- The National Clinical Research Center for Mental Disorders and Beijing Key Laboratory of Mental Disorders, Beijing Anding Hospital and The Advanced Innovation Center for Human Brain Protection, Capital Medical University, Beijing, China
Background: Epidemiological data on outbreak-associated depression of Chinese teachers are not available. This study aimed to investigate the prevalence and correlates of depression among teachers during the coronavirus disease 2019 (COVID-19) outbreak in mainland China.
Methods: A large cross-sectional online survey was conducted during the COVID-19 outbreak. Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9). The Connor-Davidson Resilience Scale 25 (CD-RISC 25) and Perceived Stress Scale-10 (PSS-10) were used to measure the mental resilience and stress of participants. The correlative factors of depression were analyzed.
Results: In this study, 1,096 teachers were analyzed with a median (range) age of 41 (20–65) years. Of them, 624 (56.9%) suffered from depression (PHQ-9 total score of >4). The multivariate analyses showed that participants with aged ≥41 years (OR = 0.752, 95% CI:0.578–0.979, p = 0.034), participating in epidemic prevention and control (OR = 1.413, 95% CI:1.070–1.867, p = 0.015), thinking prolonged school closure have bad effect (OR = 1.385, 95% CI:1.017–1.885, p = 0.038), sleep duration/day of <6 h (OR = 1.814, 95% CI:1.240–2.655, p < 0.001), physical exercise duration/day of <30 min (OR = 1.619, 95% CI:1.247–2.103, p < 0.001), spending less time with family (OR = 1.729, 95% CI: 1.063–2.655, p = 0.002), being concerned about COVID-19 (OR = 0.609, 95% CI:0.434–0.856, p = 0.004), having poor mental resilience (OR = 6.570, 95% CI:3.533–12.22, p < 0.001) and higher PSS-10 scores (OR = 9.058, 95% CI:3.817–21.50, p < 0.001) were independently associated with depression.
Conclusion: During the COVID-19 outbreak, depression was common among teachers. Age, participating in epidemic prevention and control, opinions toward distant teaching and prolonged school closure, sleep duration/day, physical exercise duration, spending time with family, attitude toward COVID-19, mental resilience and stress represented the independent factors for suffering from depression.
Introduction
Depression, a common mental disorder with severe psychomotor, affective, and cognitive sequelae (1), is a top public health concern for its high prevalence (2), chronicity (3), as well as grave ramifications, which include increased societal costs (4, 5), disability (5), and mortality (5, 6). Teaching is a not only physically but also mentally challenging occupation, and teachers use a lot of energy in daily work in addition to their familial and personal commitments, all of which are continuous source of stress (7, 8). And teaching was proved to be one of the most stressful jobs in a previous study of 26 jobs (9). Occupational stress can reduce the overall physical and mental well-being of teachers and lead to depression (7). Teachers were consistently reported to be at high risk of depression compared to those in other jobs (10, 11). Previous studies indicated that higher levels of depression may lead to teachers under performing at work (12, 13). As frontline professionals who have daily contact with students, teachers play an important role to play in the well-being and mental health of their students (14, 15). Therefore, early prevention, detection and treatment are essential to protect teachers from depressive symptoms and improve their mental health.
At the end of 2019, the corona virus disease 2019 (COVID-19) was believed to have started from Wuhan, Hubei Province, China and has gained great attention nationwide and globally (16, 17). On March 11, 2020, the COVID-19 was declared as a pandemic by the World Health Organization (WHO) (18). As of November, 2020, the COVID-19 outbreak has resulted in more than 50 million confirmed cases and more than 1.2 million deaths globally, which were far beyond the number of those caused by Middle East respiratory syndrome (MERS) and SARS in 2013 and 2003, respectively. Thus, the epidemic has caused considerable challenges worldwide.
