- 1The Center of Gerontology and Geriatrics, West China Hospital of Sichuan University, Chengdu, China
- 2Department of Psychiatry, Hospital of Chengdu Office of People's Government of Tibetan Autonomous Region, Chengdu, China
- 3Mental Health Center and Psychiatric Laboratory, West China Hospital of Sichuan University, Chengdu, China
Objective: The purpose of this meta-analysis was to summarize the prevalence and risk factors of mental health problems among healthcare workers during the COVID-19 pandemic.
Methods: We applied an optimized search strategy across the PubMed, EMBASE, Scopus, PsycINFO, and four Chinese databases, with hand searching supplemented to identify relevant surveys. Studies were eligible for inclusion if they were published in peer-reviewed literature and used a validated method to assess the prevalence and risk factors of mental health problems among healthcare workers during the COVID-19 pandemic. Heterogeneity was quantified using Q statistics and the I2 statistics. The potential causes of heterogeneity were investigated using subgroup analysis and meta-regression analysis. Sensitivity analysis was performed to examine the robustness of the results.
Results: We pooled and analyzed data from 20 studies comprising 10,886 healthcare workers. The prevalence of depression, anxiety, insomnia, post-traumatic stress symptoms, phobia, obsessive–compulsive symptoms, and somatization symptoms was 24.1, 28.6, 44.1, 25.6, 35.0, 16.2, and 10.7%, respectively. Female and nurses had a high prevalence of depression and anxiety. Frontline healthcare workers had a higher prevalence of anxiety and a lower prevalence of depression than the those in the second-line. Furthermore, the proportion of moderate–severe depression and anxiety is higher in the frontline. Additionally, four studies reported on risk factors of mental health problems.
Conclusions: In this systematic review, healthcare workers have a relatively high prevalence of depression, anxiety, insomnia, post-traumatic stress symptoms, phobia, obsessive–compulsive symptoms, and somatization symptoms during the COVID-19 pandemic, and focus should be on the healthcare workers at high risk of mental problems. Mental health problems in healthcare workers should be taken seriously, and timely screening and appropriate intervention for the high-risk group are highly recommended.
Systematic Review Registration:https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020179189.
Introduction
At the end of 2019, an emerging infectious disease named coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) broke out and caused a global pandemic that put healthcare workers (HCWs) across the world under unprecedented challenges and huge psychological impact (1, 2). In the fight against COVID-19, HCWs played a leading role. The HCWs were in the vanguard of the battle to combat COVID-19, providing medical services to the most affected areas (3). The mental health of HCWs was greatly challenged during the Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS) (4–7). As generally known, COVID-19 is more contagious than SARS and MERS (8, 9) and can bring HCWs on the frontline mental health problems (10–14). Similarly, during the COVID-19 pandemic, HCWs encountered a huge psychological burden, with a high prevalence of depression, anxiety, insomnia, and distress (15, 16). Moreover, frontline HCWs, in fighting COVID-19, have more severe degrees of mental health symptoms than other HCWs (15, 17). Beyond the effects of mental health problems on individuals, the mental health problems of HCWs may link to poor-quality patient care and increased medical errors (18, 19). A reliable estimate of the prevalence of mental health problems among HCWs during the COVID-19 pandemic is of vital importance to its prevention, identification, and treatment. To the best of our knowledge, there has not been a meta-analysis of the prevalence of mental health problems and risk factors among HCWs during the COVID-19 pandemic published in the literature. We conducted a systematic review and meta-analysis of the prevalence of mental health problems and risk factors among HCWs during the COVID-19 pandemic to identify at-risk HCWs and provide timely assistance and intervention.
Methods
Protocol
The protocol of our study has been registered on the International Prospective Register of Systematic Reviews (PROSPERO, CRD42020179189). The review methods are described in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines (20) and the Meta-analysis of Observational Studies in Epidemiology criteria (21).
Search Strategy and Study Eligibility
The search was performed in all fields in the PubMed, EMBASE, Scopus, PsycINFO, and four Chinese databases, including Chinese Biomedical Literature Database, China National Knowledge Infrastructure, China Science and Technology Journal Database, and Wanfang database, with no language restrictions, from January 1, 2020 (subsequent to the emergence of COVID-19 in China) to April 14, 2020. The detailed search terms and full strategies are available in Supplementary Material 1. Additionally, a manual search was performed by reviewing the reference lists of the related articles by two investigators. Where necessary, we contacted the authors for any additional data.
Population-based or hospital-based studies fulfilling the following criteria were included in the present analysis: (1) the HCWs including doctors, nurses, and other medical personnel who were directly or indirectly involved in the diagnosis, treatment, or care of patients with confirmed or suspected cases of COVID-19, (2) studies reported the prevalence or risk factors of mental health problems (depression, anxiety, insomnia, etc.) among HCWs which were assessed by structured interviews or validated questionnaires, (3) cross-sectional or cohort studies, and (4) published in a peer-reviewed journal.
Studies without original data and studies in which the data could not be reliably extracted after corresponding with the authors were excluded. If the same sample was reported in more than one study, the larger sample size with the longest follow-up duration will be included.
Data Extraction and Quality Assessment
Two authors independently extracted the data, reported by the selected articles, and documented the following details in a standardized table: general information of publication (first author, year and location of the study, study period, and language), study design (cohort or cross-sectional), survey method, sampling method, study sample origin (population-based or hospital-based), sample size, number of HCWs, number of female HCWs, number of mental health problems among HCWs, instrument used to assess mental health problems, risk factors of each mental health problem, and the effects of each risk factor. The methodological quality of the included cross-sectional studies was assessed using an 11-item checklist which was recommended by the Agency for Healthcare Research and Quality (AHRQ). The answer to each item is “no,” “unclear,” and “yes,” respectively. Study quality was defined as follows: low quality (0–3 yes), moderate quality (4–7 yes), and high quality (8–11 yes). Any discrepancies will be resolved by consensus, and if necessary, a third reviewer will be consulted to arbitrate.
Data Synthesis and Analysis
The pooled prevalence of each mental health problem and its 95% confidence intervals (CI) were calculated using random-effects meta-analysis that accounted for the heterogeneity of studies (22). The heterogeneity of studies was assessed by Q-test and I2. I2 > 50% and p < 0.05 in the Q-test were interpreted as the presence of significant heterogeneity (23, 24). When significant heterogeneity was identified, the source of heterogeneity was explored by subgroup analysis and meta-regression. Subgroup analyses were conducted with stratification by sample size, staff type, position, and gender. Sensitivity analysis using the leave-one-out method was performed to examine the robustness of the results. The potential publication bias was evaluated by funnel plot and the Egger linear regression test (25, 26). The statistical tests were two-sided and used a significance threshold of P < 0.05. We performed the statistical analysis in R (version 4.0.0; https://www.r-project.org/). A systematic narrative synthesis will be conducted if it is impossible to handle any meta-analysis.
