann Acad Med Singapore (2010) 39(5):345–7.
94. Gunter TD, Srinivasaraghavan J, Terry NP. Misinformed regulation of electronic medicine is unfair to responsible telepsychiatry. J Am Acad Psychiatry Law (2003) 31(1):10–4.
95. Gupta A, Agrawal A. Internet counselling and psychological services. Soc Sci Int (2012) 28(1):105–22.
96. Holmes K. How ethically we practice online: An exploration of potential online provider liability. Annu Rev CyberTher Telemed (2008b) 6:97–102.
97. Kaplan EH. Telepsychotherapy: Psychotherapy by telephone, videotelephone, and computer videoconferencing. J Psychother Pract Res (1997) 6(3):227–37.
98. McClure RF, Livingston RB, Livingston KH, Gage R. A survey of practicing psychotherapists. J Prof Couns: Pract Theory Res (2005) 33(1):35–46. doi: 10.1080/15566382.2005.12033811
99. McMinn MR, Orton JJ, Woods SW. Technology in clinical practice. J Psychol Christ (2008) 27(1):56–60.
100. Miller TE, Derse AR. Between strangers: The practice of medicine online. Health Aff (2002) 21(4):168–79. doi: 10.1377/hlthaff.21.4.168
101. Olasupo MO, Atiri OS. E-therapy: Contemporary tool in psychotherapy. Ife PsychologIA: Int J (2013) 21(3):408–13.
102. Pergament D. Internet psychotherapy: Current status and future regulation. Health Matrix: J Law Med (1998) 8(2):233–79.
103. Reamer FG. Social work in a digital age: Ethical and risk management challenges. Soc Work (2013) 58(2):163–72. doi: 10.1093/sw/swt003
104. Riemer-Reiss ML. Utilizing distance technology for mental health counseling. J Ment Health Couns (2000) 22(3):189–203.
105. Swenson J.E., III, Smothermon J, Rosenblad SR, Chalmers B. The future is here: Ethical practices of telemental health. J Psychol Christ (2016) 35(4):310–9.
106. Murphy L, Mitchell D, Hallett R. A comparison of client characteristics in cyber and in-person counseling. Annu Rev CyberTher Telemed (2011) 9:121–4.
107. Nagarajan M, S Y. Mental health counsellors' perceptions on use of technology in counselling. Curr Psychol (2019), 1–7. doi: 10.1007/s12144-018-0104-4
108. Doherty GW. Mental health and the new technologies. PsycCRITIQUES (2005) 50(11). doi: 10.1037/050042
110. Roberts BT. Telemental health comes of age with step-by-step guide (and choices) to incorporate into practice. PsycCRITIQUES (2016) 61(46). doi: 10.1037/a0040597
111. Chan S, Li L, Torous J, Gratzer D, Yellowlees PM. Review of use of asynchronous technologies incorporated in mental health care. Curr Psychiatry Rep (2018) 20(85). doi: 10.1007/s11920-018-0954-3
113. Goss S, Anthony KE. The development of ethical guidelines for online counselling and psychotherapy. In: Langrial SU, editor. Web-based behavioral therapies for mental disorders. Hershey, PA: IGI Global (2018). p. 212–40.
114. Adams Larsen M, Juntunen C. Informed consent. In: Campbell LF, Millán FA, Martin JN, editors. A telepsychology casebook: Using technology ethically and effectively in your professional practice. Washington, DC, US: American Psychological Association (2018). p. 47–67.
