- 1The Fourth Clinical Medical College of Guangzhou University of Chinese Medicine, Shenzhen, China
- 2Institute of Biomedical and Health Engineering, Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen, China
- 3Acupuncture Department, Shenzhen Traditional Chinese Medicine Hospital, Shenzhen, China
- 4CAS Key Laboratory of Human-Machine Intelligence-Synergy Systems, Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen, China
- 5School of Artificial Intelligence, University of Chinese Academy of Sciences, Beijing, China
Accumulating studies had been performed using magnetic resonance imaging (MRI) to understand the neural mechanism of acupuncture therapy for depression. However, inconsistencies remain due to differences in research designs and MRI analytical methods. Therefore, we aim to summarize the current MRI research and provide useful information for further research by identifying papers published in English and Chinese about MRI studies on acupuncture for depression up to November 2020. A total of 22 studies met the inclusion criteria, including 810 depression patients and 416 health controls (HCs). The applied designs of these studies are mainly random control trial and pre–post designs. The MRI analytical methods are mainly (fractional) amplitude of low-frequency fluctuation (fALFF/ALFF) and functional connectivity (FC), whereas a small subset of studies used voxel-based morphometry (VBM) and diffusion tensor imaging (DTI). The most consistent functional MRI (fMRI) results showed increased N-acetylaspartate/creatine (NAA/Cr) ratios, increased ALFF in the right precuneus, decreased ALFF in the inferior frontal gyrus (IFG), and increased FC of the anterior cingulate cortex (ACC). In contrast, no significant neurological changes were identified in any of the DTI or VBM studies. However, clear, reliable conclusions cannot be drawn due to the use of different designs, analytical methods, seed points selected, types of depression, acupuncture points, and so on. Improved report specifications, well-designed studies, consistent analytical methods, and larger sample sizes will enable the field to better elucidate the underlying mechanisms of acupuncture in depressed patients.
Introduction
Depression is a common mental illness, which has been recognized as a major public health problem that has a substantial impact on an individual's ability to function within daily and societal environments (1). Depressed patients may lose interest in physical activity; lose their appetite or overeat; have difficulty concentrating, remembering details, or making decisions; and more seriously may attempt suicide or commit suicide (2). In various studies, the rate of depression or depressive symptoms among students varied from 1.4 to 73.5% (3, 4), and those with suicidal ideation varied from 4.9 to 35.6% (5, 6). Major depressive disorder (MDD) is the most common and severe mental disorder with a lifetime prevalence of 6–15% (7, 8).
Antidepressant medication may be provided as an initial primary treatment for MDD, but they are far from satisfactory due to undesirable side effects and a delay in the onset of therapeutic action (9–11). Faced with limitations of conventional treatments, patients suffering from depression often seek alternative forms of treatment, such as acupuncture therapy (12), one of the world's oldest recognized medical treatments, which has been used to relieve pain and treat mental illness (13, 14) for 1,000's of years. Indeed, several systematic reviews (1, 15, 16) have shown that a single acupuncture therapy session or combination of acupuncture with a suitable adjunct was significantly effective in reducing the severity of depression. In traditional Chinese medicine (TCM) theory, the pathogenesis of depression is the stagnation of liver qi, and acupuncture can regulate qi and mental state. Experimental studies indicated that most of the action of antidepressant effects of acupuncture is mediated via the central nervous system (17). Moreover, an increasing number of animal experiment researches identified that the effective mechanism of acupuncture for depression may be through regulation of the hypothalamic–pituitary–adrenal axis (18, 19), neurotransmitter (20–22), anti-inflammatory (23–25), and signaling pathways (26–29).
However, as we all know, humans are complex animals, and the mechanism of acupuncture in treating depression may be different between animal and human studies. Therefore, it is very necessary to investigate the effects of acupuncture on depression at the human brain level. In recent years, magnetic resonance imaging (MRI), due to its minimal invasiveness, lack of radiation exposure, excellent spatial resolution, and relatively wide availability, has been widely used to quantify how acupuncture affects the function and structure of brain regions as well as brain networks (30). Therefore, it is possible for us to explore changes in brain structure, function, and metabolism about acupuncture for depression. Importantly, with the increase of research in this area, the central mechanism of acupuncture's effect on depression is becoming more and more clear. However, there are few reviews of MRI studies on acupuncture for depression. It is necessary to understand the current state of research for better exploration in the future.
Therefore, with our review, we aim to provide a systematic overview of the existing evidence regarding changes in brain structure, function, and metabolism underlying the effects of acupuncture therapy on depression by summarizing the characteristics, methods, and conclusions of relevant MRI research. A meta-analysis was further performed to identify the most reliable results.
Materials and Methods
Search Strategy and Study Selection
We conducted our systematic review in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline (31). We searched the following four electronic databases for clinical MRI research on acupuncture therapy for depression: PubMed, Wanfang, VIP information database, and China National Knowledge Infrastructure (CNKI) up to October 20, 2020. The keywords were as follows: (1) acupuncture therapy, acupuncture, acupuncture point, body acupuncture, auricular acupuncture, electroacupuncture, moxibustion; (2) depression, depressive disorder, major depression disorder; and (3) MRI, magnetic resonance imaging, resting state, fMRI, rs-fMRI, functional connectivity, task fMRI, BOLD, blood oxygen level-dependent, ReHo, ALFF, fALFF, voxel-based analysis, VBM, voxel-based morphometry, Freesurfer, surface based morphometry, cortical thickness, surface area, cortical volume, gray matter volume, gray matter density, GMV, DTI, diffusion tensor imaging, white matter, fractional anisotropy, mean diffusivity, magnetic resonance spectroscopy.
Studies that met the following criteria were included: (1) prospective observational/randomized study; (2) patients with some specific depressive disorder symptoms such as anhedonia (diminished ability to experience pleasure), diurnal variation (i.e., symptoms of depression are worse during certain periods of waking hours), and intensified guilt about being ill (32) and met established diagnostic criteria of depression, including the Diagnostic and Statistical Manual of Mental Disorders (DSM) (32), the International Classification of Diseases (ICD) (33), and the Chinese Classification of Mental Disorders (CCMD) (34); (3) the scores of Hamilton Depression Scale (HAMD-17) ≥17 or HAMD-24 ≥20 or standard score of Self-Rating Depression Scale (SDS) ≥53 or total score of Montgomery–Åsberg Depression Rating Scale (MADRS) ≥14; (4) intervention using acupuncture, electroacupuncture (EA), or laser acupuncture (LA); and (5) outcome indicators of brain response assessed using functional MRI (fMRI) or structural MRI (sMRI), and analytical methods are not restricted. Studies with following traits were excluded: (1) protocol, case reports, or case series; (2) other interventions that do not belong to traditional acupuncture, such as transcutaneous electrical nerve stimulation and transcutaneous vagus nerve stimulation; and (3) comorbid severe mental illness or neurological illness. In addition, studies with relatively consistent study design and analytical methods were included in the meta-analysis.
All the identified studies were imported into NoteExpress. After a review of the title and abstracts, studies that did not meet the inclusion criteria were excluded. Final studies were determined after a full-text review. Following this approach, 22 studies were selected (Figure 1).
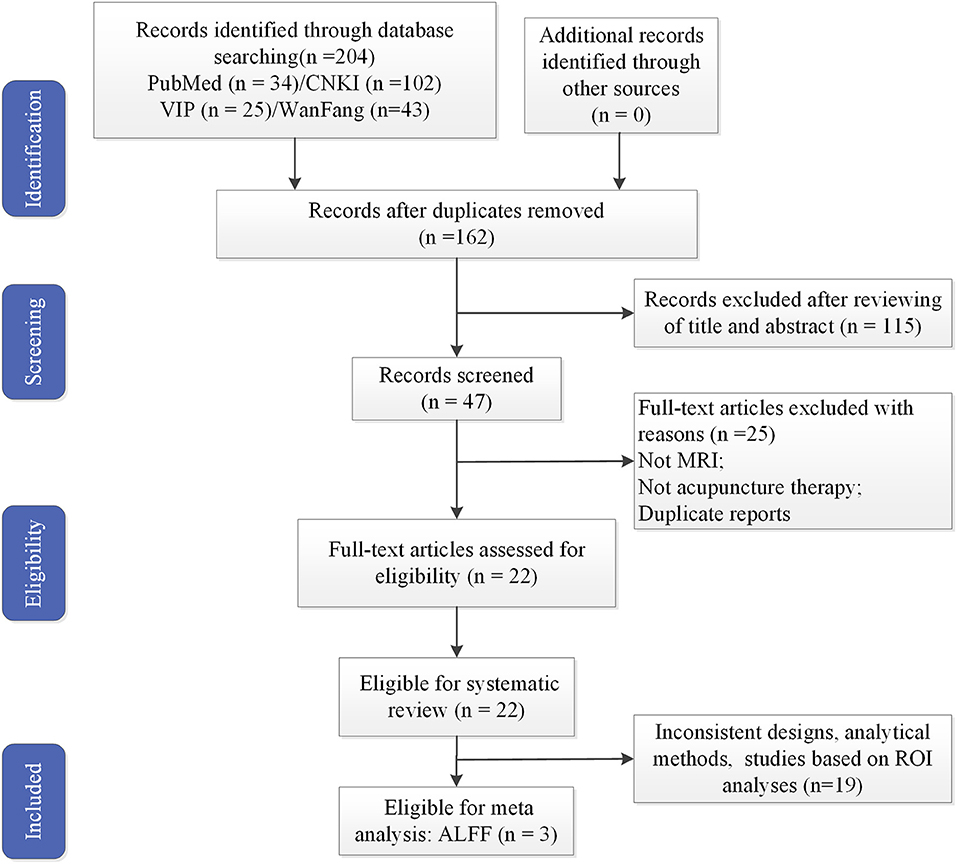
Figure 1. Flowchart of literature selection. MRI, magnetic resonance imaging; ALFF, amplitude of low-frequency fluctuation.
