- 1Nursing Department, People’s Hospital of Xiushan County, Chongqing, China
- 2The First Clinical College, Chongqing Medical University, Chongqing, China
- 3The Fifth Clinical College, Chongqing Medical University, Chongqing, China
- 4The Second Clinical College, Chongqing Medical University, Chongqing, China
- 5School of Pediatrics, Chongqing Medical University, Chongqing, China
- 6Department of Basic Courses, Chongqing Medical and Pharmaceutical College, Chongqing, China
Background: The mental health of cataract patients should not be ignored; however, little is known from existing studies about anxiety symptoms in Chinese older adults with cataracts. The aim of this study was to assess the prevalence of anxiety symptoms and their key influencing factors among Chinese older adults with cataracts.
Methods: Based on the cross-sectional data published in 2018 by the Chinese Longitudinal Healthy Longevity Survey (CLHLS), 1,320 cataract patients aged 65 and older were finally included. Anxiety symptoms were assessed using the Generalised Anxiety Disorder (GAD-7) scale. Logistic regression analyses were performed on 24 variables from three dimensions: socio-demographic characteristics, health status and lifestyle, in order to investigate the influencing factors of anxiety symptoms in older adults with cataracts. Meanwhile, this study developed an advanced Random Forest Model to rank the importance of the significant influencing factors in the logistic regression, providing an in-depth understanding for further precision prevention and management.
Results: The prevalence of anxiety symptom in Chinese older adults with cataracts was 11.06%. Logistic regression analyses showed that poor economic status (OR=3.162, 95% CI:1.719-5.817), obesity(Body Mass Index>28) (OR=2.11,95%CI:1.10-4.05), poor self-reported health (OR=1.91,95%CI:1.11-3.30), sleeping less than 7h(OR=1.98,95%CI:1.30-3.01), having fair (OR=1.61,95%CI:1.03-2.53) or poor (OR=2.70,95%CI:1.21-6.02) life satisfaction, and having hearing impairment (OR=1.72,95%CI:1.12-2.65) were risk factors for anxiety symptoms in cataract patients, eating fresh fruits (OR=0.587, 95%CI:0.369-0.933) and age (OR=0.97,95%CI:0.94-0.99) were protective factors for anxiety symptoms in cataract patients. The results of Random Forest showed that age was the most important factor affecting anxiety symptoms in cataract patients, followed by Body Mass Index, self-reported health, economic status, eating fruits or not, sleep duration, life satisfaction, and hearing impairment.
Conclusion: The results of the study showed that the anxiety symptoms of cataract patients should not be ignored and are influenced by a variety of factors. Healthcare workers should actively conduct mental health screening and strengthen the monitoring of important influencing factors in the treatment and care of cataract patients.
1 Introduction
Cataract is a chronic eye disease that causes vision loss due to clouding of the lens (1).It is also one of the leading causes of preventable blindness.According to the statistics of 2023, the total number of cataract cases in China had exceeded 18 million from 1990 to 2019, and it was projected that the number of cataract cases in China would rise to 43 million by 2030 and the prevalence of cataract in the 45–89 age group would reach 33.34% (2). In addition to causing severe disability and dysfunction, cataract is associated with an increased risk of psychological problems such as depressive symptoms, anxiety symptoms (3–5). In a 2019 study, Ann IY et al. showed that anxiety in cataract patients exacerbated insomnia symptoms in cataract patients (6). This may further delay the recovery of cataract patients after surgery and increase their mortality. Results from another study suggested that anxiety symptoms may lead to increased intraocular pressure or blood pressure in cataract patients undergoing cataract surgery (5). This may cause patients to experience more severe pain and pose a significant impediment to cataract treatment and prognosis (7). Therefore, a better understanding of the clinical epidemiological characteristics of anxiety symptoms among cataract patients would help in the early identification of those at high risk of anxiety symptoms, thereby improving patients’ physical and mental health.
Anxiety disorders are common neurological disorders that consist of three main types: trait anxiety, state anxiety, and social anxiety, which are generally characterised by excessive worry, fear, and apprehension, and are usually accompanied by specific somatic symptoms, such as sweating, dizziness, and shortness of breath or even insomnia, irritability, and muscle aches and pains (8, 9).Anxiety symptoms are highly persistent, usually manifest as chronic episodes, and often co-exist with other psychiatric disorders (10). It has been reported that approximately 4.7% of older adults in China suffer from anxiety symptoms (11). Long-term anxiety symptoms may lead to a range of health problems, such as easy fatigue and poor immunity, which can further develop into chronic illnesses, such as heart disease, stroke and other chronic condition (10). Additionally,there is also strong association between anxiety symptoms and higher rates of suicide and mortality (12). The development of anxiety symptoms is primarily linked to physical risk factors (e.g., cognitive impairment, high blood pressure, poor health self-assessment, and impaired vision or hearing), psychological risk factors (e.g., lack of self-efficacy, history of mental illness, and dysfunction), and social risk factors (e.g., lack of social support, overprotection during childhood, and low income) (13).Various factors may ultimately activate neuroinflammatory pathways, leading to neuronal pathway and neurotransmitter dysfunction i.e., reduction of serotonin, dopamine, and norepinephrine in the synaptic gap, which ultimately leads to the development of anxiety disorders (14, 15). Numerous previous studies have reported on the factors influencing anxiety symptoms in older adults. He, ZF et al. showed that being female, being widowed, and having a chronic disease were risk factors for anxiety symptoms in Chinese older adults, whereas living in a rural area and walking every day were protective factors for anxiety symptoms in older adults (16). Other studies have focused on possible measures for preventing anxiety symptoms in older adults from the perspectives of lifestyle and health status (17, 18). In addition, some studies have also reported on anxiety and depression in older adults with visual impairment, and the results suggest that relatively young age, depressive symptoms, not living alone, and working difficultly are risk factors for anxiety symptoms in older adults with visual impairment (19). Undoubtedly, the results of all of these studies have played a prominent role in preventing and ameliorating anxiety symptoms in older adults in recent years; nonetheless, the results of these studies may still be inapplicable in Chinese older adults with visual impairment, especially cataract patients. As the mental health of Chinese cataract patients remains understudied, it is important to understand the prevalence of anxiety symptoms and its main influencing factors in Chinese cataract patients in order to address this gap.
In terms of research methodology, previous studies related to cataract tend to apply traditional logistic regression analysis. As a machine learning algorithm, Random Forest(RF) is an excellent research tool because of its powerful classification ability and easy-to-interpret learning mechanism. In recent years, Random Forest has been widely used in the medical field for diagnosis and classification of disease (20), prediction of clinical outcomes (21), and estimation of the significance of exposure to pathogenic factors (22). RF is an integrated learning method based on decision trees, and by analysing the splitting points of each decision tree, we can visually understand how the model makes predictions (23). Other machine learning models such as XGBoost (Extreme Gradient Boosting) can provide better prediction accuracy, but their interpretability is relatively poor, especially when dealing with high-dimensional data, the internal mechanism of the model is more complex (24). Black-box models, such as neural networks, are also difficult to explain their internal decision-making process (25). In addition, RF is able to handle missing values, noise and small sample sizes well when the data volume is moderate (23). It requires less data preprocessing and can handle high-dimensional features, which makes it suitable for many practical problems. In the application scenario of medical research, the stability, reliability and interpretability of the model may be more important than the mere prediction accuracy. Therefore, this study proposes to combine Logistic Regression with Random Forest, and further use Random Forest Model to rank the importance of significant influencing factors in Logistic Regression. The application of this more novel approach to data analysis may help to gain a deeper understanding of the causes of anxiety symptoms in cataract patients and to intervene and manage them with precision.
In summary, given the clinical importance of anxiety symptoms among cataract patients and the limitations in previous studies, we used the national cross-sectional data published in 2018 by the Chinese Longitudinal Healthy Longevity Survey (CLHLS) to analyze the influencing factors of anxiety symptoms in older adults with cataracts in China from multiple perspectives, and measured the importance of these factors through a Random Forest Model. It has important reference value for alleviating anxiety symptoms and promoting the overall mental health of older adults with cataracts.
2 Materials and methods
2.1 Study population
The data for this study came from the Chinese Longitudinal Healthy Longevity Survey(CLHLS) organized by the Centre for Healthy Aging and Development at Peking University,which is a nationally representative prospective cohort survey of older people aged 65 years and over.It used a multi-stage, disproportionate and targeted random sampling method (26), covering 631 cities in 23 provinces of China, and included surveys on socio-demographic characteristics, social conditions, economic conditions, and health conditions. The CLHLS project was approved by the Biomedical Ethics Committee of Peking University (IRB00001052-13074). All participants or their proxy respondents provided informed consent (27).
