- 1Department of Orthopedics, Hwa Mei Hospital, University of Chinese Academy of Sciences, Ningbo, China
- 2Ningbo Institute of Life and Health Industry, University of Chinese Academy of Sciences, Ningbo, China
- 3Department of Orthopedics, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 4Department of Social Medicine and Health Management, School of Public Health, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Background: Few studies have focused on depressive symptoms among patients with chronic low back pain in China. The aim of this cross-sectional study was to assess the prevalence and associated factors of depressive symptoms in patients with chronic low back pain.
Methods: From May to August 2021, 1,172 patients with chronic low back pain were recruited in China. Depressive symptoms were assessed through the Patient Health Questionnaire. Associations of demographic characteristics, clinical characters and social-psychological factors with depressive symptoms were investigated among patients with chronic low back pain.
Results: The prevalence of depressive symptoms was 25.00%. Logistic regression analysis found that duration of pain in 1-5 years (1-3 years: OR = 2.91, 95%CI: 1.65-5.14, 3-5 years: OR = 3.09, 95%CI: 1.55-6.15) and more severe pain (OR = 1.13, 95%CI: 1.10-1.17) were associated with higher risks of depressive symptoms. Better family function (good family function: OR = 0.25, 95%CI: 0.15-0.41, moderate family dysfunction: OR = 0.47, 95%CI: 0.29-0.77) and higher pain self-efficacy (OR = 0.94, 95%CI: 0.93-0.95) were associated with lower risks of depressive symptoms.
Conclusion: Patients with chronic low back pain have a high prevalence of depressive symptoms in China. Duration of pain, pain severity, family function and pain self-efficacy were predictors of depressive symptoms among chronic low back pain patients in China. Early identification of the associated factors may be helpful for the timely management of depressive symptoms.
Introduction
Low back pain is a worldwide public health issue (1). And of which, chronic low back pain (CLBP), as a chronic health problem, has attracted much attention due to its features of persistent suffering, high disability rate and heavy medical burden (2). Studies have shown that the prevalence of CLBP has been increasing in recent years, with some countries reaching over 20%, such as Brazil (25%) and Norway (23.6%) (2–4). CLBP not only causes long-term suffering for patients, impairs their physical function and even results in disability, but also increases personal and social medical costs (5–7). Moreover, with the prolongation of pain and the progress of the disease, the risk of psychological problems in patients with CLBP also increased significantly (6).
Depressive symptoms are the most common mental health problem in patients with CLBP (8). And the prevalence of depressive symptoms in patients with CLBP is higher than that of the general population. A previous large-scale study using South Korea national representative population data showed that the prevalence of depressive symptoms in patients with CLBP was as high as 20.3%, which is much higher than 4.5% of the general population (9). A longitudinal study in Spain also showed that patients with chronic pain (such as CLBP) were 1.4 times more likely to have depressive symptoms than patients without chronic pain (8). CLBP patients with depressive symptoms will not only increase the risk of disability and decrease the quality of life, but also lead to an increase in medical costs (10–12). A previous study revealed that CLBP patients with severe depressive symptoms have a higher disability index, and depressive symptoms are the most powerful explanation for their increased disability index (11). A systematic review also found that the direct medical costs of CLBP patients with psychiatric disorders have increased significantly (12).Therefore, it is necessary to explore the prevalence of depressive symptoms and related factors in CLBP patients, thereby developing effective intervention strategies.
China has a large group of patients with CLBP due to its large population base. According to the literature, 67.3 million people in China suffered from CLBP in 2016, causing a heavy burden of disease (13). The results of the Global Burden of Disease study also showed that CLBP was the leading cause of years lived with disability in China, and it is of great significance for patients and society to have a good management of CLBP (14). However, there has been little research on the prevalence and associated factors of depressive symptoms in CLBP patients in China. Therefore, this study aimed to investigate the prevalence of depressive symptoms in CLBP patients attending hospitals and explore its related factors to provide relevant evidence for promoting the mental health of CLBP patients.
