- Department of Human Neuroscience, Unit of Child and Adolescent Neuropsychiatry, Sapienza University of Rome, Rome, Italy
Background: Tourette Syndrome (TS) and chronic tic disorders (TD) are complex neuropsychiatric conditions often associated with comorbidities. Despite their prevalence, these disorders are frequently underdiagnosed and poorly managed due to limited healthcare access and lack of specialized services. An online survey was conducted in Italy to assess access to care and the impact of TS/TD on social, educational, and occupational life.
Method: A nationwide online survey, including 100 participants (mean age 23.1, SD 14.6; M:F=77:33), was developed to assess diagnostic-therapeutic processes and quality of life (QoL) in TS/TD. The survey had three sections: 1) Access to Care, 2) Tic Severity, and 3) Impact of TS/TD.
Results: Diagnosis was delayed by an average of 7.7 years. The lack of clear information was a major issue, with caregivers reporting easier access to information than youths and adults with TS/TD (p= .042, OR: 0.37). Pharmacological treatment was the most common (53% currently, 63% previously), while psychotherapy was more common among children and early adolescents (50%) compared to older participants (25.6%) (p= .037). Specialized cognitive-behavioral treatments, such as EPT and HRT, were rare, with only 7% receiving HRT and none undergoing EPT. Comorbidities had a significantly greater impact on QoL than tics (p= .004, Cohen’s d=0.3).
Conclusion: These findings highlight the need for improved access to specialized care, greater healthcare professional awareness, and enhanced support for individuals with TS/TD and their families, especially for early diagnosis and effective cognitive behavioral treatments.
1 Introduction
According to DSM V-TR criteria, Chronic Tic Disorders (CTDs) are neurodevelopmental conditions characterized by the presence of motor and/or vocal tics that persist for at least one year. These tics are sudden, repetitive, and non-rhythmic movements or vocalizations that fluctuate in severity over time. CTDs include Chronic Motor Tic Disorder (CMTD) and Chronic Vocal Tic Disorder (CVTD), distinguished by the presence of either motor or vocal tics, respectively, but not both (1).
Tourette Syndrome (TS) is a more complex tic disorder defined by the presence of both motor and vocal tics persisting for at least one year. TS is often associated with psychiatric comorbidities, including obsessive-compulsive disorder (OCD), attention-deficit/hyperactivity disorder (ADHD), and anxiety, which significantly impact quality of life (QoL) (2). The estimated overall prevalence of TS is 0.23% among all children and adolescents aged 0–17 years (3), and up to 4% for CTDs (4), with males being affected approximately three to four times more frequently than females (5).
The expression of TS can vary significantly among individuals and is frequently accompanied by high rates of comorbid conditions, observed in up to 90% of patients (6, 7). Notably, Attention Deficit Hyperactivity Disorder (ADHD) and Obsessive Compulsive Disorder (OCD) are the most common comorbidities associated with TD (6), however many patients also experience mood disorders, impulse control difficulties, self-injury, or socially inappropriate behaviors (8).
The intensity of tics often peaks in early adolescence, with many individuals experiencing a decline in both frequency and severity after puberty (8). However, approximately 20% of children with TD continue to exhibit moderate functional impairment as they transition into adulthood (9). Despite this, in many countries, a significant concern is the lack of continuity in specialized care during this transition, potentially impacting long-term outcomes (6).
TS/TD have been associated with an impairment in quality of life (QoL), leading to adverse psychological, behavioral, social, and academic outcomes (6, 10, 11). Increased severity of tics, accompanied by the presence of comorbid conditions, significantly contributes to these negative psychosocial effects (12). It is known that sleep disturbances, such as bedtime resistance and fragmented sleep, contribute to heightened physiological and psychological stress in individuals with TS/TD, exacerbating tic severity through increased stress and impaired emotional regulation (13). Also, recent studies suggest that elevated perceived stress and impaired family functioning are among the strongest predictors of reduced QoL in adolescents with TS/TD. Family dynamics, characterized by communication difficulties and decreased cohesion, along with heightened stress sensitivity, may exacerbate emotional and social distress, regardless of tic severity (14). Furthermore, experiences of stigmatization and social rejection can exacerbate challenges, limiting opportunities for developing friendships and essential social skills (6).
Another factor contributing to the reduced QoL in this population is the lack of adequate information regarding the diagnostic and therapeutic pathways (15, 16). This informational gap not only creates barriers to obtaining a timely diagnosis but also limits access to first-line treatments for tics, such as cognitive-behavioral therapy (15).
Studies in Canada (17), the United States (18), Spain (19), and Australia (20) echo similar challenges, noting that the diagnostic process for TS/TD is often lengthy and complex. Additionally, healthcare professionals lack knowledge about tics, and there is a shortage of qualified teams to manage TS/TD and its comorbidities (15, 20).
In light of these discussed concerns, a comprehensive survey across Italy was conducted to investigate access to care, and the accessibility of diagnostic and therapeutic processes in both the National Health Service (NHS) and private facilities. This survey will also assess the long-life impact of TS/TD on social interactions, educational and employment experiences, romantic relationships, and the presence of comorbid conditions.
2 Materials and methods
A comprehensive questionnaire was developed to assess various aspects of the therapeutic-diagnostic process for TS/TD. The survey was designed by experienced neurodevelopmental neuropsychiatrists (VB, SR, GDI) and subsequently revised in collaboration with representatives from family associations of individuals with TS/TD (Associazione Tourette Roma Onlus) to ensure a thorough exploration of relevant issues. The final instrument comprised two versions: a 40-item self-report questionnaire for adult participants and a 33-item caregiver-report questionnaire for patients under 18 years of age. In particular, adult respondents completed an assessment of the quality of the transition from pediatric to adult services.
The survey was administered anonymously via Google Forms and yielded 100 responses from across Italy between October and December 2024. The questionnaire was organized into three primary sections:
- Access to Care: Adapted from the European Patients’ Forum (EPF) report (15). This section evaluates challenges related to accessing care for individuals with TS/TD (15).
- Tic Severity Rating Scales: This section is an adaptation of the Yale Global Tic Severity Scale (YGTSS) (21).
- Impact of TS/TD: A self-developed section examining the influence on various facets of life, such as social relationships, educational and occupational challenges, romantic relationships (adults only), social stigma, diagnosed comorbidities, and details regarding current and past therapies.
Participants were recruited nationally through patient association websites, complemented by direct outreach to clinicians who agreed to participate. However, since this is a self-report survey and not all patients were directly recruited by clinicians, we have no way of verifying how the diagnosis of TS/TD was made for the entire sample (e.g., clinician-confirmed diagnosis of tic disorder by DSM-IV-TR criteria). The survey, available in English in the Supplementary Material (Appendix S2), was administered voluntarily without any compensation.
