Abstract
Background:
Women’s health is an important issue worldwide, and as the population is aging, the health of middle-aged and older women is becoming increasingly vital. Although many studies have examined the relationship between cognition and depression, few studies have been conducted specifically with middle-aged and older women. This study used a longitudinal approach to examine the bidirectional relationship between cognition and depression in middle-aged and older women.
Methods:
The study used three waves (2011, 2015, and 2020) of data from the China Health and Retirement Longitudinal Study (CHARLS), enrolling a total of 4,618 middle-aged and older women aged over 45 years. Participants’ general demographic characteristics were analyzed descriptively, and changes in study variables were measured using repeated-measures analysis of variance. Generalized estimating equation (GEE) and cross-lagged models were used to investigate the longitudinal relationship between depression and cognition.
Results:
The results of the GEE and cross-lagged models revealed that previous cognitive problems lead to future depression and prior depressive conditions affect subsequent cognition.
Conclusions:
There is a bidirectional relationship between depression and cognition in middle-aged and older women over time. More clinical mechanisms need to be explored in the future.
1 Introduction
The process of population aging in China is progressing rapidly, and the situation is becoming increasingly severe (1). According to data from the Seventh National Population Census of China, approximately 300 million women aged over 45 account for 20% of the total population (2). Studies reveal that elderly Chinese women are more likely to experience poorer health outcomes compared to their male counterparts (3, 4). Furthermore, the prevalence of adverse health conditions shows an age-related increase among women. Although women across all age groups face various health challenges, middle-aged and elderly women appear to be particularly vulnerable (5, 6).
Depressive disorder is a psychiatric condition characterized by persistent low mood and/or diminished interest in daily activities. Epidemiological studies demonstrate a 50% higher prevalence rate in women compared to men (7). Notably, Yue’s national survey (8) reveals that 22.3% of Chinese middle-aged and elderly women exhibit clinically significant depressive symptoms, with particularly elevated rates observed in rural populations (25.7%) and specific female subgroups (27.9%). Postmenopausal estrogen depletion has been identified as a significant biological risk factor for depression onset in perimenopausal women (9). In older populations, depression predominantly manifests through interacting pathways including multimorbidity patterns, chronic pain syndromes, social isolation, and adverse life experiences (10, 11).
Cognitive impairment is characterized by neurodegenerative changes affecting memory and executive function (12). Impaired cognitive function is a common complaint among older women seeking care in mental health and medical facilities (13). Epidemiological data from China indicate dementia prevalence rates of approximately 10% in the elderly population, with mild cognitive impairment affecting 20%–30% of this demographic (14, 15). Notably, a longitudinal cohort study in Jamaica identified female gender and advanced age as independent risk factors for dementia progression (16).
Several studies have explored the relationship between depression and cognition. Lyu’s study demonstrated a significant correlation between depression and cognitive impairment in both sexes (17). Cross-sectional analyses showed that women and low cognitive levels were related to higher depression (18). It is even noted that in humans, women are more at risk of experiencing greater cognitive decline in Alzheimer’s disease and depression (19). Estrogen changes in menopausal women may damage neurons that regulate emotions and cognition (20). Epidemiological and clinical evidence indicates that emotion and cognition in older adults are clinically interrelated, and common neurobiological mechanisms may underlie both groups of diseases (21).
In summary, given the importance of depression and cognition in human health development, several studies have explored their relationship. However, existing research has primarily focused on population-wide or maternal populations, with limited attention to middle-aged and older women. Additionally, most studies have adopted a unidirectional approach, rarely exploring bidirectional relationships. To address these gaps, this study employs longitudinal analyses to investigate the bidirectional relationship between depression and cognition among middle-aged and older women.
2 Methods
2.1 Study population
The data for this study came from the China Health and Retirement Longitudinal Study (CHARLS). CHARLS is a tracking survey that is representative of mainland China’s population aged 45 years and older. Its national baseline survey was conducted in 2011, and four rounds of tracking surveys with routine questionnaires were conducted in 2013, 2015, 2018, and 2020, respectively (22).
The CHARLS baseline survey used a multi-stage (county/district-village/residence-household) PPS (probability proportional to size sampling) random sampling method. In the first stage, all counties and districts in the country, except Tibet, were ranked by urban–rural attributes and GDP (gross domestic product) per capita within each of the eight regions, and then 150 counties or districts were selected with a probability proportional to population size. In the second stage, within each sampled county, three secondary sampling units (villages or communities) are randomly selected with a probability proportional to population size. Thus, CHARLS is nationally as well as regionally representative. After the sampling process described above, the baseline sample for CHARLS was distributed among 450 villages and neighborhoods in 28 provinces and 150 districts and counties across the country (23).
This study used the CHARLS baseline (2011), third round (2015), and fifth round (2020) data; participants over 45 were defined as middle-aged and older women. A sample size of 4,618 women were included in this study. The inclusion and exclusion criteria for the sample were as follows: (1) There were 9,221 female participants at baseline, 1,751 participants failed to follow-up in the 2015 survey, and 1,069 participants failed to follow-up in the 2020 survey; (2) a total of 753 participants with memory-related diseases (e.g., Alzheimer’s disease, cerebral atrophy, and Parkinson’s disease) and proxy response were excluded; (3) a total of 403 participants with missing data on depression and cognition modules were removed; (4) a total of 627 participants under 45 years at baseline were likewise excluded. The specific sample selection process is shown in Figure 1.
