- 1Peking University Sixth Hospital, Peking University Institute of Mental Health, NHC Key Laboratory of Mental Health (Peking University), National Clinical Research Center for Mental Disorders (Peking University Sixth Hospital), Beijing, China
- 2Department of Psychiatry, Affiliated Psychological Hospital of Anhui Medical University, Anhui Mental Health Center, Hefei Fourth People’s Hospital, Hefei, China
- 3Peking-Tsinghua Center for Life Sciences and PKU-IDG/McGovern Institute for Brain Research, Peking University, Beijing, China
- 4Key Laboratory of High Confidence Software Technologies (MOE), Department of Computer Science and Technology, Peking University, Beijing, China
- 5National Institute on Drug Dependence and Beijing Key Laboratory of Drug Dependence, Peking University, Beijing, China
- 6Department of Pharmacology, School of Basic Medical Sciences, Peking University Health Science Center, Beijing, China
- 7Department of Psychiatry, The Fourth People’s Hospital of Dalian Jinzhou District, Dalian, China
- 8Department of Psychiatry, The Sixth People’s Hospital of Hebei Province, Baoding, China
- 9Department of Psychiatry, Rongjun Hospital of Hebei Province, Baoding, China
- 10Department of Psychiatry, Beijing HuiLongGuan Hospital, Beijing, China
- 11Department of Psychiatry, Guangzhou Psychiatric Hospital, Guangzhou, China
- 12Department of Psychiatry, Jinzhou Kangning Hospital, Jinzhou, China
- 13Department of Psychiatry, Shanghai Mental Health Center, Shanghai, China
- 14Department of Psychiatry, The People’s Hospital of Hubei Province, Wuhan, China
- 15Department of Psychiatry, The Mental Health Center of Xi’an, Xi’an, China
Background: Preventing relapse of schizophrenic patients is really a challenge. The present study sought to provide more explicit evidence and factors of different grades and weights by a series of step-by-step analysis through χ2 test, logistic regression analysis and decision-tree model. The results of this study may contribute to controlling relapse of schizophrenic patients.
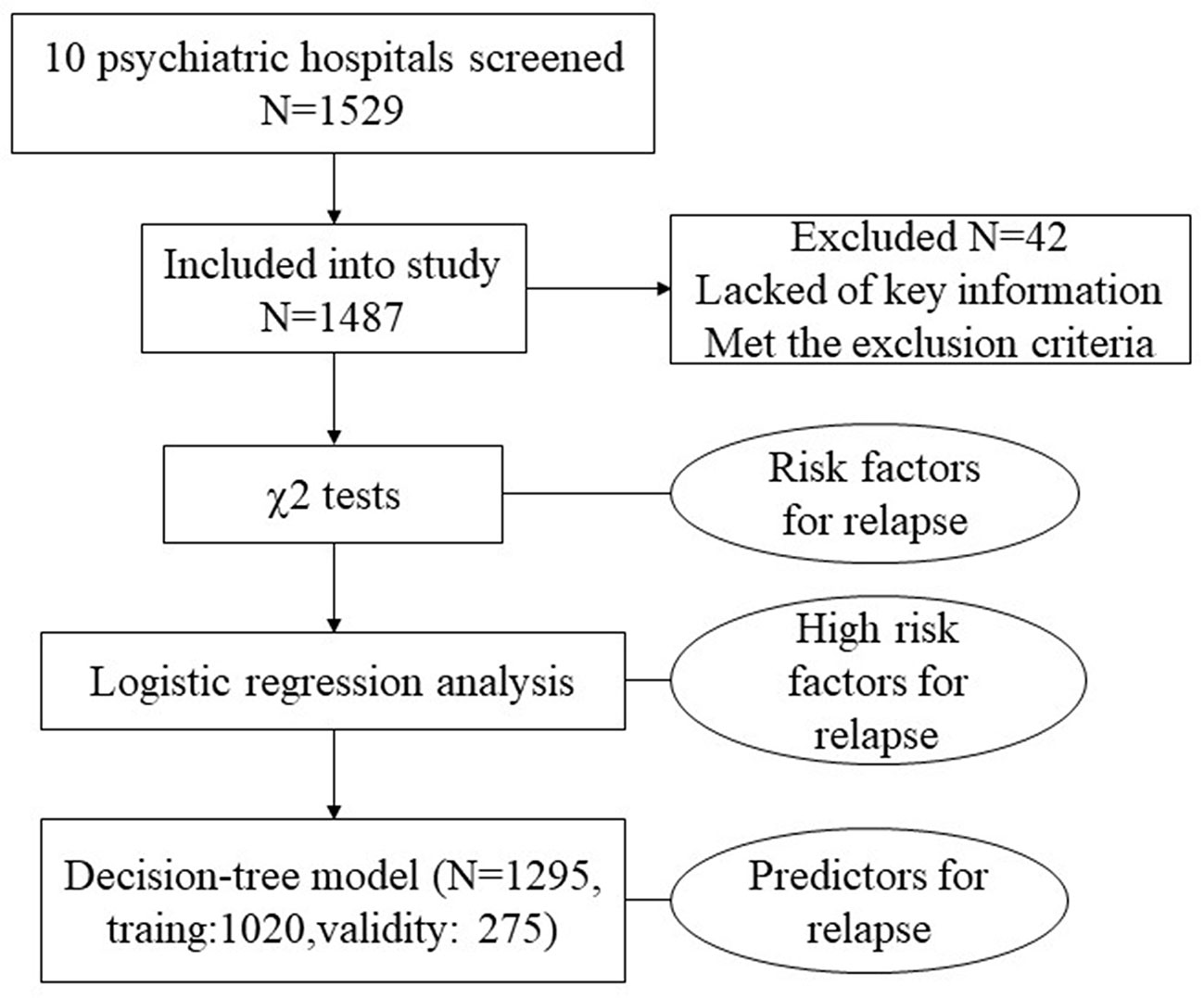
Methods: A total of 1,487 schizophrenia patients were included who were 18–65 years of age and discharged from 10 hospitals in China from January 2009 to August 2009 and from September 2011 to February 2012 with improvements or recovery of treatment effect. We used a questionnaire to collect information about relapse and correlative factors during one year after discharge by medical record collection and telephone interview. The χ2 test and logistic regression analysis were used to identify risk factors and high-risk factors firstly, and then a decision-tree model was used to find predictive factors.
