- 1Sangath, Goa, India
- 2Division of Neuroscience and Experimental Psychology, The University of Manchester, Manchester, United Kingdom
Introduction: The past decade has seen key advances in early intervention for autistic children in high-income countries, with most evidence based on specialist delivery of interventions. The care gap seen in low- and middle-income countries (LMIC) remains close to 100%. A key challenge in addressing this care gap concerns the paucity of specialists available to deliver services. Task-sharing provides an important potential solution; there is a need to identify interventions that are suitable for scaled-up delivery through task-sharing in low-resourced settings. We aimed to conduct a scoping review to identify studies which reported autism intervention delivered by non-specialists within LMIC and, using established frameworks, specify intervention components with evidence of successful non-specialist delivery.
Methods: A scoping literature search, conducted within four databases, generated 2,535 articles. Duplicates were removed, followed by screening of titles and abstracts, with 10% double-rated for reliability. 50 full text articles were then screened independently by two raters. Articles were included if studies: (a) were conducted in LMIC; (b) included samples of autistic children (age < 10); (c) evaluated psycho-social interventions delivered by non-specialists; (d) reported child outcomes; and (e) were peer-reviewed full-texts in English. Two established frameworks – @Practicewise and NDBI-Fi framework - were then used to ascertain the commonly delivered components of these interventions.
Results: Two studies met the inclusion criteria. Both studies evaluated parent-mediated interventions delivered by non-specialists in South Asia. Through the two frameworks, we identified elements and techniques that had been delivered successfully by non-specialists.
Conclusion: There is evidence from two acceptability and feasibility trials that non-specialists can be trained to deliver some intervention elements and techniques within parent-mediated interventions, with good fidelity and acceptability and evidence of effectiveness. The review points up the lack of a widespread evidence base in this area and need for further research in low resourced settings, including well-powered trials and mechanistic analyses to identify active ingredients. A focus on the pre-requisites for non-specialist delivery is critical to reduce inequity and provide universal health coverage within resource-constrained health systems.
Introduction
Autism Spectrum Disorder, more commonly referred to as autism, is a lifelong neurodevelopmental disability characterized by impairments in social communication, restricted, repetitive interests and behaviors, and differences in sensory processing, with the presence of co-occurring intellectual disability in up to a third of individuals (1). A review of global prevalence reported 1–1.8% (2), with similar findings in studies from low- and middle-income countries (LMIC), with prevalence rates of 1.04 and 1.1% in Sri Lanka and India, respectively (3, 4). In the majority of LMIC, there exist a number of obstacles to accessing care which include the low awareness of the condition and the lack of access to detection and treatment services. Many LMIC have little or no policy implementation and underfunded health care systems for child and adolescent services (5, 6). This results in a significant “detection” gap in the identification of autism in young children, as well as a “treatment gap” with a lack of evidence-based interventions for the children who do receive a diagnosis.
Low- and middle-income countries have a significant proportion of their populations in the younger demographic age groups. This, coupled with large detection and treatment gaps, makes the need to identify interventions that can be scaled up a critical component of the right to care for young children with autism but also for the attainment of the United Nations Sustainable Development Goal 3. This goal aims to ensure the healthy lives and the promotion of health for all at all ages (7). While some LMIC settings do have services, these are predominantly focused in metropolitan areas and remain impacted by the scarcity of specialists with expertise in child development, including developmental pediatricians, child psychiatrists, speech and language therapists or occupational therapists (6). There is a need for radical innovations to help scale up services in these low resource contexts. Across many areas of health, including within treatment for mental health conditions like depression, innovations have used the process of “task-sharing” to address this dearth of specialist care (8). This approach aims to systematically skill up a non-specialist or para-professional with intervention-specific knowledge and skills, such that they are competent to facilitate the delivery of an evidence-based intervention in the community. Task-sharing is usually supported by a strong supervisory framework: the non-specialist has focused knowledge in a specific intervention or area of care, but more expert advice or care is readily available in the event of complex cases or scenarios. This approach allows an intervention to be delivered by a non-specialist, with the mobility to reach out to families in the community. Thus task-sharing with accessible non-specialist community-based facilitators overcomes barriers such as the limitation of specialist services, the expenses of such services, and the geographical distance to services.
The aim of this study was to conduct a scoping review and identify interventions for young children with autism that have evidence of feasibility, acceptability and effectiveness when delivered by non-specialists in LMIC. We adopted a narrow definition of “non-specialist” informed by the availability of personnel for task sharing to deliver care to children and families in LMIC settings (9), rather than the workforce available within low-resourced settings in high-income countries. These providers are typically frontline community health workers (10) who are not specialists in child development, autism, or mental health but who are already working on the ground within local communities. Examples include the Accredited Social Health Activists working in Delhi (11), Female Community Health Volunteers in Nepal (12), and Community Health Volunteers working in Kenya (13). Other potential providers include community volunteers or parent/disability “champions”. Our definition of specialist providers included those specialist professionals largely unavailable within LMIC: pediatricians, psychiatrists, nurse practitioners, psychologists, speech and language therapists, occupational therapists, physical therapists, and students/trainees of these professions. We focused on interventions delivered within a family context rather than school-based or teacher-delivered interventions, which tend to center around educational outcomes. In addition, we sought to address inconsistency in the definition around non-specialist delivery found within the literature. We differentiated between non-specialist-mediated interventions, and non-specialist delivery, the latter being the focus of our search. The former includes a broad range of approaches in which a practitioner delivers the intervention to a dyad (e.g., parent-child, sibling-child, peer-child) and the agent of mediation between the practitioner and autistic child (e.g., parent, sibling, peer) is considered a non-specialist. Some reviews (14) identified the parent receiving the intervention as the non-specialist and included all studies of parent-mediated interventions even where the intervention was delivered to the parent by a specialist. To meet our definition, parent-mediated interventions were included only when delivery to the parent-child dyad was by a non-specialist. This was a purposeful distinction to ensure that the focus was on interventions deliverable to families by non-specialists in LMIC. We also excluded interventions which were delivered by both specialists and non-specialists in tandem (15).
Following the identification of studies meeting our criteria, we sought to characterize the common elements (defined as a therapeutic activity or strategy) and techniques (defined as skills used during a session to deliver an element) of interventions that have been delivered by non-specialists under supervision and evaluated in LMIC countries. We were guided by two published frameworks: (1) the model proposed by Chorpita et al. (16) for delineating common ingredients of interventions for young children and adolescents which allows for the design of scalable evidenced modular interventions; (2) the framework developed by Frost and colleagues (17) through an expert-led Delphi approach, which aims to characterize the common elements and components of naturalistic developmental behavioral interventions (NBDIs) for autism.
Methods
We followed the five-step framework for scoping reviews suggested by Levac and colleagues (18). We firstly defined the research question and then identified the relevant studies based on predetermined inclusion and exclusion criterion. We then charted and summarized the data. We describe these steps in detail below.