Results
Study Characteristics
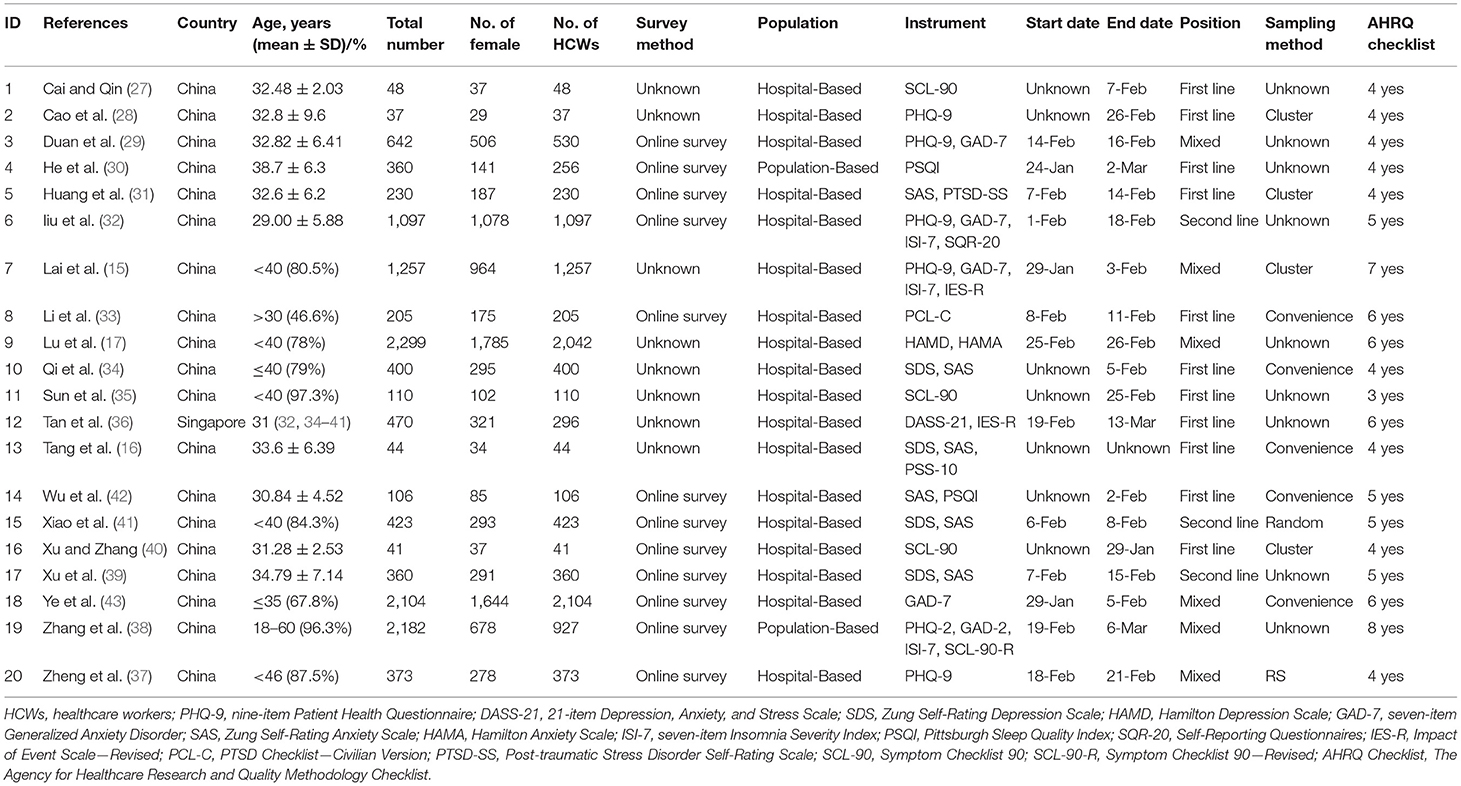
According to the search strategy, a total of 1,898 records were retrieved, and 20 records were finally included (Figure 1). All studies were of a cross-sectional design, involving a total of 10,886 HCWs in 12,788 individuals for the quantitative synthesis; 70% of all participants were women, and 80% of the research were completed by February 2020. Nineteen studies took place in China, plus one in Singapore. Five studies were published in English, and the remaining 15 studies were published in Chinese. The median of participants per study was 639 (range, 37–2,299). Various instruments were utilized. For depression, the most commonly used tools were the Zung Self-Rating Depression Scale, the nine-item Patient Health Questionnaire, the Symptom Checklist-90 (SCL-90), and the 21-item Depression, Anxiety, and Stress Scale (DASS-21). For anxiety, the Zung Self-Rating Anxiety Scale, the SCL-90, and the seven-item Generalized Anxiety Disorder were used. For insomnia, the seven-item Insomnia Severity Index and the Pittsburgh Sleep Quality Index were used. For post-traumatic stress symptoms (PTSS), the Post-traumatic Stress Disorder Self-Rating Scale (PTSD-SS), the Impact of Event Scale—Revised version (IES–R), and the PTSD Checklist—Civilian version (PCL-C) were used. Obsessive–compulsive symptoms, somatization symptoms, and phobia were assessed by the SCL-90 and the 90-item Symptom Checklist—Revised. Eleven studies included frontline HCWs only, six included both frontline and second-line HCWs, and three included second-line HCWs only. When evaluated by the AHRQ assessment criteria, one study received eight points, one received seven points, four received six points, four received five points, nine received four points, and one received three points. Most studies are of moderate quality, with methodological quality scores ranging from 4 to 7. The detailed characteristics of the included studies are shown in Table 1.
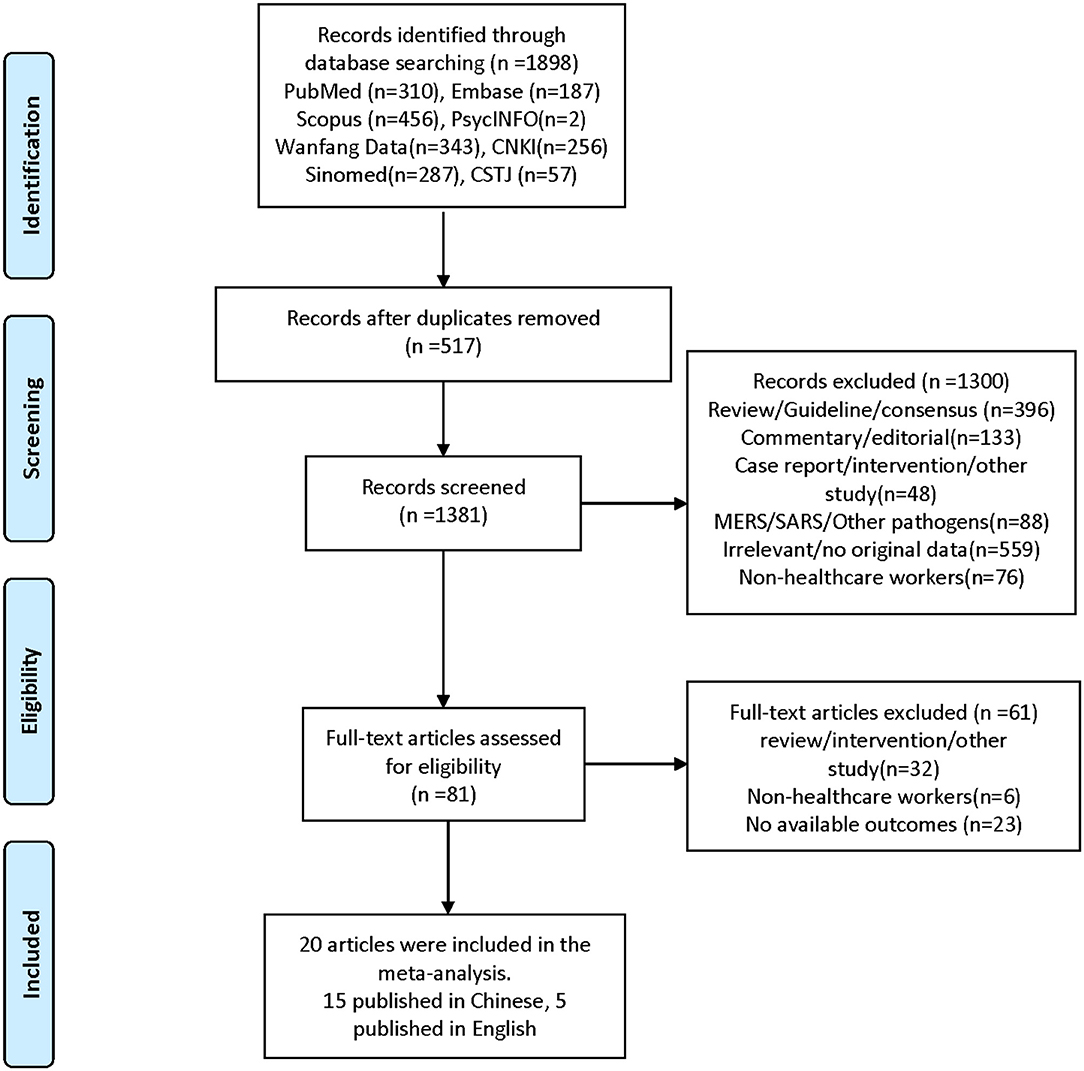
Figure 1. Preferred reporting items for systematic reviews and meta-analyses flow diagram of included studies (20).
