- 1Department of Psychiatry, Faculty of Medicine, Universitas Indonesia – Dr. Cipto Mangunkusumo General Hospital, Jakarta, Indonesia
- 2Faculty of Psychology, Universitas Tarumanegara, Jakarta, Indonesia
Adolescence is often a period of turmoil. The COVID-19 pandemic has increased adolescents' difficulty due to mental health consequences that may affect their developmental milestones. This study constructed and empirically tested a theoretical model of three predictive factors (cyberbullying, abuse, and screen time) and stress as the mediating factor in adolescent non-suicidal self-injury (NSSI). Structural equation model (SEM) analysis was applied to investigate stress as a mediating factor in the relationship between adolescent NSSI and cyberbullying, abuse, and screen time. This cross-sectional study used a “crowdsourcing” sample collection method to recruit 464 adolescents aged 11–17 years who were administered a questionnaire comprising scales on cyberbullying, abuse, screen time, stress, and NSSI. All scales had construct reliabilities ranging from 0.759 to 0.958. SEM statistical analysis was performed using Lisrel version 8.8 (Scientific Software International, USA) for Windows (Microsoft Corporation, Redmond, WA, USA). The mean (± SD) age of the cohort was 14.61 ± 1.65 years, and consisted of 66.7% females. Secondary high school was the highest educational background (58%). The study found that cyberbullying and abuse were direct positive predictors (critical t-value for the path > 1.96; p < 0.05) of adolescent NSSI; however, screen time did not have any direct relationship. Furthermore, stress was a significant full mediating factor of screen time and a partial mediating factor of cyberbullying and abuse in the relationship with adolescent NSSI (critical t-value of the path = 5.27; p < 0.05). Cyberbullying, screen time, and abuse with the mediating effect of stress could explain 48% of the variance in adolescent NSSI (R2 = 0.48). Adolescent mental health prevention and promotion programs need to be redesigned during the current COVID-19 pandemic to manage their stress and minimize the mental health consequences of cyberbullying, abuse, and inappropriately increased screen time.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has continued for more than 1 year. Globally, most schools and public places have been temporarily closed. In several countries, students have been instructed to stay at home, engage in social distancing during daily activities, and study from home (1). They used various Internet devices to stay connected to their schools and peers. Consequently, their screen time may have increased, especially of those living in urban cities in Indonesia. Internet access among adolescents has been estimated at 79.5%, and most of them use the Internet for several purposes such as to seek information for school activities, connect with their peer groups through social media networking (such as Path, Line, Whatsapp, Facebook messenger, etc.), and for entertainment (2). Adolescents have missed several important milestones, including direct social interactions with peers, making new friends, and sports activities, among others (1, 2). Moreover, they have been forced to adapt to new educational styles (i.e., online learning, examination[s], and group work), especially students in their final year of high school. Students entering the new academic year, particularly if they have transitioned to a new school, can only meet their new friends or teachers via online classes (3, 4). Therefore, their screen time has been increased compared to before the COVID-19 pandemic. It may increase the risk of cyberbullying for victims (5, 6). Moreover, adolescents may lose peers and social support, face more internal conflicts, and abuse triggered by less personal space because all family members stay at home, engage in less physical activity due to parental restrictions to leave the home, and disruptions in daily routine activities (7). Additionally, the number of COVID-19 cases and deaths has continued to increase in several countries, including India, Indonesia, the United States, and Brazil (8). In Indonesia, the number of new COVID-19 cases has increased over time. For example, in this study period (August-October 2020), the average number of new cases was estimated to be around 4,200 per day and around 100 deaths occurred due to this infection. However, it increased by 10–15 times in the middle of July 2021, with more than one thousand deaths. The Indonesian government has implemented several policies to minimize the spread of COVID-19 since April 2020, such as extending the policy of restricting public activities at the micro scale and school closures, implementing a 50–100% Work-From-Home policy, while all shopping centers and malls, worship houses, and public parks were partially or totally closed (2, 9). Thus, the COVID-19 pandemic has significantly contributed to stressful life events among adolescents and young adults. It has become a unique stressor and forces everyone, including adolescents, to rapidly acquire new adjustment skills. However, adolescents may face difficulties due to developmental challenges.
Adolescence is a transitional period between childhood and young adulthood, consisting of multidimensional transformations such as biological, psychological, cognitive, and social. From a biopsychosocial perspective, maturation of the hypothalamic-pituitary-gonadal axis marks both puberty and adolescence. Thus, hormonal changes in adolescence are associated with fluctuations in emotional experiences, increased self-esteem, a sense of self-importance, and individuality. However, at the same time, adolescents may experience self-criticism, depression, anxiety, and anger (10). Additionally, prefrontal cortex immaturity may contribute to irrational decision-making and tenuous impulse control, particularly during stressful times (11). Moreover, this can lead to greater experimentation with high-risk behaviors during the COVID-19 pandemic, such as non-suicidal self-injury (NSSI), not only among typical adolescents but also among adolescents with pre-existing mental health problems (12, 13).
In 2018, the International Society for the Study of Self-Injury defined NSSI as conscious and direct engagement in behaviors that produce body tissue damage without deliberate suicidal intention (1). However, NSSI is linked to suicidal ideation and attempt(s), and it has been estimated that individuals with NSSI are four times more likely to attempt suicide in the future (14, 15). In 2015, Plener et al. reported that NSSI typically began during early or mid-adolescence, possibly becoming chronic NSSI over a prolonged period or was carried out a few times in a significantly more discreet period (16, 17). A worldwide study demonstrated that ~17% of adolescents engaged in NSSI, and it was essentially comparable in boys and girls (18, 19). Moreover, cultural differences may impact the prevalence of NSSI, despite the paucity of prevalence studies in non-Western countries compared to Western countries (20). In the past decade, many mental health-related studies have investigated NSSI. Previous studies have indicated that gender, cyberbullying, screen time, abuse, and stress may be associated with NSSI, especially during the unconventional life events of the COVID-19 pandemic (6–8). On the other hand, several studies before the COVID-19 pandemic revealed other psychosocial and biological risk factors associated with NSSI, such as genetics, changes in brain neurotransmitters, depressive symptoms, stigmas, common misperceptions of mental illness, and family discord (20).
