- 1School of Health and Biomedical Sciences, RMIT University, Melbourne, VIC, Australia
- 2Faculty of Medicine, Macau University of Science and Technology, Macau, Macau SAR, China
- 3Specialty of Child and Adolescent Health, The University of Sydney, Sydney, NSW, Australia
- 4Faculty of Health, University of Technology Sydney, Sydney, NSW, Australia
- 5Lysn (A Danewell Health Company), Sydney, NSW, Australia
- 6Sydney Medical School, The University of Sydney, Sydney, NSW, Australia
Objective: Guidelines for the prescription of antidepressants for Depressive Disorders (DD) have been in place for a long time. However, there is a lack of systematic information on the prescribing behavior of antidepressants in evidence-based clinical practice in psychopharmacotherapy of depressive disorders. This may suggest a lack of implementation of clinical guidelines by clinicians. Existing literature mainly focuses on specific issues or medications. To provide general information on the prescribing behavior of antidepressants for depressive disorders, a systematic review of available studies since 2013 was conducted.
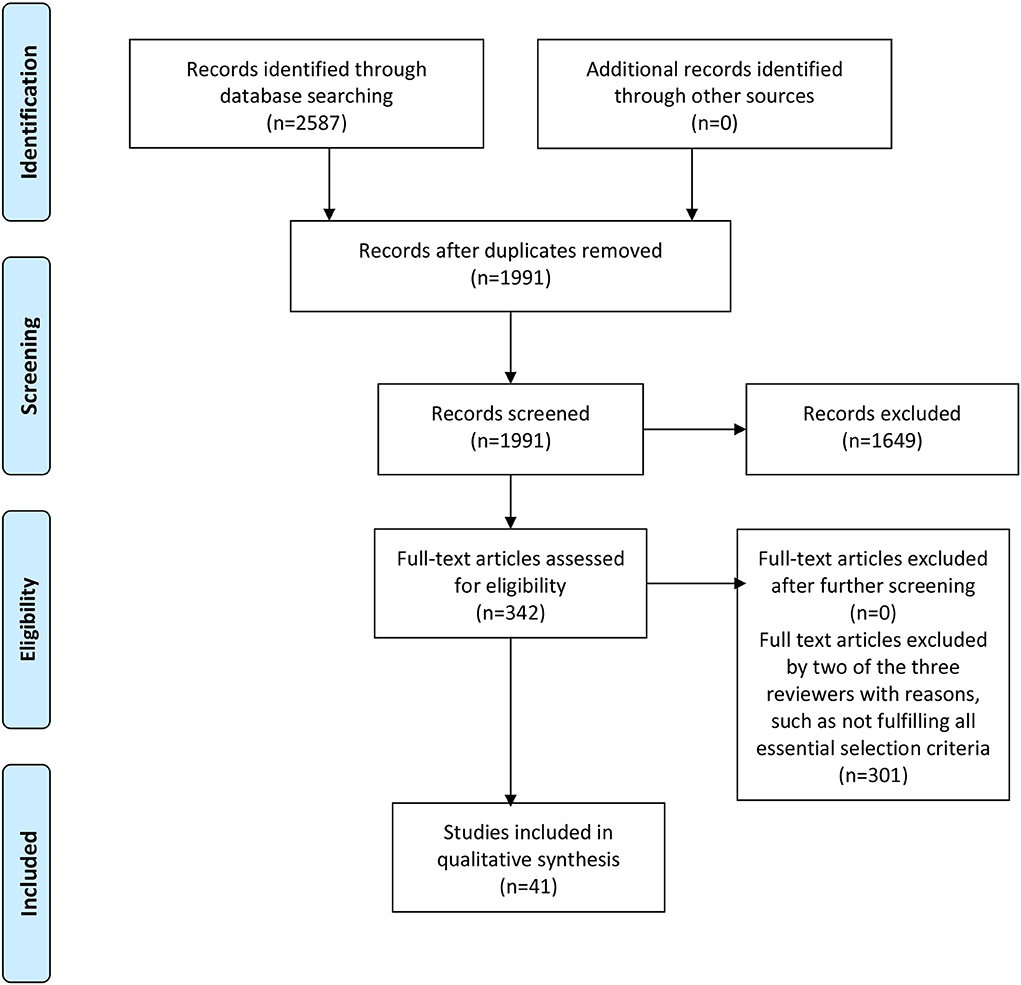
Methods and materials: To ensure a structured and systematic approach for the literature search and subsequent review process, the PRISMA guidelines for systematic reviews were followed. Major medical and health and psychological databases were used for the literature search. These included Ebsco Host, OVID, PubMed, Science Direct, Scopus, and Web of Science. The online application “Covidence” was employed to manage the titles collected and the full articles retrieved from the initial literature search. Upon finalizing the list of selected studies, data extraction was then conducted using a build-in function of the Covidence platform with the required information pre-set on a template for data extraction. The extracted information was tabulated and summarized in a table.
Results: Forty-one studies were identified after an extensive search of the literature following the PRISMA guidelines. Of these, 37 quantitative studies providing useful information were systematically reviewed and information extracted. There was a high level of heterogeneity among these studies with different foci or characteristics. Most studies were conducted in or utilized data obtained from hospital and primary healthcare settings. SSRIs were the most commonly prescribed type of antidepressant in the past decade, particularly among younger patients. Among these studies, antidepressants were mainly prescribed by psychiatrists with some by other physicians and general practitioners. This might reflect differences in legislation regarding professional requirements for prescribers or clinical practices.