Data Extraction
Data were extracted from each study by one reviewer and then verified by a second reviewer. The following key information were extracted from each study: first author, publication year, study design, sample size, characteristics of participants, imaging modality and conditions, analytical methods, main acupoints/sites, and reported results. The peak coordinates and the statistical significance level were extracted from studies with similar MRI analytical methods and designs. Any disagreements in article selection and data extraction were resolved through discussions with a third author.
Coordinate-Based Meta-Analysis
The present coordinate-based meta-analysis (CBMA) was performed using Signed Differential Mapping with Permutation of Subject Images version 6.21 (SDM-PSI) (https://www.sdmproject.com/). Briefly, CBMA was carried out with the following procedure: collection of peak coordinates and their t-values; calculation of the maps of the lower and upper bounds of possible effect sizes; estimation of the map of most likely effect size and its standard error based on the MetaNSUE algorithms; multiple imputations of the maps of the effect size of individual studies; and using a standard random-effects model and Rubin rules to pool the different meta-analyses resulting from the multiple imputations (35–37), and the specific procedures have been extensively described in the SDM-PSI reference manual (https://www.sdmproject.com/manual/).
SDM-PSI is a new-generation algorithm for CBMA. This method has significant improvements in several aspects, such as using threshold-free cluster enhancement (TFCE) statistics, small bias estimates of the overall size estimates, and multiple imputations of the study image, to avoid bias associated with single imputation (35). The detailed data processing procedures are described in our previous article (38). We reported results using uncorrected p < 0.005 thresholds with a cluster extent = 10 voxels, since it was found to be optimally balance sensitivity and specificity (36, 39).
Results
Study Characteristics
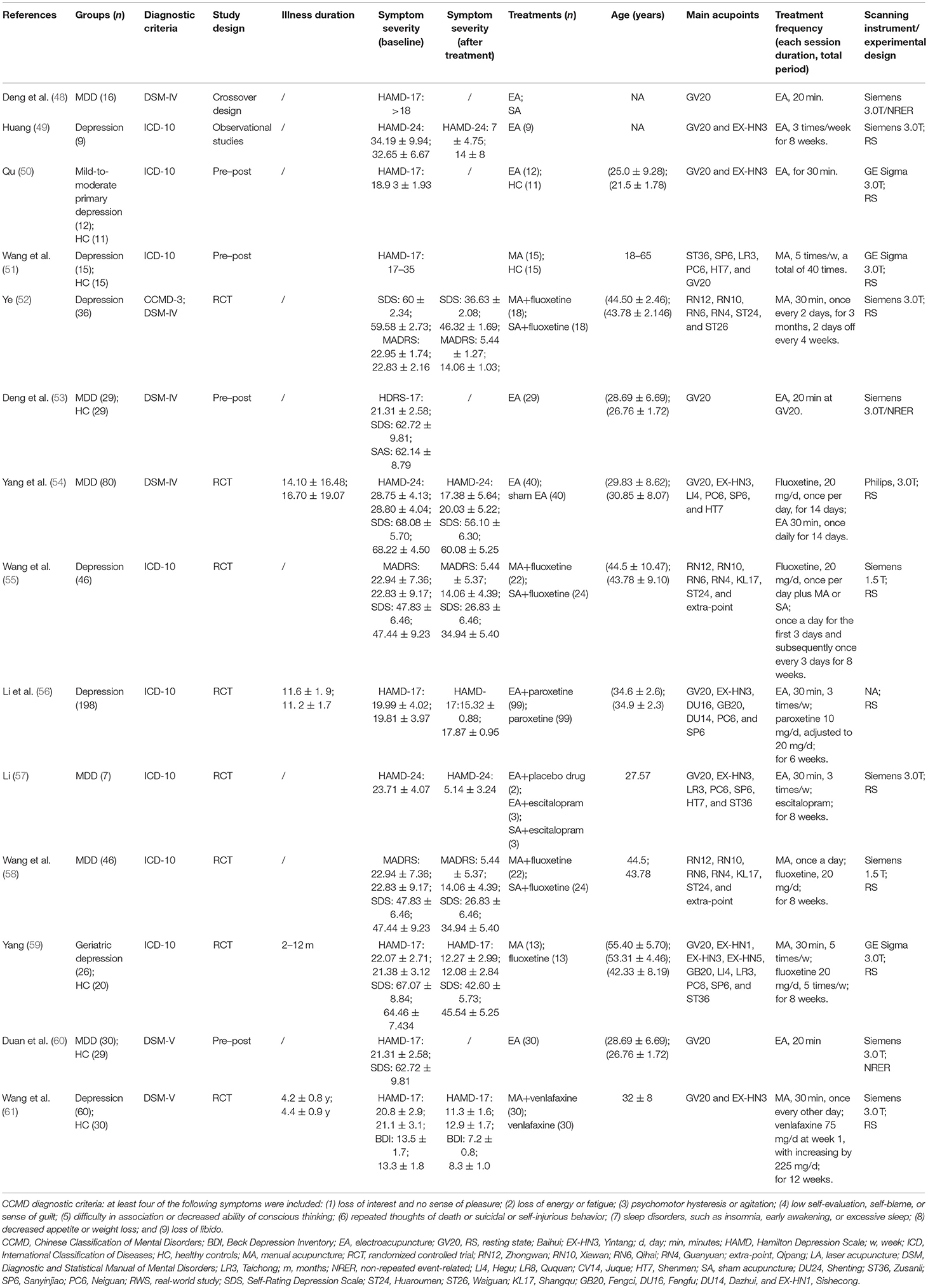
Characteristics of the included studies are reported in Table 1. A total of 22 articles were included in this review. One study was from Australia (46), and the remaining studies were from China. Six (41, 46, 53, 55, 58, 60) were indexed in the Science Citation Index. Four studies (42, 49, 53, 60) adopted one parallel-group design, three studies (40, 44, 57) involved three parallel-arm group designs, and the remaining studies adopted two parallel-arm group designs.
Study sample sizes ranged from 29 to 160, with a total of 826 depression patients and 416 health controls (HCs). For diagnostic criteria of depression, DSM-IV or DSM-V criteria were used in nine studies (44, 45, 48, 52–54, 60, 61), ICD-10 was used in nine studies (41, 49–51, 55–58), and CCMD-3 was used in four studies (40, 42, 47, 52).
In terms of depression types, MDD was diagnosed in nine studies (41, 46–48, 53, 54, 57, 58, 60), geriatric depression was diagnosed in one study (59), mild-to-moderate primary depression was diagnosed in one study (44), mild depression was diagnosed in one study (43), and the remaining were not specified.
In this study, non-repeated event-related (NRER) paradigm was adopted in three studies (42, 53, 60), and a resting-state fMRI (rs-fMRI) paradigm was used in the remaining studies.
The main treatment procedures included manual acupuncture (MA), EA, and LA, with sessions ranging from 4 to 12 weeks. The top three acupoints were GV20-Baihui (13), EX-HN3-Yintang (10), and LR3-Taichong (7). Twenty-two studies reported the needle retention time of their main interventions, with ~12 min for average duration.
Results of MRI Studies
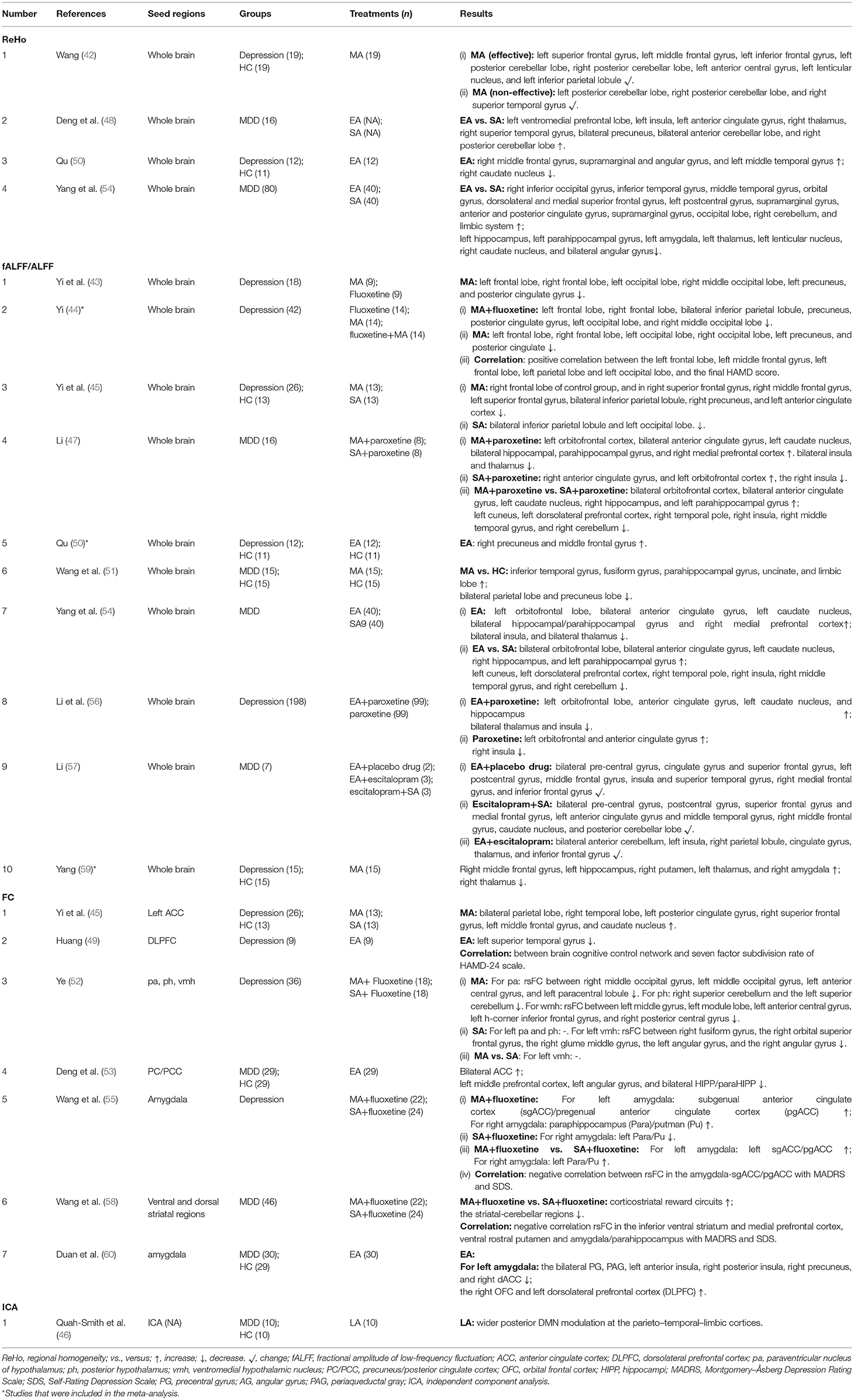
Regional homogeneity (ReHo), (fractional) amplitude of low-frequency fluctuation [(f)ALFF], and FC were applied in 22 studies; whereas magnetic resonance spectroscopy (MRS), sMRI, and diffusion tensor imaging (DTI) were only used in two studies (Tables 2–5).
