- 1Department of Neuropsychiatry, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan
- 2Graduate School of Human-Environment Studies, Kyushu University, Fukuoka, Japan
- 3Karatsu Red Cross Hospital, Karatsu, Japan
- 4Department of Clinical Radiology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan
Background: Although abnormality of cerebellar-cerebral functional connectivity at rest in obsessive-compulsive disorder (OCD) has been hypothesized, only a few studies have investigated the neural mechanism. To verify the findings of previous studies, a large sample of patients with OCD was studied because OCD shows possible heterogeneity.
Methods: Forty-seven medication-free patients with OCD and 62 healthy controls (HCs) underwent resting-state functional magnetic imaging scans. Seed-based connectivity was examined to investigate differences in cerebellar-cerebral functional connectivity in OCD patients compared with HCs. Correlations between functional connectivity and the severity of obsessive-compulsive symptoms were analyzed.
Results: In OCD, we found significantly increased functional connectivity between the right lobule VI and the left precuneus, which is a component of the default mode network (DMN), compared to HCs. However, there was no correlation between the connectivity of the right lobule VI-left precuneus and obsessive-compulsive severity.
Conclusions: These findings suggest that altered functional connectivity between the cerebellum and DMN might cause changes in intrinsic large-scale brain networks related to the traits of OCD.
Introduction
Obsessive-compulsive disorder (OCD) is characterized by recurrent, intrusive, and distressing thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) that are executed to avoid anxiety or neutralize obsessions. A large number of previous neuroimaging studies have indicated that cortico-striato-thalamo-cortical (CSTC) circuit dysfunction is a pathophysiology of OCD (1, 2).
In recent years, resting-state functional connectivity (rsFC), which is defined as temporal correlations of spontaneous blood oxygen level-dependent (BOLD) signal among spatially distributed brain regions (3) at rest, has been used to analyze neural circuits in the brain. Numerous studies of rsFC have identified intrinsic large-scale brain networks defined as the default mode network (DMN), central executive network (CEN), and salience network (SN). DMN consists of three major subdivisions: the ventromedial prefrontal cortex, posterior cingulate cortex, and precuneus (4). Activities in these cortical regions are decreased during task states (5). CEN is divided into two major subdivisions, the dorsolateral prefrontal cortex and posterior parietal cortex, and activity in them is increased during a wide range of cognitively demanding tasks (6, 7). SN consists of major two regions, the dorsal anterior cingulate cortex and anterior insular cortex (6, 8). SN works on detecting, integrating, and filtering interoceptive, autonomic, and emotional information (6). In addition, SN plays a role in switching between DMN and CEN (8).
In the last decade, several studies using resting-state data demonstrated not only functional dysconnectivity within the CSTC circuit (9–13) but also abnormal functional connectivity within and among the DMN, ECN, and SN (14–18) in OCD. These studies, however, had mainly focused on the pathophysiology in the cerebrum of OCD.
Meanwhile, a large number of studies revealed that the cerebellum is involved in not only motor function but also cognitive function (19–25). In psychiatric disorders such as mood disorder, schizophrenia, and neurodevelopmental disorders, there is abundant evidence of alteration of the cerebellum (26–29). Furthermore, some neuroimaging meta-analysis studies of patients with OCD demonstrated structural and functional abnormalities in the cerebellum. Hu et al. reported greater gray matter volume in the cerebellum in adult OCD (30). Eng et al. also indicated that the gray matter volume in the cerebellum was greater and activation was reduced during a response inhibition task in patients with OCD (31). However, the precise roles of the cerebellum in OCD pathophysiology are still unknown.
Based on rs-fMRI, the subregions in the cerebellum are coupled with specific cortical networks, and rsFC was shown to mediate executive function, the default mode, and sensorimotor function in healthy subjects (32, 33). Especially, recent study revealed that the cerebellum is two times as involved the frontoparietal network as the cerebral cortex (34).
In recent years, several studies have investigated the altered cerebellar-cerebral functional connectivity in OCD. In the first study, Xu et al. compared the cerebellar-cerebral functional connectivity of 27 patients with OCD with that of 21 healthy controls (HCs) (35). They found that OCD patients showed significantly decreased cerebellar-cerebral functional connectivity in executive control and emotion processing networks. They also demonstrated a positive correlation between OCD symptom severity and functional connectivity spanning the right Crus I in the cerebellum and the inferior parietal lobule in the OCD group. Zhang et al. found decreased functional connectivity among the left Crus II, lobule VIII, and striatum and between the right lobule VII and the right striatum and cingulate in 27 medication-free OCD patients (36). Gao et al. investigated spontaneous brain activity by measuring the fractional amplitude of low-frequency fluctuations and resting-state functional connectivity in 64 medication-free OCD patients. They demonstrated that the OCD patients showed significantly increased functional connectivity between the left dorsolateral prefrontal cortex and the left cerebellum (37).
Although these studies reported alterations of cerebellar-cerebral functional connectivity in OCD, further investigation is needed to verify these results of previous studies because there are still few studies of cerebellar-cerebral functional connectivity in OCD.
For this reason, the aim of this study was to verify the alteration of cerebellar-cerebral functional connectivity in a larger number of drug-free OCD patients than previous studies.