115. Alao AO, Soderberg M, Pohl EL, Alao AL. Cybersuicide: Review of the role of the Internet on suicide. CyberPsychol Behav (2006) 9(4):489–93. doi: 10.1089/cpb.2006.9.489
116. Baker DC, Bufka LF. Preparing for the telehealth world: Navigating legal, regulatory, reimbursement, and ethical issues in an electronic age. Prof Psychol: Res Pract (2011) 42(6):405–11. doi: 10.1037/a0025037
117. Barnett JE, Kolmes K. The practice of tele-mental health: Ethical, legal, and clinical issues for practitioners. Pract Innovations (2016) 1(1):53–66. doi: 10.1037/pri0000014
118. Barnett JE. Online counseling: New entity, new challenges. Couns Psychol (2005) 33(6):872–80. doi: 10.1177/0011000005279961
119. Barnett JE. Utilizing technological innovations to enhance psychotherapy supervision, training, and outcomes. Psychotherapy (2011) 48(2):103–8. doi: 10.1037/a0023381
120. Barsky AE. Social work practice and technology: Ethical issues and policy responses. J Technol In Hum Serv (2017) 35(1):8–19. doi: 10.1080/15228835.2017.1277906
121. Bauer S, Golkaramnay V, Kordy H. E-Mental-Health: Neue Medien in der psychosozialen Versorgung [E-mental-health: The use of new technologies in psychosocial care]. Psychotherapeut (2005) 50(1):7–15. doi: 10.1007/s00278-004-0403-0
122. Ben-Zeev D, Kaiser SM, Krzos I. Remote “hovering” with individuals with psychotic disorders and substance use: Feasibility, engagement, and therapeutic alliance with a text-messaging mobile interventionist. J Dual Diag (2014) 10(4):197–203. doi: 10.1080/15504263.2014.962336
123. Blom K, Tillgren HT, Wiklund T, Danlycke E, Forssén M, Söderström A, et al. Internet-vs. group-delivered cognitive behavior therapy for insomnia: A randomized controlled non-inferiority trial. Behav Res Ther (2015) 70:47–55. doi: 10.1016/j.brat.2015.05.002
124. Bradley LJ, Hendricks B, Lock R, Whiting PP, Parr G. E-mail communication: Issues for mental health counselors. J Ment Health Couns (2011) 33(1):67–79. doi: 10.17744/mehc.33.1.05208025375v03r7
125. Campbell LF, Millán FA, Martin JN. Afterword. In: Campbell LF, Millán F, Martin JN, editors. A telepsychology casebook: Using technology ethically and effectively in your professional practice. Washington, DC, US: American Psychological Association (2018b). p. 165–6.
126. Canning S, Hauser MJ, Gutheil TG, Bursztajn HJ. Communications in psychiatric practice: Decision making and the use of the telephone. In: Gutheil TG, Bursztajn HJ, Brodsky A, Alexander V, editors. Decision making in psychiatry and the law. Baltimore, MD, US: Williams & Wilkins Co (1991). p. 227–35.
127. Close RE. Adlerian counseling in a virtual world: Some implications of Internet practice for the development of Gemeinschaftsgefühl. J Individ Psychol (2015) 71(2):155–62. doi: 10.1353/jip.2015.0017
128. Colbow AJ. Looking to the future: Integrating telemental health therapy into psychologist training. Training Educ In Prof Psychol (2013) 7(3):155–65. doi: 10.1037/a0033454
129. Dart EH, Whipple HM, Pasqua JL, Furlow CM. Legal, regulatory, and ethical issues in telehealth technology. In: Luiselli JK, Fischer AJ, editors. Computer-assisted and web-based innovations in psychology, special education, and health. San Diego, CA, US: Elsevier Academic Press (2016). p. 339–63.
130. Davis AW. Ethical issues for psychologists using communication technology: An Australian perspective on service provision flexibility. Prof Psychol: Res Pract (2014) 45(5):303–8. doi: 10.1037/a0037081
131. De Weger E, Macinnes D, Enser J, Francis SJ, Jones FW. Implementing video conferencing in mental health practice. J Psychiatr Ment Health Nurs (2013) 20(5):448–54. doi: 10.1111/j.1365-2850.2012.01947.x
132. Depp CA, Mausbach B, Granholm E, Cardenas V, Ben-Zeev D, Patterson TL, et al. Mobile interventions for severe mental illness: Design and preliminary data from three approaches. J Nerv Ment Dis (2010) 198(10):715–21. doi: 10.1097/NMD.0b013e3181f49ea3
133. Derrig-Palumbo K, Zeine F. Online therapy: A therapist’s guide to expanding your practice. New York, NY, US: W. W. Norton & Company (2005).
134. Dickey RA. Perceived risks and benefits of emerging technologies in professional psychology. Doctor of Psychology (PsyD): George Fox University (2013).
135. Enander J, Andersson E, Mataix-Cols D, Lichtenstein L, Alström K, Andersson G, et al. Therapist guided Internet based cognitive behavioural therapy for body dysmorphic disorder: Single blind randomised controlled trial. BMJ: Br Med J (2016) 352:1–9. doi: 10.1136/bmj.i241
136. Ferrer DC, Yellowlees PM. Telepsychiatry: Licensing and professional boundary concerns. Virtual Mentor (2012) 14(6):477–82. doi: 10.1001/virtualmentor.2012.14.6.pfor1-1206
137. Finn J, Barak A. A descriptive study of e-counsellor attitudes, ethics, and practice. Couns Psychother Res (2010) 10(4):268–77. doi: 10.1080/14733140903380847
138. Frame MW. The ethics of counseling via the Internet. Family J (1997) 5(4):328–30. doi: 10.1177/1066480797054009
139. Giotakos O. Modern technologies and applications and community psychiatry. In: Stylianidis S, editor. Social and community psychiatry: Towards a critical, patient-oriented approach. Springer International Publishing: Cham, Switzerland (2016). p. 331–41.
