- 1Neuropsychiatry Department, Okasha Institute of Psychiatry, Ain Shams University, Cairo, Egypt
- 2Department of Addiction, Erada Complex and Mental Health in Dammam, Easter Health Cluster, Dammam, Saudi Arabia
Background: Methamphetamine use disorder (MUD) is linked to a variety of cognitive and neuropsychiatric deficits. One of the illegal substances that is most frequently abused is cannabis. The general consensus is that both recreational cannabis and methamphetamine use result in a wide spectrum of severe cognitive impairments, although there have been questions raised regarding conclusions derived from published material. The purpose of this work is to describe how cannabis and methamphetamine use disorder affects human cognition in a group of Saudi patients.
Methods: A cross-sectional observational study has been done at Erada Complex and Mental Health, Dammam, KSA. The study included three groups: the first group consisted of individuals who have methamphetamine use disorder, the second group included individuals with disorders related to cannabis use disorder, and the third group comprised healthy persons as a control group. The patients’ demographic information has been gathered. Urine toxicological testing for cannabis and methamphetamine has been used to evaluate recent drug use. We employed SCID-I [a semi-structured interview to diagnose mental illnesses using the standards set out in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)] to rule out other mental illnesses and confirm cannabis and methamphetamine use disorder. At the time of interview, all individuals underwent cognitive evaluations using standardized neuropsychological tests for screening by MoCA, followed by Wechsler Memory Scale and Stroop’s test for executive function.
Results: A significant difference could be seen in all aspects of cognitive functions among patients and controls upon application of MoCA, Wechsler Memory Scale, and Stroop tests. On the other hand, there was statistical significance in most of the features among patients with either methamphetamine or cannabis use disorder using the same scales.
Conclusion: Cognitive functions were affected in the studied group of Saudi patients who suffer from cannabis and methamphetamine use disorder compared to the control group, with those who were diagnosed with methamphetamine use disorder having greater effects on cognitive functions than those who were diagnosed with cannabis use disorder.
1 Introduction
Methamphetamine is a stimulant that is abused by more than 17.2 million people globally each year (1). The extent of cognitive impairments linked to methamphetamine use disorder was measured in a prior meta-analysis, which discovered that patients who are diagnosed with methamphetamine use disorder exhibit deficiencies in a number of cognitive domains, including memory consolidation, executive functioning, impulsiveness, attention, and social thinking, in comparison to healthy control subjects (2). According to Dean et al. (3), the areas with the most cognitive losses are reward- or impulse-related processes and social cognition, whereas cognitive capacity and spatial awareness show the least impact. Traditionally, methamphetamine use disorder patients have been viewed to have more neurotoxic effects than those of cannabis abuse; however, recent research has challenged this interpretation (4, 5).
According to Bernheim et al. (6), patients with methamphetamine use disorder have deficiencies in executive functioning, retention of memories, reaction suppression and set-shifting effectiveness, and psychomotor functioning. At least some of these deficits are probably related to ongoing drug use, drug pursuing, and the poor choices that come with addiction.
Several countries have updated their cannabis regulations in recent years to allow for both medicinal and recreational usage (7, 8). Concerns about how both federal and state laws affect the prevalence of cannabis usage have been raised by these shifts. More than 30 US states have authorized the use of cannabis for medical purposes, while more than 10 states have approved it for recreational consumption (9). Canada also legalized cannabis for recreational use in 2018. Evidence suggests that cannabis use disorder (CUD) and frequency of use have increased in older people (>26 years old) prior to and following medicinal and recreational regulations. There is more nuanced research on cannabis use disorder among adolescents (10, 11).
In the 1970s, when researchers first began studying the direct effects of cannabis on mental health, memory and academic issues were frequently observed. However, the findings on cognitive function have been less definitive (12, 13). According to recent studies, cannabis use disorder may be linked to long-term cognitive decline, namely, in the domains of executive functioning, memory, and visuospatial skills. These findings were also connected to changes in the cognitive functions of patients with cannabis use disorders (14). Another study illustrated that the temporal occipital fasciculus, the lateral fronto-occipital fasciculus (which plays a major role in attention and concentration), and other social cognitive regions were also shown to be affected in cannabis use disorders (15). Despite the fact that cognitive deficits in drug use disorders have been well studied in many societies (16), few studies have been conducted on Saudi patients to address this essential issue. A screening tool called the Montreal Cognitive Assessment (MoCA) assesses a number of cognitive areas, such as language, attention, memory, and visuospatial abilities. Detecting minor cognitive impairment is its intended purpose (17). Furthermore, a tool to evaluate verbal and nonverbal memory as well as perceptual–motor and cognitive capabilities is the Wechsler Memory Scale (18). Besides that, the Stroop test is a cognitive function assessment tool that evaluates selective attention, cognitive flexibility, and attentiveness. It entails identifying the ink color of words that are printed in a color that differs from the word itself (18). The purpose of the present investigation was to examine the cognitive abilities of a representative group of Saudi patients with cannabis and methamphetamine use disorder using MoCA, the Wechsler Memory Scale, and the Stroop test at Erada Complex and Mental Health in Dammam. This is crucial to develop targeted rehabilitation strategies and effective treatment plans.
2 Methods
2.1 Design and steps
This cross-sectional observational study was conducted in the Erada Complex and Mental Health in Dammam, KSA. It involved three groups: patients with methamphetamine use disorder in the first group, patients with cannabis use disorder in the second group, and healthy people in the third group as the control group. The study ran from October 2024 to March 2025.