Figure 1
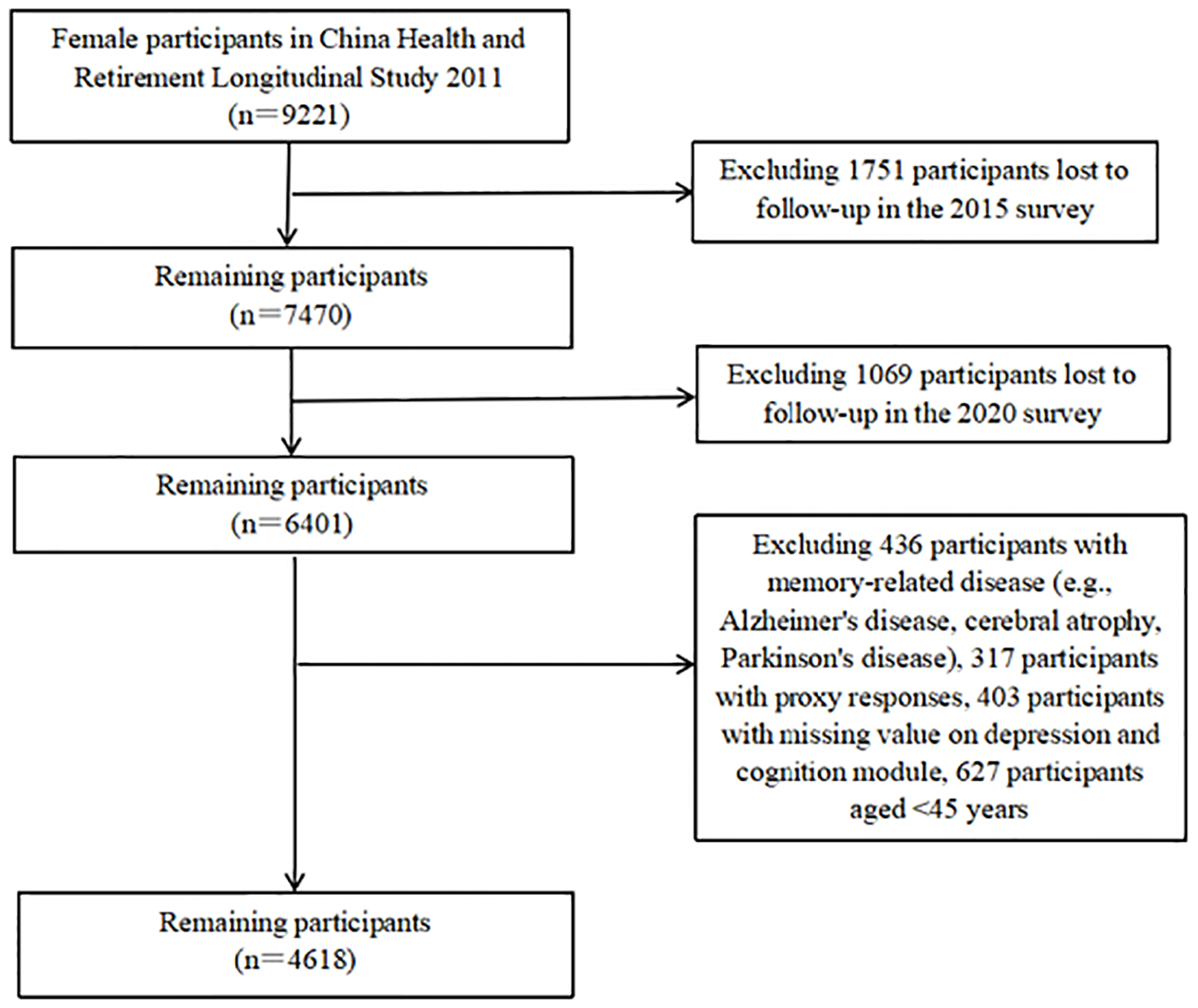
Sample selection process in this study.
2.2 Measurements
In this study, socio-demographic information includes age and education, among others. Depression was measured using the 10-item Centre for Epidemiological Studies, Depression Scale (CES-D-10). Cognition was assessed by orientation and attention, word recall, and visuospatial abilities.
2.2.1 Demographic characteristics
General demographic information included age, marital status (married with spouse present, married but not living with spouse temporarily, separated or divorced, widowed, and never married), education (no formal education, primary or incomplete primary education, secondary school, college, and above), residence (city or town, village), self-assessed health (very good, good, fair, poor, and very poor), and self-assessed memory (excellent, very good, good, fair, and poor).
2.2.2 Depression
The CES-D was developed in 1977 by Radloff at the National Institute of Mental Health in the United States (24). The scale is widely used in epidemiological surveys to screen out subjects with depressive symptoms for further examination and diagnosis. The CES-D-10 is a short version of the scale, which has been validated in Chinese middle-aged and older adults with good reliability and validity (25). There are 10 items in the CES-D-10, with each item ranging from 0 (little) to 3 (most of the time). The total score ranges from 0 to 30, ≥10 suggests a risk of depressive symptoms, and higher scores indicate more severe depressive symptoms (26).