The COVID-19 outbreak had a significant negative impact on daily life and mental health among teachers, due to negative life event and heavy occupational stress, resulting in high risk of depressive symptoms, such as sense of uncertainty, boredom, fear, anger, and loneliness associated with quarantine and challenges due to conflict with children, changes in teaching methods, and insufficient outdoor activities. In addition, the COVID-19 outbreak has raised considerable challenges on mental health services among teachers. So, it is the responsibility of all stakeholders to ensure that the mental and physical impact of the outbreak of COVID-19 on teachers is minimal (18).
However, to date, epidemiological data on outbreak-associated depression among Chinese teachers is not available. It is needed to conduct a nationwide survey to determine the prevalence and correlates of depressive symptoms among teachers during the outbreak of COVID-19 in mainland China. The present study aimed to investigate the prevalence and correlates of depression among teachers during the coronavirus disease 2019 (COVID-19) outbreak in mainland China.
Methods
Study Design and Participants
This was a national cross-sectional, online survey conducted between April 10 and 17, 2020, based on the collaborative research network of the National Clinical Research Center for Mental Disorders, China. Using a snowball sampling method, data were collected with the WeChat-based Wenjuanxing program (https://www.wjx.cn/). The Wenjuanxing program has been widely used in online survey during the COVID-19 pandemic. The inclusion criteria were as follows: (1) the primary, middle, high school and college teachers aged between 20 and 65 years old and; (2) living in mainland China during the COVID-19 epidemic. Participants who completed the questionnaire in <120 s or were not aged 20–65 years were excluded. All participants provided written informed consent. And this study was approved by the Medical Ethical Committee in Beijing Anding Hospital of the Capital Medical University, China.
Assessment Instruments and Data Collection
In the present study, a data collection sheet was used to collect socio-demographic and clinical characteristics such as gender, age, marital status, education background, professional title, school type, participating in epidemic prevention and control, being a parent, parent-child relationship, teaching graduating class, participating in distant teaching, opinions toward distant teaching and prolonged school closure, increased working intensity and time, sleep duration/day, physical exercise duration, spending time with family, attitude toward COVID-19, and presence of depression.
The presence of depression was assessed by the self-reported 9 item-Patient Health Questionnaire (PHQ-9), Chinese version (19, 20). The total score ranges from 0 to 27 (1–4: no depression, 5–9: mild depression, 10–14: moderate depression, 15–19: moderately severe depression, and 20–27: severe depression) (19). The test-retest reliability of PHQ-9 ranges from 0.76 to 0.89, and the Cronbach's alpha ranges from 0.79 to 0.89 (21).
The Connor-Davidson Resilience Scale 25 (CD-RISC 25) was developed as a brief self-evaluation instrument to help quantify participant mental resilience (22, 23). The total score ranges from 0 to 100, with higher scores indicating greater resilience (22, 23). Studies revealed the internal consistency for the CD-RISC scale as 0.89 (22) and 0.92 (24), respectively. Based on quartile deviation, resilience is scored as ≤ 50 representing the poor mental resilience and ≥ 51 representing the good mental resilience in this study.
The Perceived Stress Scale-10 (PSS-10) was used to measure the degree to which the participants identify events as stressful during the past month (25), with a good internal consistency of 0.78–0.91 (25–27). The total score ranges from 0 to 40, with higher scores indicating higher perceived stress (25).
Statistical Analyses
All statistical analyses were performed with SPSS 22.0 software (IBM Corp, Armonk, NY, USA). Statistical significance was set as a p-value < 0.05 (two-tailed). Pearson's test and chi-square test were used to determine the distribution of categorical variables, and Mann–Whitney U-test was used for continuous variables. Univariate and multivariate analyses were performed to examine the correlates of depression using the logistic regression models.
