- 1Department of Psychiatry, Chonnam National University Medical School, Gwangju, South Korea
- 2Department of Infectious Diseases Medicine, Chonnam National University Medical School, Gwangju, South Korea
- 3King's College London, Institute of Psychiatry, Psychology and Neuroscience, London, United Kingdom
- 4South London and Maudsley NHS Foundation Trust, London, United Kingdom
Background: Hospital isolation for COVID-19 may cause significant psychological stress. The association between COVID-19 symptoms and psychological symptoms has not been systematically studied. We investigated the effects of telephonic intervention on the relationship between psychological symptoms and COVID-19 symptoms at the time of hospitalization and 1 week later.
Method: We screened 461 patients with COVID-19 for psychiatric symptoms from February 29, 2020, to January 3, 2021. In total, 461 patients were evaluated 2 days after admission, and 322 (69.8%) were followed 1 week later. To assess anxiety and depressive symptoms, the Hospital Anxiety and Depression Scale (HADS) was administered to patients once per week. The Insomnia Severity Index (ISI) and item 9 of the Beck Depression Inventory (BDI-9) were used weekly to assess insomnia and suicidal ideation.
Results: Of 461 enrolled patients, we observed clinically meaningful psychological anxiety symptoms (in 75/16.3% of patients), depression (122/26.5%), insomnia (154/33.4%), and suicidal ideation (54/11.7%). Commonly reported COVID-19 symptoms are cough/sputum/sneezing (244, 52.9%), headache/dizziness (98, 21.3%), myalgia (113, 24.5%), and sore throat (89, 19.3%). Compared to baseline, significant improvements were found in anxiety, depression, and suicidal ideation at 1 week. No significant group differences in ISI score were observed.
Conclusions: COVID-19 symptoms at baseline had a significant and persistent negative impact on anxiety and depression at admission and at 1 week after hospitalization. Early intervention is essential to improve the outcomes of patients with mental illness.
Introduction
The World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) outbreak a pandemic on March 12, 2020 (1). Given the high contagion of COVID-19, many countries have adopted restrictive measures such as quarantines, lockdowns, and restrictions on movement and travel to contain the transmission. These can cause considerable psychological tension and difficulties in the general population (2). Psychological responses to infectious diseases include maladaptive behavior, emotional distress, and defensive reactions (3). In addition, previous studies have shown that inpatients with psychiatric problems have worse treatment outcomes and longer hospital stays (4, 5). Patients hospitalized for COVID-19 treatment face mental health issues of social isolation, loneliness, anxiety, depression, phobias, fear of disease progression, and insufficient resources at the time of admission (6). During hospitalization, patients continue to experience additional stresses related to COVID-19, creating new psychological problems that were not reported at the time of admission. In a meta-analysis of a recent studies of COVID-19 patients (including hospitalized and non-hospitalized patients), the prevalence of depression, anxiety, and sleep disorders was 45, 47, and 34%, respectively (7). Research on COVID-19 inpatients with psychiatric issues found that a considerable proportion of these patients reported depression (22.9–60.2%), anxiety (20.8–55.3%), and posttraumatic stress symptoms (96.2%) (8–12). However, these studies of psychological problems were single-timepoint investigations based on psychiatric assessments administered at difference timepoints, and they therefore provide only a snapshot of changing psychological symptoms.
The spectrum of COVID-19 symptom ranges from asymptomtic to critical; most infections are not severe (13, 14). Previous studies suggest that COVID-19 may affect the central nervous system through the associated inflammatory immune response and pharmacological drugs that are administered (15, 16). A chart review of hospitalized patients with COVID-19 (n = 214) found that central nervous system manifestations (e.g., dizziness, headache, or impaired cognition) occurred in 25% (17). However, the association between COVID-19 symptoms and psychological symptoms has not been systematically studied. Treatment is more difficult when physical diseases and mental problems are combined (18). Experts have underscored the need to provide psychological treatment for patients from the beginning of their isolation to minimize the impact of emotional distress. However, multidisciplinary care has not been available due to increased rates of infection and underestimates of the need for psychological intervention. Overall, acute COVID-19-related medical concerns and hospitalizations have increased the need for psychiatric approaches, but intervention has been limited.
Evidence-based interventions for psychological symptoms targeted at COVID-19 patients are scarce. Anmella et al. presented four clinical cases (delirium, psychotic symptom, anxiety, and depression) in COVID-19 inpatients and reported on the use of psychotropic medications to control psychiatric symptoms. However, it is difficult to generalize their results due to limitations of their study design. Recent research has focused on the use of online or telephonic psychological interventions to reduce the risk for infection-related emotional distress in COVID-19 (19, 20). However, the sample sizes have been relatively small, which limits the ability to detect real effects. Previously, we reported the results of telephone interventions with 33 COVID patients isolated in hospitals (20). Here, we used telephone interviews to evaluate psychological symptoms in COVID-19 patients at the time of hospitalization and 1 week thereafter (before discharge). The purpose of the telephone intervention was to provide education, empathy, encouragement, reassurance, and suggestions to quarantined COVID-19 patients, to reduce psychological symptoms and facilitate their adaptation to the ward environment. We also investigated the effects of telephonic interventions on the relationship between psychological symptoms and COVID-19 symptoms at the time of hospitalization and 1 week later.
Methods
Study Outline
The Korean government classifies COVID-19 cases by severity to place priority on treating more severe cases at hospitals, while asymptomatic to mild cases receive medical treatment and monitoring at residential treatment centers. Patients who display COVID-19 symptoms receive conservative treatment and are discharged after clinical and testing criteria have been met. During the pandemic period, we developed a consultation network for patients with confirmed COVID-19 who were admitted to both types of hospital after consulting the infectious disease and psychiatry departments. Participants were consecutively recruited from hospitalized patients with COVID-19 at the Department of Infectious Diseases, Chonnam National University Bitgoeul Hospital (CNUBH), and Chonnam National University Hospital (CNUH), Gwangju, South Korea. The recruitment process is presented in Figure 1. Patients were screened at the time of hospitalization and 1 week thereafter (before discharge) using psychological scales related to anxiety, depression, suicidal ideation, and insomnia. The follow-up evaluation was performed 7.01 ± 0.8 days after the initial evaluation. After obtaining information on the scale scores, the study psychiatrists accessed the patients by telephone.
