- 1Xiangya School of Public Health, Central South University, Changsha, China
- 2Guangzhou Medical University, Guangzhou, China
- 3School of Public Health, Guangxi Medical University, Nanning, China
- 4School of Public Health, Shandong University, Jinan, China
- 5Shenzhen Kangning Hospital, Shenzhen, China
- 6The Affiliated Brain Hospital of Guangzhou Medical University (Guangzhou Huiai Hospital), Guangzhou, China
Background: Few studies have investigated the roles of psychosocial factors such as depressive symptoms and hopelessness on the relationship between pain and suicide with inconsistent results. The study aimed to analyze the impact of pain intensity on suicide death and to estimate the degree to which depressive symptoms, hopelessness, and perceived burden may explain the association in Chinese rural elderly.
Methods: Using a 1:1 matched case–control design, we collected data from 242 elderly suicide cases and 242 living community controls by psychological autopsy method in rural China, including sociodemographic characteristics, pain intensity, depression, hopelessness, perceived burden, physical diseases, and social support. Conditional logistic regression was employed to assess the association between pain intensity and completed suicide. Mediation analysis using the KHB method was applied to explore the mediation effects from depressive symptoms, hopelessness, and perceived burden.
Results: The result of multivariable logistic regression showed that unemployment [odds ratio (OR) = 5.06, 95% confidence interval (CI): 1.76–14.49], higher levels of hopelessness (OR = 7.72, 95% CI: 3.49–17.10), depressive symptom (OR = 15.82, 95% CI: 4.53–55.25), and severe pain (OR = 3.46, 95% CI: 1.31–9.13) were significantly associated with elevated suicide risk in older adults in rural China. Depressive symptoms, hopelessness, and perceived burden significantly mediated 43.71% of the pain–suicide association (p = 0.020), with 17.39% due to depressive symptoms, 17.63% due to hopelessness, and 8.69% due to perceived burden.
Conclusions: Regular screening of pain, depressive symptoms, hopelessness, and perceived burden using simple but sensitive questions or scales for older adults with pain is vital for the prevention and early detection of suicide risk in Chinese rural areas. Moreover, the importance of pain management and psychological interventions targeted on depressive symptoms and hopelessness should be emphasized.
Introduction
Though the suicide rate in China has declined rapidly, the elderly population increasingly contributes to the overall burden of suicide (1). The average annual suicide rate among old adults was estimated to be 6.5-fold higher than the rate of the population under 65, and the rate in rural older adults was two times higher than that in urban elderly (2). Suicide among older adults in rural China remains a critical public health and mental health problem. Identification of potential risk factors for this vulnerable population is of paramount significance to design targeted suicide preventions.
Pain is highly prevalent, costly, and frequently disabling in later life (3). Almost 30% of U.S. older adults and 37.1% (34.1–40.3%) non-institutionalized older adults in Hong Kong experienced persisting pain (4, 5). Many older adults suffer silently and needlessly, resulting in severely diminished functional ability (3), interference in daily and social activities (5), and an elevated negative feeling. Previous evidence suggested that pain conditions were associated with an elevated risk of suicidal behaviors (6–8).
Depression has been found to be associated with suicide risk in individuals with pain (9, 10). One study observed that pain–suicide association reduced when controlling for psychiatric diagnoses, including depression (7), indicating that pain might be linked to suicidality via mechanisms at least related to depression.
Hopelessness has been identified as relevant in the understanding of the physical pain–suicidality link (11). A large pan-Canadian study found that patients with higher pain-related helplessness and greater pain magnification were more likely to present suicidal ideation. Besides, patients with hope toward medical cure had less suicidal thoughts (9). Higher hopelessness was associated with a higher pain threshold, which correlated with less fearlessness of death (12, 13).
The interpersonal theory of suicide proposed that perceived burdensomeness is a precursor to a desire to commit suicide (14). Individuals with pain may feel that they are creating a burden on their families. One study supported the theory by showing that perceived burdensomeness significantly predicted suicidal ideation in people with chronic pain (15). Moreover, the feeling of being a burden may be exacerbated by depression and hopelessness, finally increasing the risk of carrying out a suicidal act (16).
Though the pain–suicidality link has been reported, the mechanism may be complicated. Limited studies investigated the mediation effect of psychological factors, including depression, anxiety, and sleep problem on pain and suicidality link with inconsistent results (17–19). Moreover, most studies on the pain–suicidality association focused on suicide ideation and suicide attempts.
Using a matched case–control psychological autopsy study design, the goal of the present study was to analyze the link between pain and completed suicide among Chinese rural older adults and to estimate the degree to which depressive symptoms, hopelessness, and perceived burden may explain the association.