Results
Sample Characteristics and Prevalence of Depression
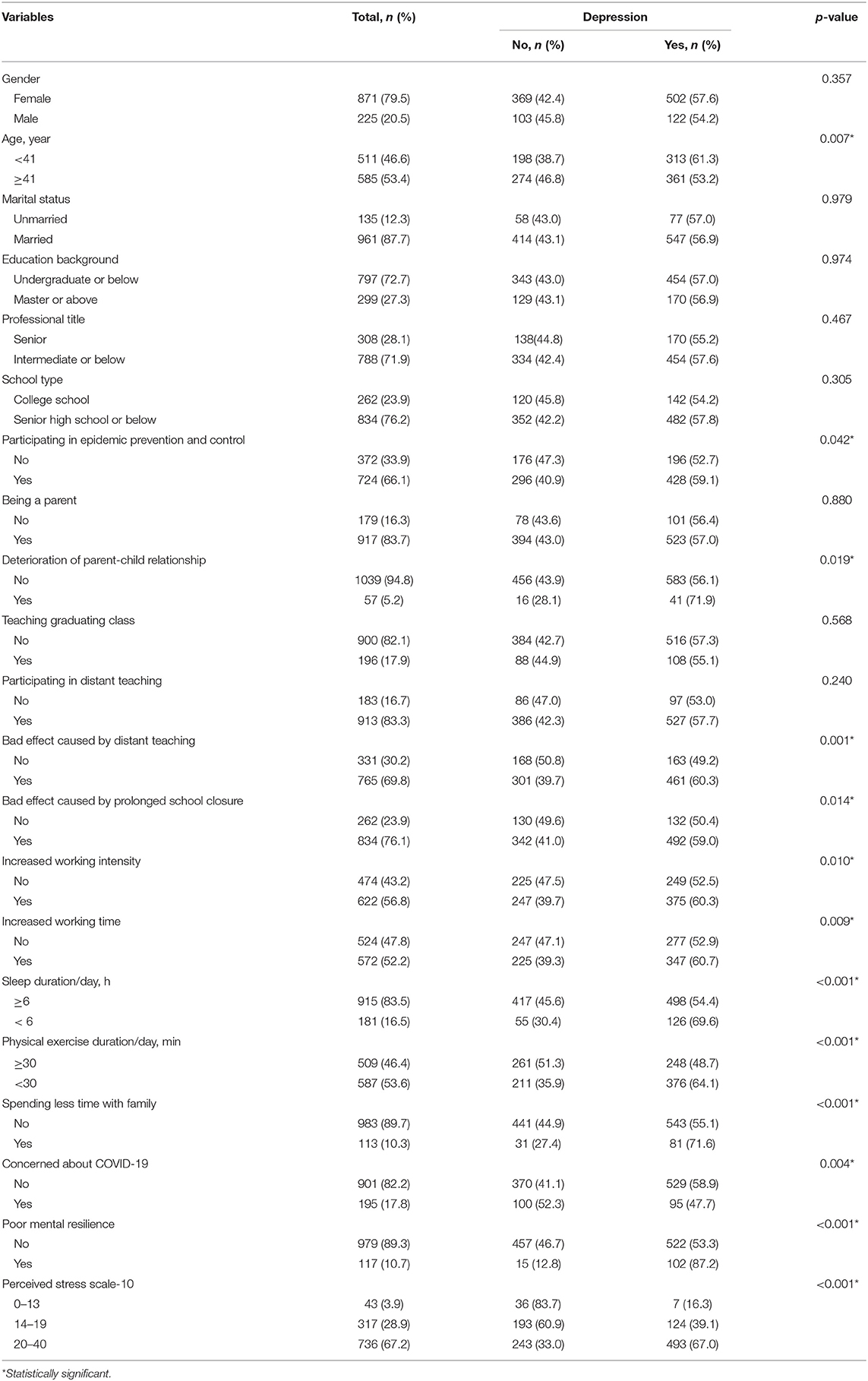
In this study, 1,124 Chinese teachers were invited to participate in the survey. Twenty-eight participants were excluded as they completed the questionnaire in <120 s (n = 18) and were not 20–65 years old (n = 10). Finally, 1,096 teachers were enrolled with a median (range) age of 41 (20–65) years. Of them, 624 (56.9%) suffered from depression with a PHQ-9 score of >4, and 177 (16.1%) suffered from moderate to severe depression with a PHQ-9 score of >9. In addition, 117 (10.7%) teachers had poor mental resilience and 1,053 (96.1%) teachers had high perceived stress with a PSS-10 score of >13. Table 1 showed the socio-demographic and clinical characteristics between depression and no depression groups. We found that depression was more common among teachers who were of <41 years old (53.2 vs. 61.3%, p = 0.007), participated in epidemic prevention and control (52.7 vs. 59.1%, p = 0.042), with deterioration of parent-child relationship (56.1 vs. 71.9%, p = 0.019), thought distant teaching have bad effects (50.4 vs. 59.0%, p = 0.001), thought prolonged school closure have bad effects (49.2 vs. 60.3%, p = 0.014), had increased working intensity or time (52.5% vs. 60.3, p = 0.010; 52.9 vs. 60.7%, p = 0.009, respectively), had sleep duration/day of <6 h (69.6 vs. 54.4%, p < 0.001), had physical exercise duration/day of <30 min (64.1 vs. 48.7%, p < 0.001), spent less time with family (55.1 vs. 71.6%, p < 0.001), not concerned about COVID-19 (47.7 vs. 58.9%, p = 0.004), had poor mental resilience (53.3 vs. 87.2%, p < 0.001), and had higher PSS-10 score (16.3 vs. 39.1% vs. 67.0%, p < 0.001).
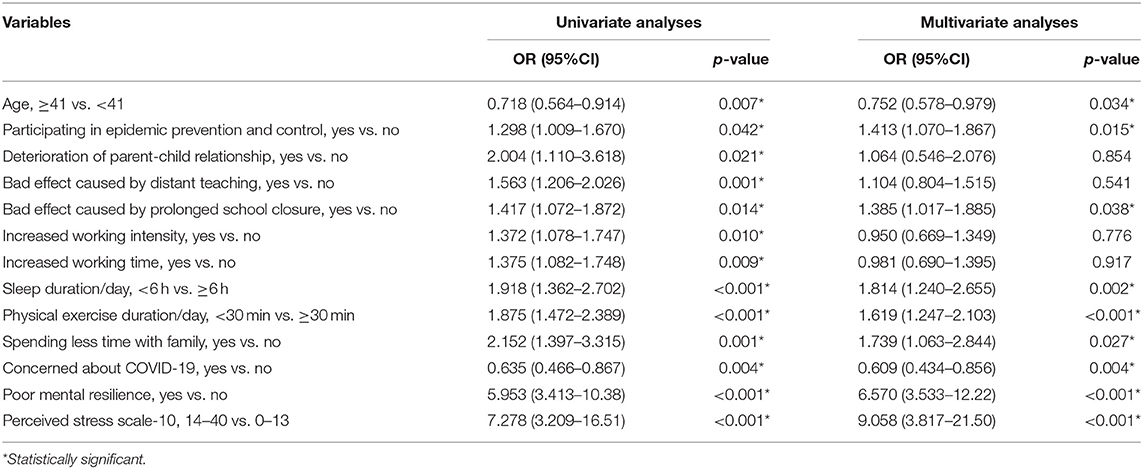
Characteristics Associated With Depression
Univariate logistic regression analysis in this study showed that participants who participated in epidemic prevention and control [odds ratio (OR) =1.298, 95% CI: 1.009–670, p = 0.042], suffered from deterioration of parent-child relationship (OR = 2.004, 95% CI: 1.110–3.618, p = 0.021), thought distant teaching have bad effect (OR = 1.563, 95% CI: 