Methods
Subjects
A total of 109 subjects, including 47 medication-free OCD patients and 62 healthy controls (HCs) matched for age and sex participated in this study. All OCD patients were recruited from the Department of Neuropsychiatry, Kyushu University Hospital, Japan. They were diagnosed primarily using the Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID) and fulfilled DSM-IV criteria. We ensured that none of them met the criteria for any current comorbid Axis I disorder and that all of them also fulfilled DSM-5 criteria for OCD. No OCD participant had taken any psychiatric medication for at least 4 weeks, and nine patients were drug-naïve. HCs were recruited from the local community, and interviewed according to the Structured Clinical Interviewed for DSM-IV non-patient Edition (SCID-NP). None of them had any psychiatric disorder. We excluded participants who had a comorbid axis I diagnosis, neurological disorder, head injury, serious medical condition, or history of drug or alcohol addiction. All of the participants completed an MRI scan, clinical assessment, and neuropsychological test within a few hours on the same day.
This study was approved by the Kyushu University Ethics Committee (No. 27-319). All participants provided written informed consent prior to study commencement.
Clinical Assessment
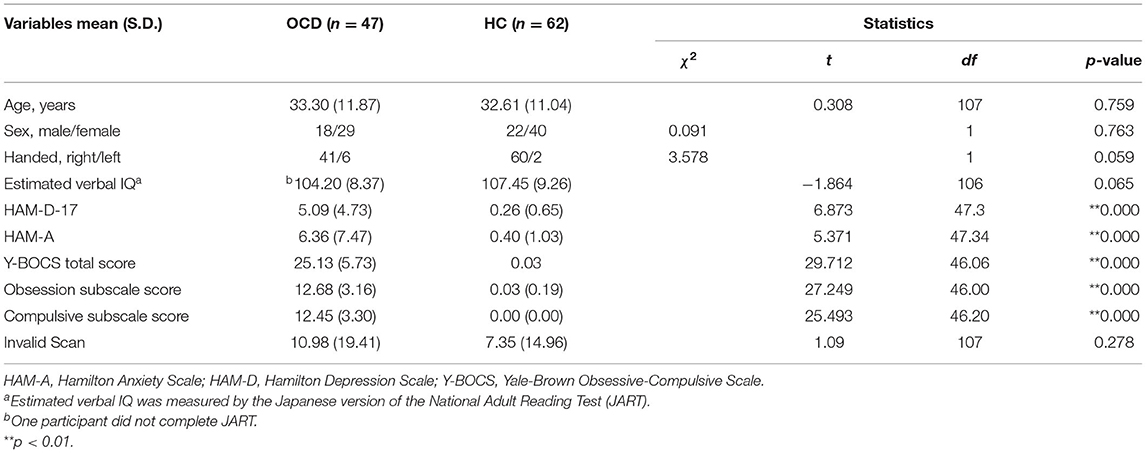
To assess the global severity of OCD symptoms, we used the Japanese version of the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) (38). The Hamilton Rating Scales for Anxiety (HAM-A) (39) and Depression (HAM-D, 17-item version) (40) were also used to quantify the degree of anxiety and depression. The Japanese version of the National Adult Reading test (JART) (41) was administered to estimate a participant's verbal intelligence quotient (IQ). We used Student's t-test and the chi-square test to compare the demographic and clinical data of the OCD and HCs groups.
Image Data Acquisition and Preprocessing
The preprocessing and processing of image data acquired in this study were described in our previous study (42). All participants underwent MRI scanning on a 3.0-Tesla MRI scanner (Achieva TX, Phillips Healthcare, Best, The Netherlands) equipped with standard phased array head coils. A T2*-weighted gradient-echo echo-planar imaging (EPI) sequence (echo time (TE), 30 ms; repetition time (TR), 2,500 ms; field of view (FOV), 212 × 212 mm; matrix, 64 × 64; slice thickness, 3.2 mm; flip angle, 80°) was acquired from each participant. After an initial 10-s dummy scan, we completed 240 real scans during a 10-min real time scan. During a resting-state fMRI scan, participants were instructed to relax with their eyes opened and watch a presented gray cross. High-resolution T1-weighted anatomical images were also acquired (TE = 3.8 ms; TR = 8.2 ms; FOV 240 × 240 mm; flip angle 8°; slice thickness, 1 mm; inversion time = 1,026 ms) after each EPI image scan. After acquisition of all image data, the arousal level during the scan of all participants was checked by the Stanford-Sleepiness Scale.
We used the CONN toolbox 17.f (http://www.nitrc.org/projects/conn) (43) running on MATLAB R2016b version 9.1.0 (MathWorks, Inc., Natick, MA, USA) on MacOS 10.12.6 to analyze functional connectivity. After discarding the first four volumes, the remaining 236 volumes were preprocessed using the CONN toolbox default spatial and temporal processing. Functional images were slice timing corrections based on the slice order, and realigned and normalized in accordance with the standard Montreal Neurological Institute (MNI) template. Six rigid-body parameters (translational and rotational) were estimated for each subject. The ART scrubbing procedure (https://www.nitrc.org/projects/artifact_detect/) was applied to exclude image artifacts due to head movement using the 97th percentile in a normative sample (with thresholds for motion = 0.9 mm and global signal z = 5). We showed invalid scans of each groups applying these thresholds (Table 1). Signal noises from the white matter and cerebrospinal fluid were discerned. Next, fMRI data were band-pass filtered at 0.008–0.09 Hz, and all functional images were smoothed using a Gaussian kernel of 6-mm full width at half-maximum. There was no significant difference between OCD and HC groups in motion parameters (max motion [t = 1.45; p = 0.149] and mean motion [t = 0.90; p = 0.368]). From anatomical image of each participants, we created white matter and cerebrospinal fluid masks in the spatial processing steps. Then BOLD signal noise from the white matter and cerebrospinal fluid (CSF) were discerned applying linear regression of white matter and CSF signal as confounding effects (43). To regress out the anatomical component-based noise, CONN toolbox has implementation of the CompCor method (44) for noise reduction along with the efficient rejection of motion and artifactual scans.
