Abstract
Objective:
Interpersonal Psychotherapy (IPT) is an evidence-based therapy. There have been increasing demand and training opportunities of IPT in China. Reviewing current evidence on its use in Chinese patients can help us understand the applicability of IPT in China and identify knowledge gaps to encourage and better future research in this field.
Method:
We did a comprehensive search of three major electronic databases: PubMed (English), Chinese National Knowledge Infrastructure (CNKI) and WanFang Data (Chinese). We examined overall study design, outcome measures, data analyses and other parameters. We only selected articles of Randomized Clinical Trials (RCT) for this review. All study findings were grouped and summarized per psychiatric diagnoses. The meta-analysis and forest plots were performed whereas studies could be combined.
Results:
After a full text review of 132 articles, 40 were selected for the final review. Comparing with control groups, evidences supported the efficacy of IPT in Chinese patients with Major Depressive Disorder (MDD), Postpartum depression, Generalized Anxiety Disorder (GAD), Social Anxiety Disorder, Post Stress Traumatic Disorder (PTSD), and Post-psychotic Depression. It was also beneficial to college students and Chinese first-time mothers. Meta-analysis using a random-effects model consistently yielded significant score differences between the IPT and control groups (p < 0.0001) on MDD.
Conclusion:
This systematic review has identified the current best evidence for IPT efficacy in Chinese population. The findings support IPT as an effective treatment in Chinese with certain psychiatric conditions, consistent with those from many other studies throughout the world.
1. Introduction
IPT is a time-limited, problem area focused, and evidence-based therapy to treat different psychiatric conditions (1). Originally developed to treat MDD, IPT has been used effectively to help patients with various diagnoses including bipolar disorder, eating disorder, perinatal depression, etc. (2).
IPT is a well-studied psychotherapy. Throughout the past five decades, more than 250 randomized controlled trials of IPT have been published by various research groups around the world (3). With or without adaptation, IPT has demonstrated a clear efficacy as both an acute and maintenance treatment option for major depression (4), bipolar disorder (5), PTSD (6), anxiety disorders (7) and eating disorders (8) for the target populations across lifespan. It has been proved to be superior to placebo, similar to medications and mostly more efficacious when combined with medications in treating depression (9–11). In anxiety disorder, IPT has shown same effect compared to CBT, and greater benefits compared to treatment as usual controls (7). In addition, a recent systematic review concluded IPT was non-inferior to CBT in treating patients with anorexia nervosa, and had same long-term efficacy in patients with bulimia nervosa (8). While it is intuitively obvious psychotherapy generally gives less side effects comparing with pharmacologic treatment, there was no report on whether IPT may adversely impact on patient’s psychological or physical condition. On the other hand, some studies have concluded that IPT is one of the most const-effective interventions in certain patient populations (12). Because of all these reasons, IPT has been included in different treatment guidelines of many countries such as Australia, Canada, United Kingdom, and United States (13). In 2015, World Health Organization (WHO) updated the Mental Health Gap Action Programme (mhGAP) guidelines and recommended IPT as one of major psychological interventions for adults, older and adolescents with depressive disorder (14). It is also listed as the first-line psychological treatment for acute MDD in the Canadian Network for Mood and Anxiety Treatments (CANMAT) guidelines (15).
China, as one of the largest countries in the world, has a current population over 1.4 billion (16). Estimated by World Health Organization (WHO), about 54 million people in China have depression and 41 million suffer from anxiety disorders (17). Over the past three decades, Chinese government has made significant efforts to expand mental health resources and increase access to treatment. Same as pharmacologic management, psychotherapy has nowadays become recognized as a scientific and effective treatment method, and has been gradually adopted as a main treatment modality in mental health care (18).
Despite good evidence for efficacy, IPT has not been commonly practiced in China. As many practitioners in China are focused on psychoanalysis and CBT as the mainstream psychotherapy options, IPT remains as an unfamiliar treatment option for majority of Chinese therapists. Given the fact that there has been an increasing demand in evidence-based psychotherapy, and rapidly growing training opportunities of IPT in China, it is important to review the up-to-date IPT related clinical studies that have been conducted on Chinese participants. As our initial online database search did not return enough number of English articles targeting Chinese subjects, we were curious to know whether many were published in Chinese. This article aims to summarize the findings of the existing studies published in the medical literature (in both Chinese and English) on the efficacy of IPT in mainland China. To our knowledge, there has been no previous systematic review undertaken on this topic. Analysis of current studies can surely help us understand the applicability of IPT in Chinese population and identify knowledge gaps to encourage and better future research in this field.
2. Materials and methods
2.1. Inclusion and exclusion criteria
This systematic review focused on reports and studies of IPT in mainland China so the main target population is Chinese. We defined IPT as the structured psychotherapy that was conceptualized by Klerman, Weissman, and colleagues. We also included its derivative adaptations such as Group IPT, Brief IPT (IPT-B) and IPT-oriented Education.
The inclusion criteria of this review were:
Studies were published in English or Chinese
Studies were original RCTs
Studies of IPT. A psychotherapy was considered IPT if it was a derivative or adaptation of the initial operationalized IPT (1), with similar techniques and interpersonal focus.
Target participants were Chinese, and the intervention was conducted in mainland China
2.2. Search strategy
As the scope of this review is limited to IPT studies in mainland China, we predicted that some articles could be published in Chinese instead of English. Therefore, the electronic databases we searched included both languages: PubMed (in English), Chinese National Knowledge Infrastructure (CNKI) and WanFang Data (in Chinese). We used database-specific combinations of the following terms or words: interpersonal psychotherapy, IPT, interpersonal therapy, China, mainland China and Chinese. There was no time limit, so all articles published before September 2022 in all three databases were included.
2.3. Study selection and quality assessment
Study selection and quality assessment were conducted by three of the authors. All titles and abstracts of the selected studies were first independently screened by two reviewers (LHT and GY). Then the three reviewers independently screened the studies for eligibility according the inclusion and exclusion criteria by reading the full text carefully. Any disagreements were resolved by discussions among the three reviewers (LHT, FZX and GY). We examined overall study design, selection bias, confounders, data collection methods, outcome measures and data analyses. Much attention was paid to the consistency and clarity of reporting. To assure the quality, we only selected RCT studies for final analysis. Case reports, commentaries, non-journal articles, qualitative studies, open trials and studies with inconsistent data were excluded. Meta-analyses were conducted when appropriate. Whereas studies could not be combined, summaries were provided.
2.4. Meta-analysis
The meta-analysis and forest plots were performed using the meta-analysis package “meta” (19, 20) and statistical software R (version 3.6.3, R Foundation, Vienna, Austria). The combined mean difference (MD) between intervention and control groups with its 95% confidence interval was estimated based on a random-effects model, taking into account between and within variation from different studies. Heterogeneity was examined based on τ2 statistic and I2 statistic from either random-effects model (if significant) or fixed-effects model (if not significant) (20).
3. Results
3.1. Study design and sample size
A total of 3,742 articles were initially retrieved from the databases. After excluding all duplicates and removing non-journal articles, application of inclusion criteria from the titles generated 355 articles and finally 132 articles were selected for full text review. Here, 40 studies were included in the final review. The PRISMA flow chart (21) is presented in Figure 1. Included in our analysis are 40 RCTs. The number of subjects in the studies varied from 21 to 176 with majority (57.5%) involved 80 or more participants. Table 1 provides a summary of all included studies.
Figure 1

Prisma flow diagram of study selection process * one study was published with additional CBT comparison so we only included the new publication.
