- 1PCCEI, University of Montpellier, INSERM, EFS, University of Antilles, Montpellier, France
- 2Haiphong University of Medicine and Pharmacy, Haiphong, Vietnam
- 3Department of Infectious and Tropical Diseases, Viet Tiep Hospital, Haiphong, Vietnam
- 4Supporting Community Development Initiatives, Hanoi, Vietnam
- 5Infectious Diseases Department, Caremeau University Hospital, Nîmes, France
- 6School of Global Public Health, New York, NY, United States
- 7CESP Inserm UMRS, Pierre Nicole Center, Paris Saclay University, Fench Red Cross, Paris, France
Background: The co-occurrence of substance use disorder and mental disorder, known as dual diagnosis, has a distressingly high prevalence among individuals grappling with either of these conditions. Mood disorders, especially depression, constitute a substantial burden for People Who Inject Drugs (PWID) and a significant public health concern in Vietnam. Identifying risk factors for depression in PWID is imperative for the development of targeted interventions.
Methods: We enrolled PWID into a cohort using the respondent-driven sampling method. Over a 36-month period, we systematically tracked the emergence of depression and employed multiple imputation in conjunction with a mixed nonlinear model to pinpoint risk factors for depression in this demographic. At inclusion, depression was screened using the PHQ-2 questionnaire, and subsequent episodes of depression were assessed semi-annually using the CES-D8.
Results: Three hundred and ninety-one PWID (26.6%) were depressed. Major risk factors for depression included being female, not having a permanent residency, having been hospitalized and using methamphetamine more than weekly. Other risk factors included age, being single, not having a health insurance card and not being on methadone.
Limitations: The exclusion of missing visits and social desirability could have led to selection and information biases. In this observational study, confusion biases are possible despite our best efforts.
Conclusion: Depression is alarmingly frequent in PWID. In this study taking in account the chronological relationship between sociodemographic and clinical factors and depression, risk factors were identified in this specific setting of low-to-middle income country. The findings highlight the need to develop innovative targeted psychiatric interventions with the help of supporting peers.
1. Introduction
Dual diagnosis, or the co-occurrence of substance use disorders (SUD) with psychiatric comorbidities (such as depression, anxiety disorders, suicidal tendencies, etc.), is relatively uncommon in the general population (approximately 2 to 3%) (1). However, it is found in an alarming prevalence ranging from 40 to 50% in patients presenting with either condition (2–5). While further elucidation is required to fully comprehend the reasons behind the frequent association of these two conditions (6, 7), it is observed that they tend to progress concurrently within the same individual, exerting mutual influence on each other’s prognosis (8). Consequently, they lead to severe consequences in socio-professional aspects (9), clinical domains (physical comorbidities, risk behaviors) (10–13), delayed detection of viral illnesses (14), and hindered access to healthcare in general (15).
The most common psychiatric condition in patients with SUD are mood disorders, with prevalence rates varying from 17% in Canada to a broader range of 27 to 85% in Australia, as reported in a meta-analysis (1, 4). More specifically, the prevalence of major depressive disorders in community and clinical settings among individuals with SUD was found to be 25% in a comprehensive meta-analysis comprising 48 studies from around the world (16). However, these rates varied depending on the studied population, type of substance and country considered.
In Vietnam, as in numerous low- to middle-income countries (LMICs), psychiatric resources are sparse, resulting in a saturated mental health system (17) managing mainly the most severely ill patients because of a lack of human and material resources.
In this context, targeting specifically people who inject drugs (PWID) who are in need of mental health support is therefore crucial for they present, among other mental health issues, significantly higher rates of depression (18). Previous studies analyzing risk factors for depression were sparse among PWID living in LMIC (19), where the expression of depression is not as prevalent as in high income countries and where associated factors might differ. Moreover, these studies with cross-sectional designs (20) identified only factors associated with depression and not risk factors for depression whose estimating requires following up the population (21, 22). Indeed, the chronological knowledge of the situation must be taken in account in order to better understanding the mechanisms and offer tailored prevention strategies.
The aim of our project is to develop a community-based innovative intervention plan to prevent and limit the burden of depression in this specific population. In order to do so, we aimed in this study to explore longitudinal associations between depressive symptoms and patient characteristics in people who inject drugs in Hai Phong, Vietnam.
2. Materials and methods
2.1. DRIVE study population and recruitment
The Drug use and Infections in Vietnam (DRIVE) program is an international project launched in 2016 whose goal was to end the HIV epidemic among PWID in Hai Phong, Vietnam (23). The DRIVE study relied on extensive HIV screening via community-based respondent-driven sampling (RDS) surveys combined with linkage to HIV care. The RDS method allows access to hard-to-reach populations, hidden from care and inaccessible through classic recruitment methods (24).
Three rounds of annual RDS surveys from November 2016 to November 2018 targeted 3,150 PWID. The inclusion criteria were being at least 18 years old, having a positive urine test for heroin or methamphetamine and having skin marks from a recent injection (23). Those unable to understand the study information or unwilling to consent were not enrolled.
Starting from the first RDS survey, two open cohorts were created: one with HIV-negative participants to estimate HIV incidence and another with HIV-positive participants to estimate the cascade of HIV care dynamics. All RDS HIV-positive participants were invited to be included in the cohort and were then provided counseling and peer support to help them connect with care and initiate or remain on antiretroviral treatment (ART) as well as encourage them to pursue methadone maintenance therapies (MMTs). HIV-negative participants were recruited until the target cohort size was reached, which was set to 400 for RDS1 and 400 for the next two RDS rounds, excluding those who reported already being treated with methadone (25). Participants were enrolled in the cohort for 12 to 36 months depending on their date of recruitment, with follow-up visits every 6 months.
2.2. Selection
In this study, sociodemographic, drug habit, psychological, behavioral and health event-related data from all PWID recruited in the previously described HIV+ and HIV- cohorts and who participated in at least one follow up visit were included.
2.3. Measures
2.3.1. Primary outcome
At baseline (RDS survey), depression was screened with a short form of the Patient Health Questionnaire (PHQ-2) (26), in face-to-face interview with trained community-based organization (CBO) member. Participants with a score strictly superior to 2 were considered depressive (27, 28).
During semiannual follow-up visits, depression was measured by trained doctors from the Hai Phong University of Medicine and Pharmacy using a short form of the Center for Epidemiologic Studies- Depression (CES-D8) questionnaire (29), shown to facilitate the efficiency of assessment during epidemiological studies (30). Because the original cutoff of ≥7 was determined in women, who represent 5% of PWID in Hai Phong, we used a lower cutoff of ≥6 (31).
2.3.2. Other psychiatric disorders
Participants were screened for anxiety at the time of the RDS survey with the short Generalized Anxiety Disorder questionnaire (GAD-2) developed to screen for anxiety in primary care patients and the general population, with a published cutoff of ≥3 (32).
Participants who screened positive for any mental health issue during the RDS survey or during follow-up were invited to meet with a psychiatrist for a full clinical assessment followed by other consultations when necessary at the study site.
2.3.3. Substance use
Data were collected by trained interviewers (CBO members) using a face-to-face questionnaire on drug and alcohol use. The questionnaire created for the study included questions on duration, age of initiation, frequency and substances injected, as well as on the use of other non-injected substances including alcohol. Its content has been described in greater detail elsewhere (25, 33). PWID were also screened for opiates, methadone, methamphetamine and cannabis by urine tests.