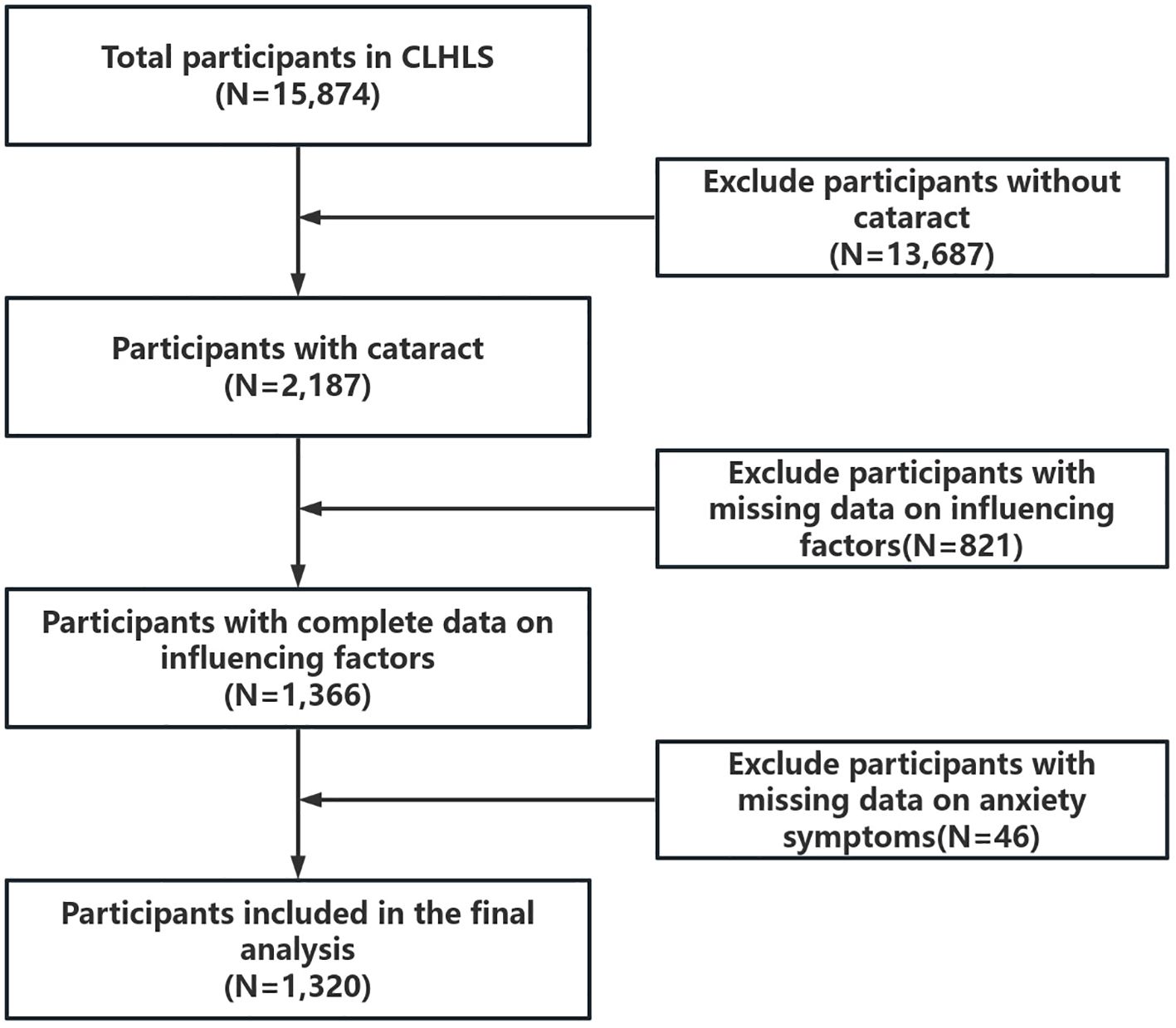
This study used data published by CLHLS in 2018.The selection of the study sample was based on the question in the questionnaire, ‘Are you currently diagnosed with cataracts by hospital?’. Respondents who answered ‘yes’ to this question were included in our study. There were 15,874 participants in CLHLS in 2018, of which 2,187 participants were diagnosed with cataract by a clinician at the hospital. Participants who lacked information on anxiety symptoms and related influencing factors were further excluded to ensure accuracy and reliability of data analysis and to reduce selection biases. The study ultimately included 1,320 participants aged 65 years or older. The detailed data cleaning process is shown in Figure 1.
2.2 Outcome variables
Anxiety symptoms in older adults were assessed using the Generalised Anxiety Disorder (GAD-7) scale (28). The GAD-7 scale consists of seven questions, including “feeling uneasy, worried, and annoyed”, “can’t stop or control worrying”, “worrying too much about things”, “very nervous and difficult to relax”, “very anxious and therefore unable to sit still”, “becoming easily annoyed”, “feeling that something terrible has happened”.Each question was scored on a scale ranging from 0 to 3 (0 = never, 1 = few days, 2 = more than half of the days, 3 = almost every day), and the total score for the seven questions ranged from 0 to 21, with a total score on the scale of greater than or equal to 5 considered to be suffering from anxiety symptoms (28). The results of previous studies have demonstrated the utility of the scale in the Chinese older adult population (29). Cronbach’s α of GAD-7 in this study was 0.914.
2.3 Influencing factors
Based on the availability of data resources in the CLHLS database and the exploration of factors influencing anxiety symptoms in Chinese older adults in previous studies (22, 30, 31), we sorted out 24 influencing factors that may affect the anxiety symptoms of cataract patients at 3 levels, namely, socio-demographic characteristics, health status, and lifestyle.
Socio-demographic characteristics included age, gender, education, marital status, place of residence, and economic status.
Health status included Body Mass Index, abdominal obesity, hearing impairment, hypertension, diabetes, cardiopathy, self-reported health, and Activities of Daily Living disability.
Lifestyle included eating vegetables and fruits, taste, sleep duration, smoking, drinking, exercise, physical labour, social activity, and life satisfaction.
Detailed variable measurements and variable assignments are shown in Appendix I.
2.4 Statistical analyses
The samples were used for descriptive statistical analysis after data cleaning. Kolmogorov-Smirnov test was used to determine normal distribution of continuous variables. Continuous variables conforming to normal distribution were expressed as mean ± standard deviation (M ± SD) and categorical variables were expressed as frequency and percentage (n (%)).Two independent samples t-test and chi-square test were used for between-group comparisons. Bonferroni correction was used to rule out the problem of multiple comparisons between variables and to avoid false-positive results. Binary logistic regression was adopted to explore the factors influencing the anxiety symptoms of cataract patients, and variance inflation factor (VIF) was used to detect possible collinearity problems between variables in the regression model, and VIF<10 was considered to be free of collinearity problems.
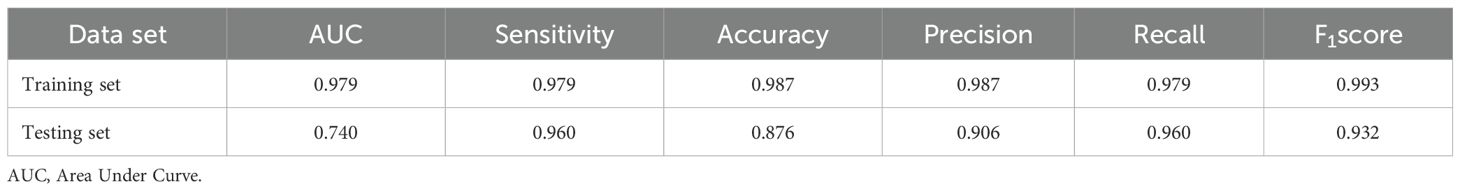
In order to assess the significance of different influencing factors, we ranked the random forest importance of statistically significant variables in the logistic regression model. Based on the statement of Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis(TRIPOD), this study was conducted by randomly selecting 70% of the overall data as the training set and 30% as the test set (32). This division criterion ensured that the model had enough data for effective training, and also ensured the representativeness of the test set to avoid overfitting or underfitting of the model, which demonstrated good utility in model construction in previous medical studies (33). The optimal parameters of the model were obtained using grid optimisation, the model was tested by the 10-fold cross-validation method, and and a random forest model with parameters mtry of 3 and ntree of 500 was finally built. Compared with traditional regression methods, the random forest algorithm can avoid increasing estimated parameters and being sensitive to missing values or outliers when dealing with multilevel categorical variables, so the application of RF reduces bias, tolerates outliers, and reduces overfitting of the model, resulting in more accurate and stable predictions for the study (34).The final order of importance of the influencing factors, as reflected in the average reduction of the Gini index, is obtained. Specifically, the greater the average decrease in the Gini index for a variable, the more important that variable is (35). The performance of the model was assessed using Area Under Curve (AUC), accuracy, sensitivity, precision, recall, and F1 score. All data analyses were performed using SPSS 26.0 and R 4.3.0 and P<0.05 (two-sided) was considered statistically significant.