140. Graff CA, Hecker LL. E-therapy: Developing an ethical online practice. In: Hecker L, editor. Ethics and professional issues in couple and family therapy. New York, NY, US: Routledge/Taylor & Francis Group (2010). p. 243–55.
141. Haberstroh S, Barney L, Foster N, Duffey T. The ethical and legal practice of online counseling and psychotherapy: A review of mental health professions. J Technol In Hum Serv (2014) 32(3):149–57. doi: 10.1080/15228835.2013.872074
142. Harris E, Younggren JN. Risk management in the digital world. Prof Psychol: Res Pract (2011) 42(6):412–8. doi: 10.1037/a0025139
143. Harwood TM, Pratt D, Beutler LE, Bongar BM, Lenore S, Forrester BT. Technology, telehealth, treatment enhancement, and selection. Prof Psychol: Res Pract (2011) 42(6):448–54. doi: 10.1037/a0026214
144. Heinlen KT, Welfel ER, Richmond EN, O'Donnell MS. The nature, scope, and ethics of psychologists’ e-therapy Web sites: What consumers find when surfing the Web. Psychother: Theory Res Pract Training (2003a) 40(1/2):112–24. doi: 10.1037/0033-3204.40.1-2.112
145. Helm S, Koyanagi C, Else I, Horton M, Fukuda M. The University of Hawai‘i Rural Health Collaboration: Partnerships to provide adult telepsychiatry services. Psychiatr Serv (2010) 61(10):961–3. doi: 10.1176/appi.ps.61.10.961
146. Hilgart M, Thorndike FP, Pardo J, Ritterband LM. Ethical issues of web-based interventions and online therapy. In: Leach MM, Stevens MJ, Lindsay G, Ferrero A, Korkut Y, editors. The Oxford handbook of international psychological ethics. New York, NY, US: Oxford University Press (2012). p. 161–75.
147. Hilty DM, Luo JS, Morache C, Marcelo DA, Nesbitt TS. Telepsychiatry: An overview for psychiatrists. CNS Drugs (2002) 16(8):527–48. doi: 10.2165/00023210-200216080-00003
148. Holmes LG. Delivering mental health services on-line: Current issues. CyberPsychol Behav (1998) 1(1):19–24. doi: 10.1089/cpb.1998.1.19
149. Hsiung RC. Suggested principles of professional ethics for the online provision of mental health services. Telemed J E-Health (2001) 7(1):39–45. doi: 10.1089/153056201300093895
150. Hsiung RC. Suggested principles of professional ethics for e-therapy. In: Hsiung RC, editor. e-Therapy: Case studies, guiding principles, and the clinical potential of the Internet. New York, NY, US: W. W. Norton & Company (2002). p. 150–65.
151. Jennett PA, Affleck Hall L, Hailey D, Ohinmaa A, Anderson C, Thomas R, et al. The socio-economic impact of telehealth: A systematic review. J Telemed Telecare (2003) 9(6):311–20. doi: 10.1258/135763303771005207
152. Jones RB, Ashurst EJ. Online anonymous discussion between service users and health professionals to ascertain stakeholder concerns in using e-health services in mental health. Health Inf J (2013) 19(4):281–99. doi: 10.1177/1460458212474908
153. Kassaw K, Gabbard GO. The ethics of e-mail communication in psychiatry. Psychiatr Clinics North America (2002) 25(3):665–74. doi: 10.1016/S0193-953X(02)00005-9
154. Kenny MC, McEachern AG. Telephone counseling: Are offices becoming obsolete? J Couns Dev (2004) 82(2):199–202. doi: 10.1002/j.1556-6678.2004.tb00302.x
155. Klaus CL, Hartshorne TS. Ethical implications of trends in technology. J Individ Psychol (2015) 71(2):195–204. doi: 10.1353/jip.2015.0012
156. Knaevelsrud C, Jager J, Maercker A. Internet-Psychotherapie: Wirksamkeit und Besonderheiten der therapeutischen Beziehung [Online-therapy: Effectiveness and peculiarities of the therapeutic relationship]. Verhaltenstherapie (2004) 14(3):174–83. doi: 10.1159/000080913
157. Kolmes K. Social media in the future of professional psychology. Prof Psychol: Res Pract (2012) 43(6):606–12. doi: 10.1037/a0028678
158. Kotsopoulou A, Melis A, Koutsompou VI, Karasarlidou C. E-therapy: The ethics behind the process. Proc Comput Sci (2015) 65:492–9. doi: 10.1016/j.procs.2015.09.120
159. Kraus R. Ethical and legal considerations for providers of mental health services online. In: Kraus R, Zack JS, Stricker G, editors. Online counseling: A handbook for mental health professionals. New York, NY, US: Elsevier Science (2004). p. 123–44.