NSSI can be characterized as an improper coping strategy for adolescents, especially to release strong negative feelings due to heightened stress and relief from their intolerable states in a very short time (13). Furthermore, NSSI may predict poorer future psychosocial well-being among adolescents (1). Several studies have reported that closure of schools and public places during the COVID-19 pandemic magnified many negative consequences of adolescents' developmental milestones and possibly increased the risk for NSSI or exacerbated self-injury behavior such as suicidal ideation or attempt in some adolescents due to elevated stress during this unstable period (1, 21). To summarize, NSSI has possibly become a new threat to adolescents' mental well-being during the COVID-19 pandemic. Therefore, the effect of screen time, cyberbullying, abuse, and stress on NSSI that emerged during the COVID-19 pandemic is a critical topic to be investigated and discussed.
The current study constructed and empirically tested a theoretical model that could predict and explain adolescent NSSI during the COVID-19 pandemic in Indonesia. Several studies have reported that NSSI has become a major public health problem worldwide during the COVID-19 pandemic, especially among adolescents (13, 20). However, to the best of our knowledge, few empirical studies have explored the effects of cyberbullying, abuse, screen time, and stress on adolescent NSSI during the COVID-19 pandemic. Accordingly, the current study developed a questionnaire for adolescents in Indonesia. The questionnaire survey method was adopted to determine how cyberbullying, screen time, abuse, and stress affected adolescent NSSI during the COVID-19 pandemic. Hence, the present study explored several primary antecedents/predictors (cyberbullying, screen time, and abuse) for NSSI among adolescents, and determined whether stress mediated cyberbullying, screen time, and abuse of adolescent NSSI. In this context, the research questions were defined as follows: Is there any possibility that mental health reactions during the COVID-19 pandemic, such as cyberbullying, screen time, and abuse, significantly predict adolescent NSSI? How does stress mediate the effects of cyberbullying, abuse, and screen time on adolescent NSSI during the COVID-19 pandemic? The results were expected to enhance the scholarly understanding of adolescent NSSI during the COVID-19 pandemic and adolescents' mental health reactions, such as cyberbullying, screen time, abuse, and stress, to enhance the knowledge base for health professionals, parents, schools, and government education authorities, and design better adolescent mental health and stress reduction programs, especially during the pandemic.
Methods
This cross-sectional study used a “crowdsourcing” sample collection method during the COVID-19 pandemic in Indonesia. Data were collected from August 21 to October 10, 2020. A questionnaire link (http://surveymonkey.com) was circulated through social media networks, such as WhatsApp, Facebook Messenger, and Line. The inclusion criteria were adolescents aged 11–17 years with secondary and high school backgrounds. Before completing the survey, participants completed an online informed consent form. During the research period, 744 questionnaires were returned. However, 247 were excluded because they were incomplete, including missing data, not fulfilling the inclusion criteria, or the absence of a signature on the online informed consent form. Therefore, the final analysis included 464 questionnaires. The Ethics Committee of the Faculty of Medicine of Universitas Indonesia approved the study protocol in April 2020 (KET-375/UN2.F1/ETIK/ PPM.00.02/2020).
Instruments
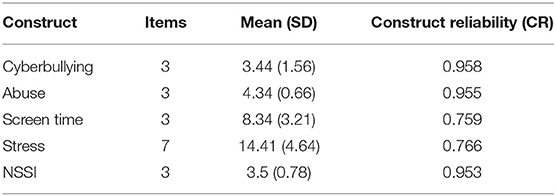
The questionnaire was developed specifically for this study. It contained information from a previously published study with multi-item scales that demonstrated good psychometric properties. The questionnaire items were determined after a thorough review of several relevant studies that addressed cyberbullying, screen time, abuse, stress, and NSSI. The item dimensions were modified to fit the context of adolescent mental health reactions during the COVID-19 pandemic and study design. Questionnaire development followed the recommendations of MacKenzie et al. and the development procedures suggested by Devellis for standard psychometric scales (22, 23). The questionnaire consisted of 24 items measured in six sections: the cyberbullying scale (three items), screen time scale (three items), abuse scale (three items), stress scale (seven items), NSSI scale (three items), and sociodemographic questions. All questions were modified into the Indonesian language and had good construct reliability (CR ranged from 0.759 to 0.955) for this study.
Cyberbullying Scale
The cyberbullying scale was developed using three items modified from Patchin and Hinduja (24), Sourander et al. (25), and Hinduja et al. (26), Sourander et al. (25), and Wiguna et al. (27). The questions were as follows: “During the past 6 months, how often have you been cyber-bullied?” “During the past 6 months, how often have you cyber-bullied others?” “During the past 6 months, how often have you been cyber-bullied and being cyber-bullied others?” Items were rated on a four-point Likert scale, scored as follows: never = 1, < 1 per week = 2, > 1 per week = 3, and almost daily = 4. The construct reliability (CR) of these three items was 0.958, which was satisfactory in terms of measuring the constructs of interest because it exceeded 0.5.
Screen Time Scale
Screen time was measured using three items modified from the Youth Screen Time Survey. The method used to measure screen time in this study followed the standard methods used in several other peer-reviewed studies. Adolescents were asked to report the number of minutes devoted to the following three typical activities on weekdays and weekends: (1) “television (movies/videos/YouTube, playing console/video games),” (2) “using personal computers (such as, laptops/tablets/iPads either for browsing, YouTube, and/or social media activities),” and (3) “smartphone devices (for online games, browsing, social media connections, and/or online shopping).” The daily time spent on each screen time activity was calculated by averaging the weekday and weekend screen times of the three typical activities and dividing by 7. The average total weekday and weekend screen time for each type of activity was divided by 7 and categorized into a six-point Likert scale as follows: < 2 h = 1, 2–4 h = 2, 4–6 h = 3, 6–8 h = 4, 8–10 h = 5, and ≥ 10 h = 6. The CR for screen time measurement was 0.759, which was satisfactory in terms of measuring the constructs of interest.
Abuse Scale
The construct of abuse was measured using three items from the Adverse Childhood Experiences (ACE) scale in the CDC-Kaiser Permanente Adverse Childhood Experiences Study (28). The three modified questions were as follows: “In the past 3 months, did a parent or other adult in the household often or very often push, grab, slap, or throw something at you? or ever hit you so hard that you had marks or were injured?” “In the past 3 months, did an adult or person at least 5 years older than you ever swear at you, insult you, or put you down?” and “In the past 3 months, did you often or very often feel that you did not have enough to eat, had to wear dirty clothes, and had no one to protect you? or your parents or anybody else in your home were not taking good care of you or giving you enough love as you needed?” The items were scored as yes = 1 and no = 2. The CR of the abuse scale was 0.955, which was satisfactory in terms of measuring the constructs of interest.