Materials and Methods
Ethics Statement
The study was approved by the Ethics Committee of Ningbo No.2 Hospital, Zhejiang, China. All participants were voluntary and provided written informed consent before being involved in the study. All data of participants were kept anonymous and confidential.
Participants and Sampling
This study adopted the convenience sampling method to select a general hospital in Ningbo, Zhejiang province and Wuhan, Hubei province in China, respectively, as the study sites. Patients with CLBP admitted to Tongji Hospital in Wuhan and the Ningbo No.2 Hospital in Ningbo during May to August 2021 were invited to participate in this survey. The inclusion criteria included: (1) aged ≥ 18 years, (2) duration of low back pain ≥ 3 months, (3) a native Chinese speaker, (4) volunteer to participate in this survey. Participants were excluded if they: (1) had a trauma or surgery on the low back within the past year, (2) had a pregnancy within the past year, (3) diagnosed severe psychiatric diseases.
We calculated the minimum sample size by a single population proportion formula: n = , where n is the sample size, p is the proportion of depressive symptoms among CLBP patients, z is the normal deviation, and d is the margin of error. In order to control type I error, we took α as 0.05; therefore, z was equal to 1.96. Based on previous research on the depressive symptoms among CLBP patients, p was assumed to be 20.3% (9). Besides, we took d as 0.15p. The calculated minimum sample size was 670. In this study, allowing a non-response rate of 20% and the final sample size was 838.
Measures
The Patient health questionnaire (PHQ-9) was used to assess depressive symptoms, which consisted of 9 items (15). Each item is evaluated by the frequency of the symptom over the last 2 weeks: “Not at all” scored 0, “Several days” scored 1, “More than half the days” scored 2, and “Nearly every day” scored 3. The total score ranges from 0 to 27, with a cut-off point of 10 differentiating depressive symptom and no depressive symptom. The PHQ-9 has been validated in Chinese patients with good reliability and validity in previous studies (16, 17). In this study, Cronbach's alpha coefficient of this scale was 0.94.
To control for the influence of potential confounding factors on depressive symptoms, we collected information on demographic characteristics, clinical characters (pain severity and duration of pain), family functioning, and pain self-efficacy. The demographic characteristics included sex, age, work status, marital status, educational level, monthly personal income, and medical insurance.
The four-item Chinese version Brief Pain Inventory subscale on pain severity (BPI-PS) was used to assess pain intensity (18). The scale has been widely used in patients with low back pain (19). The four items of BPI-PS included pain severity at “its worst” over the past 24 h, “its least” over the past 24 h, “on average” over the past 24 h, and “right now”. Patients were asked to rate the extent to pain from 0 (no pain) to 10 (pain as bad as you can imagine) at above four moments. The total score of BPI-PS ranges from 0 to 40, with higher scores indicating more severe pain. In this study, the BPI-PS had a good internal consistency (Cronbach's alpha = 0.92).
The Chinese version of the Family Adaptation, Partnership, Growth, Affection, Resolve (APGAR) index was used to evaluate participants' satisfaction with current family function, which consisted of five items, namely, adaptability, partnership, growth, affection, and resolve (20, 21). Each item was scored 0, 1, and 2 according to its response “Hardly Ever,” “Some of the time,” and “Almost Always.” The total score ranges from 0 to 10 and has been divided into three levels: 0-3 indicates severe family dysfunction, 4-6 indicates moderate family dysfunction, and 7-10 indicates good family function (22, 23). Previous studies have proven to excellent validity and reliability of the scale in Chinese families (22, 23). In this study, Cronbach's alpha coefficient of this scale was 0.88.
Pain self-efficacy was measured through the Chinese version of the Pain Self-efficacy Questionnaire (PSEQ), which has shown excellent validity and reliability in patients with CLBP (24, 25). PSEQ is a psychometric scale, which reflects an individual's confidence in completing daily tasks despite experiencing pain. The scale consists of 10 items rated on a seven-point Likert scale from 0 (lowest confidence) to 6 (highest confidence). Hence, the total score for PSEQ ranges from 0 to 60, where high scores reflect higher pain self-efficacy. In this study, the scale demonstrated good internal consistency (Cronbach's alpha = 0.98).