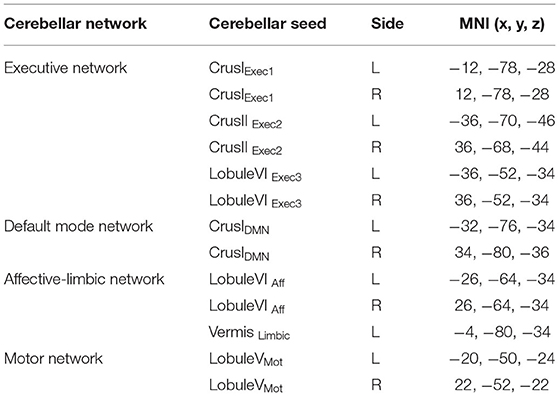
Table 1. Cerebellar seeds and coordinates grouped by network (35).
We used the spherical seed regions-of-interest (ROI) defined in a previous study (35) (Table 1), referring to the findings of healthy subjects (32, 33). Each ROI was created in each hemisphere as a 6 mm radius sphere.
Following the preprocessing steps, the blood-oxygen-level-dependent (BOLD) signal time series correlation was calculated between each pair of sources for each participant across the resting-state time series, and then a Fisher z transformation was applied. Seed-based connectivity maps were generated from each seed ROI for each participant.
We investigated the difference in functional connectivity from seed ROIs to whole brain voxels between the OCD and HC groups by using a two-sample t-test. The significance level was set at the individual voxel p < 0.001, and a cluster-size threshold of p < 0.05 false discovery rate (FDR) corrected. Then, we conducted a correlation analysis between the abnormal functional connectivity from group-level comparison and the Y-BOCS total score, obsession score, and compulsive score within the OCD group.
Results
Demographic and Clinical Characteristics
Table 2 shows the demographic characteristics of the OCD group and HCs. Both groups were well-matched for age, sex, and handedness. The mean total Y-BOCS score in the OCD group was 25.13 (S.D.= 5.73). The mean HAM-D-17 and HAM-A scores were significantly higher in the OCD group than in the HCs (p < 0.001).
Cerebellar-Cerebellum Functional Connectivity in OCD Group Relative to HCs
The OCD group showed significantly increased functional connectivity only between the right lobule VIexect3 and the left precuneus [peak MINI coordinate (−2, 60, 20), p-FDR:0.005277, cluster size: 195 voxels] (Figure 1). It, however, was not significant difference with Bonferroni correction (p-FDR < 0.0038) for adjusting 13 seeds ROIs. No decreased functional connectivity was found in the OCD group compared with HCs. There were no correlations were found between this functional connectivity from the right lobule VIexact3 to left precuneus and the Y-BOCS total score (r = 0.11) (Figure 2), obsession (r = 0.20) score, or compulsion (r = −0.014) score within the OCD group (Supplementary Figure 1). For supplemental analysis, within OCD group, we conducted voxel-wise regression analysis from right LobuleVIexact3 related to Y-BOCS total scores, while controlling for age and gender (statistical significance was set at a voxel height threshold of p < 0.001, and a cluster-size threshold of p < 0.05 FDR corrected). Though, there was no brain area that survive statistical significance.
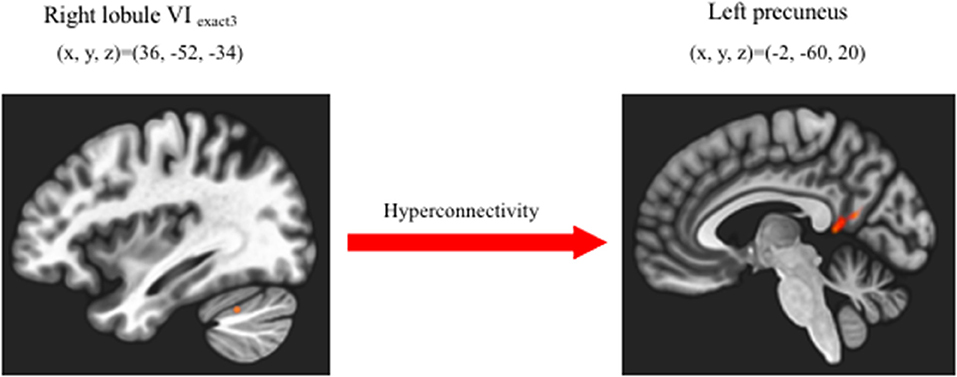
Figure 1. Increased cerebellar-cerebral functional connectivity in OCD group compared with HC group. Patients with OCD showed significantly increased functional connectivity between right lobuleVIexect3 and left precuneus than HC (cluster size corrected significance p < 0.05 FDR, after applying a per-voxel height threshold of p < 0.001).
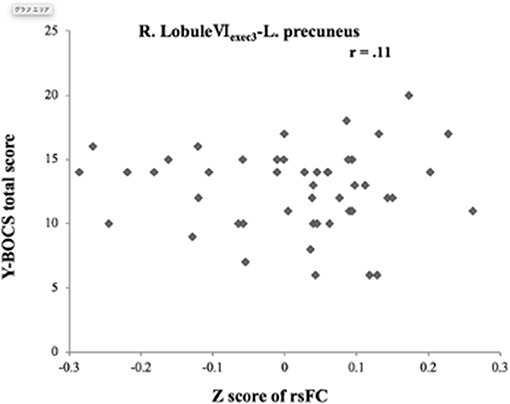
Figure 2. Correlation between altered functional connectivity with severity of obsessive-compulsive symptoms. There was no correlation of increased right lobule VIexec3-left precuneus connectivity with the Y-BOCS total score. L, left; R, right; rsFC, resting-state functional connectivity; Y-BOCS, Yale Brown Obsessive-Compulsive Scale.