Materials and Methods
Sample and Sampling
We used a multi-stage stratified cluster sampling method to select the study site. The first step was the selection of the province. We stratified 31 provinces in mainland China into three levels according to the gross domestic product per capita. Shandong province, Hunan province, and Guangxi province were chosen from the rank 1–10, 11–20, and 21–31, respectively. The second step was the selection of rural counties from the selected provinces. We stratified counties into three levels based on per capita income in each province. One county in each stratum from Shandong and Hunan and two counties in each stratum from Guangxi (as the population of the counties in Guangxi was smaller than those in the other two) were selected using a simple random sampling performed by a computer algorithm. Finally, we included 12 counties from the three selected provinces. The study was conducted from June 2014 to September 2015.
Based on the death certification system, suicide decedents aged 60 and above in rural areas (villages) were collected consecutively in each selected county. A senior suicidologist (the professor of suicidology and mental health) briefly trained all village doctors and local public health workers involved in death certification on how to determine a suicide death. They were required to report all elderly suicide deaths and possible cases that they could not determine to the local Centers for Disease Control and Prevention. After collecting all available, relevant information, trained investigators determined the manner of death.
Living comparisons were 1:1 matched with the suicides in gender, birth year (±3 years), and village. Whenever a suicide decedent was identified, the investigators would enumerate all older adults matching gender and birth year in the same village. One living comparison was then selected from the list randomly using a computer program. The investigators expanded the search to the closest village if no appropriate comparison individuals were available in the same village. Finally, we enrolled a total of 242 suicide decedents and 242 living comparisons in this study.
Procedures of Interview
We selected two informants for each suicide decedent and living comparison. The selection of proxy informants was based on the informants' familiarity with the targets. Generally, the first informant was a next of kin who lived with the suicide decedent or the living comparison. Usually, the spouse was the first choice, followed by children and other relatives. The second informant was a friend, neighbor, or remote relative. Informants who refused to participate in the study were replaced by other suitable subjects. Among 968 informants, 450 (46.5%) were relatives of the target persons. Among 245 relatives of suicide cases, 54 (22.0%) were couples, and 95 (38.8%) sons or daughters; among 205 from controls, 80 (39.0%) were couples and 59 (28.8%) were sons or daughters. Among all informants, 232 (23.97%) informants lived together with suicides/controls before suicide/investigation [122 (23.14%) in the suicide group and 120 (24.79%) in controls].
We scheduled the interviews with the informants of suicide decedents 2–6 months after the death, while interviews with informants of living comparisons were conducted as soon as the participants and their informants were identified. Each informant was interviewed separately by one trained fieldworker, and the interviews lasted 90 min on average. The procedures of subjects' selection and interview have been detailed in a previous publication (20).
All procedures were carried out in accordance with the latest version of the Declaration of Helsinki. The study was approved by the Institutional Review Boards of the Central South University, Shandong University, and Guangxi Medical University. The investigators explained the aim and procedure of the research to all participants, and obtained written informed consent from participants in the living comparison group and all the informants of suicide decedents and living comparisons after the nature of the procedures had been fully explained.
Measures
Socio-Demographic Characteristics
We collected socio-demographic characteristics, including age, gender, marital status, employment status, education level, and annual family income.
Pain Intensity
We used an 11-point visual analog scale to assess the self-perceived pain intensity. First, participants were asked, “Did you/he/she feel any pain (including any physical pain or pain with unknown reasons) before death/investigation?” Participants who endorsed “yes” were asked to report their pain intensity by circling “the one number that describes your/his/her pain on the average,” using a 0 (no pain) to 10 (the worst pain) scale (21). We categorized pain intensity into four groups: 0 means without pain, 1–3 mild pain, 4–6 moderate pain, and 7–10 severe pain. Since the number of participants in the mild pain group was small [34 (14.05%) in the suicide decedents and 31 (12.81%) in the living comparisons], we combined mild and moderate pain into a single category called “mild to moderate pain.”
Physical Diseases
We used a question asking, “Did you/he/she have diagnosed physical diseases” to investigate whether having physical diseases before death/investigation. Physical diseases were understood as any acute or chronic illness and/or condition causing significant impairment and that may lead to long-term impairment, disability, and/or death. Investigators recorded diagnoses of physical diseases made by physicians, and reviewed medical records with consent when necessary. Zero means without physical disease, 1 means with one or more physical diseases.
Social Support
We used the 23-item Duke Social Support Index (DDSI) to measure social support in the last week before suicide/investigation. A total score ranges from 11 to 45, with a higher score indicating higher social support. DSSI has been used in a previous psychological autopsy study in China and showed satisfactory reliability and validity (22). We dichotomized social support into two groups based on the median score of DSSI.
Perceived Burden
We used the question that “Did you/he/she feel that caring you/he/she bring mental or physical burden to your/his/her family?” to rank the perceived burden level. One means “no perceived burden,” and 4 means “heavy perceived burden.” Perceived burden was categorized into two groups (1 means without perceived burden; 2–4 means with perceived burden).