These studies included five different comparisons: (1) acupuncture vs. sham acupuncture (SA); (2) acupuncture plus drug vs. SA plus drug; (3) acupuncture vs. drug; (4) acupuncture plus drug vs. drug; and (5) post-acupuncture vs. pre-acupuncture.
The main findings were as follows:
(i) ReHo was used in four studies (42, 48, 50, 54), showing that acupuncture could modulate ReHo value in limbic system and cerebral cortex (Table 2).
(ii) ALFF was used in 10 studies (43–45, 47, 50, 51, 54, 56, 57, 59): these studies showed relatively consistent results that acupuncture mainly modulates brain activity in the cerebellum, limbic lobe, frontal lobe, temporal lobe, and thalamus (Table 2).
(iii) Seed-based FC was used in seven studies (45, 49, 52–54, 58, 60), whereas independent component analysis (ICA) was used in one study (46) (Table 2). Specifically, Wang et al. (55) showed that acupuncture enhanced FC between the amygdala and anterior cingulate cortex (ACC); Deng et al. (53) showed that acupuncture enhanced FC between the precuneus/posterior cingulate cortex (PC/PCC) and ACC; and one study (45) selected the ACC as the seed and found that acupuncture enhanced FC between the ACC and the bilateral parietal lobe, right temporal lobe, left posterior cingulate gyrus, etc. Therefore, acupuncture could increase FC between the ACC and other brain regions.
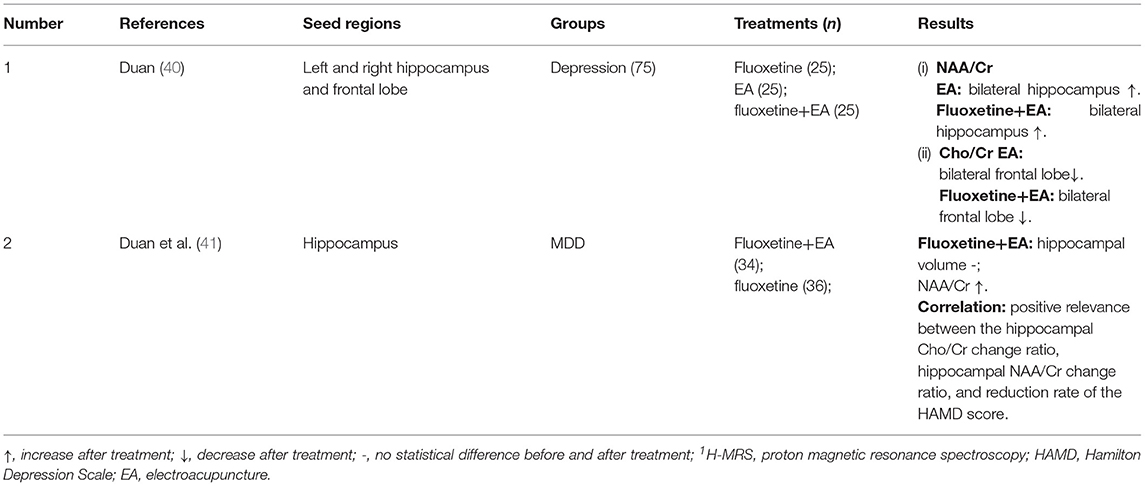
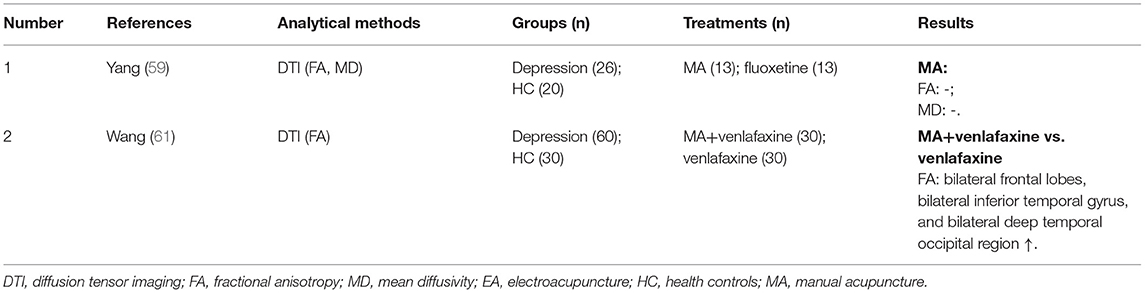
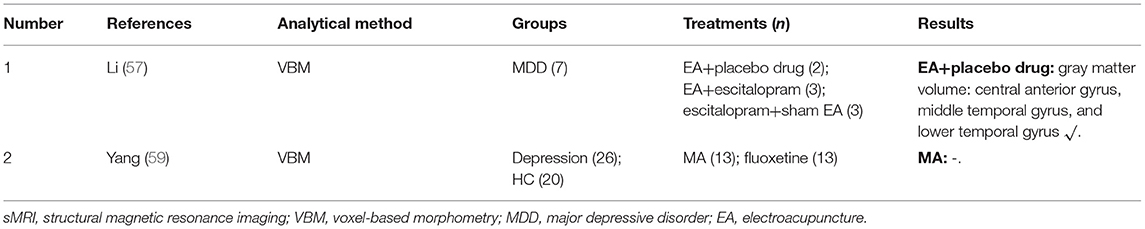
(iv) Proton MRS (1H-MRS) was used in two studies (40, 41), which showed increased N-acetylaspartate/creatine (NAA/Cr) ratio after EA treatment (Table 3). DTI was used in two studies (59, 61) (Table 4), and voxel-based morphometry (VBM) was used in two studies (57, 59) (Table 5), but none of these studies was able to detect significant neurological changes after acupuncture.
(v) In addition, a total of seven (45, 47, 48, 52, 54, 55, 58) were conducted to compare the brain response of verum acupuncture (VA) with SA on depression. The relatively consistent findings argue that acupuncture can modulate more brain activity, especially in the brain regions associated with depression compared with SA. In addition, two studies comparing acupuncture plus drugs with SA plus drugs found that the combination of acupuncture with drugs has a complex mutual influence on the central nervous system, rather than simply a combination of curative effects.
Results of Meta-Analysis
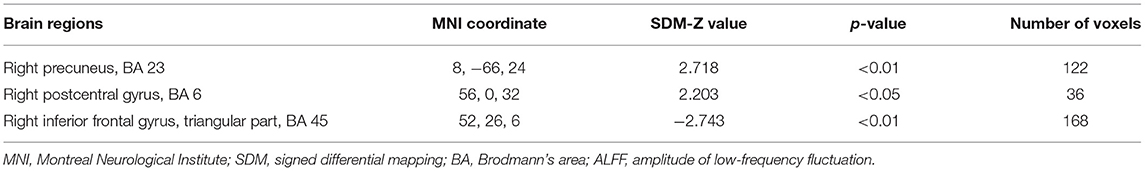
Three studies (44, 50, 59) met the criteria for meta-analysis. A total of 86 depressed patients were compared before and after acupuncture treatment for ALFF changes. This analysis revealed ALFF signals in the right precuneus and right postcentral gyrus significantly increased, and ALFF signals in the right inferior frontal gyrus (IFG) decreased in depressed patients after acupuncture treatment (Table 6 and Figures 2A–C).