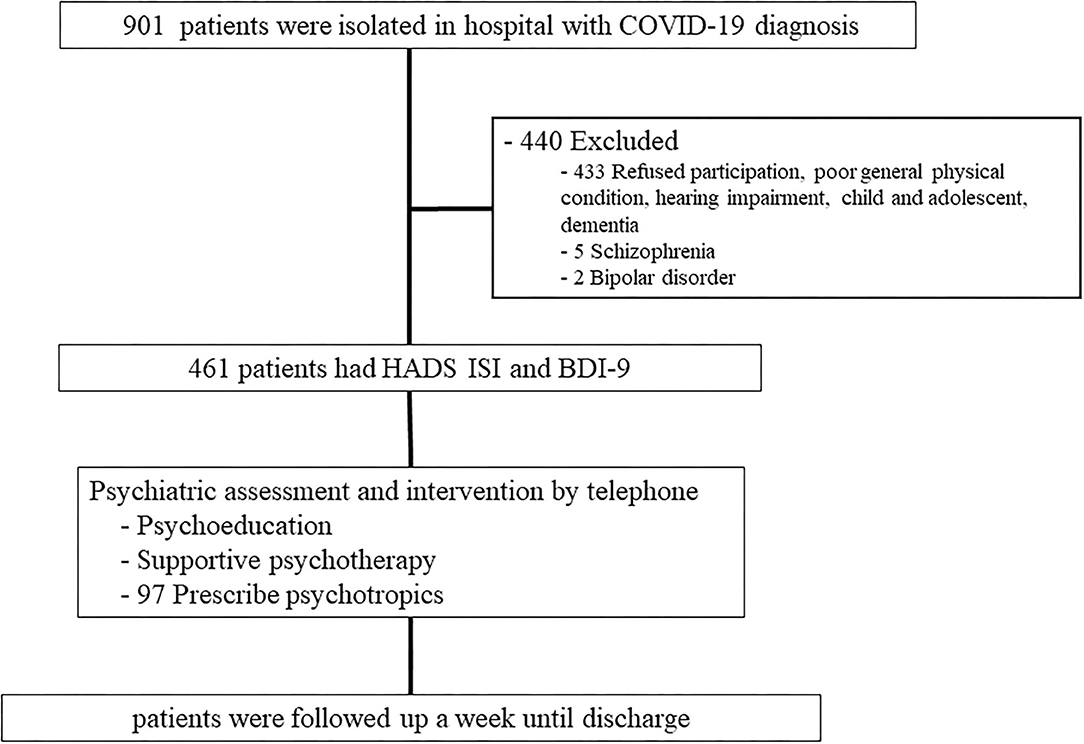
Figure 1. Flow chart of the study. HADS-A, Hospital Anxiety and Depression Scale- Anxiety; HADS-D, Hospital Anxiety and Depression Scale- Depression, ISI, Insomnia Severity Index; BDI, Beck Depression Inventory.
Participants
Criteria for inclusion were as follows: a history of COVID-19 infection according to reverse-transcription polymerase chain reaction (RT-PCR) assay and hospitalization at CNUBH or CNUH for treatment of COVID-19 infection. Patients with severe communication problems (e.g., deafness, dementia, cognitive delay) were excluded. We screened 461 patients with COVID-19 for psychiatric symptoms from February 29, 2020, to January 3, 2021. This retrospective study strictly followed the code of ethics enforced by the Institutional Review Board of Chonnam National University Hospital (IRB No. CNUH-2021–020, IRB No. CNUH-2020–100). Written informed consent was waived by the ethics committee of the designated hospital for emerging infectious diseases.
Measurement and Assessment of Psychiatric Symptoms
Psychiatric assessment was performed 2.04 ± 0.8 days after admission. The Hospital Anxiety and Depression Scale (HADS) was used to determine anxiety and depressive symptoms (21). The HADS was created to assess patients with a physical comorbidity using two seven-item subscales that evaluate depression and anxiety. A score of 8 was used as the cutoff point for each subscale to reflect a mild level of distress. The Insomnia Severity Index consist of seven questions assessing the impact of insomnia with a total score ranging from 0 to 28; a score of 8 was used as the cutoff point indicating a certain level of insomnia (22). Item 9 of the Beck Depression Inventory-II, which addresses suicidal thoughts or wishes, has a four-level response set. Suicidal ideation was considered present with a score ≥1 (23). The HADS, ISI and BDI-II were formerly translated and standardized in Korean (24–26). It was designated as creating a psychological difficulty due to COVID-19 when patients endorsed at least one question indicating depression, anxiety, insomnia, or suicidal ideation.
Assessment of COVID-19 Symptoms and Clinical Characteristics
Clinical charts and nursing records were reviewed to investigate the absence/presence of COVID-19 symptoms. Clinical presentations of COVID-19 differ substantially and can include a range from asymptomatic infection through mild upper respiratory tract illness to severe viral pneumonia (27, 28). Although some clinical features (particularly smell or taste disorders) are more common with COVID-19 than with other viral respiratory infections (28), COVID-19 has no specific symptoms or signs. We investigated the presence or absence of nausea/anosmia/anorexia, headache/dizziness, fever/chills, chest discomfort/dyspnea, cough/sputum/sneezing, diarrhea, myalgia, and sore throat including symptoms from pre-hospital to psychological assessment. Individualized treatment strategies were used according to severity and the clinical setting. Severe COVID-19 was defined by the use of therapeutic drugs (steroid, antibiotics, and antiviral agents) excluding symptomatic drug use (29). C-reactive protein (CRP) was measured on the first day of hospitalization and within ±2 days. Sociodemographic data were collected on age, sex, alcohol, smoking, employment status, past medical history, and past psychiatric history.