Baseline demographics and characteristics were summarized descriptively across groups using mean and standard deviation (SD) for continuous variables. Categorical variables were presented as frequencies and percentages. The analysis included inferential bivariate methods (t-test, chi-squared, Fisher’s test). All participants with complete data were included in the analyses (n = 100). For all comparisons, p-values less than 0.05 were considered statistically significant. Statistical analyses were performed using the Jamovi statistical software (version 2.3.28) based on the R language (22, 23).
3 Results
3.1 Description of the sample
The total sample consisted of 100 individuals, divided into patients (n 33) and caregivers (n 67) (Table 1). Participants were stratified into two age groups based on the WHO definition of youth and adolescence (19) using a 15-year threshold: children and adolescents (n 26) and youth and adults (n 74). This categorization was then applied in the statistical analyses to examine age-related differences. The demographic data are presented in Table 1.
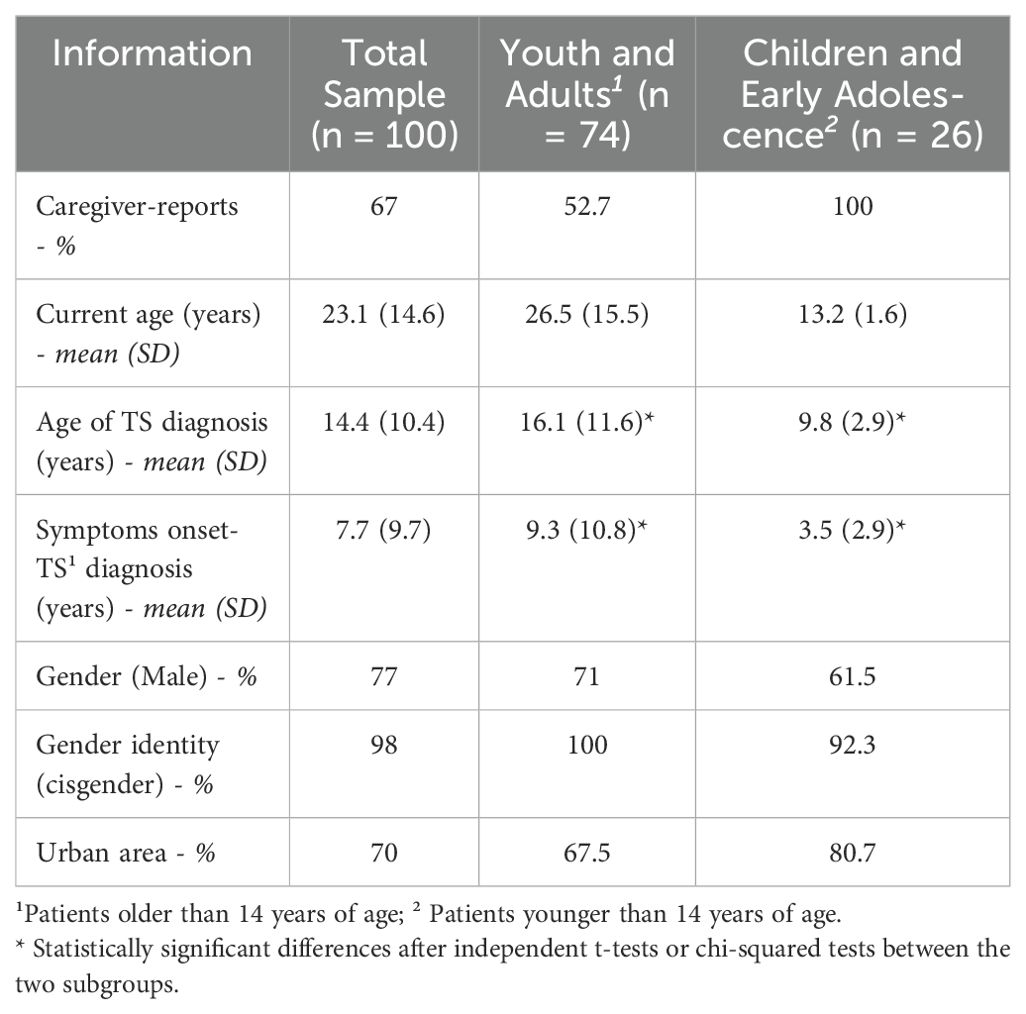
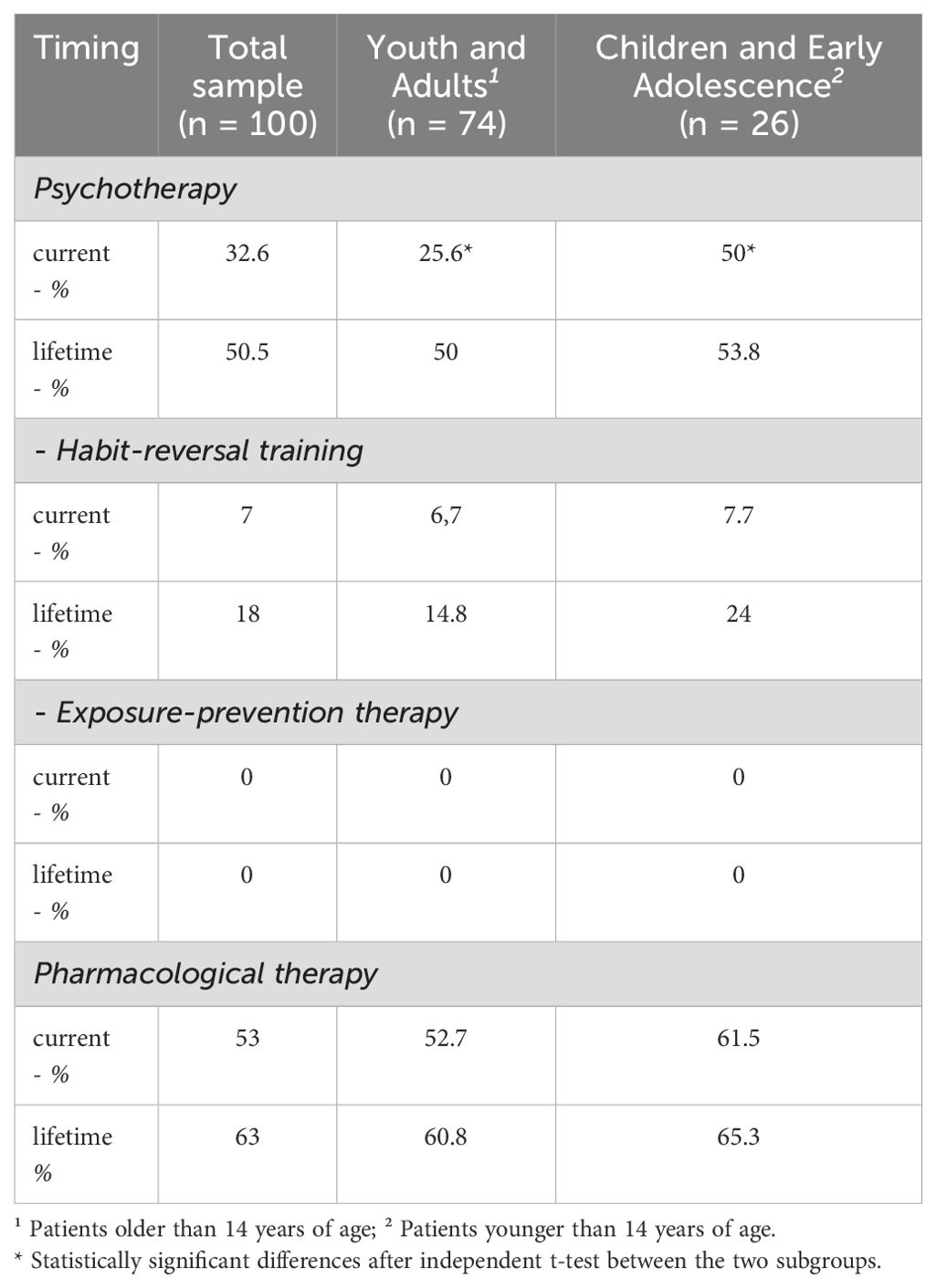
Table 1. Description of the sample divided into youth and adults and children and early adolescents.