Prevalence of Mental Health Problems in HCWs
Prevalence of Depressive Symptom
Fourteen studies (15–17, 27–29, 32, 34–41) reported that the pooled prevalence of depressive symptom among HCWs was 24.1% (95% CI: 16.2–32.1%, I2 = 99%, P < 0.01), with a range from 4.2 to 50.4% (Figure 2A). A subgroup analysis revealed that the second-line HCWs (36.2%, 95% CI: 28.9–43.5%, I2 = 94%, P < 0.01) and female HCWs (38.6%, 95% CI: 9.9–67.2%, I2 = 99%, P < 0.01) had a higher prevalence of depression symptom than frontline and male HCWs separately (Figure 3). About 9.6% of HCWs were identified by instruments as individuals with moderate to severe depression (Figure 4A). Among them, the prevalence of moderate to severe depression in frontline HCWs (14.6%, 95% CI: 6.3–23.0%, I2 = 91%, P < 0.01) is higher than those in the second-line (8.7%, 95% CI: 3.9–13.4%, I2 = 94%, P < 0.01; Figure 4B).
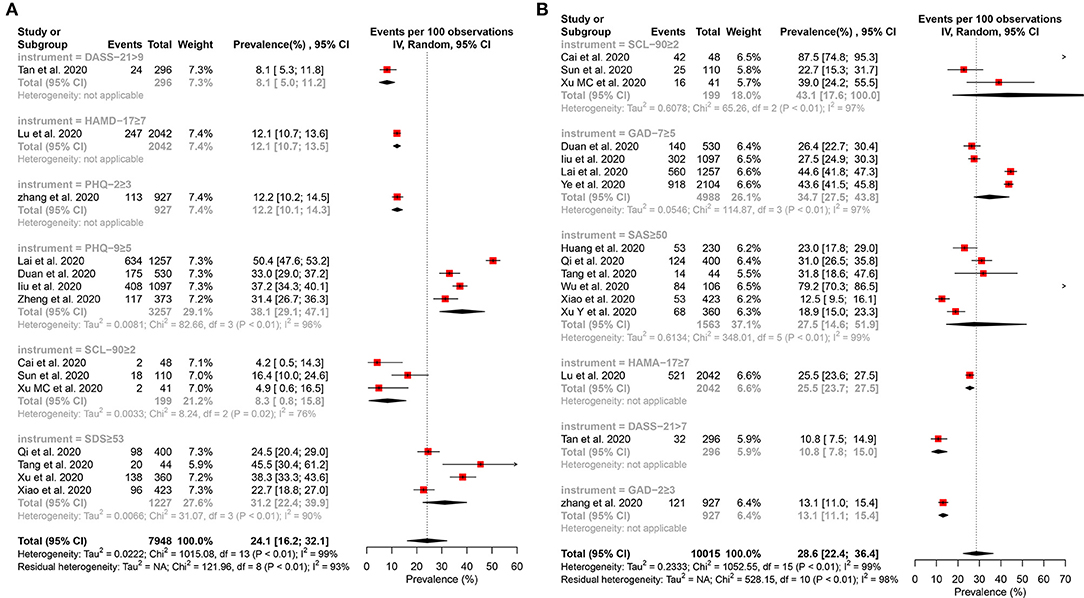
Figure 2. Forest plot for the meta-analysis of the prevalence of depression and anxiety among healthcare workers. (A) Forest plot of the prevalence of depression. (B) Forest plot of the prevalence of anxiety.
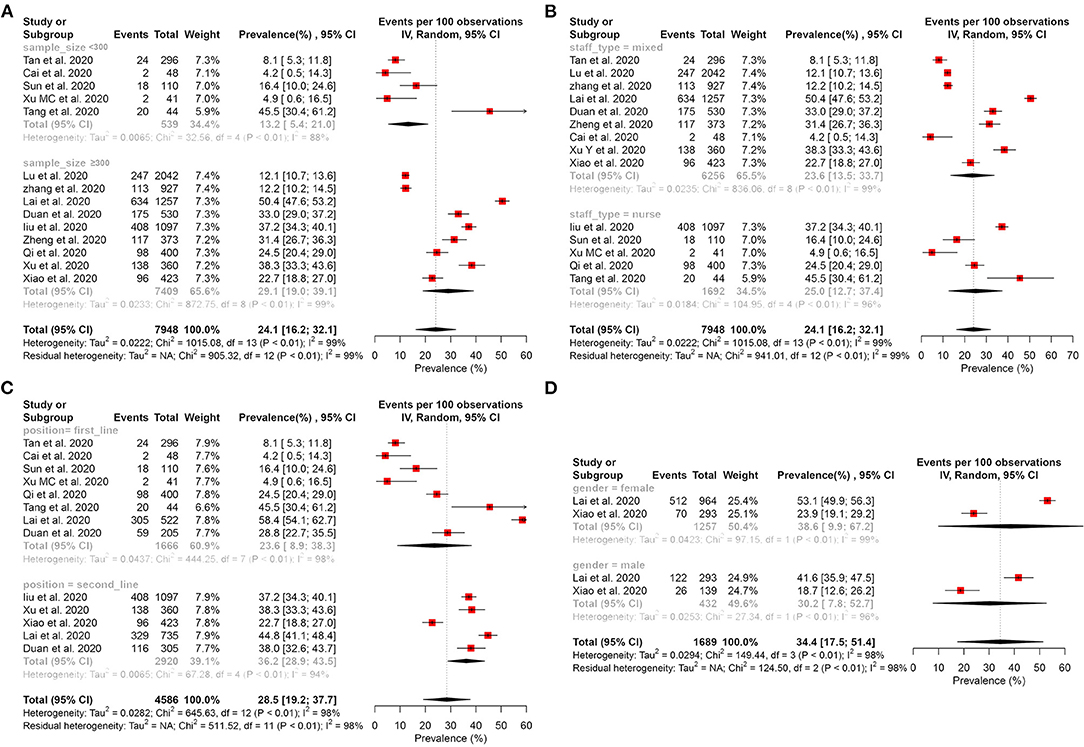
Figure 3. Subgroup analysis of the prevalence of depression among healthcare workers. (A) Subgroup analysis stratification by sample size. (B) Subgroup analysis stratification by staff type. (C) Subgroup analysis stratification by position. (D) Subgroup analysis stratification by gender.