Psychological Intervention
Participants were approached about participating in the psychological intervention program, details of which are presented in Supplementary Table 1. Briefly, psychological interventions were performed at baseline and then once or twice per week until discharge. As a non-face-to-face intervention, telephone sessions with isolated patients focused more on psychoeducation to produce short-term effects. Beginning at admission, patients should be given sufficient information about the psychological effects of infectious diseases and isolation to reduce excessive fear. In addition, therapists can correct patients' inappropriate cognitive appraisals to reduce distress. To reduce the shortcomings of telephone access, psychiatrists implemented a telephone connection to the ward where the patients were hospitalized. By doing so, it was possible to collaborate for evaluation and treatment by sharing patients' information with the treatment team. For all patients admitted to the hospital, mental health guidelines that patients should know when in isolation were distributed. For patients who agreed to psychological intervention, a psychiatrist evaluated and counseled them twice a week for 5–30 min. Psychotropic medications were allowed if needed. Before and after the interventions, the patient's information was shared between the psychiatrists and medical treatment team to facilitate collaborative care.
Follow-Up Evaluations for Psychiatric Symptoms
Each scale was administered once a week from the initial evaluation until discharge. After reviewing the scores on these scales, the psychiatrist provided treatment over the phone (routine follow-up, evaluation of psychological symptoms appearing after hospitalization, counseling regarding psychological problems, prescription of psychotropic medication, crisis intervention) according to the patient's symptoms.
Statistical Analyses
Summary statistics are presented as means and standard deviations for continuous variables and as numbers and percentages for discrete variables. The demographic and clinical characteristics at baseline were compared by the presence or absence of COVID-19 symptoms using the t-test or the chi-square (χ2) test, as appropriate. The χ2 test was used to assess associations between sex or age and each scale score as a continuously distributed dependent variable. Suicidal ideation on follow-up was compared to baseline using a binomial exact test. Finally, the associations between COVID-19 symptoms and changes in psychological scales over 1 week were assessed using repeated-measures analysis of variance (ANOVA) in the same adjusted model. Statistical significance for all tests was set at p < 0.05. All statistical analyses were carried out using SPSS 23.0 software (IBM Corp., Armonk, NY, USA).
Results
Demographic and Clinical Characteristics