The mean complexity score for tics was 1.42 (SD = 1.04; range 1–3, where 1 represents only simple tics and 3 represents severe tics) for motor tics and 1.17 (SD = 1.05; range 1–3) for vocal tics. Similarly, the mean disability score was 1.43 (SD = 1.20; range 0–4, where 0 represents no disability and 4 represents severe disability) for motor tics and 1.18 (SD = 1.03; range 0–4) for vocal tics. These scores were assessed using an adaptation of the YGTSS.
Independent t-tests indicated that youth and adults were diagnosed with TS/TD significantly later than children and adolescents (p = .012), and also experienced a longer delay between symptom onset and diagnosis (p = .011).
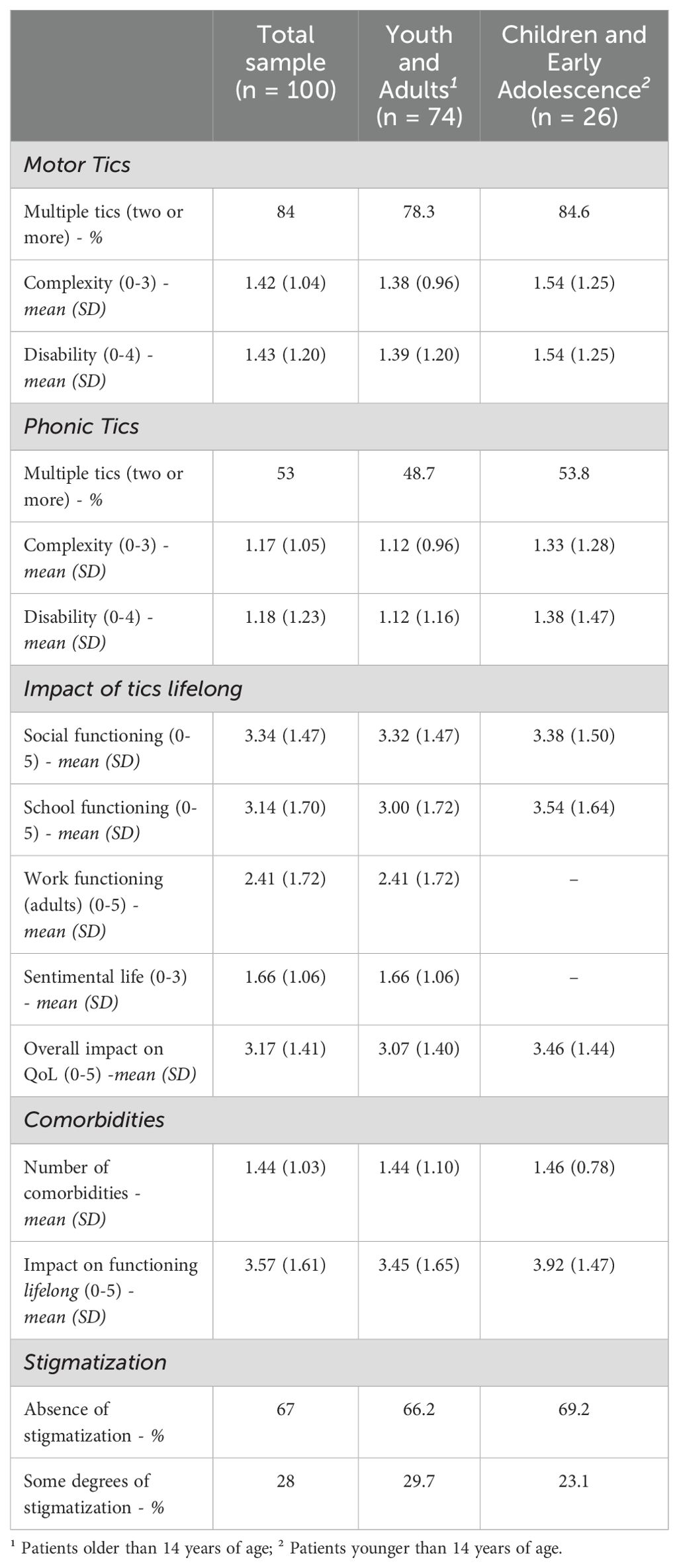
Most of the sample reported having some (39%) or great (19%) difficulties in covering medical expenses. (Figure 1B).