Conclusions: A few themes that would be considered important in terms of the effect of prescription behavior on depression, specifically children/adolescents, special target populations, and off-label prescription. The results highlighted the need for more studies on a community-based approach and the role of GPs in the treatment of DD.
Introduction
In clinical practices, prescriptions of medications must be conducted according to clinical guidelines. The guidelines for the prescription of antidepressants for Depressive Disorders (DD), which include Major Depressive Disorder (MDD), Dysthymia, and Premenstrual Disorders, have been in place for a long time. In a review of guidelines published between 2007 and 2012, Wang et al. found that of the available guidelines reviewed four were developed in the USA, one by an international group, and one in Korea (1). Upon comparing these guidelines, Wang et al. concluded there were many similarities in the recommendation of DD treatment options for the initial treatment, second step treatment in case of non-response and/or incomplete response to initial treatment, and third step treatment if patients are non-responsive to second step treatment (1). Mono-pharmacotherapy antidepressants are preferred as the first-line treatment for initial treatment of DD without psychosis, and for mild to moderate DD. Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin Norepinephrine Reuptake Inhibitors (SNRI) are the preferred antidepressants during initial treatment, with some exceptions. For second-line treatment, a combination of different antidepressants is used (1).
However, there is little systematic information on many aspects of the prescribing behavior of antidepressants from evidence-based clinical practice in psycho-pharmacotherapy of depressive disorders. There is little information regarding prescriptions for first-line treatment and subsequent treatments, the types of antidepressants commonly prescribed as monotherapy and polypharmacotherapy, the setting in which antidepressants are prescribed, and prescription patterns in different populations. To ascertain any similar and relevant existing systematic reviews on the same topic, a search of the main health-related databases was conducted prior to the commencement of the current review study. The literature scan concentrated on reviews published in the past 5 years. Results suggest the existence of previous systematic reviews in the literature on the topic of antidepressant prescribing behavior (2–9). However, most of these reviews focused on a specific antidepressant usage or a targeted patient group. For example, Swainason et al. (3) focused on the usage of ketamine in adults with MDD, and Ostuzzi et al. (4) studied antidepressants use for patients with cancer.
Few studies provide a broader and more general review of the prescribing behavior of clinicians including psychiatrists, physicians, and other health professionals. This review aims to fill this knowledge gap and provide general information on the prescribing behavior of antidepressants for depressive disorders without other co-morbidities, such as anxiety disorders, psychosis, and substance use disorders. The reason for a focus on depressive disorders only is to allow clinicians to have a fundamental view of the current prescription pattern for a major mental health issue before venturing into more complex problems.
Methods
To ensure a structured and systematic approach for the literature search and subsequent review process, the PRISMA guidelines for systematic reviews were followed. Major medical and health and psychological databases were used for the literature search. These included Ebsco Host, OVID, PubMed, Science Direct, Scopus, and Web of Science with the following search terms and combinations: (prescri*) AND (medicat* OR antidepressant) AND (behavior OR behavior OR pattern) AND (depressive OR depression). Some restrictions were imposed to ensure the studies included were peer-reviewed journal articles; written in English, were original studies, and published since 2013. A restriction was imposed on the year of publication due to the global change in clinical guidelines and practices implemented in 2012.
The online application “Covidence” was employed to manage the titles collected and the full articles retrieved from the initial literature search. The following steps were undertaken to ensure that studies selected for final data extraction satisfied all selection criteria. First, abstracts were screened and analyzed for the key topic of the study, namely prescribing behavior of antidepressants for a major depressive disorder either as the primary or a co-morbidity diagnosis. This was conducted by authors ML, LL, KBH, WC. Second, full texts of the potentially acceptable articles were examined to assess their suitability for final data extraction. This step was conducted by three authors, ML LL and KBH independently based on the selection criteria. At the end of the independent selection, the results of selection by the authors were matched for any discrepancies. Differences were discussed and discrepancies were resolved through comparison to the selection criteria.
The following criteria were applied to the selection of studies: (1) Publications with a proper study design and prescribing behavior identified; (2) Studies that provided clear descriptions allowing an accurate assessment of whether key information on important variables could be extracted; (3) Studies that included information on variables including the year of publication, country, prescribers, the target population, sample size, setting of prescription, types, and names of antidepressants, reasons for a prescription; and (4) Studies published in English. Studies that focused on the knowledge, attitudes, and perceptions of clinicians toward the prescription of antidepressants were excluded from this review.