Stress Scale
The stress scale was developed using seven items modified from the Depression Anxiety Stress Scale-21 (DASS-21) (29). It is a quantitative measure of the general symptoms of stress in the past 7 days across clinical, community, and non-clinical samples (30–32), and different countries, cultures, and languages (33–36). The seven modified items consisted of the following: “I find myself getting upset because of minor issues,” “I have a tendency to over-react to different situations,” “I find it is hard to relax,” “I find myself easily getting upset,” “I feel that I am using a lot of energy to feel worry,” “I find myself getting impatient when something needs to be postponed (i.e., queuing, waiting for class, traffic jams, etc.),” and “I am easily getting irritated.” Items were scored on a four-point Likert scale, as follows: never = 1, sometimes = 2, always = 3, and almost always = 4. The CR of the stress scale was 0.766, which was satisfactory in terms of measuring the constructs of interest.
NSSI Scale
Non-suicidal self-injury (NSSI) was measured using three items modified from Wiguna et al. and Sourander et al. (25, 27). The modified questions were as follows: “In the past 6 months, did I ever hurt myself deliberately, such as intentionally self-injured,” “In the past 6 months, did I ever seriously consider killing myself,” and “In the past 6 months, did I ever try to defeat myself.” The items were scored as yes = 1 and no = 2. The CR of the NSSI scale was 0.953, which was satisfactory for measuring the constructs of interest.
Sociodemographic Questions
The sociodemographic questions included eight items that inquired about the participants' age, sex, level of education, home-based and parental socioeconomic background. The questions were designed for nominal and categorical responses.
Data Analysis
The present study determined the primary predictors of NSSI (screen time, abuse, and cyberbullying) and confirmed that stress had a mediating effect on these predictors of adolescent NSSI during the COVID-19 pandemic. Therefore, structural equation modeling (SEM) analysis was performed using Lisrel version 8.8. The SEM analysis primarily aimed to explain the pattern of construct interaction pathways of several inter-related independence predictors simultaneously (screen time, cyberbullying, and abuse), stress as the mediating variable, and adolescent NSSI as the dependent variable or outcome (Figure 1). The SEM analysis is a strong technique for effectively addressing multicollinearity (when ≥ 2 variables are highly associated), which is one of the advantages of SEM over multiple regression and factor analysis. The mediating effect of stress can be described as follows: full mediation (a mediator fully explains the interaction of the predictor variable to predict the outcome, and there is no relationship without the mediator in the model), partial mediation (predictor variable has a direct significant interaction to predict the outcome, even when the mediator is removed from the model; the mediator only partially explained the inter-relationship), or no mediation (predictor variable does not have any direct significant interaction to predict the outcome and is not statistically significant even when the mediator is included). The construct interaction pathway to predict the adolescent NSSI in this study was considered to be statistically significant if each predictor and mediator exceeded the critical value of indicator's loading for p < 0.05 (critical t-value for the path >1.96) (37, 38).
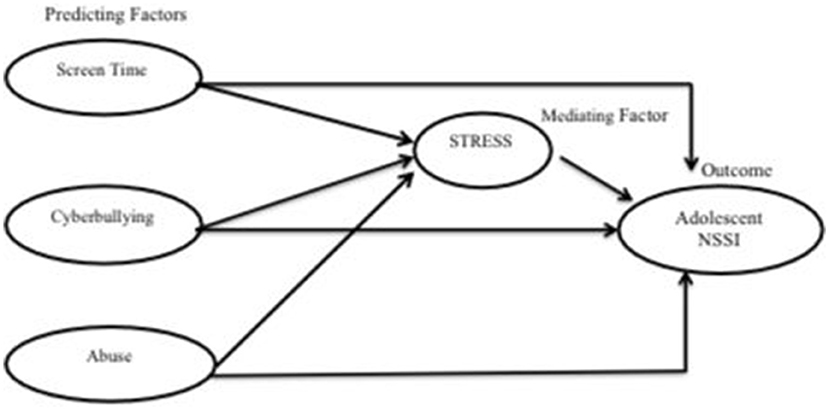
Figure 1. The pattern of construct interaction pathway of predictors (screen time, cyberbullying, abuse), stress as the mediating variable, and adolescents' NSSI as the dependent variable (outcome).
Lisrel version 8.8 was used to analyze CR, which reflects the internal consistency reliability of the variable measurement scale. Reisinger and Turner reported that the CR coefficient of each measurement scale should be ≥ 0.6 as a prerequisite for further SEM analysis (36). The obtained CR coefficient in this study ranged from 0.759 for the screen time scale to 0.958 for the cyberbullying scale, and all CR coefficients were > 0.6 (Table 1). Hence, the reliability of all scales in the present study was acceptable for further SEM analysis using Lisrel version 8.8.
Results
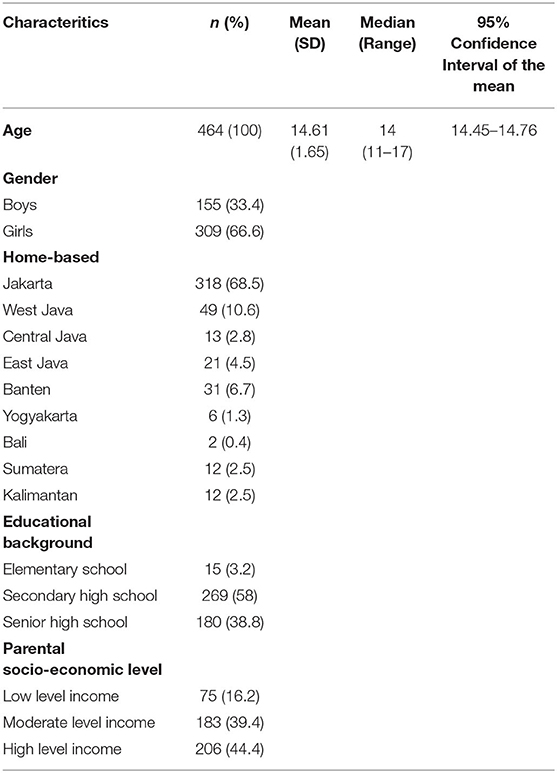
This study included 464 adolescents selected using a crowdsourcing sample collection method. The mean (± SD) age of the cohort was 14.61 ± 1.65 years, and consisted of 66.7% females. Secondary high school was the highest educational background (58%), followed by senior high school (38.8%) and elementary school (3.2%). Participants were from several provinces in Indonesia; the greatest proportion was from Jakarta (68.5%), followed by West Java (10.6%), Banten Province (6.7%), East Java (4.5%), Central Java (2.8%), and Sumatra (2.5%). Most participants had parents with middle to high economic backgrounds (83.8%), while the remainder had a lower economic background (16.2%) (Table 2).