Statistical Analysis
The normality of continuous variables was test by the Shapiro-Wilk method. Due to the distribution of all continuous variables did not satisfy the normality (P < 0.05), continuous variables were showed by medians and quartiles. Categorical variables were showed by frequencies and percentages. We used Wilcoxon rank-sum test for continuous variables, and Pearson's chi-squared test for categorical variables to compare the demographic characteristics, pain-related variables, and family function between patients with or without depressive symptoms. The binary logistic regression was conducted to assess the association between outcomes and different explanatory variables. We also used stepped modeling approach to compare the fit of three sets of variables. Model 1 only contained individual characteristics; Model 2 contained both individual and pain-related factors; Model 3 was a full model which also included family function. Parameters including −2log likelihood, Akaike's information criterion (AIC) and Schwarz criterion (SC) were used to compare these multilevel models. The −2log likelihood, AIC and SC of Model 1, Model 2, and Model 3 became smaller, indicating that the fit of the models improved (Supplementary Table S1). The Hosmer-Lemeshow goodness-of-fit test was used to examine model fitness, and its P-value was >0.05 (P = 0.9257). The strength of association was interpreted using odds ratio (OR) and 95% confidence interval (CI). All P-values were two-tailed and significance level was set at 0.05. The statistical analysis was conducted using SAS 9.4 software.
Results
A total of 1,238 patients with CLBP who met the inclusion criteria were included in this study, and 66 patients who did not complete the questionnaire were excluded. Ultimately, 1,172 patients were included in the analysis. The characteristics of participants and their association with depressive symptoms are presented in Table 1. The median age of the participants was 50.5 years, and the