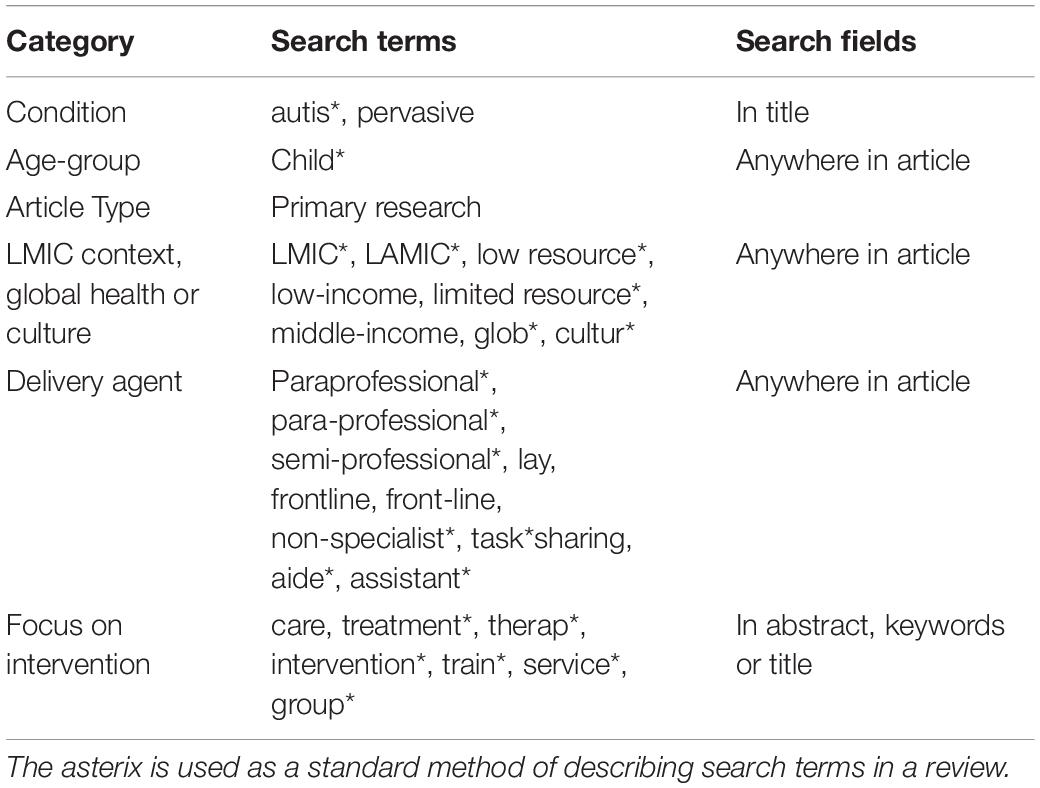
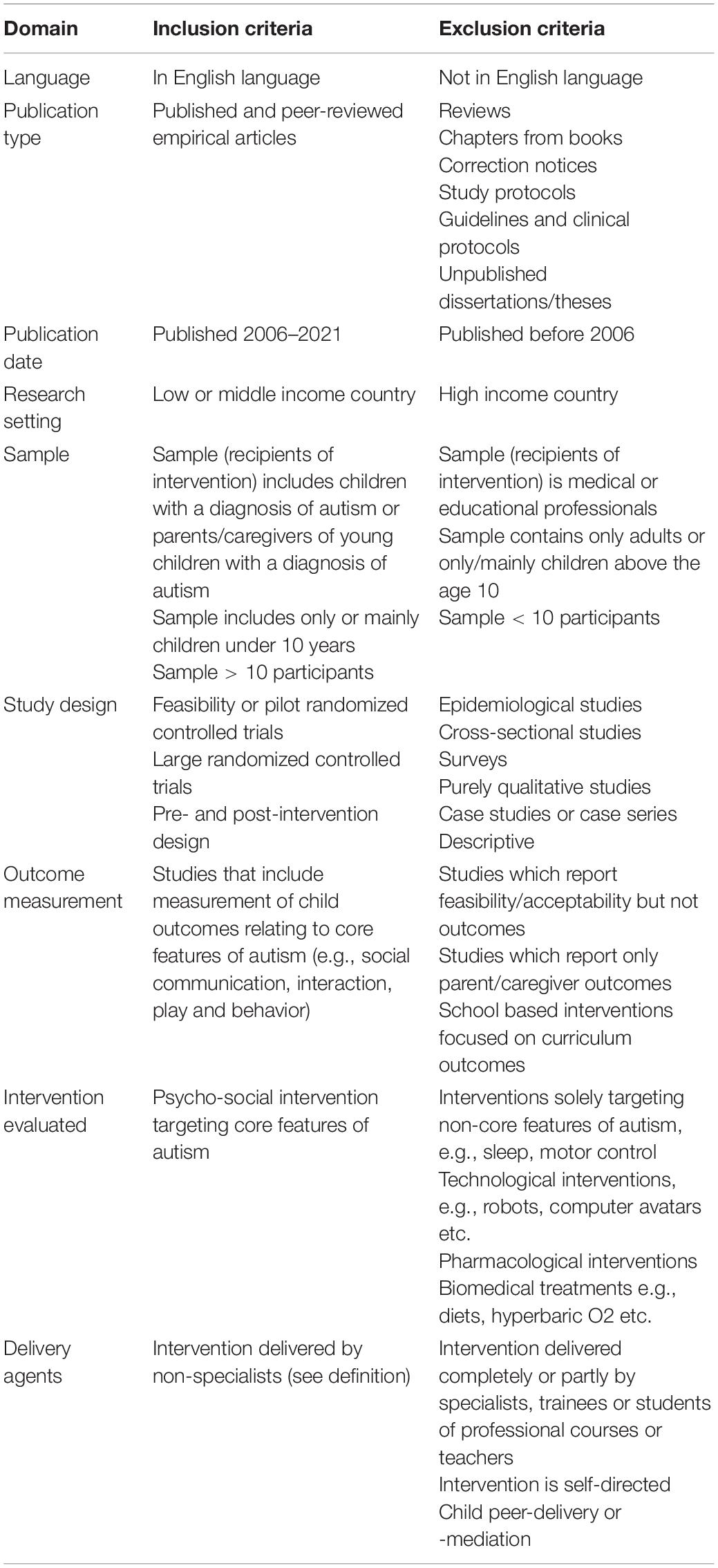
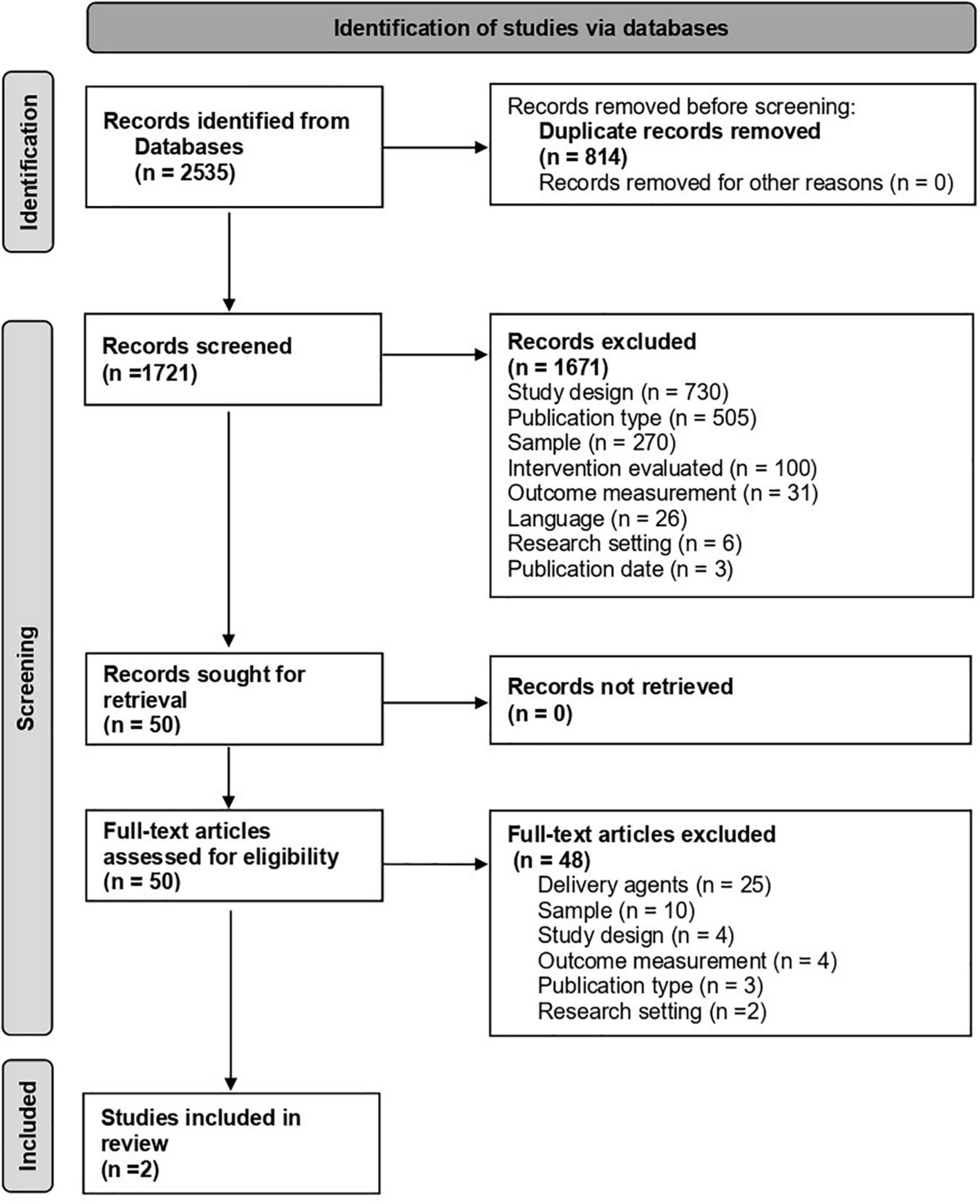
An OVID literature search was conducted within four databases (APA PsychInfo, APA Psycharticles, Ovid Medline + Epub Ahead of Print, Embase) to identify relevant studies. Search terms are shown in Table 1. This search identified 1,721 articles after 808 duplicates were identified and removed within OVID.