1.206–2.026, p = 0.001), thought prolonged school closure have bad effect (OR = 1.417, 95% CI: 1.072–1.872, p = 0.014), had increased working intensity or time (OR = 1.372, 95% CI: 1.078–1.747, p = 0.010; OR = 1.375, 95% CI: 1.082–1.748, p = 0.009, respectively), had sleep duration/day of <6 h (OR = 1.918, 95% CI: 1.362–1.748, p < 0.001), had physical exercise duration/day of <30 min (OR = 1.875, 95% CI: 1.472–2.389, p < 0.001), spent less time with family (OR = 2.152, 95% CI: 1.397–3.315, p = 0.001), had poor mental resilience (OR = 5.953, 95% CI: 3.413–10.38, p < 0.001), or had higher PSS-10 score (OR = 7.278, 95% CI: 3.209–16.51, p < 0.001) had higher odds of suffering from depression (Table 2). Those who aged ≥41 years (OR = 0.718, 95% CI: 0.564–0.914, p = 0.007), or were concerned about COVID-19 (OR = 0.635, 95% CI: 0.466–0.867, p = 0.004) were less likely to develop depression (Table 2). In the multivariate logistic regression model, participants aged ≥41 years (OR = 0.752, 95% CI:0.578–0.979, p = 0.034), participating in epidemic prevention and control (OR = 1.413, 95% CI:1.070–1.867, p = 0.015), thinking prolonged school closure have bad effect (OR = 1.385, 95% CI:1.017–1.885, p = 0.038), sleep duration/day of <6 h (OR = 1.814, 95% CI:1.240–2.655, p < 0.001), physical exercise duration/day of <30 min (OR = 1.619, 95% CI:1.247–2.103, p < 0.001), spending less time with family (OR = 1.729, 95% CI: 1.063–2.655, p = 0.002), concerned about COVID-19 (OR = 0.609, 95% CI:0.434–0.856, p = 0.004), poor mental resilience (OR = 6.570, 95% CI:3.533–12.22, p < 0.001) and high PSS-10 score (OR = 9.058, 95% CI:3.817–21.50, p < 0.001) represented the independent factors for suffering from depression (Table 2).
Discussion
Teaching was proved to be one of the most stressful jobs, which made teachers vulnerable to depression (7, 9). The outbreak of COVID-19 had a great negative impact on daily life and mental health among teachers, resulting in increased incidence of depression. Chinese is the largest ethnic group with one-fifth of the world population and has more teachers and students than other countries. In addition, higher levels