Of the initial 901 patients who were admitted for treatment of COVID-19, 461 subjects (192 male, mean age 50.42 ± 16.7, range 18–87 years) agreed to the psychological intervention described herein; their baseline sociodemographic and clinical characteristics are summarized in Table 1. At follow-up, 322 (69.8%) participants were reexamined. The mean duration of hospitalization was 12.5 days (±5.3). The remaining 139 (30.2%) patients were unable to complete the 1-week evaluation due to deterioration in COVID-19 symptoms, transfer to another hospital, or discharge from the hospital. Baseline HADS (D) scores were significantly lower in patients without than in patients with follow-up (5.2 ± 3.3 vs. 5.9 ± 4.0, P = 0.032). Fever was significantly less common in patients without than in patients with follow-up (38.5 vs. 24.5%). Otherwise, there were no substantial differences in any characteristics between participants who were and those who were not followed up (all p > 0.05).
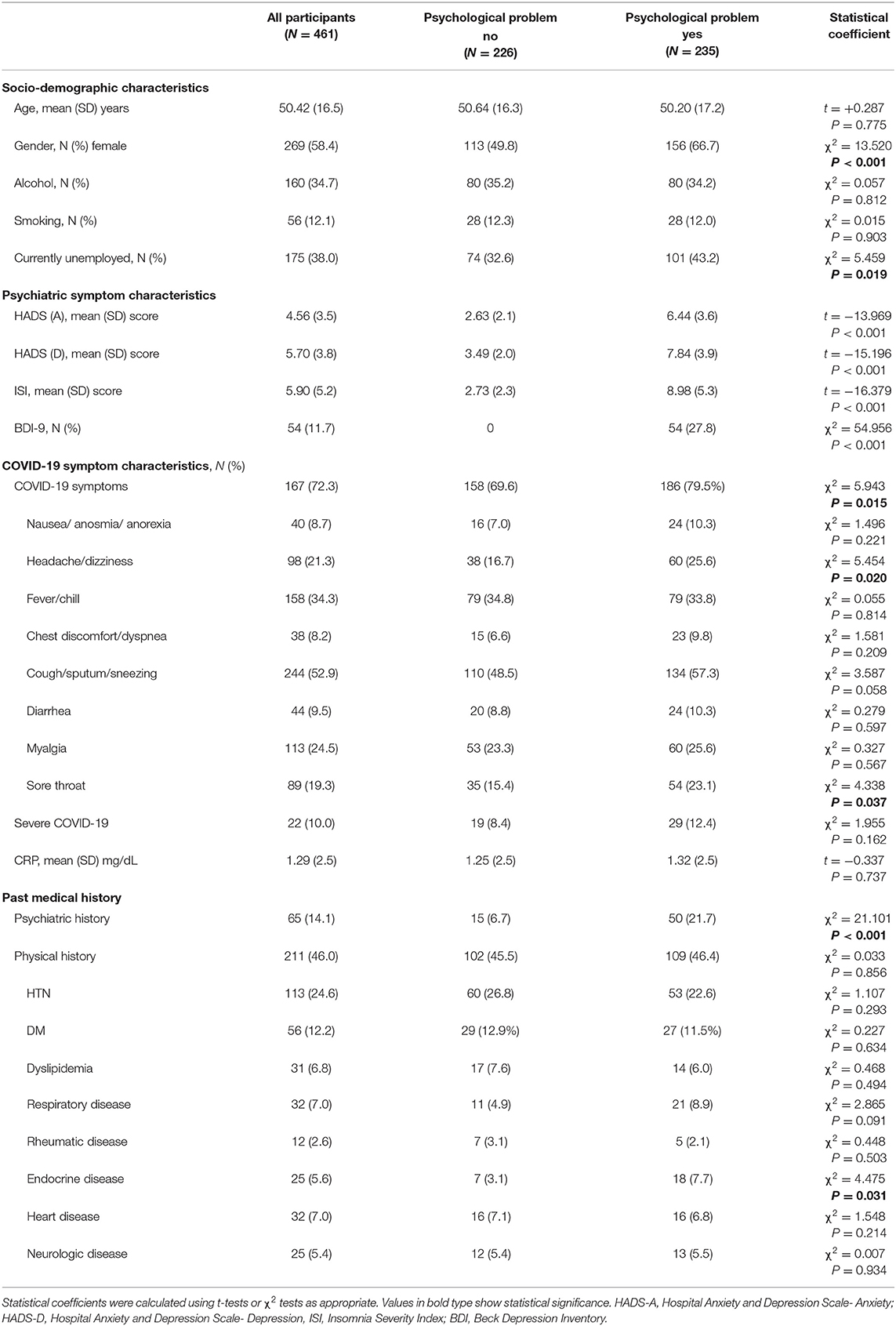
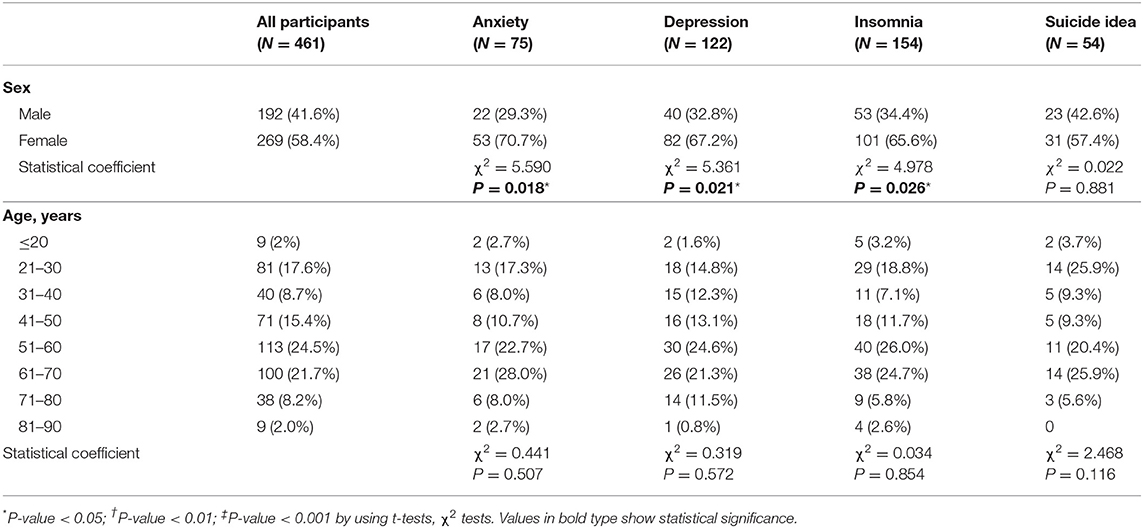
Table 1. Baseline characteristics by common mental health problem as assessed using the HADS, BDI-9, and ISI at admission after COVID-19.
Associations of COVID-19 Symptoms and Psychological Symptoms at Baseline
At the time of admission, the following clinically meaningful psychological symptoms were found: anxiety in 75 (16.3%) patients, depression in 122 (26.5%), insomnia in 154 (33.4%), and suicidal ideation in 54 (11.7%). Commonly reported COVID-19 symptoms were cough/sputum/sneezing (244, 52.9%), headache/dizziness (98, 21.3%), myalgia (113, 24.5%), and sore throat (89, 19.3%). The group with psychological symptoms (N = 235, 50.1%) were more likely to be female and jobless, to have COVID-19 symptoms of headache/dizziness and sore throat, to have a previous psychiatry history, and to have a diagnosis of previous endocrine disease. There were no significant differences between the groups in terms of alcohol use, smoking, CRP level, and severe COVID-19 status. Table 2 shows comparisons of anxiety, depression, insomnia, and suicidal ideation scale scores according to the absence/presence of COVID-19 symptoms. Baseline HADS (A) and HADS (D) scores were significantly higher in patients with COVID-19 symptoms, but the baseline ISI score did not differ significantly. There were no significant differences between the groups in BDI-9. Psychological symptoms at the time of admission according to age and sex are presented in Table 3. Women were more likely to have anxiety and depression symptoms than men (70.7 vs. 29.3%, 67.2 vs. 32.8%, respectively). There were no significant differences in psychological symptoms by age.
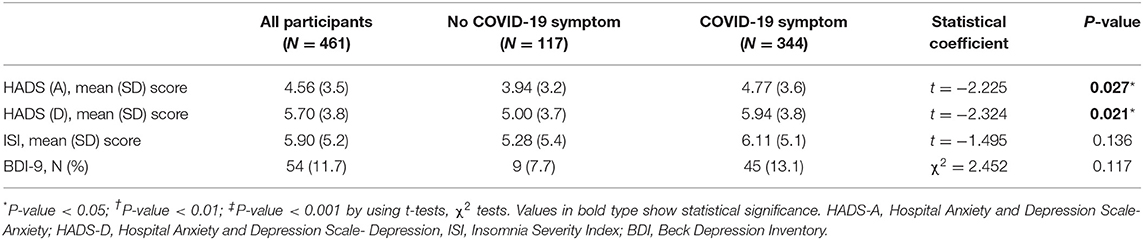
Table 2. Comparison of anxiety depression insomnia suicidal ideation among patients with/without COVID-19 symptoms.