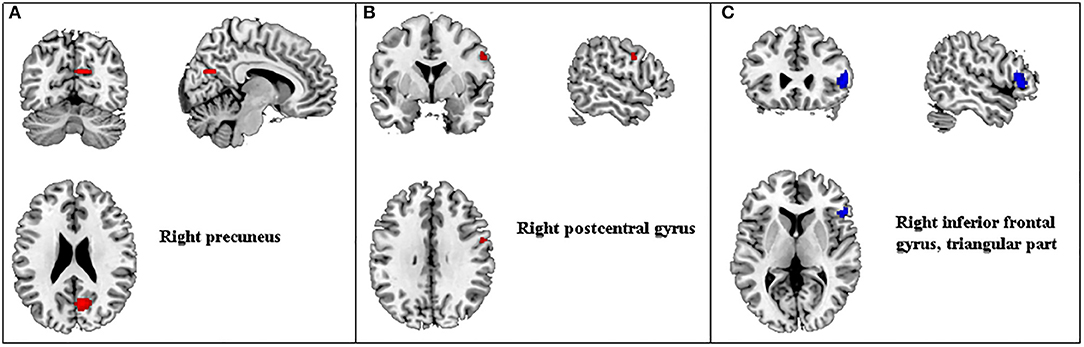
Figure 2. Regions of ALFF differences before and after acupuncture treatment in patients with depression. Red for increased ALFF (A,B) and blue for decreased ALFF (C). ALFF, amplitude of low-frequency fluctuation.
Discussion
This systematic review was designed to summarize findings of MRI studies aimed at evaluating the neurological effects of acupuncture treatment for depression. A total of 22 studies involving 810 depression patients and 416 HCs were evaluated. Importantly, further meta-analysis using SDM-PSI was conducted with three studies to explore changes in ALFF after acupuncture for depression.
Characteristics of MRI Study on Acupuncture Therapy for Depression
Among the 22 studies included in this study, 21 studies were from China, which may be explained by the fact that acupuncture originated in China over 3,000 years ago and is widely accepted in the Chinese society.
It is a common phenomenon in MRI research for the sample size of a study to be small. Although the optimal sample size needed to detect or evaluate an experimental factor has been investigated in this field (62, 63), the number of subjects is usually limited by practical constraints such as scanning time and costs (64). To reduce subject bias, it is necessary to estimate size effects, between- and within-subject variances, and temporal autocorrelation matrix (65).
In regard to the classification of depression, the patients in eight studies were considered MDD, one study examined geriatric depression, and the rest of the patients were not specified. Indeed, depression is a heterogeneous syndrome that includes a wide variety of symptoms and different responses to treatment (66). At present, several studies have shown that depression subtypes are highly correlated with brain function, which may help identify individuals who would benefit most from a particular treatment (66, 67). Our systematic review was unable to find a study that investigates the relationship between subtypes of depression and efficacy of acupuncture based on MRI techniques. Thus, future studies are needed to do this.
Regarding the types of acupuncture, MA, EA, and LA are those most often used as treatment for depression. They are different acupuncture techniques. Specifically, MA is defined as manual manipulation of needles after insertion at certain acupuncture points (16). EA is characterized by application of small current passing through acupuncture needles to produce the combined effect of electrical and needling stimulation (68). LA is a kind of non-penetrating acupuncture that uses low-power laser to stimulate acupoints (16). Anyway, all of them can stimulate acupoints. Although some studies (69–73) have compared the clinical efficacy of MA, EA, and LA for diseases, little research has been conducted to compare the differences in brain activity induced by each of the three types of acupuncture on patients using MRI methods.
The first two most common acupoints are GV20 and EX-HN3, which are located in Du meridian. Du meridian is responsible for regulating consciousness disease and organ lesions (74). GV20 is located on the highest place of the head where all the Yang meridians meet. Based on TCM theory, acupuncture on GV20 is used to clear the mind, lift the spirit, and tonify Yang (75). EX-HN3 is in charge of nourishing the brain and regulating emotional disorder (76). Moreover, animal studies have shown that the release of depression symptoms with acupuncture on GV20 and EX-HN3 may be related to decreasing serum corticosterone concentrations and increasing neurotransmitter levels (5-HT, Glu, and GABA) and protein levels of brain-derived neurotrophic factor (BDNF) (77, 78). In addition, three studies only applied one acupoint for treatment, whereas the rest combined multiple acupoints for treatment of depression. Recent studies (79, 80) have shown that a combination of acupoints can activate more areas of the brain as compared with a single acupoint. In the future, it will be important to investigate the relationship among GV20 and EX-HN3, efficacy, and activation of brain regions.
In addition, it is very hard to distinguish the activation effect of specific acupoints on the brain since combinations of different acupoints will cause some confusion, although we really want to perform them. Therefore, we summarized as much as possible studies on treating depression with the same single acupoint. Firstly, three studies (43–45) investigated brain response of acupuncture at LR3 and revealed that acupuncture could reduce ALFF in the frontal lobe, precuneus, and occipital lobe. Secondly, two studies (53, 60) involved FC of acupuncture at GV20 and demonstrated that acupuncture could modulate abnormal default mode network (DMN) in patients and could affect the FC of the amygdala. Thirdly, three studies (48, 52, 54) were conducted to investigate brain activity of acupuncture at GV20 and EX-HN3 and showed that acupuncture not only remodeled the white matter fiber bundle microstructure in certain brain regions but also increase NAA/Cr ratio, regulated FC of cognitive control networks, and activated brain activity of the middle temporal gyrus and caudate nucleus.
Experimental Designs of MRI
The fundamental experimental design of fMRI research mainly includes task-state fMRI and rs-fMRI. The earliest studies of acupuncture using fMRI were performed with a block design to observe the immediate effects of acupuncture (81–83). The needle inserted before the scan was stimulated continuously for several blocks of 30 s to 2 min. However, based on TCM theory, acupuncture induces a lasting effect that will still produce the corresponding neurological response even after holding for 30 min (82, 84). Thus, in recent years, some studies have adopted NRER designs (85–87); these designs are more in line with acupuncture methods and their effects. They also can reduce interference from the persistent effect of acupuncture that occurs when a single, prolonged acupuncture stimulation is given during the scanning process (88). However, this type of experimental design may have the limitation of a single stimulation, which is different from clinical treatment.
In a word, more and more attention is being paid to the effects of acupuncture on rs-fMRI (89, 90). This procedure of resting state is relatively simple and has several advantages that are more suitable for exploring mechanism of acupuncture effect. For example, brain function characteristics or changes in different states, such as before, during, and after acupuncture treatment, and especially any long-term cumulative effects, can be obtained through different data processing methods. Moreover, in recent years, rs-fMRI has been increasingly used to explore the effective neural mechanism of acupuncture for some diseases, such as Alzheimer's disease (91), stroke (92), and migraine (93). Rs-fMRI study is considered to be more advantageous than task fMRI in neuropsychiatric diseases (94). The above also explains why the number of rs-fMRI in this study is significantly higher than that of task states.
Study Design
Well-designed research trials are critical for determining the efficacy and effectiveness of new interventions (95). In interventional study designs, which are a subset of experimental study designs, researchers apply treatment interventions or preventive services to patients and then examine outcomes (96). The randomized controlled trial (RCT) design is typically considered as the “gold standard” for ascertaining intervention efficacy and effectiveness (97). There are other interventional study designs, including pre–post study design, non-randomized trial study design, and crossover RCT study design (80, 81).
In this review study, the experimental study design of acupuncture therapy for depression included RCT and pre–post study designs. RCTs with a placebo arm control have high internal validity and are considered a reliable method of evaluating treatment efficacy (98, 99). Only seven studies adapted placebo arms as controls. In interventional trials, blindness is often necessary, especially for patient-reported outcomes, to prevent reporting bias. However, blinding is difficult to implement due to the special nature of acupuncture, which can reduce the credibility of the research results. This is especially true for studies in which the effectiveness of acupuncture or acupuncture combined with drugs is being compared with drug treatment alone. Although this pre–post design has the disadvantages of enhanced selection bias, detection bias, and performance bias, it may be valuable to explore the first steps in the efficacy of new therapies (phase I design) at a time of increased demand for services and reduced resources (100). Thus, if the RCT is designed well, the only difference between study groups is the intervention itself (101). However, this type of design is pretty difficult to be conducted in an acupuncture study. Thus, finding a more rigorous design is an important guarantee for reaching reliable conclusions.
Analytical Methods of MRI
The most commonly used method is fMRI with ALFF and FC. ALFF is associated with blood oxygen level-dependent (BOLD) signals and can be used to detect a spontaneous, intrinsic neuronal activity (102), which has been applied in bipolar disorder patients (103), obsessive-compulsive disorder (104), and MDD (105). In our meta-analysis, we found that acupuncture could increase ALFF signals in the right precuneus and right postcentral gyrus and decreased ALFF signals in the right IFG. One meta-analysis (106) displayed increased ALFF in the bilateral precuneus of MDD patients compared with HCs. Moreover, the precuneus is a key node in the DMN (107), and low right precuneus activity has been associated with more depressive episodes in MDD patients, indicating a deleterious effect of depressive episodes on DMN (107). Several studies found that the ALFF values in the right inferior frontal significantly increased in depressive patients compared with HCs (106, 108). What is more, the IFG, as a key region in the emotion–cognition interplay (109), is involved in processing emotional information and evaluating affective salience (110). Therefore, increased ALFF signals in the right precuneus and increased ALFF signals in the IFG might be the underlying mechanism for the effects of acupuncture in depressed patients. Two previous studies (111, 112) found the fALFF in the left postcentral gyrus was significantly reduced in MDD patients. However, in our study, increased ALFF values in the right postcentral gyrus were identified. In view of these differences, additional research is necessary to confirm whether acupuncture treatment for depression produces consistent changes of ALFF values.