of teachers' depressive symptoms were associated with poorer student psychological distress and well-being (15). Thus, early prevention, detection and management are essential to protect teachers from depressive disorder and improve their mental health. In the present online cross-sectional survey, we found that 56.9% of teachers suffered from depression during the outbreak of COVID-19 and 16.1% suffered from moderate to severe depression, which required follow-up diagnosis and treatment (19). In this study, the depressive symptoms were significantly related to age, participating in epidemic prevention and control, parent-child relationship, opinions toward distant teaching and prolonged school closure, increased working intensity and time, sleep duration/day, physical exercise duration, spending time with family, attitude toward COVID-19, mental resilience and stress. This result maybe highly informative for stakeholders to develop intervention efforts for high-risk groups.
A study of 1,210 respondents from 194 cities in China indicated that the prevalence of moderate to severe depression in the general population was 16.5% (28), which was similar to 16.1% in our study. However, as for the overall prevalence, a cross-sectional study of 1,006 Japanese teachers indicated that the prevalence of depression was 20.1% (29). Another research reported that 49.7% (21,797/43,845) Mexican teachers suffered from depression (30). We found a higher depression prevalence of 56.9%, which means that the COVID-19 outbreak is an important risk factor of depression for teachers. The emergence of COVID-19 has parallels with the outbreak of severe acute respiratory syndrome, which killed thousands infected patients in China. As an unpleasant experience, the outbreak of COVID-19 led to mass quarantine, fears of infection, stress, anger, boredom, frustration, lack of family and finance, all of which are related to increased incidence of depression (18, 31, 32). Since the COVID-19 outbreak was no longer confined to China, the problems associated with home confinement and school closure also became concerned in other affected countries.