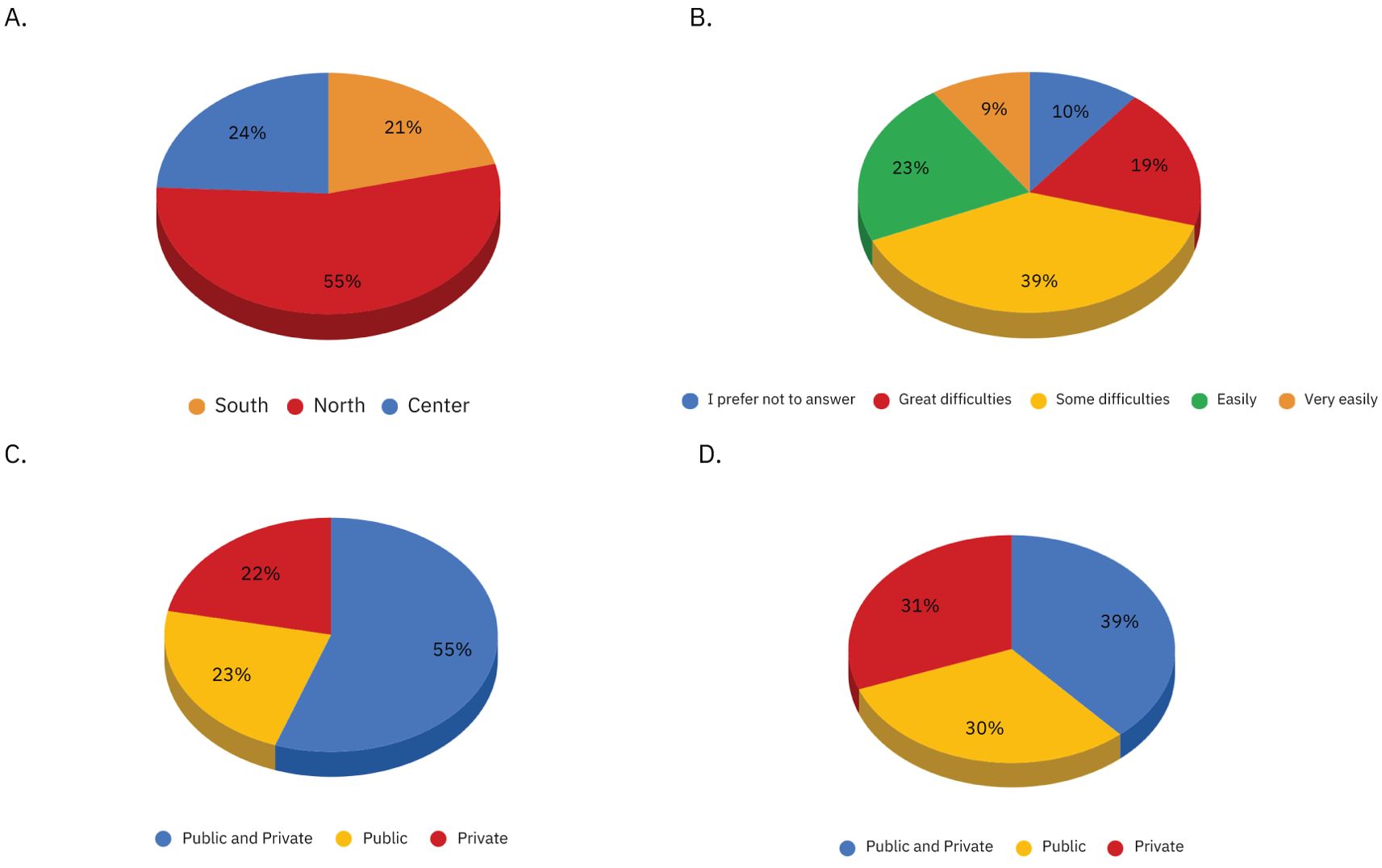
Figure 1. Figure shows the distributions of the following variables: (A) Geographical provenance of the sample, (B). Family budget, (C). Method of performing the diagnostic pathway: through the National Health System (NHS) or private facilities, (D). Method of performing the treatment course: through the National Health System (NHS) or private facilities.
Both established neuropsychiatric diagnoses and comorbid psychopathological symptoms were investigated. The most represented comorbid diagnoses within the sample were ADHD (49%), followed by mood disorder (45%). (Figure 2A).
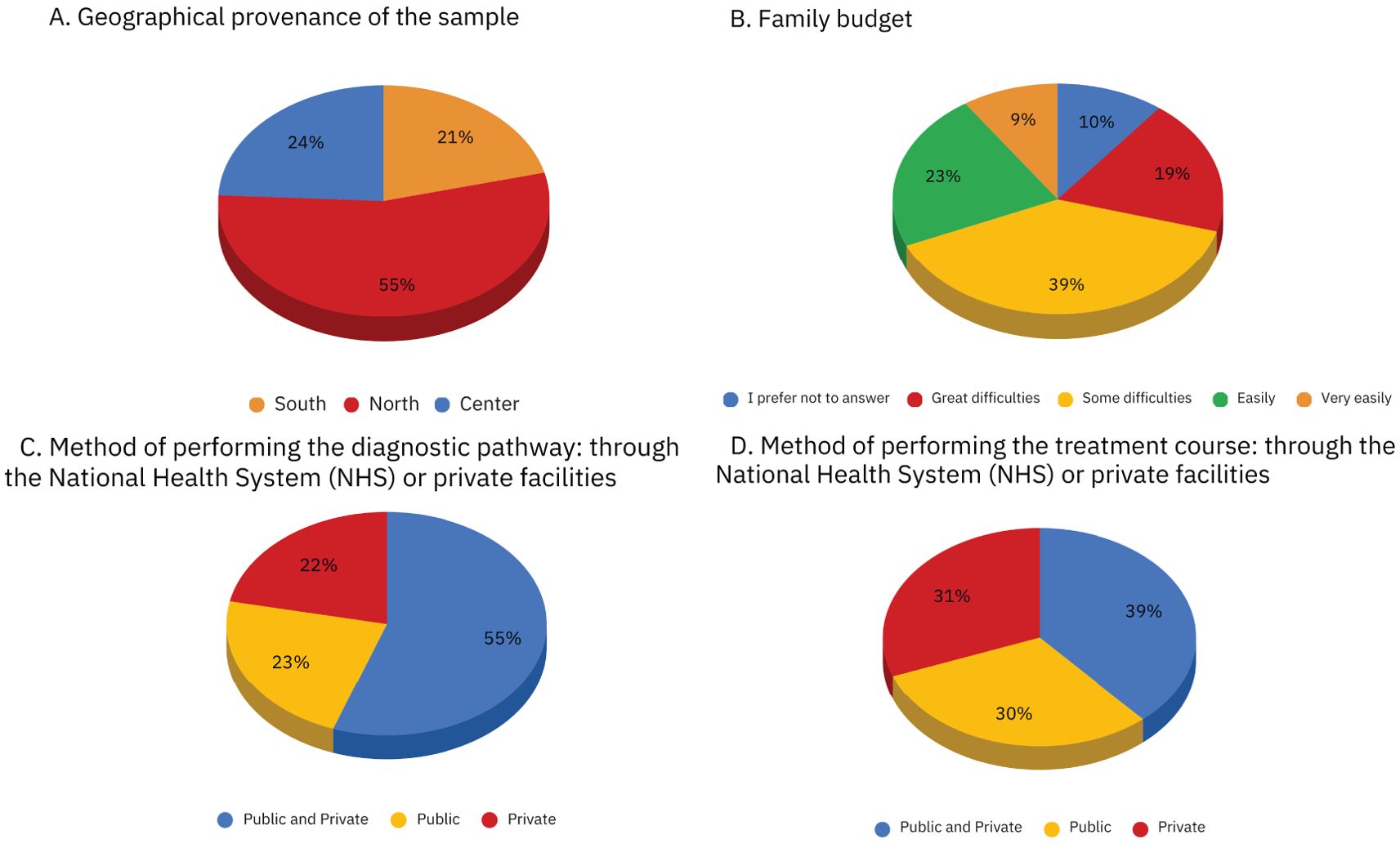
Figure 2. Graphs of the geographical proveneance, family budget, method of performing diagnostic and therapeutic pathway in our sample.