These articles were imported into Rayyan (19), a free web application designed for collaborative reviews. Rayyan identified 24 potential duplicates. These were checked manually and 6 were deleted. To establish inter-rater reliability prior to the title and abstract screen, 10% (173) were screened by all five reviewers, maintaining blind to each other’s inclusion/exclusion decisions. Agreement was reached for 130 articles (75%). Disagreements and uncertainties were resolved through discussion and clarification of terminologies and inclusion/exclusion criteria with support from two senior authors, until consensus was reached. Of these articles, 166 were excluded and 7 included for full-text review. The remaining 1,542 articles were divided up between five raters (AK, SL, LN, CB, and CG). All raters had at least a relevant undergraduate degree (CB, CG) or Masters degrees or equivalent (LN, AK, and SL) and were working within autism intervention research projects. The raters screened the title and abstracts, applying the inclusion/exclusion criteria shown in Table 2. This resulted in 1,499 articles being excluded and 43 articles put forward for a full text review. Together with the articles used for inter-rater reliability, a total of 1,671 articles were excluded and 50 articles (7 from reliability screen, plus 43 from individual screen) were put forward for full text review. The full breakdown of exclusion reasons across both stages can be found in the PRISMA (Figure 1).
The full-text review of the 50 articles was carried out independently by two raters from the pool of five raters, applying the same inclusion/exclusion criteria. There were 6 conflicts at this stage and these were resolved through discussion with the wider coding team. This led to the exclusion of 48 articles and the inclusion of 2 articles.
The next stage involved reviewing 18 articles recommended through key informants and bibliographic searches. These were divided between the 5 raters who, again, applied the same inclusion/exclusion criteria. These reviews produced two articles, which were the same articles that resulted from the search.
Common Components
Chorpita and Daleiden (20) developed a framework for identifying the components of psychosocial interventions for mental health conditions in children and adolescents which had demonstrated “favorable” results in effectiveness evaluations. The framework is descriptive in nature and does not seek to pinpoint the critical or “active” elements of these interventions. These identified elements have been collated into a coding manual called @PracticeWise (21). We examined the elements and techniques mapped in the @Practicewise common elements framework (20), and calibrated these broad definitions to encompass the needs of autism interventions along with the common components defined for the NBDI fidelity measure (17). LN and GD mapped the elements and techniques by reading the description of the intervention in the publication and manuals, plus drawing upon their professional understanding of the interventional approaches. We defined elements as a therapeutic activity or strategy and techniques as a skill that a therapist uses before or during the session to deliver an element (16).
Results
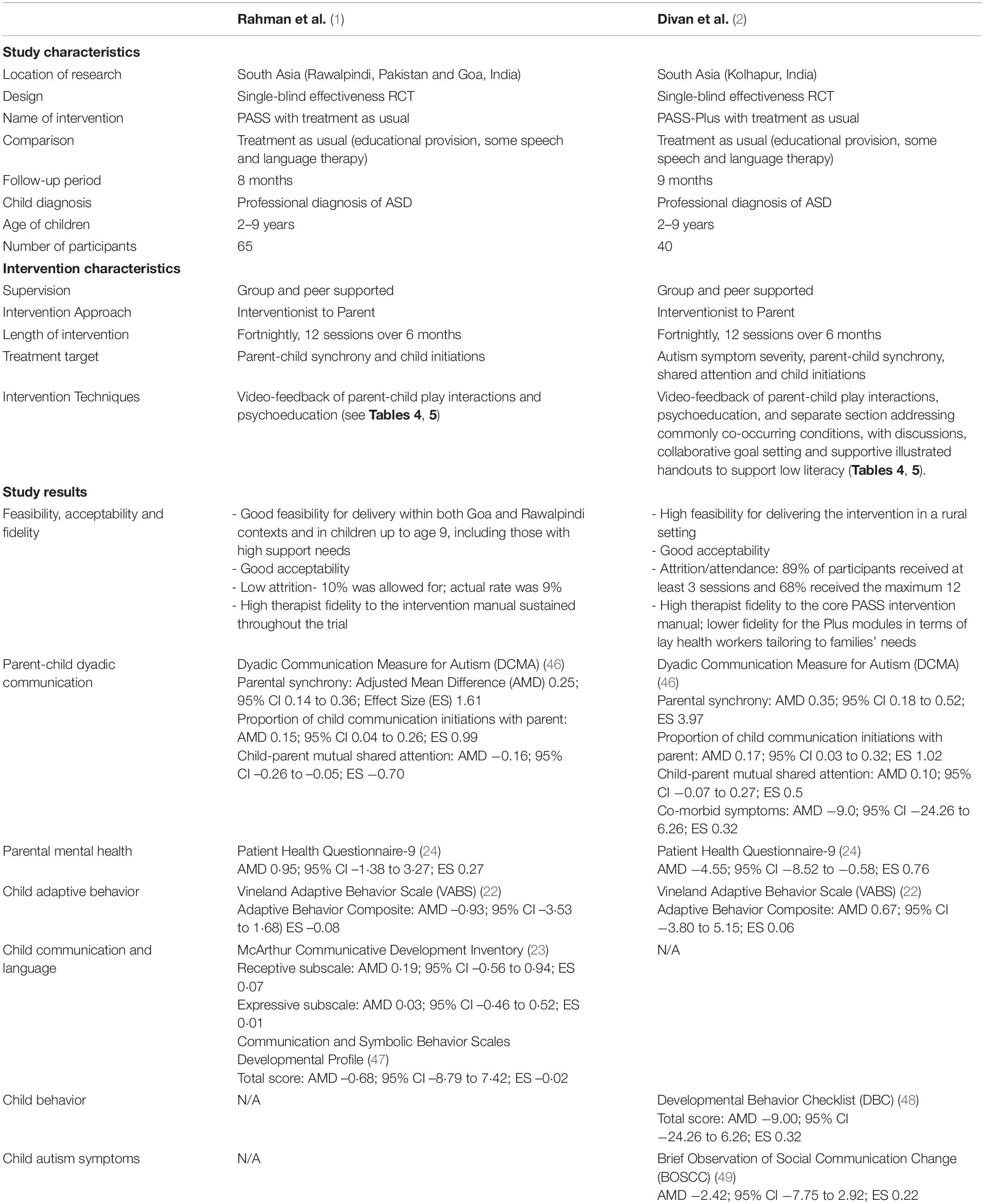
Two publications met our full search criteria, see Figure 1. Both these papers reported well-designed evaluations of interventions for young autistic children delivered in LMICs by non-specialists with no previous training in child development. Characteristics of the studies, interventions, and delivery agents are summarized in Table 3. Rahman et al. (22) trialed a parent-mediated social communication-focused intervention (Parent mediated intervention for Autism Spectrum Disorders in South Asia: PASS) delivered by non-specialist health workers, at home or in a clinic, in Rawalpindi, Pakistan and Goa, India. The intervention was an adaptation of the UK Pre-school Autism Communication Therapy (PACT), which was modified for delivery by non-specialists working within a competency-based training and supervision cascade led by specialists (23). The “non-specialists” were bachelor level graduates with no prior exposure to child development or autism. Precisely as in the original PACT intervention, they used video-feedback methods to enhance the parents’ sensitivity to their children’s non-verbal and verbal communication and refine the relevance of their responses to their child (known as parental “synchrony”). Parents were also encouraged, in later stages of the intervention process and where appropriate, to introduce action routines, repetitive language and pauses with the aim of aiding the child’s communication development. Implementation of strategies was encouraged between therapy sessions. Children with a diagnosis of autism aged 2–9 years were randomly assigned (1:1) to the PASS intervention (n = 32) or the treatment as usual (TAU) condition (n = 33), with controls for age (<6 or >6), functional impairment and treatment center location (Rawalpindi or Goa). The outcome measures for this initial effectiveness trial included parental synchrony and child communicative initiations (measured on the Dyadic Communication Measure for Autism) (24), parent reports of child adaptation and language use (measured on the Vineland Adaptive Behavior Scale (25), and the McArthur Communicative Development Inventory (26), respectively), the verbal and non-verbal aspects of social communication (measured on the Communication and Symbolic Behavior Scales Developmental Profile) (27) and maternal depressive symptoms (measured using a Patient Health Questionnaire-9) (28). The intervention proved feasible and acceptable for participants (only 9% of participants were lost to follow up). Additionally, and importantly, the intervention was delivered by the non-specialists with high and sustained therapist fidelity to the intervention manual (89% of intervention sessions meeting the pre-defined threshold for acceptable fidelity). For outcomes, in comparison to TAU, PASS increased parental synchrony and the initiation of communication by the children in the dyad, but child-specific outcomes beyond dyad were not affected. Other results are reported in Table 3.