3 Results
3.1 Descriptive analysis of the sample
3.1.1 Socio-demographic characteristics
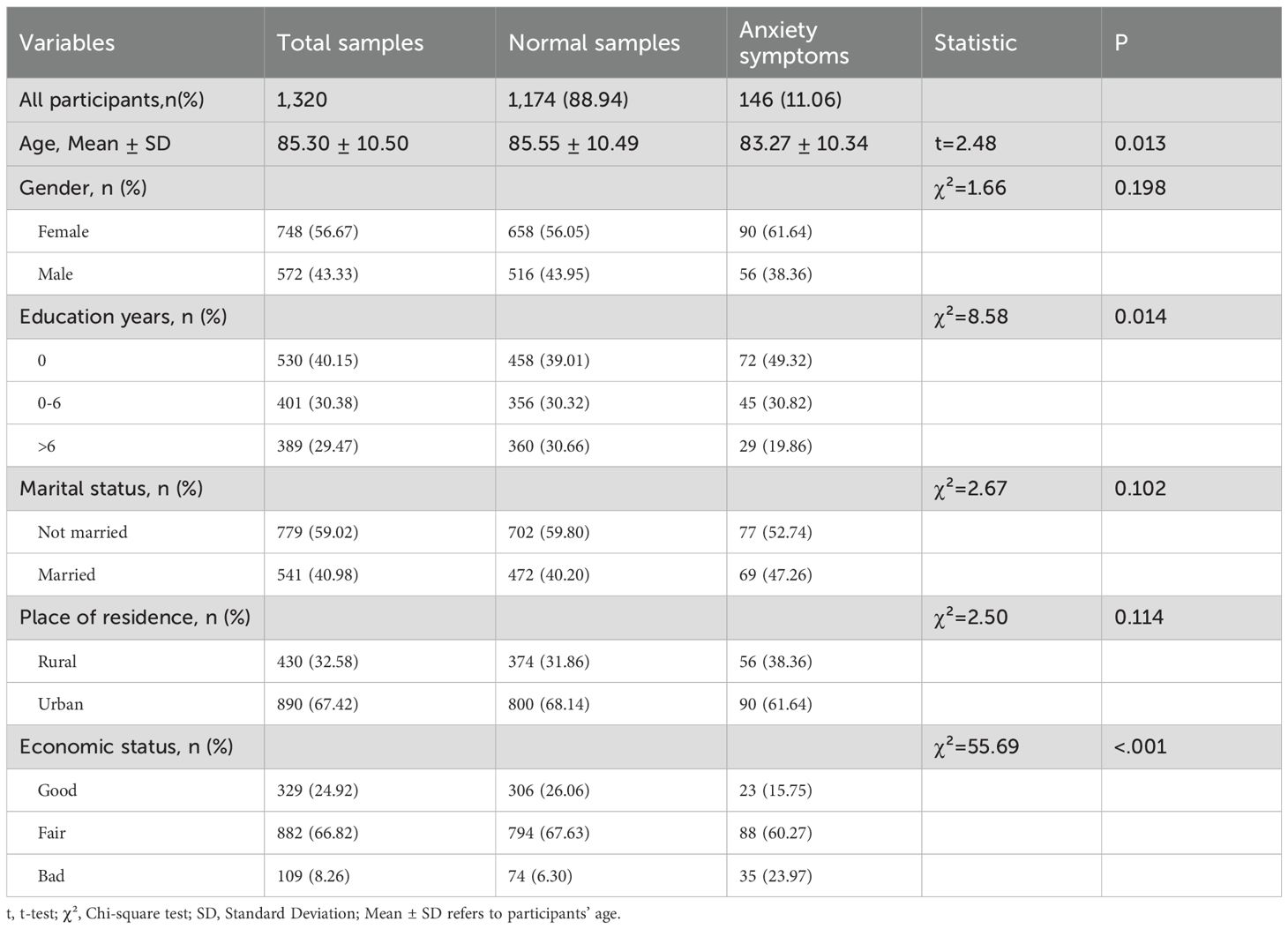
A total of 1,320 cataract patients were included in this study, of which 146 had anxiety symptoms with a prevalence of 11.06%. The mean age of the respondents was 85.30 ± 10.50. About 43.33% were males, 67.42% lived in urban areas, and 40.15% of the respondents had less than 6 years of education. Only 8.26% of the respondents were dissatisfied with their economic status. The t-test results showed that in the group of cataract patients, the mean age of patients with anxiety symptoms was lower than that of patients without anxiety symptoms (p=0.013). The results of chi-square test showed that there was a statistically significant difference in the prevalence of anxiety symptoms among cataract patients across years of education and economic status (p<0.05), and the detailed results were displayed in Table 1.
3.1.2 Health status
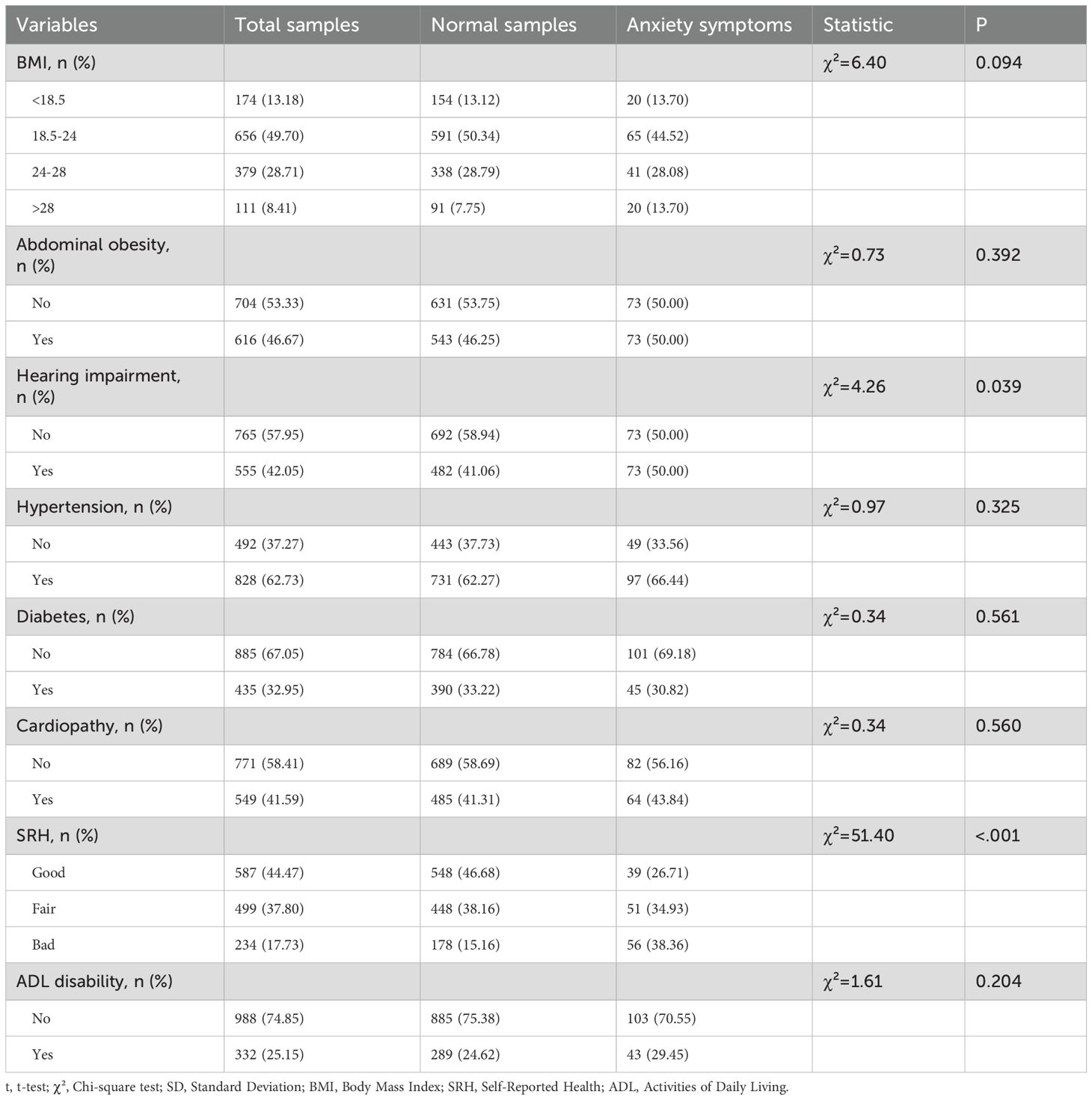
In terms of health status (Table 2), nearly half (44.47%) of the respondents in this study reported their self-reported health as “good”. At the disease-specific level, 49.7% of the respondents had a Body Mass Index within the normal range. Abdominal obesity, hearing impairment, and cardiopathy were also present in nearly half of the respondents, at 46.67%, 42.05%, and 41.59%, respectively. Fewer respondents had diabetes (32.95%) and more respondents had hypertension(62.73%). The results of chi-square test showed that the prevalence of anxiety symptoms in cataract patients was statistically significant (p<0.05) between different hearing impairment, self-reported health.