Supplementary Figure S1 (in the Supplementary Materials) shows the frequency of comorbid symptoms within the sample. The most represented were anxiety and depression (35%), followed by inattention (35%), and impulsivity (30%). Only 5% of the respondents reported no other symptomatology besides TS/TD.
3.2 Diagnostic/therapeutic process and access to care
More than half of the sample (55%) used both NHS and private facilities for the diagnosis. 23% used exclusively public facilities, while 22% used exclusively private facilities. (Figure 1C). With regard to the course of treatment, the sample appears to be more evenly distributed among those who used both public and private facilities (39%), those who relied exclusively on public care (30%), and those who used only private providers (31%). (Figure 1D).
The reasons why private facilities were chosen were also investigated, with most of the sample (62% for both diagnosis and therapy) reporting that public services for TS/TD were not available in their region. Other reasons are reported in Figures 3A, B. Table 2 presents data on how participants perceive the availability and clarity of information regarding the diagnostic and therapeutic process for TS/TD. The lack of clarity in available information is a major concern, despite caregivers reporting easier access to information than youths and adult participants with TS/TD (p= .042, OR: 0.37). The quality of the diagnostic and therapeutic process was perceived as moderate, with no significant difference emerging based on whether it was performed in a private or public setting (Table 2).
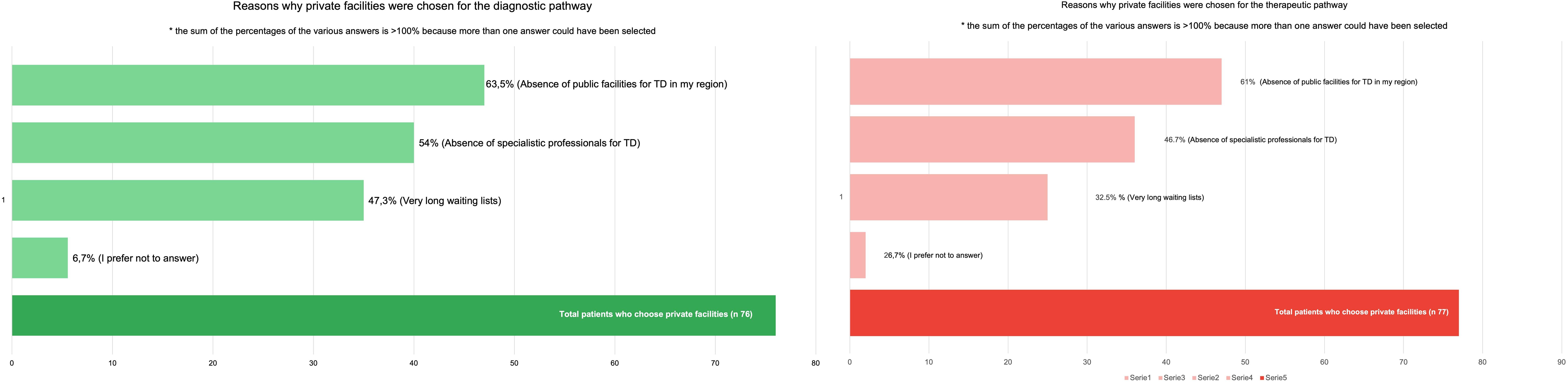
Figure 3. In this figure are showed all the reasons why our patients choose private facilities instead of public services.
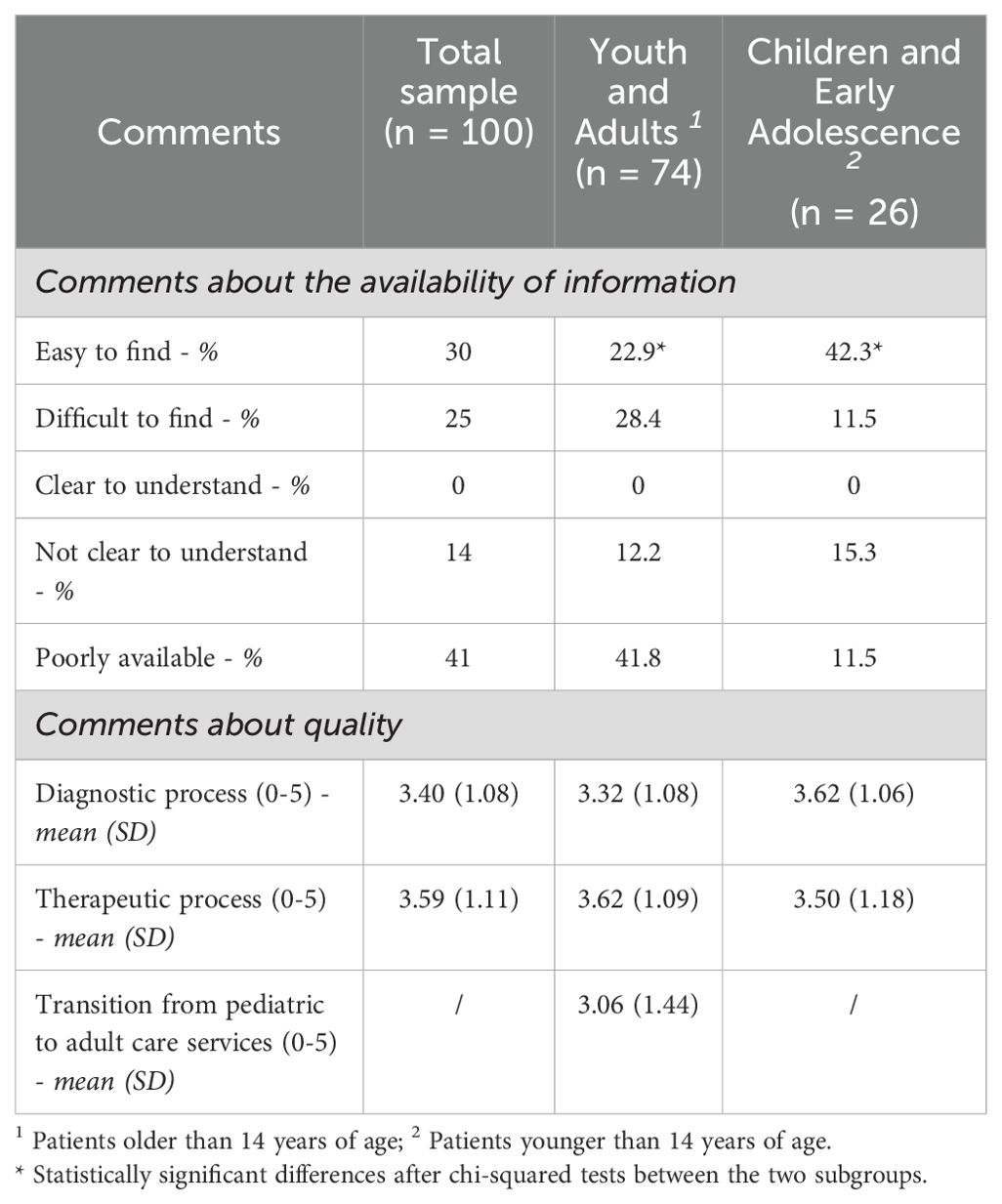
Table 2. Responses about the availability of information regarding the therapeutic-diagnostic process for Tourette syndrome and other tic disorders.