The patients have provided demographic information such as age, sex, educational attainment, marital status, employment, and social standing. The patients’ complete medical histories have been gathered, including the duration of intake, frequency, and quantity of their cannabis and methamphetamine use as well as their past experience of other drug usage.
The inclusion criteria for the study include the following: [1] adult patients (18–50 years) who were diagnosed with methamphetamine and cannabis use disorder based on DSM-IV criteria [2]. The study included individuals with average IQ only and excluded individuals taking any medications that affect cognitive functions and individuals experiencing intoxication or withdrawal effects [3]. All of the chosen participants were fulfilling the criteria of methamphetamine and cannabis use disorder (they had at least two major criteria of substance use disorder for at least a 12-month period). On the other hand, patients with a history of other neurological or mental conditions that may impact cognitive abilities and of other drug use disorders and patients with severe illnesses that impair cognitive function, such as stroke or traumatic brain injury, were excluded from the study [4]. The sample frame that was used to include all inpatients and outpatients at the time of the research study in the addiction department at Erada Complex and Mental Health in Dammam, KSA, at the time of the study was from October 2024 to March 2025 [5]. Each patient was told of this research’s purpose and extent, and their signed informed permission was acquired. The ethical committee of the Erada Complex and Mental Health in Dammam, KSA, examined and accepted the research study (MED012). The control group included healthy individuals matched to the other two groups in sociodemographic data and their family who accepted to participate and who signed the written informed consent. MedCalc Software Ltd., Acacialaan 22, Belgium, was used to calculate the sample size. With a precision of 5% at 95% CI, the sample size was 300 participants, 100 for each group, assuming that the prevalence of amphetamine use disorder in Saudi Arabia was 10%, based on the study by Hafeiz (19), and that the average admission rate was two to three patients per day. A simple random sampling method was applied.
The exclusion criteria were as follows: [1] patients with severe illnesses that impair cognitive function, such as stroke or traumatic brain injury [2], patients with below average IQ [3], patients taking any medications known to affect cognitive functions [4], patients diagnosed to be in the intoxication or withdrawal stage of substance use, and [5] patients with substance use disorders other than methamphetamine and cannabis.
The following steps were administered among all eligible participants (based on their self-reports of drug use):
1. The Erada Complex and Mental Health psychiatry sheet includes personal information and detailed history for use disorder of cannabis and methamphetamine. A review of the coexisting medical issues was also conducted.
2. To confirm methamphetamine and cannabis use disorder and exclude other psychiatric disorders. the Structured Clinical Interview for DSM-IV Axis I Disorder (SCID-I) was used (20). A version in Arabic was employed (21). Urine toxicological assessment for cannabis and methamphetamine has been used to evaluate recent substance usage (22). At least 14 days of stoppage was needed to make sure that the participants were not in the intoxication stage and also almost nearing the end of their withdrawal symptoms.
3. Cognitive function was screened generally by the use of the Montreal Cognitive Assessment (MoCA) (23). In order to get a total score between 0 and 30, it samples behavior across 14 performance tests that include different cognitive areas. The score is expressed in integers. MoCA has shown good sensitivity and adequate specificity in detecting mild to moderate cognitive decline at a cumulative score of 25 or below (24).
4. To assess intellectual function, the Wechsler Memory Scale (WMS) assessment has been added (25). The WMS consists of four subtests: two nonverbal assessments of fluid intelligence (matrix thinking and block layout) and two verbal assessments of consolidated intelligence (vocabulary and patterns). Although they contain distinct questions, the WASI separate tests are comparable to their Wechsler Memory Scale–Third Edition equivalents (26). In order to represent a broad intellectual function or “g-factor”, the full-scale IQ (FSIQ) was chosen. Patients with marginal intellectual impairment are classified as cognitively challenged if their FSIQ is less than 86 (27).
5. The Stroop test gauges set shifting, inhibition, and attentional distortion. The Stroop examination, which has three phases, was to be administered to the participants by computer. When color circles—either blue, red, yellow, or green—appear in the center of the display screen during the first phase (color cards), the participant is instructed to press the corresponding color key on the designated Num-Lock keyboard right away. The subject must press the appropriate color key in accordance with the word without paying attention to its color in the following phase, also known as the trial phase, when a word with jumbled colors displays. Although the third stage is lengthier than the second, it is comparable to the second. The mistakes and response time are measured to grade the Stroop test.
In the incongruent condition, when the color of the ink and the word are conflicting, longer reaction times signify more cognitive interference. More mistakes in the condition that is not consistent also point to inhibition issues. The results from the Stroop test, particularly in the incongruent condition, might reveal important information about a person’s capacity to control cognitive distraction and focus (28).
2.2 Statistical examination
The statistical software Statistics for Social Sciences (SPSS) version 20 from IBM (SPSS Inc., Chicago, IL, USA) was used to analyze the data. Range and mean SD, as well as numbers and percentages, were used to characterize the data. By using Student’s t-test (T), the quantitative parameters across two groups were compared. To contrast qualitative parameters, chi-square (χ2) and Fisher’s exact test were employed. Significance was defined as a P-value below 0.05. Non-significance was defined as a P-value above 0.05.