Depressive Symptoms
We used the Geriatric Depression Scale (GDS-30) to assess the depressive symptoms in the last week before death/investigation (23). A higher score means more severe depressive symptoms. A cutoff score of 10 and 20 represents mild and severe levels of depressive symptoms, respectively. The GDS-30 has shown adequate properties in the Chinese elderly (23). In the conditional logistic regression, GDS score was categorized into two groups: 0–10 means without depressive symptoms; 11–30 means with depressive symptoms.
Hopelessness
We used the Beck's Hopelessness Scale (BHS-4) to measure hopelessness in the last week before death/investigation (24). It consists of four items relevant to success, dark future, breaks, and faith. Each item is rated on a five-point scale ranging from 1 (strongly agree) to 5 (strongly disagree). A total score ranges from 4 to 20, with a higher score representing a higher level of hopelessness (24). We categorized the severity of hopelessness into two groups according to the median of BHS score.
Data Combination
We combined the information provided by the two informants as the proxy data for each suicide decedent and living comparison. For sociodemographic characteristics, we relied on the data provided by the first informant. Regarding psychosocial factors, we used information that was hypothetically associated with elevated suicide risk, considering any targeting symptoms or behaviors might exist as long as any informant may have observed (20, 25). Hence, we used the higher score of pain intensity, perceived burden, and BHS-4, and the lower score of DSSI for analysis; similarly, a positive answer of an item of GDS-30 was used if one of the two informants reported positive. We used the proxy data for analysis.
Although we could not confirm whether the suicide decedents actually had those symptoms, such as depressive symptoms, all analyses were conducted under the premise that the validity of proxy-based information has been proved fair. We used the intraclass correlation coefficient (ICC) to evaluate the agreement between subject-based and proxy-based information. For the GDS-30, subject–proxy concordance was fair (ICC = 0.590). Based on the proxy data, Cronbach's alpha was 0.871 among suicide decedents and 0.889 among the living comparisons, demonstrating good internal reliability (26). For BHS-4, the subject–proxy agreement was good (ICC = 0.682). The Cronbach's alpha was 0.834 (27). Moreover, the subject–proxy agreements on pain intensity (ICC = 0.504) and perceived burden (ICC = 0.487) were fair. Nonetheless, the validity of proxy evaluation should be considered with extreme caution.
Statistical Analyses
Descriptive analysis, chi-squared tests for categorical variables, and Student's t-tests for continuous variables were used to describe and compare the socio-demographics, pain intensity, perceived burden, hopelessness, and depressive symptoms of suicide cases and living controls. Conditional logistic regression (backward stepwise selection) was used to assess the association between pain intensity and completed suicide. Covariates adjusted were as follows: marital status, employment status, education level, annual family income, physical disease, social support, depressive symptoms, hopelessness, and perceived burden.
Mediation analysis was conducted to assess the specific contribution of depressive symptoms, hopelessness, and perceived burden in the pain–suicide association. The KHB method can be used to decomposes total effect (the effect of pain on suicide without adjustment of mediators) into direct effect (the effect of pain on suicide) and indirect effects (the mediation effects from depressive symptoms, hopelessness, and perceived burden) in conditional logistic regression (28, 29). Moreover, the confounding percentage to total effect due to mediators and the disentangle contribution of each mediator can be calculated. Marital status, employment status, education level, annual family income, physical disease, and social support were controlled in the mediation analysis. The mediation analysis was performed with the khb command. Entering method, rather than backward stepwise selection, was used in mediation analysis since the khb command is not supported by stepwise method. All analysis was performed using Stata 16.0 (College Station, Texas 77845, USA). The level of statistical significance was set at p < 0.05.