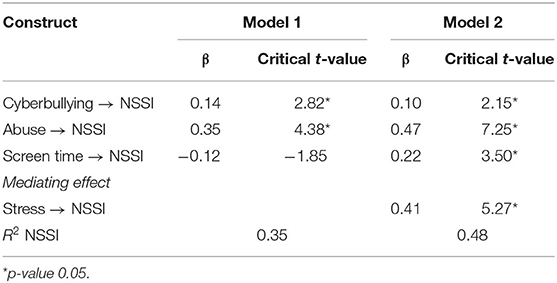
Results demonstrated that cyberbullying and abuse became significant positive direct predictors of adolescent NSSI during the COVID-19 pandemic (critical t-value for cyberbullying: 2.82; critical t-value for abuse: 4.38). However, screen time was not a direct predictor of adolescent NSSI (critical t-value: 1.85). Additionally, stress had a significant mediating effect on cyberbullying, screen time, and abuse in the relationship with adolescent NSSI (critical t-value: 5.27). Stress also had a full mediating effect on screen time in predicting adolescent NSSI, but only had a partial mediating effect on cyberbullying and abuse. Furthermore, cyberbullying, screen time, and abuse without the mediating effect of stress predicted 38% (R2 = 0.38) of the variance in adolescent NSSI. Meanwhile, cyberbullying, screen time, and abuse with the mediating effect of stress could explain 48% of the variance in adolescent NSSI (R2 = 0.48) (Table 3). Thus, stress as a mediator variable significantly multiplied the interaction between predictors (cyberbullying, screen time, and abuse) to predict adolescent NSSI during the COVID-19 pandemic in Indonesia (Figure 2). The mediating effects of stress were determined according to the significance of the interaction model (critical t-value for the path >1.96; p < 0.05). Hence, the research questions (i.e., Is there any possibility that mental health reactions during the COVID-19 pandemic, such as cyberbullying, screen time, and abuse, significantly predict adolescent NSSI? How does stress mediate the effects of cyberbullying, abuse, and screen time on adolescent NSSI during the COVID-19 pandemic?) were answered based on the SEM analysis.
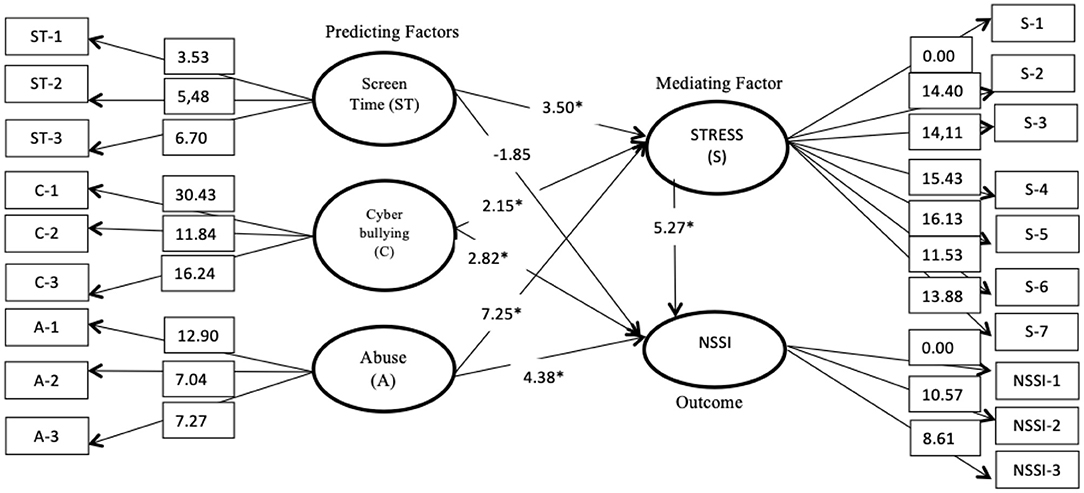
Figure 2. The construct theoretical model of adolescent NSSI based on the SEM analysis including the critical t-value (Statistically significant on critical t-value >1.96 and p < 0.05). The analysis showed that stress significantly and fully mediated the relationship between screen time and adolescent NSSI. However, it only had a partial significant mediating effect on cyberbullying and abuse. The theoretical construct analysis was significantly fit to the model. *p < 0.05; Root Mean Square Error of Approximation = 0.038, Normed Fit Index = 0.95, Comparative Fit Index = 0.98, Relative Fit Index = 0.94, Non-Normed Fit Index = 0.98, Standardized Root Mean Square Residual = 0.049, Goodness-of-Fit Index = 0.95, Adjusted Goodness-of-Fit Index = 0.93).
The structural equation path modeling in this study followed the recommendations of Turner and Reisinger (37) and Muller et al. (38) to select goodness-of-fit to measure the fitness of the structural model (37, 38). Based on confirmatory factor analysis of the structural path modeling, the construct showed a significant model of fitness (root mean square error of approximation = 0.038; normed fit index = 0.95; comparative fit index = 0.98; relative fit index = 0.94; non-normed fit index = 0.98; standardized root mean square residual = 0.049; goodness-of-fit index = 0.95; and adjusted goodness-of-fit index = 0.93).
Discussion
The COVID-19 pandemic is ongoing, and mental health consequences cannot be avoided by everyone. Adolescence is a period of turmoil, as young people seek independence and struggle to find their identity. The major developmental task during this period is to improve social skills, become empathetic individuals, and find their true identity. These developmental tasks arise through connections with peers. Therefore, disrupted connections with social contexts and peers may have several implications for their mental well-being. Moreover, the immaturity of the prefrontal cortex during adolescence may make these individuals significantly more vulnerable to various mental health consequences during this pandemic (11).