During the PASS trial it became apparent that co-occurring non-autistic difficulties were often un-treated due to the lack of other generic child development and health services in the community, and that these co-occurring problems such as those associated with sleep, toilet training, parental wellbeing, and dietary restrictions, could hinder access to the core PASS technique. A number of additional modules were therefore devised for incorporation when necessary, on the basis of the reasonable effectiveness evidence for each co-occurring difficulty but simplified such that they could be within the competence of non-specialists. The implementation of these was based on a clinical decision algorithm which helped the provider and parent identify the families’ priority co-occurring condition and the most feasible strategies that families could implement for their child. After three sessions of the PASS social communication intervention, the non-specialist health workers supported the parent to identify the co-occurring concerns most problematic for the child and family and suggested relevant advice and strategies. Subsequent sessions were then extended to include both core social communication strategies and supportive strategies as appropriate and parents were given handouts to use between sessions for the latter. These sections of the session were delivered as distinct interventions, and the separate “Plus” section was only delivered after three foundational social communication sessions were complete. The distinction between core PASS and the “Plus” elements is clarified in Table 4. In distinction to the collaborative video-feedback facilitation of the core PASS intervention for autistic development, some of the “Plus” modules for co-occurring problems contained practical strategies for the management of day-to-day challenges to caregiving and family functioning (for instance, functional analysis of toileting and sleep difficulties). Written home programs for both components supported families to practice strategies collaboratively set during the session.
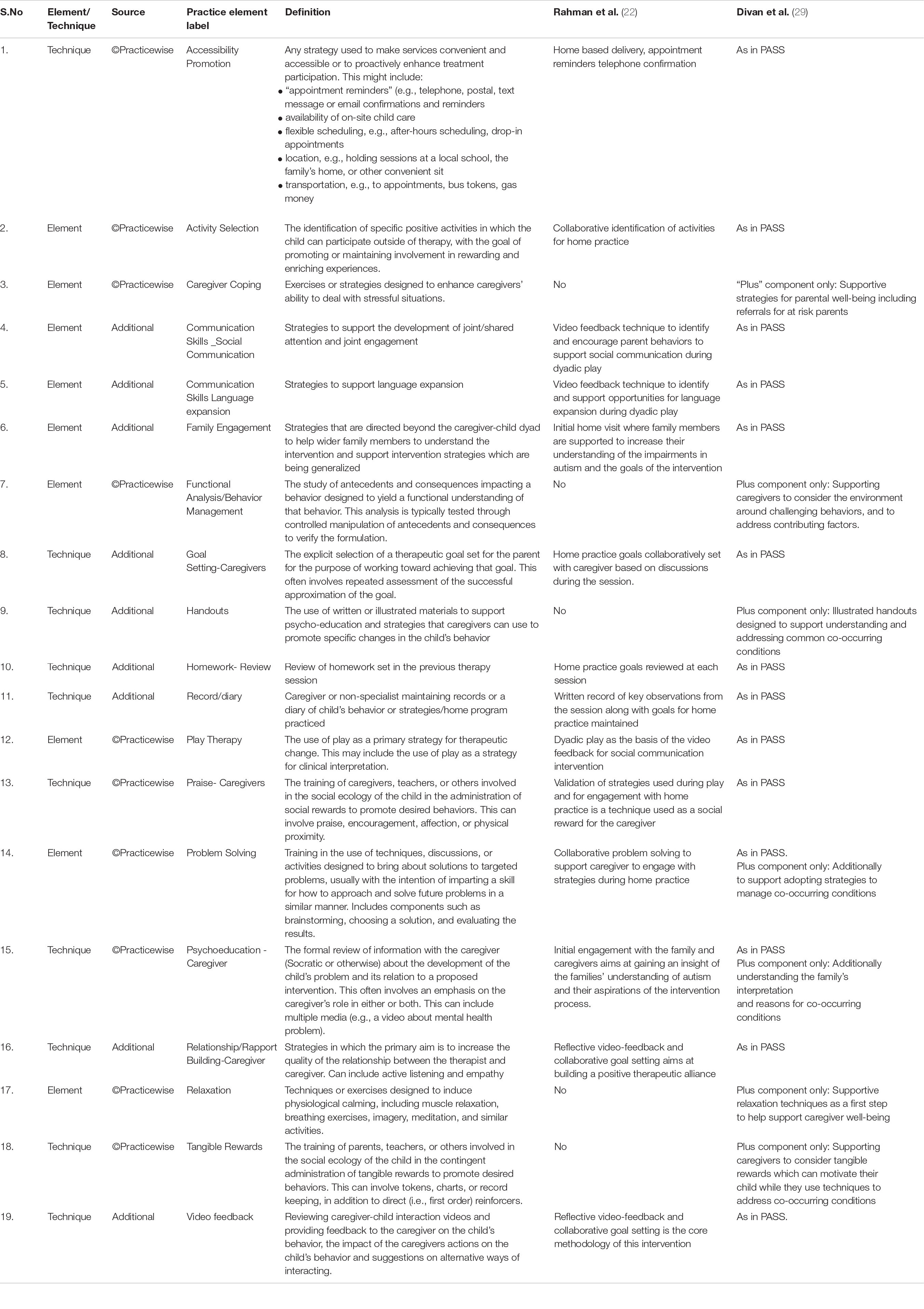
Table 4. List of common components based on the @PracticeWise framework (20).