160. Landry Poole JM, Crow BE. Confidentiality of data and information. In: Campbell LF, Millán F, Martin JN, editors. A telepsychology casebook: Using technology ethically and effectively in your professional practice. American Psychological Association: Washington, DC, US (2018). p. 69–82.
161. Lustgarten SD, Colbow AJ. Ethical concerns for telemental health therapy amidst governmental surveillance. Am Psychol (2017) 72(2):159–70. doi: 10.1037/a0040321
162. Luxton DD, Nelson E-L, Maheu MM. Establishing a telemental health practice. In: Luxton DD, Nelson E-L, Maheu MM, editors. A practitioner’s guide to telemental health: How to conduct legal, ethical, and evidence-based telepractice. Washington, DC, US: American Psychological Association (2016c). p. 47–56.
163. Luxton DD, Nelson E-L, Maheu MM. Ethical telepractice with diverse populations. In: Luxton DD, Nelson E-L, Maheu MM, editors. A practitioner’s guide to telemental health: How to conduct legal, ethical, and evidence-based telepractice. Washington, DC, US: American Psychological Association (2016d). p. 109–20.
164. Luxton DD, Nelson E-L, Maheu MM. Ethical, legal, and other risk management considerations. In: Luxton D, Nelson E-L, Maheu MM, editors. A practitioner’s guide to telemental health: How to conduct legal, ethical, and evidence-based telepractice. Washington, DC, US: American Psychological Association (2016e). p. 31–46.
165. Luxton DD, Nelson E-L, Maheu MM. Introduction. In: Luxton DD, Nelson E-L, Maheu MM, editors. A practitioner’s guide to telemental health: How to conduct legal, ethical, and evidence-based telepractice. Washington, DC, US: American Psychological Association (2016f). p. 3–8.
166. Luxton DD, Nelson E-L, Maheu MM. Overview of telemental health technologies. In: Luxton DD, Nelson E-L, Maheu MM, editors. A practitioner"s guide to telemental health: How to conduct legal, ethical, and evidence-based telepractice. Washington, DC, US: American Psychological Association (2016g). p. 17–29.
167. Luxton DD, Nelson E-L, Maheu MM. Providing direct clinical care. In: Luxton DD, Nelson E-L, Maheu MM, editors. A practitioner"s guide to telemental health: How to conduct legal, ethical, and evidence-based telepractice. American Psychological Association: Washington, DC, US (2016h). p. 71–84.
168. Luxton DD, Nelson E-L, Maheu MM. Safety planning and emergency management. In: Luxton DD, Nelson E-L, Maheu MM, editors. A practitioner"s guide to telemental health: How to conduct legal, ethical, and evidence-based telepractice. Washington, DC, US: American Psychological Association (2016i). p. 57–70.
169. Maheu MM, Pulier ML, Wilhelm FH, McMenamin JP, Brown-Connolly NE. The mental health professional and the new technologies: A handbook for practice today. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers (2005).
170. Masi D, Freedman M. The use of telephone and on line technology in assessment, counseling, and therapy. Empl Assist Q (2001) 16(3):49–63. doi: 10.1300/J022v16n03_05
171. McCarty D, Clancy C. Telehealth: Implications for social work practice. Soc Work (2002) 47(2):153–61. doi: 10.1093/sw/47.2.153
172. Mishna F, Bogo M, Root J, Sawyer JL, Khoury-Kassabri M. “It just crept in”: The digital age and implications for social work practice. Clin Soc Work J (2012) 40(3):277–86. doi: 10.1007/s10615-012-0383-4
173. Morgan J, Lack C, Storch EA. The utilization of technology in the treatment of obsessive compulsive disorder. In: Berhardt LV, editor. Advances in medicine and biology: Hauppauge: Nova Science Publishers, Inc (2010). p. 161–76.