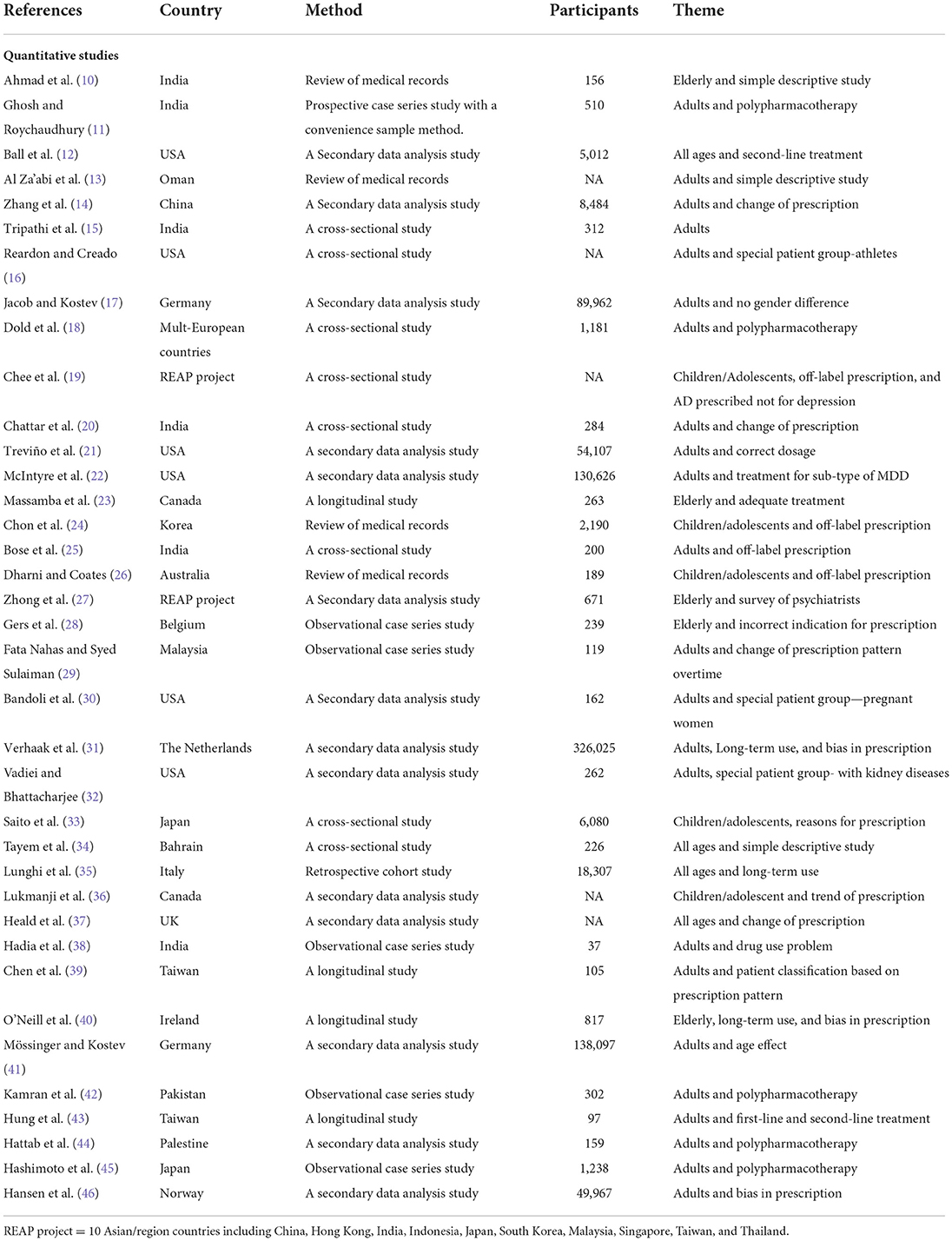
Upon finalizing the list of selected studies, data extraction was then conducted using a build-in function of the Covidence platform with the required information pre-set on a template for data extraction. The extracted information was tabulated and summarized in a table. The full articles were reviewed thoroughly to elucidate the main characteristics or themes of each study. These themes were also tabulated and presented in Table 1. Due to the observational nature of these studies, a descriptive approach was used to comment on any potential biases and/or limitations of the studies. The systematic literature searches and review process was summarized schematically in Figure 1 following the PRISMA chart format (47).
Results
In total, 41 studies were retained and reviewed after the systematic search and screening process. Of these, two were qualitative studies and were reviewed separately using qualitative review methodologies. Another two studies were surveys of clinicians regarding their choices or preferences of drug use and their perception of the drugs, and not about their prescribing behavior, leaving 37 studies for further review.
Information was extracted from the 37 quantitative studies using a systematic approach following the PRISMA guidelines. The information was tabulated in Table 1 with Supplementary materials included in the Appendix. Of these 37 studies, slightly more than half (n = 22, 56%) were published recently between 2018 and 2021 with slightly less than half (n = 16, 43%) of the studies containing data from Asian countries, followed by European countries (n = 8, 22%), and the USA (n = 6, 16%). The most common type of study design was secondary data analysis (n = 14, 38%), followed by cross-sectional studies (n = 8, 22%), and patient case-series studies (n = 6, 16%). The majority (n = 32, 86%) provided the number of patients included in the studies with a total of 836,386 patients (mean = 2,6137.1, s.d. = 65,884.1, min = 37, max = 326,025), with most studies on adults only (n = 21, 57%) and followed equally by all ages, children and adolescents, and elder ages (n = 5, 14%). One study was on pregnant women, another was among athletes, and the last was a survey of psychiatrists.