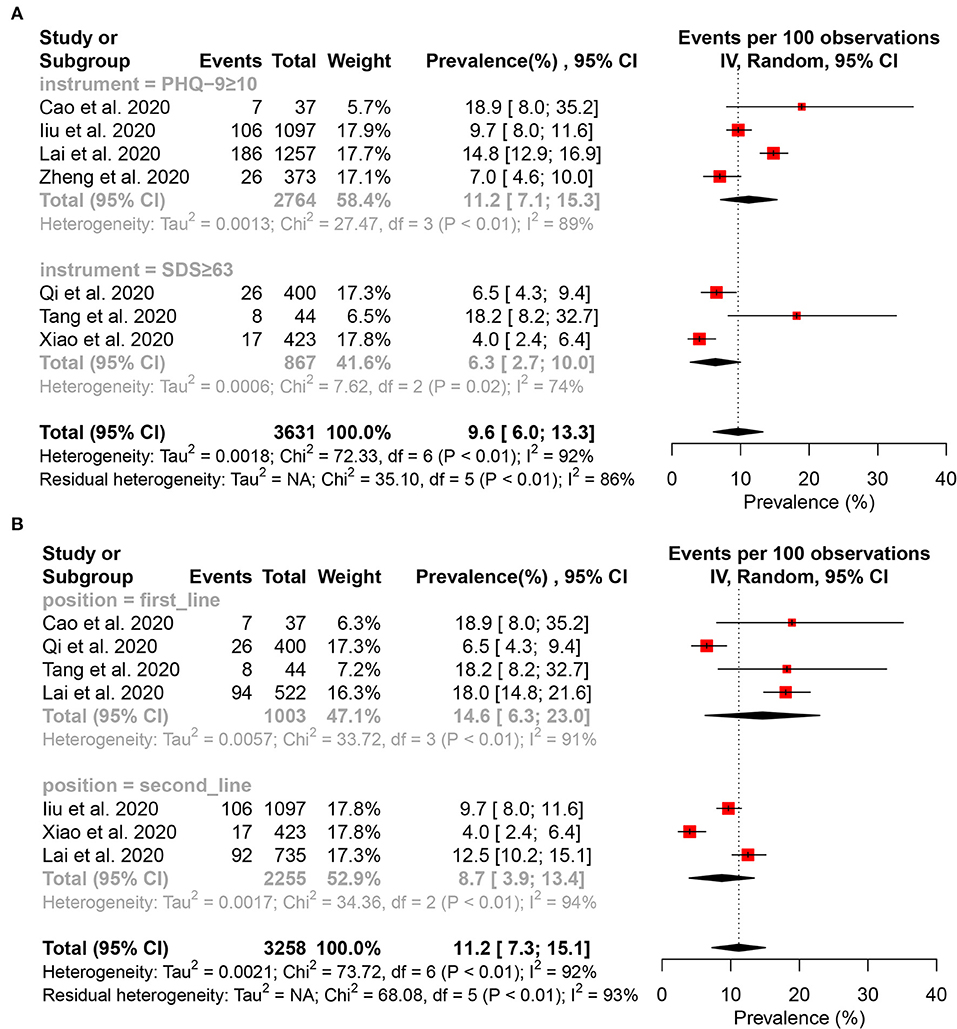
Figure 4. Forest plot for the meta-analysis of the prevalence of moderate to severe depression and subgroup analysis among healthcare workers. (A) Forest plot of the prevalence of moderate to severe depression. (B) Forest plot of moderate to severe depression stratification by position.
Prevalence of Anxiety Symptom
Sixteen studies (15–17, 27, 29, 31, 32, 34–36, 38–43) reported that the pooled prevalence of anxiety among HCWs was 28.6% (95% CI: 22.4–36.4%, I2 = 99%, P < 0.01), with a range from 10.8 to 87.5% (Figure 2B). In the subgroup analysis stratified by position, the frontline HCWs (33.5%, 95% CI: 23.5–47.7%, I2 = 98%, P < 0.01) had a higher prevalence of anxiety than the second-line HCWs (Figure 5C). Of the 16 studies, seven studies reported that the prevalence of anxiety is higher in nurses (36.8%, 95% CI: 26.8–50.5, P < 0.001) than that in the mixed staff type including nurses and doctors (Figure 5B). In the subgroup stratified by gender, female HCWs (26.6%, 95% CI: 13.1–53.9%, I2 = 98%, P < 0.01) had a higher prevalence of anxiety than male HCWs (Figure 5D). About 7.2% of HCWs were identified by instruments as individuals with moderate to severe anxiety (Figure 6A). Similar to the symptoms of depression, the anxiety symptoms of frontline HCWs are more severe than that of the second-line HCWs (Figure 6B).
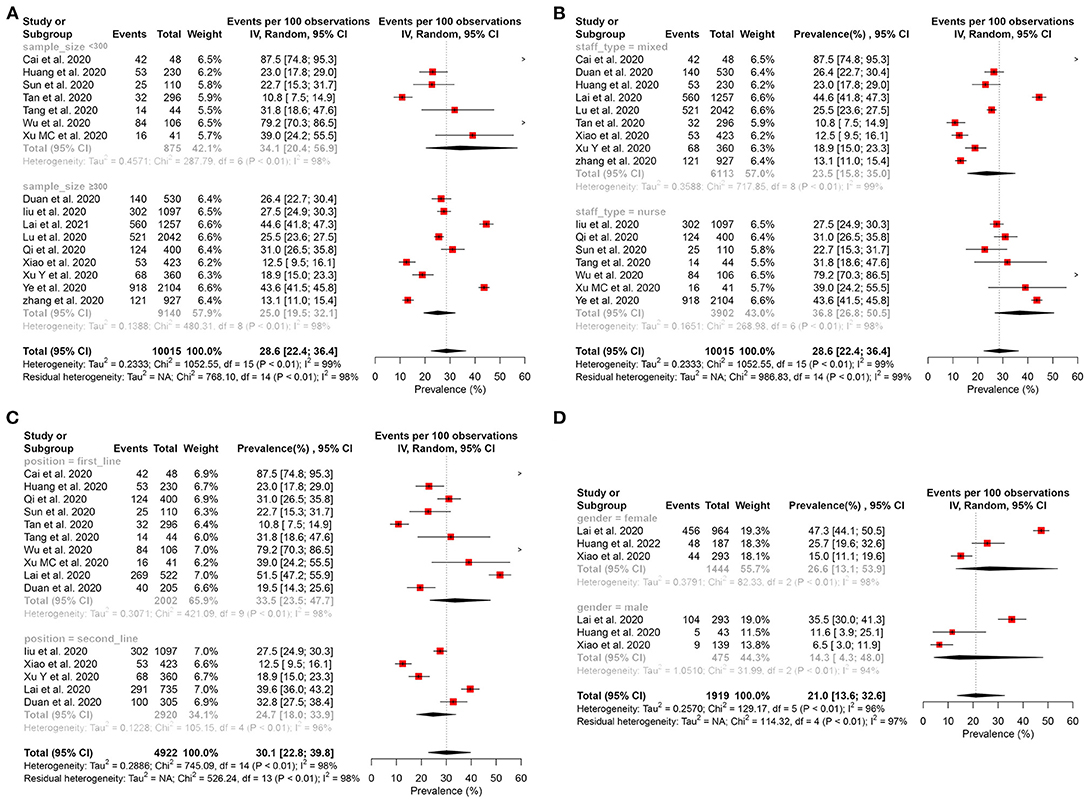
Figure 5. Subgroup analysis of the prevalence of anxiety among healthcare workers. (A) Subgroup analysis stratification by sample size. (B) Subgroup analysis stratification by staff type. (C) Subgroup analysis stratification by position. (D) Subgroup analysis stratification by gender.