3 Results
3.1 Sociodemographic classification of the study group
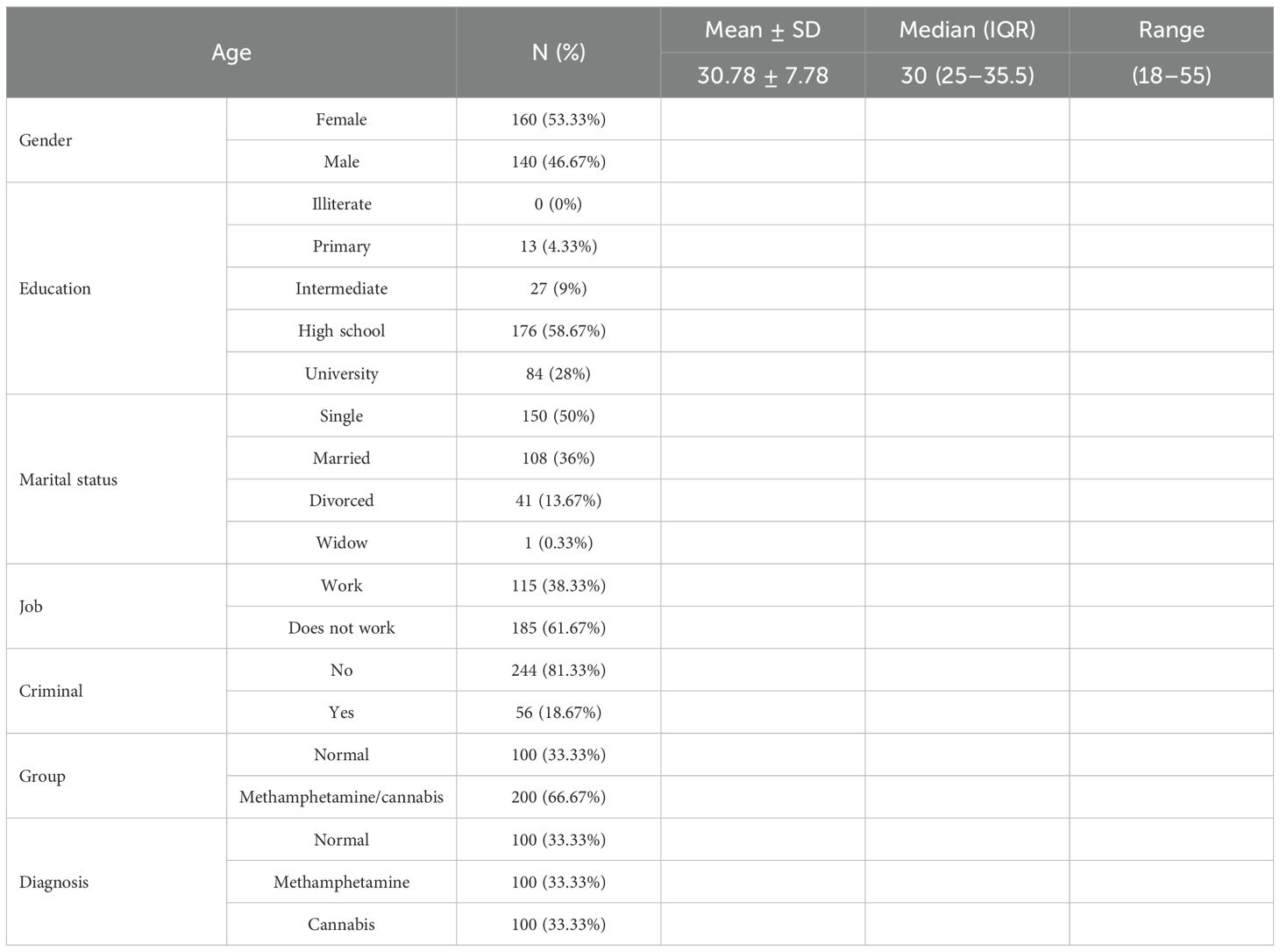
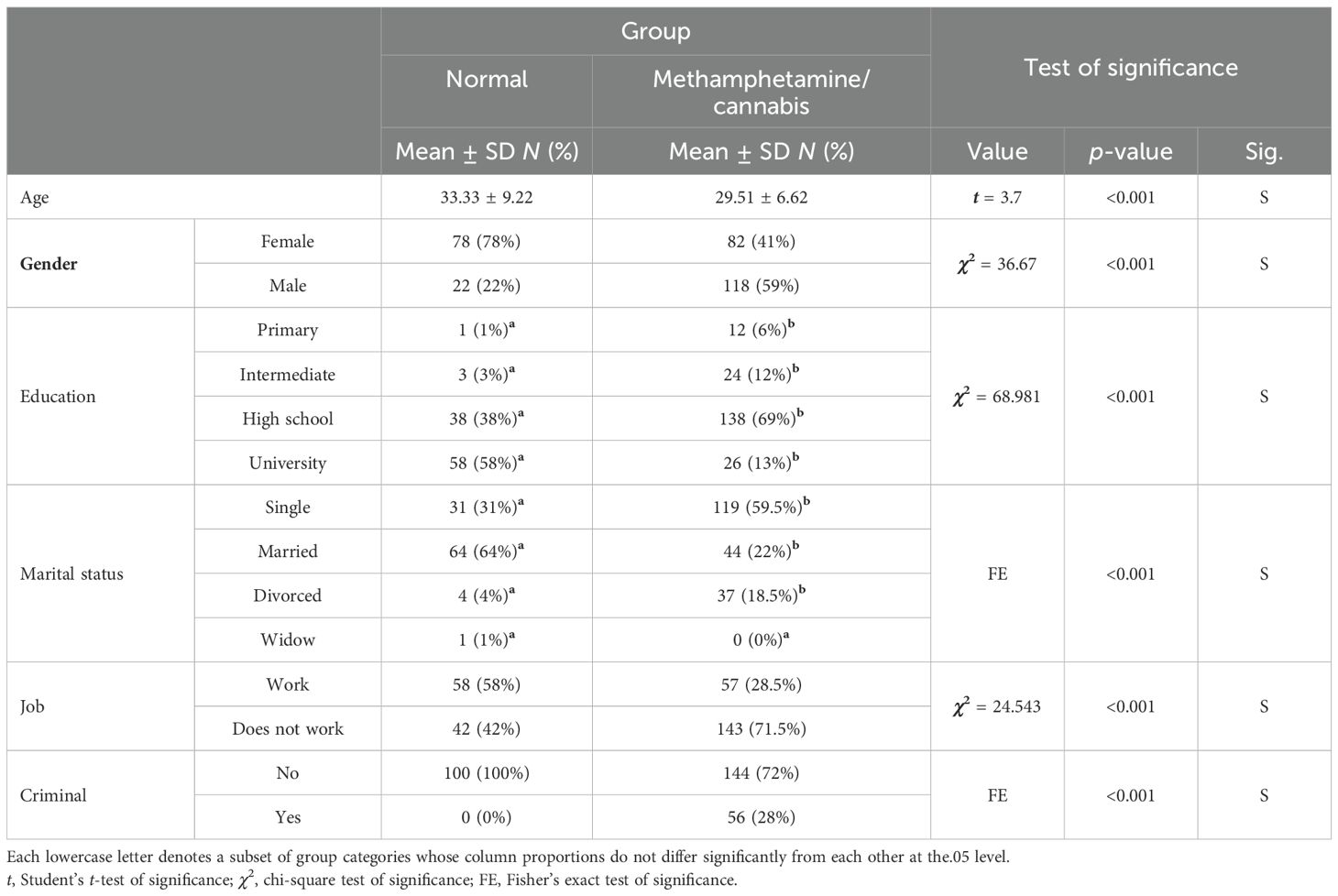
A total of 300 participants were included in this study, with a mean age of 30.78 ± 7.78 years. The study groups included 53.33% female and 46.67% male participants. Moreover, 4.33% of the study participants have completed their primary education, 9% have been in the intermediate education level, 58.67% have completed their high school education, and 28% have a university degree. Regarding their marital status, it could be noticed that 50% of the participants were single and 36% were married. Furthermore, 61.67% of the participants do not work, and 81.33% of the tested community had a criminal record. Lastly, 66.67% of the examined group of participants were diagnosed with using either methamphetamine or cannabis, as shown in Table 1. The data in Table 2 illustrate that the mean age for the control group was 33.33 ± 9.22 years, while for patients who have methamphetamine/cannabis use disorder it was 29.51 ± 6.62 years. Furthermore, the control group consisted of 78% female and 22% male participants. For patients who have methamphetamine/cannabis use disorder, it could be noticed that 41% were female and 59% were male. There is a significant difference (P < 0.001) among the study groups in terms of education, where the highest number of patients include those with high school education, while for the control the highest number comprised those who had a university degree. Besides that, there is a significant difference (P < 0.001) among the study groups in terms of marital status, where the highest number of patients included single persons, while for the control the highest number included those who were married. Additionally, the two groups had a dramatic (P < 0.001) difference for their work status, where the highest number for controls included those who have work, while for patients the highest number included those who do not work. Lastly, a significant difference (P < 0.001) could be detected among the study groups as regards their criminal record.
3.2 Evaluation of cognitive functions between study groups using different scales
Application of the MoCA test in the present work among the control group and patients who have either methamphetamine or cannabis use disorder revealed that there is a dramatic decrease (p < 0.001) in executive, naming, attention, language, abstraction, reminder, and total cognitive functions of the tested patients relative to the control group. Upon using the Wechsler Memory Scale assessment, two study groups reflect a significant decline (p < 0.001) in information, guidance, cognitive control, logic, number of repetitions, visual cues, verbal association, raw material, degree, and memory among the examined patients relative to the control group. Furthermore, using the Stroop test for measuring cognitive flexibility between two study groups revealed a significant increase (p < 0.001) in all examined aspects of the tested patients relative to the control group (Table 3).