In most of the studies (n = 29, 78%) depression was reported as the primary diagnosis, three (n = 3, 8%) reported as co-morbidity of other illnesses, and the rest did not report any details on the specific depression diagnosis, such as unipolar depression, bipolar depression, or dysthymia. About half (n = 19, 51%) of these studies were set in hospitals including both inpatients and outpatients of the public and private sectors, seven (n = 7, 19%) in primary care, five (n = 5, 14%) in multiple settings, and the rest in other settings including a specialized sports psychiatric center and patients involved in a large project involving 10 Asian countries. In terms of the prescriber of antidepressants, about half (n = 18, 49%) of the studies reported prescriptions by psychiatrists only, six (n = 6, 16%) involved GPs and other physicians, another six involved a mix of psychiatrists, GPs, and physicians, one reported other physicians, another recorded psychologist, and the rest were without a clear indication of the prescribers. This might reflect some differences in legislation regarding professional requirements for prescribers or clinical practices. No specific trends were observed among these studies regarding the change of prescribers from psychiatrists to general practitioners or a change of drug type prescribed. Among these only 6 (16%) reported the number of prescribers with a total of 1,515 (mean = 252,5, s.d. = 220.8, min-40, max = 652). For the type of antidepressants, the majority (n = 33, 89%) of the studies reported that SSRIs were prescribed, in 29 (78%) TCAs were mentioned, and 21 (57%) SNRIs were recorded. Tetracyclic Antidepressants (TeCAs) were indicated in 14 (38%) studies and Serotonin antagonist and reuptake inhibitors (SARIs) in 11 (30%). Monoamine oxidase inhibitors (MOAIs) only occurred in 3 (8%) studies and 1 study reported the use of alternative and traditional medicine (ATM).
It was noted that there was a high level of heterogeneity among these studies with different foci or characteristics. Hence, these characteristics were also extracted and summarized as themes of each study. These themes were presented in Table 1. As shown, some common themes were derived from these studies, such as specific age groups, special target populations, off-label prescription, biases in prescription, and polypharmacotherapy. Further analyzes were conducted on a few themes that would be considered important in terms of the effect of prescription behavior on depression, specifically children/adolescents, special target populations, and off-label prescription. The results were summarized below.
Children/adolescents
Five studies focused on the prescription of antidepressants for children and adolescents (19, 24, 26, 33, 36). Of these five studies, three were conducted in Asian countries (19, 24, 33), and one in Australia (26), and another in Canada (36). Nearly all studies were conducted in hospital and primary care settings, except for one in community care (26). Prescribers were mainly psychiatrists and physicians. Most studies indicated that the majority of patients were treated with mono-pharmacotherapy at a level of about 92–95% (19, 24). Multiple types of antidepressants were used for young patients with SSRIs as the most common type. Three studies also focused on the off-label use of antidepressants among young people with depression (19, 24, 26). Based on these studies, off-label prescription of antidepressants for children and adolescents was common in many countries. This was also a theme that will be further reported below.
Special target populations
In terms of different patient populations, apart from the elderly and children/adolescents, some studies concentrated on special target populations. These include the Reardon and Creado (16) study on athletes, another study by Bandoli et al. (30) on pregnant women, and the study among patients with chronic kidney disease by Vadiei abd Bhattacharjee (32). All three studies were conducted in the US. In the survey study on the prescribing practice of sports psychiatrists who were members of the International Society of Sports Psychiatry, it was found that bupropion was the top choice of medication for depression in young athletes (16). Several reasons were provided for the choice of medications including increased energy, lower tendency to cause sedation, weight gain, cardiac side effects, and tremors (16). In the Bandoli et al. study, 166 pregnant women, who had been prescribed an antidepressant between 91 days prior to the last menstrual period and 32 weeks of gestation, were followed longitudinally (30). The most common antidepressant prescribed was SSRIs (78%), followed by bupropion (14%) and tricyclics (8%), with four groups identified based on the median cumulative fluoxetine equivalent dosage (30). It was also found that the highest usage group during pregnancy was associated with reduced birth weight. However, this was a small study with only 162 patients. In a study on the prescription of antidepressants for patients with chronic kidney disease, Vadiei et al. found that half of these patients received treatment for depression. The main setting of treatment for depression was in primary care with the most prescribed antidepressant SSRIs accounting for about 35%, followed by bupropion and mirtazapine (7%) (32).
Off-label prescription
Four studies examined off-label prescriptions for depression that the usage or administration of specific types of medication was not included in the product information or not yet approved for the users' population. As aforementioned, the target population of three of these studies was children and adolescents, and adults (19, 24–26). Two of these studies were conducted in Asian countries, one in India and one in Australia, mostly in a hospital or primary care setting with only one in the community (26). Most young patients were treated with mono-pharmacotherapy, with off-label prescriptions found to be a common practice, particularly in young patients. In the study by Chee et al. almost a third (30%) of antidepressant prescriptions were for diagnoses other than depression and anxiety, while the reasons and diagnoses for off-label prescriptions were not provided in other studies (19). Chon et al. reported that escitalopram and fluoxetine were the two antidepressants approved for the treatment of depression in children and adolescents by the FDA accounting for 32 and 24% of total patients respectively. The authors concluded that a large proportion of prescriptions for depression in Korean youths were off-label (24). Dharni and Coates studied the prescription pattern of antidepressants among young people in a community mental health center in Australia and concluded that about half of young people were treated with a single antidepressant (51%), with SSRIs the most common type. These antidepressants were mostly used off-label (26). In the study by Bose et al., among Indian adults in a tertiary hospital setting, it was found that 43% of antidepressant prescriptions were used for an off-label indication and fluoxetine (44%) and escitalopram (42%) were the most frequently prescribed in that manner (25). It was also found that the off-label indications were somatoform disorder (12.5%) and followed by generalized anxiety disorder (8.5%).