Discussion
This study showed an increased rsFC between the right lobule VIexact3 and left precuneus in OCD patients compared with HCs. There was no correlation between this rsFC and obsessive-compulsive symptom severity. Our findings were different from the results of previous studies that reported hypo- or hyper-connectivity between Crus I and DMN in OCD (35, 45). However, this study had the advantages of a larger number of subjects and more seeds in the cerebellum than previous studies.
Previous studies showed that there were some intrinsic connectivity networks not only DMN, CEN but also visual, somatomotor, attention, limbic networks in the cerebrum (46) and the precuneus participated in paralimbic networks which include subsystems of the DMN (47). We, however, proceed with the discussion based on triple network model hypothesis which was proposed by Menon (48). The precuneus is mapped to the medial parietal cortex and associated with higher-order cognitive processes such as visio-spatial imagery, episodic memory retrieval, and self-processing operations (49). Moreover, the precuneus is one of the brain regions involving the DMN (50–52) which has rsFC with Crus I, Crus II, and Lobule IX in HC (32, 53, 54). Numerous studies revealed alterations of the rsFC within or between the DMN, CEN, and SN in several psychiatric disorders such as schizophrenia, major depressive disorder, and autism (55–60). Menon proposed a triple network model in which a deficit in engagement and disengagement of these core neurocognitive networks play a role in psychiatric disorders (48). In a meta-analysis study of rsFC in OCD, Gürsel et al. demonstrated consistent hypoconnectivity within the DMN, CEN, and SN and general dysconnectivity within the DMN and frontoparietal network, which is involved in CEN, as well as between the frontoparietal lobe, DMN, and SN (60). Therefore, they concluded that the pathological interplay within and between network alterations could underlie core OCD symptoms (60).
Our findings suggest that the aberrant rsFCs might occur not only in the cerebral regions but also in the cerebello-cerebral region in OCD. Patients with OCD have executive dysfunctions, such as working memory, cognitive flexibility, and response inhibition (61, 62). The deactivation of DMN that is associated with these cognitive performances usually occurs when an individual is required to focus attention on an external stimulus in HC (63–65). However, OCD patients have decreased DMN homogeneity (18) in resting conditions and difficulties with deactivation of DMN in non-resting conditions (17). Therefore, we supposed that the increased rsFC between lobule VI, which has resting functional connectivity to the CEN, and the precuneus might relate to interference with the function of DMN and involve the cognitive dysfunction in OCD (Figure 3).
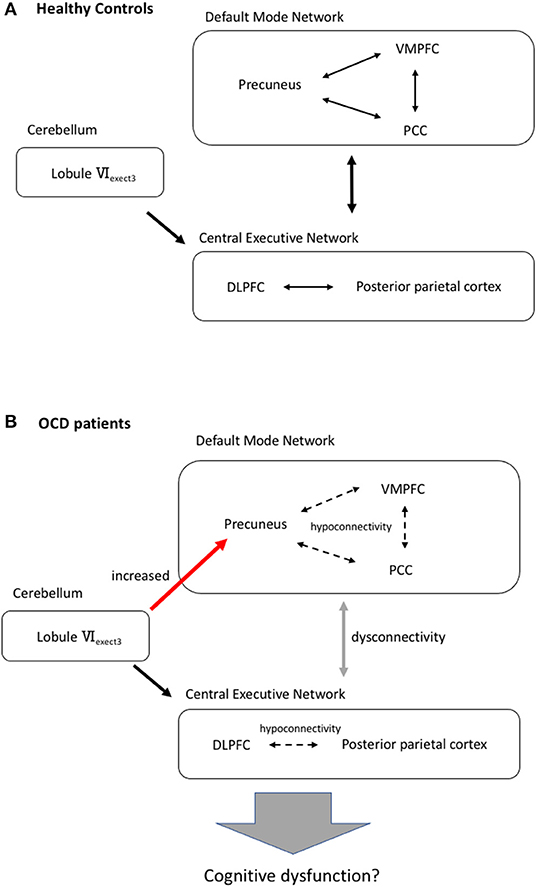
Figure 3. Our hypothesis of aberrant cerebellar-cerebral resting state functional network and cognitive dysfunction of OCD. (A) In HC, there is a resting functional connectivity between the lobuleVIexect3 and the central executive network. The allow indicates functional connectivity. DLPFC, dorsolateral prefrontal cortex; PCC, posterior cingulate cortex; VMPFC, ventromedial prefrontal cortex. (B) Cognitive dysfunction in OCD patients might be associated with increased functional connectivity from lobuleVIexect3 to the precuneus, hypoconnectivities in the default mode network and the central executive network and dysconnectivity between these large-scale intrinsic brain networks (60). Dashed line arrow means hypoconnectivity. Red arrow indicates increased connectivity.
We did not find a correlation between the functional connectivity of the right lobule VIexact3–left precuneus and the severity of obsessive-compulsive symptoms measured by Y-BOCS. This result means that the aberrant rsFC between the cerebellum and DMN is not associated directly with the obsessive-compulsive symptoms. DMN relates to response inhibition (66, 67), planning (68), and decision-making (69), which are trait markers for OCD (70). Our results, therefore, might show that this aberrant rsFC is not a state but a trait of OCD patients.