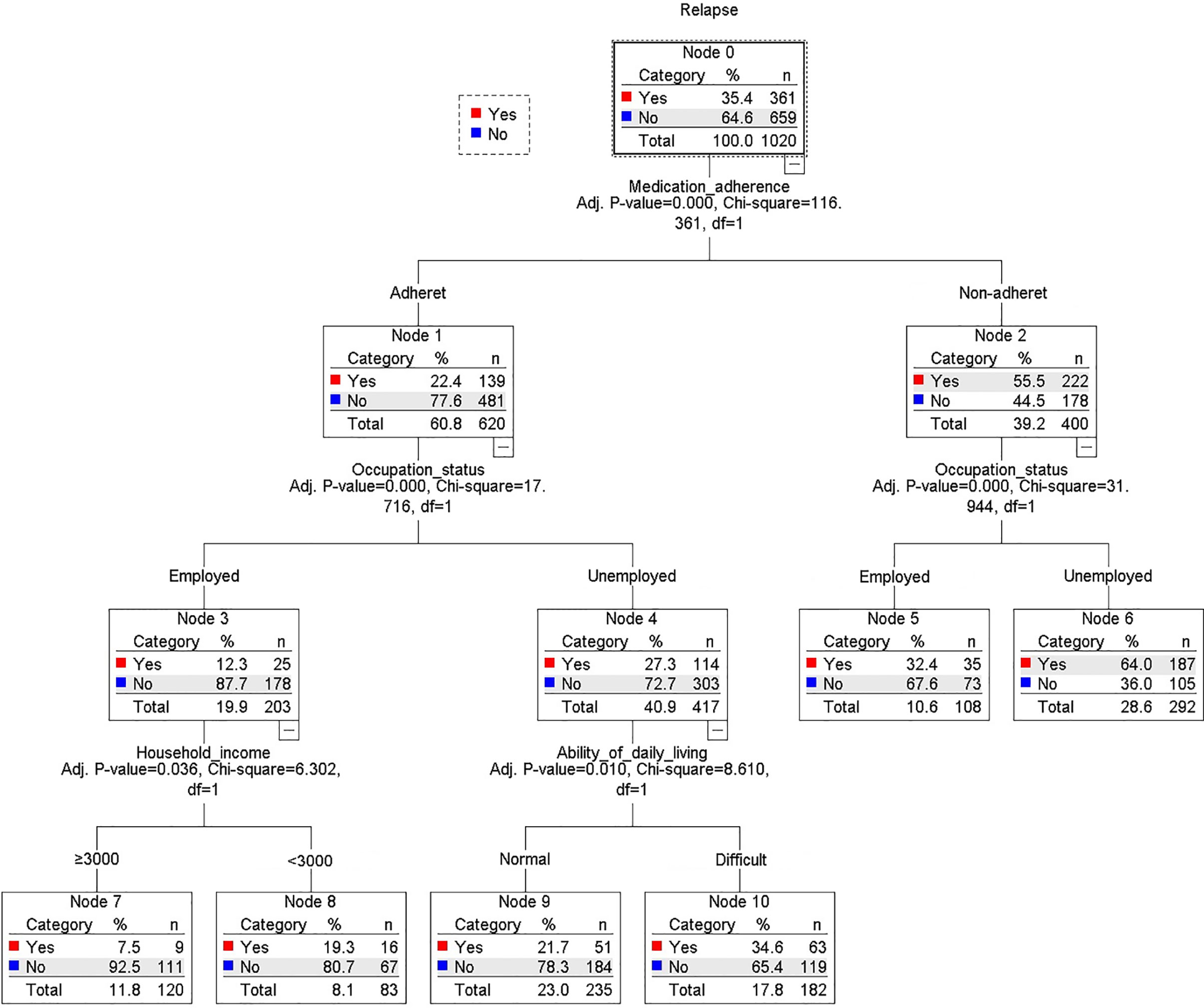
Results: The χ2 test found nine risk factors which were associated with relapse. Logistic regression analysis also showed four high-risk factors further (medication adherence, occupational status, ability of daily living, payment method of medical costs). At last, a decision-tree model revealed four predictors of relapse; it showed that medication adherence was the first grade and the most powerful predictor of relapse (relapse rate for adherence vs. nonadherence: 22.9 vs. 55.7%, χ2 = 116.36, p < 0.001). The second grade factor was occupational status (employment vs. unemployment: 19.7 vs. 42.7%, χ2 = 17.72, p < 0.001); the third grade factors were ability of daily living (normal vs. difficult: 28.4 vs. 54.3%, χ2 = 8.61, p = 0.010) and household income (household income ≥ 3000 RMB vs. <3000 RMB: 28.6 vs. 42.4%, χ2 = 6.30, p = 0.036). The overall positive predictive value (PPV) of the logistic regression was 0.740, and the decision-tree model was 0.726. Both models were reliable.
Conclusions: For schizophrenic patients discharged from hospital, who had good medication adherence, more higher household income, be employed and normal ability of daily living, would be less likely to relapse. Decision tree provides a new path for doctors to find the schizophrenic inpatient’s relapse risk and give them reasonable treatment suggestions after discharge.
Introduction
Schizophrenia is a severe psychiatric disorder that has profound effects on both individuals and society. Medical costs and productivity losses that are associated with relapse in schizophrenia are enormous (1, 2). The costs for patients who relapse are approximately three-times higher than patients who do not relapse. According to the American Psychiatric Association (3), the main goal of treatment strategies for the stabilization phase of schizophrenia is to minimize the likelihood of relapse. This emphasizes the importance of identifying and modifying the factors that determine clinical relapse in schizophrenia. Thus, developing effective prevention strategies that may contribute to lowering relapse rates and associated costs is important.
Relapse is a multidimensional event, and prognostic risk factors for relapse in schizophrenia are a longstanding, complex topic. Despite a large body of research that evaluated the factors associated with the relapse of psychosis in schizophrenia, these studies mainly focused on only a few factors, including maintenance medication, substance abuse, family support, and social adjustment (4–11). Additionally, the models that have been used to predict relapse, such as multiple regression or Cox proportional hazard regression, are relatively simplistic. Various factors that are associated with the relapse of different aspects of schizophrenia, such as in first-episode schizophrenia patients, have been investigated, including the number of relapses, reductions of medication, medical costs, and cognitive factors (9, 12–19). However, there is still lack of consensus regarding the predictors of relapse in schizophrenia, which is likely attributable to different periods of observation, statistical methods, and healthcare systems.
In the present study, we conducted a large, multicenter, retrospective, observational investigation of schizophrenia patients in 10 psychiatric hospitals in China. We collected the following information: (1) general demographic information, (2) clinical characteristics, and (3) the living environment and information on social life. We sought to test the consistency of risk factors for relapse in patients with schizophrenia 1 year after hospital discharge and evaluate the interactions between these factors. Our goal was to provide more explicit evidence and factors of different grades and weights that may contribute to controlling relapse of the patients and improving the clinical prognosis.
Materials and Methods
Participants
The patients included in the present study were outpatients with schizophrenia screened in 10 psychiatric hospitals in seven provinces in China. Patients were screened by reviewing their medical records. All of the patients were of Han Chinese origin and received treatment with antipsychotic agents after discharge from the hospital. The inclusion criteria were the following: (1) 18–65 years of age, (2) the diagnosis of schizophrenia by eligible hospitals according to the international statistical classification of diseases and related health problems, 10th revision (ICD-10), and (3) discharged from the hospital with recovery or improvement from two parts of time periods: from January 2009 to August 2009 and from September 2011 to February 2012. Patients were excluded if therapeutic effect information were unclear and had residual core symptoms at hospital discharge. The study received approval from the central ethics community of the Ethics Committee of Peking University Sixth Hospital, and it was recognized by all the other participating hospitals. Verbal informed consent was given to all patients or their caregivers in this survey.
Materials
This study had a retrospective observational design and was supported by “Survey on antipsychotics compliance and relapse of schizophrenia in China (SACRSC)” project. Our previous study reported high rates of relapse and found that poor medication adherence was the main risk factor for relapse, based on χ2 analyses of data from schizophrenia patients who were discharged from hospital between September 2011 and February 2012, and the sample size was 992 (20). And before that our work group had already collected a small sample data which contained about 537 schizophrenic patients who were discharged from the hospital with recovery or improvement from January 2009 to August 2009. And in this study, we combine the data of those two parts to enlarge the sample and try to find some more convincing evidence and predictors to support schizophrenia clinical treatment and prevent relapse. So, the study was actually conducted in two time stages: from January 2010 to August 2010 and from September 2012 to February 2013, which were one year after patients’ discharged.
We used cluster random sampling method to collect patients in both two parts of this study (January 2009 to August 2009, September 2011 to February 2012); research hospitals would randomly select one month during that two time period, and all the patients of that randomly selected month who met the inclusion criteria and did not meet the exclusion criteria were included in the study. And the final sample size was 1,487; 42 patients were not included in this study for lack of key information and meeting the exclusion criteria.
We used a questionnaire that was specifically designed for the present survey. The questionnaire included two parts. Part 1 evaluates general demographic information and disease information based on the patients’ medical records of hospital. Disease information included the duration of schizophrenia, age of onset, lifetime number of hospitalizations, duration of last hospitalization, family history of physical and psychiatric illness, and history of smoking/alcohol abuse. Part 2 was designed as a 17-item semi-structured questionnaire to investigate the rate of relapse and rehospitalization and the potential risk factors that might affect relapse. Information on this part was obtained by telephone interview 1 year after hospital discharge. Except for prescribed medications following their doctors’ recommendations, no interventions were performed after hospital discharge during the 1 year prior to the telephone interview. Given the unreliability of self-assessment, patient’s caregivers (e.g., parents, spouses, or siblings) were preferred in the telephone interview. The patients themselves were interviewed only in the case that patients lived alone or patient’s caregivers could not be reached for telephone interview. All patients or their caregivers gave verbal informed consent prior to the telephone interview. If the respondent completed the questionnaire, it represents he/she agreed to participate the survey. And this survey did not include private information. The surveyors of this study were all psychiatrists from the 10 hospitals, and all of them got the same training for the standard operating procedures of each item in the questionnaire to make sure the consistency of the survey. For the study design see Figure 1.