FC refers to the temporal correlation between spatially remote neurophysiological events (113). In this study, to understand the seed-based resting-state FC regarding acupuncture therapy for depression, the seed points selected were the left ACC, dorsolateral prefrontal cortex, posterior hypothalamus (ph), ventromedial hypothalamic nucleus (vmh), paraventricular nucleus of hypothalamus (pa), PC/PCC, amygdala, and striatum. Due to differences in the selection of seed points, the functional connections detected in various studies were also inconsistent, with the exception of the ACC, which was identified with a relatively high degree of consistency. Interestingly, a recent study (114) supported the notion of the ACC as a promising predictor of antidepressant response, which further illustrates the importance of the ACC in the pathogenesis of depression and as a target of acupuncture treatment for depression. The ACC, a limbic structure, is associated with a range of other limbic and related regions, including the amygdala and orbitofrontal cortex (OFC), involved in emotional and reward-related processing (107, 115). Collectively, these findings may give us some clues whether the effects of acupuncture on emotion-related diseases are related to its effect on the ACC.
The fMRI analytical method was the most widely used in the studies evaluated in this review, while sMRI analytical method was used relatively infrequently. One reason is that in recent years, more and more attention has been paid to fMRI and less to sMRI. The other reason is that acupuncture is more likely to modulate brain functional activity in a short period of time, whereas structural alternations may not be easy to form or be detected. However, different modalities of neuroimaging can provide information complementary to each other (116). Therefore, the important implication of this study is that maybe we should explore more analytical methods to better explain the underlying neural mechanisms of acupuncture treatment for depression.
Comparing Verum Acupuncture With Sham Acupuncture on the Brain Response
In this study, we found that VA could activate more brain activity and increase connectivity than SA. Although the superiority of VA over SA remains a global controversy, an increasing number of neuroimaging studies suggest that compared with SA, VA works in a more targeted and specialized manner on depressive patients (47, 52, 54), which is consistent with other diseases, such as migraine (117).
In clinical trials, placebo controls should be consistent with active treatment (that is, reaching the equivalence of blindness), except that they are physiologically inert (118). In regard to acupuncture, however, it is difficult to develop placebo needles satisfying both blinding and physiological inertness. At present, the devices of SA can be divided into two types based on whether they penetrate the skin. However, due to a less effective form of penetrating SA, it is rarely used anymore. Several non-penetrating devices including a foam placebo device (119), Streitberger placebo device (120), and Park device (121), have been developed to evaluate potential placebo effects. Nevertheless, not only are the effects of SA caused by psychological effects of the sham procedure, but also data from imaging studies have shown that expectations, learning, and background factors play important roles in the placebo effect (122–124).
Indeed, placebo research has revealed that the definition of placebo may not be as clear as necessary for clinical trials in non-pharmacological fields. The placebo effect is seen as a positive and useful factor in treatment, especially in clinical practice, which is considered a part of every routine treatment (125). Thus, it is unnecessary to argue about how much treatment effect depends on placebos. Instead, the most important question should focus on clinical efficacy: what will relieve patients' pain and how best to treat them. This pragmatic approach aims to maximize all the positive aspects of treatment while minimizing the risks and negative effects, including the nocebo effect (125).
Limitations
Although this review provides a detailed overview of the current literature about MRI research on the neurological effects of acupuncture therapy for depression, some limitations need to be noted. Firstly, most of the included studies are from Chinese literature, which reduces the readability of research literature and the applicability to other races. Secondly, the brain responses to acupuncture are influenced by many factors, for example, acupuncture depth, duration and course, differences in MRI devices, analytical methods, experimental designs, and patients' responses to acupuncture. Therefore, it is difficult to determine the specific factor that affects the brain during acupuncture treatment for depression. Researchers should follow the standards for reporting interventions in controlled trials of acupuncture (STRICTA) guidelines (126) when designing and reporting MRI of acupuncture research. Thirdly, due to the small samples and large heterogeneity among different acupuncture types, acupoints, design, and analytical methods, it is extremely hard to perform a comprehensive meta-analysis for more studies to draw consistent conclusions. It is essential that researchers report relevant coordinates for further deep analysis and investigation. In addition, it is extremely hard to explore how FC was altered by acupuncture treatment for depression since different seed points were involved in related studies. Fourthly, only three studies explored the correlation between brain responses to acupuncture and clinical outcomes. Anyway, these correlations play an important role in understanding biomarkers on acupuncture treatment for depression. Finally, most of the studies did not set SA as a placebo control, making it impossible to avoid placebo effects. In addition, the sample size was also small, which limited the reliability of MRI mechanism research on the mechanism of acupuncture treatment of depression.
Conclusions
In conclusion, MRI analytical methods of acupuncture treatment for depression include 1H-MRS, ReHo, (f)ALFF, FC, VBM, and DTI. Among them, fMRI was the often most used and showed that acupuncture could modulate brain function in several ways, while sMRI and DTI were used the least and did not detect any significant changes. Moreover, the relatively consistent fMRI results showed increased NAA/Cr ratio, increased ALFF in the right precuneus, decreased ALFF in the IFG, and increased FC of the ACC. However, future studies need to apply more analytical methods of MRI to investigate the neurological effects of acupuncture treatment in depression in the future. In addition, improved report specifications, well-designed experiments, consistent analytical methods, and larger sample sizes will enable the field to better elucidate the underlying mechanisms of acupuncture therapy for depressed patients.
Author Contributions
JZ and JX designed the whole study, analyzed the data, and wrote the manuscript. XW and DN searched and selected the studies. JL and YZ participated in the interpretation of data. HY and QH offered good suggestions. All authors read and approved the final manuscript.
Funding
This work was supported by National Key R&D Program of China (2019YFC1712200), International standards research on clinical research and service of Acupuncture-Moxibustion (2019YFC1712205), Shenzhen Key Basic Research Program (JCYJ20200109114816594), and Shenzhen's Sanming Project (SZSM201612001).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.670739/full#supplementary-material
References
1. Armour M, Smith CA, Wang LQ, Naidoo D, Yang GY, MacPherson H, et al. Acupuncture for depression: a systematic review and meta-analysis. J Clin Med. (2019) 8:1140. doi: 10.3390/jcm8081140
2. Gawlik S, Waldeier L, Muller M, Szabo A, Sohn C, Reck C. Subclinical depressive symptoms during pregnancy and birth outcome–a pilot study in a healthy German sample. Arch Womens Ment Health. (2013) 16:93–100. doi: 10.1007/s00737-012-0320-0
3. Prinz P, Hertrich K, Hirschfelder U, de Zwaan M. Burnout, depression and depersonalisation–psychological factors and coping strategies in dental and medical students. GMS Z Med Ausbild. (2012) 29:c10. doi: 10.3205/zma000780
4. Supe AN. A study of stress in medical students at Seth G.S. Medical College. J Postgrad Med. (1998) 44:1–6.
5. Wan YH, Gao R, Tao XY, Tao FB, Hu CL. Relationship between deliberate self-harmand suicidal behaviors in college students. Zhonghua Liu Xing Bing Xue Za Zhi. (2012) 33:474–7. doi: 10.3760/cma.j.issn.0254-6450.2012.05.006
6. Osama M, Islam MY, Hussain SA, Masroor SM, Burney MU, Masood MA, et al. Suicidal ideation among medical students of Pakistan: a cross-sectional study. J Forensic Leg Med. (2014) 27:65–8. doi: 10.1016/j.jflm.2014.08.006
7. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. (2005) 62:593–602. doi: 10.1001/archpsyc.62.6.593
8. Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, de Girolamo G, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. (2011) 9:90. doi: 10.1186/1741-7015-9-90
9. Rush AJ, Trivedi M, Fava M. Depression, IV: STAR*D treatment trial for depression. Am J Psychiatry. (2003) 160:237. doi: 10.1176/appi.ajp.160.2.237
10. Arroll B, Macgillivray S, Ogston S, Reid I, Sullivan F, Williams B, et al. Efficacy and tolerability of tricyclic antidepressants and SSRIs compared with placebo for treatment of depression in primary care: a meta-analysis. Ann Fam Med. (2005) 3:449–56. doi: 10.1370/afm.349
11. Zhu D, Gao Y, Chang J, Kong J. Placebo acupuncture devices: considerations for acupuncture research. Evid Based Complement Alternat Med. (2013) 2013:628907. doi: 10.1155/2013/628907
12. Duan DM, Tu Y, Chen LP. Assessment of effectiveness of electroacupuncture and fluoxetine for treatment of depression with physical symptoms. Zhongguo Zhen Jiu. (2008) 28:167–70.