Table 1
| References | Language | Sample characteristics | Diagnostic criteria | Study design | Intervention | Outcome measurement | Main outcomes | Statistical significance |
|---|---|---|---|---|---|---|---|---|
| MDD (general population) | ||||||||
| Ye and Li (22) | Chinese | Age:18–60, n = 60 | DMS-IV | RCT | Group IPT (12 weekly, 90 min) + antidepressant vs. antidepressant only | HAMD, SDSS | The symptom alleviation and social function improvement were more significant in IPT + medicine group. | p < 0.01 |
| Ying et al. (23) | Chinese | Age:36.2 ± 13, n = 82 | CCMD-3 | RCT | Individual IPT (12 weekly, 50–60 min) + SSRI vs. SSRI only | HAMD, Recurrence rate per CCI-CI after 6 months | The effective rates were 83.3% in the IPT and 60.0% in the control group. Recurrence rate of IPT group (7.1%) was also better than control group (22.5%). | p < 0.05 |
| Qiao and Niu (24) | Chinese | Age:18–50, n = 40 | DSM-IV | RCT | Group IPT (10 weekly, 90 min) + medicine vs. medicine only | HAMD, SDSS | The symptom alleviation and social function improvement were more significant in IPT + medicine group. | p < 0.01 |
| Zhu et al. (25) | Chinese | Age:37.63 ± 6.78, n = 58 | DSM-IV | RCT | Group IPT (12 weekly, 90 min) + medicine vs. medicine only | HAMD, SDSS | The symptom alleviation and social function improvement were more significant in IPT + medicine group. | p < 0.01 |
| Kang et al. (26) | Chinese | TRD, Age:34.3 ± 10.5, n = 100, | ICD-10 | RCT | Individual IPT (12 weekly, 50-60 min) + escitalopram + Olanzapine vs. medicine only | HAMD, HAMA, SF-36 | IPT combined with medications had better treatment effect (90.0%) than control group (72.0%). IPT improved the quality of life. | p < 0.05 |
| Kong (27) | Chinese | Age:20–50, n = 80 | ICD -10 | RCT | Group IPT (10 weekly, 100 min) + medicine vs. medicine only | HAMD, SDSS | Significant reduction in depression and improvement in social function of IPT group comparing with medicine only group. | p < 0.01 |
| Wang and Zhang (28) | Chinese | Age: 38.6 ± 5.2, n = 66 | DSM-IV | RCT | Group IPT (12 weekly, 90 min) + medicine vs. medicine only | HAMD, SDSS | Significant reduction in depression and improvement in social function of IPT group comparing with medicine only group. | p < 0.05 |
| Ren and Lei (29) | Chinese | Age:23–82, n = 86 | Clinically documented diagnoses by psychiatrists | RCT | Individual IPT + medicine (16 weekly, 50 min) vs. medicine only | SDSS, SSRS | The social functioning and social support more significantly improved in IPT group. | p < 0.001 |
| Wen et al. (30) | Chinese | Age:18–50, n = 57 | ICD-10 | RCT | Group IPT (6 weeks, 2 sessions per week, each session 120 min) + SSRIs vs. TNC + SSRIs | HAMD, SAD, SDS | Both groups demonstrated significant improvement in depression but IPT group had more improvement in social anxiety and social avoidance. | p < 0.05 |
| Xu et al. (31) | Chinese | Age:18–60, n = 60 | DSM-5 | RCT | Individual IPT (16 weeks, 45 min) + medicine vs. medicine only | HAMD, SDSS, SSRS | Significant reduction in depression and improvement in social function of IPT group comparing with medicine only group. | p < 0.05 |
| MDD (geriatrics) | ||||||||
| Sun et al. (32) | Chinese | Age: 65.3 ± 3.9, n = 84 | ICD-10 | RCT | Group IPT (12 weekly, 90 min) + escitalopram vs. escitalopram only | HAMD, SDSS GQOLI-74 | IPT group had more improvement in depressive symptoms, social function and quality of life in depressed geriatric patients. | p < 0.05 |
| Wang and Li (33) | Chinese | Age: 65–83, n = 98 | Clinically documented diagnoses by psychiatrists | RCT | Group IPT (12 weekly, 90 min) + paroxetine vs. paroxetine only | HAMD, SDSS, EPDS | IPT group had more improvement in depressive symptoms, social function and quality of life in depressed geriatric patients. | p < 0.05 |
| MDD (adolescents) | ||||||||
| Sun (34) | Chinese | Children of economic migrants Age: 13.05 ± 0.81, n = 21 | BDI ≥ 14 | RCT | Group IPT-B (6 weekly, 90 min) vs. no treatment | BDI | IPT group had better improvement in BDI than control group. | p < 0.001 |
| Postpartum depression | ||||||||
| Rao et al. (35) | Chinese | Age: 27.5 ± 13, n = 110 | DSM-IV | RCT | Group IPT (8 weekly, 90 min) vs. CBT vs. TNC | EPDS, HAMD, DAS, IIP | Both CBT and IPT had better clinical outcomes than the control group. CBT group maintained better effect than IPT at 6-month follow-up. | p < 0.05 |
| Liu (36) | Chinese | Age: 19–35, n = 120 | Not mentioned | RCT | IPT (8 weeks, details not provided) vs. TNC | EPDS | Significant reduction in EPDS scores at week 4 and 8 in IPT group in comparison to TNC. | p < 0.01 |
| Shi and Li (37) | Chinese | Primipara women Age: 23–37, n = 108 | HAMD≥17 | RCT | Group IPT (12 weekly, 60 min) vs. TNC | HAMD, SDSS, Self-report of parenting competence for neonates, breast milk production | IPT group showed better reduction in HAMD, SDSS scores, higher scores of self-report of parenting competence for neonates and more breast milk production | p < 0.05 |
| Jin et al. (38) | Chinese | Age: 20–35, n = 60 | DSM-IV | RCT | Individual IPT (12 weekly, 50 min) vs. CBT | EPDS, SSRS | Both IPT and CBT had treatment effect on postpartum depression. IPT group had a better effect on improving social support. | p < 0.01 |
| Wang (39) | Chinese | Age: 29.7 ± 1.8, n = 86 | Clinically documented diagnoses by psychiatrists | RCT | Group IPT (8 weekly, 90 min) vs. TNC | EPDS, IIP, SDSS | IPT group had better improvements in all 3 outcome measurements. | p < 0.05 |
| Lin (40) | Chinese | Age: 28.11 ± 2.42, n = 80 | Not mentioned | RCT | Individual IPT (12 weekly, 50 min) vs. TNC | HAMD, HAMA | IPT group showed better reduction in HAMD, HAMA scores and postpartum depression incidence rate. | p < 0.05 |
| MDD (patients with medical conditions) | ||||||||
| Du (41) | Chinese | Diabetic patients with depression Age: 59.78 ± 6.57, n = 62 | DSM-IV | RCT | Group IPT + antidepressant (9 weekly, 90 min) vs. antidepressant only | HAMD, FBG, 2hPBG, HbA1c | Both IPT group and control group demonstrated reduced depressive symptoms. IPT group also had better blood sugar control after treatment. | p < 0.05 |
| Hu (42) | Chinese | Diabetic Patients with depression Age: 62.7 ± 8.7, n = 120 | HAMD > 17 | RCT | Group IPT + antidepressant (8 weekly, 90 min) vs. antidepressant only | HAMD, FBG, 2hPBG, HbA1c | Both IPT group and control group demonstrated effectiveness in reducing depressive symptoms and blood sugar control. IPT group had higher rate of responses. | p < 0.05 |
| Jiang and Li (43) | Chinese | MHD depression. Age not reported, n = 44 | DMS-IV | RCT | Group IPT (14 weekly, 60–90 min) vs. TAU | SDS | Comparing with TAU, IPT group had a significant reduction in SDS score after treatment. | p < 0.01 |
| GAD | ||||||||
| Huang et al. (44) | Chinese | Age:35.56 ± 11.51, n = 90 | CCMD-3 | RCT | Individual IPT (12 weekly, 50 min) vs. CBT | HAMA, HAMD | Both IPT and CBT were effective. CBT group had better effect on sleep disturbance | p < 0.05 |
| Liang (45) | Chinese | Age: 35.6 ± 11.5, n = 80 | Clinically documented diagnoses by psychiatrists | RCT | Individual IPT (12 weekly, 50 min) vs. CBT | HAMD, HAMA, QOL | Both IPT and CBT were effective. CBT group had better effect on improving quality of life. | p < 0.05 |
| Li (46) | Chinese | Age: 36.26 ± 3.05, n = 84 | CCMD-3 | RCT | Individual IPT (12 weekly, 50 min) vs. CBT | HAMD, HAMA Quality of Life | Both IPT and CBT had treatment effect on GAD. CBT group had a better effect on improving quality of life. | p < 0.05 |
| Social anxiety disorder | ||||||||