Additionally, adult patients were asked to rate the perceived difficulty of the transition from pediatric to adult care services. This transition was perceived as difficult by the majority of them (68.7%).
3.3 Lifetime therapeutic interventions
In our sample, pharmacological therapy was the most commonly received treatment, with over half of the total sample currently under treatment (53%), and an even higher percentage having received it in the past (63%). Currently, psychotherapy is more commonly received by children and early adolescents (50%) compared to youth and adults (25.6%) (p = .037). However, a similar percentage of youth/adults (50%) and children/adolescents (53.8%) had undergone psychotherapy at some point in their lives. Habit-reversal training (HRT) was relatively uncommon, with only 7% of the total sample currently receiving it. A higher percentage of children and early adolescents (24%) had received HRT in the past compared to youth and adults (14.8%). No participant reported ever having been subjected to Exposure-Prevention Therapy (EPT), either currently or in the past (Table 3).
3.4 Impact on functioning and quality of life
The principal features of tics are described in Table 4, showing no significant differences among the age groups. Tic symptoms significantly impacted the QoL across social, school, and work functioning, with similar effects across all ages, while sentimental life was less affected. The impact of comorbidities on QoL - despite being equally distributed between the age groups - was significantly more relevant than impact of tics on functioning (p= .004, Cohen’s d=0.3).
Furthermore, no significant correlations were found between stigma and other variables, such as age, comorbidities, overall impact of tics, impact of comorbidities, and tic severity. Notably, 67% of our sample did not refer to being a victim of social stigmatization.
4 Discussion
Access to timely and specialized care is a critical factor influencing the diagnostic and therapeutic journey of individuals with TS/TD. Despite the availability of public healthcare, many families seek private services, often due to limited specialized resources and long waiting times. These barriers contribute to diagnostic delays and deviations from recommended treatment guidelines, ultimately impacting patients’ QoL and long-term outcomes.
4.1 Diagnostic process and accessibility to care
Access to care — defined as the ease of accessing health services in terms of geographical distribution, cost, time, and workforce availability (24) — is a crucial factor affecting TS/TD patients and their families, starting from the very first step of their journey: obtaining a diagnosis.
Despite the NHS offering free or low-cost public healthcare, only 23% of our sample relied exclusively on NHS facilities for diagnosis. Instead, the majority of families sought care from private providers or a combination of public and private services. This preference for private healthcare is particularly striking given the financial constraints reported by many families, with nearly 58% experiencing some degree of economic hardship in accessing care. These findings align with data from the European Patients’ Forum (15), which indicates that 60% of patients encounter financial barriers to healthcare, particularly those with multiple comorbidities (15).
Interestingly, despite the widespread use of private healthcare, there were no significant differences in the perceived quality of these services compared to public facilities. Our findings suggest that the primary motivation for choosing private providers is the lack of adequate public facilities for this specific condition. Existing literature further highlights persistent challenges in securing timely and affordable care for individuals with TS/TD, likely due to the limited availability of specialized services and trained professionals within the public healthcare sector (17, 25).
These challenges are further exacerbated by the lack of clear and accessible information regarding diagnostic procedures. Indeed, this was a significant concern for most respondents to our survey, with no participants finding the information entirely clear or easy to understand. However, caregivers reported fewer difficulties accessing information for their children than adult patients. This discrepancy may be attributed to generational differences, as information about TS/TD has likely become more widely available in recent years, facilitating access to appropriate care for parents of children with TS/TD (25). Previous studies (11, 24) investigated these topics and reported that the most frequent concerns were lack of transparency regarding costs, poor accessibility for people with disabilities, and difficulties in understanding diagnostic/therapeutic procedures (11, 25). Additionally, an analysis of widely used patient information leaflets on TS/TD identified several limitations, including the absence of explicit recommendations to consult a neuropsychiatrist for diagnostic evaluation (26).
The challenges associated with accessing the diagnostic process for TS/TD have significant negative consequences, primarily contributing to prolonged delays between symptom onset, initial clinical consultation, and final diagnosis. In our sample, the mean time from symptom onset to a formal TS/TD diagnosis was 7.7 years, consistent with previous studies reporting diagnostic delays ranging from 3 to 8 years (25). This delay could be explained also by the initial misdiagnosis with other neurodevelopmental disorders, behavioral problems (27) or pediatric conditions (e.g. asthma or allergies) (28). Notably, this delay was more pronounced in older patients, with an average of 9.3 years compared to 3.5 years in younger patients which is consistent with available literature (29).
4.2 Lifetime therapeutic interventions
Clinical guidelines for the treatment of TS/TD advocate a stepwise approach, with psychoeducation and behavioral interventions as first-line strategies and pharmacotherapy reserved for third-line use (16). However, in our sample, only about 50% of individuals have undergone psychotherapy—and notably, none received specific intervention for TS/TD such as EPT. Among those who never received any psychotherapeutic intervention, 13.4% were treated exclusively with medication. This deviation from the guidelines suggests that treatment choices are probably driven by the immediate availability and perceived convenience of pharmacological options, rather than the structured, time-intensive nature of behavioral therapies (30, 31). Moreover, barriers such as limited access to well-trained practitioners, high costs of psychotherapy, and insufficient patient education further contribute to this practice (26, 32).
4.3 Quality of life: the impact of tics and comorbidities
The impact of tics on global QoL—including social, academic, occupational, and sentimental functioning—was assessed, showing significant impairment in patients with TS/TD. All domains were similarly affected, with comparable distribution across age groups. Previous studies suggested that children with TS/TD experience higher rates of social difficulties, such as bullying, peer rejection, and challenges in forming and maintaining friendships compared to neurotypical peers (6). In this context, it is important to consider the role of comorbidities, which often exacerbate social difficulties in children with TS/TD (33). In our cohort, the most common comorbidity was ADHD, followed by mood disorders. Anxiety and depression were the most frequent comorbid symptoms, followed by inattention and impulsivity. Only five patients reported no additional symptoms, underlining the high prevalence of concurrent conditions in TS/TD (7, 34). The impact of comorbidities on overall functioning was perceived as high, with their effect on QoL being more pronounced than the global impact of tics, as shown in previous studies (35, 36), which underscores the substantial burden of comorbidities in TS/TD (37).
Another important issue is that TS/TD is frequently misunderstood, leading to social stigma and discrimination. This phenomenon is not only prevalent in social contexts but also among healthcare professionals, who may hold unhelpful beliefs about the condition (38). In our survey, nearly 30% experienced inappropriate comments or behaviors; however these occurrences might have been underestimated in caregiver reports.