Results
Characters of Suicide Decedents and Living Comparisons
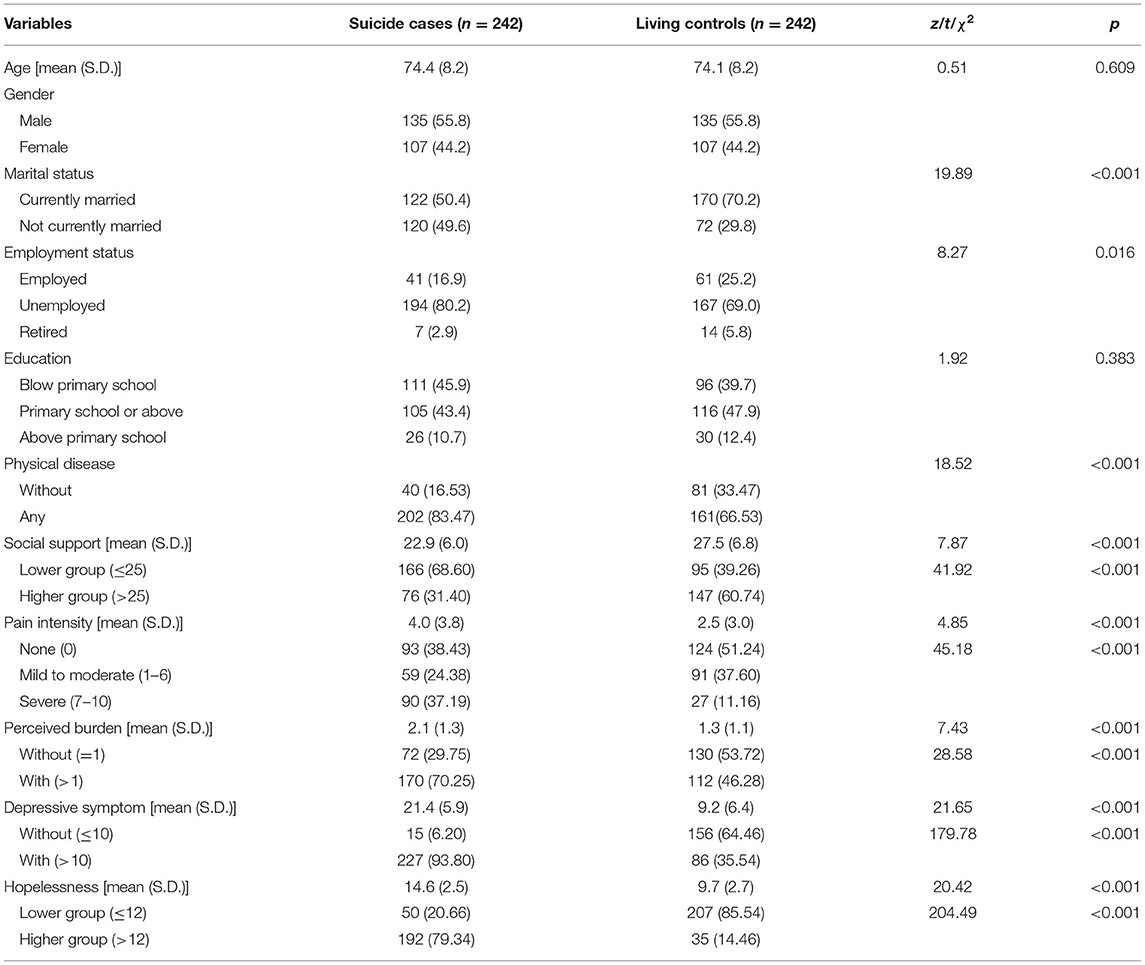
We investigated 242 suicide decedents and 242 living decedents. The mean age was 74.4 ± 8.2 years, and 55.8% were male among the suicides. The mean age was 74.1 ± 8.2 years, and 55.8% were male among living comparisons. Compared with the living controls, the suicides tended to be not currently married, unemployed, and with physical disease (all p-values <0.05). Suicide cases reported higher pain intensity, more perceived burden, higher level of depressive symptoms and hopelessness, and lower level of social support than living controls (all p-values <0.01). Descriptive data for study variables are presented in Table 1.
Logistic Regression Analysis
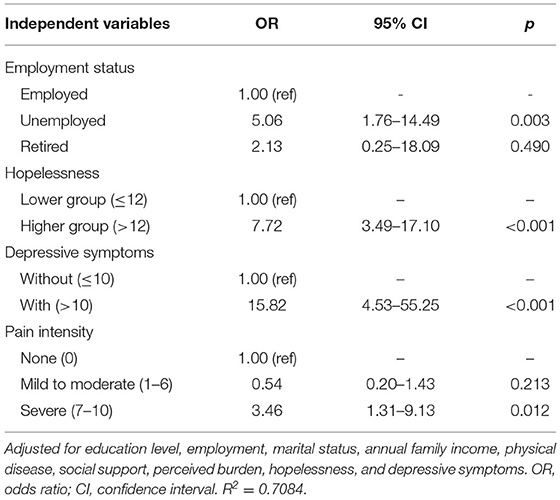
Conditional logistic regression was employed to detect risk factors of suicide completion among older adults in rural China. As shown in Table 2, unemployment [odds ratio (OR) = 5.06, 95% confidence interval (CI): 1.76–14.49], higher level of hopelessness (OR = 7.72, 95% CI: 3.49–17.10), depressive symptom (OR = 15.82, 95% CI: 4.53–55.25), and severe pain (OR = 3.46, 95% CI: 1.31–9.13) were significantly associated with suicide completion. Mild to moderate (OR = 0.54; 95% CI: 0.20–1.43) pain was not significantly associated with suicide completion.