To prevent the spread of COVID-19, the Chinese government ordered a nationwide school closure, and public activities were discouraged. Millions of teachers were confined to their homes, resulting in decreased outdoor activities and visits to others. During the COVID-19 outbreak, home confinement and prolonged school closure might have a significant negative impact on teachers' mental health, although these measures and efforts were highly commendable and necessary. Our results also indicated that less sleep duration and physical exercise were obviously associated with higher incidence of depression, which was in line with previous studies. Physical exercise was proved to be a promising antidepressant treatment (33). And three times of light to moderate intensive exercise a week for 6 to 12 weeks could bring alleviate depressive symptoms (34). The relationship between depression and short sleep duration was reported to be bidirectional (34). Additionally, accumulating evidences suggested that short sleep duration might be a prospective predictor of depression (35).
Our results indicated that those teachers who were younger, participated in epidemic prevention and control, had deterioration in parent-child relationship, held negative thoughts of distant teaching/prolonged school closure, spent less time with family or had increased workload had higher risk of depression. These teachers faced enormous pressure due to high workload, low income, fears of infection, uncertainty about how long they will last, low familiarity with remote education and lack of family (36), all of which were source of stress, which reduces the overall physical and mental well-being of teachers and leads to unpleasant emotions, such as depression (7). This may have led to the findings.
In the present survey, teachers concerned more about the outbreak of COVID-19 had lower risk of depression. Partly because clear communication and regular and accurate updates about COVID-19 could improve relevant knowledge of the disease and reduce the sense of fear and uncertainty (16). In addition, the National Health Commission of China released the national guideline of psychological crisis intervention for COVID-19, which could help teachers have a better understand COVID-19. Future studies, focused on those counterintuitive results, are needed.
Our results found that 96.1% teachers had high perceived stress, which was in somewhat in agreement with the findings of previous studies that teaching was one of the most stressful jobs (9). In this study, 10.7% teachers had poor mental resilience. Resilience may be believed to be a measure of stress coping ability and, could be an important target of treatment in depression (22). Resilience could embody the personal qualities that help one to thrive in adversity (22). This might be the reason why those teachers with high perceived stress and poor mental resilience have high risk of depression in this study.
In this study, several limitations should be noted. First of all, this is an online study, those with no access to the Internet could not join. Secondly, some data of important factors associated with depression, such as social support and physical health, were not available due to logistical reasons. Thirdly, due to the nature of cross-sectional study, causality between variables could not be assessed. Meanwhile, this study used a snowball sampling which might influence the sample's representation and lead to sampling bias. Last but not least, this study was unable to do the comparison of the difference before and after the outbreak due to the lacking of follow-up data. Thus, a well-designed study of the prevalence of depression is necessary to complement epidemiological studies and provide more conclusive evidence regarding the risk and correlative factors of depression among teachers during the COVID-19 outbreak.
Conclusion
Depression was common among teachers during the COVID-19 outbreak. Age, participating in epidemic prevention and control, opinions toward distant teaching and prolonged school closure, sleep duration/day, physical exercise duration, spending time with family, attitude toward COVID-19, mental resilience and stress represented the independent factors for suffering from depression.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Medical Ethical Committee in Beijing Anding Hospital of the Capital Medical University, China. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
XC and JL designed the study. JZ and XY wrote the protocol, analyzed the data, and wrote the first draft of manuscript with input from HY. HH and YL commented on the protocol. All authors contributed to the article and approved the submitted version.
Funding
The study was supported by the National Key R&D Program of China (2017YFC1311100), the Beijing Municipal Science & Tech Commission (D171100007017001), the Beijing Hospitals Authority Youth Program (QML20201903), and the Beijing Hospitals Authority Clinical Medicine Development of Special Funding Support (ZYLX202128).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors are appreciative of the donors, whose names are not included in the author list but who participated in this program.