During the COVID-19 pandemic, the lack of direct social connectedness with peers due to stay-at-home policies may have strengthened feelings of loneliness and social isolation. Therefore, adolescents alternatively engaged in more screen time during their daily activities (1). This study revealed that screen time did not directly predict adolescent NSSI, but demonstrated that stress was a perfect mediating factor of screen time and adolescent NSSI. Screen time is defined as the quantity of time spent and the diverse activities performed online using digital devices (39). This study found that the average screen time was around 4–6 h per day and was used for (1) watching television (such as movies/videos/YouTube and/or playing console/video games), (2) personal computers (such as laptops/tablets/iPads for browsing, YouTube, and/or social media activities), and (3) smartphone devices (for online games, browsing, social media connections, and/or online shopping). We found that the average screen time among adolescents was in keeping with the screen time prescribed by the American Academy of Child and Adolescent Psychiatry (from the recommended hours to more than 6 h). Hamilton et al. explained that an appropriate amount of screen time devoted to social media or other activities may act as a protective factor for mental health among adolescents because it can provide appropriate physical and mental health information, academic materials, maintain social connections with peers, and facilitate self-expression (40). On the other hand, several studies have focused on the potentially harmful mental health effects of increased screen time, such as high exposure to false or misinformation on physical and mental health related to the COVID-19 pandemic, cyberbullying, and age-inappropriate media programs. Moreover, many adolescents may have insufficient basic knowledge, understanding, and perception to assess the accuracy of this information because of prefrontal cortex immaturity (38–41). Thus, the cognitive processes that follow screen time for television, personal computers, or smartphones may trigger adolescents to feel stressed, leading them engage in NSSI behavior to cope with these uncomfortable feelings.
Interestingly, stress was found to be a partial mediating factor for cyberbullying and abuse (as a predictor factor) of NSSI. Cyberbullying and abuse directly and significantly predicted adolescent NSSI; however, the association was more significant through the mediator effect (stress). Cyberbullying is defined as a type of bullying exerted through devices such as computers, laptops, or smart phones on Internet and social media applications (25). In 2012, Langos explained that it can occur either directly or indirectly depending on privileged or public posts, including negative content that embarrasses others on private text messages or pictures through social media platforms (Whatsapp, Path, and Line, or private e-mail) (42). Extensive Internet use during the COVID-19 pandemic can heighten loneliness and impulsive behaviors toward other adolescents, such as domestic abuse, cyberbullying, and other high-risk and self-injurious behaviors (43–45). In 2018, Wiguna et al. found that cyberbullying increased the risk for high-risk behaviors such as self-harm, suicidal ideation, and attempted suicide (25). This process is related to brain networks. First, the socio-emotional network reacts to the reward processing part of the brain and subtle emotional stimuli. The second network is cognitive control, which plays an important role in planning, rational thinking, and self-regulation. During adolescence, the socio-emotional network becomes more dominant compared to the cognitive control network due to the immaturity of the prefrontal cortex (46). Hence, adolescents may be more easily engaged in impulsive and hostile behaviors.
The COVID-19 pandemic is a global crisis affecting every sector of life, such as health, economies, and family quality of life (47). Thus, it may cause disruptions in many family systems, not only due to lockdowns, stay-at-home orders, school from home, social distancing, and difficulties with access to health services, but also because of the sudden and possibly long-term family poverty and uncertainty (48, 49). Moreover, Martinkevich et al. explained that pandemics produce a deviant situation in which adolescents' socio-ecological systems are disrupted and, consequently, the incidence of abuse is likely to increase (50). The socio-ecological model explained that the COVID-19 pandemic may alter adolescents' cognition, emotions, behaviors, and fundamental mechanisms due to limited access to their developmental needs. Hence, these mutual interaction processes manifest as changing psychological, interpersonal, well-being, and environments, and in the ways in which adolescents adapt to and modify these environments (51). At the microsystem level, it may possibly increase oppositional and impulsive behaviors and limit testing among adolescents. This hostile behavior may elicit punitive responses from parents (52). They may also experience parental burnout, either constrained or worsened by the consequences of the pandemic. Adolescents' own stress and uncertainty regarding the pandemic may worsen the feeling of tension and they may become violent toward themselves due to limitations in their capacity to make decisions (53).
The study findings revealed that stress significantly mediated the predictors and, thus, the effects on NSSI behavior were more heightened. Liu and Miller (54) reported that stress is theoretically and empirically associated with an increased risk of self-injury, particularly in the form of suicidal ideation and behavior (55). The finding that stress possibly acts as a primary mediator of adolescent NSSI was supported by several theoretical conceptualizations that originally came from the two distinct processes with four functional elements of NSSI (56). NSSI behavior was strengthened by two distinct processes that consisted of four functional elements: positive and negative reinforcements in intrapersonal emotional regulation processes and interpersonal function processes. Intrapersonal emotional regulation processes include negative reinforcement that releases the conflict or a decrease in the negative affect following engagement in NSSI and positive reinforcement that is involved in the urge to feel pain or act on the feelings of guilt through self-punitive behavior. Interpersonal function processes include positive reinforcement wherein NSSI serves as a means of communicating with the unconscious mind for help and support and negative reinforcement that interrupts negative interpersonal interactions following NSSI. Such interpersonal functions may be relevant to adolescents because of the immaturity of brain's cognitive networks that impair interpersonal problem-solving skills and deprive them of general communication abilities (54, 57, 58). Nevertheless, stress during the COVID-19 pandemic became a mediating presence of a form of distress across the four functional elements, which could be the reason behind adolescents' engagement in NSSI to cope with this distress.