A high heroin injection frequency referred to PWID reporting more than 30 injections in the past month. Methamphetamine use had two categories, “no use or less than once per week” and “more than once per week” (34). We combined urine tests and questions about drug use in the past 6 months to define polydrug use as using any drug other than heroin or methamphetamine (ketamine, ecstasy, cocaine or cannabis) in addition to heroin, which was used by all participants.
Alcohol misuse was assessed through Audit-C, a 3-item questionnaire including the first questions of the AUDIT questionnaire, with a cutoff of ≥3 for women and ≥ 4 for men (35).
2.3.4. Other medical data
At the RDS visit, CBO members collected individual sociodemographic measures: gender, age and education level. During the cohort follow-up, they collected data on major health and life events (overdoses and arrests), as well as social and structural sociodemographic measures (relationship status, stable housing and health insurance card). PWID were also asked if they had been hospitalized during the past 6 months, whatever the reason, and were tested for HCV and HIV at every visit.
2.4. Statistical analysis
We analyzed risk factors for depressive syndrome among PWID over up to 3 years. These potential risk factors were sociodemographic (gender, age, relationship status, stable housing and health insurance card), drug habits (methamphetamine use, high heroin injection frequency, polydrug use, alcohol misuse, being on MMT and more than 10 years since the first heroin injection), and health events (having been hospitalized in the past 6 months, HCV status and HIV status). Anxiety was not entered in the model as cofounder because of anxiety-related questions within the CES-D scale (36). People with depressive syndrome at baseline according to the PHQ-2 were not included in our model. We censored participants from the time they began antidepressant treatment.
A mixed nonlinear model was used for the main analyzes in order to explore longitudinal associations between depression and patient characteristics. We developed multiple models that differed in the number of variables and the inclusion of random intercepts and then compared their quality to select the final model.
To deal with missing completely at random (MCAR) data for participants who had completed their follow-up visits, we selected complete outcome cases and used a multiple imputation technique: the model was apply to 20 datasets of possible values created via linear regression or discriminant function method depending on the variable and parameter estimates were combined to obtain final adjusted odds ratio and their 95% confidence intervals (CIs) (36–38).
The data analysis for this paper was performed using SAS software version 9.4. Copyright © 2013 SAS Institute Inc.
2.5. Ethics consideration
The DRIVE study was approved by the Institutional Review Boards of the Hai Phong University of Medicine and Pharmacy, the Icahn School of Medicine at Mount Sinai, and the New York University School of Medicine. All participants provided signed informed consent.
3. Results
3.1. Population selection
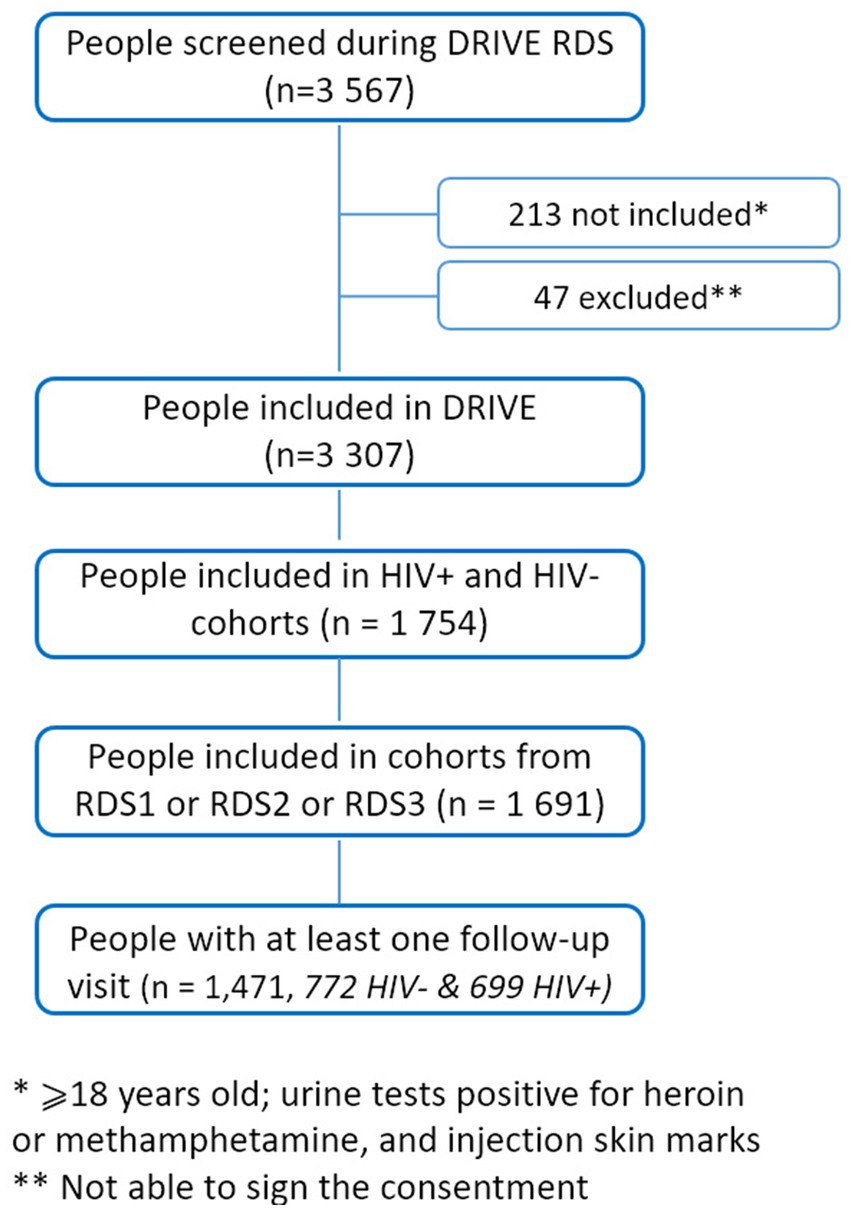
Of the 1,691 people included in the DRIVE cohort, 215 never returned for any follow-up visits, 2 died. and 3 began antidepressant treatment before the first follow-up. In total, 1,471 people were included in our study, 772 from the HIV-negative cohort and 699 from the HIV-positive cohort (Figure 1). They were followed up from 2 to 35 months (16 months on average) with a mean number of 3.3 visits. 771 PWID followed up during 6 visits, 371 during 4 visits and 329 during 2 visits were included at the first, second and last RDS survey, respectively (Supplementary Figure S1).