2.2.3 Cognition
Cognition was assessed by orientation and attention, word recall, and visuospatial abilities. First, participants were assessed for orientation and attention by asking for the year (one point), month (one point), day (one point), day of the week (one point), and current season (one point), then asked to subtract 7 (up to five times) from 100 consecutively (five points). Each correct answer scores 1 point, and the total score for these two sections is 10 points. Second, the respondents were able to immediately repeat the 10 Chinese nouns that had just been read to them (immediate recall was 10 points) and recall the same list of words a few minutes later (delayed recall was 10 points). The total mean score for both parts was 10. It is generally accepted that the average score of immediate recall and delayed recall is an episodic memory measure. Finally, visuospatial ability was tested by reproducing two pictures of overlapping pentagons, with participants scoring one point if they were successful in drawing it (one point). Cognitive ability scores ranged from 0 to 21; participants with higher scores were considered to have better cognitive functioning (Yurun Du et al., 2023; Yushan Du et al., 2023; Yang et al., 2020).
2.3 Statistical analysis
Descriptive analyses were used to demonstrate demographic characteristics at baseline, and percentages were used for qualitative variables. Repeated-measures analysis of variance (RM-ANOVA) was used to compare depression and cognition in 2011, 2015, and 2020. Longitudinal analyses use generalized estimating equation (GEE), including demographic variables. GEE has a wider application, especially for analyses of longitudinal data. It considers intra-individual correlations, focuses on estimating the average effect at the aggregate level, and does not make hypothetical estimates, making inferences about conclusions more reliable (27). The cross-lagged model is mainly applied to estimate the intertemporal effects of two or more variables at multiple points in time. It includes auto-regression effects and cross-lagged effects (28). To assess the fit of the model, we used the following indicators: (1) χ2/degree of freedom (df), (2) root mean square error of approximation (RMSEA), and (3) comparative fit index (CFI) (29). A significance level of 5% was used for all statistical tests. IBM SPSS Statistics, version 26.0 (IBM Corp., Armonk, NY, USA) and AMOS 24 were used to carry out the statistical analyses.
2.4 Ethics approval and consent to participate
Ethics approval for the study was granted by the Ethical Review Committee of Peking University. The IRB approval number is IRB00001052-11015. Informed consent was obtained at the time of participation. All methods of this study were performed in accordance with the relevant guidelines and regulations. All experimental protocols were approved by the Institutional Review Board at Peking University.
3 Results
This study included a total of 4,618 Chinese middle-aged and elderly women. Baseline characteristics of the participants are summarized in Table 1. Participants had a mean age of 57.8 ± 7.76 years. At baseline, 87.6% of participants were married, and 77.5% had a primary school education or below. Most participants lived in villages (70.2%). Approximately half of the participants rated their health as fair (53.2%), while 44.6% reported their memory as fair.
Table 1
| Variables | 2011 (n = 4,618) n (%) |
|---|---|
| Age, mean ± SD | 57.80 ± 7.76 |
| Marital status | |
| Married with spouse present | 3,797 (82.2) |
| Married but not living with spouse temporarily for reasons such as work | 250 (5.4) |
| Separated or divorced | 39 (0.8) |
| Widowed | 526 (11.4) |
| Never married | 6 (0.2) |
| Educational level | |
| No formal education | 1,866 (40.4) |
| Primary or incomplete primary education | 1,713 (37.1) |
| Secondary school | 962 (20.8) |
| College and above | 77 (1.7) |
| Residence | |
| City or town | 1,374 (29.8) |
| Village | 3,244 (70.2) |
| Self-assessed health | |
| Very good | 257 (5.6) |
| Good | 740 (16.0) |
| Fair | 2,457 (53.2) |
| Poor | 1,001 (21.7) |
| Very poor | 163 (3.5) |
| Self-assessed memory | |
| Excellent | 11 (0.2) |
| Very good | 195 (4.2) |
| Good | 519 (11.2) |
| Fair | 2,053 (44.6) |
| Poor | 1,840 (39.8) |
General demographic characteristics of participants in baseline.
Table 2 demonstrates the changes in depression and cognition. The mean for depression in 2011 was 9.18 (SD = 6.50), that for 2015 was 9.16 (SD = 6.63), and that for 2020 was 10.17 (SD = 6.71). The mean for cognition in 2011 was 9.60 (SD = 4.30), that for 2015 was 9.21 (SD = 4.49), and that for 2020 was 9.88 (SD = 4.94). Groups were significantly different based on post-hoc tests. The changing profile of depression and cognition remained relatively stable.