| Huang and Liu (47) | Chinese | Age:20 ± 2, n = 45 | DSM-IV | RCT | Group IPT (8 weekly, 120 min) vs. CBT vs. Waiting list | IAS, SADS | Both IPT and CBT had better treatment effect on social anxiety than the control group. | p < 0.05 |
| Lin et al. (48) | Chinese | Age: 21.25 ± 4.4, n = 43 | DSM-IV | RCT | Group IPT (12 weekly, 120 min) vs. no treatment | SADS, RESE questionnaire | IPT group showed improvement in perceived self-efficacy in expressing positive affect (POS) and reduction in social avoidance and distress. | p < 0.05 |
| PTSD or patients with childhood trauma | ||||||||
| Jiang et al. (49) | English | Earthquake survivors Age: 24.79 ± 11.66, n = 49 | DSM-IV | RCT | Individual IPT (12 weekly 60 min) vs. TAU | CAPS, SCID, BDI-II, GSE, CTS, STAXI, SAS, QLI | A significantly greater reduction of PTSD and MDD diagnoses was found in the IPT group (51.9, 30.1%, respectively) versus the TAU (3.4, 3.4%, respectively). Treatment gains were maintained at 6 months for the IPT group. | p < 0.01 |
| Li et al. (50) | Chinese | College students with anxiety and childhood abuse Age: 18–21, n = 48 | DSM-IV | RCT | Individual IPT (6 weeks,2 sessions/week, 30–40 min) vs. supportive psychotherapy | SAS, GAF, CD-RISC, SRFIS, DSC | IPT could alleviate the anxiety and depression symptoms and improve psychosocial functionality in college students with anxiety and history of childhood abuse. | p < 0.05 |
| Post-psychotic depression | ||||||||
| Zhou et al. (51) | Chinese | Age: 18–55, n = 82 | CCMD-3 | RCT | Group IPT (10 weekly, 60–90 min) + medicine vs. medicine only | SCL-90, SDSS | IPT had better treatment effect on stable psychotic patients’ clinical symptoms and social functionality than control group. | p < 0.05 |
| Lu and Chen (52) | Chinese | Age: 34 ± 12, n = 82 | ICD-10 | RCT | Individual IPT (12 weekly) + medicine vs. medicine only | HAMD | IPT had better clinical efficacy in depression treatment than control group. There was also a difference in medication compliance between the two groups. | p < 0.05 |
| Zhou (53) | Chinese | Age: 34.1 ± 5.91, n = 68 | ICD-10 | RCT | Individual IPT (12 weekly) + medicine vs. medicine only | HAMD | Both IPT and control group showed improvement in depression after 1 month. IPT group had better continuous improvements than control after at 2 and 3-month follow-ups. | p < 0.001 |
| Kang (54) | Chinese | Age: 34.76 ± 3.98, n = 92 | CCMD-3 | RCT | Individual IPT (6 sessions, 3 CBT + 3 IPT) + paroxetine vs. paroxetine only | HAMD, SES, PANSS, WHO-DAS II, medication compliance | IPT combined with CBT could improve depression, self-esteem, social functioning and medication compliance in patients with post-schizophrenia depression. | p < 0.05 |
| Special population and other diagnoses | ||||||||
| Li et al. (55) | English | College students with aggression Age: 18–19, n = 60 | WFSBP guidelines | RCT | Group IPT (16 weekly, 60 min) vs. no treatment | CC-BPAQ, the Social Support Scale for University Students | IPT was effective in treating aggression and improving social support level for college students. | p < 0.05 |
| Li et al. (56) | Chinese | College students with aggression Age 18–19, n = 89 | CC-BPAQ > mean + SD | RCT | Group IPT (16 weekly, 60 min) vs. Group CBT vs. no treatment | CC-BPAQ | Both IPT group and CBT group had reduced the aggressiveness level after treatment, but IPT was superior in terms of CC-BPAQ scores. | p < 0.01 |
| Guang and Li (57) | Chinese | Somatoform disorder patients Age: 41.5 ± 9.2, n = 81 | ICD-10 | RCT | Individual IPT (12 weeks, 50–60 min, 2 sessions/week) + duloxetine vs. CBT + duloxetine vs. duloxetine only | HAMD, HAMA | Both IPT (88.89%) and CBT (85.19%) had better therapeutic effect on depression and anxiety than control group (59.26%). | p < 0.05 |
| Chen et al. (58) | Chinese | Bipolar disorder patients Age: 42.3 ± 10.3, n = 150 | Clinically diagnosed, HAMD≥17, YMRS<20 | RCT | Group IPT (8 weekly, 60 min) + medicine vs. medicine only | HAMD, YMRS, WHOQOL_BREF | IPT is effective for bipolar depression and could improve the quality of life. | p < 0.05 |
| Others (IPT-oriented education) | ||||||||
| Gao et al. (59) | English | First-time childbearing women Age: ≤ 35, n = 175 | Not mentioned | RCT | IPT-oriented childbirth education (2 sessions, 90 min, + 1 telephone follow-up) vs. Routine childbirth education | EPDS, GHQ, SWIRS | IPT group had significantly better psychological well-being, fewer depressive symptoms and better interpersonal relationships at 6 weeks postpartum as compared with control group. | p < 0.001 |
| Gao et al. (60) | English | First-time childbearing women Age: ≤35, n = 175 | Not mentioned | RCT | IPT-oriented childbirth education (2 sessions, 90 min, + 1 telephone follow-up) vs. Routine childbirth education | PSSS, PSOC, EPDS, GHQ | Women in IPT-oriented education had better social support, better maternal role competence and less depressive symptoms than those in control group. | p < 0.01 |
| Gao et al. (61) | English | First-time mothers Age: 28.49 ± 2.73 and 28.67 ± 2.91 (control), n = 176 | Not mentioned | RCT | IPT-oriented childbirth education (2 sessions, 90 min, + 1 telephone follow-up) vs. Routine childbirth education | EPDS, PSSS, PSOC-E | Women receiving the IPT psychoeducation program had significantly fewer depressive symptoms, higher level of social support and better maternal role competence at 6 weeks postpartum. | p < 0.05 |
Summary of included studies (n = 40).
2hPBG, 2-h Postprandial Blood Sugar; BDI-II, Beck Depression Inventory; CAPS, Clinician Administered PTSD Scale; CBT, Cognitive Behavioral Therapy; CC-BPAQ, the Chinese Revision of the Buss-Perry Aggression Questionnaire; CCMD-3, Chinese Classification of Mental Disorders Version 3; CD-RISC, Connor-Davidson Resilience Scale; CES-D, Center for Epidemiological Survey, Depression Scale; CTS, Conflict Tactics Scale; DAS, Dyadic Adjustment Scale; DSC, Depression Symptom Checklist; DSM-IV, The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; EPDS, Edinburgh Postnatal Depression Scale; EPDS-10, The Edinburgh Postnatal Depression Scale; ESRD, End-Stage Renal Disease; FBG, Fasting Blood Sugar; GAF, Global Assessment Function; GHQ, General Health Questionnaire; GQOLI-74, Generic Quality of Life Inventory-74; GSE, Generalized Self-Efficacy; HAMD, Hamilton Rating Scale for Depression – Chinese Version; HbA1c, Hemoglobin A1c; IAS, Interaction Anxiousness Scale; ICD-10, International Classification of Diseases, Tenth Revision; IIP, The Inventory of Interpersonal Problems; MDD, major Depressive Disorder; MHD, Maintenance hemodialysis; PANSS, The Positive and Negative Syndrome Scale; PSOC, Parenting Sense of Competence Scale; PSOC-E, Parenting Sense of Competence Scale – Efficacy subscale; PSOC-S, Parenting Sense of Competence Scale – Satisfaction subscale; PSSS, Perceived Social Support Scale; QLI, Quality of Life Index; QOL, Quality of Life; RESE, Regulatory Emotional Self-efficacy; SADS, Social Avoidance and Distress Scale; SAS, Self-rating Anxiety Scale; SAS, Social Adjustment Scale; SCID, Structured Clinical Interview for DSM-IV; SDS, The Zung Self-Rating Depression Scale; SDSS, Social Disability Screening Schedule; SES, Self Esteem Scale; SRFIS, Self-rating Feeling of Insecurity Scale; SSRI, Selective Serotonin Reuptake Inhibitor; SSRS, Social Support Rating Scale; SSRS, Social Support Scale; STAXI, State Trait Anger; SWIRS, Satisfaction with Interpersonal Relationships Scale; TAU, Treatment as Usual; TNC, Traditional Nursing Care; TRD, Treatment Resistant depression; WFSBP, World Federation of Societies of Biological Psychiatry; WHO-DAS II, The World Health Organization’s Disability Assessment Scale II.