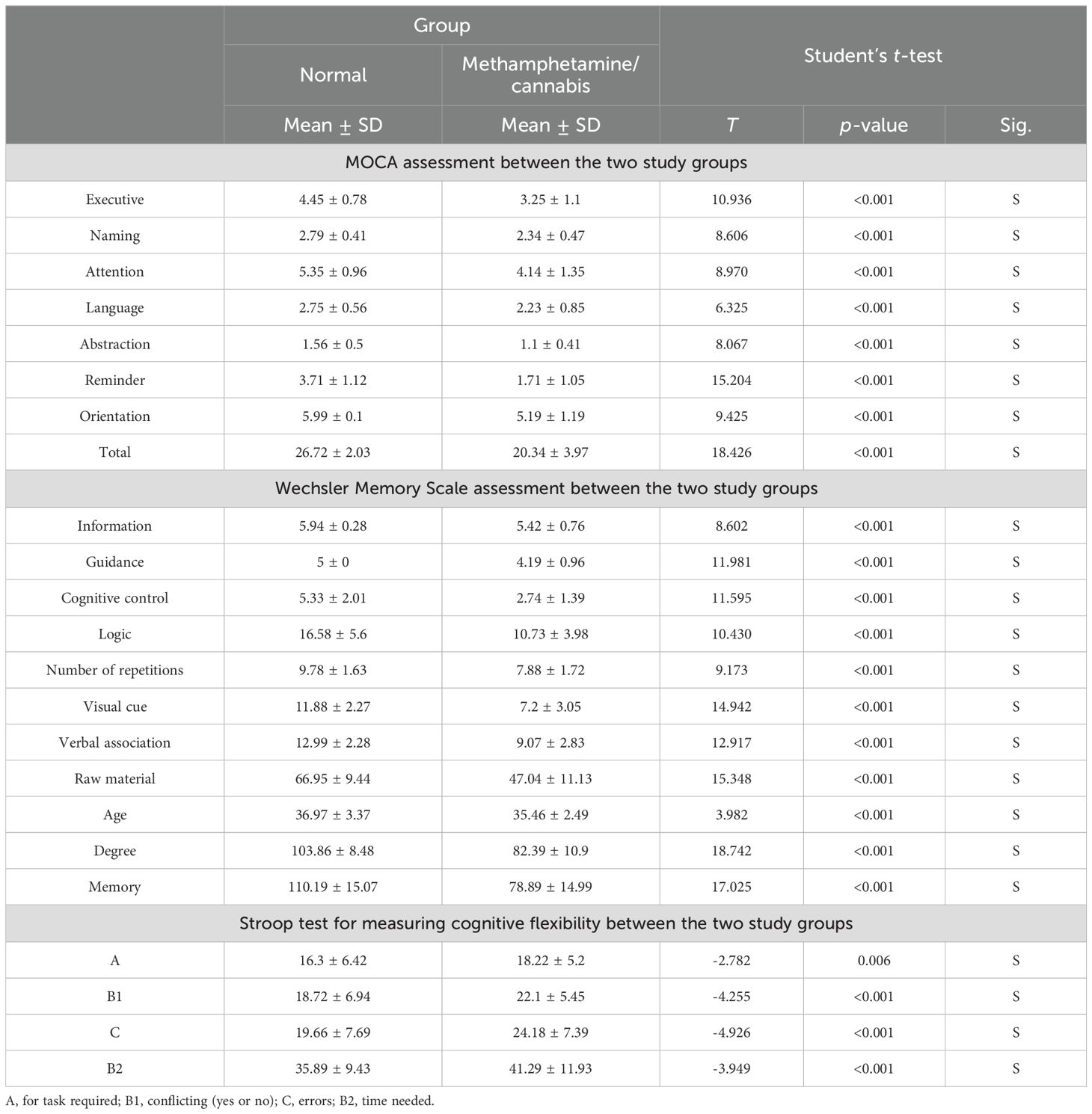
Table 3. Assessment of cognitive functions among controls and patients using methamphetamine and cannabis upon using MOCA, Wechsler Memory Scale, and Stroop test for measuring cognitive flexibility (data are presented as means ± SD).
3.3 Evaluation of cognitive functions between patients using drugs using different scales
Using the MoCA test in the current investigation among patients who have either methamphetamine or cannabis use disorder revealed that there is a dramatic difference (p < 0.001) in executive, attention, language, reminder, and total cognitive functions. Additionally, a non-significant difference could be seen in naming and abstraction (where p = 0.297 and 0.605, respectively) among the study groups. Upon using the Wechsler Memory Scale assessment, two study groups reflect a significant increase (p < 0.001) in guidance, cognitive control, logic, visual cues, verbal association, raw material, degree, and memory of patients using cannabis relative to those using methamphetamine, while there was a non-significant difference among study groups in information, number of repetitions, and age (where p = 0.578, 0.251, and 0.350, respectively). Furthermore, using the Stroop test to measure cognitive flexibility between the two study groups revealed a non-significant difference in all examined aspects except for B2 (for “time needed”, a significant difference could be seen among the study groups; p = 0.006) (Table 4).
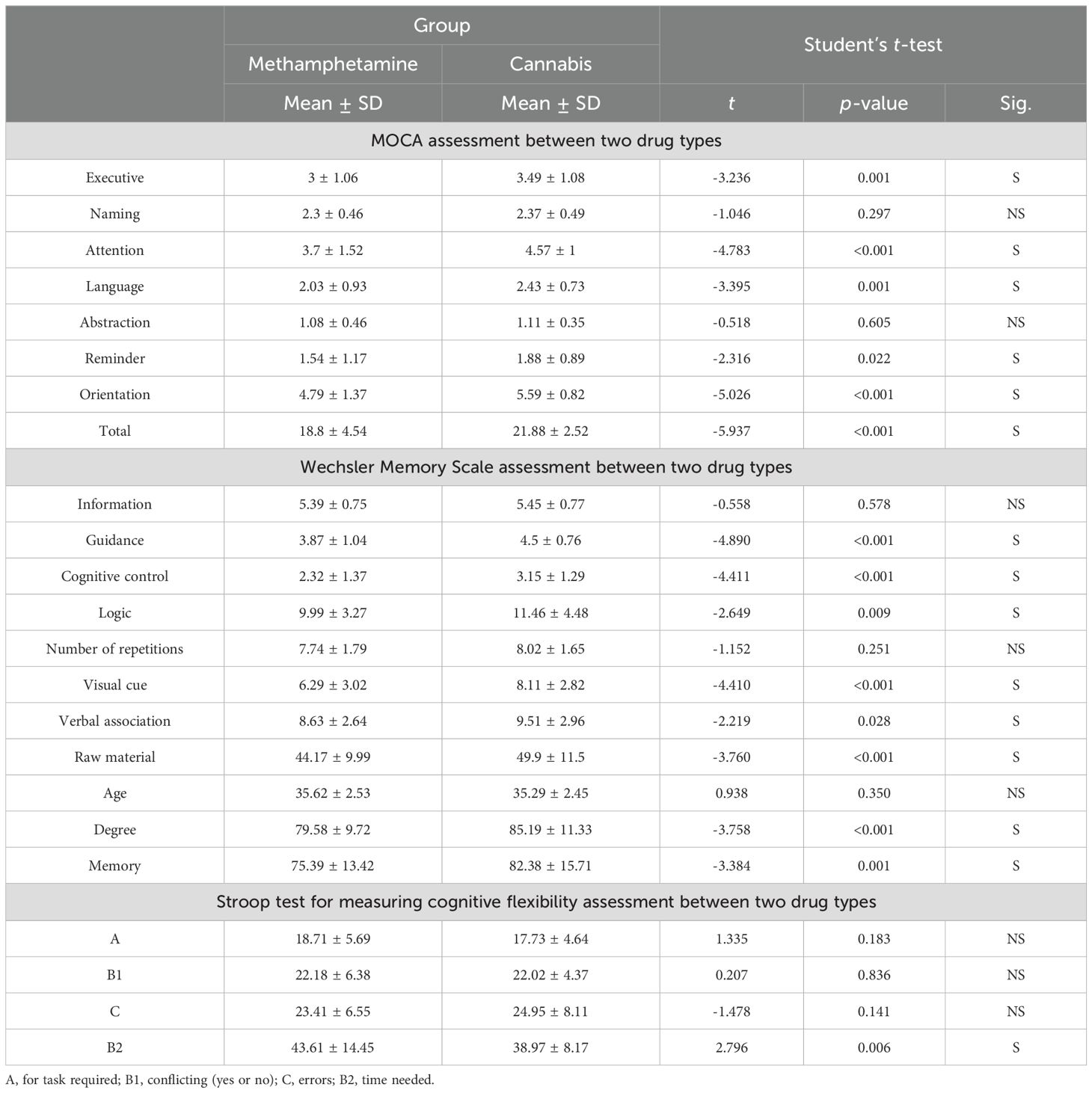
Table 4. Assessment of cognitive functions among patients using methamphetamine or cannabis use disorders upon using MOCA, Wechsler Memory Scale, and Stroop test for measuring cognitive flexibility (data are presented as means ± SD).
4 Discussion
The present research is designed to evaluate the cognitive abilities of Saudi patients with cannabis and methamphetamine use disorder, with a focus on certain cognitive abilities (attention, memory, and executive functioning) that are most impacted by both cannabis and methamphetamine use disorder. There is a significant decline in these functions in patients relative to the controls. Furthermore, there is a dramatic deterioration in most of the examined cognitive functions in patients with methamphetamine use disorder relative to patients with cannabis use disorder.
Methamphetamine is a psychostimulant that is frequently abused. It increases the extracellular amount of dopamine in the brain, which is linked to the rewarding effect, by reversing transit across the dopamine transporter. Substance use disorder, a continuously relapsing illness marked by obsessive drug consumption, an inability to restrict intake, and severe drug impulses, is caused by frequent methamphetamine use (29–31).
