- 1Department of Psychosomatic Medicine and Psychotherapy, University Hospital Tübingen, Tübingen, Germany
- 2Department for Psychosomatic Medicine, Charité Center for Internal Medicine and Dermatology, Corporate Member of Freie Universität Berlin, Berlin Institute of Health, Charité - Universitätsmedizin Berlin, Humboldt-Universität zu Berlin, Berlin, Germany
- 3Department of Internal Medicine 1, University Hospital Tübingen, Tübingen, Germany
- 4German Center for Infection Research (DZIF), Clinical Research Unit for Healthcare Associated Infections, Tübingen, Germany
Introduction
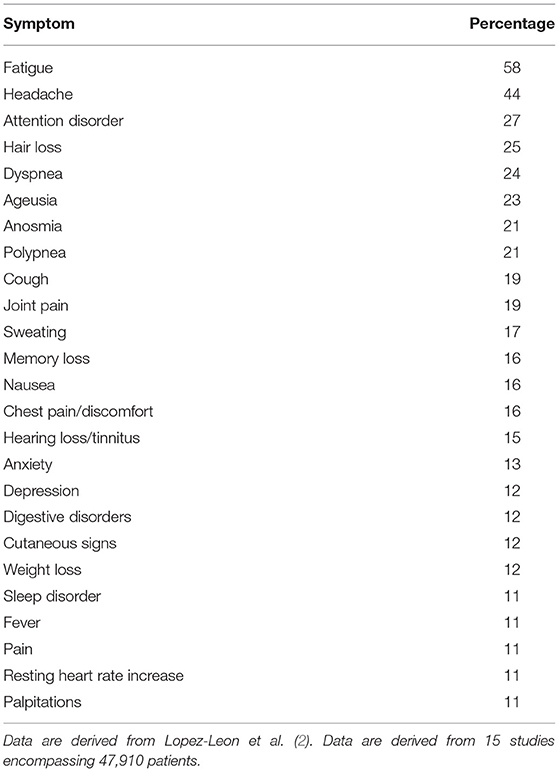
Since the start of the pandemic until now (end of February 2021), more than 113 million people worldwide have been infected (encompassing people with and without symptoms) with SARS-CoV-2, with 89 million of those (78.8%) being classified as recovered (1). However, it became more and more apparent that people infected can have symptoms not only in the acute phase but also with a considerable delay. A recent meta-analysis from 15 studies encompassing 47,910 patients showed that 80% of patients develop at least one symptom during follow–up times ranging from 2 weeks to 4 months post viral infection (2). This condition is termed heterogeneously, namely, long COVID, post-COVID, or recently post-acute sequelae of SARS-CoV2 (PASC). The most common symptoms were fatigue (58%), headache (44%), attention disorder (27%), hair loss (25%), and dyspnea (24%) (Table 1) (2). The long-term outcome of these symptoms remains to be investigated. The current opinion article will discuss the current state of knowledge on the development of long COVID symptoms with a special focus on post-COVID fatigue being the most common symptom.
Discussion
Early on, it was reported that patients after hospitalization due to SARS-CoV-2 infection may develop persistent breathlessness (53%) and cough (34%) during the following months post discharge (3). Among those patients, one third had persistently elevated d-dimer levels; in 10% of patients, the C-reactive protein levels were elevated (3), giving rise to an ongoing inflammatory reaction. This was also reflected in a high percentage (38%) of pathological chest x-rays likely due to active endothelitis/vasculitis as recently discussed (4). Several risk factors for the development of these persistent symptoms have been identified: besides the severity of the initial SARS-CoV-2 infection, higher age, higher body mass index, and pre-existing lung diseases were associated with a greater risk (5).
Interestingly, the majority of these patients described above also reported other symptoms. Two thirds (69%) also complained about fatigue; another 13 and 12% patients showed signs of anxiety and depression, respectively (3). However, another publication showed that fatigue developed irrespective of a preceding hospitalization and was therefore not associated with the severity of the initial SARS-CoV-2 disease (6). Moreover, female sex (7) and previous episodes of depression or anxiety were observed more often in patients developing fatigue (6), which contrasts with the risk factors for the development of the vascular long COVID symptoms. A perceived high level of perceived social stigmatization due to the infection status was associated with an increased risk of developing impaired general mental health post SARS-CoV-2 infection, while a high level of social support showed the opposite association (8).
Patients with fatigue did not show differences in autonomic functions (assessed using electrocardiogram and blood pressure monitoring during deep breathing, active standing, Valsalva maneuver, and cold-pressor testing) compared to subjects that underwent a SARS-CoV-2 infection without developing fatigue (9). This gives rise to a functional origin of the fatigue symptoms.
It is well-known that irritable bowel syndrome (IBS), a highly prevalent (worldwide prevalence around 10–15%) functional gastrointestinal disorder (10), can develop after acute gastroenteritis, also known as post-infectious IBS (11). Symptoms often encompass diarrhea and abdominal pain, being not different from those of a non-post-infectious genesis of IBS (10). Likewise, the treatment does not differ as no persistent inflammatory changes are present that would explain the magnitude of complaints (10). Therefore, also these complaints are classified as functional. The current pathogenetic model explaining the pathogenesis of functional disorders is the biopsychosocial model encompassing biological (e.g., genetic factors) and psycho-social (e.g., life events, acute triggering somatic, or psychological stressors) factors (12). According to the new International Classification of Diseases 11th revision (ICD-11), this will be best categorized as bodily distress disorder, “characterized by the presence of bodily symptoms that are distressing to the individual and excessive attention directed toward the symptoms which may be manifest by repeated contact with health care providers” (13). “Typically, the disorder involves multiple bodily symptoms that may vary over time. Occasionally there is a single symptom—usually pain or fatigue—that is associated with the other features of the disorder” (13).