In terms of the study design, the majority were reviews of medical records, secondary data analysis, and cross-sectional studies. Few adopted a study design that would provide evidence with greater strength in terms of evidence-based practice. Of the 37, four were longitudinal studies that follow patients for some time (23, 39, 40, 43). These studies would be considered more pertinent in terms of the information provided by the patients. Another study worth noting was the large Italian retrospective cohort study of 18,307 patients of all ages by Lunghi et al. (35). This study investigated the long-term prescription patterns and provided detailed information on the changes in these prescriptions.
For some of the topics mentioned in the introduction, such as prescriptions for first-line treatment and subsequent treatments, little information was provided by these studies. This also applied to the types of antidepressants commonly prescribed as monotherapy and polypharmacotherapy.
Discussion and conclusion
This study aims to investigate the prescription behavior of antidepressants for depressive disorders by reviewing recently published reports. Of interest in this review is the systematically generated information on different aspects of the prescribing behavior of antidepressants with special attention to some prescribing patterns that may impact the health outcomes of depressed patients. A few outstanding observations have resulted from this review. First, most of the reviewed studies were conducted in, or utilized, data obtained from hospital and primary healthcare settings. Only one study was carried out in a community mental health center. Second, the past decade has seen SSRIs used as a commonly prescribed type of antidepressant, particularly among younger patients. However, there is a more recent trend to prescribe SNRIs and miscellaneous types of antidepressants, such as bupropion and mirtazapine. Third, most of these studies are focused on prescriptions of antidepressants by psychiatrists and other physicians. Not many studies involved GPs and other health professionals. Fourth, due to the high level of heterogeneity in the reviewed studies in terms of objectives, only a few common themes emerged.
The results obtained from this review provide some insights into the current status of antidepressant prescriptions for the treatment of DD. The very fact that only one study focused on the community mental health setting is revealing. This reflects a lack of attention on community-based pharmacotherapy treatment in terms of appropriate and effective treatment options for DD. There may be many reasons for such a lack of attention. One reason is that most patients with DD receiving community-based treatment are mainly in a sub-acute phase of the disorder. Pharmacotherapy treatment may mainly focus on the maintenance of the medication for treatment stabilization. Another reason may be due to the fact that other treatment options or approaches are available for DD in a community setting, such as counseling or cognitive behavioral therapy, in conjunction with other therapeutic approaches. These treatment options may be provided in a complementary or supplementary manner by specialized health professionals such as the Community Mental Health Team (CMHT). As a result, pharmacotherapy may play a slightly different role in the treatment of DD in comparison to patients in the acute phase of the disorder. Another point worth noting is the lack of studies on GPs and other healthcare professionals as prescribers of antidepressants. This may be because most of these studies have been conducted by psychiatrists and thus demonstrate a bias toward their profession. On the other hand, this may also reflect a lack of attention to GPs and other healthcare professionals as an important resources for providing treatment and services for people with mental health problems in the community.
When comparing the results obtained from this review with the current clinical guidelines on the antidepressant prescription provided by professional bodies, such as the Royal Australian and New Zealand College of Psychiatrists (RANZCP) Mood Disorder Guidelines 2020 (48) and the National Institute for Health and Care Excellence (NICE) Guidelines Depression in adults: treatment and management 2022 (49), some observations are noted. RANZCP does not outline specific antidepressant classes for first, second, and third-line treatment. The guidelines recommend seven antidepressants from seven classes (escitalopram, vortioxetine, agomelatine, venlafaxine, mirtazapine, bupropion, amitriptyline). The choice of antidepressant is based on clinical judgement patient factors, efficacy and tolerability. Based on this, the RANZCP guidelines are not reflected in the study findings that showed high weighting toward the prescription of SSRIs, SNRIs and TCAs. If the RANZCP guidelines were followed, a wider spread across antidepressant classes may be seen. However, clinicians, particularly in primary care, may be most familiar with SSRIs and SNRIs and continue to predominantly prescribe those. The study covered a range of countries, and there can be local variation in antidepressant availability. Not all medications on the RANZCP list may be available in all countries. On the other hand, NICE recommends that “less severe depression” be treated with SSRIs, and “more severe depression” treated with SSRIs or SNRIs, or another antidepressant if indicated based on previous clinical treatment history. NICE recommend that TCAs and MAOIs be used in secondary care settings. The study findings showed concordance with the NICE guidelines, in that SSRIs and SNRIs were very commonly prescribed. TCAs were prescribed more than expected based on the NICE guidelines, which commented on their toxicity in overdose, and recommended prescription of these medications in specialized settings.
There are strengths and limitations in this systematic review as in all others. This review study followed the PRISMA guidelines for systematic reviews ensuring the quality of the systematic review. Reviewers have observed the selection criteria for the inclusion of studies in the review with a dual process of article selection and data extraction. The use of the Covidence online platform has aided in implementing standardized procedures. In terms of limitations pertaining to individual studies, comments were made in the information extraction table. However, some general limitations have been identified. First, due to the heterogeneity of these studies with different objectives, information is missing on some variables, such as reasons for prescription and the average dosage prescribed. Second, most studies were conducted in a hospital or primary care setting by psychiatrists. Moreover, there is an uneven distribution of geographical origin of these studies with nearly half of the studies being conducted in Asian countries. Hence, this may constitute a publication bias. Finally, due to the heterogeneity of these studies, very few common themes could be derived, thus only the more obvious themes were discussed.