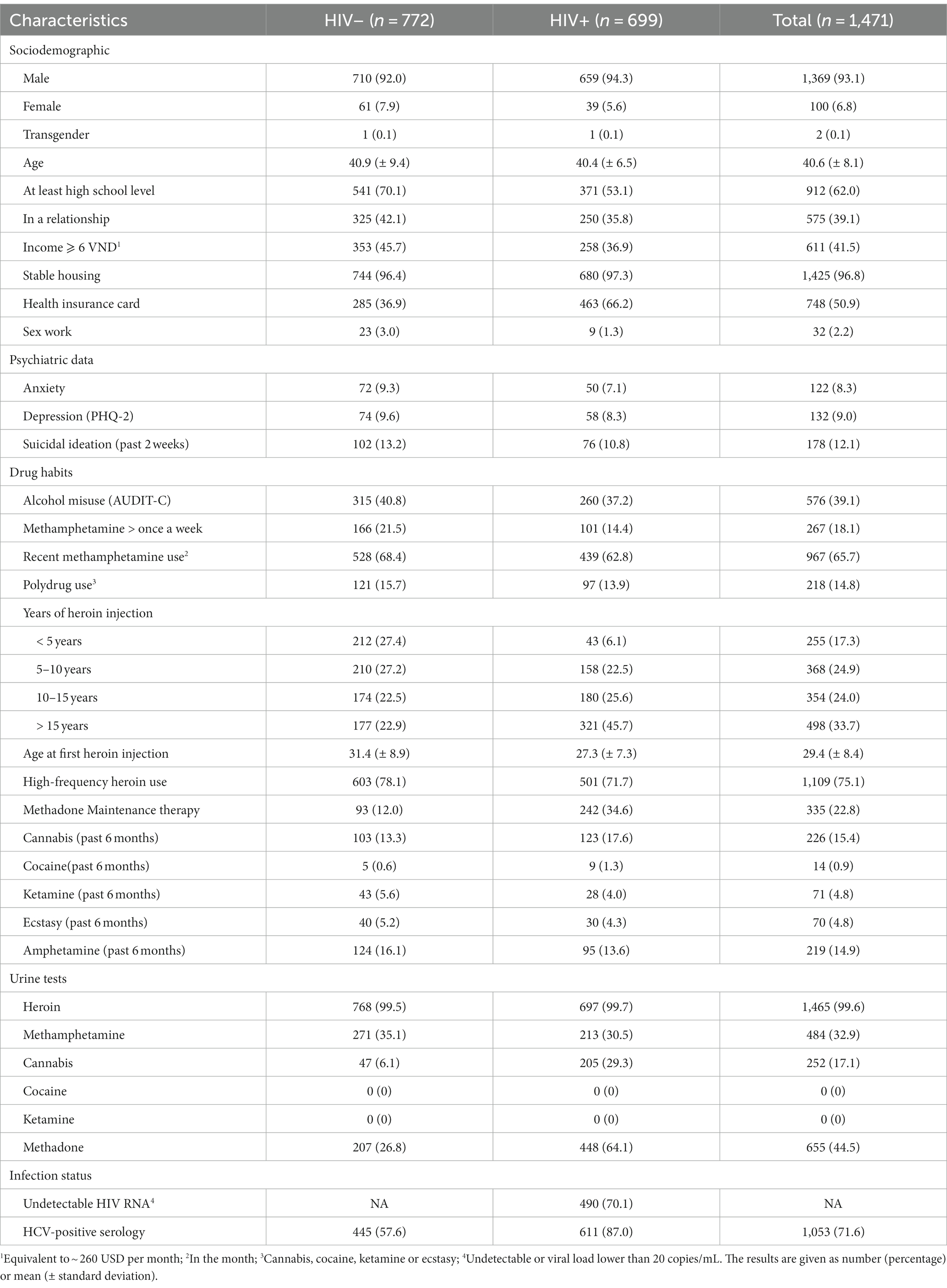
3.2. Population characteristics
All participants were heroin users, 93% were male, and their mean age was 41 years (Table 1). Overall, HIV-infected participants were less educated (53% vs. 70%), injected heroin for longer (63% used it for more than 10 years vs. 37%), and were more often on MMT (35% vs. 12%).
Of our 6,768 planned follow-up visits, 5,201 (76.8%) were completed. During follow-up, 56 people had died, including 1 from suicide, 2 from overdoses and 2 for unknown reasons. Other causes of death had no direct link with depression. 394 (5.8%) visits were attended but had incomplete data on the CES-D8 questionnaire.
The 329 participants who dropped out (22%) were younger, were less likely to be in a relationship or in a stable housing, were more depressed at inclusion, and were more likely to use methamphetamine more than once per week. They were less likely to be enrolled in methadone maintenance therapy and less likely to be infected by HIV (Supplementary Table S1).
3.3. Prevalence of depression
The proportion of depressed participants was 11.9% at baseline. The number of PWID depressed at one or more visits was 391 (26.6%). Among people free from depression in the 2 weeks prior to inclusion based on the PHQ-2, 320 (23.8%) developed depression over the mean 16 months of follow-up.
3.4. Risk factors for depression
No permanent residency [OR = 5.6, 95% CI (2.2–14.6)], gender [female: OR = 4.0, 95% CI (2.0–7.9)], having been hospitalized and using methamphetamine at least once a week [OR = 3.1, 95% CI (1.8–5.2)], not being in relationship nor on methadone [OR = 2.0, 95% CI (1.1–3.5)], not having an insurance card [OR = 1.7, 95% CI (1.2–2.4)], age [OR = 1.3, 95% CI (1.0–1.7) for every 10 years] were all significant risk factors for depression. Time since inclusion in the cohort was a protective factor against depression [OR = 0.6, 95% CI (0.5–0.8) for each year in the cohort]. Being infected with HCV tended to be associated with depression without statistically significant (Figure 2).
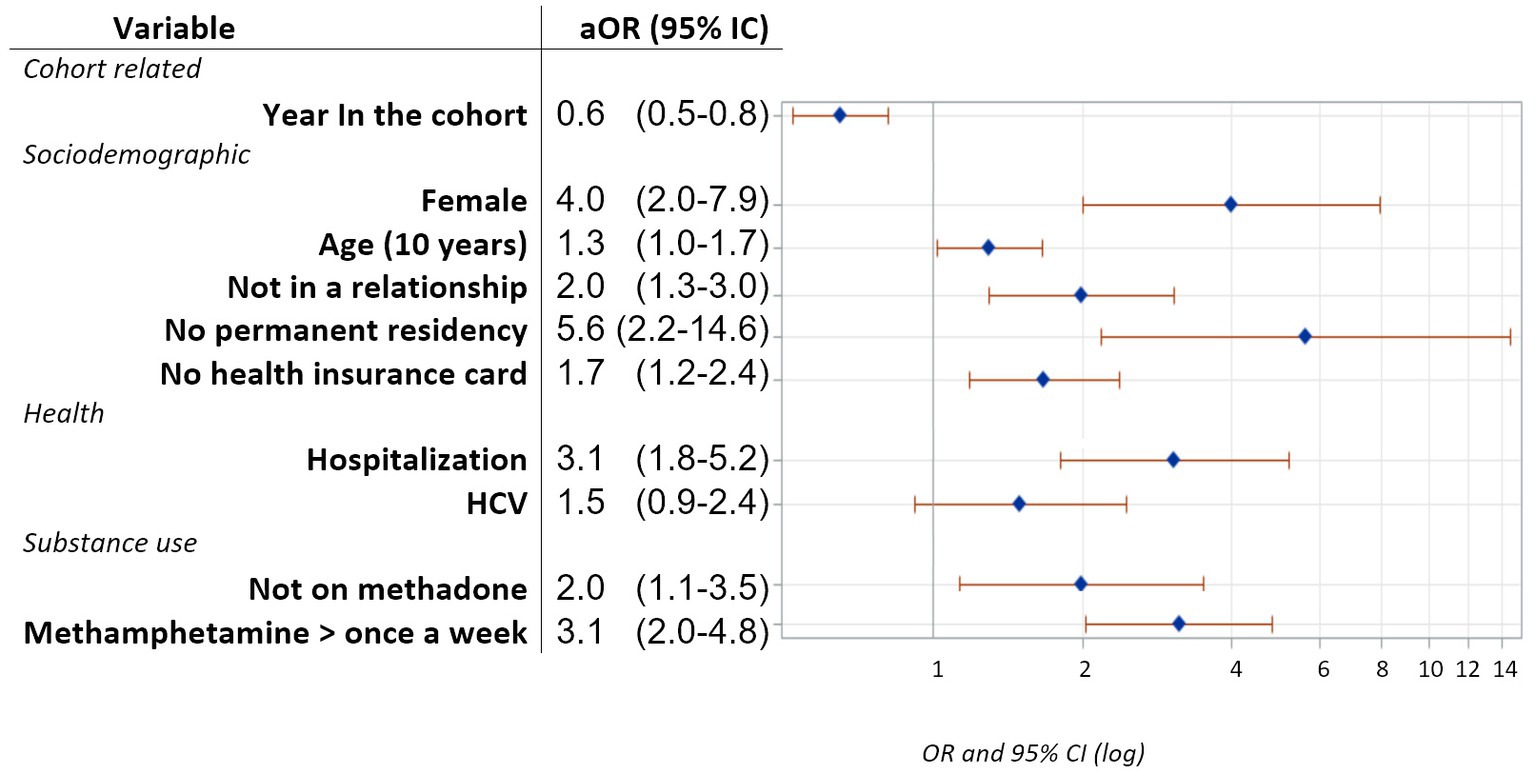
Figure 2. Adjusted odds ratios and their 95% confidence intervals for factors associated with depression obtained using a nonlinear mixed model with a cutoff CES-D8 score ⩾ 6 for people free from depression according to the PHQ-2 data at inclusion.