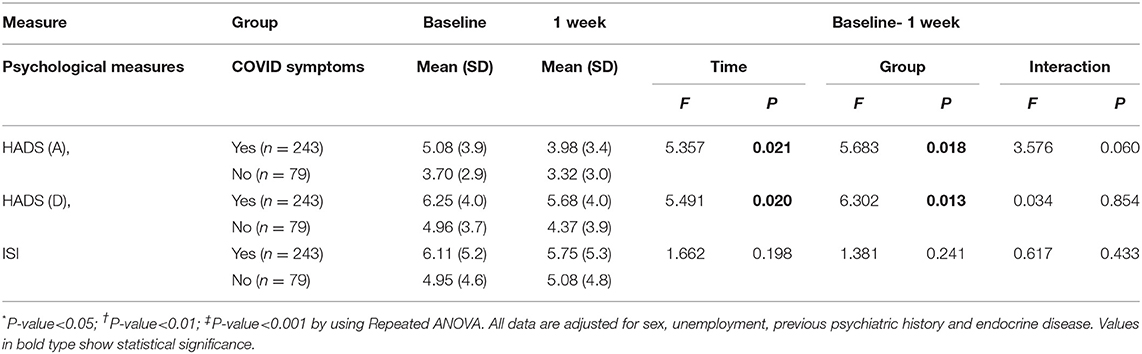
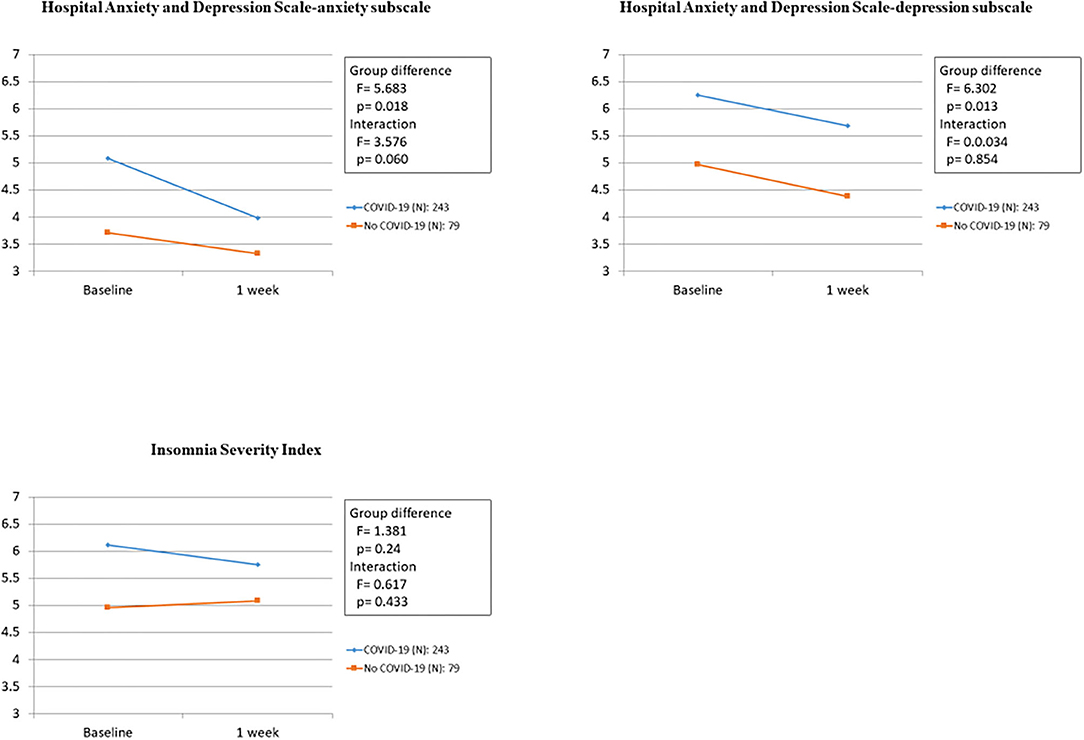
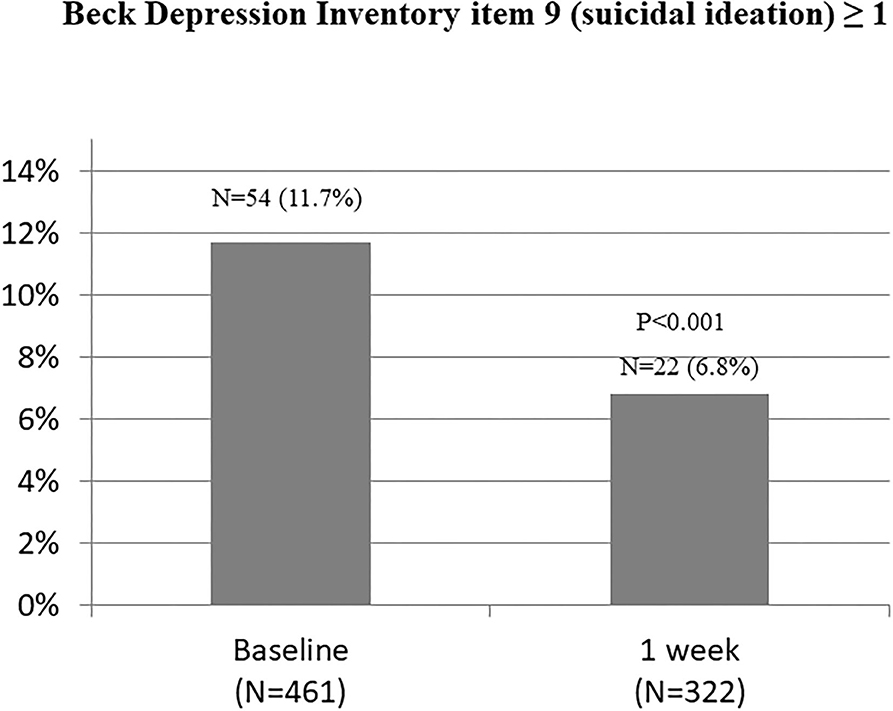
Associations Between COVID-19 Symptoms and Psychological Symptoms at 1 Week
The associations between COVID-19 symptoms during admission and changes in the HADS (A), HADS (D), and ISI scores over 1 week in the 322 participants who completed the follow-up evaluation are shown in Table 4 and Figure 2. Compared to baseline, significant improvements were found in HADS (A) and HADS (D) scores at 1 week (P = 0.021 and P = 0.020, respectively). Changes in the HADS (A) and HADS (D) scores showed significant group differences after adjusting for sex, employment status, history of psychiatric problem, and history of endocrine disease. No significant group differences were observed for ISI scores. There was no significant group × time interaction for changes in the HADS (A), HADS (D), and ISI scores after adjusting for sex, employment status, previous history of psychiatric problems, and rheumatic disease. Figure 3 shows the changes in suicidal ideation between baseline and 1 week. Compared to baseline, significant improvements were found in suicidal ideation at 1 week. The impacts of psychiatric and physical comorbidities on the HADS (A), HADS (D), and ISI scores are shown in Supplementary Table 2. Changes in the HADS (A), HADS (D), and ISI scores showed significant time, group, and group × time interaction effects after adjusting for confounding variables. Participants with these comorbidities showed significantly greater decreases on various psychological measures.