Divan and colleagues (29) evaluated this “PASS PLUS” intervention in a small effectiveness evaluation, delivered one-on-one by non-specialist health workers in family homes, this time in rural Kolhapur, India. Children with a diagnosis of autism aged 2–9 years were randomly assigned to the PASS PLUS intervention (n = 21) or usual care condition (n = 19) with stratification for age (<5 or >5) and functional impairment. In practice, the Plus modules were delivered to 79% of the dyads (n = 15/19), with 4 families (21%) stating no expressed needs for further support. The most commonly delivered modules in decreasing order were for behavioral challenges (n = 12), sensory difficulties (n = 7), toileting support (n = 5), parental well-being (n = 4), sleep problems (n = 3) and feeding difficulties (n = 2). The study demonstrated high feasibility and intervention sessions met high therapist fidelity thresholds, with 92% of the core PASS procedures meeting fidelity thresholds for mandatory manualized content, and 96% meeting thresholds for quality. This was lower for the supplementary Plus modules, with fidelity thresholds to these manual components being met in 75% of sessions, and 81% meeting quality thresholds. The intervention was reported to be acceptable, and with regards to attendance, 89% of participants in the trial arm received at least the minimum 3 sessions and 68% received the maximum 12. For outcomes, the results showed that there was no evidence that additional delivery of these rather different strategies had a negative effect on the effectiveness of the core PASS video-aided communication intervention; the positive changes in parent synchrony and child initiations in the dyad were replicated as in PASS (22). In addition, PASS PLUS showed some evidence of a trend toward improvement in parental mental wellbeing (as measured by the PHQ-9), (28) but did not lead to significant changes, relative to the control group, in child outcomes such as co-occurring symptom levels (as measured by the Developmental Behavior Checklist, DBC) (30) or autism symptom severity as measured by the Brief Observation of Social Communication Change (BOSCC) (31). A large scale-up effectiveness and cost-effectiveness evaluation of this PASS Plus intervention is currently underway using delivery by frontline workers embedded in the established health system in urban India (32). The Communication-centered Parent mediated treatment for Autism Spectrum Disorders in South Asia (“COMPASS”) trial in this way represents the first large scale effectiveness test of an intervention for autism in a LMIC.
Common Components
Reviewing the described interventions in the publications along with the knowledge of the intervention, common components across the identified interventions are represented in Tables 4, 5.
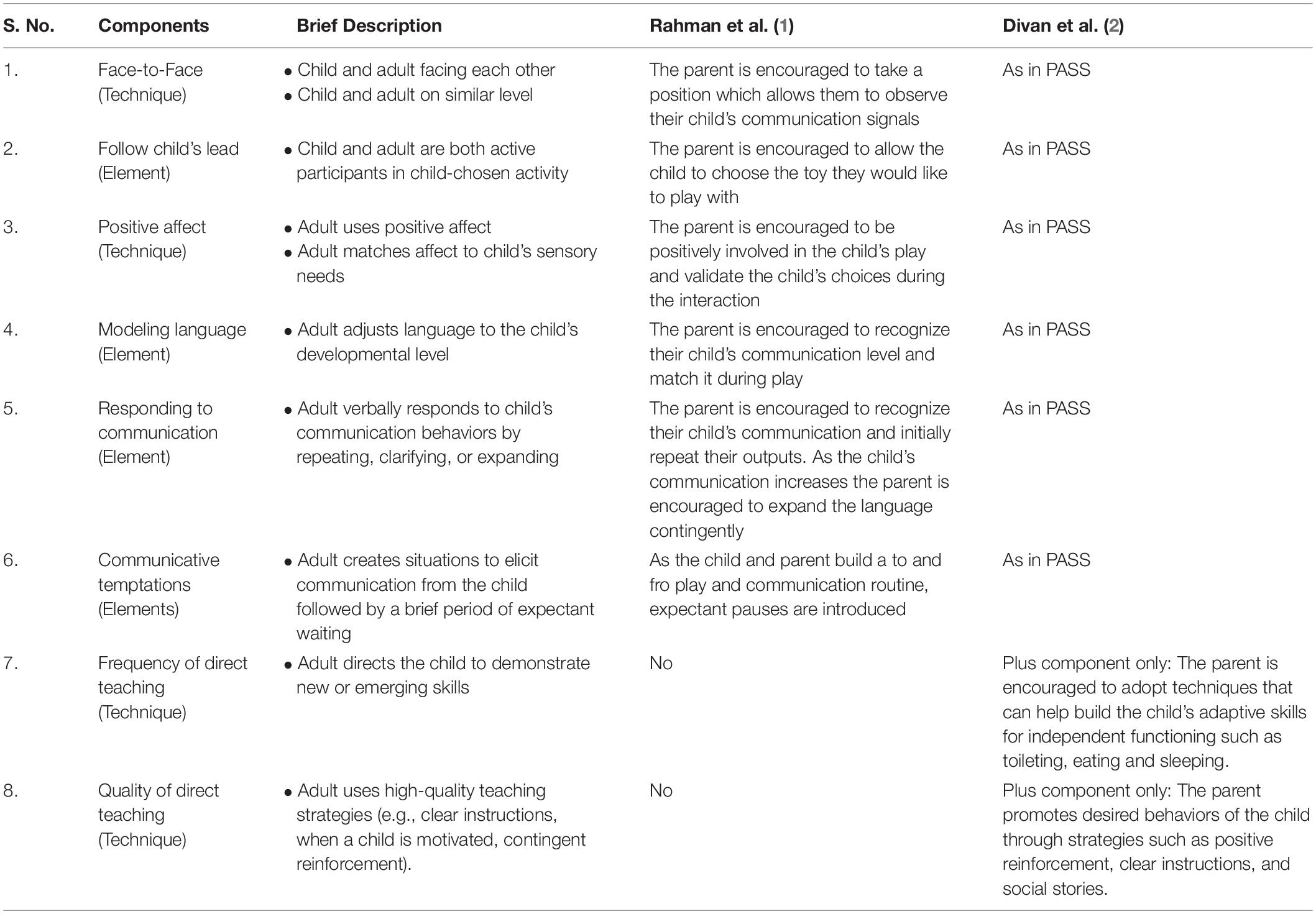
Table 5. List of common components based on the NDBI-Fi framework (11).
Discussion
This scoping review set out to identify interventions for young autistic children that have been delivered by non-specialists in low- and middle-income countries (LMIC) with evidence of feasibility, acceptability, and effectiveness. It was hoped that the review would elucidate the intervention elements that have evidence of successful delivery in LMIC by non-specialist providers and offer indications for the future direction in the design, mechanistic evaluation, and delivery of scalable interventions for low resource settings. This review identified only two studies that have evaluated the effectiveness of interventions for young autistic children and their families delivered by non-specialists in LMIC. Both these studies were conducted by teams that included senior authors of this review and both evaluated interventions that were parent-mediated and primarily communication-focused, where the non-specialist had no direct contact with the child beneficiary. There is, therefore, a striking lack of diverse empirical evidence to guide scalable intervention design and delivery within the countries of the world in which most of the world’s autistic children live.
Further clinical research in LMIC is urgently needed to provide evidence that is directly applicable to the key needs of LMIC health systems, to inform task-sharing and non-specialist delivery of autism interventions. This will help reduce inequity and achieve universal coverage within health systems which have an acute paucity of human and economic resources.
This review adopted a narrow definition of non-specialist providers to accurately reflect the most abundant workforce resource available to task-sharing approaches within LMIC: frontline community health workers, community volunteers or parent/disability champions. This focus allows the results to be more directly applicable to these settings. Other reviews (33) have investigated “non-specialist” delivery but adopted a wider definition of practitioners who are not relevant to the many LMIC settings that we are discussing. Frontline community health workers provide advice and support around issues such as maternity care, nutrition, immunization, child growth and development. They are often educated through high school but are not necessarily graduates; they have no formal healthcare or child development training but receive focused training around specific issues. They often live within the communities they serve and therefore likely to be trusted by the community. These frontline workers are an invaluable and flexible resource that can be trained, supervised, and incentivized to deliver interventions to children with neurodevelopmental disabilities and their families.
In this review we used two pre-established frameworks to classify intervention components, within the two interventions identified. We showcase that non-specialists – supported by a carefully established and implemented supervisory framework - can deliver a range of intervention elements and techniques to parents of young autistic children, with preliminary evidence of feasibility, acceptability, and effectiveness. Six elements from the @Practisewise framework (20) and four elements from the NDBI framework (17) along with three additional elements, were shown to be successfully delivered in this way. These included supporting parents to understand the communication development of their autistic child and to use strategies (e.g., language expansion, communication temptations) to support communication and language development. Similarly, we identified four techniques from the @Practisewise framework (20) and four from the NDBI framework (17) along with five additional techniques, including collaborative goal setting, parental psychoeducation, and the use of positive social or tangible rewards. It is important to note that we have not identified any tests of whether non-specialists could deliver intervention components directly with the autistic child or whether they could deliver interventions targeting other developmental domains or more complex co-occurring conditions, such as anxiety. These are important foci for future work. Another important clarification is that we are not proposing that the elements and techniques that we have identified are active ingredients. This would require in-depth mechanistic studies of each element and their interactions with each other and with outcomes (34, 35). A priority for future research should be to identify such active ingredients but also to evaluate the extent to which those ingredients can be delivered by non-specialists. Our conclusions on components must be tempered by the fact that they are based on a very small number of studies testing two interlinked interventions. However, this analysis can help clinicians and researchers to select from these evidence-based intervention components which have proved to be feasible for non-specialist delivery to inform scalable autism interventions implemented through the task-sharing approach.