174. Murphy JM, Pomerantz AM. Informed consent: An adaptable question format for telepsychology. Prof Psychol: Res Pract (2016) 47(5):330–9. doi: 10.1037/pro0000098
175. Nelson E-L, Duncan AB. Cognitive behavioral therapy using televideo. Cogn Behav Pract (2015) 22(3):269–80. doi: 10.1016/j.cbpra.2015.03.001
176. Nelson E-L, Velasquez SE. Implementing psychological services over televideo. Prof Psychol: Res Pract (2011) 42(6):535–42. doi: 10.1037/a0026178
177. Norris L, Swartz L, Tomlinson M. Mobile phone technology for improved mental health care in South Africa: Possibilities and challenges. South Afr J Psychol (2013) 43(3):379–88. doi: 10.1177/0081246313493376
178. Perez-Garcia GJ. Ethics of telepsychiatry. In: Sadler JZ, Fulford KWM, van Staden W, editors. The Oxford handbook of psychiatric ethics. New York, NY, US: Oxford University Press (2015). p. 1346–59.
179. Putnam DE, Maheu MM. Online sexual addiction and compulsivity: Integrating web resources and behavioral telehealth in treatment. Sex Addict Compulsivity (2000) 7(1-2):91–112. doi: 10.1080/10720160008400209
180. Ragusea AS, VandeCreek L. Suggestions for the ethical practice of online psychotherapy. Psychother: Theory Res Pract Training (2003) 40(1/2):94–102. doi: 10.1037/0033-3204.40.1-2.94
181. Ragusea AS. The more things change, the more they stay the same: Ethical issues in the provision of telehealth. In: Knapp SJ, Gottlieb MC, Handelsman MM, VandeCreek LD, editors. APA handbook of ethics in psychology: Practice, teaching, and research. Washington, DC, US: American Psychological Association (2012). p. 183–98.
182. Reed RN, Messler EC, Coombs TE, Quevillon RP. Social media use and the acceptability of telepsychological services in rural populations. J Rural Ment Health (2014) 38(1):2–8. doi: 10.1037/rmh0000007
183. Rehm LP. How far have we come in teletherapy? Comment on “Telephone-Administered Psychotherapy”. Clin Psychol: Sci Pract (2008) 15(3):259–61. doi: 10.1111/j.1468-2850.2008.00136.x
184. Richards D, Viganò N. Online counseling. In: Yan Z, editor. Encyclopedia of cyber behavior. Hershey, PA, US: IGI Global (2012). p. 699–713.
185. Robinson P, Serfaty M. Computers, e-mail and therapy in eating disorders. Eur Eat Disord Rev (2003) 11(3):210–21. doi: 10.1002/erv.516
186. Robson D, Robson M. Ethical issues in Internet counselling. Couns Psychol Q (2000) 13(3):249–57. doi: 10.1080/09515070010037911
187. Rosenfield M. Electronic technology for social work education and practice: The application of telephone technology to counselling. J Technol In Hum Serv (2002) 20(1-2):173–81. doi: 10.1300/J017v20n01_13
188. Sabin JE, Harland JC. Professional ethics for digital age psychiatry: Boundaries, privacy, and communication. Curr Psychiatry Rep (2017) 19(9):55. doi: 10.1007/s11920-017-0815-5
189. Sabin JE, Skimming K. A framework of ethics for telepsychiatry practice. Int Rev Psychiatry (2015) 27(6):490–5. doi: 10.3109/09540261.2015.1094034
190. Sampson D, Mueller M. Integrating behavioral health into rural primary care clinics utilizing a telemental health model. In: Maheu MM, Drude KP, Wright SD, editors. Career paths in telemental health. Springer International Publishing: Cham, Switzerland (2017). p. 277–83.