Mediation Analysis
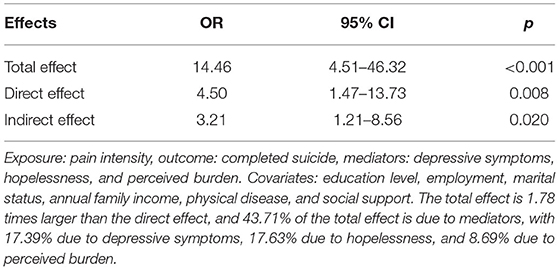
The results of the mediation analysis are shown in Table 3. To simplify interpretation of OR, pain intensity was dichotomized as “moderate or less” and “severe” because increased risk of suicide completion was observed only in the older adults with severe pain. Depressive symptoms, hopelessness, and perceived burden significantly mediated the association between pain and completed suicide (p = 0.020). The total effect of pain intensity on suicide completion was 1.78 times larger than the direct effect, and 43.71% of the total effect was due to mediators (indirect effect). In terms of the specific contributions of mediators, depressive symptoms explained 17.39% of the association between severe pain and suicide completion, hopelessness explained 17.63%, and perceived burden explained 8.69%. Depressive symptoms alone could not significantly mediate pain–suicide association. Nor could hopelessness, or perceived burden. Any combinations of two factors did not have a significant mediational effect (all p > 0.05) (Supplementary Material).
Discussion
As of our knowledge, our study is the first one to use suicide completion as the outcome to investigate the mediation effect of depressive symptoms, hopelessness, and perceived burden on the pain–suicide association and to quantify the individual mediational effect. We find that pain was an independent risk factor of suicide completion in older adults in rural China. Furthermore, our results indicated that depressive symptoms, hopelessness, and perceived burden significantly but partially mediated the pain–suicide association.
Previous studies found that patients with pain had increased risk of suicidal outcomes compared with the general population. A large cohort study demonstrated that veterans with self-reported severe pain were more likely to die by suicide than patients experiencing moderate or less pain (HR: 1.33, 95% CI: 1.15–1.54) (30). A case–control study among older adults in Canada also found that severe pain (OR: 4.07, 95% CI: 2.51–6.59) elevated the risk of suicide death (31). However, the study only considered patients with prescribed pain medication. Consistent with previous studies, the present study found that severe pain was more common in suicide cases than in controls (37.19% vs. 11.16%). We proved that older adults with severe pain predicted 3.46 times of suicide completion risk than those without pain. Older adults with severe pain may view suicide as a way to escape from suffering (32). The risk for suicide among the older population with severe pain merits particular attention.
One major finding was that 56.29% of the total effect of pain intensity on suicide was from pain directly, and perceived burden, hopelessness, and depressive symptoms significantly mediated 43.71% of the association between pain and suicide. These results were consistent with one recent study proving that depression and anxiety disorders had mediational effects on the relationships between pain and suicidal behaviors (17). Though this study only used suicide ideation and suicide attempt as outcomes, the study used a large, representative sample of the English adult population to prove the partial mediation effect of depression. However, several studies found different results that the pain–suicide ideation relationship was fully mediated by depression (18, 33). A possible reason for this discrepancy might be due to the different outcomes (suicide completion vs. suicidal ideation/attempt) and different populations across these studies.
Moreover, we measured the individual mediational effect. Depressive symptoms, hopelessness, and perceived burden explained 17.39, 17.63, and 8.69% of the total effect of pain intensity on suicide completion, respectively. Many studies suggested that hopelessness significantly predicted suicidal behaviors. A meta-analysis of longitudinal studies found that hopelessness significantly predicted suicidal ideation, suicide attempt, and suicide death (34). Moreover, helplessness/hopelessness in patients with pain has been reported as a significant predictor of suicidal ideation in previous studies (9, 15, 35). Our results suggest that further investigation should focus more on hopelessness in the pain–suicide association.
Consistent with prior evidences (36), we also found the mediating effect of the perceived burden on the pain–suicide association. The interpersonal theory of suicide proposed that thwarted belongingness and perceived burdensomeness were key factors contributing to a suicide desire (14). Perceived burden has been identified as a critical predictor of suicidality in patients with pain (15, 37). It is reasonable to expect that the older adults suffering from pain felt that they created a burden to their family. The current finding provided further evidence for the need to consider perceived burdens in preventing suicide for older adults with pain in rural areas.
Previous studies have reported depression as the most common mental illness among suicide decedents (20, 38, 39). Moreover, higher pain severity was a significant predictor of the onset of depression (40). Our results are in line with previous evidence. We further demonstrated that depression partially mediated the impact of pain on suicide.