percentage of male was 50.00%. Most participants were married (82.08%), secondary school (29.69%), non-manual worker (38.57%), low-income group (58.19%), with medical insurance (89.16%), with good family function (54.86%), with the duration of pain <6 months (35.32%). The median score of the participants with respect to pain severity and pain self-efficacy was 12 and 41, respectively.
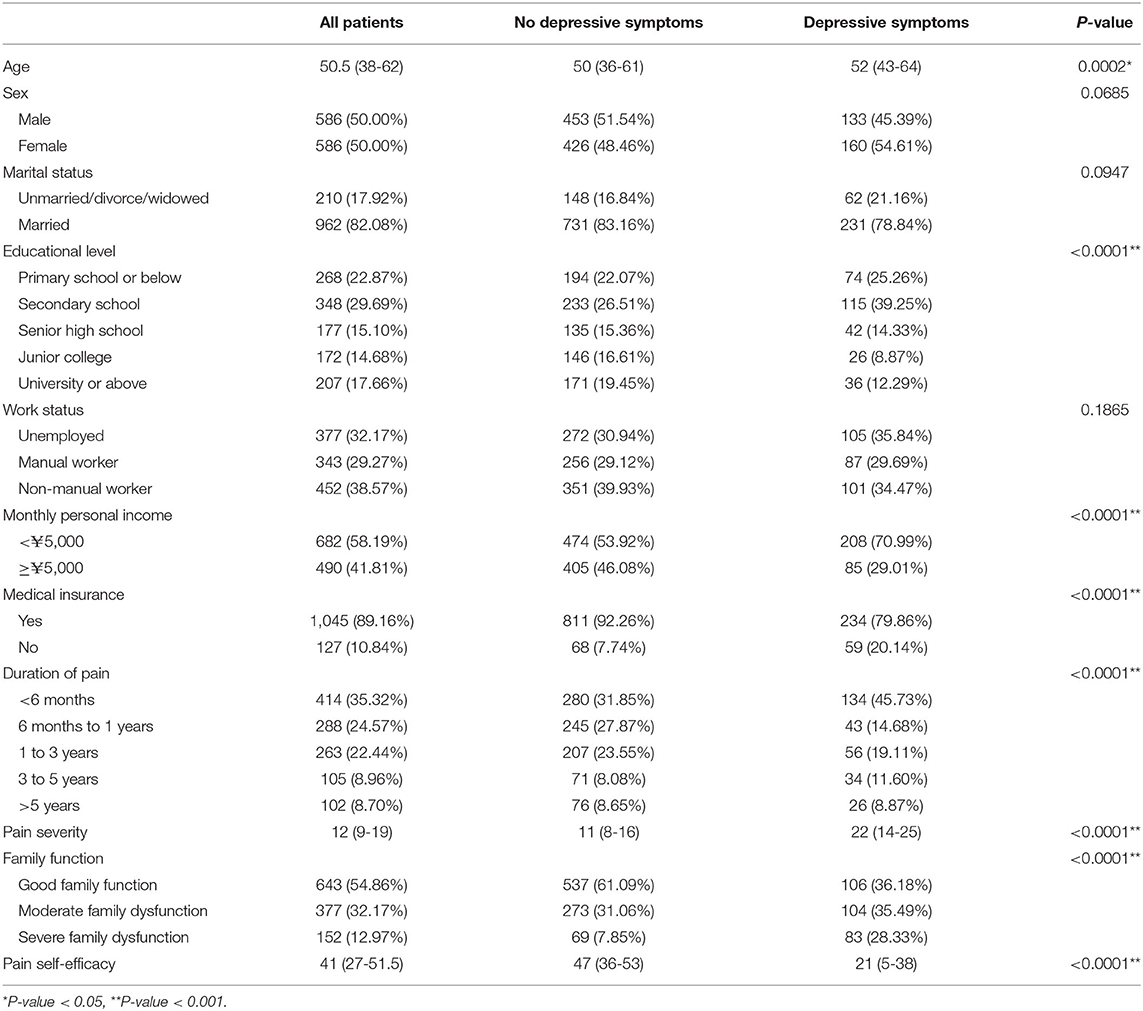
Table 1. Demographic and clinical characteristics of patients with chronic low back pain according to presence of depressive symptoms.
In this study, the prevalence of depressive symptoms in participants was 25.00% (n = 292). The univariable analysis showed that age, educational level, monthly personal income, medical insurance, duration of pain, family function, the score of pain severity and pain self-efficacy were significantly different between patients with and without depressive symptom (Table 1).
Logistic regression analysis showed that duration of pain, pain severity, family function, pain self-efficacy was significantly associated with depressive symptoms. The results found that patients with pain duration of 1-3 years (OR = 2.91, 95% CI: 1.65-5.14) and 3-5 years (OR = 3.09, 95% CI: 1.55-6.15) were more likely to suffer from depressive symptoms than those with a duration of <6 months. Patients with CLBP who had higher scores of pain severity were at higher risk of developing depressive symptoms (OR = 1.13, 95% CI: 1.10-1.17), while higher score of pain self-efficacy was associated with a decreased likelihood of depressive symptoms (OR = 0.94, 95% CI: 0.93-0.95). Compared to those with severe family dysfunction, those with good family function (OR = 0.25, 95% CI: 0.15-0.41) and moderate family dysfunction (OR = 0.47, 95 % CI: 0.29-0.77) were less likely to have depressive symptoms (Table 2).
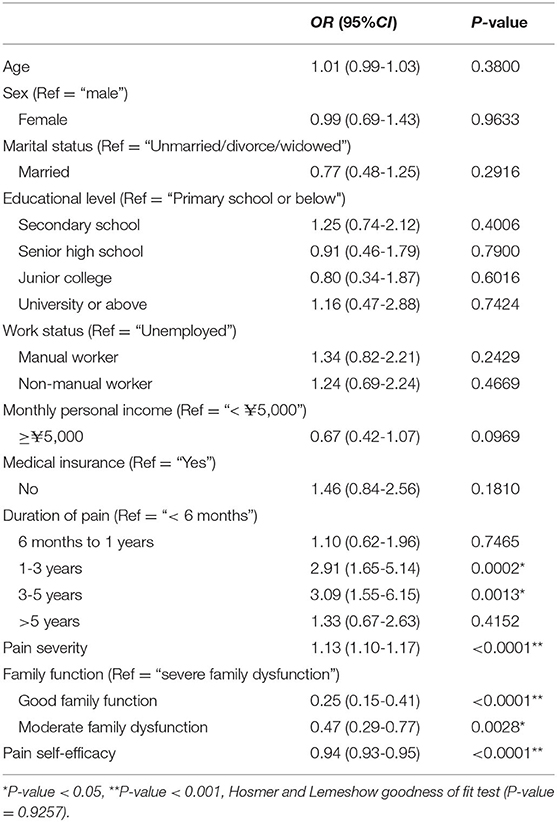
Table 2. Binary Logistic analysis of depressive symptoms related factors in patients with chronic low back pain.