Definition of Relapse
Currently, no consistent criteria were established in the world to define relapse in schizophrenia. In our study, we defined relapse based on previous study that clinically significant exacerbation of psychotic symptoms during telephone interviews according to self-report or the caregiver’s report. Four operational evaluation criteria were proposed to assess exacerbation of symptoms: a change in antipsychotic treatment, more frequent hospital visits, rehospitalization, and closer supervision because of self-harm, aggressive behavior, and/or suicidal or homicidal ideation (21). Patients who met at least one of the above four criteria were considered to have relapsed (20).
Definition of Medication Adherence
In this study, adherence was assessed based on the medication-taking behavior reported by respondents. Discontinuation of drugs was regarded as extreme nonadherence behavior. According to the timing of nonadherence with regard to the prescription or duration of discontinued medication after discharge, adherence was graded as one of three levels: (1) adherent (adherence to medication most of the time, total time of nonadherence less than 2 months, or medication discontinued for less than 2 weeks), (2) moderately nonadherent (adherence to medication half of the time, total time of nonadherence more than 2 months but less than 6 months, or medication discontinued for more than 2 weeks but less than 2 months), and (3) severely nonadherent (almost no adherence to medication, total time of nonadherence more than 6 months, or medication discontinued for more than 2 months) (22, 23).
Statistical Analysis
After completing the surveys of schizophrenia patients, each hospital sent the questionnaires to the study initiator (Peking University Sixth Hospital) for data analysis. All statistical analysis was performed using Statistiscal Package for the Social Sciences 16.0 software (SPSS, Chicago, IL, USA). We used a series of step-by-step analysis through Chi Square (χ2) test, logistic regression analysis, and decision-tree model. The χ2 test was performed to identify risk factors associated with relapse. Logistic regression analysis was conducted to model the potentially risk factors of relapse. In logistic regression model, we use medication adherence, occupational status, interpersonal relationships, household income, therapeutic effects, payment of medical costs, family communication, hospital rank as independent variables and relapse as dependent variable (Controlled with gender and medication pattern at time of survey as covariates). Results of the logistic regression models were reported as odds ratios (ORs) with 95% confidence intervals (CIs). No adjustments were made for multiple outcome measures. Collinear analysis between potentially risk factors is reported in Table S1 in the supplementary material.