Interestingly, we found that only depressive symptoms could not mediate the association between pain and suicide completion. Nor did the perceived burden or hopelessness. The relationship between pain and suicide is complex and involves several psychological and psychosocial factors (32). Moreover, those factors might interact with each other, and the interactions may affect the pain–suicidality relationship. A study in back pain patients found that pain intensity showed indirect effects due to pain-related helplessness/hopelessness on depression (41). Depressive symptoms were found to be a significant predictor of self-perceived burdensomeness in patients with chronic pain (42). Furthermore, a community-based study suggested that hopelessness and the interaction between perceived burdens and hopelessness were significantly associated with suicide plans and attempts (43).
Depression, hopelessness, and perceived burden might interact with and exacerbate each other, finally increasing the vulnerability to commit suicide. Though we found the mediators and their respective indirect effects, further studies on the interactions among mediators are needed for a comprehensive understanding of pain–suicide association.
The current study has several limitations. First, though psychological autopsy is a widely used method to explore the risk factors of completed suicide, the validity of data provided by proxy informants is a concern. However, previous studies had proved that subject–proxy concordance for the GDS-30 and BHS-4 were fair in the living controls (26). Second, we measured pain with a single question concerning the intensity of pain without data on the location, type, and duration. More detailed questions on pain might be better for the comprehensive understanding between pain and suicide completion. However, most research generally examines only a limited number of types or locations of pain. Moreover, a review had suggested that pain itself, irrespective of which type or location, was a determinant of suicidality based on abundant evidence (44). Furthermore, it seems that there is no strong link between pain duration and suicidality. As the duration of suffering pain increases, suicidal behaviors may be less related to pain symptoms (44). Also, prior studies had demonstrated that sleep disturbance was a mediator in the pain–suicidality link (19). Nevertheless, we did not include information on sleep quality. Further research is warranted to examine this possibility. Finally, we estimated the pain–suicide death association and mediational effects in older adults in rural China. The results might not be suitable to generalize to older adults in other areas and should be interpreted with caution.
Conclusions
Despite these limitations, our study added to a growing body of evidence indicating that pain independently increased the risk of committing suicide and that perceived burden, hopelessness, and depressive symptoms partially mediated the pain–suicide association. Given the undertreated pain in late life and backward mental health services in rural areas, regular screening of pain, depressive symptoms, hopelessness, and perceived burden using simple but sensitive questions or scales for older adults with pain is vital for the prevention and early detection of suicide risk. Furthermore, treatment of pain and psychological interventions for alleviating depressive symptoms and feelings of hopelessness are critical for suicide prevention.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Boards of Central South University, Shandong University, and Guangxi Medical University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
CJ, ZM, and LZ contributed to the study design. GW contributed to data collection. JW and JX conducted the data analysis. JW drafted the article. LZ provided substantial editorial input in the drafting of the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the American Foundation for Suicide Prevention [Grant No. SRG-0-169-12] and Science and Technology Plan Project of Guangdong Province [No. 2019B030316001].
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank all fieldworkers and participants of this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.779178/full#supplementary-material
References
1. Li M, Katikireddi SV. Urban-rural inequalities in suicide among elderly people in China: a systematic review and meta-analysis. Int J Equity Health. (2019) 18:2. doi: 10.1186/s12939-018-0881-2
2. Zhong BL, Chiu HF, Conwell Y. Rates and characteristics of elderly suicide in China, 2013-14. J Affect Disord. (2016) 206:273–9. doi: 10.1016/j.jad.2016.09.003
3. Brown ST, Kirkpatrick MK, Swanson MS, McKenzie IL. Pain experience of the elderly. Pain Manag Nurs. (2011) 12:190–6. doi: 10.1016/j.pmn.2010.05.004
4. Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, et al. Prevalence of chronic pain and high-impact chronic pain among adults–United States, 2016. MMWR Morb Mortal Wkly Rep. (2018) 67:1001–6. doi: 10.15585/mmwr.mm6736a2