Discussion
The results of this study showed that the prevalence of depressive symptoms in patients with CLBP in China was 25.00%, significantly higher than that in Chinese community-dwelling population (12.30%) (26). This finding was consistent with previous studies (9, 27). The high prevalence of depressive symptoms may be related to the pain of the disease and its negative effects on life (28). Compared with international studies of depressive symptoms in CLBP patients using the PHQ-9 to assess depressive symptoms, our result was higher than those in Korea (20.3%) (9) and Japan (16.47%) (28), which also suggested that health authorities should pay more attention to the problem of severe depressive symptoms in patients with CLBP in China.
Notably, there is no significant association between medical insurance and depressive symptoms in CLBP patients in this study. This result is contrary to studies in some countries in Southeast Asia (29, 30). This may be because China started to establish a basic medical insurance system covering all people in 2009. Statistics showed that the basic medical insurance coverage rate in China has been as high as 95% by 2020 (31). This is consistent with nearly 90% of the participants in this study with medical insurance.
Pain-related factors were significant related to depressive symptoms in CLBP patients. Our study found that CLBP patients who had pain duration of 1-5 years were at higher risk of developing depressive symptoms, which was similar to previous studies (32, 33). The reason may be that long-term low back pain has a negative impact on the patients' family, social and work activities, which can lead to more prone to depressive symptoms (33). However, in this study, the risk of depressive symptoms did not increase in CLBP patients with a duration of pain more than 5 years. One possible explanation is that as the duration of disease increases, patients may regard pain as more normative and adopt aggressive coping strategies, mitigating the negative effects of disease to physical and psychological health (34). Pain intensity was a risk factor for depressive symptoms in CLBP patients. The results of two previous studies in Japanese CLBP patients showed that more severe pain was associated with worse mental health conditions (28, 35). This suggests that while strengthening pain management of patients with CLBP, it is also important to focus on the psychological status of patients with pain duration of 1-5 years and higher pain severity, thereby timely identifying their psychological problems and providing psychological guidance services.
This study also found that family function was a significant protective factor for depressive symptoms (36–38). When CLBP patients are in a state of family dysfunction, they are more likely to cope with their illness negatively due to conflicting family roles, poor communication, and hampered problem solving, which makes them vulnerable to depressive symptoms (39). In contrast, when family function is good, CLBP patients will get more support from their family members and better cope with the disease and its related adverse emotions (39). In addition, CLBP patients with higher pain self-efficacy had a lower risk of depressive symptoms. Pain self-efficacy refers to the confidence or belief in one's ability to achieve behavioral goals in the context of pain (24). Patients with high levels of pain self-efficacy may make it easier for them to acknowledge the objective reality of the existence of CLBP, to actively manage and cope with the various adverse stresses associated with CLBP, with a correspondingly significantly lower risk of pain-related distress and psychological disorders (40). Therefore, the risk of depressive symptoms in patients with CLBP can be reduced by improving family function and pain self-efficacy.
To our best knowledge, this study is the first to investigate the prevalence of depressive symptoms in Chinese patients with CLBP and to explore the influencing factors in terms of demographic characteristics, clinical characters, individual psychological factors and social factors, which provides evidence for the prevention and treatment of depressive symptoms in patients with CLBP. However, there are some limitations of this study. First, this was a cross-sectional study, and it was difficult to clarify the causal relationship between depressive symptoms and related factors. Second, the convenience sample was adopted in this study, which limited representativeness and generalizability of the results. Third, this study was conducted in two provinces of China, and thus, the generalizability of our results to patients with CLBP in other regions of China may be limited. Further large-scale studies are needed on a national scale.