Discussion
The principal findings of this study indicate that psychological symptoms at baseline in COVID-19 patients are associated with female sex, lack of employment, previous psychiatric history and endocrine disease, headache/dizziness, sore throat, and the presence of COVID-19 symptoms. Moreover, the presence of such symptoms at baseline had a significant and persistent negative impact on anxiety and depression at admission and at 1 week after hospitalization.
The overall prevalence of depression, anxiety, sleep disturbances, and suicidal ideation among COVID-19 inpatients was 16.3, 26.5, 33.4, and 11.7%, respectively. The prevalence of depression, anxiety, insomnia, and suicide assessed at 1 week after hospitalization was 13.9, 27.6, 29.3, and 6.8%, respectively. Current evidence on the prevalence of mental illness in COVID-19 inpatients varies widely among studies. Previous studies have reported that a considerable proportion of patients exhibit depression (22.9–60.2%), anxiety (20.8–55.3%), and sleep disturbance (34%, CI: 19–50%) (7–12). The reasons for the difference in prevalence among studies are numerous. First, the screening tools used to assess psychological symptoms have a significant impact on the outcome prevalence values. For example, regarding depression assessment, PHQ-9 (with a cutoff of ≥5) showed similar prevalence rates at 52–53%. However, this prevalence estimate is substantially higher than the prevalence indicated by HADS-D at a cutoff of ≥8, which estimated the prevalence at 19–20% (7). Second, the prevalence depends on the current status of COVID-19 in the country where the study was conducted. The mortality rate and prevalence of COVID-19 affect people's psychology. In a recent psychological evaluation of COVID-19 inpatients in Bangladesh, the prevalence of depression and anxiety was reported as 87.3 and 55.7%, respectively (30). Third, it seems that differences in the time point of psychological evaluations in each study have an effect on the results. Patients were invited to participate in some studies at any time prior to discharge, whereas other papers failed to report the study participation process.
Psychological difficulties in the early phase of COVID-19 were associated with female sex, unemployed status, previous psychiatric history, endocrine disease, headache/dizziness, sore throat, and presence of COVID-19 symptoms. Unemployment, a risk factor that has not yet been investigated in COVID-19 patients, is likely a marker of low socioeconomic status, which is associated with a higher prevalence of depression (31). A psychiatric history is a risk factor for mental disorders such as depression, anxiety disorders, and schizophrenia. In this study, among patients hospitalized for COVID-19, those with a psychiatric history experienced psychological difficulties in the early stages of hospitalization (32, 33). We also found that females were at higher risk for psychological symptoms, which is consistent with previous findings that females were more susceptible to stress-related mental disorders, including depression in COVID-19 inpatients than males (11). The higher prevalence of depression in women is associated with hormonal changes and genetic loadings (34, 35). In general, dysregulation of the endocrine system, such as the thyroid and the hypothalamic–pituitary–adrenal axis, can lead to neuropsychiatric problems (32, 36). Considering these factors, patients with endocrine disorders may experience irregular and unpredictable mental states in early stages of COVID-19. Our results suggest that patients with endocrine disorders are more likely to have psychological problems when infected with COVID-19. However, because the number of patients with endocrine disorders in our study was small, follow-up studies related to this question should be performed. There is a significant association between the prevalence of physical symptoms and psychological distress among health-workers in a pandemic, which is probably bi-directional (37). However, the association between COVID-19 symptoms and psychological symptoms has not been systematically studied. Our research shows that the presence of COVID-19 symptoms is associated with the prevalence of psychological symptoms. In particular, among several COVID-19 symptoms, headache/dizziness and sore throat were associated with psychological symptoms. Furthermore, the presence of COVID-19 symptoms at baseline had a significant and persistent negative impact on anxiety and depression at admission and 1 week after hospitalization. It is also noteworthy that the emergence of symptoms at the time of hospitalization is greater when psychiatric and physical symptoms are present. These results suggest that the presence or absence of COVID-19 symptoms and degree of recovery also affect patient psychology. In the future, research on the mechanism by which these somatic symptoms affect patient psychology should be conducted.
Hospitalized patients who have been diagnosed with COVID-19 are vulnerable to mental health problems (8–12). Patients who are subjected to activity limitations, interpersonal disconnection, economic difficulties, and inadequate supplies while confined to a small hospital room may suffer from distress, including loneliness, disconnection, and anxiety. Furthermore, frustration and anger may increase as patients experience disappointment when their initial expectations are not met and they are forced to deal with long hospital stays and other people's negative responses to their COVID-19 infection. In summary, as the problems experienced by patients vary widely and change over time, it is crucial to evaluate changes in patients' conditions. Moreover, targeted multidisciplinary interventions are needed to support inpatients with COVID-19 by simultaneously addressing both the infectious disease and the psychological symptoms during hospitalization. We developed a consultation network for telephone intervention with COVID-19 patients. We found that telephone-based interventions significantly reduced psychological distress (anxiety, depression, suicidal ideation), except for insomnia, during the first week of hospitalization. The insomnia intervention was probably ineffective because the environment of isolation continues to have a negative impact. Activity restrictions, sudden changes in the sleep environment, and sharing space with other patients seem to be sufficient to induce insomnia in patients. Research and evidence-based guidelines targeting insomnia in inpatients with COVID-19 are needed.