4. Discussion
4.1. Identifying PWID with a high depression risk
In this cohort of PWID recruited through RDS surveys, almost a quarter had depressive symptoms develop or reoccur during a follow-up of 16 months on average. This is more than previously found in a Canadian open cohort of PWID (39) but lower than in other PWID populations, whether in LMICs (40) or in high-income countries (41). This could be explained by the different methodologies (population selection, screening tools) used to measure the prevalence of depression. Furthermore, in Asian settings, the expressiveness of depressive symptoms has been shown to vary: depressive people from LMICs show fewer mood-related symptoms, which are what the CES-D8 mainly measures, and more somatic symptoms (42, 43).
The gender gap in depression has been extensively studied in the general population and could be attributed to various factors. Hormonal fluctuations (44, 45), differences in expressed genes and neural and cerebral circuitry architecture (44), personality traits (46, 47), societal factors such as the lower levels of education (48, 49), life stressors (50), and gender norms influencing answers of certain CES-D8 questions (51) could all be part of the explanation. Nevertheless, in this particular population of female PWID, the stigma associated with drug use could have a significant impact on depressive symptoms (52). This effect has been observed not only globally (53) but also in Vietnam, where female PWID experience higher levels of stigmatization, both from men and women (54), which may have concerning implications for their mental health (55).
Another potential explanation could be gender disparities in involvement in sex work. While we could not establish gender differences in sex work due to underreported or unanswered questions in this study, another article from the DRIVE project, focusing on a similar population, found that being a woman was linked to engagement in sex work (56), a known risk factor for depression (57). Although reaching sex workers is difficult (fear of stigma, desirability biases, conditions of life, night work, pimp control, etc.), psychological interventions, screening for mental health in health care services targeting female sex workers, and training “gatekeepers” to support women at risk, should be implemented (58). More generally, targeted prevention efforts should consider that women may be at a higher risk of depression and offer them dedicated interventions.
Other factors reflecting social precariousness emerged. “Living on the edge” without stable housing or a health insurance card has already been identified as a risk factor for mental illness (59). The concerns and anxiety this causes could exacerbate or trigger the onset of mental illness, acting as additional stress on a potentially compromised state of mental resilience already affected by substance use. Similarly, social support, as defined in our study as being in a relationship, was a protective factor for depression, probably because of both its social and its emotional support impacts (60, 61).
The prevalence of depression increases with age in both the general population and PWID (62, 63). This may be explained by age-related biological changes and comorbidities or chronic conditions, all of which are strongly associated with depression (64). As we did not have data about comorbidities, it is possible that age acted as a proxy of chronic health problems (65). The association found between depression and hospitalization during follow-up, probably reflecting the decompensation of somatic comorbidities, is consistent with this hypothesis.
Indeed, having been hospitalized during the follow-up increased the risk of depression. Despite the fact that we had no information on the causes of these hospital admissions, they might be related to complications or treatments of infections, which are frequent in our cohort population, as well as a degraded state of health, commonly associated with depression (12).
We found that HCV had a tendency to increase the risk of depression, although not significantly. In literature, this observed association (66) has been described as linked to poor health-related quality of life and physical, mental and social illnesses due to the disease (67), the treatments (68), and even direct HCV neuro-invasion, and metabolic derangements (69). Nevertheless, as new cost-effective direct-acting antivirals for HCV have recently been developed with lower psychiatric side effects (70–72), we can see how they will become widespread, including among LMICs, thus reducing the mental health burden of HCV.
Generally, we observed that time since inclusion was a protective factor. Our patients participated in a research program offering them the opportunities to be tested, examined and treated. Furthermore, the positive social impact of being enrolled in a cohort and going to regular meetings with CBO-trained members for social support, harm reduction and social and administrative counseling might have helped reduce the risk of depression. Being part of a community also offers, in the context of layered drug- and HIV-related stigma, the possibility to disclose their situation to someone (73).
4.2. Taking care of PWID with a high depression risk
In many countries, where access to psychiatric care is notably limited, alternative and original strategies that rely on nonprofessional or peer workers could be crucial. Using simple screening tools in the community to introduce drug users to their mental health may be the first step.
A simplified psychiatric screening tool adapted to nonprofessional/CBO members was developed as part of the DRIVE project. This 9-item questionnaire validated among PWID with acceptable psychometric characteristics and good acceptability (74, 75) allows a discussion of mental health, depression, psychiatric consequences of regular drug use and their treatment with trained CBO members, particularly for PWID with multiple risk factors. Depending on the score, a consultation with a psychiatrist in situ is proposed. Screening followed by delocalized psychiatric consultation is one of the innovative approaches that allows the care and monitoring of hard-to-reach vulnerable populations.
Psychiatric complications, particularly depression but also psychotic manifestations, are very common among frequent methamphetamine users and need special attention and tailored harm reduction interventions (76). Adapted information on drug use and the benefits of reducing should be provided by peers or social workers. For users who want to adapt their use, they should be given the means to change his or her behavior, thus limiting the risk of depression (77, 78).
Enrollment in MMT should be encouraged, since having the easiest possible access to MMT was found to be a protective factor (41, 79–81). Methadone-induced biological stabilization protected the patients from craving phases and allowed them personal and social stabilization (82, 83). Regular opioid use could even have a protective effect against psychiatric comorbidities (84). Indeed, this enables a decline in risk practices and the patient to be in touch with care professionals (85). Of course, the decision to initiate a patient in an MMT program should be made by a physician, following a thorough assessment of contraindications and in agreement with the patient. This decision should be preceded by informed consent, which includes a discussion of the risks and benefits of such a program, as well as alternative treatments, to enable the patient to make an informed decision.
It has become necessary to promote the development of psychiatric interventions in environments dedicated to drug users (methadone or HIV clinics) (78). In this aim, basic training on the association between mental health and addiction is required for all stakeholders, which implies acceptance of delocalized psychiatric interventions in specialized settings or CBO offices (86). Reducing the stigma associated with drug use and mental health disorders is urgent, and recognizing mutual competencies and roles of peers and healthcare workers is crucial (87).