Table 2
| Variables | Depression (CES-D) | Cognition |
|---|---|---|
| Repeated-measures analysis of variance (RM-ANOVA) | ||
| 2011 (mean ± SD) | 9.18 ± 6.50 | 9.60 ± 4.30 |
| 2015 (mean ± SD) | 9.16 ± 6.63 | 9.21 ± 4.49 |
| 2020 (mean ± SD) | 10.17 ± 6.71 | 9.88 ± 4.94 |
| F | 64.817 | 73.797 |
| P | <0.001 | <0.001 |
| Post-hoc analysis (Depression) | ||
| 2011–2015 (p) | 0.856 | |
| 2011–2020 (p) | <0.001 | |
| 2015–2020 (p) | <0.001 | |
| Post-hoc analysis (Cognition) | ||
| 2011–2015 (p) | <0.001 | |
| 2011–2020 (p) | <0.001 | |
| 2015–2020 (p) | <0.001 | |
Depression and cognition in 2011, 2015, and 2020.
Table 3 illustrates the findings of the GEE analysis, with depression established as the dependent variable. The results demonstrate that age, marital status, education, residence, self-assessed health, self-assessed memory, and cognition are significantly associated with depression. Participants who were middle-aged and widowed, had no formal education, lived in a city or town, and had poorer self-assessed health and memory were more depressed. Cognition and depression were significantly correlated (β = −0.197, p < 0.001). over time, participants with poorer cognitive status became more depressed.
Table 3
| Variables | β | SE | 95% CI | p |
|---|---|---|---|---|
| Age | −0.032 | 1.284 | 5.834 to 10.865 | 0.002 |
| Marital status | ||||
| Married with spouse present | 1.0 | |||
| Married but not living with spouse temporarily for reasons such as work | 0.213 | 0.324 | −0.422 to 0.847 | 0.511 |
| Separated or divorced | 1.784 | 0.928 | −0.035 to 3.602 | 0.055 |
| Widowed | 1.038 | 0.230 | 0.587 to 1.489 | <0.001 |
| Never married | 1.905 | 1.147 | −0.342 to 4.152 | 0.097 |
| Educational level | ||||
| No formal education | 1.0 | |||
| Primary or incomplete primary education | 0.276 | 0.170 | −0.057 to 0.610 | 0.105 |
| Secondary school | −0.202 | 0.221 | −0.635 to 0.231 | 0.361 |
| College and above | −1.037 | 0.449 | −1.917 to −0.157 | 0.021 |
| Residence | ||||
| City or town | 1.0 | |||
| Village | 0.654 | 0.158 | 0.345 to 0.963 | <0.001 |
| Self-assessed health | ||||
| Very good | 1.0 | |||
| Good | 0.842 | 0.292 | 0.270 to 1.415 | 0.004 |
| Fair | 2.365 | 0.270 | 1.836 to 2.894 | <0.001 |
| Poor | 4.905 | 0.309 | 4.300 to 5.510 | <0.001 |
| Very poor | 7.211 | 0.494 | 6.243 to 8.180 | <0.001 |
| Self-assessed memory | ||||
| Excellent | 1.0 | |||
| Very good | 0.082 | 1.153 | −2.178 to 2.342 | 0.943 |
| Good | 0.274 | 1.139 | −1.959 to 2.507 | 0.810 |
| Fair | 1.007 | 1.130 | −1.207 to 3.222 | 0.373 |
| Poor | 2.569 | 1.135 | 0.345 to 4.794 | 0.024 |
| Cognition | −0.197 | 0.017 | −0.230 to −0.163 | <0.001 |
GEE results of cognition and depression (dependent variable: depression).
Table 4 presents the results of the GEE with cognition as the dependent variable. Age, marital status, education, residence, self-assessed health, and depression are significantly correlated. Cognitive functioning was worse among participants who were older, widowed, or unmarried, had no formal education, lived in a village, and had poorer self-assessed health. Depression and cognition were significantly correlated (β = −0.068, p < 0.001). Over time, more depressed participants had poorer cognitive functioning.
Table 4
| Variables | β | SE | 95% CI | p |
|---|---|---|---|---|
| Age | −0.076 | 0.006 | −0.088 to −0.065 | <0.001 |
| Marital status | ||||
| Married with spouse present | 1.0 | |||
| Married but not living with spouse temporarily for reasons such as work | −0.349 | 0.188 | −0.717 to 0.019 | 0.063 |
| Separated or divorced | −0.392 | 0.389 | −1.153 to 0.370 | 0.313 |
| Widowed | −0.370 | 0.137 | −0.639 to −0.101 | 0.007 |
| Never married | −1.781 | 0.741 | −3.234 to −0.328 | 0.016 |
| Educational level | ||||
| No formal education | 1.0 | |||
| Primary or incomplete primary education | 3.301 | 0.101 | 3.102 to 3.499 | <0.001 |
| Secondary school | 5.238 | 0.120 | 5.003 to 5.473 | <0.001 |
| College and above | 6.607 | 0.245 | 6.126 to 7.088 | <0.001 |
| Residence | ||||
| City or town | 1.0 | |||
| Village | −1.081 | 0.095 | −1.267 to −0.895 | <0.001 |
| Self-assessed health | ||||
| Very good | 1.0 | |||
| Good | −0.296 | 0.196 | −0.681 to 0.089 | 0.132 |
| Fair | −0.441 | 0.178 | −0.789 to −0.093 | 0.013 |
| Poor | −0.430 | 0.196 | −0.814 to −0.047 | 0.028 |
| Very poor | −0.687 | 0.299 | −1.272 to −0.102 | 0.021 |
| Self-assessed memory | ||||
| Excellent | 1.0 | |||
| Very good | 1.189 | 1.060 | −0.889 to 3.266 | 0.262 |
| Good | 1.139 | 1.051 | −0.922 to 3.199 | 0.279 |
| Fair | 1.103 | 1.047 | −0.949 to 3.156 | 0.292 |
| Poor | 0.010 | 1.049 | −2.046 to 2.066 | 0.992 |
| Depression | −0.068 | 0.006 | −0.079 to −0.056 | <0.001 |
GEE results of cognition and depression (dependent variable: cognition).