A decision tree classification model for relapse was reconstructed using the Chi Square interaction automatic detection analysis (CHIAD) by identifying cutoffs of probabilities for each risk group (24). It gives graded and weighted predictive factors and is helpful for assessing the prognosis of schizophrenia. Specifically, by using the CHIAD method, the most significant risk factor split the sample into two or more subgroups, which are subsequently divided by the next most significant risk factor, and so on until there are no significant risk factors. P-values less than 0.05 were considered to be statistically significant.
Decision-Tree Model and Validity
We defined validity as that in a new group of data, those independent variables related to high risk of relapse predicted relapse in schizophrenia by the given model. We take 1,020 of the total samples as training samples to obtain risk factors, and then the remaining 275 of our overall sample are used as verification or validity samples to test the risk factors.
All of the items were analyzed as categorical variables [e.g., medication adherence (nonadherent, adherent)]. More details of the classifications of each factor are provided in Table 1. Values of p < 0.05 were considered statistically significant. A 95% confidence interval (CI) of the odds ratio (OR) that overlaps 1 (include OR = 1) indicates no statistical significance. A lower-limit value of the 95% CI that is greater than 1 indicates a greater risk factor or predictor of relapse. An upper-limit value of the 95% CI that is less than 1 indicates a higher likelihood of nonrelapse.
Results
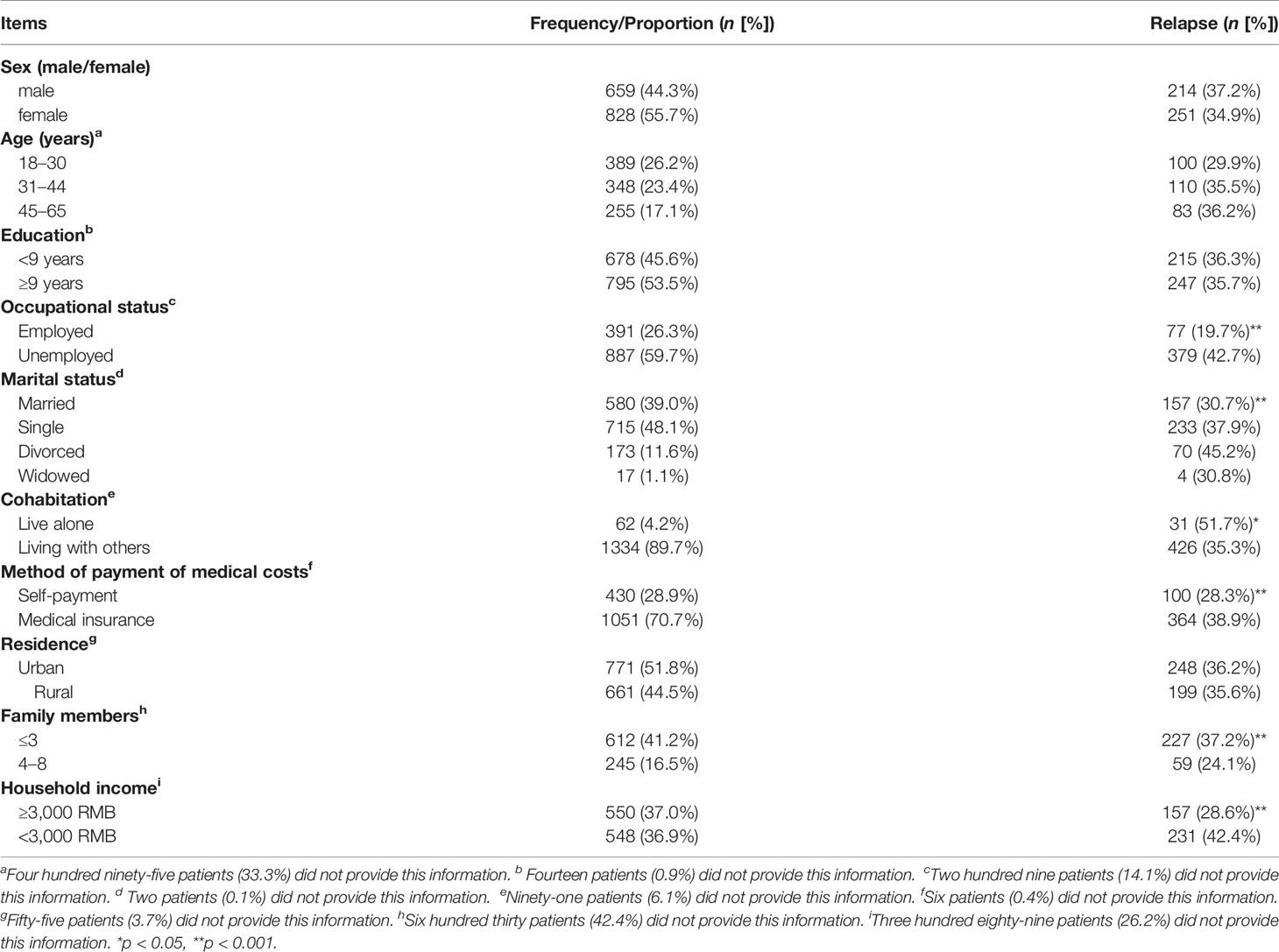
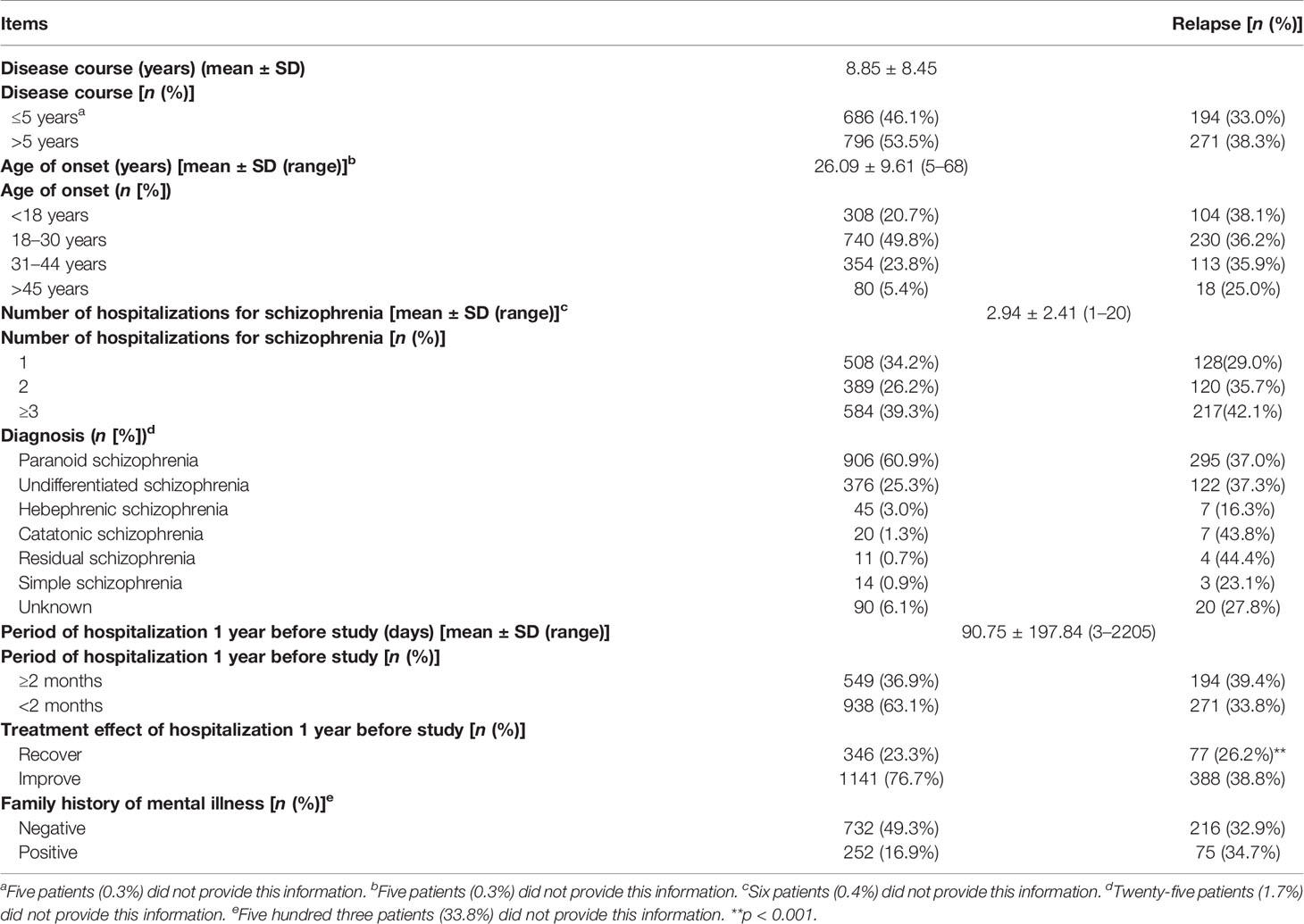
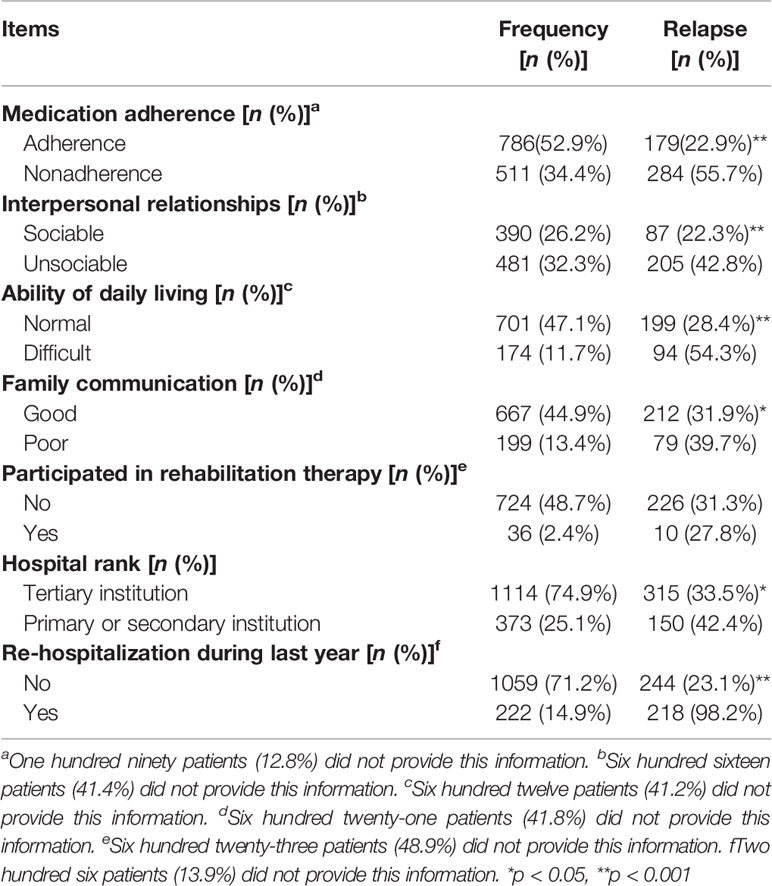
We received a total of 1,529 completed questionnaires, of which 1,487 were eligible for inclusion criteria in the statistical analysis (97.3%). For these patients, the main age was (35.45 ± 11.48) years; of them, 828 were female (55.7%), and 659 were male (44.3%). Information on relapse was obtained from 1,295 of the patients, of which 465 (35.9%) relapsed. We defined “moderately nonadherent” and “severely nonadherent” cases together as nonadherent, and the proportion of “adherent” participants was 52.9% (786/1,487). The general demographic information and general disease information of the participants are presented in Table 1, and we found the patients’ social and family support factors may greatly influence their relapse.