5. Wong WS, Fielding R. Prevalence and characteristics of chronic pain in the general population of Hong Kong. J Pain. (2011) 12:236–45. doi: 10.1016/j.jpain.2010.07.004
6. Calati R, Bakhiyi CL, Artero S, Ilgen M, Courtet P. The impact of physical pain on suicidal thoughts and behaviors: meta-analyses. J Psychiatr Res. (2015) 71:16–32. doi: 10.1016/j.jpsychires.2015.09.004
7. Ilgen MA, Kleinberg F, Ignacio RV, Bohnert AS, Valenstein M, McCarthy JF, et al. Noncancer pain conditions and risk of suicide. JAMA Psychiatry. (2013) 70:692–7. doi: 10.1001/jamapsychiatry.2013.908
8. Park MJ, Choi KW, Na EJ, Hong JP, Cho MJ, Fava M, et al. Multiple types of somatic pain increase suicide attempts and depression: a nationwide community sample of Korean adults. Compr Psychiatry. (2019) 90:43–8. doi: 10.1016/j.comppsych.2018.12.006
9. Racine M, Sanchez-Rodriguez E, Galan S, Tome-Pires C, Sole E, Jensen MP, et al. Factors associated with suicidal ideation in patients with chronic non-cancer pain. Pain Med. (2017) 18:283–93. doi: 10.1093/pm/pnw115
10. Bromberg MH, Law EF, Palermo TM. Suicidal ideation in adolescents with and without chronic pain. Clin J Pain. (2017) 33:21–7. doi: 10.1097/AJP.0000000000000366
11. Tang NK, Crane C. Suicidality in chronic pain: a review of the prevalence, risk factors and psychological links. Psychol Med. (2006) 36:575–86. doi: 10.1017/S0033291705006859
12. Orbach I, Mikulincer M, King R, Cohen D, Stein D. Thresholds and tolerance of physical pain in suicidal and nonsuicidal adolescents. J Consult Clin Psychol. (1997) 65:646–52. doi: 10.1037/0022-006X.65.4.646
13. Ribeiro JD, Witte TK, Van Orden KA, Selby EA, Gordon KH, Bender TW, et al. Fearlessness about death: the psychometric properties and construct validity of the revision to the acquired capability for suicide scale. Psychol Assess. (2014) 26:115–26. doi: 10.1037/a0034858
14. Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE. Jr. The interpersonal theory of suicide. Psychol Rev. (2010) 117:575–600. doi: 10.1037/a0018697
15. Wilson KG, Heenan A, Kowal J, Henderson PR, McWilliams LA, Castillo D. Testing the interpersonal theory of suicide in chronic pain. Clin J Pain. (2017) 33:699–706. doi: 10.1097/AJP.0000000000000451
16. Fishbain DA, Lewis JE, Gao J. The pain suicidality association: a narrative review. Pain Med. (2014) 15:1835–49. doi: 10.1111/pme.12463
17. Jacob L, Maria Haro J, Koyanagi A. The association between pain and suicidal behavior in an English national sample: the role of psychopathology. J Psychiatr Res. (2018) 98:39–46. doi: 10.1016/j.jpsychires.2017.12.007
18. Lewcun B, Kennedy TM, Tress J, Miller KS, Sherker J, Sherry DD. Predicting suicidal ideation in adolescents with chronic amplified pain: the roles of depression and pain duration. Psychol Serv. (2018) 15:309–15. doi: 10.1037/ser0000210
19. Owen-Smith AA, Ahmedani BK, Peterson E, Simon GE, Rossom RC, Lynch FL, et al. The mediating effect of sleep disturbance on the relationship between nonmalignant chronic pain and suicide death. Pain Practice. (2019) 19:382–9. doi: 10.1111/papr.12750
20. Zhou L, Wang G, Jia C, Ma Z. Being left-behind, mental disorder, and elderly suicide in rural China: a case-control psychological autopsy study. Psychol Med. (2019) 49:458–64. doi: 10.1017/S003329171800106X
21. Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. Pain. (1999) 83:157–62. doi: 10.1016/S0304-3959(99)00101-3
22. Zhang J, Conwell Y, Wieczorek WF, Jiang C, Jia S, Zhou L. Studying Chinese suicide with proxy-based data: reliability and validity of the methodology and instruments in China. J Nerv Ment Dis. (2003) 191:450–7. doi: 10.1097/01.NMD.0000081613.03157.D9
23. He X, Xiao S, Zhang G. Reliability and validity of the chinese version of geriatric depression scale: a study in a population of chinese rural community-dwelling elderly. Chin J Clin Psychol. (2008) 16:473–5. doi: 10.16128/j.cnki.1005-3611.2008.05.003
24. Yip PS, Cheung YB. Quick assessment of hopelessness: a cross-sectional study. Health Qual Life Outcomes. (2006) 4:13. doi: 10.1186/1477-7525-4-13
25. Zhang J, Wang Y, Fang L. How to integrate proxy data from two informants in life event assessment in psychological autopsy. BMC Psychiatry. (2018) 18:115. doi: 10.1186/s12888-018-1698-7
26. Niu L, Jia C, Ma Z, Wang G, Yu Z, Zhou L. Validating the geriatric depression scale with proxy-based data: a case-control psychological autopsy study in rural China. J Affect Disord. (2018) 241:533–8. doi: 10.1016/j.jad.2018.08.066
27. Ma Z, He Q, Nie G, Jia C, Zhou L. Reliability and validity of short Beck Hopelessness Scale in psychological autopsy study among Chinese rural elderly. Int Psychogeriatr. (2020) 32:525–31. doi: 10.1017/S1041610219001315
28. Breen R, Karlson KB, Holm A. Total, direct, and indirect effects in logit and probit models. Sociol Methods Res. (2013) 42:164–91. doi: 10.1177/0049124113494572
29. Kohler U, Karlson, K,. KHB: Stata Module to Decompose Total Effects Into Direct Indirect Via KHB-Method. (2010). Available online at: https://ideas.repec.org/c/boc/bocode/s457215.html (accessed February 24, 2019).