Based on the study findings, expanding adolescent mental health programs that can promote better coping strategies to manage stress related to cyberbullying, abuse, and increased screen time, such as coping with stress and positive attitudes toward stress, may be redesigned to ensure adequate self-adjustment during this pandemic. Furthermore, adolescent stress-reduction programs may be developed to improve coping strategies on these difficult days. Adolescent mental health programs are usually conducted at schools because adolescents spend most of their time at school. However, during the pandemic period, this program may be conducted online. Hence, adolescent mental health intervention programs that promote effective coping strategies to manage stress during the COVID-19 pandemic, such as active solution-orientation, stress resolution, conflict with stress, mindfulness, and positive attitude instead of holding back problems to one self may be designed to ensure adequate emotional adjustment (59). Several studies reported that sufficient regulation of emotions, including correct problem-solving skills and creating positive emotions in daily life through shared actions using networks and information and communication technologies (ICT) were very helpful to reduce stress during this COVID-19 pandemic (60, 61). Alternatively, psychoeducation programs may be developed in a very small group of adolescents in a “safe-haven” environment to enhance coping strategies and emotional regulation toward stress (62). Even for adolescents learning from home, schools should strive to intensify social support, encouragement, reassurance, and offer mental health services and programs, especially to those with existing mental health issues that enhance their vulnerability to stress (63).
Nevertheless, this study had several limitations. First, other factors that may be associated with adolescent NSSI, such as genetics, parenting, the role of devices, subjective feelings during the COVID-19 pandemic, and previous mental health history were not addressed. Therefore, further studies can elaborate these using a similar model. Second, the questionnaire relied on adolescents' self-reporting recruited through crowdsourcing, which may introduce biases related to misunderstanding or misreporting to avoid stigma and forgetting experiences that have already happened that triggered the recall/response bias. However, the study minimized these biases by providing detailed text explanations before the participants started the survey and provided a detailed explanation of each question. Third, the study was conducted online and may have only covered adolescents with access to the Internet. Future studies may be designed with mixed method data collection (i.e., online and offline surveys) so that it can include more adolescents, especially those without access to the Internet. Data were collected from August to early October 2020. This period was considered to be the second wave of the COVID-19 pandemic, and it came together with the beginning of the new online academic semester; therefore, the participants may have been overwhelmed. Future studies should consider the time period required for data collection to reduce unpredictable bias. Meanwhile, the study was conducted with a cross-sectional design, and it may not reflect the cause-and-effect relationship. Therefore, future studies can be designrd to determine the cause-effect relationship between adolescent NSSI, stress, cyberbullying, and other related factors.
To our knowledge, this study was the first in Indonesia and, perhaps, in Southeast Asia, to construct and analyze a theoretical model that can predict and explain adolescent NSSI during the COVID-19 pandemic. Stress was found to be a mediating factor in the relationship of adolescent NSSI with screen time, cyberbullying, and abuse. Therefore, the theoretical model can be applied further to design adolescent mental health programs, especially those associated with coping with stress in daily life.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Faculty of Medicine of Universitas Indonesia. Informed consent to participate in this study was provided by the study participants.
Author Contributions
TW: designing, analyzing, and writing the results and discussion. KM: designing, writing discussion, and results analyzing. FK and RI: designing and writing discussion. EW: results analyzing and wrting discussion. BM: designing and results analyzing. KP: editing the document and contributing in the table analyzing. All authors contributed equally for this paper.
Funding
The publication was supported by the PUTI Grant Universitas Indonesia with contract number NKB-4136/UN2.RST/HKP.05.00/2020. The funder did not have any involvement in the study design or report writing.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank all adolescents that participated on this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.743329/full#supplementary-material
References
1. Hasking P, Lewis SP, Bloom E, Brausch A, Kaess M, Robinson K. Impact of the COVID-19 pandemic on students at elevated risk of self-injury: the importance of virtual and online resources. Sch Psychol Int. (2020) 42:57–78. doi: 10.1177/0143034320974414
2. Wiguna T, Anindyajati G, Kaligis F, Ismail RI, Minayati K, Hanafi E, et al. Brief research report on adolescent mental well-being and school closures during the COVID-19 pandemic in Indonesia. Front Psychiatry. (2020) 11:598756. doi: 10.3389/fpsyt.2020.598756
3. Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. (2020) 4:421. doi: 10.1016/S2352-4642(20)30109-7
4. Huckins JF, daSilva AW, Wang W, Hedlund E, Rogers C, Nepal SK, et al. Mental health and behavior of college students during the early phases of the COVID-19 pandemic: longitudinal smartphone and ecological momentary assessment study. J Med Internet Res. (2020) 22:e20185. doi: 10.2196/20185
5. Nagata JM, Abdel Magid HS, Pettee Gabriel K. Screen time for children and adolescents during the coronavirus Disease 2019 pandemic. Obesity. (2020) 28:1582–3. doi: 10.1002/oby.22917
6. Armitage R. Bullying during COVID-19: the impact on child and adolescent health. Br J Gen Pract. (2021) 71:122. doi: 10.3399/bjgp21X715073
7. Kiekens G, Hasking P, Nock MK, Boyes M, Kirtley O, Bruffaerts R, et al. Fluctuations in affective states and self-efficacy to resist non-suicidal self-injury as real-time predictors of non-suicidal self-injurious thoughts and behaviors. Front Psychiatry. (2020) 11:214. doi: 10.3389/fpsyt.2020.00214
8. World Health Organization. Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update Geneva: WHO (2021).
9. COVID-19 Developments in Indonesia. Available online at: https://indonesien.ahk.de/en/infocenter/news/news-details/covid-19-developments-in-indonesia (accessed 29 August 2021).