The present findings revealed that patients who have cannabis and methamphetamine use disorder had a higher risk of cognitive impairment than the controls. In accordance with other research studies, which reported that determining the degree of cognitive decline in this susceptible patient population may aid in customizing educational, career, and psychotherapy plans for them, it has been suggested that cerebral plasticity and the reconfiguration of certain brain circuits are involved in the genetic and cellular underpinnings of drug addiction, but these processes are not fully understood (32, 33). Additionally, there is growing evidence that methamphetamine and cannabis use disorder, respectively, have cognitive impairments in areas including working memory, ability to concentrate, scrutiny, social cognition, and adaptability. Additionally, patients who have cannabis and methamphetamine use disorder have changed decision-making (34, 35). The high likelihood of resurgence even after continuous abstinence with psychological assistance may be caused by cognitive disorders and impaired decision-making in methamphetamine and cannabis use disorder (36).
The present work uses different scales, including MoCA, Wechsler Memory Scale, and Stroop test, to screen the cognitive functions in the tested group of participants. Julayanont and colleagues designed the Montreal Cognitive Assessment-Basic (MoCA-B) in 2015 in order to test for moderate cognitive impairment in older individuals who are illiterate or have low levels of education (37). Furthermore, the Wechsler Memory Scale’s paired-associate learning test was used to gauge retrieval and the capacity to create new connections between two objects (38). Besides that, a variety of management, prominence, and cognitive network functions are measured using Stroop tasks (39, 40). From the lists of items written on three printed pages to be looked at as quickly as practical, the Stroop test has changed to two words on an electronic monitor with the question, “Does the color of the upper word match the concept of the lower word?”, followed by a yes/no button (41, 42).
Information, guidance, cognitive control, logic, numerical repetition, visual cues, verbal association, raw material, age, degree, and memory are some of the cognitive areas where the current findings indicate that methamphetamine and cannabis use disorder patients have worse cognition. In the same line, Potvin et al. (2) conducted a meta-analysis of users of methamphetamine use disorder and found a correlation with social cognition.
According to the current findings, consumption of methamphetamine and cognition in patients with substance use disorder was much more correlated than cannabis use disorder. In the same line, Scheffler et al. (43) showed that methamphetamine is positively correlated with cognitive functions. Besides that, according to recent meta-analyses of research on healthy populations, cannabis use disorder patients exhibit worse cognitive performance in a variety of cognitive areas when compared to non-users (44, 45). Furthermore, an investigation of longitudinal studies indicated that while consumption of cannabis was related to cognitive deterioration, the relationships were moderate, were evident primarily for the strongest users of cannabis, and were not obvious after correcting for potential confounding variables (46, 47).