4.3. Study limitations
First, owing to limitations in resources, staffing, and organizational capacity, we were unable to conduct psychiatric evaluations based on international criteria. The PHQ-2 used at baseline has a sensitivity of 72% (28), meaning that we did not exclude some people with clinical depression. Moreover, the questionnaire relates only to symptoms in the past 2 weeks, which could have biased our selection of people without depression. Although the presence and severity of depressive symptoms are known to vary over time, we did not evaluate history of depression. Furthermore, the semiannual assessment of depression involved a different screening tool with different psychometric properties, the CES-D. This questionnaire focus on symptoms in the last week, and we use a short 8-item version. However, this version has a correlation of 0.93 with the complete scale (30). Additionally, in another part of the DRIVE project (not shown here), psychiatric evaluation and the CES-D8 were found to have good agreement, indicating that as imperfect as this outcome was, it still served as a suitable proxy for depression assessment. The limitations of using different questionnaires in the study are well acknowledged by the investigators but provide insight into the evolution of depressive symptoms in a context of participant attrition. If these limitations were to introduce biases, they would likely be of minor magnitude and should not undermine the findings.
Second, we had to restrict our data to people with at least one follow-up visit; some were lost to follow-up, and we considered only visits with completed outcomes. This could induce some selection biases because it is plausible that people with high depression risk are the least able to visit, meaning that the more severe cases of depression were not as represented as others. We observed this phenomenon when we compared people with missed or excluded visits with the rest; the former presented more risk factors for depression.
Third, sampling biases could occur because our recruitment method included a large majority of male PWID. Our findings are representative of Vietnam and South Asia (88) but might not be extrapolated to populations of PWID with a lower proportion of males (approximately 75% around the world) (89). Similarly, our cohort overrepresented HIV-positive participants (approximately half), whereas the estimated prevalence of HIV among PWID is 30% in Hai Phong (24). In our analyzes, HIV status had no association with depression, which may seem surprising, as the link between depression and HIV status has been shown (90). In our cohort, however, we speculate that HIV-positive participants are less depressed because of greater support and free access to care offered by the DRIVE project.
Finally, avoided sensitive questions and missing data could be explained by desirability biases. For instance, questions about heroin experience and sex work were often not answered. Recall bias could also have occurred since questions were related to past behaviors.
5. Conclusion
The co-occurrence of addiction and depression is a scourge with catastrophic consequences for individuals affected by it. In this large longitudinal study focusing on people who inject drugs in a low-to-middle income country setting, we found a concerning high prevalence of depression.
This work was able for the first time in this setting to consider the temporal relationships of the factors studied and their impact on depressive symptomatology. We found that being a woman was strongly associated with depression. Certain factors of social precariousness were also identified as risk factors, as well as the consumption of methamphetamine in addition to substance injection. The beneficial effect of being on a MMT program was also emphasized.
All these results drive, in the context of limited psychiatric resources, the development of innovative interventions focusing on these vulnerable sub-populations, such as simple screening tools, delocalized psychiatric consultations, peer support, free treatment, etc.… Other interventions remain to be designed and tested in these specific settings.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Institutional Review Board of the Hai Phong University of Medicine and Pharmacy, the Institutional Review Board of the Icahn School of Medicine at Mount Sinai, and the Institutional Review Board of the New York University School of Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LiM: conceptualization, methodology, software, formal analysis, writing–original draft, and visualization. SL: investigation, validation, and writing–review and editing. VH: investigation and writing–review and editing. DH and DD: funding acquisition, supervision, and writing–review and editing. KM and J-PM: resources, supervision, and writing–review and editing. KO: funding acquisition and writing–review and editing. DR and CQ: resources, supervision, data curation, and writing–review and editing. TT: supervision and writing–review and editing. RV: data curation and writing–review and editing. GH: supervision, data curation, and writing–review and editing. DL and JF: writing–review and editing. LaM: supervision, conceptualization, methodology, and writing–review and editing. NN: funding acquisition, supervision, conceptualization, methodology, and writing–review and editing. All authors contributed to the article and approved the submitted version.
Funding
This work was cosupported by the French Agence Nationale de Recherches sur le SIDA et les hépatites virales (ANRS) [12299] and the US National Institute of Drug Abuse (NIDA) [P30DA011041].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1233844/full#supplementary-material
References
1. Rush, B, Urbanoski, K, Bassani, D, Castel, S, Wild, TC, Strike, C, et al. Prevalence of co-occurring substance use and other mental disorders in the Canadian population. Can J Psychiatr. (2008) 53:800–9. doi: 10.1177/070674370805301206
2. Compton, WM, Thomas, YF, Stinson, FS, and Grant, BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the National Epidemiologic Survey on alcohol and related conditions. Arch Gen Psychiatry. (2007) 64:566–76. doi: 10.1001/archpsyc.64.5.566
3. Conner, KR, Pinquart, M, and Duberstein, PR. Meta-analysis of depression and substance use and impairment among intravenous drug users (IDUs). Addiction. (2008) 103:524–34. doi: 10.1111/j.1360-0443.2007.02118.x
4. Kingston, REF, Marel, C, and Mills, KL. A systematic review of the prevalence of comorbid mental health disorders in people presenting for substance use treatment in Australia: comorbidity in substance use treatment. Drug Alcohol Rev. (2017) 36:527–39. doi: 10.1111/dar.12448
5. Schuckit, MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. (2006) 101:76–88. doi: 10.1111/j.1360-0443.2006.01592.x
6. Boumendjel, M, and Benyamina, A. Les «pathologies duelles» en addictologie: état des lieux et prise en charge In: M Reynaud, editor. Traité d’Addictologie. Cachan: Lavoisier (2016). 139–49.
7. Couteron, JP, Blaise, M, Julien, JP, Berne, E, Hans, C, Péquart, C, et al. Addictions et troubles psychiatriques. Fédération Addiction, p. 106. (2019). Available at: https://fr.calameo.com/read/0055448589de9b5897807.