An important question concerns the equivalence of task-sharing approaches in comparison to specialist-delivered approaches. The task-sharing approach has evidence of feasibility and acceptability within the context of adult mental health across diverse low resource settings (36–39) and some supportive evidence of equivalence. For example, a head-to-head comparison within a depression treatment study (40) found that a simpler psychological treatment delivered using the task-sharing approach had the same effect as a costlier intervention delivered by specialists. This suggests that well-designed training and supervision cascades led by highly qualified and expensive experts can support less qualified individuals to deliver complex interventions with similar effectiveness but to more people and at a lower cost. We do not have any directly comparable results on task-sharing versus specialist delivery for autism interventions and this is an important focus for future research if we are to ensure health equity across populations.
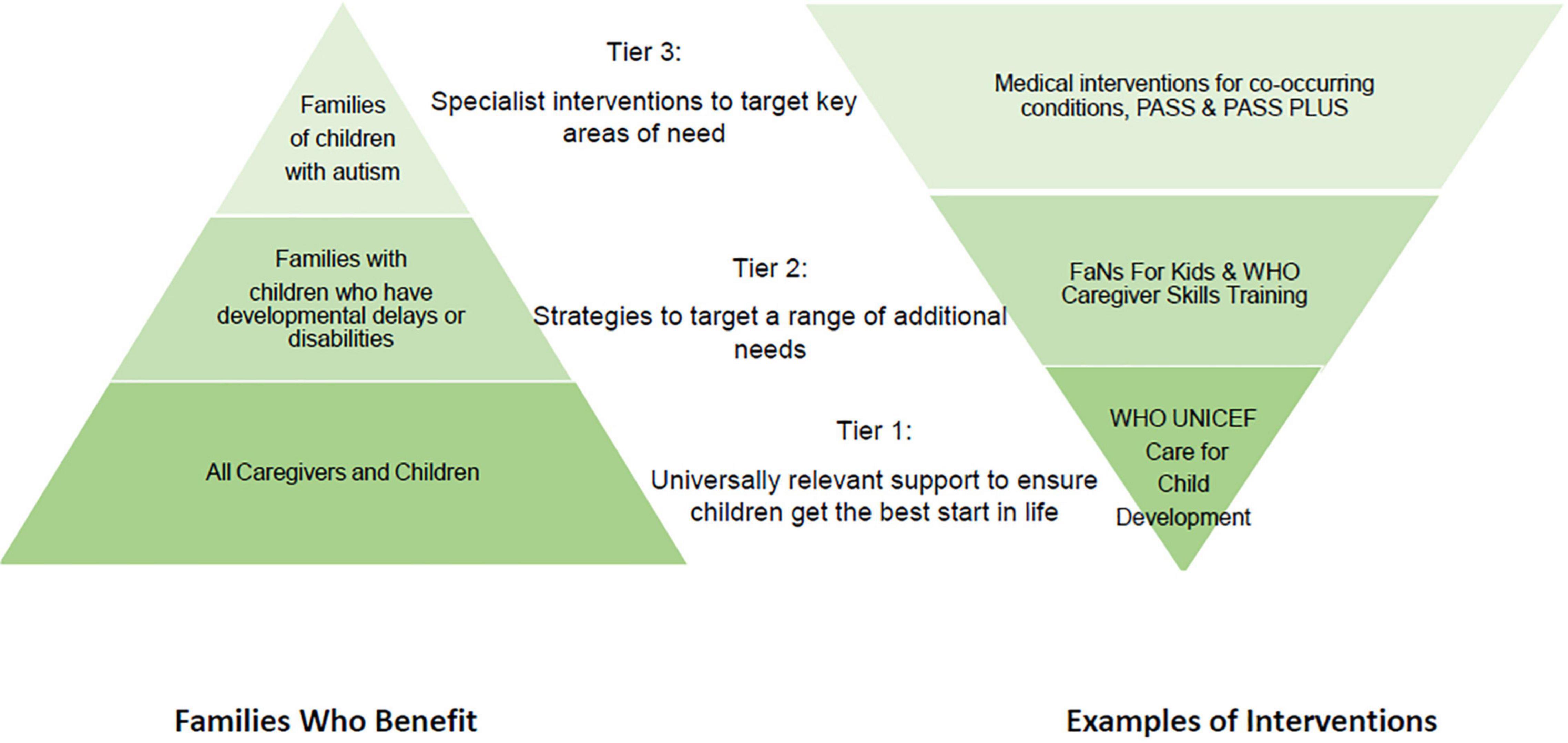
The Lancet commission on the Future of Care and Clinical Research for Autism (41) recognizes the prohibitive costs and lack of access to evidence-based interventions in most of the world. The authors recommend a stepped care personalized approach to care, (5, 42) and we would suggest that interventions containing the common components identified here could be evaluated as WHO tier 3 interventions for delivery in low resource settings, allowing more complex cases to be triaged up to specialist care. As part of this stepped care approach, non-specialist delivery could be used to widen access to support, potentially benefiting many additional children, including those with other neurodevelopmental disabilities (Figure 2).
That said, even these common components delivered in one setting may have challenges in others, which may include the professional and personal workload of the frontline worker. Additionally, there will need to be contextual adaptations based on community perceptions and needs along with structural systemic changes to support career progression of frontline workers who may be trained to deliver such complex interventions.
In addition to our two identified papers, there were studies which did not meet our inclusion criteria, but which may also inform decisions around non-specialist delivery. We have included a couple of informative examples here. Hamdani and colleagues (43) conducted a large (n = 540) single-blinded, cluster randomized controlled trial in rural Rawalpindi, Pakistan. The trial evaluated the “FaNs for Kids” intervention compared to enhanced treatment-as-usual for parents of children aged 2–12 with a range of developmental delays and disabilities. The sample included children with communication disabilities but not formally diagnosed autism and, for this reason, did not meet the inclusion criteria of our search. FaNs for Kids was a group-based, psycho-education intervention adapted from the WHO Mental Health Gap Intervention Guidelines (mhGap-IG). The programme targeted child development and functioning (communication, socioemotional development, co-occurring conditions, and motor difficulties), as well as caregiver psychological well-being, and was delivered by “family champions,” volunteers with family experience of disability, under the supervision of master trainers. The intervention was technologically assisted: caregivers accessed training videos on a tablet device and then met in nine group-based sessions to discuss different scenarios and build management plans around their child’s needs. The study found that FaNs for Kids resulted in improved health-related quality of life in caregivers, but there were no significant improvements on child outcomes, relative to the control group.
Through this study, Hamdani and colleagues demonstrated that technology can be an effective medium to deliver psychosocial interventional components to parents within low resourced settings. This highlights the potential held by technology-assisted interventions to scale-up intervention delivery in such settings which because of the standardized messaging can help maintain program fidelity as well as ensure intervention dosage by non-specialists. In PASS (22) and PASS Plus (29) non-specialists also make use of digital technology, through the use of video feedback techniques. Within an ongoing trial of the PASS Plus intervention delivered by frontline health workers in Delhi, India, digital technology is being harnessed further to overcome the challenges presented by the COVID-19 pandemic and enable ongoing training and supervision of the workforce and intervention delivery to families using video-conferencing and telephonic technology (44). Lakhera and colleagues evaluated the feasibility of this digitally assisted delivery of PASS Plus and the acceptability of virtually adapted sessions to 50 families of children with autism, 34 families who transitioned from receiving home based delivery of PASS Plus, and 16 families who received virtual delivery only. Though there were several barriers to virtual delivery of sessions, including a family preference for home-based delivery, the lack of access to the internet and lack of digital literacy, most families and non-specialist providers adapted successfully to the remote delivery of the intervention. Such innovations of technology – if integrated within the existing health care system – may help to leap-frog barriers to scaling up service delivery.