Figure 2 displays the results of the cross-lagged model. Cross-lagged regression showed that depression in 2011 had a significant effect on cognition in 2015 (β = −0.03, p < 0.05) and depression in 2015 had a significant effect on cognition in 2020 (β = −0.03, p < 0.05). Cognition in 2011 had a significant effect on depression in 2015 (β = 0.02, p < 0.01) and cognition in 2015 had a significant effect on depression in 2020 (β = −0.06, p < 0.001). Auto-regression effects in depression were significant (2011 to 2015: β = 0.70, p < 0.001; 2015 to 2020: β = 0.60, p < 0.001). Auto-regression effects in cognition were significant (2011 to 2015: β = 0.65, p < 0.001; 2015 to 2020: β = 0.71, p < 0.001). The fit metrics for this model were as follows: χ2/df >5, RMSEA = 0.10, and CFI = 0.80; the χ2/df is large due to the sample size, but the model is generally acceptable (30).
Figure 2
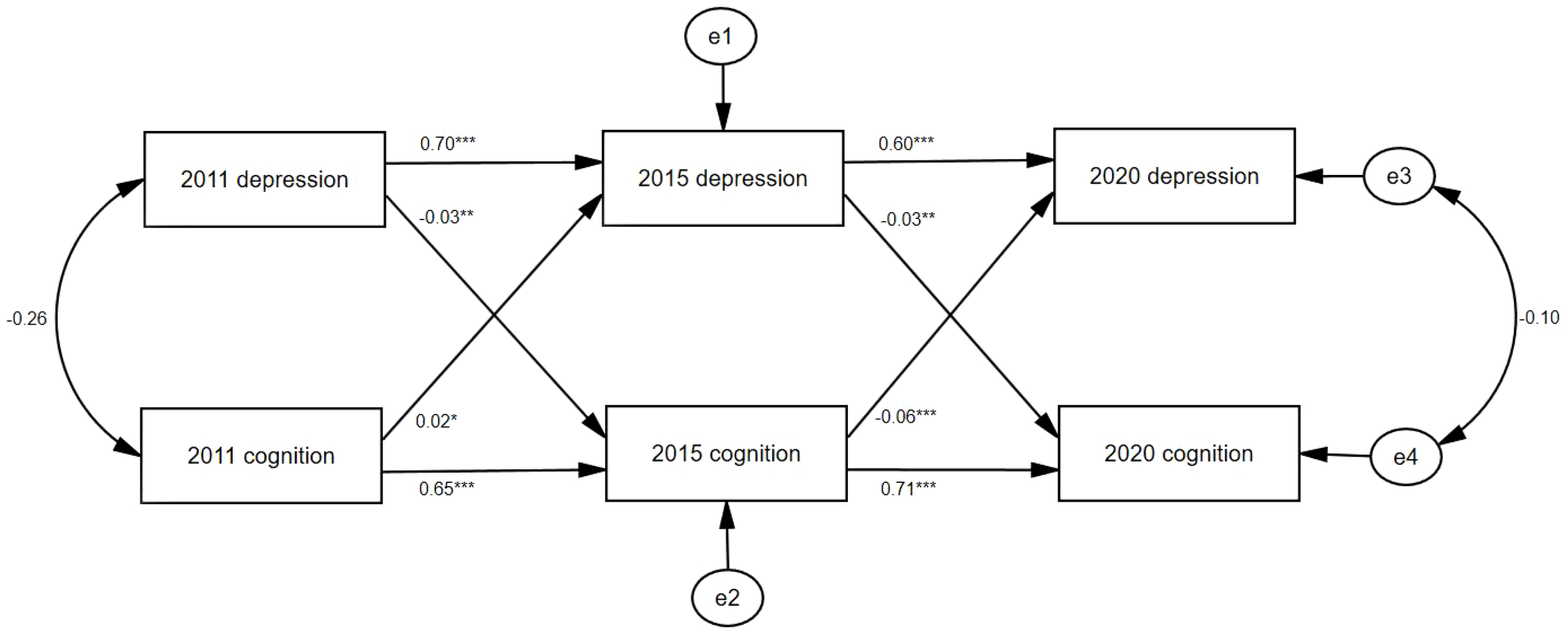
Cross-lagged model of depression and cognition. e1, e2, e3, and e4: potential errors; *p < 0.05, **p < 0.01, ***p < 0.001.
4 Discussion
This study is one of the few that examine the bidirectional relationship between depression and cognition in Chinese middle-aged and older women. The latest round of CHARLS (2020) data was used. Three rounds of longitudinal data were used to demonstrate the bidirectional relationship between depression and cognition. A key finding is the bidirectional relationship between depression and cognition: higher depression severity predicted worse cognitive function, and conversely, lower cognitive function predicted increased depressive symptoms. These findings highlight that we need to improve the health conditions among middle-aged and older women by improving depression and cognitive status.