3.1.3 Lifestyle
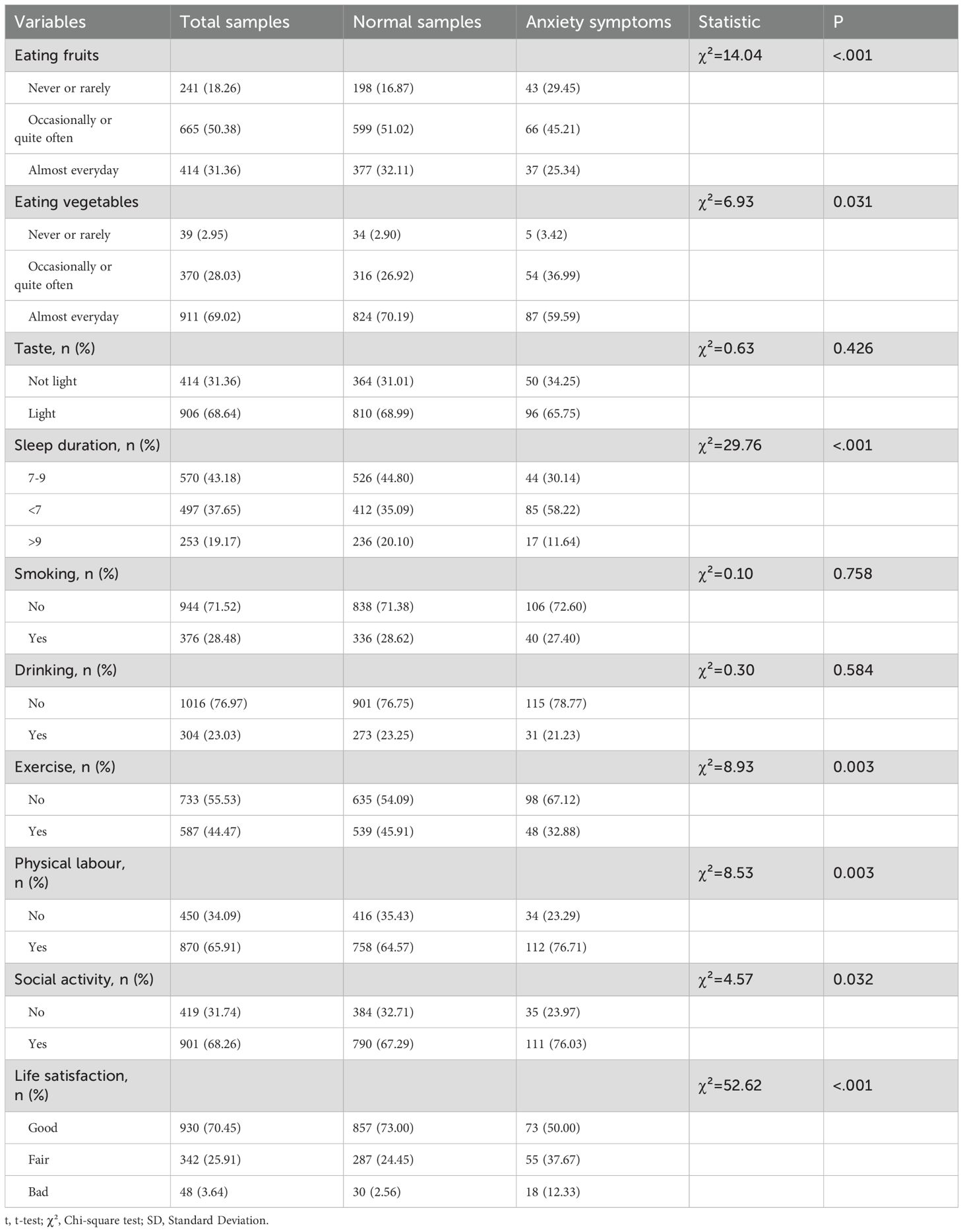
In terms of lifestyle (Table 3), 31.36% of the respondents consumed fruits almost every day, 69.02% consumed vegetables almost every day, 68.64% maintained a light diet, and 62.35% slept for more than 7 hours. About 44.47% of the respondents exercised regularly, 28.48% smoked, and 23.03% drank. About 65.91% of the participants were engaged in physical labor and 68.26% experienced low social activities. Only 3.64% of the respondents rated their quality of life as “poor”. The results of the chi-square test showed a statistically significant difference (p<0.05) in the prevalence of anxiety symptoms among cataract patients between different frequency of eating fruits, frequency of eating vegetables, sleep duration, exercise, physical labor, social activities and life satisfaction.
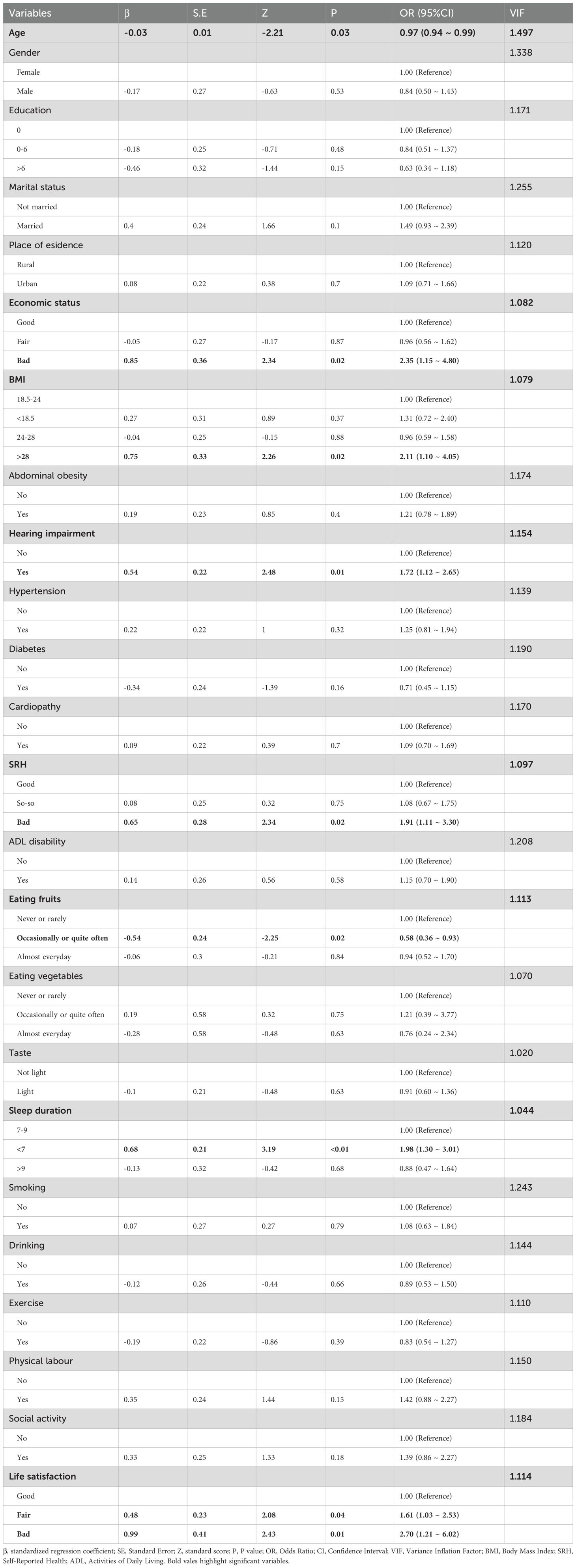
3.2 Binary logistic regression results
Multifactional logistic regression analysis suggested that age, BMI, SRH, economic status, eating fruits, sleep duration, life satisfaction, and hearing impairment were significant influencing factors on anxiety symptoms in cataract patients (Table 4, Figure 2).