3.2. Systematic review of IPT on Chinese patients with different psychiatric diagnoses
3.2.1. MDD (general population)
Comparing with medication-only, combination of IPT with antidepressants is significantly more effective for depressive symptoms and social functioning improvement (22–31). Among the 10 studies we reviewed, 9 used HAMD, 7 included SDSS in outcome measurements. A meta-analysis was performed and the results are detailed in 3.3.
In summary, 4 studies compared individual IPT plus medicine with medicine only (23, 26 29, 31). Follow-up assessments consistently showed improvement in HAMA and HAMD scores at 8- and 12- weeks for both groups and the effect (score reduction) was superior in those who received IPT. One study (26) targeted TRD (treatment resistant depression) subjects (tried at least 2 antidepressants at optimal doses with clinically appropriate durations, current HAMD ≥18) showed IPT group had better quality of life as reflected by higher SF-36 scores after treatment. Two others (29, 30) included social functionality and social support as outcome measurements. Both found better improvement in SDSS and SSRS in IPT groups.
Six studies (22, 24, 25, 27, 28, 30) investigated the effectiveness of IPT-G for MDD patients. Antidepressant was also used by both intervention and control groups. The intervention groups received 10 to 12 sessions of 50- to 100-min group IPT. All studies were conducted on inpatient subjects and excluded those with active suicidal ideations. Again, the results of all studies supported statistically better HAMD improvement in those received both IPT-G and medications. Most also showed lower SDSS scores after treatment in both IPT-G and control groups, with better reduction in IPT-G patients (22, 24, 25, 27, 28).
3.2.2. MDD (geriatrics)
Two studies conducted on Chinese geriatric patients found that 12 weekly IPT in combination with escitalopram or paroxetine showed more reductions in HAMDS and SDSS scores comparing with the medication-only group (p < 0.05) (32, 33). The sample sizes for the two studies were 84 and 98, both split evenly between IPT and control groups. One study (32) also checked GQOLI -74 and concluded that the total score and sub-scores of dimensions of social function and psychological function of the GQOLI -74 in the IPT group were significantly higher than those of the control group (p < 0.01), reflecting better overall self-reported wellbeing after IPT treatment. The results support that IPT and antidepressant together can help elder people improve depressive symptoms, social function, and quality of life.
3.2.3. MDD (adolescents)
Unfortunately, only one RCT study targeting adolescent population was retrieved. This study investigated the effectiveness of group IPT-B (6 weekly 90-min sessions) in treating junior middle school adolescents whose parents were economic migrants (34). After screening 113 candidates who met the screening criteria, the research team recruited 21 subjects who scored moderate to severe depression on BDI. Among those, 11 were randomly selected for group IPT. The result showed only IPT group had significantly decreased BDI following the intervention and the treatment effect was maintained at 90-day follow-ups (p < 0.001).
3.2.4. Postpartum depression
Six RCT studies showed promise of IPT for postpartum depression (35–40). One study compared 8 weekly 90-min IPT-G vs. 8 weekly 60-min CBT vs. traditional nursing care and concluded that comparing with traditional care, while both IPT-G and CBT had significantly better clinical outcomes in terms of EPDS, HAMD, DAS and IIP at 3 and 6 month follow ups, CBT group showed superiority in maintaining therapeutic effect in depression and dysfunctional attitudes (as measured by EPDS, HAMD and DAS) at 6-month follow-up (35). Three other studies (36, 37, 39) conferred the effectiveness of IPT-G in similar population comparing with TAU, and one found that those received IPT-G even achieved higher scores of self-report of parenting competence for neonates and more breast milk production (37). Furthermore, a recent study (38) compared individual IPT with CBT on 60 outpatients with PPD (30 for each group). Both groups received 12 weekly 50-min individual therapy sessions. The results showed reduced scores of EPDS and increased ratings in SSRS in both groups, indicating significant improvement in depression and social support. It also found that the total and sub scores of social support scale in IPT group were significantly higher than those in the CBT group (p < 0.05).
3.2.5. MDD (patients with medical conditions)
Two studies investigated IPT-G use in diabetic patients with depression. The results showed that Group IPT plus antidepressant can effectively reduce depressive symptoms and better blood sugar control (p < 0.05) (41, 42). Comparing with antidepressant-only group, those who also received 8–9 weekly 90-min group IPT demonstrated better FBG, 2hPBG and HbA1c after treatment. For end stage renal disease (ESDR) patients on MHD, depression could significantly affect treatment compliance and overall life quality. One study in this population showed that IPT-G was effective in alleviating affective, cognitive, behavioral, and somatic symptoms of depression (p < 0.01) (43).
3.2.6. GAD and social anxiety disorder
Three RCT studies compared IPT with CBT in treating GAD. Huang et al. studied 90 GAD patients who all scored ≥14 on HAMA at the time of recruitment (44). Thirty-one (31/45, complete rate 68.9%) completed 12 weekly 50-min IPT, and 33 (33/45, complete rate 73.3%) finished 12 weekly 50-min CBT. Both groups demonstrated significant reduction in HAMA total scores and a t-test showed no difference between the two groups in terms of reductions in total score and sub-scores except sleep disturbance, where CBT group had better effect (44). Two other studies (45, 46) on similar demographically comparable GAD subjects (n = 80 and 84) also supported the effectiveness of IPT in improving depression and anxiety measured by HAMA and HAMD, although CBT was superior in terms of improvement of quality of life. For social anxiety disorder patients, IPT and CBT performed better than the waiting list group in symptoms control (p < 0.05) (47); and patients received 12 weekly 120-min group IPT showed improvement in perceived self-efficacy in expressing positive affect (POS) and reduction in social avoidance and distress (p < 0.05) (48).
3.2.7. PTSD or patients with childhood trauma
A study on adults affected by the Sichuan 2008 earthquake showed the efficacy of IPT for PTSD (49). Those who received IPT, compared with TAU, had a significantly greater reduction of PTSD diagnoses (51.9% versus 3.4% p < 0.01). Another study investigated 48 college students with history of childhood abuse. After randomization, 25 subjects received 12-session individual IPT (2 times per week, each session 30–40 min) while the rest had TAU (50). The result supported that IPT could alleviate the anxiety and depression symptoms and improve psychosocial functionality in college students with childhood trauma. The degree of improvement was also found to be positively related to alleviation of subjects’ psychological insecurity and enhancement of their resilience.
3.2.8. Post-psychotic depression
PPD is the development of depression during the phase of remission of schizophrenia. Four studies found group and individual IPTs in addition to antidepressant can effectively alleviate depressive symptoms and improve overall functionality (51–54). Furthermore, it was also found that after treatment, the PANSS scores and WHO-DAS II scores of the combined group were significantly lower than the control group (p < 0.05), same as for compliance with antipsychotics (52, 54).
3.2.9. Special population and other diagnoses
For young college students (age 18–19), Group IPT or CBT, comparing with no treatment, could significantly reduce the aggressiveness level and improve social support; and IPT was superior in terms of sub-scores of Impulsivity and Hostility of CC-BPAQ (55, 56). Although studies are still lacking in IPT use in other psychiatric diagnoses in Chinese population, one study investigated the use of IPT plus duloxetine in treatment of somatoform disorder patients. The result showed that individual IPT (2 times per week, 50–60 min per session, total 12 sessions) plus duloxetine had a better therapeutic effect (p < 0.05) on depression and anxiety symptoms comparing with duloxetine alone (57). Also included in the same study was an arm of CBT plus duloxetine. No significant difference was found between IPT and CBT groups in terms of HAMA and HAMD score reductions. As for bipolar depression, one study compared IPT-G (8 weekly 60-min sessions) plus Lithium (750 mg – 1,500 mg per day) and Lithium only. Both groups had high HAMD-17 (≥17) for depression and low YMRS (<20) for mania at entry point. The result showed IPT-G group not only was effective (p < 0.05) in reducing HAMD score for bipolar depression but also could improve the quality of life measured by WHOQOL_BREF (58).