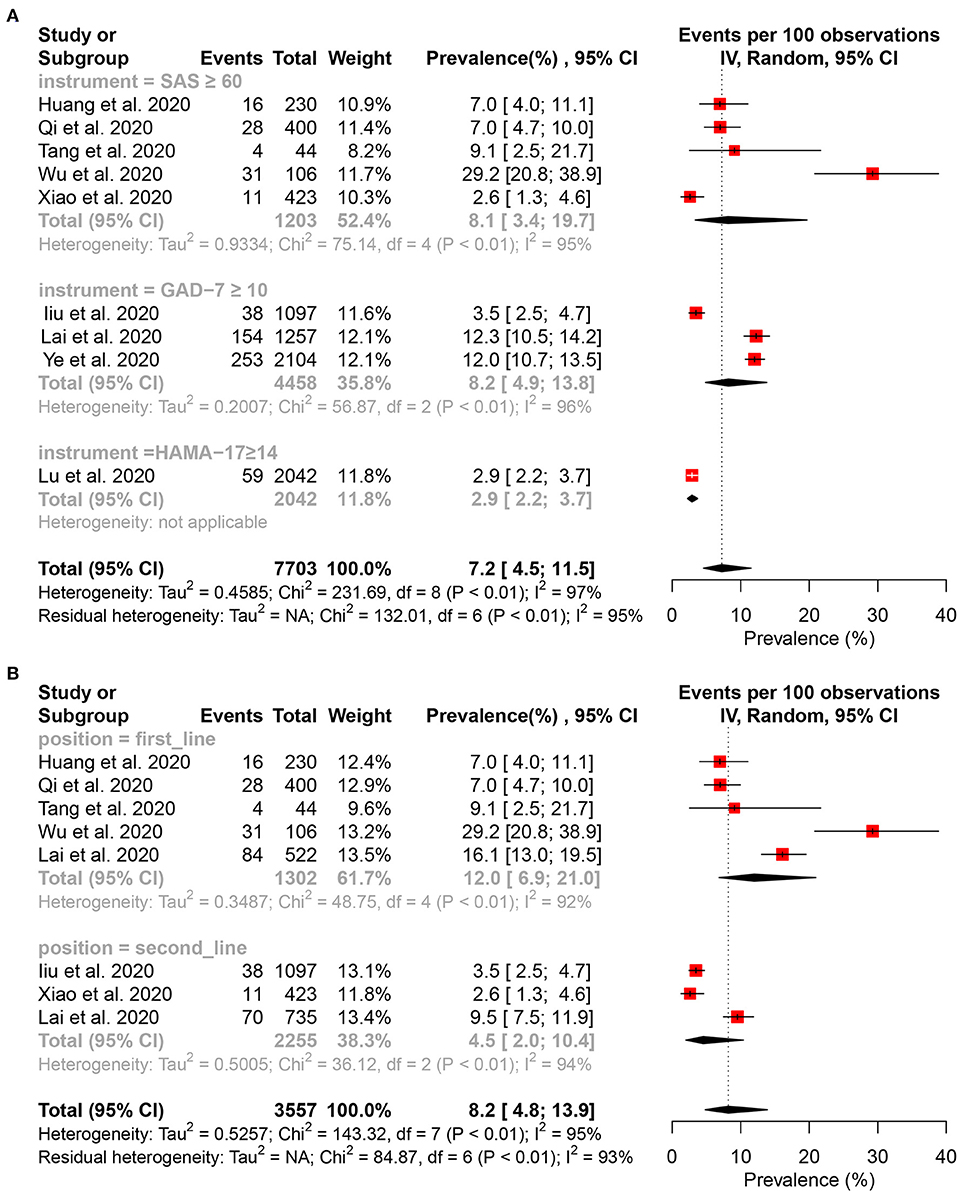
Figure 6. Forest plot for the meta-analysis of the prevalence of moderate to severe anxiety and subgroup analysis among healthcare workers. (A) Forest plot of the prevalence of moderate to severe anxiety. (B) Forest plot of moderate to severe anxiety stratification by position.
Prevalence of Insomnia
Five studies (15, 30, 32, 38, 42) reported that the pooled prevalence of insomnia among HCWs was 44.1% (95% CI: 31.3–57.0%, I2 = 98%, P < 0.01), with a range from 21.3 to 65.2% (Figure 7A). About 11.8% of the HCWs were identified by instruments to be with moderate to severe anxiety (Figure 7B).
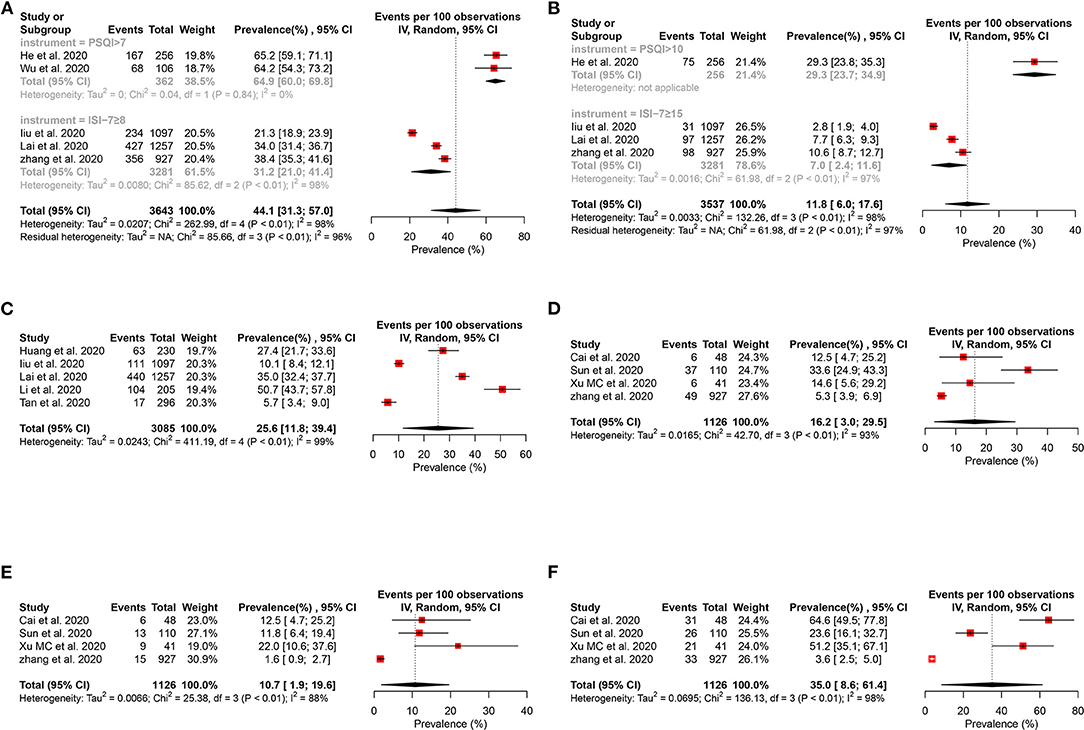
Figure 7. Forest plot for the meta-analysis of the prevalence of other mental health problems among healthcare workers. (A) Forest plot of the prevalence of insomnia. (B) Forest plot of the moderate to severe insomnia. (C) Forest plot of the prevalence of distress. (D) Forest plot of the prevalence of obsessive–compulsive symptoms. (E) Forest plot of the prevalence of somatization symptoms. (F) Forest plot of the prevalence of phobia.
Prevalence of PTSS
Five studies (15, 31–33, 36) reported that the pooled prevalence of PTSS among the HCWs was 25.6% (95% CI: 11.8–39.4%, I2 = 99%, P < 0.01), with a range from 5.7 to 50.7% (Figure 7C).
Other Mental Health Problems
Four studies (27, 35, 38, 40) evaluated obsessive–compulsive symptoms (Figure 7D), somatization symptoms (Figure 7E), and phobia (Figure 7F), and their prevalence were 16.2% (95% CI: 3.0–29.5%, I2 = 93%, P < 0.01), 10.7% (95% CI: 1.9–19.6%, I2 = 88%, P < 0.01), and 35.0% (95% CI: 8.6–61.4%, I2 = 98%, P < 0.01) separately.