Author contributions
ML: study design, title and abstract screen, full text screen, data extraction, and write manuscript. LL: full text screen, data extraction, and write manuscript. KB-H: study design, database search and upload papers to Covidence, title and abstract screen, and full text screen. JK, TC, PS, and KD: comment and edit manuscript. WC: study design and title and abstract screen. All authors contributed to the article and approved the submitted version.
Funding
This review study has received funding support from Lysn.
Conflict of interest
This research is sponsored by Lysn Pty Ltd (an online mental health service) to find out clinicians' prescribing behavior of antidepressants for depressive disorders.
Authors JK, TC, PS, and KD are employed by Lysn Pty Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.918040/full#supplementary-material
References
1. Wang HR, Bahk WM, Seo JS, Woo YS, Park YM, Jeong JH, et al. Korean medication algorithm for depressive disorder: Comparisons with other treatment guidelines. Clin Psychopharmacol Neurosci. (2017) 15:199–209. doi: 10.9758/cpn.2017.15.3.199
2. Kato M, Hori H, Inoue T, Iga J, Iwata M, Inagaki T, et al. Discontinuation of antidepressants after remission with antidepressant medication in major depressive disorder: a systematic review and meta-analysis. Mol Psychiatry. (2021) 26:118–33. doi: 10.1038/s41380-020-0843-0
3. Swainson J, McGirr A, Blier P, Brietzke E, Richard-Devantoy S, Ravindran N, et al. The Canadian Network for Mood and Anxiety Treatments (CANMAT) Task Force Recommendations for the Use of Racemic Ketamine in Adults with Major Depressive Disorder: Recommandations Du Groupe De Travail Du Réseau Canadien Pour Les Traitements De L'humeur Et De L'anxiété (Canmat) Concernant L'utilisation De La Kétamine Racémique Chez Les Adultes Souffrant De Trouble Dépressif Majeur. Canad J Psychiatr. (2021) 66:113–25. doi: 10.1177/0706743720970860
4. Ostuzzi G, Matcham F, Dauchy S, Barbui C, Hotopf M. Antidepressants for the treatment of depression in people with cancer. Cochran Database Systemat Rev. (2018) 4:CD011006. doi: 10.1002/14651858.CD011006.pub3
5. Boaden K, Tomlinson A, Cortese S, Cipriani A. Antidepressants in children and adolescents: meta-review of efficacy, tolerability and suicidality in acute treatment. Front Psychiatr. (2020) 2:717. doi: 10.3389/fpsyt.2020.00717
6. Ghaffari Darab M, Hedayati A, Khorasani E, Bayati M, Keshavarz K. Selective serotonin reuptake inhibitors in major depression disorder treatment: an umbrella review on systematic reviews. Int J Psychiatry Clin Pract. (2020) 24:357–70. doi: 10.1080/13651501.2020.1782433
7. Yuan Z, Chen Z, Xue M, Zhang J, Leng L. Application of antidepressants in depression: a systematic review and meta-analysis. J Clinic Neurosci. (2020) 80:169–81. doi: 10.1016/j.jocn.2020.08.013
8. Hetrick SE, McKenzie JE, Bailey AP, Sharma V, Moller C, et al. New generation antidepressants for depression in children and adolescents: a network meta-analysis. Cochrane Database Syst Rev. (2021) 24:CD013674. doi: 10.1002/14651858.CD013674.pub2
9. Furukawa TA, Salanti G, Cowen PJ, Leucht S, Cipriani A. No benefit from flexible titration above minimum licensed dose in prescribing antidepressants for major depression: systematic review. Acta Psychiatr Scand. (2020) 141:401–9. doi: 10.1111/acps.13145
10. Ahmad F, Singh PP, Kumar A, Gaur RK. Drug prescribing pattern for major depressive psychosis patients in geriatric clinic of a teaching hospital in northern India. Int J Pharm Pharmaceutic Sci. (2013) :269−72.
11. Ghosh S, Roychaudhury S. Prescribing pattern of antidepressant drugs in a tertiary care hospital of eastern India. J Chem Pharmaceutic Res. (2014) 6:2593–7.
12. Ball S, Classi P, Dennehy EB. What happens next?: a claims database study of second-line pharmacotherapy in patients with major depressive disorder (MDD) who initiate selective serotonin reuptake inhibitor (SSRI) treatment. Annal General Psychiatr. (2014) 13:8. doi: 10.1186/1744-859X-13-8
13. Al Za'abi M, Al Jabri AS, Al Bartamani JK. Utilization pattern of anti-depressants at a tertiary hospital in Oman: a retrospective analysis. Afric J Psychiatr. (2014) 17:163. doi: 10.4172/1994-8220.1000163
14. Zhang L, Chen Y, Yue L, Liu Q, Montgomery W, Zhi L, et al. Medication use patterns, health care resource utilization, and economic burden for patients with major depressive disorder in Beijing, People's Republic of China. Neuropsychiatr Dis Treat. (2016) 12:941–9. doi: 10.2147/NDT.S97407
15. Tripathi A, Avasthi A, Desousa A, Bhagabati D, Shah N, Kallivayalil RA, et al. Prescription pattern of antidepressants in five tertiary care psychiatric centres of India. Indian J. Med. Res. (2016) 143:507–13. doi: 10.4103/0971-5916.184289
16. Reardon CL, Creado S. Psychiatric medication preferences of sports psychiatrists. Physician Sports Med. (2016) 44:397–402. doi: 10.1080/00913847.2016.1216719
17. Jacob L, Kostev K. Gender-based differences in the antidepressant treatment of patients with depression in German psychiatric practices. Ger Med Sci. (2016) 14:Doc02. doi: 10.3205/000229
18. Dold M, Kautzky A, Bartova L, Rabl U, Souery D, Mendlewicz J, et al. Pharmacological treatment strategies in unipolar depression in European tertiary psychiatric treatment centers—a pharmacoepidemiological cross-sectional multicenter study. Euro Neuropsychopharmacol. (2016) 26:1960–71. doi: 10.1016/j.euroneuro.2016.10.005
19. Chee K, Tripathi A, Avasthi A, Chong M, Xiang Y, Sim K, et al. Prescribing pattern of antidepressants in children and adolescents: findings from the research on asia psychotropic prescription pattern prescribing pattern of antidepressants in children and adolescents. East Asian Arch Psychiatr. (2016) 26:1.