Risk Factors for Relapse
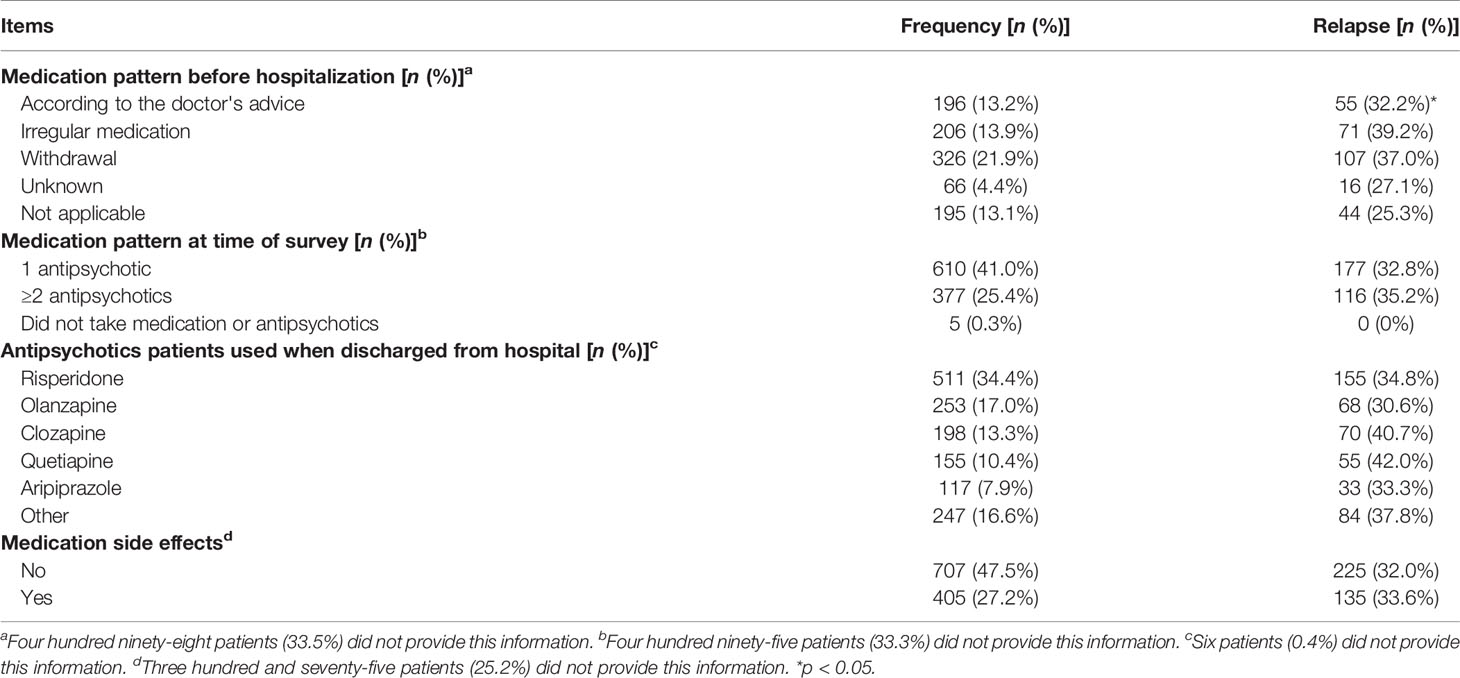
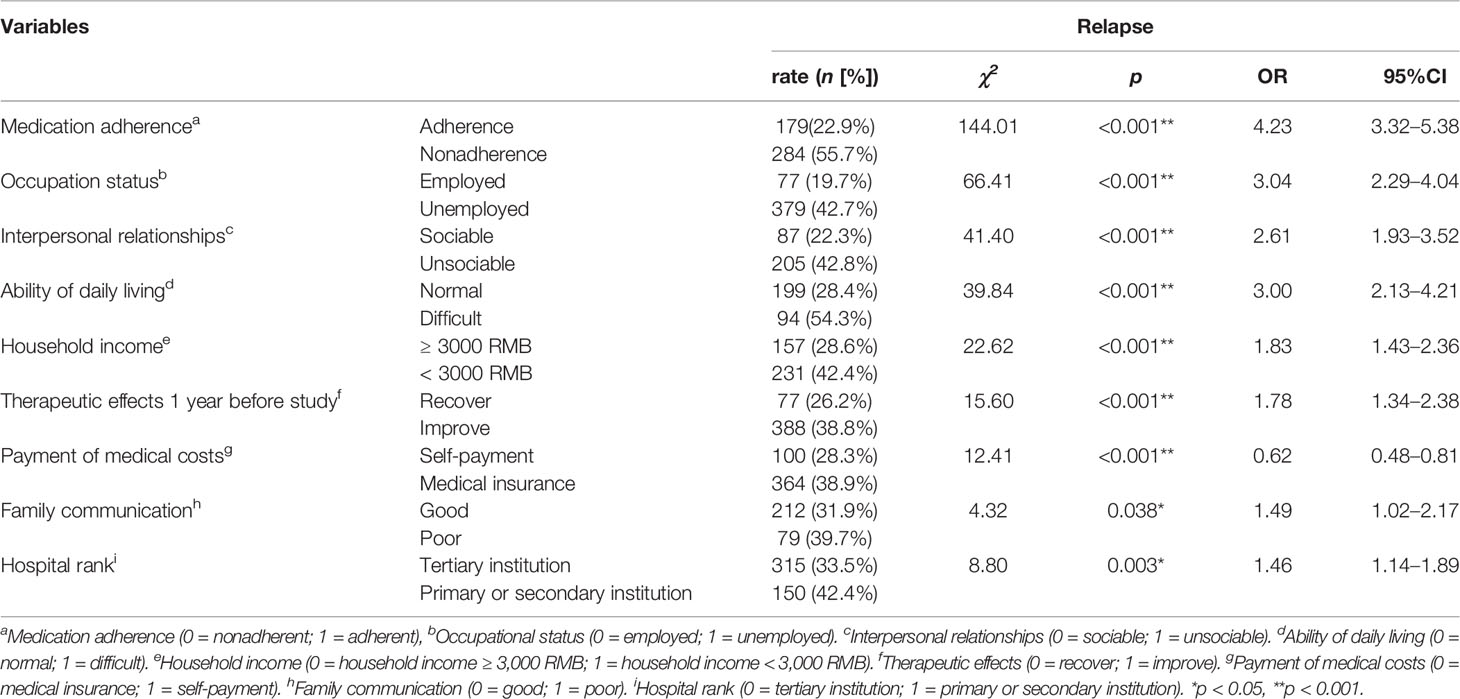
χ2 tests were conducted to determine the risk factors for relapse. Highly related risk factors are presented in Table 2, and unrelated factors are presented in Supplemental Table S1. Multivariable analyses showed that these factors were independent of each other, and no correlation existed between them. Nine risk factors for relapse were identified: (1) In terms of medication adherence, patient who has medication adherence had a lower risk of relapse than those with nonadherence (relapse rate for adherence vs. nonadherence: 22.9 vs. 55.7%, OR = 4.23, 95% CI = 3.32–5.38). (2) In terms of occupational status, those who were employed had a lower risk of relapse than those unemployed (relapse rate for employment vs. unemployment: 19.7 vs. 42.7%, OR = 3.04, 95% CI = 2.29–4.04). (3) In terms of interpersonal relationships, patient who has sociable relationships had a lower risk of relapse than that with unsociable relationships (relapse rate for sociability vs. unsociability: 22.3 vs. 42.8%, OR = 2.61, 95% CI = 1.93–3.52). (4) In terms of ability of daily living, patients with difficult daily living was prone to relapse than those with normal daily living (relapse rate for normal daily living vs. difficult daily living: 28.4 vs. 54.3%, OR = 3.00, 95% CI = 2.13–4.21). (5) In terms of household income, patients with house income over 3,000 RMB every month has a lower risk of relapse than patients whose house income were lower than 3,000 RMB (relapse rate for household income over 3,000 RMB vs. less than 3,000 RMB: 28.6 vs. 42.4%, OR = 1.83, 95% CI = 1.43–2.36). (6) In terms of therapeutic effects on discharge, patients who were improved has a higher risk of relapse than those recovered (relapse rate for recovery vs. improvement: 26.2 vs. 38.8%, OR = 1.78, 95% CI = 1.34–2.38). (7) In terms of method of payment of medical costs, people who self-paid has a lower risk of relapse than those paid via medical insurance (relapse rate for self-payment vs. medical insurance: 28.3 vs. 38.9%, OR = 0.62, 95% CI = 0.48–0.81). (8) In terms of family communication, patients with good communication between family members has a lower risk of relapse than those with poor communication (relapse rate for good communication vs. poor communication: 31.9 vs. 39.7%, OR = 1.49, 95% CI = 1.02–2.17), and (9) in terms of hospital rank, people who went to tertiary institution verse primary or secondary institution for treatment had a lower risk of relapse (relapse rate for tertiary institution vs. primary or secondary institution: 33.5 vs. 42.4%, OR = 1.46, 95% CI = 1.14–1.89; Table 2).
In χ2 tests, we also found statistical significance in different groups’ relapse rate of marital status, cohabitation, family members, and medication pattern before hospitalization, re-hospitalization during the last year (Table 1). But after correction, all the above five variables had too large difference in group sample number (for example: in a variable, one group number was more than 1,300 and the other was less than 100), and the groups in the same variable cannot combine at all, and some variables had significant correlation (cohabitation and family members). Thus, the statistical tests were not convincing and stable enough for those five variables, and we did not include them in our results and next step analysis. We also showed nonsignificant variables for relapse of χ2 tests in Supplemental Table S2.