A second programme of research that did not meet our inclusion criteria but that may also inform decisions around non-specialist delivery is the World Health Organization Caregiver Skills Training programme (CST) (45). The CST is a trans-diagnostic, family centered intervention designed to be delivered by non-specialists and to fit within Tier 2 of the World Health Organisation (WHO) stepped-care model (i.e., targeted support for children with identified developmental needs; see Figure 2) and thereby bridge the treatment gap for children in low resource settings (46). The CST combines group sessions for caregivers with home visits to tailor the intervention to each family and set individual goals for each child (47). The intervention is informed by a range of approaches including psycho-education, social communication interventions, functional analysis, positive parenting, and self-care methods with a strong foundation in the WHO-UNICEF Nurturing Care Framework (48). At the point of this scoping review, there were no published systematic evaluations of effectiveness using non-specialist providers. However, feasibility and acceptability studies have been conducted (49, 50), and we have been informed of evaluations of non-specialist delivery under review. The intervention has been pre-piloted through specialist workers in Italy and is now being field tested, including with non-specialist providers, in more than 30 countries around the world (50).
The strengths of this publication are that we have conducted a rigorous scoping review and have used two frameworks to classify intervention components allowing us to identify key techniques and strategies that non-specialists have delivered with evidence of effectiveness in three settings of urban and rural South Asia to families of young children with autism. A further strength concerns the explicit definition of non-specialist adopted in this review. However, this process has highlighted the acute lack of empirical data that is directly applicable to the needs of LMIC health systems, and is an urgent indication for more relevant research to support families of children with autism in the most underserved populations of the world.
Data Availability Statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author Contributions
GD and KL conceived the idea for the research manuscript and defined the inclusion criteria for the search. LN, CG, AK, CB, and SL screened abstracts and full-text manuscript based on the search criteria on Rayyan software with support from GD and KL. LN, CG, CB, AK, KL, and GD drafted the first version of the manuscript and contributed to subsequent versions. All authors read and approved the final manuscript.
Funding
This work has been conducted with the support of a Medical Research Council, UK grant. Grant Reference MR/R006164/1. We acknowledge funding from the UK MRC/Wellcome/DfID and Joint Global Health Trials Award: MR/R006164/1.
Conflict of Interest
LN, AK, SL, and GD were employed by the not-for-profit Sangath. GD has led on the development and evaluation of the PASS and PASS Plus interventions and has received funding from Autism Speaks US and Grand Challenges Canada for this work. KL was also supported by an Autism Speaks grant for work on these interventions.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank Supriya Bhavnani, Jonathan Green, and Stephanie Shire for their invaluable inputs into this study.
References
1. Baio J, Wiggins L, Christensen DL, Maenner MJ, Daniels J, Warren Z, et al. Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR Surveill Summ. (2018) 67:1. doi: 10.15585/mmwr.ss6706a1
2. Elsabbagh M, Divan G, Koh YJ, Kim YS, Kauchali S, Marcín C, et al. Global prevalence of autism and other pervasive developmental disorders. Autism Res. (2012) 5:160–79. doi: 10.1002/aur.239
3. Perera H, Wijewardena K, Aluthwelage R. Screening of 18–24-month-old children for autism in a semi-urban community in Sri Lanka. J Trop Pediatr. (2009) 55:402–5. doi: 10.1093/tropej/fmp031
4. Arora NK, Nair MK, Gulati S, Deshmukh V, Mohapatra A, Mishra D, et al. Neurodevelopmental disorders in children aged 2–9 years: population-based burden estimates across five regions in India. PLoS Med. (2018) 15:e1002615. doi: 10.1371/journal.pmed.1002615
5. Divan G, Bhavnani S, Leadbitter K, Ellis C, Dasgupta J, Abubakar A, et al. Annual research review: achieving universal health coverage for young children with autism spectrum disorder in low-and middle-income countries: a review of reviews. J Child Psychol Psychiatry. (2021) 62:514–35. doi: 10.1111/jcpp.13404
7. United Nations. Goal 3, The Sustainable Development Goals Report. (2021). Available online at: https://sdgs.un.org/goals/goal3 (accessed February 28, 2022).
8. Raviola G, Naslund JA, Smith SL, Patel V. Innovative models in mental health delivery systems: task sharing care with non-specialist providers to close the mental health treatment gap. Curr Psychiatry Rep. (2019) 21:1–3. doi: 10.1007/s11920-019-1028-x
9. Singla DR, Kohrt BA, Murray LK, Anand A, Chorpita BF, Patel V. Psychological treatments for the world: lessons from low-and middle-income countries. Annu Rev Clin Psychol. (2017) 13:149–81. doi: 10.1146/annurev-clinpsy-032816-045217
10. Van Ginneken N, Tharyan P, Lewin S, Rao GN, Meera SM, Pian J, et al. Non-specialist health worker interventions for the care of mental, neurological and substance-abuse disorders in low-and middle-income countries. Cochr Database Syst Rev. (2013) 2013: CD009149.
11. Mane Abhay B, Khandekar Sanjay V. Strengthening primary health care through Asha workers: a novel approach in India. Primary Health Care. (2014) 4:2167–1079.
12. Shrestha R, Barbaro J, Dissanayake C. Changes in knowledge on the signs of autism in young children (11–30 months) among female community health volunteers in Nepal. J Autism Dev Disord. (2022) 52:219–39. doi: 10.1007/s10803-021-04944-7
13. Aseyo RE, Mumma J, Scott K, Nelima D, Davis E, Baker KK, et al. Realities and experiences of community health volunteers as agents for behaviour change: evidence from an informal urban settlement in Kisumu, Kenya. Hum Resour Health. (2018) 16:1–2. doi: 10.1186/s12960-018-0318-4
14. Naveed S, Waqas A, Amray AN, Memon RI, Javed N, Tahir MA, et al. Implementation and effectiveness of non-specialist mediated interventions for children with autism spectrum disorder: a systematic review and meta-analysis. PLoS One. (2019) 14:e0224362. doi: 10.1371/journal.pone.0224362
15. Nair MK, Russell PS, George B, Prasanna GL, Bhaskaran D, Leena ML, et al. CDC Kerala 9: effectiveness of low intensity home based early intervention for autism spectrum disorder in India. Indian J Pediatr. (2014) 81:115–9. doi: 10.1007/s12098-014-1474-8
16. Chorpita BF, Daleiden EL, Weisz JR. Identifying and selecting the common elements of evidence based interventions: a distillation and matching model. Ment Health Servic Res. (2005) 7:5–20. doi: 10.1007/s11020-005-1962-6
17. Frost KM, Brian J, Gengoux GW, Hardan A, Rieth SR, Stahmer A, et al. Identifying and measuring the common elements of naturalistic developmental behavioral interventions for autism spectrum disorder: development of the NDBI-Fi. Autism. (2020) 24:2285–97. doi: 10.1177/1362361320944011
18. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. (2010) 5:1–9.
19. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. (2016) 5:1–0. doi: 10.1186/s13643-016-0384-4
20. Chorpita BF, Daleiden EL. Mapping evidence-based treatments for children and adolescents: application of the distillation and matching model to 615 treatments from 322 randomized trials. J Consult Clin Psychol. (2009) 77:566–79. doi: 10.1037/a0014565
21. PracticeWise. Psychosocial and Combined Treatments Coding Manual. Satellite Beach, FL: PracticeWise (2012).
22. Rahman A, Divan G, Hamdani SU, Vajaratkar V, Taylor C, Leadbitter K, et al. Effectiveness of the parent-mediated intervention for children with autism spectrum disorder in south Asia in India and Pakistan (PASS): a randomised controlled trial. Lancet Psychiatry. (2016) 3:128–36. doi: 10.1016/S2215-0366(15)00388-0
23. Divan G, Hamdani SU, Vajartkar V, Minhas A, Taylor C, Aldred C, et al. Adapting an evidence-based intervention for autism spectrum disorder for scaling up in resource-constrained settings: the development of the PASS intervention in South Asia. Glob Health Action. (2015) 8:27278. doi: 10.3402/gha.v8.27278
24. Aldred C, Green J, Adams C. A new social communication intervention for children with autism: pilot randomised controlled treatment study suggesting effectiveness. J Child Psychol Psychiatry. (2004) 45:1420–30. doi: 10.1111/j.1469-7610.2004.00848.x
25. Sparrow SS, Cicchetti DV, Balla DA. Vineland Adaptive Behavior Scales. 2nd ed. Livonia, MN: Pearson Assessment (2006).