References
1. Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, et al. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Arch Gen Psychiatry. (2011) 68:90–100. doi: 10.1001/archgenpsychiatry.2010.180
2. Hirschfeld RM. The epidemiology of depression and the evolution of treatment. J Clin Psychiatry. (2012) 73(Suppl. 1):5–9. doi: 10.4088/JCP.11096su1c.01
3. Hardeveld F, Spijker J, De Graaf R, Nolen WA, Beekman AT. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand. (2010) 122:184–91. doi: 10.1111/j.1600-0447.2009.01519.x
4. Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. (2015) 76:155–62. doi: 10.4088/JCP.14m09298
5. Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the global burden of disease study 2010. Lancet. (2013) 382:1575–86. doi: 10.1016/S0140-6736(13)61611-6
6. Cuijpers P, Vogelzangs N, Twisk J, Kleiboer A, Li J, Penninx BW. Comprehensive meta-analysis of excess mortality in depression in the general community versus patients with specific illnesses. Am J Psychiatry. (2014) 171:453–62. doi: 10.1176/appi.ajp.2013.13030325
7. Desouky D, Allam H. Occupational stress, anxiety and depression among Egyptian teachers. J Epidemiol Glob Health. (2017) 7:191–8. doi: 10.1016/j.jegh.2017.06.002
8. Kaur S. Comparative study of occupational stress among teachers of private and govt. Schools in relation to their age, gender and teaching experience. Int J Educ Plan Administr. (2011) 1:151–60.
9. Johnson S, Cooper C, Cartwright S, Donald I, Taylor P, Millet C. The experience of work-related stress across occupations. J Manag Psychol. (2005) 20:178–87. doi: 10.1108/02683940510579803
10. Kidger J, Brockman R, Tilling K, Campbell R, Ford T, Araya R, et al. Teachers' wellbeing and depressive symptoms, and associated risk factors: a large cross sectional study in English secondary schools. J Affect Disord. (2016) 192:76–82. doi: 10.1016/j.jad.2015.11.054
11. Stansfeld SA, Rasul FR, Head J, Singleton N. Occupation and mental health in a national UK survey. Soc Psychiatry Psychiatr Epidemiol. (2011) 46:101–10. doi: 10.1007/s00127-009-0173-7
12. Beck A, Crain AL, Solberg LI, Unützer J, Glasgow RE, Maciosek MV, et al. Severity of depression and magnitude of productivity loss. Ann Fam Med. (2011) 9:305–11. doi: 10.1370/afm.1260
13. Jain G, Roy A, Harikrishnan V, Yu S, Dabbous O, Lawrence C. Patient-reported depression severity measured by the PHQ-9 and impact on work productivity: results from a survey of full-time employees in the United States. J Occup Environ Med. (2013) 55:252–8. doi: 10.1097/JOM.0b013e31828349c9
14. Reinke WM, Stormont M, Herman KC, Puri R, Goel N. Supporting children's mental health in schools: teacher perceptions of needs, roles, and barriers. Sch Psychol Quart. (2011) 26:1–13. doi: 10.1037/a0022714
15. Harding S, Morris R, Gunnell D, Ford T, Hollingworth W, Tilling K, et al. Is teachers' mental health and wellbeing associated with students' mental health and wellbeing? J Affect Disord. (2019) 242:180–7. doi: 10.1016/j.jad.2018.08.080
16. Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. (2020) 7:228–9. doi: 10.1016/S2215-0366(20)30046-8
17. The L. Emerging understandings of 2019-nCoV. Lancet. (2020) 395:311. doi: 10.1016/S0140-6736(20)30186-0
18. Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. (2020) 395:945–7. doi: 10.1016/S0140-6736(20)30547-X
19. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
20. Wittkampf KA, Naeije L, Schene AH, Huyser J, van Weert HC. Diagnostic accuracy of the mood module of the patient health questionnaire: a systematic review. Gen Hosp Psychiatry. (2007) 29:388–95. doi: 10.1016/j.genhosppsych.2007.06.004
21. Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. (2011) 155:529–36. doi: 10.7326/0003-4819-155-8-201110180-00009
22. Connor KM, Davidson JR. Development of a new resilience scale: the connor-davidson resilience scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
23. Fu C, Leoutsakos JM, Underwood C. An examination of resilience cross-culturally in child and adolescent survivors of the 2008 China earthquake using the connor-davidson resilience scale (CD-RISC). J Affect Disord. (2014) 155:149–53. doi: 10.1016/j.jad.2013.10.041
24. Lamond AJ, Depp CA, Allison M, Langer R, Reichstadt J, Moore DJ, et al. Measurement and predictors of resilience among community-dwelling older women. J Psychiatr Res. (2008) 43:148–54. doi: 10.1016/j.jpsychires.2008.03.007
25. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
26. Lu W, Bian Q, Wang W, Wu X, Wang Z, Zhao M. Chinese version of the perceived stress scale-10: a psychometric study in Chinese university students. PLoS ONE. (2017) 12:e0189543. doi: 10.1371/journal.pone.0189543
27. Wang Z, Chen J, Boyd JE, Zhang H, Jia X, Qiu J, et al. Psychometric properties of the Chinese version of the perceived stress scale in policewomen. PLoS ONE. (2011) 6:e28610. doi: 10.1371/journal.pone.0028610
28. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
29. Nakada A, Iwasaki S, Kanchika M, Nakao T, Deguchi Y, Konishi A, et al. Relationship between depressive symptoms and perceived individual level occupational stress among Japanese schoolteachers. Ind Health. (2016) 54:396–402. doi: 10.2486/indhealth.2015-0195
30. Soria-Saucedo R, Lopez-Ridaura R, Lajous M, Wirtz VJ. The prevalence and correlates of severe depression in a cohort of Mexican teachers. J Affect Disord. (2018) 234:109–16. doi: 10.1016/j.jad.2018.02.036
31. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
32. Wang L, Feng Z, Yang G, Yang Y, Wang K, Dai Q, et al. Depressive symptoms among children and adolescents in western china: an epidemiological survey of prevalence and correlates. Psychiatry Res. (2016) 246:267–74. doi: 10.1016/j.psychres.2016.09.050
33. Carter T, Morres ID, Meade O, Callaghan P. The effect of exercise on depressive symptoms in adolescents: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. (2016) 55:580–90. doi: 10.1016/j.jaac.2016.04.016
34. Roberts RE, Roberts CR, Duong HT. Sleepless in adolescence: prospective data on sleep deprivation, health and functioning. J Adolesc. (2009) 32:1045–57. doi: 10.1016/j.adolescence.2009.03.007
35. Roberts RE, Duong HT. The prospective association between sleep deprivation and depression among adolescents. Sleep. (2014) 37:239–44. doi: 10.5665/sleep.3388
Keywords: prevalence, factor, depression, teacher, COVID-19
Citation: Zhou J, Yuan X, Huang H, Li Y, Yu H, Chen X and Luo J (2021) The Prevalence and Correlative Factors of Depression Among Chinese Teachers During the COVID-19 Outbreak. Front. Psychiatry 12:644276. doi: 10.3389/fpsyt.2021.644276
Received: 20 December 2020; Accepted: 02 June 2021;
Published: 29 June 2021.
Edited by:
Roger C. Ho, National University of Singapore, SingaporeReviewed by:
Aurelio Olmedilla, University of Murcia, SpainLiu Sha, First Hospital of Shanxi Medical University, China
Copyright © 2021 Zhou, Yuan, Huang, Li, Yu, Chen and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xu Chen, eWludW8wMzExQDE2My5jb20=; Jia Luo, TFVPSklBXzAyMTBAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Jiaojiao Zhou†
Jiaojiao Zhou† Xu Chen
Xu Chen