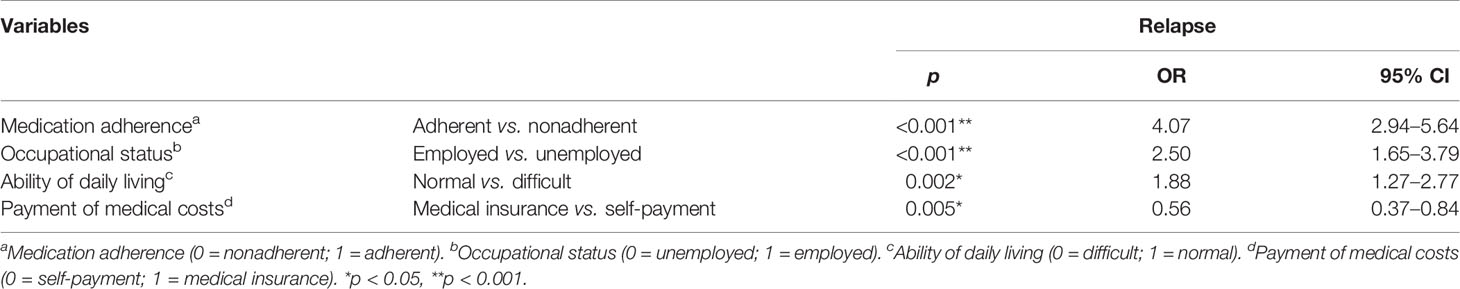
High-Risk Factors for Relapse
Logistic regression analysis was conducted to identify the stronger risk factors of relapse. We found that medication adherence (OR = 4.07, 95% CI = 2.94–5.64, p < 0.001), occupational status (OR = 2.50, 95% CI = 1.65–3.79, p < 0.001), ability of daily living (OR = 1.88, 95% CI = 1.27–2.77, p = 0.002), and method of payment of medical costs (OR = 0.56, CI = 0.37–0.84, p = 0.005) highly predicted relapse (Table 3). For schizophrenic patient discharged from the hospital, those who had good medication adherence, employed, normal ability of daily living and self-payment, would less likely to relapse.
Predictors for Relapse
As expected, poor medication adherence, unemployment, poor ability of daily living, and low household income highly predicted relapse (training samples see Figure 2, validity samples see Supplementary Materials, Figure S1). Medication adherence was the first differentiator (or grade, node) of cases (Figure 2). Occupational status produced the second split (it was significant in both medication adherent and nonadherent group; adherent: p < 0.001, nonadherent: p < 0.001). Among the patients who were adherent and employed, the third predictor of relapse was lower household income (<3,000 RMB). Among the patients who were adherent and unemployed, the third-grade predictor of relapse was difficult ability of daily living.
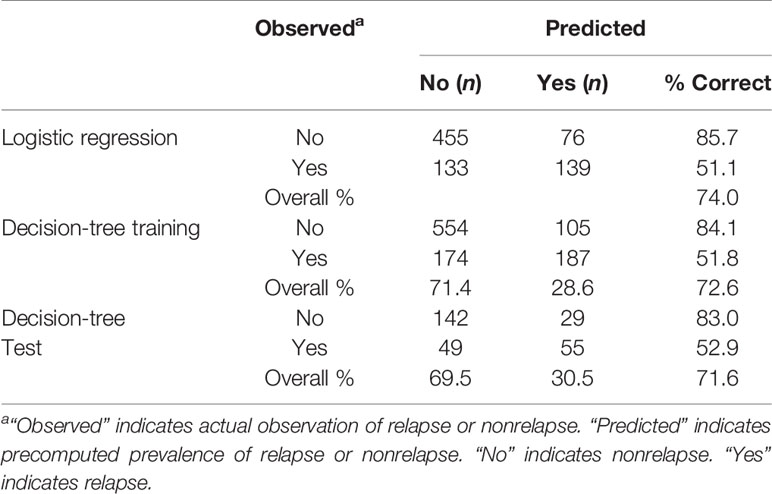
The predicted performance of the logistic regression analysis and decision tree model is presented in Table 4. The decision-tree model had a positive predictive value (PPV) of 0.726, meaning that it correctly predicted 72.6% of relapse cases. The overall PPV of the logistic regression was 0.740. Both models reliably predicted relapse.
Discussion
In the present study, we found that poor medication adherence, unemployment, difficult ability of daily living, medical insurance of medical costs, and low household income were highly related to relapse by using χ2 tests, logistic regression analysis, and decision-tree models. As expected, poor medication adherence was the most significant predictor of relapse, and 55.8% of the nonadherent patients relapsed compared with only 23% of the adherent patients (Figure 2).
Medication nonadherence is a critical factor of relapse in schizophrenia patients. Poor adherence increases the risk of relapse and hospital readmission (17, 19, 25–27). The consequences of inadequate medication adherence include poor clinical outcomes, increases in morbidity and disability, a lower quality of life, decreases in work and personal productivity, and an increase in healthcare costs (14, 28). The causes of nonadherence are multifactorial. Negative attitudes about medications play an important role in nonadherence (29, 30). Medication adherence is one of the most effective means of preventing relapse in schizophrenia (31, 32).
Unemployment is a high-risk factor for relapse in schizophrenia patients. Reports of the prevalence of unemployment showed that 75–90% of adults with schizophrenia are unemployed, and unemployment contributes to disease recurrence (33). Theoretically, unemployment may associate with another high-risk factor, for example, household income. However, according to colinear analysis, there was no collinearity between these two factors. One possible explanation for this is that the household income did not correctly reflect patients own income, and only small part (4.2%) of the patients were living alone. We also found that difficult ability of daily living predicted relapse in schizophrenia patients 1 year after hospital discharge. Social skills’ training is highly recommended to improve schizophrenia patients’ deficits in the ability of daily life (34). In addition to many well-documented factors that are associated with psychotic relapse, our work also emphasizes the important role of self-payment of medical costs and household income in relapse. An explanation offered by the decision tree model was that patients with lower income or unemployed appeared as predictors of medical costs and household income. These two risk factors were not regarded as predictors of relapse in previous studies that were conducted in developed countries (23, 25, 35, 36), which may be attributable to these countries’ comparatively advanced healthcare systems and public services. Hospitals in China are organized according to a three-tier system (i.e., primary, secondary, and tertiary institutions) that recognizes a hospital’s ability to provide medical care (29). Patients who receive treatment in nontertiary institutions (primary and secondary institutions) are more likely to relapse; that was also an important result of this study, and in the future, we may do more work to improve primary and secondary institutions’ mental disease treatment.
In the present study both logistic regression and decision-tree models were used to identify high-risk factors and predictors for relapse. Since we use categorical variables and some variables may have interacted with each other, while, logistic regression cannot properly deal with problems of nonlinear and interactive effects of explanatory variables (37). Therefore, it is necessary to verify the findings of logistic regression by decision trees. In addition, the decision tree model has some advantages over generalized linear models (logistic regression). First, compared with generalized linear models, decision tree model is easier to understand because the results exported in the decision tree model were resembling clinical decision-making processes. Second, tree-structures are more flexible to distribute the response variable without pre-assumption. And we found an article that used the same strategy with our study in which they used χ2 followed by logistic regression and decision tree consecutively (38). Our results from the decision-tree analysis were corroborated by both the logistic regression and χ2 analyses. Moreover, we verified the results using data from 275 separate patients (approximately 20% of the total number of patients who were included in the study). Therefore, the results of these models were robust, and our findings may provide further evidence for preventing relapse of schizophrenia patients.
It is also important to mention the factors that did not significantly predict first year relapse in patients with schizophrenia. In the present study, the initial χ2 tests indicated that smoking, alcohol dependence, rural residence, side effects of medication, a low level of education (<9 years), period of hospitalization (≤2 months), disease course (>5 years), and a family history of schizophrenia were not significantly related to relapse at the end of the first year. These findings contrast with previous studies (9, 39, 40). This discrepancy might be attributable to differences in the definition of relapse or periods of observation. Further examinations of these factors in different situations are needed to provide more precise recommendations for the clinical prognosis of relapse.