Risk Factors of Mental Health Problems
A total of four studies reported on the risk factors of mental health problems (15, 17, 29, 38). Due to a lack of consistency in methods, outcome metrics, and control groups, a narrative synthesis of risk factors was conducted, with the main findings tabulated (Table 2). Poor health status/organic diseases, female, working in a secondary hospital, intermediate technical title, and frontline/high-risk contact with COVID-19 were the risk factors for depression. Compared with non-medical staff working in hospitals, the occupational attributes of medical staff were a protective factor. For anxiety, the risk factors were as follows: fear of COVID-19 infection, poor health status/organic diseases, female, working in a secondary hospital, intermediate technical title, frontline/high-risk contact with COVID-19, and living in rural areas. Similar to the protective factor of depression, the professional attribute of medical staff was the protective factor relative to non-medical staff working in hospitals. Working in frontline, living in rural areas, contact with COVID-19 patients, and organic diseases were the risk factors of insomnia. Female, intermediate technical title, and frontline were the risk factors of PTSS, while working outside Hubei province was the protective factor. Living in rural areas, organic diseases, and contact with patients with COVID-19 were the risk factors of obsessive–compulsive symptoms. The risk factors for somatization symptoms were living in rural areas and organic diseases.
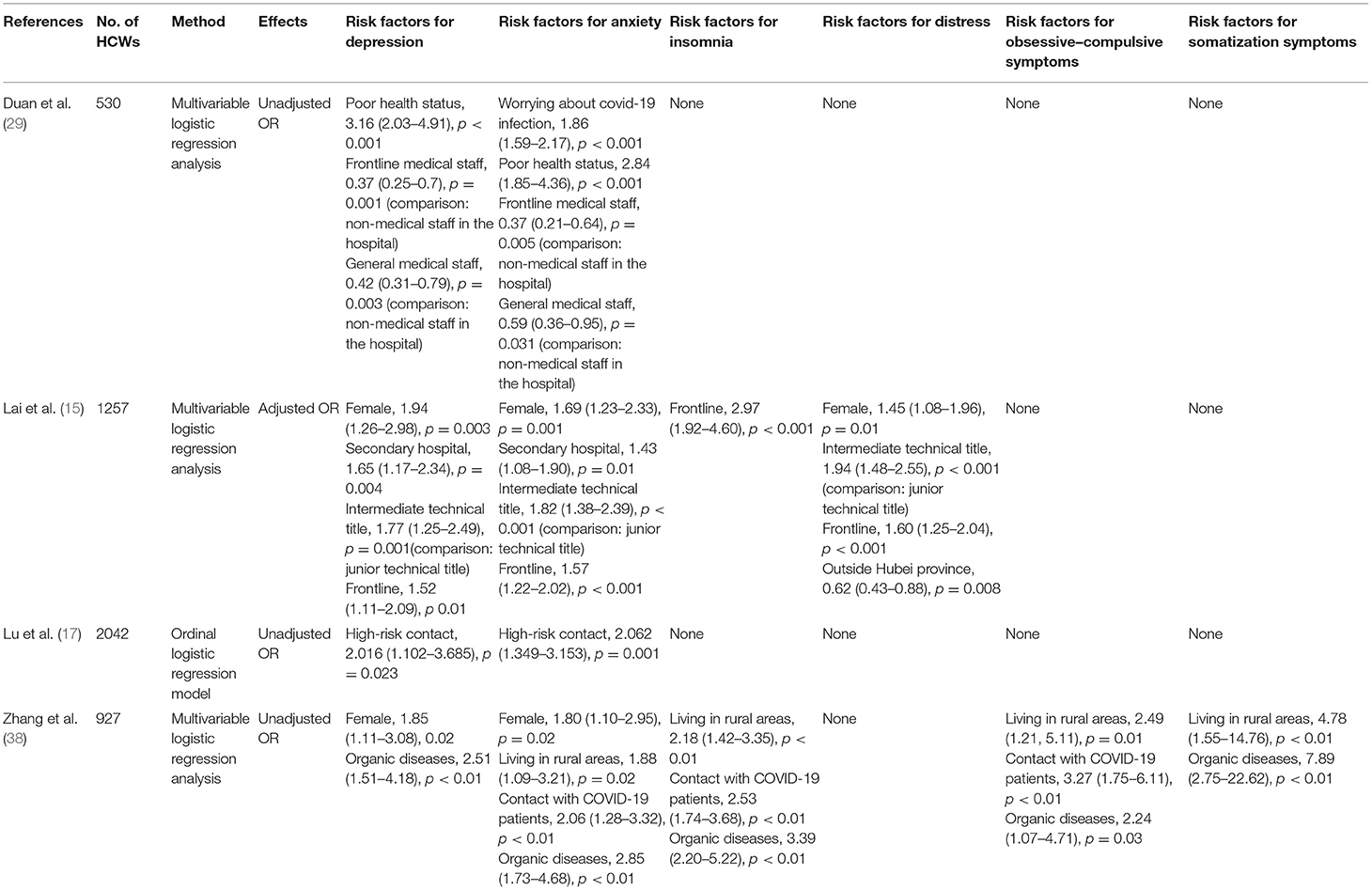
Table 2. Risk factors of mental health problems among healthcare workers during the COVID-19 pandemic.
Heterogeneity Analysis
To identify potential sources of heterogeneity, a subgroup analysis was conducted. However, high heterogeneity was not significantly explained by sample size, staff type, position, and gender (Figures 3, 5). In the univariate meta-regression analyses of the prevalence of depression, a significant estimate was found for the covariate of instruments with R2 (amount of heterogeneity accounted for) = 67.75%, P < 0.0001. No significant estimates were found for the covariates of sample size (less or more than 300), hospital (survey in one or more hospital), country (China or another country), position (frontline or second-line), or staff type (nurses or mixed with nurses and doctors). The meta-regression showed that country was significantly associated with the prevalence of anxiety (R2 = 4.63%, P < 0.0001); however, it was not significantly correlated with instrument (R2 = 18.11%, P = 0.0533), sample size (R2 = 19.56%, P = 0.1469), hospital (R2 = 0.00%, P = 0.7880), position (R2 = 11.11%, P = 0.1744), and staff type (R2 = 0.00%, P = 0.1030). A sensitivity analysis was conducted by excluding, one by one, the included studies that demonstrated no substantial alteration (Supplementary Tables 1, 2: Supplementary Figures 1, 2).
Publication Bias
The funnel plot for the primary outcomes seems somewhat asymmetrical (Supplementary Figures 3, 4). However, the Egger's linear regression test of funnel plot asymmetry was performed, and it indicated no significant asymmetry (Pdepression = 0.3001, Panxiety = 0.1045).
Discussion
The present study investigates the prevalence and risk factors of mental health problems among HCWs during the COVID-19 pandemic based on 10,886 HCWs summarized in 20 cross-sectional studies. According to our research, the prevalence of depression, anxiety, insomnia, PTSS, phobia, obsessive–compulsive symptoms, and somatization symptoms was 24.1, 28.6, 44.1, 25.6, 35.0, 16.2, and 10.7%, respectively. These findings highlight an important issue in HCWs during the COVID-19 pandemic.
It is no surprise that HCWs have a much higher prevalence of mental health problems during the COVID-19 pandemic. There are many factors that can explain this. The ever-increasing number of confirmed and suspected cases, overwhelming workload, depletion of personal protection equipment, widespread media coverage, lack of specific drugs, and feelings of being inadequately supported may all contribute to the mental burden of these HCWs (44). Previous studies showed that HCWs feared contagion and infection of their family and experienced high levels of PTSS, anxiety, and depression symptoms during the outbreak of SARS in 2003 (45, 46). The mental health problems faced by medical staff may be related to many difficulties in work safety, such as the insufficient understanding of the disease at the initial stage, the lack of knowledge concerning prevention and control, the long-term heavy workload, the high risk of exposure to confirmed or suspected cases, the shortage of medical protective equipment, the lack of rest, and the exposure to critical life events during the COVID-19 pandemic (38, 47).