10. Steinberg L. Risk taking in adolescence: new perspectives from brain and behavioral science. Curr Dir Psychol Sci. (2007) 16:55–9. doi: 10.1111/j.1467-8721.2007.00475.x
11. Grootens-Wiegers P, Hein IM, van den Broek JM, de Vries MC. Medical decision-making in children and adolescents: developmental and neuroscientific aspects. BMC Pediatr. (2017) 17:120. doi: 10.1186/s12887-017-0869-x
12. Guessoum SB, Lachal J, Radjack R, Carretier E, Minassian S, Benoit L, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. (2020) 291:113264. doi: 10.1016/j.psychres.2020.113264
13. Carosella KA, Wiglesworth A, Silamongkol T, Tavares N, Falke CA, Fiecas MB, et al. Non-suicidal self-injury in the context of COVID-19: the importance of psychosocial factors for female adolescents. J Affect Disord Rep. (2021) 4:100137. doi: 10.1016/j.jadr.2021.100137
14. Ferrey AE, Hughes ND, Simkin S, Locock L, Stewart A, Kapur N, et al. The impact of self-harm by young people on parents and families: a qualitative study. BMJ Open. (2016) 6:e009631. doi: 10.1136/bmjopen-2015-009631
15. Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, et al. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychol Med. (2016) 46:225–36. doi: 10.1017/S0033291715001804
16. Plener PL, Schumacher TS, Munz LM, Groschwitz RC. The longitudinal course of non-suicidal self-injury and deliberate self-harm: a systematic review of the literature. Borderline Personal Disord Emot Dysregulation. (2015) 2:2. doi: 10.1186/s40479-014-0024-3
17. Barrocas AL, Giletta M, Hankin BL, Prinstein MJ, Abela JRZ. Nonsuicidal self-injury in adolescence: longitudinal course, trajectories, and intrapersonal predictors. J Abnorm Child Psychol. (2015) 43:369–80. doi: 10.1007/s10802-014-9895-4
18. Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threat Behav. (2014) 44:273–303. doi: 10.1111/sltb.12070
19. Bresin K, Schoenleber M. Gender differences in the prevalence of nonsuicidal self-injury: a meta-analysis. Clin Psychol Rev. (2015) 38:55–64. doi: 10.1016/j.cpr.2015.02.009
20. Brown RC, Witt A. Social factors associated with non-suicidal self-injury (NSSI). Child Adolesc Psychiatry Ment Health. (2019) 13:23. doi: 10.1186/s13034-019-0284-1
21. Ghosh R, Dubey MJ, Chatterjee S, Dubey S. Impact of COVID-19 on children: special focus on the psychosocial aspect. Minerva Pediatr. (2020) 72:226–35. doi: 10.23736/S0026-4946.20.05887-9
22. MacKenzie SB, Podsakoff PM, Podsakoff NP. Construct measurement and validation procedures in MIS and behavioral research: integrating new and existing techniques. MIS Q. (2011) 35:293–334. doi: 10.2307/23044045
23. DeVellis R. Scale Development: Theory and Applications. 4th ed. Los Angeles, CA: SAGE Publications (2021). p. 24–35
24. Hinduja S, Patchin JW. Connecting adolescent suicide to the severity of bullying and cyberbullying. J Sch Viol. (2019) 18:333–46. doi: 10.1080/15388220.2018.1492417
25. Sourander A, Brunstein Klomek A, Ikonen M, Lindroos J, Luntamo T, Koskelainen M, et al. Psychosocial risk factors associated with Cyberbullying among adolescents: a population-based study. Arch Gen Psychiatry. (2010) 67:720–8. doi: 10.1001/archgenpsychiatry.2010.79
26. Hinduja S, Patchin JW, Hinduja S, Patchin JW. Bullying, cyberbullying. bullying, cyberbullying, and suicide. Arch Suicide Res. (2010) 14:206–21. doi: 10.1080/13811118.2010.494133
27. Wiguna T, Irawati Ismail R, Sekartini R, Setyawati Winarsih Rahardjo N, Kaligis F, Prabowo AL, et al. The gender discrepancy in high-risk behaviour outcomes in adolescents who have experienced cyberbullying in Indonesia. Asian J Psychiatr. (2018) 37:130–5. doi: 10.1016/j.ajp.2018.08.021
28. Center for Disease Control and Prevention. About the CDC-kaiser ACE Study. (2021). Available online at: https://www.cdc.gov/violenceprevention/aces/about.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fviolenceprevention%2Facestudy%2Fabout.html (accessed June 15, 2021).
29. Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
30. Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the depression anxiety stress scales in clinical groups and a community sample psychometric properties of the 42-Item and 21-Item versions of the depression anxiety stress scales in clinical. G Psychol Assess. (1998) 10:176–81. doi: 10.1037/1040-3590.10.2.176
31. Clara IP, Cox BJ, Enns MW. Confirmatory factor analysis of the depression–anxiety–stress scales in depressed and anxious patients. J Psychopathol Behav Assess. (2001) 23:61–7. doi: 10.1023/A:1011095624717
32. Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. (2005) 44:227–39. doi: 10.1348/014466505X29657
33. Mellor D, Vinet EV, Xu X, Hidayah Bt Mamat N, Richardson B, Román F. Factorial invariance of the DASS-21 among adolescents in four countries. Eur J Psychol Assess. (2014) 31:138–42. doi: 10.1027/1015-5759/a000218
34. Scholten S, Velten J, Bieda A, Zhang XC, Margraf J. Testing measurement invariance of the Depression, Anxiety, and Stress Scales (DASS-21) across four countries. Psychol Assess. (2017) 29:1376–90. doi: 10.1037/pas0000440
35. Kyriazos TA, Stalikas A, Prassa K, Yotsidi V. Can the depression anxiety stress scales short be shorter? factor structure and measurement invariance of DASS-21 and DASS-9 in a Greek, non-clinical sample. Psychology. (2018) 9:1095–127. doi: 10.4236/psych.2018.95069
36. Wang K, Shi HS, Geng FL, Zou LQ, Tan SP, Wang Y, et al. Cross-cultural validation of the depression anxiety stress scale−21 in China. Psychol Assess. (2016) 28:e88–100. doi: 10.1037/pas0000207
37. Turner LW, Reisinger Y, Witt SF. Tourism demand analysis using structural equation modelling. Tour Econ. (1998) 4:301–23. doi: 10.1177/135481669800400401
38. Muller D, Judd CM, Yzerbyt VY. When moderation is mediated and mediation is moderated. J Pers Soc Psychol. (2005) 89:852–63. doi: 10.1037/0022-3514.89.6.852
39. DataReportal. Digital. Global Digital Overview. Available online at: https://datareportal.com/reports/digital-2020-global-digital- overview (accessed October 02, 2021).