In summary, a SARS-CoV-2-infection might trigger post-COVID fatigue as a variant of long COVID. Whether this is specific for SARS-CoV-2 or rather a broader risk factor for the development of a functional disease/bodily distress disorder as observed before for, e.g., post-infectious IBS, will have to be further investigated. Moreover, more emphasis should be given to the characterization of risk factors for the development of functional post-COVID symptoms so patients at higher risk can be given higher attention in a personalized approach, screened early, and provided early help to avoid over-diagnosing and iatrogenic somatic fixation. Hereby, the close collaboration of internal medicine practitioners and those specialized in psychosomatic medicine/psychiatry is key to offer treatment in an integrated manner. It is likely that treatments encouraging active participation of patients (e.g., exercise or psychotherapy) might be more effective than passive options (e.g., medication alone) as described for other functional disorders before (14).
Author Contributions
AS prepared the first draft of the article. All authors critically reviewed and finalized the opinion article.
Funding
We acknowledge support by Deutsche Forschungsgemeinschaft and the Open Access Publishing Fund of the University of Tübingen.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. WHO. WHO Coronavirus (COVID-19) Dashboard. Available online at: https://covid19.who.int/ (accessed February 28, 2021).
2. Lopez-Leon S, Wegman-Ostrosky T, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A, et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. medRxiv. (2021). doi: 10.1101/2021.01.27.21250617
3. Mandal S, Barnett J, Brill SE, Brown JS, Denneny EK, Hare SS, et al. 'Long-COVID': a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax. (2020). doi: 10.1136/thoraxjnl-2020-215818. [Epub ahead of print].
4. Sollini M, Ciccarelli M, Cecconi M, Aghemo A, Morelli P, Gelardi F, et al. Vasculitis changes in COVID-19 survivors with persistent symptoms: an [(18)F]FDG-PET/CT study. Eur J Nucl Med Mol Imaging. (2021) 48:1460–6. doi: 10.1007/s00259-020-05084-3
5. Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J Med Virol. (2021) 93:1013–22. doi: 10.1002/jmv.26368
6. Townsend L, Dowds J, O'Brien K, Sheill G, Dyer AH, O'Kelly B, et al. Persistent poor health post-COVID-19 is not associated with respiratory complications or initial disease severity. Ann Am Thorac Soc. (2021). doi: 10.1513/AnnalsATS.202009-1175OC. [Epub ahead of print].
7. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. (2021) 397:220–32. doi: 10.1016/S0140-6736(20)32656-8
8. Qi R, Chen W, Liu S, Thompson PM, Zhang LJ, Xia F, et al. Psychological morbidities and fatigue in patients with confirmed COVID-19 during disease outbreak: prevalence and associated biopsychosocial risk factors. medRxiv. (2020). doi: 10.1101/2020.05.08.20031666
9. Townsend L, Moloney D, Finucane C, McCarthy K, Bergin C, Bannan C, et al. Fatigue following COVID-19 infection is not associated with autonomic dysfunction. PLoS ONE. (2021) 16:e0247280. doi: 10.1371/journal.pone.0247280
10. Enck P, Aziz Q, Barbara G, Farmer AD, Fukudo S, Mayer EA, et al. Irritable bowel syndrome. Nat Rev Dis Primers. (2016) 2:16014. doi: 10.1038/nrdp.2016.14
11. Schwille-Kiuntke J, Mazurak N, Enck P. Systematic review with meta-analysis: post-infectious irritable bowel syndrome after travellers' diarrhoea. Aliment Pharmacol Ther. (2015) 41:1029–37. doi: 10.1111/apt.13199
12. Henningsen P, Zipfel S, Sattel H, Creed F. Management of functional somatic syndromes and bodily distress. Psychother Psychosom. (2018) 87:12–31. doi: 10.1159/000484413
13. First MB, Reed GM, Hyman SE, Saxena S. The development of the ICD-11 clinical descriptions and diagnostic guidelines for mental and behavioural disorders. World Psychiatry. (2015) 14:82–90. doi: 10.1002/wps.20189
Keywords: anxiety, chronic COVID, depression, functional, long covid, post-infectious, psychosomatic, post-acute sequelae of SARS-CoV-2 infection (PASC)
Citation: Stengel A, Malek N, Zipfel S and Goepel S (2021) Long Haulers—What Is the Evidence for Post-COVID Fatigue? Front. Psychiatry 12:677934. doi: 10.3389/fpsyt.2021.677934
Received: 08 March 2021; Accepted: 12 April 2021;
Published: 21 May 2021.
Edited by:
Martin Teufel, University of Duisburg-Essen, GermanyReviewed by:
Hannah Kohler, University of Duisburg-Essen, GermanyCopyright © 2021 Stengel, Malek, Zipfel and Goepel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andreas Stengel, QW5kcmVhcy5zdGVuZ2VsQG1lZC51bmktdHVlYmluZ2VuLmRl
 Andreas Stengel
Andreas Stengel Nisar Malek3
Nisar Malek3 Stephan Zipfel
Stephan Zipfel