13. Mallory MJ, Do A, Bublitz SE, Veleber SJ, Bauer BA, Bhagra A. Puncturing the myths of acupuncture. J Integr Med. (2016) 14:311–4. doi: 10.1016/S2095-4964(16)60269-8
14. Asher GN, Gerkin J, Gaynes BN. Complementary therapies for mental health disorders. Med Clin North Am. (2017) 101:847–64. doi: 10.1016/j.mcna.2017.04.004
15. Zhang ZJ, Chen HY, Yip KC, Ng R, Wong VT. The effectiveness and safety of acupuncture therapy in depressive disorders: systematic review and meta-analysis. J Affect Disord. (2010) 124:9–21. doi: 10.1016/j.jad.2009.07.005
16. Smith CA, Armour M, Lee MS, Wang LQ, Hay PJ. Acupuncture for depression. Cochrane Database Syst Rev. (2018) 3:D4046. doi: 10.1002/14651858.CD004046.pub4
17. Fang J, Jin Z, Wang Y, Li K, Kong J, Nixon EE, et al. The salient characteristics of the central effects of acupuncture needling: limbic-paralimbic-neocortical network modulation. Hum Brain Mapp. (2009) 30:1196–206. doi: 10.1002/hbm.20583
18. Li S, Wang Y, Gao G, Guo X, Zhang Y, Zhang Z, et al. Transcutaneous auricular vagus nerve stimulation at 20 Hz improves depression-like behaviors and down-regulates the hyperactivity of HPA axis in chronic unpredictable mild stress model rats. Front Neurosci. (2020) 14:680. doi: 10.3389/fnins.2020.00680
19. Le JJ Yi T, Qi L, Li J, Shao L, Dong JC. Electroacupuncture regulate hypothalamic-pituitary-adrenal axis and enhance hippocampal serotonin system in a rat model of depression. Neurosci Lett. (2016) 615:66–71. doi: 10.1016/j.neulet.2016.01.004
20. Lee B, Shim I, Lee HJ, Yang Y, Hahm DH. Effects of acupuncture on chronic corticosterone-induced depression-like behavior and expression of neuropeptide Y in the rats. Neurosci Lett. (2009) 453:151–6. doi: 10.1016/j.neulet.2009.01.076
21. Mo Y, Yao H, Song H, Wang X, Chen W, Abulizi J, et al. Alteration of behavioral changes and hippocampus galanin expression in chronic unpredictable mild stress-induced depression rats and effect of electroacupuncture treatment. Evid Based Complement Alternat Med. (2014) 2014:179796. doi: 10.1155/2014/179796
22. Han X, Wu H, Yin P, Chen Z, Cao X, Duan Y, et al. Electroacupuncture restores hippocampal synaptic plasticity via modulation of 5-HT receptors in a rat model of depression. Brain Res Bull. (2018) 139:256–62. doi: 10.1016/j.brainresbull.2018.03.004
23. Song C, Halbreich U, Han C, Leonard BE, Luo H. Imbalance between pro- and anti-inflammatory cytokines, and between Th1 and Th2 cytokines in depressed patients: the effect of electroacupuncture or fluoxetine treatment. Pharmacopsychiatry. (2009) 42:182–8. doi: 10.1055/s-0029-1202263
24. Lu J, Shao RH, Hu L, Tu Y, Guo JY. Potential antiinflammatory effects of acupuncture in a chronic stress model of depression in rats. Neurosci Lett. (2016) 618:31–8. doi: 10.1016/j.neulet.2016.02.040
25. Lu J, Shao RH, Jin SY, Hu L, Tu Y, Guo JY. Acupuncture ameliorates inflammatory response in a chronic unpredictable stress rat model of depression. Brain Res Bull. (2017) 128:106–12. doi: 10.1016/j.brainresbull.2016.11.010
26. Zhang X, Song Y, Bao T, Yu M, Xu M, Guo Y, et al. Antidepressant-like effects of acupuncture involved the ERK signaling pathway in rats. BMC Complement Altern Med. (2016) 16:380. doi: 10.1186/s12906-016-1356-x
27. Jiang H, Zhang X, Wang Y, Zhang H, Li J, Yang X, et al. Mechanisms underlying the antidepressant response of acupuncture via PKA/CREB signaling pathway. Neural Plast. (2017) 2017:4135164. doi: 10.1155/2017/4135164
28. Li W, Zhu Y, Saud SM, Guo Q, Xi S, Jia B, et al. Electroacupuncture relieves depression-like symptoms in rats exposed to chronic unpredictable mild stress by activating ERK signaling pathway. Neurosci Lett. (2017) 642:43–50. doi: 10.1016/j.neulet.2017.01.060
29. Yang X, Guo Z, Lu J, Zhao B, Fei Y, Li J, et al. The role of MAPK and dopaminergic synapse signaling pathways in antidepressant effect of electroacupuncture pretreatment in chronic restraint stress rats. Evid Based Complement Alternat Med. (2017) 2017:2357653. doi: 10.1155/2017/2357653
30. Huang W, Pach D, Napadow V, Park K, Long X, Neumann J, et al. Characterizing acupuncture stimuli using brain imaging with FMRI–a systematic review and meta-analysis of the literature. PLoS ONE. (2012) 7:e32960. doi: 10.1371/journal.pone.0032960
31. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:b2535. doi: 10.1136/bmj.b2535
32. Malhi GS, Coulston CM, Fritz K, Lampe L, Bargh DM, Ablett M, et al. Unlocking the diagnosis of depression in primary care: which key symptoms are GPs using to determine diagnosis and severity? Aust N Z J Psychiatry. (2014) 48:542–7. doi: 10.1177/0004867413513342
33. World Health Organization. The ICD-10 Classification of Mental and Behavioral Disorders Researching Criteria. Geneva: World Health Organization (1992).
34. Chinese Society of Psychiatry. The Chinese Classification and Diagnostic Criteria of Mental Disorders Version 3 (CCMD-3). Jinan: Chinese Society of Psychiatry (2001).
35. Albajes-Eizagirre A, Solanes A, Vieta E, Radua J. Voxel-based meta-analysis via permutation of subject images (PSI): theory and implementation for SDM. Neuroimage. (2019) 186:174–84. doi: 10.1016/j.neuroimage.2018.10.077
36. Radua J, Mataix-Cols D, Phillips ML, El-Hage W, Kronhaus DM, Cardoner N, et al. A new meta-analytic method for neuroimaging studies that combines reported peak coordinates and statistical parametric maps. Eur Psychiatry. (2019) 27:605–11. doi: 10.1016/j.eurpsy.2011.04.001
37. Albajes-Eizagirre A, Solanes A, Fullana MA, Ioannidis J, Fusar-Poli P, Torrent C, et al. Meta-analysis of voxel-based neuroimaging studies using seed-based d mapping with permutation of subject images (SDM-PSI). J Vis Exp. (2019) 2019:59841. doi: 10.3791/59841
38. Zhang J, Liu Y, Lan K, Huang X, He Y, Yang F, et al. Gray matter atrophy in amnestic mild cognitive impairment: a voxel-based meta-analysis. Front Aging Neurosci. (2021) 13:627919. doi: 10.3389/fnagi.2021.627919
39. Lieberman MD, Cunningham WA. Type I and Type II error concerns in fMRI research: re-balancing the scale. Soc Cogn Affect Neurosci. (2009) 4:423–8. doi: 10.1093/scan/nsp052
40. Duan D. The Study on Clinical Effect and Mechanism of Electric-Acupuncture Therapy for Depression.Beijing: Beijing University of Chinese Medicine. (2008).
41. Duan D, Tu Y, Jiao S, Qin W. The relevance between symptoms and magnetic resonance imaging analysis of the hippocampus of depressed patients given electro-acupuncture combined with Fluoxetine intervention — a randomized, controlled trial. Chin J Integr Med. (2011) 17:190–9. doi: 10.1007/s11655-011-0666-6
42. Wang B. A fMRI Study on the Effects of Bo-Shi Abdominal Acupuncture on Women With Depression.Guangzhou: Guangzhou University of Chinese Medicine. (2011).
43. Yi Y, Zhao Y, Cha JF, Zhang B. Acupuncture Taichong point for treatment of mild depression patients: an fMRI study. Med J Chinese People Armed Police Forces. (2011) 22:760–3. doi: 10.3969/j.issn.1004-3594.2011.09.008
44. Yi Y. Correlation Between the Liver Meridian and the Frontal Lobe in Depression by Needling at Taichong (LV3): A Resting-State fMRI Study. Chongqing: Chongqing Medical University. (2011).
45. Yi Y, Xu F, Xie P, Lv JF, Lin Y, Wu Y, et al. Acupuncturing Taichong point for regulating the brain function of depression patients: resting-state fMRI study. Chin J Trad Chin Med. (2012) 27:369–73.
46. Quah-Smith I, Suo C, Williams MA, Sachdev PS. The antidepressant effect of laser acupuncture: a comparison of the resting brain's default mode network in healthy and depressed subjects during functional magnetic resonance imaging. Medical Acupuncture. (2013) 25:124–33. doi: 10.1089/acu.2012.0901
47. Li Y. Central Mechanism involved in Acupuncture Depression based on fMRI Study. Chengdu: Chengdu University of Traditional Chinese Medicine (2014).
48. Deng D, Duan G, Liao H, Pang Y, He Q, Liu H, et al. Acupuncture Baihui activated the functional brain areas of major depressive disorder patients with regional homogeneity. Chin J Med Imag Technol. (2015) 31:683–7. doi: 10.13929/j.1003-3289.2015.05.011
49. Huang Z. Effects of Electroacupuncture Intervention on Brain Cognitive Control Network in Depression.Beijing: Beijing University of Chinese Medicine. (2015).
50. Qu S. The Clinical and Rs-fMRI Study on Mild-to-Moderate Primary Deprssion Treated With Electro-Acupuncture at GV24 and GV29. Guangzhou: Southern Medical University (2015).
51. Wang Y, Li X, Lv F, Ren Y, et al. A fMRI study on acupuncture of strengthening spleen and soothing liver method on patients with major depressive disorder. Liaoning J Trad Chin Med. (2015) 42:1611–4. doi: 10.13192/j.issn.1000-1719.2015.09.003
52. Ye G. Abdominal Acupuncture Combined Medicine in MRI Study of Brain Functional Connectivity With Major Depression Disorder. Guangzhou: Guangzhou University of Chinese Medicine. (2015).
53. Deng D, Liao H, Duan G, Liu Y, He Q, Liu H, et al. Modulation of the default mode network in first-episode, drug-naïve major depressive disorder via acupuncture at Baihui (GV20) Acupoint. Front Hum Neurosci. (2016) 10:230. doi: 10.3389/fnhum.2016.00230
54. Yang M, Zhou Y, Wu Y, Ge X, Wu Q. Clinical observation of electroacupuncture for depression and its brain response monitored by fMRI. Sichuan Mental Health. (2016) 29:132–6. doi: 10.11886/j.issn.1007-3256.2016.02.008
55. Wang X, Wang Z, Liu J, Chen J, Liu X, Nie G, et al. Repeated acupuncture treatments modulate amygdala resting state functional connectivity of depressive patients. NeuroImage Clin. (2016) 12:746–52. doi: 10.1016/j.nicl.2016.07.011
56. Li K, Guo J, Chen Y. Efficacy of electro-acupuncture combined with antidepressant medicine in the treatment of primary depression with Rs-fMRI technique. J Clin Acupunct Moxibustion. (2017) 33:26–9. doi: 10.3969/j.issn.1005-0779.2017.12.008
57. Li J. Exploration of Anti-Depression Mechanism of Acupuncture Based on Magnetic Resonance Multimodal Analysis.Beijing: Beijing University of Chinese Medicine. (2017).