Finally, Gao et al. has done extensive studies on effects of an IPT-oriented postnatal program for Chinese first-time mothers (59–61). The intervention consisted of a 60-min education session before hospital discharge plus one telephone follow-up within 2 weeks. The program utilized specific IPT techniques, such as information giving, use of affect, clarification, reviewing relationship and communication patterns, and providing social support. The results showed women receiving IPT-oriented education had significantly fewer depressive symptoms (p = 0.026), higher level of social support (p = 0.009) and better maternal role competence (p < 0.001) at 6 weeks postpartum as compared with those who received only routine postnatal care. Because of high adherence rate, they also concluded that the IPT-oriented childbirth education could be an acceptable treatment option to facilitate the Chinese first-time mothers’ transition to motherhood.
3.3. Meta-analysis
We performed a meta-analysis on 10 studies conducted on MDD subjects (22–31). Our qualitative analysis of the efficacy of IPT in this population highlighted two forest plots.
The first forest plot (Figure 2) included all 9 studies that compared HAMD scores between IPT plus medication and medication-only groups before treatment and at 12 weeks. The overall efficacy of IPT was analyzed using a random-effects model and yielded a significant score difference of −3.45 [−4.05; −2.84] between the two groups (p < 0.0001). This difference is in favor of IPT plus antidepressant group as lower HAMD score reflects better improvement in depression.
Figure 2
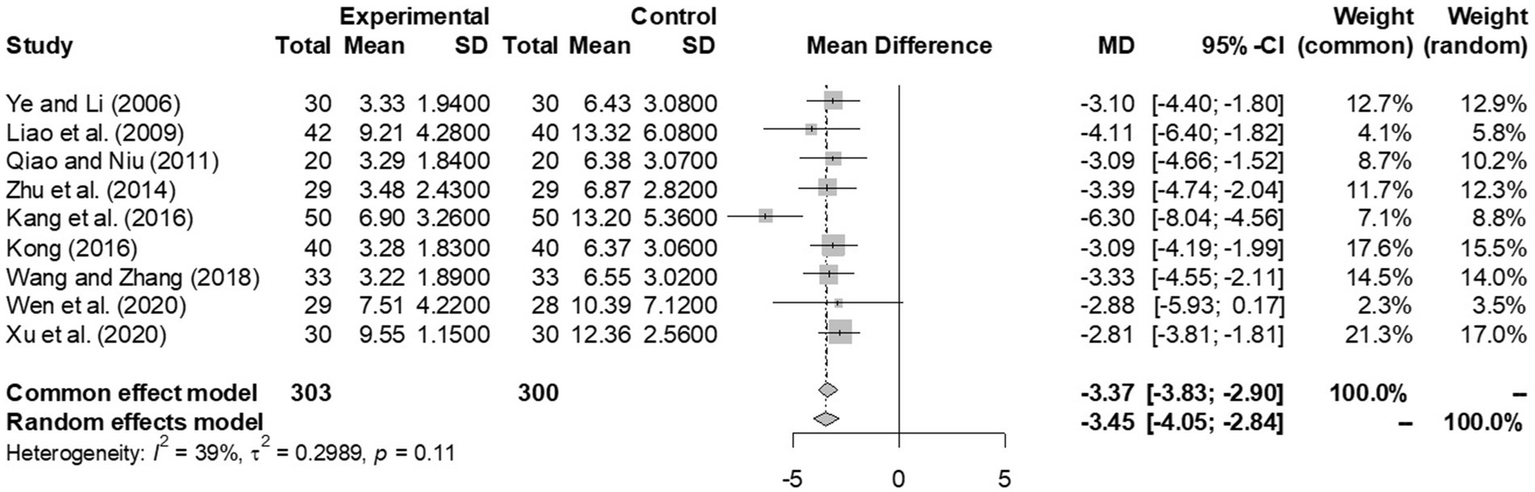
A forest plot outlining the overall HAMD score difference by 12 weeks in experimental (IPT + antidepressant) and control (antidepressant only) groups (p < 0.0001 from meta-analysis).
Including a study (29) that only used SDSS and SSRS as outcome measurement, a second forest plot (Figure 3) was generated to present the treatment efficacy of IPT by overall SDSS score change. One study only provided SDSS sub-scores (31) so was not included in this plot. Again, the random effects model resulted a score difference of −2.27 [−2.96; −1.59] in favor of the IPT group with a statistically significant difference (95% CI of −2.96 to −1.59, p < 0.001). Note that the random-effects model was the better approach since an I2 of 86%, the IPT outcome analysis revealed heterogeneity (p < 0.01) of all 6 studies included.
Figure 3
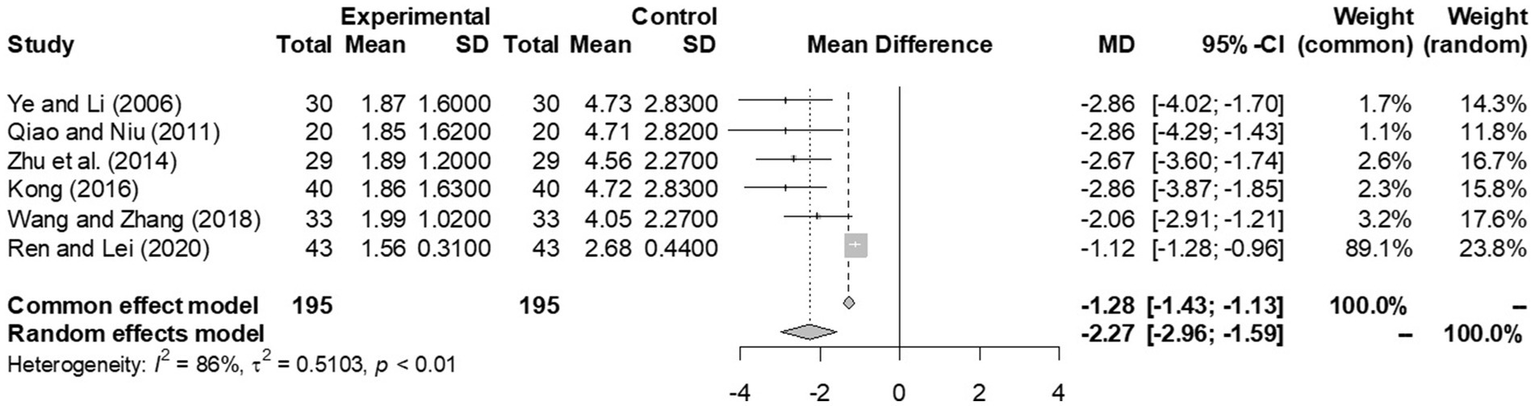
A forest plot outlining the overall SDSS score difference by 12 weeks in experimental (IPT + antidepressant) and control (antidepressant only) groups (p < 0.0001 from meta-analysis).
Unfortunately, due to limited number of studies, we were not able to conduct meta-analysis on IPT use in other Chinese populations.
3.4. Increasing number of IPT studies in China and their geographical distribution
Although IPT has not been commonly practiced in China, last two decades have seen an increasing number of clinical studies on IPT in Chinese population. While there were only 1 publication retrieved before 2006, we found 25 studies published in both Chinese and English journals after 2015. Figure 4 showed a geographical distribution map of IPT studies in mainland China. There was a noticeable regional difference in terms of the number of articles.