There are several reasons for the differences in the results between the previous study and the current study. First, OCD has heterogeneity (71). It, therefore, has been pointed out that replication of the findings has been variable (71). Second, functional organization of the cerebellum is individual specific (34). Marek et al. (34) revealed that there were differences across individuals from the group average in terms of relative amount of cerebellum associated with each intrinsic cerebral network. Third, there is methodological difference in imaging data analysis between the previous study and current study. We used CONN toolbox (43) which was commonly used in many previous studies, though previous study which was conducted Xu et al. (35) used the Data Processing & Analysis for Brain Imaging (72). We do not think that either of these two methods of analysis is better than the other.
There are several limitations in this study. First, we did not investigate the correlation between aspects of the neuropsychological performance such as response inhibition and aberrant rsFC in the OCD group. Therefore, we could not verify our suggestion that altered cerebellar-cerebral connectivity might relate to the cognitive dysfunction and be a trait of OCD. Second, we did not consider other aspects of OCD heterogeneity, such as the age at onset, duration of the illness, and OCD dimensional symptoms. Future studies with neuropsychological tests and more comprehensive clinical data would validate our study. Third, we had not used the newest validated seed regions which Seitzman et al. (73) had revealed. We, however, use the seed regions which were used in the previous study (35) since the aim of this study was to verify that study. In the future, it is necessary to conduct new analysis using the newest seed regions.
Conclusion
In conclusion, we found increased functional connectivity between lobule VI and the precuneus at rest in medication-free patients with OCD. There was no correlation between the functional connectivity and severity of obsessive-compulsive symptoms. These findings suggest that aberrant resting state cerebellar-cerebral functional connectivity might be associated with executive dysfunction in OCD patients and be a trait of OCD.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by Kyushu University Ethics Committee. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
KM designed the study, collected data, and wrote the initial draft of the manuscript. HT collected data, designed the study, and critically reviewed the manuscript. ST, AO, and MK contributed to analysis and interpretation of data. SH, TM, KK, OT, and AH contributed to data collection. TN critically reviewed the manuscript. All authors approved the final version of the manuscript.
Funding
This work was supported by JSPS KAKENHI Grant Number JP16H06280, JP16K10253, and JP19K08076.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.659616/full#supplementary-material
References
1. Menzies L, Chamberlain SR, Laird AR, Thelen SM, Sahakian BJ, Bullmore ET. Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: the orbitofronto-striatal model revisited. Neurosci Biobehav Rev. (2008) 32:525–49. doi: 10.1016/j.neubiorev.2007.09.005
2. Pauls DL, Abramovitch A, Rauch SL, Geller DA. Obsessive-compulsive disorder: an integrative genetic and neurobiological perspective. Nat Rev Neurosci. (2014) 15:410–24. doi: 10.1038/nrn3746
3. Woodward ND, Cascio CJ. Resting-state functional connectivity in psychiatric disorders. JAMA Psychiatry. (2015) 72:743–4. doi: 10.1001/jamapsychiatry.2015.0484
4. Greicius MD, Krasnow B, Reiss AL, Menon V. Functional connectivity in the resting brain: a network analysis of the default mode hypothesis. Proc Natl Acad Sci USA. (2003) 100:253–8. doi: 10.1073/pnas.0135058100
5. Raichle ME. The brain's default mode network. Ann Rev Neurosci. (2015) 38:433–47. doi: 10.1146/annurev-neuro-071013-014030
6. Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, et al. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. (2007) 27:2349–56. doi: 10.1523/JNEUROSCI.5587-06.2007
7. Fox MD, Snyder AZ, Vincent JL, Corbetta M, Van Essen DC, Raichle ME. The human brain is intrinsically organized into dynamic, anticorrelated functional networks. Proc Natl Acad Sci USA. (2005) 102:9673–8. doi: 10.1073/pnas.0504136102
8. Sridharan D, Levitin DJ, Menon V. A critical role for the right fronto-insular cortex in switching between central-executive and default-mode networks. Proc Natl Acad Sci USA. (2008) 105:12569–74. doi: 10.1073/pnas.0800005105
9. Harrison BJ, Soriano-Mas C, Pujol J, Ortiz H, Lopez-Sola M, Hernandez-Ribas R, et al. Altered corticostriatal functional connectivity in obsessive-compulsive disorder. Arch Gen Psychiatry. (2009) 66:1189–200. doi: 10.1001/archgenpsychiatry.2009.152