191. Sansom-Daly UM, Wakefield CE, McGill BC, Wilson HL, Patterson P. Consensus among international ethical guidelines for the provision of videoconferencing-based mental health treatments. JMIR Ment Health (2016) 3(2):e17. doi: 10.2196/mental.5481
192. Santhiveeran J. Compliance of social work e-therapy websites to the NASW Code of Ethics. Soc Work In Health Care (2009) 48(1):1–13. doi: 10.1080/00981380802231216
193. Schopp LH, Demiris G, Glueckauf RL. Rural backwaters or front-runners? Rural telehealth in the vanguard of psychology practice. Prof Psychol: Res Pract (2006) 37(2):165–73. doi: 10.1037/0735-7028.37.2.165
194. Schwartz TJ, Lonborg SD. Security management in telepsychology. Prof Psychol: Res Pract (2011) 42(6):419–25. doi: 10.1037/a0026102
195. Shaw HE, Shaw SF. Critical ethical issues in online counseling: Assessing current practices with an ethical intent checklist. J Couns Dev (2006) 84(1):41–53. doi: 10.1002/j.1556-6678.2006.tb00378.x
196. Shore JH, Hilty DM, Yellowlees P. Emergency management guidelines for telepsychiatry. Gen Hosp Psychiatry (2007) 29(3):199–206. doi: 10.1016/j.genhosppsych.2007.01.013
197. Skinner A, Zack JS. Counseling and the Internet. Am Behav Sci (2004) 48(4):434–46. doi: 10.1177/0002764204270280
198. Stricker G. Psychotherapy in cyberspace. Ethics Behav (1996) 6(2):175–7. doi: 10.1207/s15327019eb0602_12
199. Taintor Z. Review of e-therapy: Case studies, guiding principles, and the clinical potential of the Internet. Psychiatr Serv (2003) 54(10):1422. doi: 10.1176/appi.ps.54.12.1584
200. Tang S, Helmeste D. Digital psychiatry. Psychiatry Clin Neurosci (2000) 54(1):1–10. doi: 10.1046/j.1440-1819.2000.00628.x
201. Terry NP. The legal implications of e-therapy. In: Hsiung RC, editor. e-therapy: Case studies, guiding principles, and the clinical potential of the Internet. New York, NY, US: W. W. Norton & Company (2002). p. 166–93.
202. Turvey CL, Myers K. Introduction. In: Myers K, Turvey CL, editors. Telemental health: Clinical, technical, and administrative foundations for evidence-based practice. Amsterdam, Netherlands: Elsevier (2013). p. 3–9.
203. Tyler JM, Sabella RA. Using technology to improve counseling practice: A primer for the 21st century. Alexandria, VA, US: American Counseling Association (2004).
204. Vally Z. Cybertherapy: Development and usage in the South African context. Ife PsychologIA: Int J (2006) 14(2):151–65. doi: 10.4314/ifep.v14i2.23716
205. Van Allen J, Roberts MC. Critical incidents in the marriage of psychology and technology: A discussion of potential ethical issues in practice, education, and policy. Prof Psychol: Res Pract (2011) 42(6):433–9. doi: 10.1037/a0025278
206. Wade ME, Moorhead HJH, Levitt DH. Online counseling. In: Levitt DH, Moorhead HJH, editors. Values and ethics in counseling: Real-life ethical decision making. New York, NY, US: Routledge/Taylor & Francis Group (2013). p. 195–201.
207. Wade VA, Eliott JA, Hiller JE. A qualitative study of ethical, medico-legal and clinical governance matters in Australian telehealth services. J Telemed Telecare (2012) 18(2):109–14. doi: 10.1258/jtt.2011.110808
208. Wallwork E. Ethical aspects of teletherapy. In: Scharff JS, editor. Psychoanalysis online: Mental health, teletherapy, and training. Karnac Books: London, England (2013). p. 85–94.
209. Wallwork E. Thinking ethically about beginning online work. In: Scharff JS, editor. Psychoanalysis online 2: Impact of technology on development, training, and therapy. London, England: Karnac Books (2015). p. 83–92.
210. Webb C, Orwig J. Expanding our reach: Telehealth and licensure implications for psychologists. J Clin Psychol In Med S (2015) 22(4):243–50. doi: 10.1007/s10880-015-9440-9
211. Weitz P. Establishing an online practice. In: Weitz P, editor. Psychotherapy 2.0: Where psychotherapy and technology meet. London, England: Karnac Books (2014). p. 147–89.
212. Welfel ER, Heinlen KT. Ethics in technology and mental health. In: Cucciare MA, Weingardt KR, editors. Using technology to support evidence-based behavioral health practices: A clinician"s guide. New York, NY, US: Routledge/Taylor & Francis Group (2010). p. 267–90.