It was found that women in China in the 1960s had a very low level of education, and education had a significant effect on depression and cognition. This is in line with many studies (31–33). Having an extra year of schooling has a huge and significant protective effect on mental health and memory (34). Mexican research has revealed that women’s education has an even higher impact on cognition, with more pronounced cognitive benefits in the future (35).
The bidirectional relationship between cognition and depression is consistent with the results of longitudinal studies in Europe (36) and Korea (37). In addition, Rebecca’s study found a stable negative correlation between depression and cognition only in women (38). As age increases, it is inevitable to experience deteriorating cognitive functions, especially reduced memory and impaired judgment, which can affect social functions such as interpersonal interactions in work, life, and family, and further lead to depression or other negative mental issues (39). Shaikh’s study similarly confirms that memory changes in older adults could have an impact on daily life, such as limitations on lifestyle activities and negative emotions (40). There are also studies that have come to the opposite conclusion, suggesting that early cognitive impairment does not lead to feelings of depression in later life, perhaps because of differences in study populations and samples (41).
The findings of this study indicate that for middle-aged and older women, previous depression affects later cognition, which is consistent with the findings of many previous studies (42). The explanation in Jutta’s study is that depressive symptoms may trigger hypercortisolism, increase autonomic responses associated with cardiovascular disease, lead to inflammation, and, in turn, lead to neurotoxicity. These processes accelerate cognitive decline in the aging process (43). Yuan’s comparable study in China found that depression preceded cognitive decline in older adults, and initial depression affected subsequent cognitive function, particularly immediate and delayed recall, converging with the results of the present study (44). However, a study based on the UK female birth cohort showed that most aspects of midlife mental health were not prospectively associated with cognition (45).
In conclusion, the data used in this study further support the feasibility of conducting a longitudinal study in a population of middle-aged and elderly women. Future studies should aim to explore the clinical mechanisms underlying the interplay between depression and cognition in order to propose effective clinical interventions. Our findings have important implications for middle-aged and elderly women’s health research, suggesting that there is a bidirectional association between depression and cognition, with depression leading to worse cognitive status over time and prior cognitive impairment leading to subsequent depressive symptoms, which is an original finding for middle-aged and elderly women’s research. Based on our findings, it is recommended that society consider cognitive factors when treating depression in middle-aged and older women, and improve depressive states by improving educational and cognitive levels, as well as considering depressive states when treating cognitive decline.
5 Limitations
This study has several limitations. Firstly, all findings are based on self-reported data, which may deviate from objective reality. Self-rated memory or mood assessments could be subject to recall bias (e.g., participants may exaggerate or forget symptoms) and social desirability bias (e.g., concealing true feelings). Secondly, survey results might be influenced by the training level of investigators and environmental conditions. Variations in data collectors’ expertise, testing locations, and timing could affect response consistency and participants’ cognitive performance or emotional states. Thirdly, this study only examined the relationship between depression and cognition without adjusting for other confounding factors (e.g., age, education, and chronic diseases). Furthermore, the cognitive assessment tools in CHARLS have not undergone extensive, population-wide, and psychometrically robust validation, which may compromise the reliability of the findings and hinder comparability with prior studies. Fourthly, no adjustments were made for censored data. Subsequent studies should conduct sensitivity analyses to explore how different data handling approaches and subgroups affect variable relationships. Finally, the majority of participants in this study were married, resided in rural areas, and had only primary school education. Caution is warranted when generalizing these findings to broader populations.
6 Conclusions
Our study provides significant evidence on the relationship between depression and cognition in Chinese middle-aged and older women. The strength of our findings suggests that cognition and depression have a bidirectional relationship. The health of middle-aged and older women should be improved by treating depressive states and increasing cognition, which also suggests the value of implementing such clinical interventions.
Statements
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://charls.charlsdata.com/pages/data/111/zh-cn.html.
Ethics statement
The studies involving humans were approved by Ethical Review Committee of Peking University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XJ: Data curation, Formal Analysis, Writing – original draft. ZJ: Conceptualization, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article. This study was supported by the Natural Science Foundation of Shandong Province (ZR2022MH137).
Acknowledgments
The authors express gratitude to all respondents who participated in the survey and to everyone who organized and conducted the survey. Special thanks to the National School of Development, Peking University (NSD) and the Institute of Social Science Survey (ISSS) providing the CHARLS data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
ChenRXuPSongPWangMHeJ. China has faster pace than Japan in population aging in next 25 years. Biosci Trends. (2019) 13:287–91. doi: 10.5582/bst.2019.01213
2
Office of the Leading Group of the Seventh National Population Census of the State Council. China population census yearbook 2020(2023). Available online at: https://www.stats.gov.cn/sj/pcsj/rkpc/7rp/zk/indexch.htm (Accessed August 9, 2024).