20. Chattar KB, Karve AV, Subramanyam A, Tondare SB. Prescription pattern analysis of antidepressants in psychiatric outpatient department of tertiary care hospital in India. Asian J Pharma Clin Res. (2016) 9:77–9. Available online at: https://innovareacademics.in/journals/index.php/ajpcr/article/view/11061
21. Treviño LA, Ruble MW, Treviño K, Weinstein LM, Gresky DP. Antidepressant medication prescribing practices for treatment of major depressive disorder. Psychiatric Serv. (2017) 68:199–202. doi: 10.1176/appi.ps.201600087
22. Mcintyre RS, Ng-Mak D, Chuang CC, Halpern R, Patel PA, Rajagopalan K, et al. Major depressive disorder with subthreshold hypomanic (mixed) features: A real-world assessment of treatment patterns and economic burden. J Affect Disord. (2017) 210:332–7. doi: 10.1016/j.jad.2016.12.033
23. Massamba V, Vasiliadis HM, Préville M. Determinants of follow-up care associated with incident antidepressant use in older adults. BMC Research Notes. (2017) 10:1. doi: 10.1186/s13104-017-2714-6
24. Chon MW, Lee J, Chung S, Kim Y, Kim HW. Prescription pattern of antidepressants for children and adolescents in Korea based on nationwide data. J Korean Med Sci. (2017) 32:1694–701. doi: 10.3346/jkms.2017.32.10.1694
25. Bose D, Muraraiah S, Chandrashekar H. Evaluation of patterns and predictors of off-label prescribing of antidepressants in psychiatry at a tertiary care hospital—an analytical cross-sectional study. Nat J Physiol Pharm Pharmacol. (2017) 7:183–8. doi: 10.5455/njppp.2017.7.0822216082016
26. Dharni A, Coates D. Psychotropic medication profile in a community youth mental health service in Australia. Child Youth Serv Rev. (2018) 90:8–14. doi: 10.1016/j.childyouth.2018.05.007
27. Zhong XM, Dong M, Wang F, Zhang Q, Ungvari GS, Ng CH, et al. Physical comorbidities in older adults receiving antidepressants in Asia. Psychogeriatrics. (2018) 18:351–6. doi: 10.1111/psyg.12327
28. Gers L, Petrovic M, Perkisas S, Vandewoude M. Antidepressant use in older inpatients: current situation and application of the revised STOPP criteria. Therapeutic Adv Drug Safety. (2018) 9:373–84. doi: 10.1177/2042098618778974
29. Fata Nahas AR, Syed Sulaiman SA. Prescribing patterns of antidepressants among depressive men in Malaysia: A survey. J Young Pharmac. (2018) 10:98–101). doi: 10.5530/jyp.2018.10.22
30. Bandoli G, Kuo GM, Sugathan R, Chambers CD, Rolland M, Palmsten K. Longitudinal trajectories of antidepressant use in pregnancy and the postnatal period. Archiv Women's Ment Health. (2018) 21:411–9. doi: 10.1007/s00737-018-0809-2
31. Verhaak PFM, de Beurs D, Spreeuwenberg P. What proportion of initially prescribed antidepressants is still being prescribed chronically after 5 years in general practice? a longitudinal cohort analysis. BMJ Open. (2019) 9, 2. doi: 10.1136/bmjopen-2018-024051
32. Vadiei N, Bhattacharjee S. Patterns and predictors of depression treatment among adults with chronic kidney disease and depression in ambulatory care settings in the United States. Int Urol Nephrol. (2019) 51:303–9. doi: 10.1007/s11255-018-2034-3
33. Saito T, Reines EH, Florea I, Dalsgaard MK. Management of depression in adolescents in Japan. J Child Adolesc Psychopharmacol. (2019) 29:753–63. doi: 10.1089/cap.2019.0023
34. Tayem YI, Jahrami HA, Ali MK, Hattab SW. Ambulatory pharmacotherapy of five psychiatric disorders in bahrain: a descriptive study. Psychiatric Q. (2020) 91:289–98. doi: 10.1007/s11126-019-09705-5
35. Lunghi C, Antonazzo IC, Burato S, Raschi E, Zoffoli V, Forcesi E, et al. Prevalence and determinants of long-term utilization of antidepressant drugs: A retrospective cohort study. Neuropsychiatr Dis Treat. (2020) 16:1157–70. doi: 10.2147/NDT.S241780
36. Lukmanji A, Pringsheim T, Bulloch AG, Stewart DG, Chan P, Tehrani A, et al. Antidepressant prescriptions, including tricyclics, continue to Increase in Canadian Children. J Child Adolesc Psychopharmacol. (2020) 30:381–8. doi: 10.1089/cap.2019.0121