Conclusion
The prevalence of depressive symptoms is high among Chinese patients with CLBP. In the clinic, CLBP patients with pain duration of 1-5 years should be paid more attention. Moreover, pain should be actively managed to reduce pain intensity in CLBP patients. In addition to the treatment of somatic pathological changes, the psychological well-being of CLBP patients should also be promoted by enhancing patients' family function and pain self-efficacy.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics Statement
The study was approved by the Ethics Committee of Ningbo No.2 Hospital, Zhejiang, China. Participation was voluntary and all participants provided written informed consent before being involved in the study. All data of participants were kept anonymous and confidential.
Author Contributions
YH, ZY, and NG were responsible for the conception, design, and writing of the manuscript. YL and YX were responsible for the acquisition of data and literature research. MT and NJ were responsible for the analysis and interpretation of data. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.820782/full#supplementary-material
Abbreviations
CLBP, chronic low back pain; PHQ-9, Patient health Questionnaire; BPI-PS, Brief Pain Inventory subscale on pain severity; APGAR, Adaptation, Partnership, Growth, Affection, Resolve; PSEQ, Pain Self-efficacy Questionnaire; OR, odds ratio; CI, confidence interval.
References
1. Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. (2012) 64:2028-37. doi: 10.1002/art.34347
2. Alleva J, Hudgins T, Belous J, Kristin Origenes A. Chronic low back pain. Dis Mon. (2016) 62:330-3. doi: 10.1016/j.disamonth.2016.05.012
3. Leopoldino AA, Diz JB, Martins VT, Henschke N, Pereira LS, Dias RC, et al. Prevalence of low back pain in older Brazilians: a systematic review with meta-analysis. Rev Bras Reumatol Engl Ed. (2016) 56:258-69. doi: 10.1016/j.rbr.2016.01.004
4. Heuch I, Hagen K, Heuch I, Nygaard O, Zwart JA. The impact of body mass index on the prevalence of low back pain. the HUNT study. Spine. (2010) 35:764-8. doi: 10.1097/BRS.0b013e3181ba1531
5. Last AR, Hulbert K. Chronic low back pain: evaluation and management. Am Fam Physician. (2009) 79:1067-74. doi: 10.1080/20786204.2010.10873969
6. Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, Guzman J, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: cochrane systematic review and meta-analysis. BMJ. (2015) 350:h444. doi: 10.1136/bmj.h444
7. Manchikanti L, Singh V, Falco FJ, Benyamin RM, Hirsch JA. Epidemiology of low back pain in adults. Neuromodulation. (2014) 17(Suppl 2):3-10. doi: 10.1111/ner.12018
8. Fernandez M, Colodro-Conde L, Hartvigsen J, Ferreira ML, Refshauge KM, Pinheiro MB, et al. Chronic low back pain and the risk of depression or anxiety symptoms. insights from a longitudinal twin study. Spine J. (2017) 17:905-12. doi: 10.1016/j.spinee.2017.02.009
9. Park SM, Kim HJ, Jang S, Kim H, Chang BS, Lee CK, et al. Depression is closely associated with chronic low back pain in patients over 50 years of age: a cross-sectional study using the Sixth Korea National Health and Nutrition Examination Survey (KNHANES VI-2). Spine. (2018) 43:1281-8. doi: 10.1097/BRS.0000000000002595
10. Keeley P, Creed F, Tomenson B, Todd C, Borglin G, Dickens C. Psychosocial predictors of health-related quality of life and health service utilisation in people with chronic low back pain. Pain. (2008) 135:142-50. doi: 10.1016/j.pain.2007.05.015
11. Hung CI, Liu CY, Fu TS. Depression: an important factor associated with disability among patients with chronic low back pain. Int J Psychiatry Med. (2015) 49:187-98. doi: 10.1177/0091217415573937
12. Baumeister H, Knecht A, Hutter N. Direct and indirect costs in persons with chronic back pain and comorbid mental disorders–a systematic review. J Psychosom Res. (2012) 73:79-85. doi: 10.1016/j.jpsychores.2012.05.008