3
LuBZhangRChaoJ. Health status and associated factors among the community-dwelling elderly women in China. Arch Gerontol Geriatr. (2018) 79:78–82. doi: 10.1016/j.archger.2018.08.005
4
YangLPengW. Prevalence and factors associated with body pain: results of a nationally representative survey of 9,586 Chinese adults aged 60 and over. Front Public Health. (2021) 9:634123. doi: 10.3389/fpubh.2021.634123
5
KimEChoiHY. Factors associated with poor self-rated health among older women living alone. Int J Environ Res Public Health. (2022) 19:11182. doi: 10.3390/ijerph191811182
6
KrobischVGebertPGülKSchenkL. Women bear a burden: gender differences in health of older migrants from Turkey. Eur J Ageing. (2021) 18:467–78. doi: 10.1007/s10433-020-00596-1
7
World Health Organization. Depressive disorder (depression)(2023). Available online at: https://www.who.int/news-room/fact-sheets/detail/depression (Accessed August 12, 2024).
8
WenYLiuCLiaoJYinYWuD. Incidence and risk factors of depressive symptoms in 4 years of follow-up among mid-aged and elderly community-dwelling Chinese adults: findings from the China Health and Retirement Longitudinal Study. BMJ Open. (2019) 9:e029529. doi: 10.1136/bmjopen-2019-029529
9
HanGChoiJChaS-YKimBIKhoHKJangM-Jet al. Effects of radix polygalae on cognitive decline and depression in estradiol depletion mouse model of menopause. Curr Issues Mol Biol. (2021) 43:1669–84. doi: 10.3390/cimb43030118
10
HandingEPStroblCJiaoYFelicianoLAicheleS. Predictors of depression among middle-aged and older men and women in Europe: A machine learning approach. Lancet Reg Health - Eur. (2022) 18:100391. doi: 10.1016/j.lanepe.2022.100391
11
MuYZhengZ. Multimorbidity patterns, social networks, and depression among chinese older women. Curr Psychol. (2023) 42:30902–10. doi: 10.1007/s12144-022-04122-7
12
LivingstonGHuntleyJSommerladAAmesDBallardCBanerjeeSet al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. (2020) 396:413–46. doi: 10.1016/S0140-6736(20)30367-6
13
BadgioPCWordenBL. Cognitive functioning and aging in women. J Women Aging. (2007) 19:13–30. doi: 10.1300/J074v19n01_02
14
RenYDongYHouTHanXLiuRWangYet al. Prevalence, incidence, and progression of cognitive impairment, no dementia among rural-dwelling Chinese older adults. J Alzheimers Dis. (2022) 85:1583–92. doi: 10.3233/JAD-215236
15
WangCJiXWuXTangZZhangXGuanSet al. Frailty in relation to the risk of Alzheimer’s disease, dementia, and death in older Chinese adults: A seven-year prospective study. J Nutr Health Aging. (2017) 21:648–54. doi: 10.1007/s12603-016-0798-7
16
Eldemire-ShearerDJamesKJohnsonPGibsonRWillie-TyndaleD. Dementia among older persons in Jamaica: prevalence and policy implications. West Indian Med J. (2017) 67:1–8. doi: 10.7727/wimj.2017.133
17
LyuJKimH-Y. Gender-specific incidence and predictors of cognitive impairment among older Koreans: findings from a 6-year prospective cohort study. Psychiatry Invest. (2016) 13:473. doi: 10.4306/pi.2016.13.5.473
18
Portellano-OrtizCConde-SalaJL. Cognition and its association with the factors of the EURO-D: Suffering and Motivation. Findings from SHARE Wave 6. Int J Geriatr Psychiatry. (2018) 33:1645–53. doi: 10.1002/gps.4967
19
YagiSGaleaLAM. Sex differences in hippocampal cognition and neurogenesis. Neuropsychopharmacology. (2019) 44:200–13. doi: 10.1038/s41386-018-0208-4
20
ZhangSHuJFanWLiuBWenLWangGet al. Aberrant cerebral activity in early postmenopausal women: A resting-state functional magnetic resonance imaging study. Front Cell Neurosci. (2018) 12:454. doi: 10.3389/fncel.2018.00454
21
KumarAAjiloreOKepeVBarrioJRSmallG. Mood, cognition and in vivo protein imaging: the emerging nexus in clinical neuroscience. Int J Geriatr Psychiatry. (2008) 23:555–63. doi: 10.1002/gps.1941
22
ZhaoYHuYSmithJPStraussJYangG. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
23
ZhaoYJohnSYangGJohnGHuPHuYet al. China Health and Retirement Longitudinal Study: 2011–2012 National Baseline User’s Guide. Peking University: National School of Development (2013).
24
RadloffLS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. (1977) 1:385–401. doi: 10.1177/014662167700100306
25
ChenHMuiAC. Factorial validity of the Center for Epidemiologic Studies Depression Scale short form in older population in China. Int Psychogeriatr. (2014) 26:49–57. doi: 10.1017/S1041610213001701
26
AndresenEMMalmgrenJACarterWBPatrickDL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. (1994) 10:77–84. doi: 10.1016/S0749-3797(18)30622-6
27
ShiY. Large sample properties of generalized estimation equations with longitudinal data. Guangxi University (2023).