One important consideration when treating patients by telephone involves allowing sufficient time for a thorough evaluation while not interfering with patients' other treatment modalities. To this end, mental health professionals and other members of the treatment team should share information to facilitate collaborative care. Such collaboration reduces unnecessary contact with the patient and enables mental health professionals to obtain information that is difficult to collect by telephone. In addition, the shortage of assessment time can be offset using appropriate psychometric measures. The Hospital Anxiety and Depression Scale, Insomnia Severity Index, and Beck Depression Inventory (item 9) are considered suitable brief evaluations of anxiety, depression, insomnia, and suicidal thoughts (18–21). When administered to patients isolated with COVID-19, these measures identify boredom, loneliness, anxiety, and insomnia due to hospitalization. However, therapists should further evaluate other psychological symptoms (e.g., guilt, anger, impulsivity, frustration, and so forth) that are not assessed by these formal measures. Patients with COVID-19 have reported feeling guilty and ruminating about whether they have infected their loved ones or others. Furthermore, human rights violations, which have frequently been cited in discussions of Korea's COVID-19 response, have been a major stressor for isolated patients. The exposure of personal information, including behavior prior to hospitalization, often angers and frustrates patients. Thus, therapists should evaluate psychological changes that cannot be evaluated by formal scales.
Limitations of this study were as follows. First, the findings are limited by the one-arm design and the single study site. This may limit the generalizability of the findings, although it facilitates consistency of evaluation and treatment. Findings were also drawn exclusively from a Korean population, and replication is needed in other ethnic groups. Second, our study, which did not include a control group, was unable to differentiate between the effectiveness of telephone based interventions and direct face-to-face interventions. However, we found that telephone-based interventions significantly reduced psychological discomfort in the first week of hospitalization. Third, a semi-structured interview method was not used in this study to evaluate psychological distress, although a semi-structured psychological intervention protocol was employed, as detailed in Supplementary Table 1. Due to the limited timeframe of this study, only one item of the BDI-II was used to evaluate suicide. In the future, it will be important to evaluate suicide in hospitalized patients with COVID-19 using a structured scale. Finally, research on mental health aspects of COVID-19 is still lacking, particularly in terms of the variables that can influence mental health outcomes.
Conclusion
COVID-19 survivors may have a significantly higher rate of psychiatric problems (38). Early intervention is essential to improve outcomes in patients with mental illness. It is necessary to understand not only COVID-19 treatment but also its psychosocial effects. During the COVID-19 outbreak, patients isolated in hospitals manifest risk factors for, and symptoms of, psychosocial problems. Therefore, various intervention strategies are recommended to manage psychological problems in these patients.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by IRB No. CNUH-2021–020, IRB No. CNUH-2020–100. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
J-WK and J-MK had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. S-WK and J-MK study concept and design. J-WK, S-JK, and S-IJ acquisition of data. J-WK, H-JK, RS, S-WK, and J-MK analysis and interpretation of data. J-WK and J-MK drafting of the manuscript. J-WK, RS, S-JK, S-IJ, S-WK, and J-MK critical revision of the manuscript for important intellectual content. J-WK, RS, S-WK, and J-MK statistical analysis. J-MK obtained funding. J-WK, MJ, SR, J-YL, and I-SS administrative, technical, or material support. S-WK and J-MK study supervision. All authors contributed to the article and approved the submitted version.
Funding
The study was funded by a grant of National Research Foundation of Korea Grant (NRF- 2019M3C7A1031345) and was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and future Planning (NRF- 2020R1A2C2003472). RS is part-funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at the South London and Maudsley NHS Foundation Trust and King's College London.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.721532/full#supplementary-material
References
1. World Health Organization. Available online at: https://www.who.int/emergencies/diseases/novelcoronavirus-2019/events-as-they-happen (accessed June 29, 2020).
2. Ryu SH, Park IH, Kim MN, Lee YR, Lee JH, Kim HN, et al. Network study of responses to unusualness and psychological stress during the COVID-19 outbreak in Korea. PLoS ONE. (2021) 16:e0246894. doi: 10.1371/journal.pone.0246894
3. Taylor S. The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease. Newcastle upon Tyne, Cambridge Scholars Publishing. (2019).
4. Dennis M, Kadri A, Coffey J. Depression in older people in the general hospital: a systematic review of screening instruments. Age Ageing. (2012) 41:148–54. doi: 10.1093/ageing/afr169
5. Kim JM, Stewart R, Lee YS, Lee HJ, Kim MC, Kim JW, et al. Effect of Escitalopram vs placebo treatment for depression on long-term cardiac outcomes in patients with acute coronary syndrome: a randomized clinical trial. JAMA. (2018) 320:350–8. doi: 10.1001/jama.2018.9422
6. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
7. Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. (2021) 1486:90–111. doi: 10.1111/nyas.14506
8. Paz C, Mascialino G, Adana-Díaz L, Rodríguez-Lorenzana A, Simbaña-Rivera K, Gómez-Barreno L, et al. Anxiety and depression in patients with confirmed and suspected COVID-19 in Ecuador. Psychiatry Clin Neurosci. (2020) 74:554–5. doi: 10.1111/pcn.13106