13. Wu A, Dong W, Liu S, Cheung JPY, Kwan KYH, Zeng X, et al. The prevalence and years lived with disability caused by low back pain in China, 1990 to 2016: findings from the global burden of disease study 2016. Pain. (2019) 160:237-45. doi: 10.1097/j.pain.0000000000001396
14. Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. (2015) 386:743-800. doi: 10.1016/S0140-6736(15)60692-4
15. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606-13. doi: 10.1046/j.1525-1497.2001.016009606.x
16. Sun Y, Fu Z, Bo Q, Mao Z, Ma X, Wang C. The reliability and validity of PHQ-9 in patients with major depressive disorder in psychiatric hospital. BMC Psychiatry. (2020) 20:474. doi: 10.1186/s12888-020-02885-6
17. Feng Y, Huang W, Tian TF, Wang G, Hu C, Chiu HF, et al. The psychometric properties of the Quick Inventory of Depressive Symptomatology-Self-Report (QIDS-SR) and the Patient Health Questionnaire-9 (PHQ-9) in depressed inpatients in China. Psychiatry Res. (2016) 243:92-6. doi: 10.1016/j.psychres.2016.06.021
18. Wang XS, Mendoza TR, Gao SZ, Cleeland CS. The Chinese version of the Brief Pain Inventory (BPI-C): its development and use in a study of cancer pain. Pain. (1996) 67:407-16. doi: 10.1016/0304-3959(96)03147-8
19. Chiarotto A, Maxwell LJ, Ostelo RW, Boers M, Tugwell P, Terwee CB. Measurement properties of visual analogue scale, numeric rating scale, and pain severity subscale of the brief pain inventory in patients with low back pain: a systematic review. J Pain. (2019) 20:245-63. doi: 10.1016/j.jpain.2018.07.009
20. Good M-JD, Smilkstein G, Good BJ, Shaffer T, Arons T. The family APGAR index. a study of construct validity. J Fam Pract. (1979) 8:577-82.
21. Chau TT, Hsiao TM, Huang CT, Liu HW. [A preliminary study of family Apgar index in the Chinese]. Kaohsiung J Med Sci. (1991) 7:27-31.
22. Huang Y, Liu Y, Wang Y, Liu D. Family function fully mediates the relationship between social support and perinatal depression in rural Southwest China. BMC Psychiatry. (2021) 21:151. doi: 10.1186/s12888-021-03155-9
23. Chen YM, Yu TW, Wang CC, Huang KT, Hsu LW, Lin CC, et al. Characteristics of psychosocial factors in liver transplantation candidates with alcoholic liver disease before transplantation: a retrospective study in a single center in Taiwan. Int J Environ Res Public Health. (2020) 17:8696. doi: 10.3390/ijerph17228696
24. Nicholas MK. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain. (2007) 11:153-63. doi: 10.1016/j.ejpain.2005.12.008
25. Xiao J, Wu WX, Teng HL, Wang NN. Testing the reliablility and validity of Chinese version pain self-efficacy questionnaire in a population with chronic low back pain. J Nurs Sci. (2013) 28:32-4. doi: 10.3870/hlxzz.2013.03.032
26. Ma L, Tang Z, Zhang L, Sun F, Li Y, Chan P. Prevalence of frailty and associated factors in the community-dwelling population of China. J Am Geriatr Soc. (2018) 66:559-64. doi: 10.1111/jgs.15214
27. Bener A, Verjee M, Dafeeah EE, Falah O, Al-Juhaishi T, Schlogl J, et al. Psychological factors. anxiety, depression, and somatization symptoms in low back pain patients. J Pain Res. (2013) 6:95-101. doi: 10.2147/JPR.S40740
28. Montgomery W, Vietri J, Shi J, Ogawa K, Kariyasu S, Alev L, et al. The relationship between pain severity and patient-reported outcomes among patients with chronic low back pain in Japan. J Pain Res. (2016) 9:337-44. doi: 10.2147/JPR.S102063
29. Ogbo FA, Mathsyaraja S, Koti RK, Perz J, Page A. The burden of depressive disorders in South Asia, 1990-2016: findings from the global burden of disease study. BMC Psychiatry. (2018) 18:333. doi: 10.1186/s12888-018-1918-1
30. Misra S, Wyatt LC, Wong JA, Huang CY, Ali SH, Trinh-Shevrin C, et al. Determinants of depression risk among three asian american subgroups in New York City. Ethn Dis. (2020) 30:553–62. doi: 10.18865/ed.30.4.553
31. China Daily. Moving the Agenda Forward. (2021). Available online at: https://www.chinadaily.com.cn/a/202107/16/WS60f0cc51a310efa1bd6623be.html (Accessed December 1, 2021).