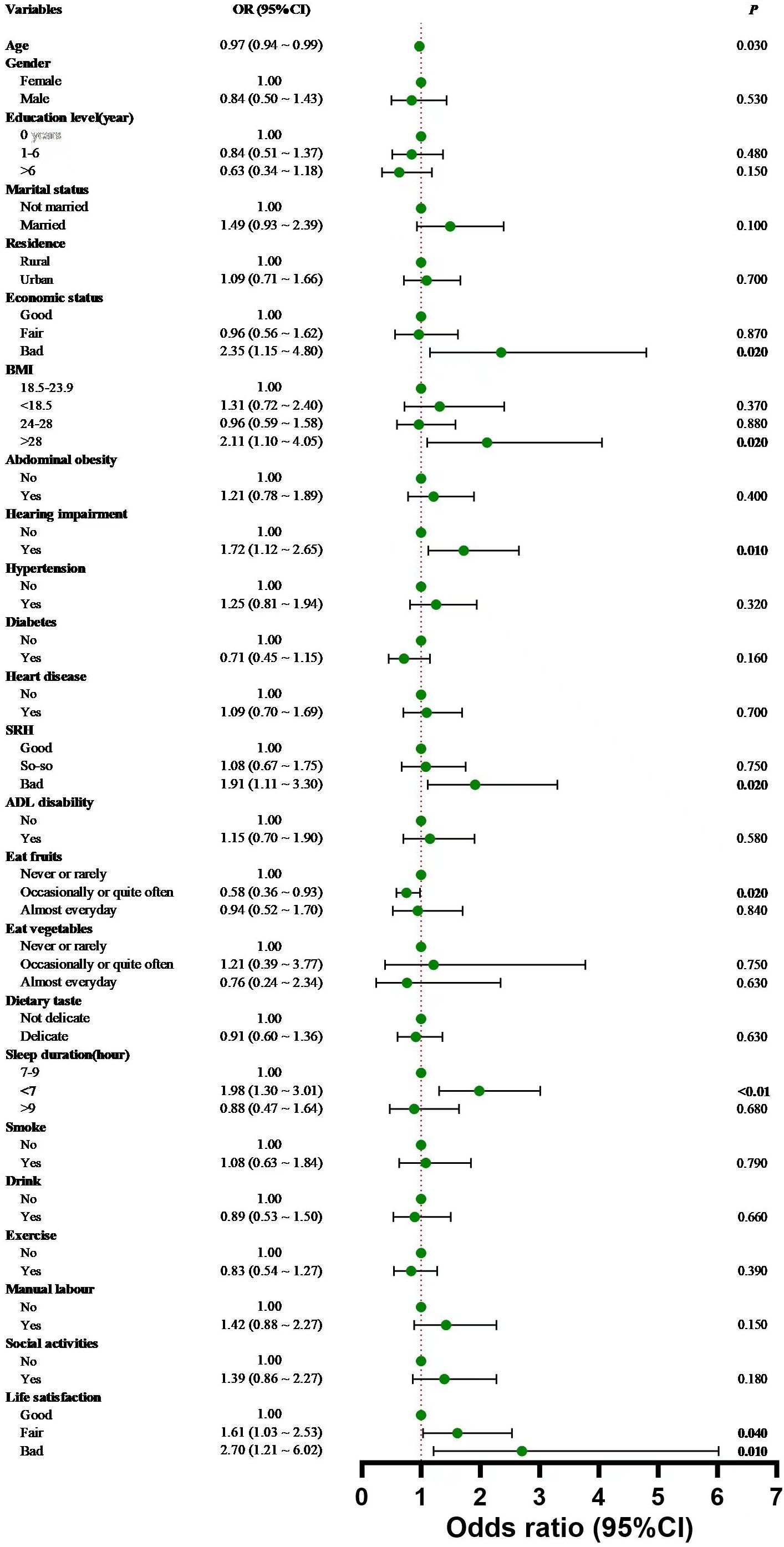
Figure 2. Forest plot based on the results of Binary logistic regression analysis. Error bars represent 95% confidence intervals, and dots indicate odds ratios.
Specifically, for each additional year of age, the risk of anxiety symptoms in cataract patients decreased by 3% (OR = 0.97, 95% CI:0.94 ~ 0.99). Cataract patients with poor economic status (OR=2.35, 95%CI:1.15 ~ 4.80) had a higher risk of prevalence of anxiety symptoms compared to those with good economic status. Cataract patients who ate fruits (OR=0.58; 95%CI:0.36 ~ 0.93) were 42% less likely to develop anxiety symptoms compared to those who did not eat fruits. Cataract patients (OR=1.98, 95%CI:1.30 ~ 3.01) who slept fewer hours of sleep (<7h) had a 1.98-fold increased risk of suffering from anxiety symptoms compared to those who had normal sleep hours(7-9h). Compared with cataract patients with good life satisfaction, those with fair (OR=1.61, 95%CI:1.03 ~ 2.53) or poor (OR=2.70, 95%CI:1.21 ~ 6.02) life satisfaction had a 1.61-fold and 2.70-fold increased risk of suffering from anxiety symptoms, respectively. Cataract patients with a BMI >28 (OR=2.11, 95%CI:1.10 ~ 4.05) were 2.11 times more likely to have anxiety symptoms than those with a normal BMI (18.5-24). Cataract patients with poor self-reported health(OR=1.91, 95%CI:1.11 ~ 3.30) had a 1.91-fold increased risk of suffering from anxiety symptoms compared to those with good self-reported health. Cataract patients with hearing impairment (OR=1.72, 95% CI:1.12-2.65) had a higher risk of prevalence of anxiety symptoms compared to those without hearing impairment. There was no collinearity among all variables.
3.3 Random forest results
The results of the Random Forest showed that age was the most important factor affecting anxiety symptoms in cataract patients, followed by BMI, self-reported health, economic status, eating fruits or not, sleep duration, life satisfaction and hearing impairment(Figure 3). Table 5 displays the performance indicators of the random forest model on the training set and the test set.
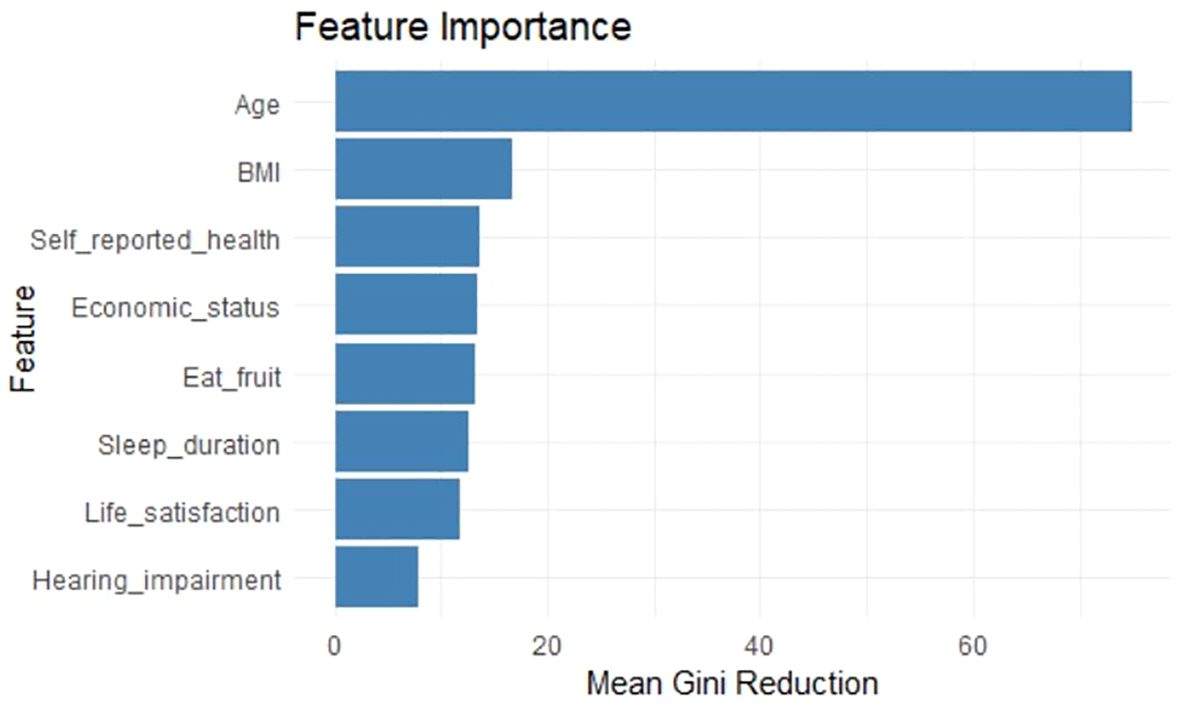
Figure 3. Importance ranking of variables with decreasing average Gini index based on random forest model. The bar graph represents the extent to which each variable affects the dependent variable and the rank of importance in the random forest model.
4 Discussion
To the best of our knowledge, this study is the first to report on the prevalence of anxiety symptoms and its influencing factors in Chinese older adults with cataracts. Based on a nationally representative database, we explored the factors influencing anxiety symptoms in cataract patients in terms of socio-demographic characteristics, lifestyle and health status, and introduced Random Forest(RF) to rank the importance of significant factors. Our findings showed that the prevalence of anxiety symptoms among Chinese older adults with cataracts was 11.06%, which was higher than 7.6% reported by Huang Y et al. (36). The results of a study among Australian older adults with cataracts demonstrated a prevalence of anxiety symptoms of 10.08%, which was significantly higher than 8.3% in normal Australian older adults (37).This may be explained by the findings of Evans, JR et al., that people with cataracts have reduced vision and are more likely to have other symptoms or diseases, that increase the risk of anxiety and depression compared to people with normal vision (38).