58. Wang Z, Wang X, Liu J, Chen J, Liu X, Nie G, et al. Acupuncture treatment modulates the corticostriatal reward circuitry in major depressive disorder. J Psychiatr Res. (2017) 84:18–26. doi: 10.1016/j.jpsychires.2016.09.014
59. Yang H. Clinical Basic Research on Mechanism of Acupuncture Treatment for geriatric depression Based on Magnetic Resonance Imaging Technology. Chengdu: Chengdu University of Traditional Chinese Medicine (2018).
60. Duan G, He Q, Pang Y, Chen W, Liao H, Liu H, et al. Altered amygdala resting-state functional connectivity following acupuncture stimulation at BaiHui (GV20) in first-episode drug-Naïve major depressive disorder. Brain Imaging Behav. (2020) 14:2269–80. doi: 10.1007/s11682-019-00178-5
61. Wang P, Yang C, Lian Z, Zhou Y, Xianping C, Yu L. Therapeutic effect of the combined treatment with acupuncture and venlafaxine hydrochloride on depression based on diffusion tensor imaging technology. Chin Acupunct Moxibustion. (2019) 39:571–5. doi: 10.13703/j.0255-2930.2019.06.001
62. Desmond JE, Glover GH. Estimating sample size in functional MRI (fMRI) neuroimaging studies: statistical power analyses. J Neurosci Methods. (2002) 118:115–28. doi: 10.1016/S0165-0270(02)00121-8
63. Mumford JA, Nichols TE. Power calculation for group fMRI studies accounting for arbitrary design and temporal autocorrelation. Neuroimage. (2008) 39:261–8. doi: 10.1016/j.neuroimage.2007.07.061
64. Murphy K, Garavan H. An empirical investigation into the number of subjects required for an event-related fMRI study. Neuroimage. (2004) 22:879–85. doi: 10.1016/j.neuroimage.2004.02.005
65. Guo Q, Thabane L, Hall G, Mckinnon M, Goeree R, Pullenayegum E, et al. Systematic review of the reporting of sample size calculations and corresponding data components in observational functional magnetic resonance imaging studies. Neuroimage. (2014) 86:172–81. doi: 10.1016/j.neuroimage.2013.08.012
66. Drysdale AT, Grosenick L, Downar J, Dunlop K, Mansouri F, Meng Y, et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat Med. (2017) 23:28–38. doi: 10.1038/nm.4246
67. Dinga R, Schmaal L, Penninx B, van Tol MJ, Veltman DJ, van Velzen L, et al. Evaluating the evidence for biotypes of depression: methodological replication and extension of. Neuroimage Clin. (2019) 22:101796. doi: 10.1016/j.nicl.2019.101796
68. Zhang J, Liu Y, Huang X, Chen Y, Hu L, Lan K, et al. Efficacy comparison of different acupuncture treatments for functional dyspepsia: a systematic review with network meta-analysis. Evid Based Complement Alternat Med. (2020) 2020:3872919. doi: 10.1155/2020/3872919
69. Nascimento FF, Marques VI, Crociolli GC, Nicacio GM, Nicacio I, Cassu RN. Analgesic efficacy of laser acupuncture and electroacupuncture in cats undergoing ovariohysterectomy. J Vet Med Sci. (2019) 81:764–70. doi: 10.1292/jvms.18-0744
70. Seo SY, Lee KB, Shin JS, Lee J, Kim MR, Ha IH, et al. Effectiveness of acupuncture and electroacupuncture for chronic neck pain: a systematic review and meta-analysis. Am J Chin Med. (2017) 45:1573–95. doi: 10.1142/S0192415X17500859
71. Casimiro L, Barnsley L, Brosseau L, Milne S, Robinson VA, Tugwell P, et al. Acupuncture and electroacupuncture for the treatment of rheumatoid arthritis. Cochrane Database Syst Rev. (2005) 2005:D3788. doi: 10.1002/14651858.CD003788.pub2
72. Meyer-Hamme G, Friedemann T, Greten HJ, Plaetke R, Gerloff C, Schroeder S, et al. - ACUpuncture and laser acupuncture for treatment of DIabetic peripheral Neuropathy: a randomized, placebo-controlled, partially double-blinded trial. BMC Neurol. (2018) 18:40. doi: 10.1186/s12883-018-1037-0
73. Chang WD, Lai PT, Tsou YA. Analgesic effect of manual acupuncture and laser acupuncture for lateral epicondylalgia: a systematic review and meta-analysis. Am J Chin Med. (2014) 42:1301–14. doi: 10.1142/S0192415X14500815
74. Guo LK, Zhang CX, Guo XF. Acupuncture combined with Chinese herbal medicine Plantain and Senna Granule in treatment of functional constipation: a randomized, controlled trial. Zhong Xi Yi Jie He Xue Bao. (2011) 9:1206–14. doi: 10.3736/jcim20111108
75. Shen EY, Chen FJ, Chen YY, Lin MF. Locating the Acupoint Baihui (GV20) beneath the cerebral cortex with MRI reconstructed 3D neuroimages. Evid Based Complement Alternat Med. (2011) 2011:362494. doi: 10.1093/ecam/neq047
76. Acar HV, Cuvas O, Ceyhan A, Dikmen B. Acupuncture on Yintang point decreases preoperative anxiety. J Altern Complement Med. (2013) 19:420–4. doi: 10.1089/acm.2012.0494
77. Tanahashi N, Takagi K, Amagasu N, Wang G, Mizuno K, Kawanoguchi J, et al. Effect of acupuncture stimulation on rats with depression induced by water-immersion stress. Neurosci Lett. (2016) 618:99–103. doi: 10.1016/j.neulet.2016.02.051
78. Duan DM, Tu Y, Liu P, Jiao S. Antidepressant effect of electroacupuncture regulates signal targeting in the brain and increases brain-derived neurotrophic factor levels. Neural Regen Res. (2016) 11:1595–602. doi: 10.4103/1673-5374.193238
79. Zhang J, Cai X, Wang Y, Zheng Y, Qu S, Zhang Z, et al. Different brain activation after acupuncture at combined acupoints and single acupoint in hypertension patients: an Rs-fMRI study based on ReHo analysis. Evid Based Complement Alternat Med. (2019) 2019:5262896. doi: 10.1155/2019/5262896
80. Liu L, Wu Y, Zheng J, Lai X, Zeng D, Li H, et al. Cerebral activation effects of acupuncture using Zusanli (ST36) and Yanglingquan (GB34) points based on Regional Homogeneity indices: a resting-state fMRI study. J Xray Sci Technol. (2016) 24:297–308. doi: 10.3233/XST-160557
81. Hui KK, Liu J, Makris N, Gollub RL, Chen AJ, Moore CI, et al. Acupuncture modulates the limbic system and subcortical gray structures of the human brain: evidence from fMRI studies in normal subjects. Hum Brain Mapp. (2000) 9:13–25. doi: 10.1002/(SICI)1097-0193(2000)9:1<13::AID-HBM2>3.0.CO;2-F
82. Bai L, Qin W, Tian J, Liu P, Li L, Chen P, et al. Time-varied characteristics of acupuncture effects in fMRI studies. Hum Brain Mapp. (2009) 30:3445–60. doi: 10.1002/hbm.20769
83. Cho ZH, Chung SC, Jones JP, Park JB, Park HJ, Lee HJ, et al. New findings of the correlation between acupoints and corresponding brain cortices using functional MRI. Proc Natl Acad Sci USA. (1998) 95:2670–3. doi: 10.1073/pnas.95.5.2670
84. Bai L, Tian J, Zhong C, Xue T, You Y, Liu Z, et al. Acupuncture modulates temporal neural responses in wide brain networks: evidence from fMRI study. Mol Pain. (2010) 6:73. doi: 10.1186/1744-8069-6-73
85. Feng Y, Bai L, Ren Y, Chen S, Wang H, Zhang W, et al. FMRI connectivity analysis of acupuncture effects on the whole brain network in mild cognitive impairment patients. Magn Reson Imaging. (2012) 30:672–82. doi: 10.1016/j.mri.2012.01.003
86. Zhang Y, Li K, Ren Y, Cui F, Xie Z, Shin J, et al. Acupuncture modulates the functional connectivity of the default mode network in stroke patients. Evid Based Complement Alternat Med. (2014) 2014:1–7. doi: 10.1155/2014/765413
87. Bai L, Tao Y, Wang D, Wang J, Sun C, Hao N, et al. Acupuncture induces time-dependent remodelling brain network on the stable somatosensory first-ever stroke patients: combining diffusion tensor and functional MR imaging. Evid Based Complement Alternat Med. (2014) 2014:740480. doi: 10.1155/2014/740480
88. Liu P, Qin W, Zhang Y, Tian J, Bai L, Zhou G, et al. Combining spatial and temporal information to explore function-guide action of acupuncture using fMRI. J Magn Reson Imaging. (2009) 30:41–6. doi: 10.1002/jmri.21805
89. Zhang Y, Jiang Y, Glielmi CB Li L, Hu X, Wang X, et al. Long-duration transcutaneous electric acupoint stimulation alters small-world brain functional networks. Magn Reson Imaging. (2013) 31:1105–11. doi: 10.1016/j.mri.2013.01.006