213. Yuen EK, Goetter EM, Herbert JD, Forman EM. Challenges and opportunities in Internet-mediated telemental health. Prof Psychol: Res Pract (2012) 43(1):1–8. doi: 10.1037/a0025524
214. Basavarajappa C, Chand PK. Digital platforms for mental health-care delivery. Indian J psychol Med (2017) 39(5):703–6. doi: 10.4103/IJPSYM.IJPSYM_209_17
215. Bolle SR, Trondsen MV, Stensland GO, Tjora A. Usefulness of videoconferencing in psychiatric emergencies—a qualitative study. Health Technol (2018) 8(1-2):111–7. doi: 10.1007/s12553-017-0189-z
216. Ebert DD, Van Daele T, Nordgreen T, Karekla M, Compare A, Zarbo C, et al. Internet- and mobile-based psychological interventions: Applications, efficacy, and potential for improving mental health: A report of the EFPA E-Health Taskforce. Eur Psychol (2018) 23(2):167–87. doi: 10.1027/1016-9040/a000318
217. Eichenberg C, Hübner L. Psychoanalyse via Internet: Aktueller Stand der Diskussion um Möglichkeiten und Grenzen [Psychoanalysis via internet: Current state of the discussion on possibilities and limitations]. Psychotherapeut (2018) 63(4):283–90. doi: 10.1007/s00278-018-0294-0
218. Glueckauf RL, Maheu MM, Drude KP, Wells BA, Wang Y, Gustafson DJ, et al. Survey of psychologists' telebehavioral health practices: Technology use, ethical issues, and training needs. Prof Psychol: Res Pract (2018) 49(3):205–19. doi: 10.1037/pro0000188
219. Ignatowicz A, Atherton H, Bernstein CJ, Bryce C, Court R, Sturt J, et al. Internet videoconferencing for patient-clinician consultations in long-term conditions: A review of reviews and applications in line with guidelines and recommendations. Digit Health (2019) 5:1–27. doi: 10.1177/2055207619845831
220. Karyotaki E, Furukawa TA, Efthimiou O, Riper H, Cuijpers P. Guided or self-guided internet-based cognitive-behavioural therapy (iCBT) for depression? Study protocol of an individual participant data network meta-analysis. BMJ Open (2019) 9:e026820. doi: 10.1136/bmjopen-2018-026820
221. Lowman RL, Cooper SE. Emerging ethical issues and challenges. In: Lowman RL, Cooper SE, editors. The ethical practice of consulting psychology. Washington, DC, US: American Psychological Association (2018). p. 77–95.
222. Magnavita JJ. Intoduction: How can technology advance mental health treatment? In: Magnavita JJ, editor. Using technology in mental health practice. Washington, DC, US: : (2018). p. 3–10.
223. Reamer FG. Evolving standards of care in the age of cybertechnology. Behav Sci Law (2018) 36(2):257–69. doi: 10.1002/bsl.2336
224. Rubeis G, Steger F. Internet- und mobilgestützte Interventionen bei psychischen Stoürungen: Implementierung in Deutschland aus ethischer Sicht [Internet and mobile-assisted interventions in mental disorders: Implementation in Germany from an ethical perspective]. Nervenarzt (2019) 90(5):497–502. doi: 10.1007/s00115-018-0663-5
225. Shore JH, Yellowlees P, Caudill R, Johnston B, Turvey C, Mishkind M, et al. Policy: Best practices in videoconferencing-based telemental health April 2018. Telemed J e-Health (2018) 40(11):827–32. doi: 10.1089/tmj.2018.0237
226. Smucker Barnwell S, Campbell LF. Ethical and legal aspects of the practice of teletherapy. In: Walfish S, Barnett JE, Zimmerman J, editors. Handbook of private practice: Keys to success for mental health practitioners. New York, NY, US: Oxford University Press (2017). p. 492–505.
227. Sobelman SA, Santopietro JM. Managing risk: Aligning technology use with the law, ethics codes, and practice standards. In: Magnavita JJ, editor. Using technology in mental health practice. American Psychological Association: Washington, DC, US (2018). p. 13–24.
228. Ventriglio A, Torales J, Castaldelli-Maia J. Telepsychiatry and social psychiatry. Int J Soc Psychiatry (2017) 63(5):387–8. doi: 10.1177/0020764017694661
229. Zimmerman J, Magnavita JJ. Adopting new technology for your practice: How to assess fit and risks. In: Magnavita JJ, editor. Using technology in mental health practice. Washington, DC, US: American Psychological Association (2018). p. 209–21.
230. Haveren RV, Habben CJ, Kuther TL. New psychologists online: Changing the face of psychology through technology. In: Morgan RD, Kuther TL, Habben CJ, editors. Life after graduate school in psychology: Insider’s advice from new psychologists. New York, NY, US: Psychology Press (2005). p. 321–7.
231. Monnier J, Knapp RG, Frueh BC. Recent advances in telepsychiatry: An updated review. Psychiatr Serv (2003) 54(12):1604–9. doi: 10.1176/appi.ps.54.12.1604
232. Palomares RS. Standards of care in the delivery of telepsychology services. In: Campbell LF, Millán F, Martin JN, editors. A telepsychology casebook: Using technology ethically and effectively in your professional practice. Washington, DC, US: American Psychological Association (2018). p. 27–46.