8. Benyamina, A. Pathologie duelle, actualités et perspectives. Ann Méd Psychol Rev Psychiatr. (2018) 176:742–5. doi: 10.1016/j.amp.2018.08.016
9. Steger, MF, and Kashdan, TB. Depression and everyday social activity, belonging, and well-being. J Couns Psychol. (2009) 56:289–300. doi: 10.1037/a0015416
10. Harris, EC, and Barraclough, B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. (1997) 170:205–28. doi: 10.1192/bjp.170.3.205
11. Hutton, HE, Lyketsos, CG, Zenilman, JM, Thompson, RE, and Erbelding, EJ. Depression and HIV risk behaviors among patients in a sexually transmitted disease clinic. AJP. (2004) 161:912–4. doi: 10.1176/appi.ajp.161.5.912
12. Kang, HJ, Kim, SY, Bae, KY, Kim, SW, Shin, IS, Yoon, JS, et al. Comorbidity of depression with physical disorders: research and clinical implications. Chonnam Med J. (2015) 51:8–18. doi: 10.4068/cmj.2015.51.1.8
13. Levintow, SN, Pence, BW, Powers, KA, Sripaipan, T, Ha, TV, Chu, VA, et al. Estimating the effect of depression on HIV transmission risk behaviors among people who inject drugs in Vietnam: a causal approach. AIDS Behav. (2020) 25:438–46. doi: 10.1007/s10461-020-03007-9
14. Swartz, MS, Swanson, JW, Hannon, MJ, Bosworth, HS, Osher, FC, Essock, SM, et al. Regular sources of medical care among persons with severe mental illness at risk of hepatitis C infection. Psychiatr Serv. (2003) 54:854–9. doi: 10.1176/appi.ps.54.6.854
15. Ann Priester, M, Browne, T, Iachini, A, Clone, S, DeHart, D, and Seay, KD. Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: an integrative literature review. J Subst Abus Treat. (2016) 61:47–59. doi: 10.1016/j.jsat.2015.09.006
16. Hunt, GE, Malhi, GS, Lai, HMX, and Cleary, M. Prevalence of comorbid substance use in major depressive disorder in community and clinical settings, 1990–2019: systematic review and meta-analysis. J Affect Disord. (2020) 266:288–304. doi: 10.1016/j.jad.2020.01.141
17. Vuong, DA, Van Ginneken, E, Morris, J, Ha, ST, and Busse, R. Mental health in Vietnam: burden of disease and availability of services. Asian J Psychiatr. (2011) 4:65–70. doi: 10.1016/j.ajp.2011.01.005
18. Pham Minh, K, Vallo, R, Duong Thi, H, Khuat Thi Hai, O, Jarlais, DCD, Peries, M, et al. Psychiatric comorbidities among people who inject drugs in Hai Phong, Vietnam: the need for screening and innovative interventions. Biomed Res Int. (2018) 20:1–13. doi: 10.1155/2018/8346195
19. Shaw, SA, El-Bassel, N, Gilbert, L, Terlikbayeva, A, Hunt, T, Primbetova, S, et al. Depression among people who inject drugs and their intimate partners in Kazakhstan. Community Ment Health J. (2016) 52:1047–56. doi: 10.1007/s10597-015-9883-3
20. Iskandar, S, Kamal, R, and De Jong, CA. Psychiatric comorbidity in injecting drug users in Asia and Africa. Curr Opin Psychiatry. (2012) 25:213–8. doi: 10.1097/YCO.0b013e3283523d66
21. Barroga, EF, and Kojima, T. Research study designs: an appraisal for peer reviewers and science editors. Eur Sci Edit. (2013) 39:2.
23. Jarlais, DD, Huong, DT, Pham, MK, Oanh, KTH, Thanh, NTT, Arasteh, K, et al. Integrated respondent driven sampling and peer support for persons who inject drugs in Haiphong, Vietnam: a case study with implications for interventions. AIDS Care. (2016) 28:1312–5. doi: 10.1080/09540121.2016.1178698
24. Jarlais, DD, Khue, PM, Feelemyer, J, Arasteh, K, Huong, DT, Oanh, KTH, et al. Using dual capture/recapture studies to estimate the population size of persons who inject drugs (PWID) in the city of Hai Phong, Vietnam. Drug Alcohol Depend. (2018) 185:106–11. doi: 10.1016/j.drugalcdep.2017.11.033
25. Michel, L, Des Jarlais, DC, Thi, HD, Hai, OKT, Minh, KP, Peries, M, et al. Intravenous heroin use in Haiphong, Vietnam: need for comprehensive care including methamphetamine use-related interventions. Drug Alcohol Depend. (2017) 179:198–204. doi: 10.1016/j.drugalcdep.2017.07.004
26. Kroenke, K, Spitzer, RL, Williams, JBW, and Löwe, B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. (2009) 50:613–21. doi: 10.1176/appi.psy.50.6.613
27. Kroenke, K, Spitzer, RL, and Williams, JBW. The patient health Questionnaire-2: validity of a two-item depression screener. Med Care. (2003) 41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C
28. Levis, B, Sun, Y, He, C, Wu, Y, Krishnan, A, Bhandari, PM, et al. Accuracy of the PHQ-2 alone and in combination with the PHQ-9 for screening to detect major depression: systematic review and Meta-analysis. JAMA. (2020) 323:2290–300. doi: 10.1001/jama.2020.6504
29. Melchior, LA, Huba, GJ, Brown, VB, and Reback, CJ. A short depression index for women. Educ Psychol Meas. (1993) 53:1117–25. doi: 10.1177/0013164493053004024
30. Santor, DA, and Coyne, JC. Shortening the CES-D to improve its ability to detect cases of depression. Psychol Assess. (1997) 9:233–43. doi: 10.1037/1040-3590.9.3.233
31. Zauszniewski, JA, and Graham, GC. Comparison of short scales to measure depressive symptoms in elders with diabetes. West J Nurs Res. (2009) 31:219–34. doi: 10.1177/0193945908326065
32. Kroenke, K, Spitzer, RL, Williams, JBW, Monahan, PO, and Löwe, B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. (2007) 146:317–25. doi: 10.7326/0003-4819-146-5-200703060-00004
33. Duong, HT, Jarlais, DD, Khuat, OHT, Arasteh, K, Feelemyer, J, Khue, PM, et al. Risk behaviors for HIV and HCV infection among people who inject drugs in Hai Phong, Viet Nam, 2014. AIDS Behav. (2018) 22:2161–71. doi: 10.1007/s10461-017-1814-6
34. McKetin, R, McLaren, J, Lubman, DI, and Hides, L. The prevalence of psychotic symptoms among methamphetamine users. Addiction. (2006) 101:1473–8. doi: 10.1111/j.1360-0443.2006.01496.x
35. Dawson, DA, Smith, SM, Saha, TD, Rubinsky, AD, and Grant, BF. Comparative performance of the AUDIT-C in screening for DSM-IV and DSM-5 alcohol use disorders. Drug Alcohol Depend. (2012) 126:384–8. doi: 10.1016/j.drugalcdep.2012.05.029
36. Sterne, JAC, White, IR, Carlin, JB, Spratt, M, Royston, P, Kenward, MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. (2009) 338:b2393. doi: 10.1136/bmj.b2393
37. Littell, RC, Pendergast, J, and Natarajan, R. Modelling covariance structure in the analysis of repeated measures data. Stat Med. (2000) 19:1793–819. doi: 10.1002/1097-0258(20000715)19:13<1793::AID-SIM482>3.0.CO;2-Q
38. Liu, Y, and De, A. Multiple imputation by fully conditional specification for dealing with missing data in a large epidemiologic Study. Int J Stat Med Res. (2015) 4:287–95. doi: 10.6000/1929-6029.2015.04.03.7
39. Reddon, H, Pettes, T, Wood, E, Nosova, E, Milloy, MJ, Kerr, T, et al. Incidence and predictors of mental health disorder diagnoses among people who inject drugs in a Canadian setting. Drug Alcohol Rev. (2018) 37 Suppl 1:S285–93. doi: 10.1111/dar.12631
40. Gu, J, Lau, JTF, Chen, H, Chen, X, Liu, C, and Liu, J. Mental health and interpersonal factors associated with HIV-related risk behaviors among non-institutionalized female injection drug users who are also sex Workers in China. Women Health. (2010) 50:20–36. doi: 10.1080/03630241003601137
41. Maremmani, AGI, Rovai, L, Pani, PP, Pacini, M, Lamanna, F, Rugani, F, et al. Do methadone and buprenorphine have the same impact on psychopathological symptoms of heroin addicts? Ann General Psychiatry. (2011) 10:17. doi: 10.1186/1744-859X-10-17
42. Chee, KY, Tripathi, A, Avasthi, A, Chong, MY, Xiang, YT, Sim, K, et al. Country variations in depressive symptoms profile in Asian countries: findings of the research on Asia psychotropic prescription (REAP) studies: country variations in depressive profile. Asia Pac Psychiatry. (2015) 7:276–85. doi: 10.1111/appy.12170