37. Heald AH, Stedman M, Davies M, Farman S, Upthegrove R, Taylor D, et al. Influences on the use of antidepressants in primary care: all England general practice-level analysis of demographic, practice-level and prescriber factors. Human Psychopharmacology. (2020) 35:2741. doi: 10.1002/hup.2741
38. Hadia R, Sanghani B, Sajan S, Mathew T, Rathod T, Joshi D, et al. A drug use evaluation study on antidepressants in psychiatric patients at a tertiary care teaching hospital. J Pharmaceutic Res Int. (2021) 1:66–75. doi: 10.9734/jpri/2021/v33i40A32222
39. Chen HC, Hsu HH, Lu ML, Huang MC, Chen CH, Wu TH, et al. Subgrouping time-dependent prescribing patterns of first-onset major depressive episodes by psychotropics dissection. World J Psychiatr. (2021) 11:1116–28. doi: 10.5498/wjp.v11.i11.1116
40. O'Neill A, Mcfarland J, Kelly D. Long-term antidepressant use in a cohort of older people. Int J Geriatric Psychiatr. (2021) 36:1241–51. doi: 10.1002/gps.5518
41. Mössinger H, Kostev K. Age effects on treatment patterns in 138,097 patients with unipolar depression followed in general practices in Germany. J Psychiatr Res. (2021) 144:208–16. doi: 10.1016/j.jpsychires.2021.10.033
42. Kamran S, Khan Z, Saqlain M, Nazar Z, Khan M, Ali Z, et al. Prescription analysis and cost of antidepressant drugs in major depressive disorder outpatients at the tertiary care hospital of Pakistan: a prospective approach. Expert Rev Pharmacoecon Outcomes Res. (2021) 22:845-51. doi: 10.1080/14737167.2022.2021073
43. Hung YC, Chen HC, Kuo PH, Lu ML, Huang MC, Chen CH, et al. Visualizing patterns of medication switching among major depressive patients with various stability and difficulty to treatments. Neuropsychiatr Dis Treat. (2021) 17:1953–63. doi: 10.2147/NDT.S311429
44. Hattab S, Qasarweh L, Ahmaro M, Atatre Y, Tayem Y, Ali M, et al. Prescribing patterns of psychotropic medications in psychiatric disorders: a descriptive study from Palestine. Int J Clin Pharm. (2021) 43:1101–8. doi: 10.1007/s11096-020-01223-w
45. Hashimoto N, Yasui-Furukori N, Hasegawa N, Ishikawa S, Numata S, Hori H, et al. Characteristics of discharge prescriptions for patients with schizophrenia or major depressive disorder: real-world evidence from the effectiveness of guidelines for dissemination and education (EGUIDE) psychiatric treatment project. Asian J Psychiatr. (2021) 63:44. doi: 10.1016/j.ajp.2021.102744
46. Hansen AB, Baste V, Hetlevik O, Haukenes I, Smith-Sivertsen T, Ruths S. GPs' Drug Treatment for Depression by Patients' Educational Level: Registrybased Study. BJGP Open. (2021) 5:1–10. doi: 10.3399/BJGPO-2020-0122
47. Moher D, Liberati A, Tetzlaff J, Altman DG, and The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the prisma statement. Annal Intern Med. (2009) 151:4. doi: 10.7326/0003-4819-151-4-200908180-00135
48. Malhi GS, Bell E, Bassett D, Boyce P, Bryant R, Hazell P, et al. RANZCP Guidelines: The 2020 Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatr. (2021) 55:7–117. doi: 10.1177/0004867420979353
49. NICE. Depression in adults: treatment and management. NICE guideline [NG222]. (2022). Available online at: https://www.nice.org.uk/guidance/ng222/chapter/Recommendations (accessed August 09, 2022).
Keywords: antidepressants, depressive disorder, systematic review, prescribing behavior, psychopharmacotherapy
Citation: Lam MK, Lam LT, Butler-Henderson K, King J, Clark T, Slocombe P, Dimarco K and Cockshaw W (2022) Prescribing behavior of antidepressants for depressive disorders: A systematic review. Front. Psychiatry 13:918040. doi: 10.3389/fpsyt.2022.918040
Received: 12 April 2022; Accepted: 12 August 2022;
Published: 09 September 2022.
Edited by:
Marijn Lijffijt, Baylor College of Medicine, United StatesReviewed by:
Paroma Mitra, New York University, United StatesNeven Henigsberg, University of Zagreb, Croatia
Copyright © 2022 Lam, Lam, Butler-Henderson, King, Clark, Slocombe, Dimarco and Cockshaw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mary K. Lam, bWFyeS5sYW1Acm1pdC5lZHUuYXU=
 Mary K. Lam
Mary K. Lam Lawrence T. Lam
Lawrence T. Lam Kerryn Butler-Henderson
Kerryn Butler-Henderson Jonathan King
Jonathan King Tahnee Clark5
Tahnee Clark5 Katherine Dimarco
Katherine Dimarco