10. Harrison BJ, Pujol J, Cardoner N, Deus J, Alonso P, Lopez-Sola M, et al. Brain corticostriatal systems and the major clinical symptom dimensions of obsessive-compulsive disorder. Biol Psychiatry. (2013) 73:321–8. doi: 10.1016/j.biopsych.2012.10.006
11. Fitzgerald KD, Stern ER, Angstadt M, Nicholson-Muth KC, Maynor MR, Welsh RC, et al. Altered function and connectivity of the medial frontal cortex in pediatric obsessive-compulsive disorder. Biol Psychiatry. (2010) 68:1039–47. doi: 10.1016/j.biopsych.2010.08.018
12. Jang JH, Kim JH, Jung WH, Choi JS, Jung MH, Lee JM, et al. Functional connectivity in fronto-subcortical circuitry during the resting state in obsessive-compulsive disorder. Neurosci Lett. (2010) 474:158–62. doi: 10.1016/j.neulet.2010.03.031
13. Sakai Y, Narumoto J, Nishida S, Nakamae T, Yamada K, Nishimura T, et al. Corticostriatal functional connectivity in non-medicated patients with obsessive-compulsive disorder. Eur Psychiatry. (2011) 26:463–9. doi: 10.1016/j.eurpsy.2010.09.005
14. Fan J, Zhong M, Gan J, Liu W, Niu C, Liao H, et al. Altered connectivity within and between the default mode, central executive, and salience networks in obsessive-compulsive disorder. J Affect Disord. (2017) 223:106–14. doi: 10.1016/j.jad.2017.07.041
15. Chen Y, Meng X, Hu Q, Cui H, Ding Y, Kang L, et al. Altered resting-state functional organization within the central executive network in obsessive-compulsive disorder. Psychiatry Clin Neurosci. (2016) 70:448–56. doi: 10.1111/pcn.12419
16. Peng ZW, Xu T, He QH, Shi CZ, Wei Z, Miao GD, et al. Default network connectivity as a vulnerability marker for obsessive compulsive disorder. Psychol Med. (2014) 44:1475–84. doi: 10.1017/S0033291713002250
17. Goncalves OF Soares JM Carvalho S Leite J Ganho-Avila A Fernandes-Goncalves A . Patterns of default mode network deactivation in obsessive compulsive disorder. Sci Rep. (2017) 7:44468. doi: 10.1038/srep44468
18. Chen Y, Ou Y, Lv D, Yang R, Li S, Jia C, et al. Altered network homogeneity of the default-mode network in drug-naive obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry. (2019) 93:77–83. doi: 10.1016/j.pnpbp.2019.03.008
19. Buckner RL. The cerebellum and cognitive function: 25 years of insight from anatomy and neuroimaging. Neuron. (2013) 80:807–15. doi: 10.1016/j.neuron.2013.10.044
20. Strick PL, Dum RP, Fiez JA. Cerebellum and nonmotor function. Ann Rev Neurosci. (2009) 32:413–34. doi: 10.1146/annurev.neuro.31.060407.125606
21. Steinlin M. The cerebellum in cognitive processes: supporting studies in children. Cerebellum. (2007) 6:237–41. doi: 10.1080/14734220701344507
22. Schmahmann JD. The cerebellum and cognition. Neurosci Lett. (2019) 688:62–75. doi: 10.1016/j.neulet.2018.07.005
23. Stoodley CJ. The cerebellum and cognition: evidence from functional imaging studies. Cerebellum. (2012) 11:352–65. doi: 10.1007/s12311-011-0260-7
24. Guell X, Gabrieli JDE, Schmahmann JD. Triple representation of language, working memory, social and emotion processing in the cerebellum: convergent evidence from task and seed-based resting-state fMRI analyses in a single large cohort. Neuroimage. (2018) 172:437–49. doi: 10.1016/j.neuroimage.2018.01.082
25. Brissenden JA, Levin EJ, Osher DE, Halko MA, Somers DC. Functional evidence for a cerebellar node of the dorsal attention network. J Neurosci. (2016) 36:6083–96. doi: 10.1523/JNEUROSCI.0344-16.2016
26. Lupo M, Siciliano L, Leggio M. From cerebellar alterations to mood disorders: a systematic review. Neurosci Biobehav Rev. (2019) 103:21–8. doi: 10.1016/j.neubiorev.2019.06.008
27. Lungu O, Barakat M, Laventure S, Debas K, Proulx S, Luck D, et al. The incidence and nature of cerebellar findings in schizophrenia: a quantitative review of fMRI literature. Schizophr Bull. (2013) 39:797–806. doi: 10.1093/schbul/sbr193
28. Sathyanesan A, Zhou J, Scafidi J, Heck DH, Sillitoe RV, Gallo V. Emerging connections between cerebellar development, behaviour and complex brain disorders. Nat Rev Neurosci. (2019) 20:298–313. doi: 10.1038/s41583-019-0152-2
29. Moberget T, Doan NT, Alnaes D, Kaufmann T, Cordova-Palomera A, Lagerberg TV, et al. Cerebellar volume and cerebellocerebral structural covariance in schizophrenia: a multisite mega-analysis of 983 patients and 1349 healthy controls. Mol Psychiatry. (2018) 23:1512–20. doi: 10.1038/mp.2017.106
30. Hu X, Du M, Chen L, Li L, Zhou M, Zhang L, et al. Meta-analytic investigations of common and distinct grey matter alterations in youths and adults with obsessive-compulsive disorder. Neurosci Biobehav Rev. (2017) 78:91–103. doi: 10.1016/j.neubiorev.2017.04.012
31. Eng GK, Sim K, Chen SH. Meta-analytic investigations of structural grey matter, executive domain-related functional activations, and white matter diffusivity in obsessive compulsive disorder: an integrative review. Neurosci Biobehav Rev. (2015) 52:233–57. doi: 10.1016/j.neubiorev.2015.03.002