40. Hamilton JL, Nesi J, Choukas-Bradley S. Teens and social media during the COVID-19 pandemic: staying socially connected while physically distant. PsyArXiv. (2020). doi: 10.31234/osf.io/5stx4
41. Poitras VJ, Gray CE, Janssen X, Aubert S, Carson V, Faulkner G, et al. Systematic review of the relationships between sedentary behaviour and health indicators in the early years (0–4 years). BMC Public Health. (2017) 17(Suppl. 5):868. doi: 10.1186/s12889-017-4849-8
42. Radesky JS, Schumacher J, Zuckerman B. Mobile and interactive media use by young children: the good, the bad, and the unknown. Pediatrics. (2015) 135:1–3 LP – 3. doi: 10.1542/peds.2014-2251
43. Sharma V, Reina Ortiz M, Sharma N. Risk and protective factors for adolescent and young adult mental health within the context of COVID-19: a perspective from Nepal. J Adolesc Health. (2020) 67:135–7. doi: 10.1016/j.jadohealth.2020.04.006
44. Langos C. Cyberbullying: the challenge to define. Cyberpsychol Behav Soc Netw. (2012) 15:285–9. doi: 10.1089/cyber.2011.0588
45. Han Z, Wang Z, Li Y. Cyberbullying involvement, resilient coping, and loneliness of adolescents during Covid-19 in rural China. Front Psychol. (2021) 12:664612. doi: 10.3389/fpsyg.2021.664612
46. Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. (2020) 59:1218–39.e3. doi: 10.1016/j.jaac.2020.05.009
47. Okruszek Ł, Aniszewska-Stańczuk A, Piejka A, Wiśniewska M, Zurek K. Safe but lonely? Loneliness, anxiety, and depression symptoms and COVID-19. Front Psychol. (2020) 11:579181. doi: 10.3389/fpsyg.2020.579181 doi: 10.31234/osf.io/9njps
48. Weiss JW, Mouttapa M, Cen S, Johnson CA, Unger J. Longitudinal effects of hostility, depression, and bullying on adolescent smoking initiation. J Adolesc Health. (2011) 48:591–6. doi: 10.1016/j.jadohealth.2010.09.012
49. Prime H, Wade M, Browne DT. Risk and resilience in family well-being during the COVID-19 pandemic. Am Psychol. (2020) 75:631–43. doi: 10.1037/amp0000660
50. Anser MK, Yousaf Z, Khan MA, Nassani AA, Alotaibi SM, Qazi Abro MM, et al. Does communicable diseases (including COVID-19) may increase global poverty risk? a cloud on the horizon. Environ Res. (2020) 187:109668. doi: 10.1016/j.envres.2020.109668
51. Peterman A, Potts A, Donnell MO, Shah N, Oertelt-Prigione S, Van Gelder N, et al. Pandemics and Violence Against Women and Children. Washington, DC (2021).
52. Martinkevich P, Larsen LL, Græsholt-Knudsen T, Hesthaven G, Hellfritzsch MB, Petersen KK, et al. Physical child abuse demands increased awareness during health and socioeconomic crises like COVID-19. Acta Orthop. (2020) 91:527–33. doi: 10.1080/17453674.2020.1782012
53. Pereda N, Díaz-Faes DA. Family violence against children in the wake of COVID-19 pandemic: a review of current perspectives and risk factors. Child Adolesc Psychiatry Ment Health. (2020) 14:40. doi: 10.1186/s13034-020-00347-1
54. Liu RT, Miller I. Life events and suicidal ideation and behavior: a systematic review. Clin Psychol Rev. (2014) 34:181–92. doi: 10.1016/j.cpr.2014.01.006
55. Humphreys KL, Myint MT, Zeanah CH. Increased risk for family violence during the COVID-19 pandemic. Pediatrics. (2020) 146:e20200982. doi: 10.1542/peds.2020-0982
56. Griffith AK. Parental burnout and child maltreatment during the COVID-19 pandemic. J Fam Violence. (2020) 1:1–7. doi: 10.1007/s10896-020-00172-2
57. Bentley KH, Nock MK, Barlow DH. The four-function model of nonsuicidal self-injury: key directions for future research. Clin Psychol Sci. (2014) 2:638–56. doi: 10.1177/2167702613514563
58. Hilt LM, Cha CB, Nolen-Hoeksema S. Nonsuicidal self-injury in young adolescent girls: moderators of the distress-function relationship. J Consult Clin Psychol. (2008):76:63–71. doi: 10.1037/0022-006X.76.1.63
59. Nock MK. Suicidal behavior among adolescents: correlates, confounds, and (the search for) causal mechanisms. J Am Acad Child Adolesc Psychiatry. (2009) 48:237–9. doi: 10.1097/CHI.0b013e318196b944
60. Liu RT, Cheek SM, Nestor BA. Non-suicidal self-injury and life stress: a systematic meta-analysis and theoretical elaboration. Clin Psychol Rev. (2016) 47:1–14. doi: 10.1016/j.cpr.2016.05.005
61. Morales Rodríguez FM. Relationships between coping with daily stress, self-concept, social skills and emotional intelligence. Eur J Educ Psychol. (2017) 10:41–8. doi: 10.1016/j.ejeps.2017.04.001
62. Valero N, Vélez M, Durán A, Portillo M. COVID-19 coping: stress, fear, anxiety, and depression? Enferm Inv. (2020) 5:63–70. doi: 10.31243/ei.uta.v5i3.913.2020
Keywords: COVID-19, adolescents, Indonesia, cyberbullying, abuse, screen time, stress, non-suicidal self-injury
Citation: Wiguna T, Minayati K, Kaligis F, Ismail RI, Wijaya E, Murtani BJ and Pradana K (2021) The Effect of Cyberbullying, Abuse, and Screen Time on Non-suicidal Self-Injury Among Adolescents During the Pandemic: A Perspective From the Mediating Role of Stress. Front. Psychiatry 12:743329. doi: 10.3389/fpsyt.2021.743329
Received: 18 July 2021; Accepted: 22 October 2021;
Published: 12 November 2021.
Edited by:
Haibo Yang, Tianjin Normal University, ChinaReviewed by:
Md Irteja Islam, The University of Sydney, AustraliaDat Tan Nguyen, Can Tho University of Medicine and Pharmacy, Vietnam
Copyright © 2021 Wiguna, Minayati, Kaligis, Ismail, Wijaya, Murtani and Pradana. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tjhin Wiguna, dHdpZ2EwMEB5YWhvby5jb20=; dGppbi53aWd1bmFAdWkuYWMuaWQ=
 Tjhin Wiguna
Tjhin Wiguna Kusuma Minayati
Kusuma Minayati Fransiska Kaligis
Fransiska Kaligis Raden Irawati Ismail1
Raden Irawati Ismail1 Belinda Julivia Murtani
Belinda Julivia Murtani Kent Pradana
Kent Pradana