Our finding that age has a protective effect on anxiety symptoms in cataract patients is consistent with the results of a longitudinal study exploring the development of depression and anxiety symptoms in older adults with visual impairment (19). Other findings addressing physiological mechanisms in older adults suggest a different view, namely that aging increases the risk of developing anxiety symptoms (39–41). Risk assessment for anxiety symptoms often requires a combination of physiological, psychological and social perspectives. Psychologically, older adults are better able to cope with changing situations because their stress tolerance and self-regulation ability increase with experience. It is not difficult to speculate that the vision problems caused by cataracts may increase anxiety symptoms, but aging may allow for more mature coping mechanisms, which may perhaps further alleviate the development of anxiety symptoms. From a social perspective, compared to younger people, older adults have more satisfying social networks (42) and fewer negative interactions with family members and social network members (43, 44), which can have a positive impact on older adults’ mental health. At the same time, older people have fewer social responsibilities, and their life, work, and marital stresses may be correspondingly lower, which also helps the older adults to avoid negative emotions such as anxiety and depression.
Body Mass Index(BMI) also has a more significant effect on anxiety symptoms in cataract patients. Previous studies have shown that obesity is associated with the development of anxiety symptoms (45). Obesity may contribute to the development of anxiety disorders through a variety of pathways. Psychologically, obesity-induced discrimination and shame (46) as well as reduced quality of life (47) may lead to the development of anxiety symptoms in obese individuals. Physiologically, the range of chronic diseases and dysfunctions caused by obesity may also further increase the risk of developing anxiety symptoms (48, 49). At the same time, anxiety symptoms may also further bring about weight gain by triggering a hypothalamic-axis-driven passive response, whereby an increase in cortisol stimulates cravings for high-calorie foods, further contributing to accumulation of fat (50, 51).In addition to this, it has been shown that the risk of cortical clouding of the lens also increases with a rise in BMI (52),i.e. there is also a link between obesity and the development or exacerbation of cataracts.
Other factors that have a more pronounced effect on the anxiety symptoms of cataract patients include self-reported health(SRH) and economic status. SRH refers to an individual’s self-assessment of his or her health, which is not only a measure of subjective perception of health, but also a reflection of psychological state of the individual, such as the sense of well-being (53). The results of the present study revealed that patients who reported their health as poor were more prone to anxiety. It has been shown that SRH is related to the development of anxiety symptoms, and that there is an correlation between the level of SRH and the severity of anxiety symptoms (54, 55). Self-reported economic status is an important indicator of an individual’s economic status. Previous studies have shown that economic status affects mental health through both material and psychosocial pathways, with a positive correlation between better economic status and lower likelihood of developing psychological disorders (56). More favorable material conditions can reduce the psychological burden of cataract patients due to daily life consumption and the cost of medical care for chronic diseases. At the same time, lower levels of SRH and economic status have also been found to be associated with an increased prevalence of chronic diseases, which may further affect patients’ anxiety symptoms (57, 58).
Fruits consumption habit and sleep duration, two lifestyle-related factors, also demonstrated a significant correlation with anxiety symptoms in cataract patients in the present study. Previous studies have confirmed that fruits contain a variety of substances such as vitamins that are beneficial to mental health (59), suggesting that fruits intake is associated with anxiety symptoms to some extent, which is consistent with the results of the present study. Sleep duration is to some extent an indicator of sleep quality, and the results of the present study revealed that cataract patients with low sleep duration (less than 7h/day) were more likely to experience anxiety symptoms. Evidence from other studies also suggests that poor sleep quality negatively affects the mental health of the population (60), which in turn causes the onset of anxiety symptoms in patients. Therefore, sleep is one of the important influencing factors on anxiety symptoms in cataract patients.
In addition to this, life satisfaction has a more significant effect on anxiety symptoms in cataract patients. Life satisfaction can be seen as a subjective assessment of the quality of life. Many studies have confirmed the negative correlation between quality of life and anxiety symptoms in people (61). This finding applies to cataract patients. In addition, hearing impairment is one of the most important factors influencing anxiety symptoms in cataract patients. Studies have confirmed the association between hearing impairment and psychiatric disorders such as anxiety symptoms, but further research is needed to investigate the direction of causation and other correlations (62). Hearing impairment may cause anxiety symptoms in patients by limiting their social connections in daily life. It has even been found that the dual impairment of hearing and vision exacerbates the occurrence of anxiety symptoms and psychiatric disorders in patients compared with those with visual impairment (63). This is consistent with the finding in the present study that hearing impairment is associated with anxiety symptoms in patients with cataracts, but the specific physiological mechanisms of the effect need to be further investigated.
The results of the study also demonstrated that age was the most important factor affecting anxiety symptoms in older adults with cataracts, and the other factors were, in order of importance, BMI, SRH, economic status, eating fruits or not, sleep duration, life satisfaction, and hearing impairment. Therefore, the primary improvement strategies for anxiety symptoms in older adults with cataracts should focus on the impact of age. This suggests that under the current trend of vigorously exploring nursing strategies for the older adults in the medical industry, it is still necessary to pay attention to the mental health needs of the younger elderly groups. Secondly, for cataract patients with higher or lower BMI, clinicians should provide personalised intervention programmes, including nutritional guidance, sensible diet, and exercise interventions, to help patients improve their weight status and thus reduce anxiety symptoms. Healthcare providers such as hospitals can promote interdisciplinary collaboration among ophthalmologists, dietitians, psychologists and exercise therapists to provide comprehensive weight management and mental health interventions for cataract patients. In addition, there is an urgent need for the public health sector to take action to deepen cataract patients’ knowledge and assessment of their own health status by widely disseminating health knowledge through diversified channels such as community forums, television and radio media and online platforms. Public health education and promotion should emphasise the importance of individual assessment and perception of their own health status, and encourage cataract patients to conduct regular health self-assessment and to detect and report psychological problems in a timely manner. This study calls on the government and the community to pay attention to the economic plight of cataract patients, and to effectively reduce their financial burden by improving health insurance policies, providing medical assistance and financial support. In terms of nutritional guidance, a balanced diet should be advocated, and the intake of foods rich in vitamins and minerals, especially fruits, should be appropriately increased in order to strengthen the body’s resistance. For cataract patients with hearing impairment, hearing screening should be implemented and hearing assistive devices or interventions should be provided to reduce the negative impact of hearing impairment on mental health. In summary, this study suggests that public health departments should consider a comprehensive multilevel intervention strategy to enhance the quality of life and reduce anxiety symptoms in older adults with cataracts.
5 Conclusion
Based on the CLHLS database, this study assessed the prevalence of anxiety symptoms and related influencing factors in Chinese older adults with cataracts aged 65 years and older, and ranked the importance of the influencing factors using the random forest model.The results of the study showed that the prevalence of anxiety symptoms among Chinese older adults with cataracts was 11%. Poor economic status, social inactivity, obesity(Body Mass Index>28), poor self-reported health(SRH), sleep duration less than 7h, fair or poor life satisfaction, and hearing impairment were risk factors for anxiety symptoms in cataract patients, and eating fresh fruits and age were protective factors for anxiety symptoms in cataract patients. Age had the greatest effect on the anxiety symptoms of cataract patients, followed by Body Mass Index, SRH, economic status, eating fruits, sleep duration, life satisfaction, and hearing impairment. Based on this, we suggest that healthcare professionals should conduct extensive psychological surveys when treating and caring for older cataract patients, strengthen the monitoring of the above-mentioned influencing indicators, and take psychological as well as pharmacological interventions in a timely manner. Due to the limitations of our use of publicly available databases, future studies should conduct more comprehensive and precise studies on the mental health of cataract patients to verify and consider some factors that may not be adequately considered.
6 Limitations
Firstly, the results of this study were based on cross-sectional data, which made it difficult to make causal inference about the etiology. Therefore, we need to further discuss this topic in future studies in conjunction with a longitudinal study design. Second, thesamples included in this study were all older cataract patients, and the effects of these factors on non-cataract patients were not further explored. Future studies may consider setting up a control group of non-cataract patients to further investigate the role of influencing factors in this context. Third, the data in this study were all derived from self-reporting by the respondents, and there may be subjective information biases, which may affect the objectivity and authenticity of the results. Fourth, the data in this study was limited by the content of the public database, and some potentially important influencing factors were not included in the study (e.g., taking medications, healthcare services, cataract surgery, other types of chronic diseases, etc.). What’s more, the database did not further collect diagnostic histories of cataracts and anxiety symptoms, which should be considered as part of a more comprehensive design for investigation in future studies. Fifth, there may also be other interferences related to eye diseases in the screening process of cataract patients, and future studies should consider further eliminating these interferences. Finally, due to the specificity of the cataract patient population, the national representativeness of the sample used in our study may have been somewhat insufficient, and thus all the conclusions in this paper deserve further justification in future studies with large samples.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://opendata.pku.edu.cn/dataset.xhtml?persistentId=doi:10.18170/DVN/WBO7LK, Chinese Longitudinal Healthy Longevity Survey.