43. Niemi, M, Målqvist, M, Giang, KB, Allebeck, P, and Falkenberg, T. A narrative review of factors influencing detection and treatment of depression in Vietnam. Int J Ment Health Syst. (2013) 7:15. doi: 10.1186/1752-4458-7-15
44. Albert, PR. Why is depression more prevalent in women? J Psychiatry Neurosci. (2015) 40:219–21. doi: 10.1503/jpn.150205
45. Cheslack-Postava, K, Keyes, KM, Lowe, SR, and Koenen, KC. Oral contraceptive use and psychiatric disorders in a nationally representative sample of women. Arch Womens Ment Health. (2015) 18:103–11. doi: 10.1007/s00737-014-0453-4
46. Goodwin, RD, and Gotlib, IH. Gender differences in depression: the role of personality factors. Psychiatry Res. (2004) 126:135–42. doi: 10.1016/j.psychres.2003.12.024
47. Jeronimus, BF, Riese, H, Sanderman, R, and Ormel, J. Mutual reinforcement between neuroticism and life experiences: a five-wave, 16-year study to test reciprocal causation. J Pers Soc Psychol. (2014) 107:751–64. doi: 10.1037/a0037009
48. Eugenia Alvarado, B, Victoria Zunzunegui, M, Béland, F, Sicotte, M, and Tellechea, L. Social and gender inequalities in depressive symptoms among urban older adults of Latin America and the Caribbean. J Gerontol B Psychol Sci Soc Sci. (2007) 62:S226–36. doi: 10.1093/geronb/62.4.S226
49. Miech, RA, Eaton, WW, and Brennan, K. Mental health disparities across education and sex: a prospective analysis examining how they persist over the life course. J Gerontol. (2005) 60:S93–8. doi: 10.1093/geronb/60.Special_Issue_2.S93
50. Keita, GP. Psychosocial and cultural contributions to depression in women: considerations for women midlife and beyond. JMCP. (2007) 13:12–5. doi: 10.18553/jmcp.2007.13.9-a.12
51. Carleton, RN, Thibodeau, MA, Teale, MJN, Welch, PG, Abrams, MP, Robinson, T, et al. The Center for Epidemiologic Studies Depression Scale: a review with a theoretical and empirical examination of item content and factor structure. PLoS One. (2013):e58067. doi: 10.1371/journal.pone.0058067
52. Khuat, OT, Morrow, M, Nguyen, TN, and Armstrong, G. Social context, diversity and risk among women who inject drugs in Vietnam: descriptive findings from a cross-sectional survey. Harm Reduct J. (2015) 12:35. doi: 10.1186/s12954-015-0067-9
53. Meyers, SA, Earnshaw, VA, D’Ambrosio, B, Courchesne, N, Werb, D, and Smith, LR. The intersection of gender and drug use-related stigma: a mixed methods systematic review and synthesis of the literature. Drug Alcohol Depend. (2021) 223:108706. doi: 10.1016/j.drugalcdep.2021.108706
54. Trang, NT, Jauffret-Roustide, M, Giang, LM, and Visier, L. “I’m not like others”: stigma navigation by people who inject drugs in Vietnam. Drugs. (2022) 29:85–94. doi: 10.1080/09687637.2021.1874875
55. Wang, DF, Zhou, YN, Liu, YH, Hao, YZ, Zhang, JH, Liu, TQ, et al. Social support and depressive symptoms: exploring stigma and self-efficacy in a moderated mediation model. BMC Psychiatry. (2022) 22:117. doi: 10.1186/s12888-022-03740-6
56. Giang, HT, Duc, NQ, Khue, PM, Quillet, C, Oanh, KTH, Thanh, NTT, et al. Gender differences in HIV, HCV risk and prevention needs among people who inject drug in Vietnam. AIDS Behav. (2023) 27:1989–97. doi: 10.1007/s10461-022-03932-x
57. Rael, CT, and Davis, A. Depression and key associated factors in female sex workers and women living with HIV/AIDS in the Dominican Republic. Int J STD AIDS. (2017) 28:433–40. doi: 10.1177/0956462416651374
58. Beattie, TS, Smilenova, B, Krishnaratne, S, and Mazzuca, A. Mental health problems among female sex workers in low- and middle-income countries: a systematic review and meta-analysis. PLoS Med. (2020) 17:e1003297. doi: 10.1371/journal.pmed.1003297
59. McKee, M, Reeves, A, Clair, A, and Stuckler, D. Living on the edge: precariousness and why it matters for health. Arch Public Health. (2017) 75:13. doi: 10.1186/s13690-017-0183-y
60. Gordillo, V, Fekete, EM, Platteau, T, Antoni, MH, Schneiderman, N, Nöstlinger, C, et al. Emotional support and gender in people living with HIV: effects on psychological well-being. J Behav Med. (2009) 32:523–31. doi: 10.1007/s10865-009-9222-7
61. Wang, X, Cai, L, Qian, J, and Peng, J. Social support moderates stress effects on depression. Int J Ment Health Syst. (2014) 8:41. doi: 10.1186/1752-4458-8-41
62. Kessler, RC, Birnbaum, H, Bromet, E, Hwang, I, Sampson, N, and Shahly, V. Age differences in major depression: results from the National Comorbidity Surveys Replication (NCS-R). Psychol Med. (2010) 40:225–37. doi: 10.1017/S0033291709990213
63. Li, Y, Hershow, R, Irwanto, I, Praptoraharjo, I, Setiawan, M, and Levy, J. Factors associated with symptoms of depression among injection drug users receiving antiretroviral treatment in Indonesia. J AIDS Clin Res. (2014) 5:303. doi: 10.4172/2155-6113.1000303
64. Fiske, A, Wetherell, JL, and Gatz, M. Depression in older adults. Annu Rev Clin Psychol. (2009) 5:363–89. doi: 10.1146/annurev.clinpsy.032408.153621
65. Roberts, RE, Kaplan, GA, Shema, SJ, and Strawbridge, WJ. Prevalence and correlates of depression in an aging cohort: the Alameda County Study. J Gerontol B Psychol Sci Soc Sci. (1997) 52B:S252–8. doi: 10.1093/geronb/52B.5.S252
66. Younossi, Z, Park, H, Henry, L, Adeyemi, A, and Stepanova, M. Extrahepatic manifestations of hepatitis C: a Meta-analysis of prevalence, quality of life, and economic burden. Gastroenterology. (2016) 150:1599–608. doi: 10.1053/j.gastro.2016.02.039
67. Modabbernia, A, Poustchi, H, and Malekzadeh, R. Neuropsychiatric and psychosocial issues of patients with Hepatitis C infection: a selective literature review. Hepat Mon. (2013) 13:e8340. doi: 10.5812/hepatmon.8340
68. Davoodi, L, Masoum, B, Moosazadeh, M, Jafarpour, H, Haghshenas, MR, and Mousavi, T. Psychiatric side effects of pegylated interferon-α and ribavirin therapy in Iranian patients with chronic hepatitis C: a meta-analysis. Exp Ther Med. (2018) 16:971–8. doi: 10.3892/etm.2018.6255
69. Yarlott, L, Heald, E, and Forton, D. Hepatitis C virus infection, and neurological and psychiatric disorders – a review. J Adv Res. (2017) 8:139–48. doi: 10.1016/j.jare.2016.09.005
70. Due, OT, Thakkinstian, A, Thavorncharoensap, M, Sobhonslidsuk, A, Wu, O, Phuong, NK, et al. Cost-utility analysis of direct-acting antivirals for treatment of chronic hepatitis C genotype 1 and 6 in Vietnam. Value Health. (2020) 23:1180–90. doi: 10.1016/j.jval.2020.03.018
71. Pockros, PJ. New direct-acting antivirals in the development for hepatitis C virus infection. Ther Adv Gastroenterol. (2010) 3:191–202. doi: 10.1177/1756283X10363055
72. Sundberg, I, Lannergård, A, Ramklint, M, and Cunningham, JL. Direct-acting antiviral treatment in real world patients with hepatitis C not associated with psychiatric side effects: a prospective observational study. BMC Psychiatry. (2018) 18:157. doi: 10.1186/s12888-018-1735-6
73. Rudolph, AE, Davis, WW, Quan, VM, Ha, TV, Minh, NL, Gregowski, A, et al. Perceptions of community- and family-level injection drug user (IDU)- and HIV-related stigma, disclosure decisions and experiences with layered stigma among HIV-positive IDUs in Vietnam. AIDS Care. (2012) 24:239–44. doi: 10.1080/09540121.2011.596517
74. Le, SM, Trouiller, P, Duong, TH, Khuat, THO, Pham, MK, Vallo, R, et al. Development and assessment of a community-based screening tool for mental health disorders among people who inject drugs. Drug Alcohol Rev. (2022) 41:697–705. doi: 10.1111/dar.13402
75. Michel, L. Screening for mental health disorders in the community (DRIVE project): Validation of a quick screening tool (QST) among people who inject drugs with community-based organizations (CBO). (2019). Available at: hri.global/abstracts/abstracthr19/719/print.