Finally, the transition from child and adolescent neuropsychiatry to adult services also was perceived as a significant challenge within our population. The majority of individuals reported having faced some or great difficulties in continuing their care after reaching adulthood, due to complex bureaucracy. Previous studies suggested that the transition from child to adult healthcare services is often poorly planned and executed, leading to challenges such as lack of continuity, inadequate support, and increased anxiety, highlighting the need for improved transition models and psychological interventions (39).
5 Limitation and future directions
Although all participants reported receiving a diagnosis of TS or TD from a specialist, the self-reported nature of our survey prevents us from verifying the specific diagnostic criteria used in each case.
Patients were not selected based on their primary diagnosis because comorbidities, which can significantly impact functional outcomes, may be underreported in self-report surveys. Excluding individuals with some kind of comorbidities could have overlooked those with TS/TD who experience a greater negative impact on their QoL due to these conditions.
In our sample, the child and adolescent population was less represented, limiting the possibility of generalizing the results obtained in this age group. Further studies on a larger sample might make it possible to overcome this limitation.
For future research, it would be beneficial to adopt a more precise patient stratification, potentially by focusing solely on individuals diagnosed by clinicians. This would also allow psychiatric and internal medicine comorbidities to be investigated more accurately, as well as the different types of drug therapy administered. However, this approach could limit the survey’s reach and unintentionally disadvantage patients who face greater challenges in accessing specialist care—a group that was notably represented in our study.
6 Conclusion
Our study underscores significant barriers to accessing specialized care for individuals with TS/TD, despite the availability of public healthcare in our country. Limited specialized services, financial constraints, and unclear diagnostic information contribute to prolonged diagnostic delays—particularly among older patients—and drive many families to seek private care.
Notably, deviations from clinical guidelines are relevant: only about half of the patients received psychotherapy during their lifetime, while a notable proportion relied exclusively on pharmacotherapy. This pattern suggests that treatment choices are more influenced by the immediate availability of medication than by evidence-based, stepwise interventions. Of particular significance, the use of specialized cognitive-behavioral interventions for TS/TD — specifically, EPT and HRT — was exceedingly rare, with only 7% of patients receiving HRT and none undergoing EPT, regardless of geographic location.
Finally, the substantial impact of TS/TD on QoL, compounded by frequent comorbidities and challenges in transitioning from pediatric to adult services, highlights the urgent need for improved care models, enhanced provider training, and better patient education to facilitate timely diagnosis and effective, integrated treatment strategies.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
VB: Conceptualization, Data curation, Writing – review & editing. DE: Formal Analysis, Methodology, Writing – review & editing. IN: Investigation, Visualization, Writing – original draft. GD: Conceptualization, Data curation, Writing – review & editing. SR: Conceptualization, Data curation, Formal Analysis, Writing – original draft. FP: Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors would like to express our sincere gratitude to the Associazione Tourette Roma Onlus (https://www.touretteroma.it/) for their invaluable support throughout this study. In particular, we extend our heartfelt thanks to Fabiola Oliva and Lucia Masullo for their exceptional assistance and dedication, which greatly contributed to the success of this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1581666/full#supplementary-material
References
1. Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed., text rev.; DSM-5-TR). Washington, DC: American Psychiatric Publishing (2022).
2. Conte G, Costanza C, Novelli M, Scarselli V, Arigliani E, Valente F, et al. Comorbidities and disease duration in tourette syndrome: impact on cognition and quality of life of children. Children. (2024) 11:226. doi: 10.3390/children11020226
3. Xiong Y, O’Brien M, Yang W, Zang X, Bao W, Xu G. Prevalence of Tourette syndrome among children and adolescents in the United States, 2016–2022. BMC Public Health. (2024) 24:2699. doi: 10.1186/s12889-024-20216-2
4. Bihun EC, Iverson A, Ranck SA, Grossen S, Ding J, Greene DJ, et al. Tic prevalence by direct observation in an elementary school(2022). Available online at: https://osf.io/bv86n (Accessed February 19, 2025).
5. Hu SJ, Li Y, Yang QH, Yang K, Jun JH, Cui YH, et al. Family functioning mediation in tic severity and quality of life for children with Tourette syndrome. World J Psychiatry. (2024) 14:1641–51. doi: 10.5498/wjp.v14.i11.1641
6. O’Hare D, Eapen V, Helmes E, McBain K, Reece J, Grove R. Factors impacting the quality of peer relationships of youth with Tourette’s syndrome. BMC Psychol december. (2015) 3:34. doi: 10.1186/s40359-015-0090-3
7. Cavanna AE, Purpura G, Riva A, Nacinovich R. Co-morbid tics and stereotypies: a systematic literature review. Neurol Sci. (2024) 45:477–83. doi: 10.1007/s10072-023-07095-y
8. Kompoliti K. Sources of disability in tourette syndrome: children vs. Adults. Tremor Hyperkinetic Mov. (2016). doi: 10.5334/tohm.270
9. Liu S, Zheng L, Zheng X, Zhang X, Yi M, Ma X. The subjective quality of life in young people with tourette syndrome in China. J Atten Disord. (2017) 21:426–32. doi: 10.1177/1087054713518822
10. Cavanna AE, Servo S, Monaco F, Robertson MM. The Behavioral Spectrum of Gilles de la Tourette Syndrome. J Neuropsychiatry Clin Neurosci. (2009) 21:13–23. doi: 10.1176/jnp.2009.21.1.13
11. Conelea CA, Woods DW, Zinner SH, Budman C, Murphy T, Scahill LD, et al. Exploring the impact of chronic tic disorders on youth: results from the tourette syndrome impact survey. Child Psychiatry Hum Dev. (2011) 42:219–42. doi: 10.1007/s10578-010-0211-4
12. Budman CL, Rockmore L, Stokes J, Sossin M. Clinical phenomenology of episodic rage in children with Tourette syndrome. J Psychosom Res. (2003) 55:59–65. doi: 10.1016/S0022-3999(02)00584-6
13. Li N, Hong X, Cui Y, Li Y. Clinical tics and quality of life in children and adolescents with tic disorders: The mediating role of sleep. Sleep Med. (2024) 124:217–22. doi: 10.1016/j.sleep.2024.09.030
14. Watson KH, Eckland M, Schwartzman JM, Molnar A, Boon W, Hiller M, et al. The association of quality of life with psychosocial factors in adolescents with tourette syndrome. Child Psychiatry Hum Dev. (2024). https://link.springer.com/10.1007/s10578-023-01656-0.
15. European Patients Forum. Access to healthcare EPF’s survey – final report(2016). Available online at: http://chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://www.eu-patient.eu/globalassets/policy/access/final-access-survey-report_16-dec.pdf (Accessed February 19, 2025).