26. Fenson L, Marchman VA, Thal DJ, Dale PS, Reznick JS. MacArthur-Bates Communicative Development Inventories. 2nd ed. Baltimore, MD: Paul H. Brookes (2007).
27. Wetherby AM, Prizant BM. Communication and Symbolic Behavior Scales: Developmental Profile. Baltimore, MD: Paul H. Brookes (2002).
28. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
29. Divan G, Vajaratkar V, Cardozo P, Huzurbazar S, Verma M, Howarth E, et al. The feasibility and effectiveness of PASS plus, a lay health worker delivered comprehensive intervention for autism spectrum disorders: pilot RCT in a rural low and middle income country setting. Autism Res. (2019) 12:328–39. doi: 10.1002/aur.1978
30. Einfeld SL, Tonge BJ. Manual for the Developmental Behaviour Checklist (Primary Carer Version). Melbourne, VIC: Monash University Centre for Developmental Psychiatry (1994).
31. Grzadzinski R, Carr T, Colombi C, McGuire K, Dufek S, Pickles A, et al. Measuring changes in social communication behaviors: preliminary development of the brief observation of social communication change (BOSCC). J Autism Dev Disord. (2016) 46:2464–79. doi: 10.1007/s10803-016-2782-9
32. Sangath. Communication-Centred Parent-Mediated Treatment for Autism Spectrum Disorder in South Asia (COMPASS). Delhi: Sangath (2018).
33. Reichow B, Servili C, Yasamy MT, Barbui C, Saxena S. Non-specialist psychosocial interventions for children and adolescents with intellectual disability or lower-functioning autism spectrum disorders: a systematic review. PLoS Med. (2013) 10:e1001572. doi: 10.1371/journal.pmed.1001572
34. Green J, Garg S. Annual research review: the state of autism intervention science: progress, target psychological and biological mechanisms and future prospects. J Child Psychol Psychiatry. (2018) 59:424–43. doi: 10.1111/jcpp.12892
35. Gulsrud AC, Hellemann G, Shire S, Kasari C. Isolating active ingredients in a parent-mediated social communication intervention for toddlers with autism spectrum disorder. J Child Psychol Psychiatry. (2016) 57:606–13. doi: 10.1111/jcpp.12481
36. Ali BS, Rahbar MH, Naeem S, Gul A, Mubeen S, Iqbal A. The effectiveness of counseling on anxiety and depression by minimally trained counselors: a randomized controlled trial. Am J Psychother. (2003) 57:324–36. doi: 10.1176/appi.psychotherapy.2003.57.3.324
37. Chatterjee S, Chowdhary N, Pednekar S, Cohen A, Andrew G, Andrew G, et al. Integrating evidence-based treatments for common mental disorders in routine primary care: feasibility and acceptability of the MANAS intervention in Goa, India. World Psychiatry. (2008) 7:39–46. doi: 10.1002/j.2051-5545.2008.tb00151.x
38. Chibanda D, Mesu P, Kajawu L, Cowan F, Araya R, Abas MA. Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health. (2011) 11:828. doi: 10.1186/1471-2458-11-828
39. Rahman A, Malik A, Sikander S, Roberts C, Creed F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet. (2008) 372:902–9. doi: 10.1016/S0140-6736(08)61400-2
40. Richards DA, Ekers D, McMillan D, Taylor RS, Byford S, Warren FC, et al. Cost and outcome of behavioural activation versus cognitive behavioural therapy for depression (COBRA): a randomised, controlled, non-inferiority trial. Lancet. (2016) 388:871–80. doi: 10.1016/S0140-6736(16)31140-0
41. Lord C, Charman T, Havdahl A, Carbone P, Anagnostou E, Boyd B, et al. The lancet commission on the future of care and clinical research in autism. Lancet. (2022) 399:271–334. doi: 10.1016/S0140-6736(21)01541-5
42. Green J, Leadbitter K, Ainsworth J, Bucci S. An integrated early care pathway for autism. Lancet Child Adolesc Health. (2022) 6:335–44. doi: 10.1016/S2352-4642(22)00037-2
43. Hamdani SU, Suleman N, Akhtar P, Nazir H, Masood A, Tariq M, et al. Effectiveness of a technology-assisted, family volunteers delivered, brief, multicomponent parents’ skills training intervention for children with developmental disorders in rural Pakistan: a cluster randomized controlled trial. Int J Ment Health Syst. (2021) 15:1–7. doi: 10.1186/s13033-021-00476-w
44. Lakhera S, Roy SG, Laithani N, Sangwan P, Azar Z, Menon S, et al. Adaptation of a parent mediated communication intervention for autism for virtual delivery, in India. In: Proceedings of the International Society for Autism Research. (2021).
45. Salomone E, Pacione L, Shire S, Brown FL, Reichow B, Servili C. Development of the WHO caregiver skills training program for developmental disorders or delays. Front Psychiatry. (2019) 10:769. doi: 10.3389/fpsyt.2019.00769
46. World Health Organisation. WHO Caregivers Skills Training for Families of Children With Developmental Delays and Disorders. (2022). Available online at: https://www.who.int/teams/mental-health-and-substance-use/treatment-care/who-caregivers-skills-training-for-families-of-children-with-developmental-delays-and-disorders (accessed March 3, 2022).
47. Tekola B, Girma F, Kinfe M, Abdurahman R, Tesfaye M, Yenus Z, et al. Adapting and pre-testing the World Health Organization’s caregiver skills training programme for autism and other developmental disorders in a very low-resource setting: findings from Ethiopia. Autism. (2020) 24:51–63. doi: 10.1177/1362361319848532
48. World Health Organization, United Nations Children’s Fund, World Bank Group. Nurturing Care for Early Childhood Development: a Framework for Helping Children Survive and Thrive to Transform Health and Human Potential. Geneva: World Health Organisation (2018).
49. Sengupta K, Shah H, Ghosh S, Sanghvi D, Mahadik S, Dani A, et al. World Health Organisation-caregiver skills training (WHO-CST) program: feasibility of delivery by non-specialist providers in real-world urban settings in India. J Autism Dev Disord. (2021) 51:1–8. doi: 10.1007/s10803-021-05367-0
Keywords: low- and lower-middle-income countries, non-specialist delivery, autism intervention components, autism spectrum disorder (ASD), low resource setting
Citation: Naithani L, Goldie C, Kaur A, Butter C, Lakhera S, Leadbitter K and Divan G (2022) Early Autism Intervention Components Deliverable by Non-specialists in Low- and Middle-Income Countries: A Scoping Review. Front. Psychiatry 13:914750. doi: 10.3389/fpsyt.2022.914750
Received: 07 April 2022; Accepted: 23 May 2022;
Published: 29 June 2022.
Edited by:
Diana Schendel, Drexel University, United StatesReviewed by:
Aldina Venerosi, National Institute of Health (ISS), ItalyOlivia Herrington, Yale University, United States
Copyright © 2022 Naithani, Goldie, Kaur, Butter, Lakhera, Leadbitter and Divan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gauri Divan, Z2F1cmkuZGl2YW5Ac2FuZ2F0aC5pbg==
†These authors share last authorship
 Lavangi Naithani
Lavangi Naithani Caitlin Goldie
Caitlin Goldie Abhipreet Kaur
Abhipreet Kaur Charlotte Butter
Charlotte Butter Shweta Lakhera1
Shweta Lakhera1 Kathy Leadbitter
Kathy Leadbitter Gauri Divan
Gauri Divan