Ethics statement
The studies involving humans were approved by The Biomedical Ethics Committee of Peking University (IRB00001052-13074). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
FZ: Writing – original draft, Writing – review & editing. XL: Writing – original draft, Formal analysis. KL: Writing – original draft, Formal analysis. LX: Writing – original draft, Investigation, Methodology. LW: Writing – original draft, Investigation, Methodology. SC: Methodology, Writing – original draft, Supervision. YF: Supervision, Writing – original draft. TN: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We thank each participant for their support of our study. At the same time, we would like to express our sincere thanks to the staff of the Chinese Longitudinal Healthy Longevity Survey (CLHLS) database.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1534863/full#supplementary-material
Abbreviations
CLHLS, Chinese Longitudinal Healthy Longevity Survey; GAD-7, Generalised Anxiety Disorder; RF, Random Forest; XGBoost,Extreme Gradient Boosting; TRIPOD, Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis; M ± SD, mean ± standard deviation Variance Inflation Factor, VIF; β: standardized regression coefficient; SD, Standard Deviation; SE, Standard Error; Z, standard score; P, P value; OR, Odds Ratio; CI, Confidence Interval; BMI, Body Mass Index; SRH, Self-Reported Health; ADL, Activities of Daily Living; AUC, Area Under Curve.
References
1. Liu Y-C, Wilkins M, Kim T, Malyugin B, and Mehta JS. Cataracts. Lancet. (2017) 390:600–12. doi: 10.1016/s0140-6736(17)30544-5
2. Wu T-H, Liu W-M, Li J-Q, Song Z-Y, and Lu P-R. Time trends and gender disparities of Chinese cataract burden and their predictions. Int J Ophthalmol. (2023) 16:1527–34. doi: 10.18240/ijo.2023.09.21
3. Bohman E, Wyon M, Lundström M, and Dafgård Kopp E. A comparison between patients with epiphora and cataract of the activity limitations they experience in daily life due to their visual disability. Acta Ophthalmol. (2017) 96:77–80. doi: 10.1111/aos.13447
4. Deng X, Geng Z, Yu J, Dai X, Kuang X, Chen X, et al. The association between cataract and cognitive functions in older adults: A longitudinal cohort study. J Alzheimer’s Dis. (2023) 91:1097–105. doi: 10.3233/JAD-220963
5. Wang S, Du Z, Lai C, Seth I, Wang Y, Huang Y, et al. The association between cataract surgery and mental health in older adults: A review. Int J Surg. (2024) 110:2300–12. doi: 10.1097/js9.0000000000001105
6. Ahn IY, Lee SJ, Han YS, Park CS, Kim BJ, Lee CS, et al. Effects of emotional stability on insomnia through anxiety in patients with cataracts. Psychiatry Invest. (2019) 16:93–6. doi: 10.30773/pi.2018.11.13
7. van der Aa HP, Comijs HC, Penninx BW, van Rens GH, and van Nispen RM. Major depressive and anxiety disorders in visually impaired older adults. Invest Ophthalmol Vis Sci. (2015) 56(2):849–54. doi: 10.1167/iovs.14-15848
8. Fujihara Y, Guo K, and Liu CH. Relationship between types of anxiety and the ability to recognize facial expressions. Acta Psychol. (2023) 241:104100. doi: 10.1016/j.actpsy.2023.104100
9. Gelenberg AJ. Psychiatric and somatic markers of anxiety: identification and pharmacologic treatment. Prim Care Companion J Clin Psychiatry. (2000) 2:49–54. doi: 10.4088/pcc.v02n0204
11. Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, et al. Prevalence of mental disorders in China: A cross-sectional epidemiological study. Lancet Psychiatry. (2019) 6:211–24. doi: 10.1016/s2215-0366(18)30511-x
12. Allan NP, Gorka SM, Saulnier KG, and Bryan CJ. Anxiety sensitivity and intolerance of uncertainty: transdiagnostic risk factors for anxiety as targets to reduce risk of suicide. Curr Psychiatry Rep. (2023) 25:139–47. doi: 10.1007/s11920-023-01413-z
13. Vink D, Aartsen MJ, and Schoevers RA. Risk factors for anxiety and depression in the elderly: A review. J Affect Disord. (2008) 106:29–44. doi: 10.1016/j.jad.2007.06.005
14. Idahosa SO, Diarra R, Ranu HK, Nasiri RH, and Higuchi S. Evidence and mechanism of bile acid-mediated gut-brain axis in anxiety and depression. Am J Pathol. (2025) 195:163–73. doi: 10.1016/j.ajpath.2024.10.019
15. Guo B, Zhang M, Hao W, Wang Y, Zhang T, and Liu C. Neuroinflammation mechanisms of neuromodulation therapies for anxiety and depression. Transl Psychiatry. (2023) 13:5. doi: 10.1038/s41398-022-02297-y
16. He ZF, Tan WY, Ma H, Shuai Y, Shan Z, Zhai J, et al. Prevalence and factors associated with depression and anxiety among older adults: A large-scale cross-sectional study in China. J Affect Disord. (2024) 346:135–43. doi: 10.1016/j.jad.2023.11.022
17. Wang X, Yin Z, Yang Y, Fu X, Guo C, Pu K, et al. Association of plant-based dietary patterns with depression and anxiety symptoms in Chinese older adults: A nationwide study. J Affect Disord. (2024) 350:838–46. doi: 10.1016/j.jad.2024.01.159
18. Chen Y, Guo H, Li Z, Huang L, Hong T, and Wang H. Association of self-reported arthritis with depression, anxiety, and comorbid depression/anxiety among the older Chinese adults: A cross-sectional study. J Affect Disord. (2024) 354:323–30. doi: 10.1016/j.jad.2024.03.086
19. Heesterbeek TJ, van der Aa HPA, van Rens G, Twisk JWR, and van Nispen RMA. The incidence and predictors of depressive and anxiety symptoms in older adults with vision impairment: A longitudinal prospective cohort study. Ophthalmic Physiol Optics: J Br Coll Ophthalmic Opticians (Optometrists). (2017) 37:385–98. doi: 10.1111/opo.12388
20. Wang ST, Wang YY, Wang DJ, Yin YQ, Wang YZ, and Jin YC. An improved random forest-based rule extraction method for breast cancer diagnosis. Appl Soft Comput. (2020) 86:105941. doi: 10.1016/j.asoc.2019.105941
21. Guo L, Wang Z, Du Y, Mao J, Zhang J, Yu Z, et al. Random-forest algorithm based biomarkers in predicting prognosis in the patients with hepatocellular carcinoma. Cancer Cell Int. (2020) 20:251. doi: 10.1186/s12935-020-01274-z
22. Liu Y, Xu Y, Yang X, Miao G, Wu Y, and Yang S. The prevalence of anxiety and its key influencing factors among the elderly in China. Front Psychiatry. (2023) 14:1038049. doi: 10.3389/fpsyt.2023.1038049
23. Hu JC and Szymczak S. A review on longitudinal data analysis with random forest. Briefings Bioinf. (2023) 24(2):1–11. doi: 10.1093/bib/bbad002
24. Hou NZ, Li MZ, He L, Xie B, Wang L, Zhang RM, et al. Predicting 30-days mortality for mimic-iii patients with sepsis-3: A machine learning approach using Xgboost. J Trans Med. (2020) 18(1):462. doi: 10.1186/s12967-020-02620-5
25. Doya K, Friston K, Sugiyama M, and Tenenbaum J. Neural networks special issue on artificial intelligence and brain science. Neural Networks. (2022) 155:328–9. doi: 10.1016/j.neunet.2022.08.018
26. Zheng Z. Twenty years’ Follow-up on elder people’s health and quality of life. China Popul Dev Stud. (2020) 3:297–309. doi: 10.1007/s42379-020-00045-7
27. Chinese longitudinal healthy longevity survey. Available online at: https://opendata.pku.edu.cn/dataverse/CHADS. (Accessed January 25, 2024)
28. Spitzer RL, Kroenke K, Williams JBW, and Löwe B. A brief measure for assessing generalized anxiety disorder -: the Gad-7. Arch Internal Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
29. Huang M, Liu K, Liang C, Wang Y, and Guo Z. The relationship between living alone or not and depressive symptoms in older adults: A parallel mediation effect of sleep quality and anxiety. BMC Geriatr. (2023) 23(1):506. doi: 10.1186/s12877-023-04161-0
30. Zhang P, Wang L, Zhou Q, Dong X, Guo Y, Wang P, et al. A network analysis of anxiety and depression symptoms in Chinese disabled elderly. J Affect Disord. (2023) 333:535–42. doi: 10.1016/j.jad.2023.04.065
31. Xue SP, Lu AT, Chen WY, Li JY, Ke XY, and An YN. A latent profile analysis and network analysis of anxiety and depression symptoms in Chinese widowed elderly. J Affect Disord. (2024) 366:172–80. doi: 10.1016/j.jad.2024.08.181
32. Correction: transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (Tripod): the tripod statement. Ann Internal Med. (2015) 162:600. doi: 10.7326/l15-0078-4
33. Chen XD, Lin SW, Zheng YX, He LX, and Fang Y. Long-term trajectories of depressive symptoms and machine learning techniques for fall prediction in older adults: evidence from the China health and retirement longitudinal study (Charls). Arch Gerontol Geriatr. (2023) 111:105012. doi: 10.1016/j.archger.2023.105012
34. Chen Z, Ying TC, Chen J, Wang Y, Wu C, and Su Z. Assessment of renal fibrosis in patients with chronic kidney disease using shear wave elastography and clinical features: A random forest approach. Ultrasound Med Biol. (2023) 49:1665–71. doi: 10.1016/j.ultrasmedbio.2023.03.024
35. Grömping U. Variable importance assessment in regression: linear regression versus random forest. Am Stat. (2009) 63:308–19. doi: 10.1198/tast.2009.08199
36. Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. The lancet Psychiatry. (2019) 6(3):211–24.