9. Bo H-X, Li W, Yang Y, Wang Y, Zhang Q, Cheung T, et al. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. (2020) 27:1–2. doi: 10.1017/S0033291720000999
10. Zhang J, Lu H, Zeng H, Zhang S, Du Q, Jiang T, et al. The differential psychological distress of populations affected by the COVID19 pandemic. Brain Behav Immun. (2020) 87:49–50. doi: 10.1016/j.bbi.2020.04.031
11. Guo Q, Zheng Y, Shi J, Wang J, Li G, Li C, et al. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav Immun. (2020) 88:17–27. doi: 10.1016/j.bbi.2020.05.038
12. Ma YF, Li W, Deng HB, Wang L, Wang Y, Wang PH, et al. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J Affect Disord. (2020) 275:145–8. doi: 10.1016/j.jad.2020.06.033
13. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
14. Chan JF, Yuan S, Kok KH, To KKW, Chu H, yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. (2020) 395:514–23. doi: 10.1016/S0140-6736(20)30154-9
15. Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P. Fusar-poli P, Znadi MS, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. (2020) 7:611–27. doi: 10.1016/S2215-0366(20)30203-0
16. Romero-Sánchez CM, Díaz-Maroto I, Fernández-Díaz E, Sánchez-Larsen Á, Layos-Romero A, García-García J, et al. Neurologic manifestations in hospitalized patients with COVID-19: The ALBACOVID registry. Neurology. (2020) 95:e1060. doi: 10.1212/WNL.0000000000009937
17. Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. (2020) 77:683–90. doi: 10.1001/jamaneurol.2020.1127
18. Sartorius N. Comorbidity of mental and physical diseases: a main challenge for medicine of the 21st century. Shanghai Arch Psychiatry. (2013) 25:68–9. doi: 10.3969/j.issn.1002-0829.2013.02.002
19. Wei N, Huang B-C, Lu SJ, Hu JB, Zhou XY, Hu CC, et al. Efficacy of internet-based integrated intervention on depression and anxiety symptoms in patients with COVID-19. J Zhejiang Univ Sci B. (2020) 21:400–4. doi: 10.1631/jzus.B2010013
20. Kim JW, Stewart R, Kang SJ, Jung SI, Kim SW, Kim JM. Telephone based interventions for psychological problems in hospital isolated patients with COVID-19. Clin Psychopharmacol Neurosci. (2020) 18:616–20. doi: 10.9758/cpn.2020.18.4.616
21. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
22. Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
23. Beck AT, Ward CH, Mendelson M, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. (1961) 4:561–471. doi: 10.1001/archpsyc.1961.01710120031004
24. Oh SM, Min KJ, Park DB A. study on the standardization of the hospital anxiety and depression scale for Koreans: a comparison of normal, depressed and anxious groups. J Korean Neuropsychiatr Assoc. (1999) 38:289–96.
25. Lim S-U, Lee E-H, Hwang S-T, Hong S-H, Kim J-H. The Beck Depression Inventory-Second Edition: Psychometric properties in Korean adult populations. Korean Journal of Clinical Psychology. (2019) 3:300–7. doi: 10.15842/kjcp.2019.38.3.003
26. Cho YW, Song ML, Morin CM. Validation of a Korean version of the insomnia severity index. J Clin Neurol. (2014) 10:210–5. doi: 10.3988/jcn.2014.10.3.210
27. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. (2020) 395:507–13. doi: 10.1016/S0140-6736(20)30211-7
28. Zayet S, Kadiane-Oussou NJ, Lepiller Q, Zahra H, Royer PY, Toko L, et al. Clinical features of COVID-19 and influenza: a comparative study on Nord Franche-Comte cluster. Microbes Infect. (2020) 22:481–8. doi: 10.1016/j.micinf.2020.05.016
29. National Institutes of Health. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. https://covid19treatmentguidelines.nih.gov/ (accessed on February 08, 2021).
30. Hasan MJ, Tabssum T, Ambia NE, Zaman MS, Rahman M, Khan AS. Mental health of the COVID-19 patients in Bangladesh. Mymensingh Med J. (2021) 30:189–95.
31. Freeman A, Tyrovolas S, Koyanagi A, Chatterji S, Leonardi M, Ayuso-Mateos JL, et al. The role of socio-economic status in depression: results from the COURAGE (aging survey in Europe). BMC Public Health. (2016) 16:1098. doi: 10.1186/s12889-016-3638-0
32. Yehuda R, Hoge CW, McFarlane AC, Vermetten E, Kanius RA, Nievergelt CM, et al. Post-traumatic stress disorder. Nat Rev Dis Primers. (2015) 1:15057. doi: 10.1038/nrdp.2015.57
33. Wiseman TA, Curtis K, Lam M, Foster K. Incidence of depression, anxiety and stress following traumatic injury: a longitudinal study. Scand J Trauma Resusc Emerg Med. (2015) 23:29. doi: 10.1186/s13049-015-0109-z
34. Marrocco J, McEwen BS. Sex in the brain: hormones and sex differences. Dialogues Clin Neurosci. (2016) 18:373–83. doi: 10.31887/DCNS.2016.18.4/jmarrocco
35. Kang HJ, Park YM, Yoo KH, Kim KT, Kim ES, Kim JW, et al. Sex differences in the genetic architecture of depression. Sci Rep. (2020) 10:9927. doi: 10.1038/s41598-020-66672-9
36. Loh HH, Lim LL, Yee A, Loh HS. Association between subclinical hypothyroidism and depression: an updated systematic review and meta-analysis. BMC Psychiatry. (2019) 19:12. doi: 10.1186/s12888-018-2006-2
37. Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
Keywords: depression, anxiety, COVID-19 inpatients, insomnia, suicide idea
Citation: Kim J-W, Kang H-J, Jhon M, Ryu S, Lee J-Y, Kang S-J, Jung S-I, Shin I-S, Kim S-W, Stewart R and Kim J-M (2021) Associations Between COVID-19 Symptoms and Psychological Distress. Front. Psychiatry 12:721532. doi: 10.3389/fpsyt.2021.721532
Received: 07 June 2021; Accepted: 20 July 2021;
Published: 17 August 2021.
Edited by:
Annunziata Romeo, University of Turin, ItalyReviewed by:
Seon-Cheol Park, Hanyang University Guri Hospital, South KoreaAgata Benfante, University of Turin, Italy
Copyright © 2021 Kim, Kang, Jhon, Ryu, Lee, Kang, Jung, Shin, Kim, Stewart and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sung-Wan Kim, c3draW1AY2hvbm5hbS5hYy5rcg==; Jae-Min Kim, am1raW1AY2hvbm5hbS5hYy5rcg==
 Ju-Wan Kim1
Ju-Wan Kim1 Ju-Yeon Lee
Ju-Yeon Lee Sung-Wan Kim
Sung-Wan Kim Jae-Min Kim
Jae-Min Kim