Methamphetamine and cannabis use disorder patients are identified in the present investigation as risk factors for cognitive deficits in the Saudi patient group that was evaluated. Cognitive functions were affected in the studied group of Saudi patients who have cannabis and methamphetamine use disorder compared to the control group, with those who were diagnosed with methamphetamine use disorder having greater effects on cognitive functions than those who use cannabis. Future studies are needed to determine the possible neurocognitive dysfunctions in patients associated with other substance use disorders (e.g., opiates, synthetic cannabinoids, alcohol, etc.).
The study has some limitations, including the following:
1. The details of substance use were not fully assessed in depth, as they were not accurately assessed due to differences in the pattern of use regarding the amount of actual use and route of administration.
2. This study focused on a specific region in Saudi Arabia, and further studies across different regions in Saudi Arabia are needed.
3. Follow-up studies are needed to determine the long-term effect of methamphetamine and cannabis use on human cognition.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Ethics statement
The ethical committee for Erada Complex and Mental Health examined and accepted the research study (MED012). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ASSA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AS: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MSAA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. IA-s: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. FA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AmA-ZA-D: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AfA-ZA-D: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AAA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MIA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1621261/full#supplementary-material
References
1. Mizoguchi H and Yamada K. Methamphetamine use causes cognitive impairment and altered decision-making. Neurochemistry Int. (2019) 124:106–13. doi: 10.1016/j.neuint.2018.12.019
2. Potvin S, Pelletier J, Grot S, Hébert C, Barr AM, and Lecomte T. Cognitive deficits in individuals with methamphetamine use disorder: A meta-analysis. Addict Behav. (2018) 80:154–60. doi: 10.1016/j.addbeh.2018.01.021
3. Dean AC, Morales AM, Hellemann G, and London ED. Cognitive deficit in methamphetamine users relative to childhood academic performance: link to cortical thickness. Neuropsychopharmacology. (2018) 43:1745–52. doi: 10.1038/s41386-018-0065-1
4. Fernandez-Serrano MJ, Perez-Garcia M, and Verdejo-Garcia A. What are the specific vs. generalized effects of drugs of abuse on neuropsychological performance? Neurosci Biobehav Rev. (2011) 35:377–406.
5. Okita K, Morales AM, Dean AC, Johnson MC, Lu V, Farahi J, et al. Striatal dopamine D1-type receptor availability: no difference from control but association with cortical thickness in methamphetamine users. Mol Psychiatry. (2018) 23:1320–7. doi: 10.1038/mp.2017.172
6. Bernheim A, See RE, and Reichel CM. Chronic methamphetamine self-administration disrupts cortical control of cognition. Neurosci Biobehav Rev. (2016) 69:36–48. doi: 10.1016/j.neubiorev.2016.07.020
7. Guerin AA, Bonomo Y, Lawrence AJ, Baune BT, Nestler EJ, and Rossell SL and Kim JH. Cognition and related neural findings on methamphetamine use disorder: insights and treatment implications from schizophrenia research. Front Psychiatry. (2019) 10:880. doi: 10.3389/fpsyt.2019.00880
8. Cerdá M, Mauro C, Hamilton A, NS L, Santaella-Tenorio J, Hasin D, et al. Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiatry. (2020) 77:165–71. doi: 10.1001/jamapsychiatry.2019.3254
9. Williams AR, Santaella-Tenorio J, CM M, FR L, and Martins SS. Loose regulation of medical marijuana programs associated with higher rates of adult marijuana use but not cannabis use disorder. Addiction. (2017) 112:1985–91.
10. Sarvet Al, Wall MM, DS F, Greene E, Le A, AE B, et al. Medical marijuana laws and adolescent marijuana use in the United States: a systematic review and meta-analysis. Addiction. (2018) 113:1003–16. doi: 10.1111/add.14136
11. Dilley JA, SM R, Kilmer B, RL P, MB S, and Cerdá M. Prevalence of cannabis use in youths after legalization in Washington state. JAMA Pediatrics. (2019) 173:192–3.
12. Crean RD, NA C, and Mason BJ. An evidence-based review of acute and long-term effects of cannabis use on executive cognitive functions. J Addict Med. (2011) 5:1–8. doi: 10.1097/ADM.0b013e31820c23fa
13. Burggren AC, Shirazi A, Ginder N, and London ED. Cannabis effects on brain structure, function, and cognition: considerations for medical uses of cannabis and its derivatives. Am J Drug Alcohol Abuse. (2019) 45:563–79.
14. Elrassas HH, Elsayed YAR, Abdeen MS, Mohamed AT, and El Nagar ZM. Synthetic cannabinoids impact on cognitive functions. Egypt J Neurol Psychiatry Neurosurg. (2023) 59:151. doi: 10.1186/s41983-023-00756-x
15. Hill SY, Wang S, Carter H, MD M, Zezza N, and Stiffler S. Amygdala volume in offspring from multiplex for alcohol dependence families: the moderating influence of childhood environment and 5-HTTLPR variation. J Alcohol Drug Depend. (2013) Suppl 1:001.