37. Eramudugolla R, Wood J, and Anstey KJ. Co-morbidity of depression and anxiety in common age-related eye diseases: A population-based study of 662 adults. Front Aging Neurosci. (2013) 5:56. doi: 10.3389/fnagi.2013.00056
38. Evans J R FAE and Wormald RPL. Depression and anxiety in visually impaired older people. Ophthalmology. (2007) 114:283–8. doi: 10.1016/j.ophtha.2006.10.006
39. Gao X, Geng T, Jiang M, Huang N, Zheng Y, Belsky DW, et al. Accelerated biological aging and risk of depression and anxiety: evidence from 424,299 Uk biobank participants. Nat Commun. (2023) 14:2277. doi: 10.1038/s41467-023-38013-7
40. Rutherford BR, Taylor WD, Brown PJ, Sneed JR, and Roose SP. Biological aging and the future of geriatric psychiatry. J Gerontol Ser A Biol Sci Med Sci. (2017) 72:343–52. doi: 10.1093/gerona/glw241
41. Picard M, Trumpff C, and Burelle Y. Mitochondrial psychobiology: foundations and applications. Curr Opin Behav Sci. (2019) 28:142–51. doi: 10.1016/j.cobeha.2019.04.015
42. Carstensen LL. Social and emotional patterns in adulthood: support for socioemotional selectivity theory. Psychol Aging. (1992) 7:331–8. doi: 10.1037//0882-7974.7.3.331
43. Charles ST and Piazza JR. Memories of social interactions: age differences in emotional intensity. Psychol Aging. (2007) 22:300–9. doi: 10.1037/0882-7974.22.2.300
44. Birditt KS and Fingerman KL. Age and gender differences in adults’ Descriptions of emotional reactions to interpersonal problems. J Gerontol B Psychol Sci Soc Sci. (2003) 58:P237–45. doi: 10.1093/geronb/58.4.p237
45. Gariepy G, Nitka D, and Schmitz N. The association between obesity and anxiety disorders in the population: A systematic review and meta-analysis. Int J Obes. (2010) 34:407–19. doi: 10.1038/ijo.2009.252
46. Carr D and Friedman MA. Is obesity stigmatizing? Body weight, perceived discrimination, and psychological well-being in the United States. J Health Soc Behav. (2005) 46:244–59. doi: 10.1177/002214650504600303
47. Kolotkin RL, Meter K, and Williams GR. Quality of life and obesity. Obes Rev: an Off J Int Assoc Study Obes. (2001) 2:219–29. doi: 10.1046/j.1467-789x.2001.00040.x
48. Seravalle G and Grassi G. Obesity and hypertension. Pharmacol Res. (2017) 122:1–7. doi: 10.1016/j.phrs.2017.05.013
49. Golay A and Ybarra J. Link between obesity and type 2 diabetes. Best Pract Res Clin Endocrinol Metab. (2005) 19:649–63. doi: 10.1016/j.beem.2005.07.010
50. Torres SJ and Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. (2007) 23:887–94. doi: 10.1016/j.nut.2007.08.008
51. Hill D, Conner M, Clancy F, Moss R, Wilding S, Bristow M, et al. Stress and eating behaviours in healthy adults: A systematic review and meta-analysis. Health Psychol Rev. (2022) 16:280–304. doi: 10.1080/17437199.2021.1923406
52. Hiller R, Podgor MJ, Sperduto RD, Nowroozi L, Wilson PW, D’Agostino RB, et al. A longitudinal study of body mass index and lens opacities. Framingham Stud Ophthalmol. (1998) 105:1244–50. doi: 10.1016/s0161-6420(98)97029-4
53. Reinwarth AC, Wicke FS, Hettich N, Ernst M, Otten D, Brähler E, et al. Self-rated physical health predicts mortality in aging persons beyond objective health risks. Sci Rep. (2023) 13:19531. doi: 10.1038/s41598-023-46882-7
54. Xie Q, Xu YM, and Zhong BL. Anxiety symptoms in older Chinese adults in primary care settings: prevalence and correlates. Front Public Health. (2022) 10:1009226. doi: 10.3389/fpubh.2022.1009226
55. Östberg D and Nordin S. Three-year prediction of depression and anxiety with a single self-rated health item. J Ment Health (Abingdon England). (2022) 31:402–9. doi: 10.1080/09638237.2021.2022610
56. Said MA, Thangiah G, Abdul Majid H, Ismail R, Maw Pin T, Rizal H, et al. Income disparity and mental wellbeing among adults in semi-urban and rural areas in Malaysia: the mediating role of social capital. Int J Environ Res Public Health. (2022) 19(11):660. doi: 10.3390/ijerph19116604
57. Yang H, Deng Q, Geng Q, Tang Y, Ma J, Ye W, et al. Association of self-rated health with chronic disease, mental health symptom and social relationship in older people. Sci Rep. (2021) 11:14653. doi: 10.1038/s41598-021-94318-x
58. Mojtabai R, Stuart EA, Hwang I, Susukida R, Eaton WW, Sampson N, et al. Long-term effects of mental disorders on employment in the national comorbidity survey ten-year follow-up. Soc Psychiatry Psychiatr Epidemiol. (2015) 50:1657–68. doi: 10.1007/s00127-015-1097-z
59. Głąbska D, Guzek D, Groele B, and Gutkowska K. Fruit and vegetable intake and mental health in adults: A systematic review. Nutrients. (2020) 12(1):115. doi: 10.3390/nu12010115
60. Short NA, Ennis CR, Oglesby ME, Boffa JW, Joiner TE, and Schmidt NB. The mediating role of sleep disturbances in the relationship between posttraumatic stress disorder and self-injurious behavior. J Anxiety Disord. (2015) 35:68–74. doi: 10.1016/j.janxdis.2015.09.004
61. Olatunji BO, Cisler JM, and Tolin DF. Quality of life in the anxiety disorders: A meta-analytic review. Clin Psychol Rev. (2007) 27:572–81. doi: 10.1016/j.cpr.2007.01.015
62. Blazer DG and Tucci DL. Hearing loss and psychiatric disorders: A review. psychol Med. (2019) 49:891–7. doi: 10.1017/s0033291718003409
Keywords: anxiety symptoms, cataracts, influencing factors, random forest, mental health
Citation: Zhang F, Li X, Liu K, Xie L, Wan L, Cao S, Fu Y and Niu T (2025) Prevalence and main factors influencing anxiety symptoms in Chinese older adults with cataracts: a national cross-sectional survey. Front. Psychiatry 16:1534863. doi: 10.3389/fpsyt.2025.1534863
Received: 26 November 2024; Accepted: 06 May 2025;
Published: 02 June 2025.
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Ayman Mohamed El-Ashry, Al Jouf University, Saudi ArabiaZainol Akbar Zainal, National University of Malaysia, Malaysia
Copyright © 2025 Zhang, Li, Liu, Xie, Wan, Cao, Fu and Niu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tengfei Niu, bml1dGVuZ2ZlaTE5ODYwMzI4QDEyNi5jb20=
 Fadong Zhang1
Fadong Zhang1 Xiang Li
Xiang Li Shiwei Cao
Shiwei Cao Tengfei Niu
Tengfei Niu