76. Glasner-Edwards, S, Marinelli-Casey, P, Hillhouse, M, Ang, A, Mooney, LJ, and Rawson, R. Depression among methamphetamine users. J Nerv Ment Dis. (2009) 197:225–31. doi: 10.1097/NMD.0b013e31819db6fe
77. Parkes, T, Matheson, C, Carver, H, Budd, J, Liddell, D, Wallace, J, et al. Supporting harm reduction through peer support (SHARPS): testing the feasibility and acceptability of a peer-delivered, relational intervention for people with problem substance use who are homeless, to improve health outcomes, quality of life and social functioning and reduce harms: study protocol. Pilot Feasibility Stud. (2019) 5:64. doi: 10.1186/s40814-019-0447-0
78. Pinkham, S, and Stone, K. A global review of the harm reduction response to amphetamines: A 2015 update. London: Harm Reduction International (2015).
79. Teesson, M, Ross, J, Darke, S, Lynskey, M, Ali, R, Ritter, A, et al. One year outcomes for heroin dependence: findings from the Australian treatment outcome Study (ATOS). Drug Alcohol Depend. (2006) 83:174–80. doi: 10.1016/j.drugalcdep.2005.11.009
80. Xiao, L, Wu, Z, Luo, W, and Wei, X. Quality of life of outpatients in methadone maintenance treatment clinics. J Acquir Immune Defic Syndr. (2010) 53:S116–20. doi: 10.1097/QAI.0b013e3181c7dfb5
81. Yin, W, Pang, L, Cao, X, McGoogan, JM, Liu, M, Zhang, C, et al. Factors associated with depression and anxiety among patients attending community-based methadone maintenance treatment in China. Addiction. (2015) 110:51–60. doi: 10.1111/add.12780
82. Sun, HM, Li, XY, Chow, EPF, Li, T, Xian, Y, Lu, YH, et al. Methadone maintenance treatment programme reduces criminal activity and improves social well-being of drug users in China: a systematic review and meta-analysis. BMJ Open. (2015) 5:e005997. doi: 10.1136/bmjopen-2014-005997
83. Wang, Y, Wang, H, Li, W, Zhu, J, Gold, MS, Zhang, D, et al. Reduced responses to heroin-cue-induced craving in the dorsal striatum: effects of long-term methadone maintenance treatment. Neurosci Lett. (2014) 581:120–4. doi: 10.1016/j.neulet.2014.08.026
84. Le, SM, Trouiller, P, Duong Thi, H, Khuat Thi Hai, O, Pham Minh, K, Vallo, R, et al. Daily heroin injection and psychiatric disorders: a cross-sectional survey among people who inject drugs (PWID) in Haiphong, Vietnam. Drug Alcohol Depend. (2020) 216:108334. doi: 10.1016/j.drugalcdep.2020.108334
85. Woody, G, Bruce, D, Korthuis, PT, Chhatre, S, Hillhouse, M, Jacobs, P, et al. HIV risk reduction with buprenorphine-naloxone or methadone: findings from a randomized trial. J Acquir Immune Defic Syndr. (2014) 66:288–93. doi: 10.1097/QAI.0000000000000165
86. Castillo, EG, Ijadi-Maghsoodi, R, Shadravan, S, Moore, E, Mensah, MO, Docherty, M, et al. Community interventions to promote mental health and social equity. Curr Psychiatry Rep. (2019) 21:35. doi: 10.1007/s11920-019-1017-0
87. Livingston, JD, Milne, T, Fang, ML, and Amari, E. The effectiveness of interventions for reducing stigma related to substance use disorders: a systematic review. Addiction. (2012) 107:39–50. doi: 10.1111/j.1360-0443.2011.03601.x
88. Nguyen, VT, and Scannapieco, M. Drug abuse in Vietnam: a critical review of the literature and implications for future research. Addiction. (2008) 103:535–43. doi: 10.1111/j.1360-0443.2007.02122.x
89. Degenhardt, L, Peacock, A, Colledge, S, Leung, J, Grebely, J, Vickerman, P, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. (2017) 5:e1192–207. doi: 10.1016/S2214-109X(17)30375-3
Keywords: mental health, mood disorder, substance abuse, Vietnam, PWID, depression, prevention, dual diagnosis
Citation: Moulis L, Le SM, Hai VV, Huong DT, Minh KP, Oanh KTH, Rapoud D, Quillet C, Thi TTN, Vallo R, Hoang GT, Moles J-P, Laureillard D, Feelemyer J, Des Jarlais DC, Michel L, Nagot N and the DRIVE Study Team (2023) Gender, homelessness, hospitalization and methamphetamine use fuel depression among people who inject drugs: implications for innovative prevention and care strategies. Front. Psychiatry. 14:1233844. doi: 10.3389/fpsyt.2023.1233844
Edited by:
Kunhua Lee, National Tsing Hua University, TaiwanReviewed by:
Maurizio Coppola, Department of Addiction ASLCN1, ItalyLaura Roe, University of St, Andrews, United Kingdom
Copyright © 2023 Moulis, Le, Hai, Huong, Minh, Oanh, Rapoud, Quillet, Thi, Vallo, Hoang, Moles, Laureillard, Feelemyer, Des Jarlais, Michel, Nagot and the DRIVE Study Team. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lionel Moulis, bC1tb3VsaXNAY2h1LW1vbnRwZWxsaWVyLmZy
 Lionel Moulis
Lionel Moulis Sao Mai Le
Sao Mai Le Vinh Vu Hai3
Vinh Vu Hai3 Duong Thi Huong
Duong Thi Huong Delphine Rapoud
Delphine Rapoud Giang Thi Hoang
Giang Thi Hoang Jean-Pierre Moles
Jean-Pierre Moles Didier Laureillard
Didier Laureillard Jonathan Feelemyer
Jonathan Feelemyer Don C. Des Jarlais
Don C. Des Jarlais Nicolas Nagot
Nicolas Nagot the DRIVE Study Team
the DRIVE Study Team