Figure 4
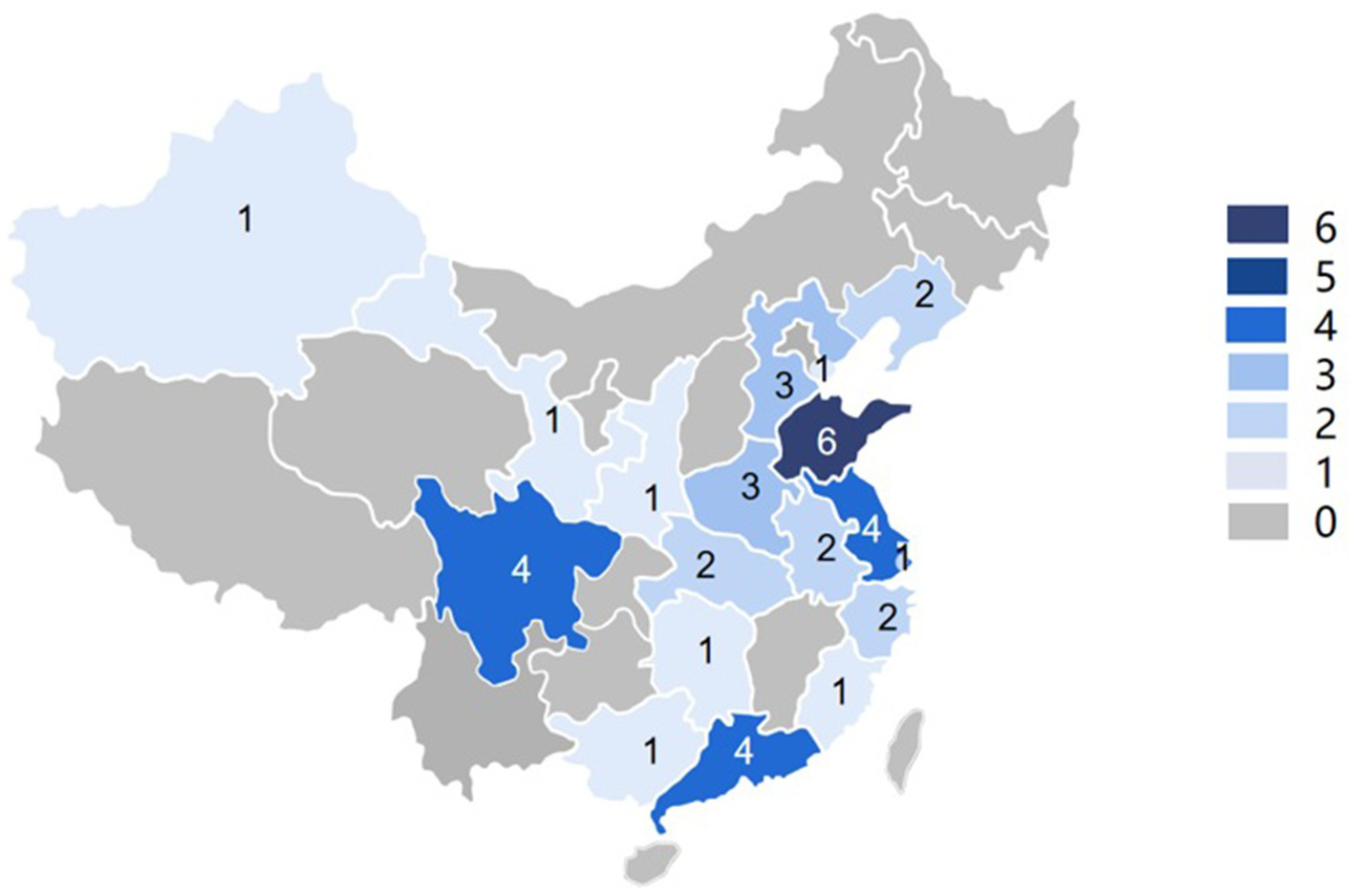
Map distribution of included IPT studies in mainland China.
4. Discussion
We conducted a comprehensive review of IPT clinical studies in China. Forty relevant publications in Chinese and English were carefully reviewed and included in our analyses. For quality control reason, only randomized controlled trials were included. The findings of the reviewed studies and our meta-analysis showed IPT is an effective treatment for MDD, postpartum depression, GAD, post-psychotic depression, and some other mental health conditions. There were symptom improvements after the treatment and the differences were statistically significant pre- and post-, and comparing with the control groups. This is consistent with IPT studies conducted internationally throughout the past decades (1–13).
Out of 40 articles, 35 were published in Chinese and 5 were in English. All 35 Chinese articles were published in Chinese indexed academic journals. Majority (27/40, 67.50%) were 2–3 pages and about half (19/40, 47.50%) had less than 3,000 words in length. Due to the brevity and limited article length, some of the articles did not present enough details of study design, subject recruitment, and randomization process. Besides age, gender and psychiatric diagnoses, other baseline characteristics of participants were rarely described. Only 10 studies provided data on treatment adherence and attrition. An additional caveat is the uncertainty about the professional qualification of IPT therapists. The professional backgrounds of intervention providers varied from therapists and psychiatrists to nurses and midwives. The majority did not report any formal IPT training. Only 11 studies (27.5%) reported that providers undertook some professional training in IPT. One study reported that their therapist had IPT certificate. IPT supervision was also deficient. Only 10 studies (25%) mentioned the availability of supervision during the intervention. In addition, very few studies mentioned the need for and importance of cultural adaptation.
Nonetheless, in this systematic review, we carefully selected studies with research designs that are rigorous enough to rule out potential confounds and alternative explanations of treatment outcomes. In general, all studies included were RCTs and clearly described clinical settings, general study design, targeting psychiatric diagnosis, and IPT treatment details (individual vs. group, phases, frequency, and duration). Most of the studies used direct comparison between IPT and a control group which enabled us to clarify differences in treatment effects. All GAD studies included CBT as a known effective intervention for comparison. Moreover, the sample sizes of all studies were sufficient to draw statistical conclusions; and the outcome measures were standardized rating scales that have been validated in Chinese populations.
The results of the current study have several important implications for IPT research and knowledge dissemination in China. First, the findings of current studies have shown the efficacy of IPT in certain mental disorders particularly depression. It provides scientific evidence that IPT is effective and beneficial to Chinese population. Given the complex history of modern psychotherapy in China and its exponentially growing demand among nearly 1.4 billion citizens, our study paved the way for further promoting IPT as a treatment modality in mental health care, for developing evidence-based psychotherapy guidelines, and for improving the quality of clinical care. Second, the use of standardized measurement methods that allow for the assessment of treatment outcomes has become non-exceptional in psychotherapy studies in China. This is imperative in any mental health studies. Our study helps future Chinese IPT researchers understand the importance of this and hopefully can encourage those standard instruments to be used to supplement traditional clinical measures of treatment effectiveness, even in daily psychotherapy practices. Third, this review is a call for formal training and supervision of IPT therapists in China. This is important both in research and clinical practice. To maintain high standards and consistency in IPT, creation of a formal training and certification process in China has become a priority. This would not only help therapists improve their quality of care but also be recognized for their expertise in IPT. In addition, given that the majority of the trials were conducted in coastal and central part of China, we hope future IPT resources can be more properly allocated to cover those provinces and cities where mental health treatment was less accessible. Finally, incorporating cultural components into IPT practice is an imminent need. IPT was originally developed and tested in Western cultures. Questioning the extent of this treatment option’s effectiveness for Chinese people deep rooted with Confucius cultural background is legitimate. Even if interpersonal issues are universal, one important concern is whether IPT can be adapted to address Chinese cultures without changing its fundamental theories and elements. As none of the reviewed articles mentioned cultural modifications when practicing IPT in China, our study highlighted the importance of adapted and local IPT research and suggested for such a consideration in future related research. We emphasize this because the final acceptance of a Western psychotherapy model like IPT for people with a totally different cultural background depends on not only whether it is effective, but also how applicable it is in their values and beliefs.
Our study is not without limitations. First, the number of retrieved studies is relatively small, given a country with such a large population. Even for the most well-researched MDD population, there were only 10 randomized controlled trials included in the meta-analysis. Second, as mentioned above, some studies did not provide enough details on subject recruitment and participant demographics therefore the comparability and overall quality of the study may not be good enough to convince the efficacy of IPT as an intervention. Other issues included therapist qualification, subject selection bias, small samples, accuracy of diagnosis and concurrent use of other medications may be confounding factors that contributed significantly to the treatment outcomes. After all, none of the studies was conducted at more than one site. The results are not necessarily generalizable to other clinical sites or settings. Finally, like other meta-analyses, when we combined those studies using same diagnosis, outcome measures and same follow up schedules, the summary effect may ignore important differences between studies therefore be biased to certain extent.