It is worth noting that 25.6% of HCWs suffer from PTSS. Post-traumatic stress disorder (PTSD) is a common consequence of major disasters. During the COVID-19 pandemic, HCWs have endured huge threats and unprecedented challenges, which may cause them to develop acute stress disorder that will potentially degenerate into chronic PTSD over time. A survey conducted 2 months after the outbreak of SARS in Singapore revealed that ~20% of HCWs were suffering from PTSD (48). What is more, a cohort study that lasted 30 months post-SARS among SARS survivors found that HCWs have a much higher percentage of chronic PTSD than non-HCWs (40.7 vs. 19%; P = 0.031) (49). Additionally, female, working in frontline, and intermediate technical title were the risk factors of PTSS during the COVID-19 pandemic; however, working outside Hubei province was the protective factor (15).
We found that 70% of all participants were female (most of whom were nurses). Moreover, a subgroup analysis revealed that females and nurses had a high prevalence of depression and anxiety. During the SARS outbreak, a study conducted among HCWs in emergency departments also showed that nurses were more likely to develop distress than physicians (50). During the COVID-19 pandemic, frontline nurses may be at risk of infection due to the close and frequent contact with patients and the longer-than-usual working hours during the COVID-19 pandemic. This also reminds us that the society should be more concerned on the mental health of women and nurses during the major epidemic.
Another important finding in the subgroup analysis revealed that the frontline HCWs had a higher prevalence of anxiety and a lower prevalence of depression than the second-line HCWs. A high level of anxiety in the early stage of the emerging infectious disease may be an adaptive defense mechanism response to potentially threatening events (51). However, when it is chronic or disproportionate, it becomes harmful and can be a key component in the development of various psychiatric disorders (51, 52). What deserves our attention is that, compared with the second-line HCWs, the proportions of moderate-to-severe anxiety and depression are higher among the frontline staff. Working in the center of a pandemic area such as Wuhan or high-risk contact with COVID-19 patients in frontline positions, such as the emergency department, respiratory department, fever clinic, etc., is a risk factor for mental health problems (15, 17, 38). For this reason, we should pay more attention to the frontline medical staff. Timely screening and appropriate intervention are important to reduce the severity and chronicity of mental health problems.
In addition, the physical condition of medical staff was an important risk factor for mental health problems. The prevalence of depression, anxiety, insomnia, obsessive–compulsive symptoms, and somatization symptoms of medical staff with poor health conditions or comorbidities of organic diseases is higher than that of the healthy ones (29, 38). Surprisingly, living in rural areas is a risk factor for anxiety, insomnia, obsessive–compulsive symptoms, and somatization symptoms (38). Differences in the working environment, medical technology, and the knowledge of COVID-19 may partially explain this phenomenon.
Limitations should be considered when interpreting the findings of this study. First, it was limited in scope. Of the 20 studies, 19 are from China, 15 of which are published in Chinese and thus limiting the generalization of other countries. Second, it is important to note that the vast majority of participants were assessed by a self-rating scale rather than by gold-standard diagnostic clinical interviews for mental health disorders, and the duration of symptoms of most participants did not meet the diagnostic criteria. The sensitivity and the specificity of these instruments for diagnosing mental health problems vary substantially. Third, all studies are cross-sectional studies, and there is no longitudinal study. Moreover, most of them were completed in February 2020 or earlier. With the increasingly arduous situation, the mental health symptoms of HCWs could become more severe. Fourth, many other factors that could predispose medical staff to anxiety, for example, family history and emotional trauma, could not be assessed due to the wide variability of factors examined in the studies. Finally, only a few studies have explored the risk factors of mental health problems, which are not sufficient to fully understand the problem. Moreover, all studies on risk factors were of a cross-sectional design, without baseline control and follow-up data, so it is impossible to determine the causal relationship between them. Some risk factor studies have not controlled for confounding factors and cannot exclude the influence of factors such as working position, COVID-19 exposure intensity, and some sociodemographic factors.
Conclusions
In this systematic review, HCWs have a relatively high prevalence of depression, anxiety, insomnia, PTSS, phobia, obsessive–compulsive symptoms, and somatization symptoms during the COVID-19 pandemic, and focus should be on the HCWs at high risk of mental health problems. Further research is needed to identify effective strategies for preventing and treating mental health problems among HCWs during the COVID-19 pandemic.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
QH, DW, HW, and QW contributed to research conception and study design and contributed to data analysis/interpretation. QH, DW, MX, YT, YD, LZ, MD, and YW contributed to search and data acquisition. QH and DW contributed to statistical analysis and manuscript writing. QW and HW took responsibility that this study has been reported honestly, accurately, transparently, and contributed very important intellectual content during manuscript drafting or revision and accepts accountability for the work. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.567381/full#supplementary-material
References
1. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. (2020) 382:1199–207. doi: 10.1056/NEJMoa2001316
2. Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. (2020) 368:m1211. doi: 10.1136/bmj.m1211
3. Xiang YT, Jin Y, Wang Y, Zhang Q, Zhang L, Cheung T. Tribute to health workers in China: a group of respectable population during the outbreak of the COVID-19. Int J Biol Sci. (2020) 16:1739–40. doi: 10.7150/ijbs.45135
4. Chen CL. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry. (2004) 185:127–33. doi: 10.1192/bjp.185.2.127
5. Qushmaq IA. Healthcare workers emotions, perceived stressors and coping strategies during MERS-CoV outbreak. Clin MedRes. (2016) 14:7–14. doi: 10.3121/cmr.2016.1303
6. Lu J. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatr Rev Can Psychiat. (2009) 54:302–11. doi: 10.1177/070674370905400504
7. Park JK. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. (2018) 87:123–7. doi: 10.1016/j.comppsych.2018.10.003
8. Liu Y, Gayle AA, Wilder-Smith A, Rocklov J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Travel Med. (2020) 27:taaa021. doi: 10.1093/jtm/taaa021
9. Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. Early release-high contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg infect Dis. (2020) 26:1470–7. doi: 10.3201/eid2607.200282
10. Lima CKT, Carvalho PMM, Lima I, Nunes J, Saraiva JS, de Souza RI, et al. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Res. (2020) 287:112915. doi: 10.1016/j.psychres.2020.112915
11. Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. (2020) 7:228–9. doi: 10.1016/S2215-0366(20)30046-8
12. Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. (2020) 7:e14. doi: 10.1016/S2215-0366(20)30047-X
13. Torales J, O'Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. (2020) 66:317–20. doi: 10.1177/0020764020915212
14. Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. (2020) 383:510–2. doi: 10.1056/NEJMp2008017
15. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
16. Tang HH, Lu XY, Cai SX, Gong J, Wang L, Li X. Investigation and analysis on mental health status of frontline nurses in wuhan during COVID-19 epidemic. Int Infect Dis. (2020) 9:296–7.
17. Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatr Res. (2020) 288:112936. doi: 10.1016/j.psychres.2020.112936
18. Melnyk BM, Orsolini L, Tan A, Arslanian-Engoren C, Melkus GDE, Dunbar-Jacob J, et al. A national study links nurses' physical and mental health to medical errors and perceived worksite wellness. J Occup Environ Med. (2018) 60:126–31. doi: 10.1097/JOM.0000000000001198
19. Taylor C, Graham J, Potts H, Candy J, Richards M, Ramirez A. Impact of hospital consultants' poor mental health on patient care. Br J Psychiatry. (2007) 190:268–9. doi: 10.1192/bjp.bp.106.023234
20. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:b2535. doi: 10.1136/bmj.b2535
21. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of observational studies in epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
22. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Method. (2010) 1:97–111. doi: 10.1002/jrsm.12
23. Higgins JPT, Thompson SG. Higgins JPT, thompson SGQuantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
24. Higgins JPT, Thompson SG, Decks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
25. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
26. Sterne JAC, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. (2001) 54:1046–55. doi: 10.1016/S0895-4356(01)00377-8
27. Cai HH, Qin Y. Investigation and intervention of psychological status of frontline medical staff in the fight against novel coronavirus pneumonia. Chin General Prac Nurs. (2020) 18:827–8. doi: 10.12104/j.issn.1674-4748.2020.07.045
28. Cao J, Wei J, Zhu H, Duan Y, Geng W, Hong X, et al. A study of basic needs and psychological wellbeing of medical workers in the fever clinic of a tertiary general hospital in Beijing during the COVID-19 outbreak. Psychother Psychosom. (2020) 89:252–4. doi: 10.1159/000507453
29. Duan LS, Guo YM, Sun JN, Jiang YT, Jiang RH, Su B. Mental health status of officers and soldiers in a military hospital amid the epidemic of COVID-19. Med J Chin Peoples Armed Police Force. (2020) 31:191–4. doi: 10.14010/j.cnki.wjyx.20200312.003
30. He YH, Wang Y, Wang JS, Hou JB, Wan X. Impact of COVID-19 outbreak on sleep quality of medical staff in Wuhan. Med J Wuhan Univ. (2020) 41:711–4. doi: 10.14188/j.1671-8852.2020.0159
31. Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Chin J Ind Hygiene Occup Dis. (2020) 38:192–5. doi: 10.3760/cma.j.cn121094-20200219-00063
32. Liu XL, Cheng YS, Wang MY, Pan Y, Guo H, Jiang RH, et al. Psychological state of nursing staff in a large scale of general hospital during COVID-19 epidemic. Chin J Nosocomiol. (2020) 30:1634–9. doi: 10.11816/cn.ni.2020-200572
33. Li CS, Mi YY, Chu J, Zhu LQ, Zhang ZY, Liang LY, et al. Investigation and analysis of novel coronavirus front-line nurses' post traumatic stress disorder. J Nurses Train. (2020) 35:615–8. doi: 10.16821/j.cnki.hsjx.2020.25.003
34. Qi JJ, Liu LM, Li WT, Xu YH, Shan X. Investigation and analysis of clinical nurses' psychological status in face of novel coronavirus pneumonia. Chin General Practice Nurs. (2020) 18:703–4. doi: 10.12104/j.issn.1674-4748.2020.06.053
35. Sun SY, Huang Y, Wang Z. Investigation and analysis of nurses' psychological problems in fever clinic during the outbreak of COVID-19. Med J Nat Defend Forces Northwest Chin. (2020) 41:133–8. doi: 10.16021/j.cnki.1007-8622.2020.03.001
36. Tan BYQ, Chew NWS, Lee GKH, Jing M, Goh Y, Yeo LLL, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. (2020) 173:317–20. doi: 10.7326/M20-1083
37. Zheng CM, Shen F, Tian GQ, Zhang L. Investigation on the stress level and depression of medical staff during the novel coronavirus pneumonia. Zhejiang Med J. (2020) 42:406–414. doi: 10.12056/j.issn.1006-2785.2020.42.4.2020-656
38. Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. (2020) 89:242–20. doi: 10.1159/000507639
39. Xu Y, Zhao M, Tang XL, Zhu XY, Chen J. Correlation study between mental health and coping style of medical staff during COVID-19 epidemic. Anhui Med J. (2020) 37:1–4. Available online at: http://kns.cnki.net/kcms/detail/34.1077.R.20200414.0946.002.html
40. Xu MC, Zhang Y. Psychological status survey of first clinical first? line support nurses fighting against pneumonia caused by a 2019 novel coronavirus infection. Chin Nurs Res. (2020) 34:368–70. doi: 10.12102/j.issn.1009-6493.2020.03.002
41. Xiao C, Wang L, Liu JR, Shen XM, Li BR, Zhang SY, et al. Anxiety and depression status among non-first-line medical staff during the outbreak of COVID-19. Sichuan Mental Health. (2020) 33:15–8. doi: 10.11886/scjsws20200214002
42. Wu JJ, Rong X, Chen F, Diao YJ, Chen DC, Jing XC, et al. Investigation on sleep quality of first line nurses in fighting against corona virus disease 2019 and its influencing factors. Chin Nurs Res. (2020) 34:558–62. doi: 10.12102/j.issn.1009-6493.2020.04.107
43. Ye JR, Xia ZC, Xiao AX, Li SY, Lin JK, Nie S, et al. Investigation on nurses' anxiety status and influencing factors during the outbreak of COVID-19. Sichuan Mental Health. (2020) 33:11–4.
44. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. (2020) 323:2133–4. doi: 10.1001/jama.2020.5893
45. Maunder R, Hunter J, Vincent L, Bennett J, Mazzulli T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Can Med Assoc J. (2003) 168:1245–51. Available online at: https://www.cmaj.ca/content/168/10/1245.long
46. Lee AM, Wong JG, Mcalonan GM, Cheung V, Cheung C, Sham PC, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. (2007) 52:233–40. doi: 10.1177/070674370705200405
47. World Health Organization. Shortage of Personal Protective Equipment Endangering Health Workers Worldwide. (2020). Available online at: https://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide (accessed May 10, 2020).
48. Chan AO, Huak CY. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med. (2004) 54:190–6. doi: 10.1093/occmed/kqh027
49. Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. (2009) 31:318–26. doi: 10.1016/j.genhosppsych.2009.03.001
50. Wong TW, Yau JK, Chan CL, Kwong RS, Ho SM, Lau CC, et al. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Euro J Emerge Med. (2005) 12:13–8. doi: 10.1097/00063110-200502000-00005
51. Ornell F, Schuch JB, Sordi AO, Kessler FHP. “Pandemic fear” and COVID-19: mental health burden and strategies. Braz J Psychiatry. (2020) 42:232–5. doi: 10.1590/1516-4446-2020-0008
Keywords: coronavirus disease, healthcare workers, mental health, prevalence, risk factors, meta-analysis
Citation: Hao Q, Wang D, Xie M, Tang Y, Dou Y, Zhu L, Wu Y, Dai M, Wu H and Wang Q (2021) Prevalence and Risk Factors of Mental Health Problems Among Healthcare Workers During the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Front. Psychiatry 12:567381. doi: 10.3389/fpsyt.2021.567381
Received: 29 May 2020; Accepted: 10 May 2021;
Published: 15 June 2021.
Edited by:
Gian Mauro Manzoni, University of eCampus, ItalyReviewed by:
Rossella Procaccia, University of eCampus, ItalyXiancang Ma, First Affiliated Hospital of Xi'an Jiaotong University, China
Copyright © 2021 Hao, Wang, Xie, Tang, Dou, Zhu, Wu, Dai, Wu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongmei Wu, ZHJ3aG1AMTYzLmNvbQ==; Qiang Wang, d2FuZ3FpYW5nMTMwQHNjdS5lZHUuY24=
†ORCID: Qinjian Hao orcid.org/0000-0002-6917-1751
‡These authors have contributed equally to this work
 Qinjian Hao
Qinjian Hao Dahai Wang2‡
Dahai Wang2‡ Yiguo Tang
Yiguo Tang Qiang Wang
Qiang Wang