233. Shapiro DE, Schulman CE. Ethic and legal issues in e-mail therapy. Ethics Behav (1996) 6(2):107–24. doi: 10.1207/s15327019eb0602_3
234. Smucker Barnwell S, McCann R, McCutcheon S. Competence of the psychologist. In: Campbell LF, Millán F, Martin JN, editors. A telepsychology casebook: Using technology ethically and effectively in your professional practice. Washington, DC, US: American Psychological Association (2018). p. 7–26.
235. Welfel ER. Emerging issues in the duty to protect. In: Werth JL Jr., Welfel ER, Benjamin GAH, editors. The duty to protect: Ethical, legal, and professional considerations for mental health professionals. Washington, DC, US: American Psychological Association (2009). p. 229–47.
236. Wiederhold MD. Review of technology in counselling and psychotherapy: A practitioner’s guide. CyberPsychol Behav (2004) 7(1):119–20. doi: 10.1089/109493104322820192
237. Recupero PR, Felthous AR. Introduction to this special issue: The internet, cybertechnology and the law. Behav Sci Law (2018) 36(2):131–5. doi: 10.1002/bsl.2341
238. Jenkins PE, Luck A, Burrows A, Boughton N. Comparison of face-to-face versus email guided self-help for binge eating: Study protocol for a randomised controlled trial. Trials (2014) 15:181. doi: 10.1186/1745-6215-15-181
239. Bloom JW. The ethical practice of WebCounseling. Br J Guid Couns (1998) 26(1):53–9. doi: 10.1080/03069889800760061
240. Campbell LF, Millán F, Martin JN. Introduction. In: Campbell LF, Millán F, Martin JN, editors. A telepsychology casebook: Using technology ethically and effectively in your professional practice. Washington, DC, US: American Psychological Association (2018a). p. 3–6.
241. Fisher CB, Fried AL. Internet-mediated psychological services and the American Psychological Association Ethics Code. In: Bersoff DN, editor. Ethical conflicts in psychology, 4th ed. Washington, DC, US: American Psychological Association (2008). p. 376–83.
242. Huggins R. Using mobile phone communication for therapeutic intervention. In: Goss S, Anthony K, Stretch LS, Nagel DM, editors. Technology in mental health: Applications in practice, supervision and training, 2nd ed. Springfield, IL, US: Charles C Thomas Publisher (2016). p. 28–42.
243. Hyler SE, Gangure DP. Legal and ethical challenges in telepsychiatry. J Psychiatr Pract (2004) 10(4):272–6. doi: 10.1097/00131746-200407000-00011
244. Maheu MM, Gordon BL. Counseling and therapy on the Internet. Prof Psychol: Res Pract (2000) 31(5):484–9. doi: 10.1037/0735-7028.31.5.484
245. Schlosser B. Transmitter v. Hedonia. Ethics Behav (1996) 6(2):172–4. doi: 10.1207/s15327019eb0602_11
246. Smucker Barnwell S, Adams Larsen M. Disposal of data, information, and technologies. In: Campbell LF, Millán F, Martin JN, editors. A telepsychology casebook: Using technology ethically and effectively in your professional practice. Washington, DC, US: American Psychological Association (2018). p. 99–119.
247. Campbell LF, Norcross JC. Do you see what we see? Psychology’s response to technology in mental health. Clin Psychol Sci Pract (2018) 25(2):e12237. doi: 10.1111/cpsp.12237
248. Langarizadeh M, Moghbeli F, Aliabadi A. Application of ethics for providing telemedicine services and information technology. Med Arch (2017) 71(5):351–5. doi: 10.5455/medarh.2017.71.351-355
Keywords: online psychotherapy, telepsychology, telepsychiatry, ethics, technology
Citation: Stoll J, Müller JA and Trachsel M (2020) Ethical Issues in Online Psychotherapy: A Narrative Review. Front. Psychiatry 10:993. doi: 10.3389/fpsyt.2019.00993
Received: 16 September 2019; Accepted: 13 December 2019;
Published: 11 February 2020.
Edited by:
Cynthia H. Y. Fu, University of East London, United KingdomReviewed by:
Warren Mansell, University of Manchester, United KingdomJanardhan Y. C. Reddy, National Institute of Mental Health and Neurosciences, India
Copyright © 2020 Stoll, Müller and Trachsel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Manuel Trachsel, bWFudWVsLnRyYWNoc2VsQHV6aC5jaA==
 Julia Stoll
Julia Stoll Jonas Adrian Müller
Jonas Adrian Müller Manuel Trachsel
Manuel Trachsel