5. Conclusion
In summary, in this comprehensive review of IPT use in China, we have identified the current best evidence for IPT efficacy in a variety of psychiatric disorders. Although the findings show the effectiveness of IPT in Chinese patients with certain psychiatric conditions, as this is the first systematic review of this topic, we caution not to overstate the apparent effects, given very few studies were available for each population. Still, due to lack of structured training and supervision opportunities, there remain substantial gaps in our knowledge of where, how, and when IPT should be implemented, and who can be trained and qualified to deliver IPT service in mainland China.
Funding
This study was funded by the Medical Science and Technology Project of Zhejiang Province, China (Funding Number: 2022503897).
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Statements
Author contributions
WZ: conceptualization, methodology, validation, investigation, resources, writing – original draft and review and editing, and supervision. LT: conceptualization, methodology, data collection, reviewing, writing – original draft, and review and editing. FX and GY: methodology, data collection, reviewing, and writing – original draft. CL: statistical analysis and validation. SW: methodology, statistical analysis, validation, and writing – original draft. All authors contributed to the article and approved the submitted version.
Acknowledgments
We thank the Tong De Hospital of Zhejiang Province for kindly supporting our study and the Department of Epidemiology and Biostatistics, West Virginia University for providing statistical support to this project
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Klerman GL Weissman MM . Interpersonal psychotherapy of depression: a brief, focused, specific strategy. New York: Jason Aronson Inc. (1994).
2.
Weissman MM Markowitz JC Klerman GL . The guide to interpersonal psychotherapy. New York: Oxford University Press (2018).
3.
"Overview of IPT. (n.d.) International Society of Interpersonal Psychotherapy – ISIPT. Available at: https://interpersonalpsychotherapy.org/ipt-basics/overview-of-ipt (Accessed June 14, 2023).
4.
Zhou SG Hou YF Liu D Zhang XY . Effect of cognitive behavioral therapy versus interpersonal psychotherapy in patients with major depressive disorder: a meta-analysis of randomized controlled trials. Chin Med J. (2017) 130:2844–51. doi: 10.4103/0366-6999.219149
5.
Novick DM Swartz HA . Evidence-based psychotherapies for bipolar disorder. Focus (Am Psychiatr Publ). (2019) 17:238–48. doi: 10.1176/appi.focus.20190004
6.
Markowitz JC Choo TH Neria Y . Do acute benefits of interpersonal psychotherapy for posttraumatic stress disorder endure?Can J Psychiatr. (2018) 63:37–43. doi: 10.1177/0706743717720690
7.
Markowitz JC Lipsitz J Milrod BL . Critical review of outcome research on interpersonal psychotherapy for anxiety disorders. Depress Anxiety. (2014) 31:316–25. doi: 10.1002/da.22238
8.
Miniati M Callari A Maglio A Calugi S . Interpersonal psychotherapy for eating disorders: current perspectives. Psychol Res Behav Manag. (2018) 11:353–69. doi: 10.2147/PRBM.S120584
9.
Cuijpers P Geraedts AS van Oppen P Andersson G Markowitz JC van Straten A . Interpersonal psychotherapy for depression: a meta-analysis. Am J Psychiatry. (2011) 168:581–92. doi: 10.1176/appi.ajp.2010.1010141
10.
de Mello MF de Jesus MJ Bacaltchuk J Verdeli H Neugebauer R . A systematic review of research findings on the efficacy of interpersonal therapy for depressive disorders. Eur Arch Psychiatry Clin Neurosci. (2005) 255:75–82. doi: 10.1007/s00406-004-0542-x
11.
Swartz HA Grote NK Graham P . Brief interpersonal psychotherapy (IPT-B): overview and review of evidence. Am J Psychother. (2014) 68:443–62. doi: 10.1176/appi.psychotherapy.2014.68.4.443. PMID: 26453346; PMCID: PMC4603530
12.
Morrell CJ Sutcliffe P Booth A Stevens J Scope A Stevenson M et al . A systematic review, evidence synthesis and meta-analysis of quantitative and qualitative studies evaluating the clinical effectiveness, the cost-effectiveness, safety and acceptability of interventions to prevent postnatal depression. Health Technol Assess. (2016) 20:1–414. doi: 10.3310/hta20370. PMID: 27184772; PMCID: PMC4885009
13.
Ravitz P Watson P Lawson A Constantino MJ Bernecker S Park J et al . Interpersonal psychotherapy: a scoping review and historical perspective (1974–2017). Harv Rev Psychiatry. (2019) 27:165–80. doi: 10.1097/HRP.0000000000000219. PMID: 30883446
14.
World Health Organization . mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings: Mental health gap action programme (mhGAP). Geneva: WHO (2016).
15.
Parikh SV Quilty LC Ravitz P Rosenbluth M Pavlova B Grigoriadis S et al . Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder: Section 2. Psychological Treatments. Can J Psychiatry. (2016) 619:524–39. doi: 10.1177/0706743716659418
16.
NBSC (National Bureau of Statistics of China) . Main data of the seventh national population census. Beijing: National Bureau of Statistics of China.
17.
World Health Organization . (n.d.). Mental health in China. Available at: https://www.who.int/china/health-topics/mental-health (Accessed January 25, 2023).
18.
Chen H Phillips M Cheng H Chen Q Chen X Fralick D et al . Mental Health Law of the People's Republic of China (English translation with annotations): translated and annotated version of China's new Mental Health Law. Shanghai Arch Psychiatry. (2012) 24:305–21. doi: 10.3969/j.issn.1002-0829.2012.06.001
19.
Schwarzer G . meta: an R package for meta-analysis. R News. (2007) 7:40–5.
20.
Schwarzer G Efthimiou O Rücker G . Inconsistent results for Peto odds ratios in multi-arm studies, network meta-analysis and indirect comparisons. Res Synth Methods. (2021) 12:849–54. doi: 10.1002/jrsm.1503
21.
Page MJ McKenzie JE Bossuyt PM Boutron I Hoffmann TC Mulrow CD et al . The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 29:n71. doi: 10.1136/bmj.n71. PMID: ; PMCID: PMC8005924
22.
Ye HP Li M . Group interpersonal psychotherapy for inpatient with major depression. Chin Ment Health J. (2006) 20:524–37. doi: 10.3321/j.issn:1000-6729.2006.08.013
23.
Ying L Xiaomao Z Kebin W . A control study of interpersonal psychotherapy combined with SSRI in depression. J Clin Psychosom Dis. (2009, 2009) 15:534–6. doi: 10.3969/j.issn.1672-187X.2009.06.025.0534-03
24.
Qiao ST Niu XL . Effect study of team interpersonal psychotherapy on inpatients with depression. Chin J of Clinical Rational Drug Use. (2011) 4:40–1. doi: 10.3969/j.issn.1674-3296.2011.26.027
25.
Zhu JJ Zhu FX Yang ZW . Effectiveness of group interpersonal psychotherapy for improving the clinical symptoms and social functions of inpatient patients with depression. Contemp Med Forum. (2014) 12:110–1. doi: 10.3969/j.issn.2095-7629.2014.11.104
26.
Kang H Hang J Zemg Q Tao JQ Liang SW . The efficacy of interpersonal psychotherapy combined with medicine in treatment of patients with treatment-resistant depression. Intern Med. (2016) 11:521–4. doi: 10.16121/j.cnki.cn45-1347/r.2016.04.05
27.
Kong HT . The effect of group interpersonal psychotherapy on inpatients with depression. Guide China Med. (2016) 14:174–5.
28.
Wang ST Zhang YH . Analysis of efficacy of group interpersonal psychotherapy on inpatients with depression. World Latest Med Informat (Electronic Version). (2018) 18:76–9. doi: 10.19613/j.cnki.1671-3141.2018.30.043
29.
Ren DM Lei SH . Effect of interpersonal psychotherapy on social function of patients with depression. Healthful Friend. (2020) 21:102.
30.
Wen M Sun HY Liu Y Wang JJ . Effectiveness of group interpersonal psychotherapy(IPT) for improving the depressive symptoms and social functions of patients with depression. Home Med. (2020) 4:396–7.
31.