32. Cho CH, Jung SW, Park JY, Song KS, Yu KI. Is shoulder pain for three months or longer correlated with depression, anxiety, and sleep disturbance? J Shoulder Elbow Surg. (2013) 22:222-8. doi: 10.1016/j.jse.2012.04.001
33. Ranger TA, Cicuttini FM, Jensen TS, Manniche C, Heritier S, Urquhart DM. Catastrophization, fear of movement, anxiety, and depression are associated with persistent, severe low back pain and disability. Spine J. (2020) 20:857-65. doi: 10.1016/j.spinee.2020.02.002
34. Wettstein M, Eich W, Bieber C, Tesarz J. Pain intensity, disability, and quality of life in patients with chronic low back pain. does age matter? Pain Med. (2019) 20:464-75. doi: 10.1093/pm/pny062
35. Tsuji T, Matsudaira K, Sato H, Vietri J. The impact of depression among chronic low back pain patients in Japan. BMC Musculoskelet Disord. (2016) 17:447. doi: 10.1186/s12891-016-1304-4
36. Kaczynski K, Gambhir R, Caruso A, Lebel A. Depression as a mediator of the relation between family functioning and functional disability in youth with chronic headaches. Headache. (2016) 56:491-500. doi: 10.1111/head.12709
37. Jackson T, Wang Y, Wang Y, Fan H. Self-efficacy and chronic pain outcomes: a meta-analytic review. J Pain. (2014) 15:800-14. doi: 10.1016/j.jpain.2014.05.002
38. Cheng ST, Leung CMC, Chan KL, Chen PP, Chow YF, Chung JWY, et al. The relationship of self-efficacy to catastrophizing and depressive symptoms in community-dwelling older adults with chronic pain: a moderated mediation model. PLoS ONE. (2018) 13:e0203964. doi: 10.1371/journal.pone.0203964
39. Akbari F, Dehghani M, Khatibi A, Vervoort T. Incorporating family function into chronic pain disability: the role of catastrophizing. Pain Res Manag. (2016) 2016:6838596. doi: 10.1155/2016/6838596
Keywords: depressive symptoms, chronic low back pain, prevalence, risk factors, patients
Citation: Hu Y, Yang Z, Li Y, Xu Y, Tian M, Jiang N and Guo N (2022) Prevalence and Associated Factors of Depressive Symptoms Among Patients With Chronic Low Back Pain: A Cross-Sectional Study. Front. Psychiatry 12:820782. doi: 10.3389/fpsyt.2021.820782
Received: 23 November 2021; Accepted: 20 December 2021;
Published: 13 January 2022.
Edited by:
Samrat Singh Bhandari, Sikkim Manipal University, IndiaReviewed by:
Saumen Gupta, Sikkim Manipal University, IndiaUddip Talukdar, Fakhruddin Ali Ahmed Medical College and Hospital, India
Copyright © 2022 Hu, Yang, Li, Xu, Tian, Jiang and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ningfeng Guo, ZmxjMTcyM0AxNjMuY29t
†These authors have contributed equally to this work
 Yueming Hu1,2†
Yueming Hu1,2† Ningfeng Guo
Ningfeng Guo