90. Zhang Y, Liang J, Qin W, Liu P, von Deneen KM, Chen P, et al. Comparison of visual cortical activations induced by electro-acupuncture at vision and non-vision-related acupoints. Neurosci Lett. (2009) 458:6–10. doi: 10.1016/j.neulet.2009.04.027
91. Liang P, Wang Z, Qian T, Li K. Acupuncture stimulation of Taichong (Liv3) and Hegu (LI4) modulates the default mode network activity in Alzheimer's disease. Am J Alzheimers Dis Other Demen. (2014) 29:739–48. doi: 10.1177/1533317514536600
92. Chen SQ, Cai DC, Chen JX, Yang H, Liu LS. Altered brain regional homogeneity following contralateral acupuncture at Quchi (LI 11) and Zusanli (ST 36) in ischemic stroke patients with left hemiplegia: an fMRI study. Chin J Integr Med. (2020) 26:20–5. doi: 10.1007/s11655-019-3079-6
93. Zou Y, Tang W, Li X, Xu M, Li J. Acupuncture reversible effects on altered default mode network of chronic migraine accompanied with clinical symptom relief. Neural Plast. (2019) 2019:5047463. doi: 10.1155/2019/5047463
94. Takamura T, Hanakawa T. Clinical utility of resting-state functional connectivity magnetic resonance imaging for mood and cognitive disorders. J Neural Transm. (2017) 124:821–39. doi: 10.1007/s00702-017-1710-2
95. Mohr DC, Spring B, Freedland KE, Beckner V, Arean P, Hollon SD, et al. The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychother Psychosom. (2009) 78:275–84. doi: 10.1159/000228248
96. Hasegawa H. Design an Intervention Study. Methods Mol Biol. (2018) 1868:235–41. doi: 10.1007/978-1-4939-8802-0_24
97. Sullivan GM. Getting off the “gold standard:” randomized controlled trials and education research. J Grad Med Educ. (2011) 3:285–9. doi: 10.4300/JGME-D-11-00147.1
98. Gotzsche PC. Is there logic in the placebo? Lancet. (1994) 344:925–6. doi: 10.1016/S0140-6736(94)92273-X
99. Walach H, Loef M. Using a matrix-analytical approach to synthesizing evidence solved incompatibility problem in the hierarchy of evidence. J Clin Epidemiol. (2015) 68:1251–60. doi: 10.1016/j.jclinepi.2015.03.027
100. Thiese MS. Observational and interventional study design types; an overview. Biochem Med. (2014) 24:199–210. doi: 10.11613/BM.2014.022
101. Meyer AM, Wheeler SB, Weinberger M, Chen RC, Carpenter WR. An overview of methods for comparative effectiveness research. Semin Radiat Oncol. (2014) 24:5–13. doi: 10.1016/j.semradonc.2013.09.002
102. Zang YF, He Y, Zhu CZ, Cao QJ, Sui MQ, Liang M, et al. Altered baseline brain activity in children with ADHD revealed by resting-state functional MRI. Brain Dev. (2007) 29:83–91. doi: 10.1016/j.braindev.2006.07.002
103. Zhang Z, Bo Q, Li F, Zhao L, Wang Y, Liu R, et al. Increased ALFF and functional connectivity of the right striatum in bipolar disorder patients. Prog Neuropsychopharmacol Biol Psychiatry. 2020:110140. doi: 10.1016/j.pnpbp.2020.110140
104. Xia J, Fan J, Du H, Liu W, Li S, Zhu J, et al. Abnormal spontaneous neural activity in the medial prefrontal cortex and right superior temporal gyrus correlates with anhedonia severity in obsessive-compulsive disorder. J Affect Disord. (2019) 259:47–55. doi: 10.1016/j.jad.2019.08.019
105. Hu L, Xiao M, Ai M, Wang W, Chen J, Tan Z, et al. Disruption of resting-state functional connectivity of right posterior insula in adolescents and young adults with major depressive disorder. J Affect Disord. (2019) 257:23–30. doi: 10.1016/j.jad.2019.06.057
106. Gong J, Wang J, Qiu S, Chen P, Luo Z, Wang J, et al. Common and distinct patterns of intrinsic brain activity alterations in major depression and bipolar disorder: voxel-based meta-analysis. Transl Psychiatry. (2020) 10:353. doi: 10.1038/s41398-020-01036-5
108. Yu HL, Liu WB, Wang T, Huang PY, Jie LY, Sun JZ, et al. Difference in resting-state fractional amplitude of low-frequency fluctuation between bipolar depression and unipolar depression patients. Eur Rev Med Pharmacol Sci. (2017) 21:1541–50.
109. Okon-Singer H, Hendler T, Pessoa L, Shackman AJ. The neurobiology of emotion-cognition interactions: fundamental questions and strategies for future research. Front Hum Neurosci. (2015) 9:58. doi: 10.3389/fnhum.2015.00058
110. Rota G, Sitaram R, Veit R, Erb M, Weiskopf N, Dogil G, et al. Self-regulation of regional cortical activity using real-time fMRI: the right inferior frontal gyrus and linguistic processing. Hum Brain Mapp. (2009) 30:1605–14. doi: 10.1002/hbm.20621
111. Zeng M, Yu M, Qi G, Zhang S, Ma J, Hu Q, et al. Concurrent alterations of white matter microstructure and functional activities in medication-free major depressive disorder. Brain Imaging Behav. (2020) 411:6. doi: 10.1007/s11682-020-00411-6
112. Liu CH Li F, Li SF, Wang YJ, Tie CL, Wu HY, et al. Abnormal baseline brain activity in bipolar depression: a resting state functional magnetic resonance imaging study. Psychiatry Res. (2012) 203:175–9. doi: 10.1016/j.pscychresns.2012.02.007
113. Friston KJ, Frith CD, Liddle PF, Frackowiak RS. Functional connectivity: the principal-component analysis of large (PET) data sets. J Cereb Blood Flow Metab. (1993) 13:5–14. doi: 10.1038/jcbfm.1993.4
114. Godlewska BR, Browning M, Norbury R, Igoumenou A, Cowen PJ, Harmer CJ. Predicting treatment response in depression: the role of anterior cingulate cortex. Int J Neuropsychopharmacol. (2018) 21:988–96. doi: 10.1093/ijnp/pyy069
116. Hu D, Zhang H, Wu Z, Wang F, Wang L, Smith JK, et al. Disentangled-multimodal adversarial autoencoder: application to infant age prediction with incomplete multimodal neuroimages. IEEE Trans Med Imaging. (2020) 39:4137–49. doi: 10.1109/TMI.2020.3013825
117. Li Z, Zeng F, Yin T, Lan L, Makris N, Jorgenson K, et al. Acupuncture modulates the abnormal brainstem activity in migraine without aura patients. Neuroimage Clin. (2017) 15:367–75. doi: 10.1016/j.nicl.2017.05.013
118. Chae Y. The dilemma of placebo needles in acupuncture research. Acupunct Med. (2017) 35:382–3. doi: 10.1136/acupmed-2017-011394
119. Goddard G, Shen Y, Steele B, Springer N. A controlled trial of placebo versus real acupuncture. J Pain. (2005) 6:237–42. doi: 10.1016/j.jpain.2004.12.009
120. Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. (1998) 352:364–5. doi: 10.1016/S0140-6736(97)10471-8
121. Park J, White A, Stevinson C, Ernst E, James M. Validating a new non-penetrating sham acupuncture device: two randomised controlled trials. Acupunct Med. (2002) 20:168–74. doi: 10.1136/aim.20.4.168
122. Enck P, Benedetti F, Schedlowski M. New insights into the placebo and nocebo responses. Neuron. (2008) 59:195–206. doi: 10.1016/j.neuron.2008.06.030
123. Wager TD, Atlas LY. The neuroscience of placebo effects: connecting context, learning and health. Nat Rev Neurosci. (2015) 16:403–18. doi: 10.1038/nrn3976
124. Geuter S, Koban L, Wager TD. The cognitive neuroscience of placebo effects: concepts, predictions, and physiology. Annu Rev Neurosci. (2017) 40:167–88. doi: 10.1146/annurev-neuro-072116-031132
125. Evers A, Colloca L, Blease C, Annoni M, Atlas LY, Benedetti F, et al. Implications of placebo and nocebo effects for clinical practice: expert consensus. Psychother Psychosom. (2018) 87:204–10. doi: 10.1159/000490354
Keywords: magnetic resonance imaging, acupuncture, depression, treatment, systematic review
Citation: Zhang J, Wu X, Nie D, Zhuo Y, Li J, Hu Q, Xu J and Yu H (2021) Magnetic Resonance Imaging Studies on Acupuncture Therapy in Depression: A Systematic Review. Front. Psychiatry 12:670739. doi: 10.3389/fpsyt.2021.670739
Received: 23 February 2021; Accepted: 12 July 2021;
Published: 20 August 2021.
Edited by:
Yong-Ku Kim, Korea University, South KoreaReviewed by:
Chien-Han Lai, National Yang-Ming University, TaiwanJe-Yeon Yun, Seoul National University Hospital, South Korea
Copyright © 2021 Zhang, Wu, Nie, Zhuo, Li, Hu, Xu and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haibo Yu, MTM2MDMwNjYwOThAMTYzLmNvbQ==; Jinping Xu, anAueHVAc2lhdC5hYy5jbg==
 Jinhuan Zhang
Jinhuan Zhang Xiaoxiong Wu1
Xiaoxiong Wu1