32. Habas C, Kamdar N, Nguyen D, Prater K, Beckmann CF, Menon V, et al. Distinct cerebellar contributions to intrinsic connectivity networks. J Neurosci. (2009) 29:8586–94. doi: 10.1523/JNEUROSCI.1868-09.2009
33. Krienen FM, Buckner RL. Segregated fronto-cerebellar circuits revealed by intrinsic functional connectivity. Cerebral Cortex. (2009) 19:2485–97. doi: 10.1093/cercor/bhp135
34. Marek S, Siegel JS, Gordon EM, Raut RV, Gratton C, Newbold DJ, et al. Spatial and temporal organization of the individual human cerebellum. Neuron. (2018) 100:977–93 e7. doi: 10.1016/j.neuron.2018.10.010
35. Xu T, Zhao Q, Wang P, Fan Q, Chen J, Zhang H, et al. Altered resting-state cerebellar-cerebral functional connectivity in obsessive-compulsive disorder. Psychol Med. (2019) 49:1156–65. doi: 10.1017/S0033291718001915
36. Zhang H, Wang B, Li K, Wang X, Li X, Zhu J, et al. Altered functional connectivity between the cerebellum and the cortico-striato-thalamo-cortical circuit in obsessive-compulsive disorder. Front Psychiatry. (2019) 10:522. doi: 10.3389/fpsyt.2019.00522
37. Gao J, Zhou Y, Yang X, Luo J, Meng F, Zheng D, et al. Abnormalities within and beyond the cortico-striato-thalamo-cortical circuitry in medication-free patients with OCD revealed by the fractional amplitude of low-frequency fluctuations and resting-state functional connectivity. Neurosci Lett. (2019) 712:134449. doi: 10.1016/j.neulet.2019.134449
38. Nakajima T, Nakamura M, Taga C, Yamagami S, Kiriike N, Nagata T, et al. Reliability and validity of the Japanese version of the yale-brown obsessive-compulsive scale. Psychiatry Clin Neurosci. (1995) 49:121–6. doi: 10.1111/j.1440-1819.1995.tb01875.x
39. Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. (1959) 32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x
40. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. (1960) 23:56–62. doi: 10.1136/jnnp.23.1.56
41. Matsuoka K, Uno M, Kasai K, Koyama K, Kim Y. Estimation of premorbid IQ in individuals with Alzheimer's disease using Japanese ideographic script (Kanji) compound words: Japanese version of National Adult Reading Test. Psychiatry Clin Neurosci. (2006) 60:332–9. doi: 10.1111/j.1440-1819.2006.01510.x
42. Tomiyama H, Nakao T, Murayama K, Nemoto K, Ikari K, Yamada S, et al. Dysfunction between dorsal caudate and salience network associated with impaired cognitive flexibility in obsessive-compulsive disorder: a resting-state fMRI study. Neuroimage Clin. (2019) 24:102004. doi: 10.1016/j.nicl.2019.102004
43. Whitfield-Gabrieli S, Nieto-Castanon A. Conn: a functional connectivity toolbox for correlated and anticorrelated brain networks. Brain Connect. (2012) 2:125–41. doi: 10.1089/brain.2012.0073
44. Behzadi Y, Restom K, Liau J, Liu TT. A component based noise correction method (CompCor) for BOLD and perfusion based fMRI. Neuroimage. (2007) 37:90–101. doi: 10.1016/j.neuroimage.2007.04.042
45. Lv D, Ou Y, Chen Y, Yang R, Zhong Z, Jia C, et al. Increased cerebellar-default-mode network connectivity at rest in obsessive-compulsive disorder. Eur Arch Psychiatry Clin Neurosci. (2019) 270:1015–24. doi: 10.1007/s00406-019-01070-5
46. Yeo BT, Krienen FM, Sepulcre J, Sabuncu MR, Lashkari D, Hollinshead M, et al. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J Neurophysiol. (2011) 106:1125–65. doi: 10.1152/jn.00338.2011
47. Yeo BT, Krienen FM, Chee MW, Buckner RL. Estimates of segregation and overlap of functional connectivity networks in the human cerebral cortex. Neuroimage. (2014) 88:212–27. doi: 10.1016/j.neuroimage.2013.10.046
48. Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. (2011) 15:483–506. doi: 10.1016/j.tics.2011.08.003
49. Cavanna AE, Trimble MR. The precuneus: a review of its functional anatomy and behavioural correlates. Brain. (2006) 129:564–83. doi: 10.1093/brain/awl004
50. Fransson P, Marrelec G. The precuneus/posterior cingulate cortex plays a pivotal role in the default mode network: evidence from a partial correlation network analysis. Neuroimage. (2008) 42:1178–84. doi: 10.1016/j.neuroimage.2008.05.059
51. Hagmann P, Cammoun L, Gigandet X, Meuli R, Honey CJ, Wedeen VJ, et al. Mapping the structural core of human cerebral cortex. PLoS Biol. (2008) 6:e159. doi: 10.1371/journal.pbio.0060159
52. Utevsky AV, Smith DV, Huettel SA. Precuneus is a functional core of the default-mode network. J Neurosci. (2014) 34:932–40. doi: 10.1523/JNEUROSCI.4227-13.2014
53. Buckner RL, Krienen FM, Castellanos A, Diaz JC, Yeo BT. The organization of the human cerebellum estimated by intrinsic functional connectivity. J Neurophysiol. (2011) 106:2322–45. doi: 10.1152/jn.00339.2011
54. O'Reilly JX, Beckmann CF, Tomassini V, Ramnani N, Johansen-Berg H. Distinct and overlapping functional zones in the cerebellum defined by resting state functional connectivity. Cerebral Cortex. (2010) 20:953–65. doi: 10.1093/cercor/bhp157