The present study has some limitations. First, the study was not designed to assess adherence to specific antipsychotic medications; we only controlled medication pattern as covariate in both regression and decision tree models. We focused on external risk factors beyond pharmacological effects that may indirectly affect medication adherence and relapse. Second, the data may have been influenced by a “social desirability response” during the telephone interview, which refers to the tendency of survey respondents to answer questions in a manner that will be viewed favorably by others (41). Cultural idioms provide some protection against stigma among respondents in China (42, 43). Third, although all of the investigators were trained and licensed psychiatrists and information on general demographic information and disease information was obtained from the patients’ medical records of hospital, data about relapse were provided by the respondents which may give false information, and it was easily prone to recall bias. It is an inevitable limitation for retrospective study. Fourth, risk factors associated with relapse in schizophrenia did not imply casual relationships. Further study was needed to explore the predictor of relapse in patients. However, it may not often feasible to study the relationships because of various confounding variables in the real world.
Conclusions
In summary, this study considered several important variables and used three statistical models to evaluate the risk factors, high-risk factors or predictors associated with relapse in schizophrenia. Our work provides strong evidence that poor medication adherence, unemployment, difficult ability of daily living, medical insurance of medical costs, and low household income were main predictors of relapse in schizophrenia patients 1 year after hospital discharge. Medication adherence was the first-grade predictors of relapse. Clinicians should be fully aware of this risk and provide accurate information to patients about the risk of relapse. Further studies evaluating intervention strategies focused on reducing relapse and improving insight into schizophrenia should be encouraged.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Peking University Sixth Hospital and recognized by all the other participating hospitals. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
W-FM conceived of the study. W-FM, and T-TF participated in its design and coordination and drafted the manuscript. X-MC and J-BX performed the statistical analysis and interpretation of the data. W-FM, ST, T-TF, X-MC, Y-PB, YH, L-ZL, YS, L-HG, X-ZW, Y-QL, Z-MW, J-XC, F-CW, W-BM, H-FL, W-DX, and F-HL participated in the coordination of the study and performed the measurements. WX, H-YZ, and LL contributed to the critical revision of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Beijing Municipal Science and Technology Commission (project number: Z151100003915121, Z181100001718157), National Key Research and Development Program of China (project number: 2016YFC1304400), National Science and Technology Major Project for IND (project number: 2018ZX09734-005). The funding organization had no influence on the design and conduct of the study, collection, management, analysis, and interpretation of the data, preparation, review, or approval of the manuscript, or the decision to submit the manuscript for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor declared a shared affiliation with one of the authors [H-FL] at time of review.
Acknowledgments
The authors would like to thank all doctors in study centers for their assistance in the conduct of this research and the respondents for participating in this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.574763/full#supplementary-material
Abbreviations
CHIAD, Chi Square interaction automatic detection analysis; CI, confidence interval; OR, odds ratio; PPV, positive predictive value.
References
1. Weiden PJ, Olfson M. Cost of relapse in schizophrenia. Schizophr Bull (1995) 21(3):419–29. doi: 10.1093/schbul/21.3.419
2. Laidi C, Prigent A, Plas A, Leboyer M, Fond G, Chevreul K. Factors associated with direct health care costs in schizophrenia: Results from the FACE-SZ French dataset. Eur Neuropsychopharmacol J Eur Coll Neuropsychopharmacol (2018) 28(1):24–36. doi: 10.1016/j.euroneuro.2017.11.020
3. Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, et al. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry (2004) 161(2 Suppl):1–56.
4. Linszen DH, Dingemans P, Scholte WF, Lenior ME, Goldstein MJ. Early recognition, internsive intervention and other protective and risk factors for psychotic relapse in patients with first psychotic episodes in schizophrenia. Int Clin Psychopharmacol (1998) 13(1):S7–S12. doi: 10.1097/00004850-199801001-00003
5. Ayuso-Gutiérrez JL, del Río Vega JM. Factors influencing relapse in the long-term course of schizophrenia. Schizophr Res (1997) 28(2-3):199–206. doi: 10.1016/s0920-9964(97)00131-x
6. Curson DA, Barnes TR, Bamber RW, Platt SD, Hirsch SR, Duffy JC. Long-term depot maintenance of chronic schizophrenic out-patients: the seven year follow-up of the Medical Research Council fluphenazine/placebo trial. III. Relapse postponement or relapse prevention? The implications for long-term outcome. Br J Psychiatry J Ment Sci (1985) 146:474–80. doi: 10.1192/bjp.146.5.474
7. Hui CL, Tang JY, Leung CM, Wong GH, Chang WC, Chan SK, et al. A 3-year retrospective cohort study of predictors of relapse in first-episode psychosis in Hong Kong. Aust New Z J Psychiatry (2013) 47(8):746–53. doi: 10.1177/0004867413487229
8. Eisner E, Drake R, Barrowclough C. Assessing early signs of relapse in psychosis: review and future directions. Clin Psychol Rev (2013) 33(5):637–53. doi: 10.1016/j.cpr.2013.04.001
9. Schennach R, Obermeier M, Meyer S, Jager M, Schmauss M, Laux G, et al. Predictors of relapse in the year after hospital discharge among patients with schizophrenia. Psychiatr Serv (Washington DC) (2012) 63(1):87–90. doi: 10.1176/appi.ps.201100084
10. Hrdlicka J, Klema J. Schizophrenia prediction with the adaboost algorithm. Stud Health Technol Inf (2011) 169:574–8. doi: 10.3233/978-1-60750-806-9-574
11. Kerz M, Folarin A, Meyer N, Begale M, MacCabe J, Dobson RJ. SleepSight: A wearables-based relapse prevention system for Schizophrenia. Acm International Joint Conference (2016) 113–6. doi: 10.1145/2968219.2971419
12. Ascher-Svanum H, Zhu B, Faries DE, Salkever D, Slade EP, Peng X, et al. The cost of relapse and the predictors of relapse in the treatment of schizophrenia. BMC Psychiatry (2010) 10:2. doi: 10.1186/1471-244x-10-2
13. Chen EY, Hui CL, Dunn EL, Miao MY, Yeung WS, Wong CK, et al. A prospective 3-year longitudinal study of cognitive predictors of relapse in first-episode schizophrenic patients. Schizophr Res (2005) 77(1):99–104. doi: 10.1016/j.schres.2005.02.020
14. Jeste SD, Patterson TL, Palmer BW, Dolder CR, Goldman S, Jeste DV. Cognitive predictors of medication adherence among middle-aged and older outpatients with schizophrenia. Schizophr Res (2003) 63(1-2):49–58. doi: 10.1016/s0920-9964(02)00314-6
15. Lipkovich I, Deberdt W, Csernansky JG, Buckley P, Peuskens J, Kollack-Walker S, et al. Predictors of risk for relapse in patients with schizophrenia or schizoaffective disorder during olanzapine drug therapy. J Psychiatr Res (2007) 41(3-4):305–10. doi: 10.1016/j.jpsychires.2006.07.016