16. Bhikram T, Elmaghraby R, Abi-Jaoude E, Sandor P. An international survey of health care services available to patients with tourette syndrome. Front Psychiatry. (2021) 12:621874. doi: 10.3389/fpsyt.2021.621874
17. Munce SEP, Pitzul KB, Guilcher SJT, Bereket T, Kwan M, Conklin J, et al. Health and community-based services for individuals with neurological conditions. Can J Neurol Sci. (2017) 44:670–5. doi: 10.1017/cjn.2017.207
18. Wolicki SB, Bitsko RH, Danielson ML, Holbrook JR, Zablotsky B, Walkup JT, et al. Children with tourette syndrome in the United States: parent-reported diagnosis, co-occurring disorders, severity, and influence of activities on tics. J Dev Behav Pediatr. (2019) 40:407–14. doi: 10.1097/DBP.0000000000000667
19. Rivera-Navarro J, Cubo E, Almazán J. The diagnosis of tourette’s syndrome: communication and impact. Clin Child Psychol Psychiatry. (2009) 14:13–23. doi: 10.1177/1359104508100127
20. Efron D, Payne J, Gulenc A, Chan E. Assessment and management of tic disorders and Tourette syndrome by Australian paediatricians. J Paediatr Child Health. (2020) 56:136–41. doi: 10.1111/jpc.14541
21. Leckman JF, Riddle MA, Hardin MT, Ort SI, Swartz KL, Stevenson J, et al. The yale global tic severity scale: initial testing of a clinician-rated scale of tic severity. J Am Acad Child Adolesc Psychiatry. (1989) 28:566–73. doi: 10.1097/00004583-198907000-00015
22. The jamovi project. jamovi (Version 2.5)(2024). Available online at: https://www.jamovi.org (Accessed 20 December 2024).
23. R: A Language and Environment for Statistical Computing, version 4.1; Computer Software; R Packages Retrieved from MRAN Snapshot 2022-01-01 (2021). Vienna, Austria: R Core Team. Available online at: https://cran.r-project.org (Accessed 20 December 2024).
24. Gulliford M, Figueroa-Munoz J, Morgan M, Hughes D, Gibson B, Beech R, et al. What does «access to health care» mean? J Health Serv Res Policy. (2002) 7:186–8. doi: 10.1258/135581902760082517
25. Travis E, Juarez-Paz AVO. Experiences of tourette syndrome caregivers with supportive communication. Qual Health Res. (2020) 30:1480–90. doi: 10.1177/1049732320915444
26. Cavanna AE, Hale O. 18 What information is provided to patients with tourette syndrome? J Neurol Neurosurg Psychiatry. (2017) 88:A34.2–A35.
27. Shilon Y, Pollak Y, Benarroch F, Gross-Tsur V. Factors influencing diagnosis delay in children with Tourette syndrome. Eur J Paediatr Neurol. (2008) 12:398–400. doi: 10.1016/j.ejpn.2007.10.006
28. Wand R, Shady G, Broder R, Furer P, Staley D. Tourette syndrome: Issues in diagnosis. Neurosci Biobehav Rev. (1992) 16:449–51. doi: 10.1016/S0149-7634(05)80186-1
29. Billnitzer A, Jankovic J. Current management of tics and tourette syndrome: behavioral, pharmacologic, and surgical treatments. Neurotherapeutics. (2020) 17:1681–93. doi: 10.1007/s13311-020-00914-6
30. Capriotti MR, Himle MB, Woods DW. Behavioral treatments for Tourette syndrome. J Obsessive-Compuls Relat Disord. (2014) 3:415–20. doi: 10.1016/j.jocrd.2014.03.007
31. Scahill L, Specht M, Page C. The prevalence of tic disorders and clinical characteristics in children. J Obsessive-Compuls Relat Disord. (2014) 3:394–400. doi: 10.1016/j.jocrd.2014.06.002
32. O’Hare D, Helmes E, Reece J, Eapen V, McBain K. The differential impact of tourette’s syndrome and comorbid diagnosis on the quality of life and functioning of diagnosed children and adolescents. J Child Adolesc Psychiatr Nurs. (2016) 29:30–6.
33. Bloch MH, Leckman JF. Clinical course of Tourette syndrome. J Psychosom Res. (2009) 67:497–501. doi: 10.1016/j.jpsychores.2009.09.002
34. Eddy CM, Cavanna AE, Gulisano M, Agodi A, Barchitta M, Calì P, et al. Clinical correlates of quality of life in Tourette syndrome. Mov Disord. (2011) 26:735–8. doi: 10.1002/mds.23434
35. Eapen V, Cavanna AE, Robertson MM. Comorbidities, social impact, and quality of life in tourette syndrome. Front Psychiatry. (2016) 7:97/abstract. doi: 10.3389/fpsyt.2016.00097/abstract
36. Martindale JM, Ringheanu VM, Pring KA, Norona S, Wiseman K, Strowd RE, et al. Study protocol for measuring stigmatization in persistent tic disorders: development and validation of the Tourette discrimination-stigmatization scale. Front Psychol. (2024) 15:1381063. doi: 10.3389/fpsyg.2024.1381063
37. Hart LC. Improving transition to adult care for those with developmental disabilities: an unclear path. Pediatrics. (2020) 146:e2020024398. doi: 10.1542/peds.2020-024398
38. Hollis C, Pennant M, Cuenca J, Glazebrook C, Kendall T, Whittington C, et al. Clinical effectiveness and patient perspectives of different treatment strategies for tics in children and adolescents with Tourette syndrome: a systematic review and qualitative analysis. Health Technol Assess. (2016) 20:1–450. doi: 10.3310/hta20040
39. Francés L, Caules J, Ruiz A, Soler CV, Hervás A, Fernández A, et al. An approach for prevention planning based on the prevalence and comorbidity of neurodevelopmental disorders in 6-year-old children receiving primary care consultations on the island of Menorca. BMC Pediatr. (2023) 23:32. doi: 10.1186/s12887-023-03844-2
Keywords: Tourette syndrome, tics, healthcare, quality of life, stigma, access to care
Citation: Baglioni V, Esposito D, Notaristefano I, Di Iorio G, Romano S and Pisani F (2025) Growing up with tic disorders: an Italian survey on quality of life and access to care. Front. Psychiatry 16:1581666. doi: 10.3389/fpsyt.2025.1581666
Received: 22 February 2025; Accepted: 14 April 2025;
Published: 13 May 2025.
Edited by:
Renata Rizzo, University of Catania, ItalyReviewed by:
Valeria Sajin, Asklepios Klinik St.Georg, GermanyAdriana Prato, University of Messina, Italy
Copyright © 2025 Baglioni, Esposito, Notaristefano, Di Iorio, Romano and Pisani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: S. Romano, c2FyYS5yb21hbm9AdW5pcm9tYTEuaXQ=
†These authors have contributed equally to this work
 V. Baglioni
V. Baglioni D. Esposito†
D. Esposito† I. Notaristefano
I. Notaristefano G. Di Iorio
G. Di Iorio S. Romano
S. Romano F. Pisani
F. Pisani