55. Kaiser RH, Andrews-Hanna JR, Wager TD, Pizzagalli DA. Large-scale network dysfunction in major depressive disorder: a meta-analysis of resting-state functional connectivity. JAMA Psychiatry. (2015) 72:603–11. doi: 10.1001/jamapsychiatry.2015.0071
56. Mulders PC, van Eijndhoven PF, Schene AH, Beckmann CF, Tendolkar I. Resting-state functional connectivity in major depressive disorder: a review. Neurosci Biobehav Rev. (2015) 56:330–44. doi: 10.1016/j.neubiorev.2015.07.014
57. Hu ML, Zong XF, Mann JJ, Zheng JJ, Liao YH, Li ZC, et al. A review of the functional and anatomical default mode network in schizophrenia. Neurosci Bull. (2017) 33:73–84. doi: 10.1007/s12264-016-0090-1
58. Kim YK, Yoon HK. Common and distinct brain networks underlying panic and social anxiety disorders. Prog Neuropsychopharmacol Biol Psychiatry. (2018) 80:115–22. doi: 10.1016/j.pnpbp.2017.06.017
59. Padmanabhan A, Lynch CJ, Schaer M, Menon V. The default mode network in autism. Biol Psychiatry Cogn Neurosci Neuroimaging. (2017) 2:476–86. doi: 10.1016/j.bpsc.2017.04.004
60. Gürsel DA, Avram M, Sorg C, Brandl F, Koch K. Frontoparietal areas link impairments of large-scale intrinsic brain networks with aberrant fronto-striatal interactions in OCD: a meta-analysis of resting-state functional connectivity. Neurosci Biobehav Rev. (2018) 87:151–60. doi: 10.1016/j.neubiorev.2018.01.016
61. Marzuki AA, Pereira de Souza A, Sahakian BJ, Robbins TW. Are candidate neurocognitive endophenotypes of OCD present in paediatric patients? A systematic review. Neurosci Biobehav Rev. (2020) 108:617–45. doi: 10.1016/j.neubiorev.2019.12.010
62. Abramovitch A, Abramowitz JS, Mittelman A. The neuropsychology of adult obsessive-compulsive disorder: a meta-analysis. Clin Psychol Rev. (2013) 33:1163–71. doi: 10.1016/j.cpr.2013.09.004
63. Mayer JS, Roebroeck A, Maurer K, Linden DE. Specialization in the default mode: task-induced brain deactivations dissociate between visual working memory and attention. Hum Brain Mapp. (2010) 31:126–39. doi: 10.1002/hbm.20850
64. Singh KD, Fawcett IP. Transient and linearly graded deactivation of the human default-mode network by a visual detection task. Neuroimage. (2008) 41:100–12. doi: 10.1016/j.neuroimage.2008.01.051
65. Uddin LQ, Kelly AM, Biswal BB, Castellanos FX, Milham MP. Functional connectivity of default mode network components: correlation, anticorrelation, and causality. Hum Brain Mapp. (2009) 30:625–37. doi: 10.1002/hbm.20531
66. Zhang S, Li CS. Functional networks for cognitive control in a stop signal task: independent component analysis. Hum Brain Mapp. (2012) 33:89–104. doi: 10.1002/hbm.21197
67. Tian L, Ren J, Zang Y. Regional homogeneity of resting state fMRI signals predicts stop signal task performance. Neuroimage. (2012) 60:539–44. doi: 10.1016/j.neuroimage.2011.11.098
68. Vriend C, Wagenmakers MJ, van den Heuvel OA, van der Werf YD. Resting-state network topology and planning ability in healthy adults. Brain Struct Funct. (2020) 225:365–74. doi: 10.1007/s00429-019-02004-6
69. Bolt T, Laurienti PJ, Lyday R, Morgan A, Dagenbach D. Graph-theoretical study of functional changes associated with the iowa gambling task. Front Hum Neurosci. (2016) 10:314. doi: 10.3389/fnhum.2016.00314
70. Bora E. Meta-analysis of neurocognitive deficits in unaffected relatives of obsessive-compulsive disorder (OCD): comparison with healthy controls and patients with OCD. Psychol Med. (2020) 50:1257–66. doi: 10.1017/S0033291720001634
71. Stein DJ, Costa DLC, Lochner C, Miguel EC, Reddy YCJ, Shavitt RG, et al. Obsessive-compulsive disorder. Nat Rev Dis Primers. (2019) 5:52. doi: 10.1038/s41572-019-0102-3
72. Yan CG, Wang XD, Zuo XN, Zang YF. DPABI: data processing & analysis for (resting-state) brain imaging. Neuroinformatics. (2016) 14:339–51. doi: 10.1007/s12021-016-9299-4
Keywords: obsessive-compulsive disorder, cerebellum, functional connectivity, default-mode network, precuneus
Citation: Murayama K, Tomiyama H, Tsuruta S, Ohono A, Kang M, Hasuzawa S, Mizobe T, Kato K, Togao O, Hiwatashi A and Nakao T (2021) Aberrant Resting-State Cerebellar-Cerebral Functional Connectivity in Unmedicated Patients With Obsessive-Compulsive Disorder. Front. Psychiatry 12:659616. doi: 10.3389/fpsyt.2021.659616
Received: 27 January 2021; Accepted: 29 March 2021;
Published: 23 April 2021.
Edited by:
Odile Van Den Heuvel, VU University Medical Center, NetherlandsReviewed by:
Anders Lillevik Thorsen, Haukeland University Hospital, NorwayGuido van Wingen, University of Amsterdam, Netherlands
Copyright © 2021 Murayama, Tomiyama, Tsuruta, Ohono, Kang, Hasuzawa, Mizobe, Kato, Togao, Hiwatashi and Nakao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Keitaro Murayama, bXVyYXlhbWEua2VpdGFyby4wMDNAbS5reXVzaHUtdS5hYy5qcA==
 Keitaro Murayama
Keitaro Murayama Hirofumi Tomiyama1
Hirofumi Tomiyama1 Akio Hiwatashi
Akio Hiwatashi