16. Robinson D, Woerner MG, Alvir JM, Bilder R, Goldman R, Geisler S, et al. Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry (1999) 56(3):241–7. doi: 10.1001/archpsyc.56.3.241
17. Svarstad BL, Shireman TI, Sweeney JK. Using drug claims data to assess the relationship of medication adherence with hospitalization and costs. Psychiatr Serv (2001) 52(6):805–11. doi: 10.1176/appi.ps.52.6.805
18. Ucok A, Polat A, Cakir S, Genc A. One year outcome in first episode schizophrenia. Predictors of relapse. Eur Arch Psychiatry Clin Neurosci (2006) 256(1):37–43. doi: 10.1007/s00406-005-0598-2
19. Valenstein M, Copeland LA, Blow FC, McCarthy JF, Zeber JE, Gillon L, et al. Pharmacy data identify poorly adherent patients with schizophrenia at increased risk for admission. Med Care (2002) 40(8):630–9. doi: 10.1097/01.mlr.0000021003.43524.64
20. Xiao J, Mi W, Li L, Shi Y, Zhang H. High relapse rate and poor medication adherence in the Chinese population with schizophrenia: results from an observational survey in the People’s Republic of China. Neuropsychiatr Dis Treat (2015) 11:1161–7. doi: 10.2147/ndt.s72367
21. Gleeson JF, Alvarez-Jimenez M, Cotton SM, Parker AG, Hetrick S. A systematic review of relapse measurement in randomized controlled trials of relapse prevention in first-episode psychosis. Schizophr Res (2010) 119(1-3):79–88. doi: 10.1016/j.schres.2010.02.1073
22. Morken G, Widen JH, Grawe RW. Non-adherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry (2008) 8:32. doi: 10.1186/1471-244x-8-32
23. Novick D, Haro JM, Suarez D, Perez V, Dittmann RW, Haddad PM. Predictors and clinical consequences of non-adherence with antipsychotic medication in the outpatient treatment of schizophrenia. Psychiatry Res (2010) 176(2-3):109–13. doi: 10.1016/j.psychres.2009.05.004
24. Yokoyama JS, Bonham LW, Sears RL, Klein E, Karydas A, Kramer JH, et al. Decision tree analysis of genetic risk for clinically heterogeneous Alzheimer’s disease. BMC Neurol (2015) 15:47. doi: 10.1186/s12883-015-0304-6
25. Ascher-Svanum H, Faries DE, Zhu B, Ernst FR, Swartz MS, Swanson JW. Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. J Clin Psychiatry (2006) 67(3):453–60. doi: 10.4088/JCP.v67n0317
26. Sullivan G, Wells KB, Morgenstern H, Leake B. Identifying modifiable risk factors for rehospitalization: a case-control study of seriously mentally ill persons in Mississippi. Am J Psychiatry (1995) 152(12):1749–56. doi: 10.1176/ajp.152.12.1749
27. Weiden PJ, Kozma C, Grogg A, Locklear J. Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatr Serv (2004) 55(8):886–91. doi: 10.1176/appi.ps.55.8.886
28. Nosé M, Barbui C, Tansella M. How often do patients with psychosis fail to adhere to treatment programmes? A systematic review. psychol Med (2003) 33(7):1149–60. doi: 10.1017/s0033291703008328
29. Rüsch N, Todd AR, Bodenhausen GV, Weiden PJ, Corrigan PW. Implicit versus explicit attitudes toward psychiatric medication: Implications for insight and treatment adherence. Schizophr Res (2009) 112(1-3):119–22. doi: 10.1016/j.schres.2009.04.011
30. Yalcin-Siedentopf N, Wartelsteiner F, Kaufmann A, Biedermann F, Edlinger M, Kemmler G, et al. Measuring adherence to medication in schizophrenia: the relationship between attitudes toward drug therapy and plasma levels of new-generation antipsychotics. Int J Neuropsychopharmacol (2014) 18(5):pyu091. doi: 10.1093/ijnp/pyu091
31. Velligan DI, Weiden PJ, Sajatovic M, Scott J, Carpenter D, Ross R, et al. Strategies for addressing adherence problems in patients with serious and persistent mental illness: recommendations from the expert consensus guidelines. J Psychiatr Pract (2010) 16(5):306–24. doi: 10.1097/01.pra.0000388626.98662.a0
32. Gray R, White J, Schulz M, Abderhalden C. Enhancing medication adherence in people with schizophrenia: an international programme of research. Int J Ment Health Nurs (2010) 19(1):36–44. doi: 10.1111/j.1447-0349.2009.00649.x
33. Haslett WR, McHugo GJ, Bond GR, Drake RE. Use of Software for Tablet Computers to Promote Engagement With Supported Employment: Results From an RCT. Psychiatr Serv (Washington DC) (2014) 65(7):954–6. doi: 10.1176/appi.ps.201300275
34. Fervaha G, Foussias G, Agid O, Remington G. Amotivation and functional outcomes in early schizophrenia. Psychiatry Res (2013) 210(2):665–8. doi: 10.1016/j.psychres.2013.07.024
35. Allen CG, Sugarman MA, Wennerstrom A. Community Health Workers: a Resource to Support Antipsychotic Medication Adherence. J Behav Health Serv Res (2016) 44(2):341–6. doi: 10.1007/s11414-016-9515-x
36. Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry (2002) 63(10):892–909. doi: 10.4088/jcp.v63n1007
37. Khemphila A, Boonjing V eds. Comparing performances of logistic regression, decision trees, and neural networks for classifying heart disease patients. In: 2010 international conference on computer information systems and industrial management applications (CISIM). Krackow (2010). p. 193–8. doi: 10.1109/CISIM.2010.5643666
38. Vilaseca I, Nogués-Sabaté A, Avilés-Jurado FX, Berenguer J, Grau JJ, Verger E, et al. Factors of local recurrence and organ preservation with transoral laser microsurgery in laryngeal carcinomas; CHAID decision-tree analysis. Head Neck (2019) 41(3):756–64. doi: 10.1002/hed.25422
39. Doering S, Müller E, Köpcke W, Pietzcker A, Gaebel W, Linden M, et al. Predictors of relapse and rehospitalization in schizophrenia and schizoaffective disorder. Schizophr Bull (1998) 24(1):87–98. doi: 10.1093/oxfordjournals.schbul.a033316
40. Gilbert PL, Harris MJ, McAdams LA, Jeste DV. Neuroleptic withdrawal in schizophrenic patients. A review of the literature. Arch Gen Psychiatry (1995) 52(3):173–88. doi: 10.1001/archpsyc.1995.03950150005001
41. Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. J Consult Psychol (1960) 24:349–54. doi: 10.1037/h0047358
42. WonPat-Borja AJ, Yang LH, Link BG, Phelan JC. Eugenics, genetics, and mental illness stigma in Chinese Americans. Soc Psychiatry Psychiatr Epidemiol (2012) 47(1):145–56. doi: 10.1007/s00127-010-0319-7
43. Yang LH, Lo G, WonPat-Borja AJ, Singla DR, Link BG, Phillips MR. Effects of labeling and interpersonal contact upon attitudes towards schizophrenia: implications for reducing mental illness stigma in urban China. Soc Psychiatry Psychiatr Epidemiol (2012) 47(9):1459–73. doi: 10.1007/s00127-011-0452-y
Keywords: schizophrenia, relapse, risk factors, predictors, decision-tree model
Citation: Mi W-F, Chen X-M, Fan T-T, Tabarak S, Xiao J-B, Cao Y-Z, Li X-Y, Bao Y-P, Han Y, Li L-Z, Shi Y, Guo L-H, Wang X-Z, Liu Y-Q, Wang Z-M, Chen J-X, Wu F-C, Ma W-B, Li H-F, Xiao W-D, Liu F-H, Xie W, Zhang H-Y and Lu L (2020) Identifying Modifiable Risk Factors for Relapse in Patients With Schizophrenia in China. Front. Psychiatry 11:574763. doi: 10.3389/fpsyt.2020.574763
Received: 21 June 2020; Accepted: 24 August 2020;
Published: 11 September 2020.
Edited by:
Tianhong Zhang, Shanghai Jiao Tong University, ChinaReviewed by:
Qiang Wang, West China Hospital, Sichuan University, ChinaLi Hui, Suzhou Guangji Hospital, China
Copyright © 2020 Mi, Chen, Fan, Tabarak, Xiao, Cao, Li, Bao, Han, Li, Shi, Guo, Wang, Liu, Wang, Chen, Wu, Ma, Li, Xiao, Liu, Xie, Zhang and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hong-Yan Zhang, aG9uZ3lhbnpoYW5nQGJqbXUuZWR1LmNu; Lin Lu, bGlubHVAYmptdS5lZHUuY24=; Wen Xie, eGlld2VuMDgwOEBzaW5hLmNvbQ==
†These authors have contributed equally to this work
 Wei-Feng Mi
Wei-Feng Mi Xiao-Min Chen2†
Xiao-Min Chen2† Teng-Teng Fan
Teng-Teng Fan Yan-Ping Bao
Yan-Ping Bao Ying Han
Ying Han Jing-Xu Chen
Jing-Xu Chen Wen Xie
Wen Xie Lin Lu
Lin Lu