Xu LX Shi YS Xiong CE Liu ZS Hang CP Zeng DZ et al . Effect of interpersonal psychotherapy on social function of patients with depression. Chin J Health Psychol. (2020) 05:641–4. doi: 10.13342/j.cnki.cjhp.2020.05.001
32.
Sun L Wang Y Chen QG Yang JL . Effect of escitalopram combined with team interpersonal psychotherapy on social function and life quality of geriatric depression patients. Sichuan Mental Health. (2016) 29:311–4. doi: 10.11886/j.issn.1007-3256.2016.04.005
33.
Wang XB Li M . Effects of paroxetine combined with group interpersonal psychotherapy on SDSS score and HAMD-17 in elderly patients with depression. Hebei Medical Journal. (2022) 18:2786. doi: 10.3969/j.issn.1002-7386.2022.18.014
34.
Sun H Zhang T . The effectiveness of group interpersonal psychotherapy to immigrant children in junior middle school with depression. Chin J Clin Psych. (2020) 28:212–6. doi: 10.16128/j.cnki.1005-3611.2020.01.044
35.
Rao SZ ,LiCH,ShenWLZhangHZhanGLXuPet al. A comparative evaluation on the efficacy of cognitive behavioral therapy and group interpersonal psychotherapy for postpartum depression. J Neurosci Mental Health (2009)9: 305–308 doi:10.3969/j.issn.1009-6574.2009.04.010
36.
Liu Q . Analysis of the effect of nursing care intervention on postpartum depression. Med Inf. (2010) 10:2864–5. doi: 10.3969/j.issn.1006-1959.2010.10.238
37.
Shi YJ Li FL . Effect of group interpersonal psychotherapy on clinical symptoms, milk secretion ability to take care of baby and social function in primiparas with postpartum depression. Chin J Health Psychol. (2019) 27:248–51. doi: 10.13342/j.cnki.cjhp.2019.02.024
38.
Jin M Zhao H Liu J Lei H Wang JJ . Influence of interpersonal psychotherapy and cognitive behavior therapy on treatment effect and social support of postpartum depression. J Clin Psychiatry. (2020) 30:273–5.
39.
Wang JJ . The application value of interpersonal psychotherapy for postpartum depression patients. Health Must Read Magaz. (2021) 33:13–4.
40.
Lin CC . The effect of interpersonal psychotherapy on mental health status and postpartum depression incidence of primiparas. Big Health. (2020) 35:196.
41.
Du W . The effect of group interpersonal psychotherapy on diabetes patients with depression. China High Med Educat. (2012) 2:147. doi: 10.3969/j.issn.1002-1701.2012.02.071
42.
Hu CL . The efficacy of group interpersonal psychotherapy on diabetic patients with depression. Chin J Health Psychol. (2013) 21:1229–30.
43.
Jiang L Li XD . Effect of group interpersonal psychotherapy on depression in maintenance hemodialysis patients. Clin J Med Offic. (2010) 38:855–6. doi: 10.3969/j.issn.16713826.2010.05.069
44.
Huang HL Liu XM Wang RQ Wu YG Jiang Q Jin MQ . Effects of interpersonal psychotherapy and cognitive behavioral therapy on generalized anxiety disorder: a controlled study. Chin J Health Psychol. (2016) 24:186–9. doi: 10.13342/j.cnki.cjhp.2016.02.00
45.
Liang WF . The effect of interpersonal psychotherapy and cognitive behavior therapy on generalized anxiety disorder. Med Diet Health. (2019) 5:45.
46.
Li J . Effect of interpersonal psychotherapy and cognitive behavior therapy on generalized anxiety disorder. CHSM. (2021) 10:43–5. doi: 10.3969/j.issn.1674-9316.2021.10.015
47.
Huang HL Liu XM . Effects of group interpersonal psychotherapy and group cognitive behavioral therapy on social anxiety in college students. Chin Ment Health J. (2011) 25:324–8. doi: 10.3969/j.issn.1000-6729.2011.05.002
48.
Lin ZJ Wang CL Lin HX Yang C . A study on the effect of the group interpersonal psychotherapy in the regulatory emotional self-efficacy of social phobia adolescents. Chin J Gen Pract. (2018) 16:1507–151. doi: 10.16766/j.cnki.issn.1674-4152.000412
49.
Jiang RF Tong HQ Delucchi KL Neylan TC Shi Q Meffert SM . Interpersonal psychotherapy versus treatment as usual for PTSD and depression among Sichuan earthquake survivors a randomized clinical trial. Confl Heal. (2014) 8:14. doi: 10.1186/1752-1505-8-14
50.
Li JJ Wei XY Zheng YL Gao JS . Effect of interpersonal psychotherapy on anxiety disorder of 48 college students. Chin J School Doctor. (2022) 36:432–5.
51.
Zhou LL Sun QK Liu SP Jia JT . The effect of group interpersonal psychotherapy on social function of convalescent mental illness patients. J Chin Psychiatry. (2013) 22:66.
52.
Lu ZS Chen Z . Observation on the effect of interpersonal psychotherapy in the treatment of post-schizophrenia depression. J Psychiatry. (2014) 27:460–1. doi: 10.3969/j.issn.1009-7201.2014.06.021
53.
Zhou RL . The effect of interpersonal psychotherapy on post-schizophrenia depression. China Contin Med Educ. (2018) 10:73–5. doi: 10.3969/j.issn.1674-9308.2018.08.035
54.
Kang J . Prospective randomized cohort study on the efficacy of interpersonal psychotherapy and cognitive therapy in the treatment of post-schizophrenia depression. Clin Res Pract. (2019) 8:19–21. doi: 10.19347/j.cnki.2096-1413. 201908008
55.
Li Y Roslan SB Ahmad NAB Omar ZB Zhang L . Effectiveness of group interpersonal psychotherapy for decreasing aggression and increasing social support among Chinese university students. J Affect Disord. (2019) 251:274–9. doi: 10.1016/j.jad.2018.12.051
56.
Li YT Zhang YL . Ma L the intervention of group cognitive behavior therapy and interpersonal psychotherapy on high aggressive college freshmen. Comput Campus. (2019) 5:7763–5.
57.
Guan L Li S . A comparative study of interpersonal psychotherapy and cognitive-behavioral therapy in the treatment of somatoform disorders. Med Philos. (2016) 73:36–7. doi: 10.12014/j.issn.1002-0772.2016.02b.11
58.
Chen SF Liu Y Li SZ Zhang L . The clinical application of group interpersonal psychotherapy for depressive episodes in bipolar disorder. J Int Psychiatry. (2017) 44:1015–7.
59.
Gao LL Chan SW Li X Chen S Hao Y . Evaluation of an interpersonal-psychotherapy-oriented childbirth education programme for Chinese first-time childbearing women a randomised controlled trial. Int J Nurs Stud. (2010) 47:1208–16. doi: 10.1016/j.ijnurstu.2010.03.002
60.
Gao LL Chan SW Sun K . Effects of an interpersonal-psychotherapy oriented childbirth education programme for Chinese first-time childbearing women at 3-month follow up: randomised controlled trial. Int J Nurs Stud. (2012) 49:274–81. doi: 10.1016/j.ijnurstu.2011.09.010
61.
Gao LL Xie W Yang X Chan SW . Effects of an interpersonal-psychotherapy-oriented postnatal programme for Chinese first-time mothers: a randomized controlled trial. Int J Nurs Stud. (2015) 52:22–9. doi: 10.1016/j.ijnurstu. 2014.06.006
Summary
Keywords
IPT, interpersonal psychotherapy, China, psychotherapy, therapy
Citation
Tang L, Xu F, Yu G, Li C, Wen S and Zheng W (2023) Efficacy of interpersonal psychotherapy in mainland China: a systematic review and meta-analysis. Front. Psychiatry 14:1160081. doi: 10.3389/fpsyt.2023.1160081
Received
06 February 2023
Accepted
19 June 2023
Published
12 July 2023
Volume
14 - 2023
Edited by
Paola Bozzatello, University of Turin, Italy
Reviewed by
Holly Swartz, University of Pittsburgh, United States; Claudio Brasso, University of Turin, Italy
Updates
Copyright
© 2023 Tang, Xu, Yu, Li, Wen and Zheng.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wanhong Zheng, wzheng@hsc.wvu.eduLuhan Tang, tlhwork@163.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.