28
ZyphurMJAllisonPDTayLVoelkleMCPreacherKJZhangZet al. From data to causes I: building A general cross-lagged panel model (GCLM). Organ Res Methods. (2020) 23:651–87. doi: 10.1177/1094428119847278
29
HuLBentlerPM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. (1999) 6:1–55. doi: 10.1080/10705519909540118
30
HaydukLALittvayL. Should researchers use single indicators, best indicators, or multiple indicators in structural equation models? BMC Med Res Methodol. (2012) 12:159. doi: 10.1186/1471-2288-12-159
31
CintronDWCalmasiniCBarnesLLMungasDMWhitmerRAEngCWet al. Evaluating interpersonal discrimination and depressive symptoms as partial mediators of the effects of education on cognition: Evidence from the Study of Healthy Aging in African Americans (STAR). Alzheimers Dement. (2023) 19:3138–47. doi: 10.1002/alz.12957
32
JesterDJKohnJNTibiriçáLThomasMLBrownLLMurphyJDet al. Differences in social determinants of health underlie racial/ethnic disparities in psychological health and well-being: study of 11,143 older adults. Am J Psychiatry. (2023) 180:483–94. doi: 10.1176/appi.ajp.20220158
33
OliveiraWLMeloRCDCachioniMFalcãoDVDSBatistoniSSTOrdonezTNet al. Higher purpose in life and education were associated with better cognition among older adults. Arq Neuropsiquiatr. (2024) 82:001–10. doi: 10.1055/s-0044-1779506
34
CrespoLLópez-NovalBMiraP. Compulsory schooling, education, depression and memory: New evidence from SHARELIFE. Econ Educ Rev. (2014) 43:36–46. doi: 10.1016/j.econedurev.2014.09.003
35
Díaz-VenegasCSamper-TernentRMichaels-ObregónAWongR. The effect of educational attainment on cognition of older adults: results from the Mexican Health and Aging Study 2001 and 2012. Aging Ment Health. (2019) 23:1586–94. doi: 10.1080/13607863.2018.1501663
36
BestJRCoscoTD. An analysis of dynamic, bidirectional associations between memory and verbal fluency with depressive symptoms in middle- and older-aged adults: A cohort study. J Affect Disord. (2022) 318:400–8. doi: 10.1016/j.jad.2022.09.019
37
ZhaoBJiangXKongFNamEW. Relationship between Cognition, Depression, and Oral health status in Older adults: A longitudinal cross-lagged analysis. J Affect Disord. (2023) 330:158–64. doi: 10.1016/j.jad.2023.02.142
38
ChalmersRACervinMChooCBauneBTTrollorJNNumbersKet al. Networks of inflammation, depression, and cognition in aging males and females. Aging Clin Exp Res. (2022) 34:2387–98. doi: 10.1007/s40520-022-02198-6
39
KaserMZamanRSahakianBJ. Cognition as a treatment target in depression. Psychol Med. (2017) 47:987–9. doi: 10.1017/S0033291716003123
40
ShaikhKTTathamELVandermorrisSPatersonTStokesKFreedmanMet al. The impact of memory change on everyday life among older adults: association with cognition and self-reported memory. J Int Neuropsychol Soc. (2021) 27:896–904. doi: 10.1017/S1355617720001344
41
KaarreJAbzhandadzeTSunnerhagenK. Predictors for self-reported feeling of depression three months after stroke: A longitudinal cohort study. J Rehabil Med. (2021) 53:jrm00170. doi: 10.2340/16501977-2816
42
DotsonVMMcClintockSMVerhaeghenPKimJUDraheimAASyzmkowiczSMet al. Depression and cognitive control across the lifespan: a systematic review and meta-analysis. Neuropsychol Rev. (2020) 30:461–76. doi: 10.1007/s11065-020-09436-6
43
LindertJPaulKCLachmanMERitzBSeemanTE. Depression-, anxiety-, and anger and cognitive functions: findings from a longitudinal prospective study. Front Psychiatry. (2021) 12:665742. doi: 10.3389/fpsyt.2021.665742
44
YuanJWangYLiuZ. Temporal relationship between depression and cognitive decline in the elderly: a two-wave cross-lagged study in a Chinese sample. Aging Ment Health. (2023) 27:2179–86. doi: 10.1080/13607863.2023.2225432
45
NakanishiMYamasakiSNishidaARichardsM. Midlife psychological well-being and its impact on cognitive functioning later in life: an observational study using a female British birth cohort. J Alzheimers Dis. (2019) 72:835–43. doi: 10.3233/JAD-190590
Summary
Keywords
depression, cognition, Chinese middle-aged and older females, CHARLS, longitudinal
Citation
Jiang X and Jiang Z (2025) Bidirectional association between depression and cognition in Chinese middle-aged and older women: a 10-year longitudinal study. Front. Psychiatry 16:1531202. doi: 10.3389/fpsyt.2025.1531202
Received
20 November 2024
Accepted
07 April 2025
Published
02 May 2025
Volume
16 - 2025
Edited by
Xiao Zhang, Peking University Sixth Hospital, China
Reviewed by
Rogerio Panizzutti, Federal University of Rio de Janeiro, Brazil
Javier Vicente-Alba, University Hospital Complex of Vigo, Spain
Updates
Copyright
© 2025 Jiang and Jiang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zheng Jiang, doctorjiangzheng@126.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.