30. Ilgen MA, Zivin K, Austin KL, Bohnert AS, Czyz EK, Valenstein M, et al. Severe pain predicts greater likelihood of subsequent suicide. Suicide Life Threat Behav. (2010) 40:597–608. doi: 10.1521/suli.2010.40.6.597
31. Juurlink DN, Herrmann N, Szalai JP, Kopp A, Redelmeier DA. Medical illness and the risk of suicide in the elderly. Arch Intern Med. (2004) 164:1179–84. doi: 10.1001/archinte.164.11.1179
32. Hooley JM, Franklin JC, Nock MK. Chronic pain and suicide: understanding the association. Curr Pain Headache Rep. (2014) 18:435. doi: 10.1007/s11916-014-0435-2
33. Cho S, Hwang H, Lee J-H. Pain intensity and suicidal ideation of people in chronic pain: mediating effects of depression. Soc Behav Pers. (2013) 41:509–16. doi: 10.2224/sbp.2013.41.3.509
34. Ribeiro JD, Huang X, Fox KR, Franklin JC. Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. Br J Psychiatry. (2018) 212:279–86. doi: 10.1192/bjp.2018.27
35. Racine M, Choiniere M, Nielson WR. Predictors of suicidal ideation in chronic pain patients: an exploratory study. Clin J Pain. (2014) 30:371–8. doi: 10.1097/AJP.0b013e31829e9d4d
36. Shim E, Song YW, Park SH, Lee KM, Go DJ, Hahm BJ. Examining the relationship between pain catastrophizing and suicide risk in patients with rheumatic disease: the mediating role of depression, perceived social support, and perceived burdensomeness. Int J Behav Med. (2017) 24:501–12. doi: 10.1007/s12529-017-9648-1
37. Fishbain DA, Bruns D, Bruns A, Gao J, Lewis JE, Meyer LJ, et al. The perception of being a burden in acute and chronic pain patients is associated with affirmation of different types of suicidality. Pain Med. (2016) 17:530–8. doi: 10.1111/pme.12889
38. Zhang J, Zhou L. A case control study of suicides in China with and without mental disorder. Crisis. (2009) 30:68–72. doi: 10.1027/0227-5910.30.2.68
39. Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M. Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet. (2002) 360:1728–36. doi: 10.1016/S0140-6736(02)11681-3
40. Gerrits MMJG, van Oppen P, van Marwijk HWJ, Penninx BWJH, van der Horst HE. Pain and the onset of depressive and anxiety disorders. Pain. (2014) 155:53–9. doi: 10.1016/j.pain.2013.09.005
41. Hulsebusch J, Hasenbring MI, Rusu AC. Understanding pain and depression in back pain: the role of catastrophizing, help-/hopelessness, and thought suppression as potential mediators. Int J Behav Med. (2016) 23:251–9. doi: 10.1007/s12529-015-9522-y
42. Kowal J, Wilson KG, McWilliams LA, Péloquin K, Duong D. Self-perceived burden in chronic pain: relevance, prevalence, and predictors. Pain. (2012) 153:1735–41. doi: 10.1016/j.pain.2012.05.009
43. Kleiman EM, Liu RT, Riskind JH. Integrating the interpersonal psychological theory of suicide into the depression/suicidal ideation relationship: a short-term prospective study. Behav Ther. (2014) 45:212–21. doi: 10.1016/j.beth.2013.10.007
Keywords: suicide, older adults, depressive symptoms, hopelessness, perceived burden, pain intensity
Citation: Wang J, Xu J, Ma Z, Jia C, Wang G and Zhou L (2021) The Mediating Role of Depressive Symptoms, Hopelessness, and Perceived Burden on the Association Between Pain Intensity and Late-Life Suicide in Rural China: A Case–Control Psychological Autopsy Study. Front. Psychiatry 12:779178. doi: 10.3389/fpsyt.2021.779178
Received: 18 September 2021; Accepted: 04 November 2021;
Published: 13 December 2021.
Edited by:
Debanjan Banerjee, Private Practitioner, Kolkata, IndiaReviewed by:
Bhavika Vajawat, National Institute of Mental Health and Neurosciences (NIMHANS), IndiaSiddharth Sarkar, All India Institute of Medical Sciences, India
Copyright © 2021 Wang, Xu, Ma, Jia, Wang and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liang Zhou, bGlhbmd6aG91X2NzdUB2aXAuMTYzLmNvbQ==
 Jiali Wang
Jiali Wang Jiahuan Xu2
Jiahuan Xu2 Zhenyu Ma
Zhenyu Ma Cunxian Jia
Cunxian Jia Liang Zhou
Liang Zhou