16. Ramey T and Regier PS. Cognitive impairment in substance use disorders. CNS Spectr. (2019) 24:102–13. doi: 10.1017/S1092852918001426
17. Series H and Burns A. Cognitive testing and the hazards of cut-offs. BJPsych Adv. (2025) 31:20–7. doi: 10.1192/bja.2024.10
18. Salzman T, Sarquis-Adamson Y, Son S, Montero-Odasso M, and Fraser S. Associations of multidomain interventions with improvements in cognition in mild cognitive impairment: A systematic review and meta-analysis. JAMA Netw Open. (2022) 5:e226744. doi: 10.1001/jamanetworkopen.2022.6744
19. Webster-Cordero F and Giménez-Llort L. A systematic review on subjective cognitive complaints: main neurocognitive domains, myriad assessment tools, and new approaches for early detection. Geriatrics (Basel). (2025) 10:65. doi: 10.3390/geriatrics10030065
20. First MB, Spitzer RL, Williams W, and Gibbon M. Structured clinical interview for DSM-IV axis I disorders (SCID-I). In: Rush AJ, First MB, and Blacker D, editors. Handbook of psychiatric measures. American Psychiatric Association, Washington (1995).
21. Missiry A, Sorour A, Sadek A, Fahy T, and Mawgoud M and Asaad A. Homicide and psychiatric illness: an Egyptian study [MD thesis]. Cairo, Egypt: Faculty of Medicine, Ain Shams University (2004).
22. Schalk DR and Lewis JL. An evaluation of the clinical tools used to monitor illicit methamphetamine use among chronic pain patients: A cross-sectional retrospective study. Hosp Pharmacy. (2023) 58:621–7. doi: 10.1177/00185787231174752
23. Amro I, Hamadi AMA, Salem AAE, Chivese T, Wilkins SS, and Khaled SM. Population-based norms for the montreal cognitive assessment in arab adults. Brain Behav. (2025) 15:e70287. doi: 10.1002/brb3.70287
24. Hetland J, Hagen E, Lundervold AJ, and Erga AH. Performance on cognitive screening tests and long-term substance use outcomes in patients with polysubstance use disorder. Eur Addict Res. (2023) 29:150–9. doi: 10.1159/000528921
25. Abu-Hilal MM, Al-Baili MA, Sartawi A, Abdel-Fattah F, and Al-Qaryouti IA. Psychometric properties of the Wechsler abbreviated scale of intelligence (WASI) with an Arab sample of school students. Individ Dif Res. (2011) 9:219–30.
26. Hagen E, Erga AH, Nesvag SM, McKay JR, Lundervold AJ, and Walderhaug E. One-year abstinence improves ADHD symptoms among patients with polysubstance use disorder. Addict Behav Rep. (2017) 6:96–101. doi: 10.1016/j.abrep.2017.08.005
27. Braatveit KJ, Torsheim T, and Hove O. The prevalence and characteristics of intellectual and borderline intellectual disabilities in a sample of inpatients with substance use disorders: preliminary clinical results. J Ment Health Res Intellect Disabilities. (2018) 11:203–20.
28. Al-Ghatani A, Obonsawin M, and Al-Moutaery K. The Arabic version of the Stroop Test and its equivalency to the English version. Pan Arab J Neurosurgery. (2010) 14:112–5.
29. Chen T, Su H, Zhong N, Tan H, Li X, Meng Y, et al. Disrupted brain network dynamics and cognitive functions in methamphetamine use disorder: insights from EEG microstates. BMC Psychiatry. (2020) 20:334. doi: 10.1186/s12888-020-02743-5
30. Wang W, Sun G, Li C, Qiu C, Fan J, and Jin Y. Exploring the mechanism of trait depression and cognitive impairment on the formation of among individuals with methamphetamine use disorder under varying degrees of social support. Front Public Health. (2025) 13:1435511. doi: 10.3389/fpubh.2025.1435511
31. Shirley K, O’Neil M, Boyd S, and Loftis JM. Differences in rates of impairment in adults who use methamphetamine using two sets of demographically corrected norms. Appl Neuropsychol Adult. (2025) 32:216–24.
32. Koob GF and Volkow ND. Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry. (2016) 3:760–73. doi: 10.1016/S2215-0366(16)00104-8
33. Friedman NP and Robbins TW. The role of prefrontal cortex in cognitive control and executive function. Neuropsychopharmacol. (2022) 47:72–89.
34. Ren W and Fishbein D. Prospective, longitudinal study to isolate the impacts of marijuana use on neurocognitive functioning in adolescents. Front Psychiatry. (2023) 14:1048791. doi: 10.3389/fpsyt.2023.1048791
35. Khan R, Turner A, Berk M, Walder K, Rossell S, Guerin AA, et al. Genes, cognition, and their interplay in methamphetamine use disorder. Biomolecules. (2025) 15:306.
36. May AC, Aupperle RL, and Stewart JL. Dark times: the role of negative reinforcement in methamphetamine addiction. Front Psychiatry. (2020) 11:114. doi: 10.3389/fpsyt.2020.00114
37. Julayanont P, Tangwongchai S, Hemrungrojn S, Tunvirachaisakul C, Phanthumchinda K, Hongsawat J, et al. The Montreal Cognitive Assessment-Basic: a screening tool for mild cognitive impairment in illiterate and low-educated elderly adults. J Am Geriatr Soc. (2015) 63:2550–4. doi: 10.1111/jgs.13820
38. Wang HC, Wass M, and Castles A. Paired-associate learning ability accounts for unique variance in orthographic learning. Sci Stud Reading. (2016) 21:5–16.
39. ElKholy N, Tawfik HM, Ebeid S, Elsayed Madkor OR, and Hamza SA. A model of cognitive evaluation battery for diagnosis of mild cognitive impairment and dementia in educated and illiterate Egyptian elderly people. Egypt J Neurol Psychiatry Neurosurg. (2020) 56:95. doi: 10.1186/s41983-020-00223-x
40. Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol. (1935) 18:643–62. doi: 10.1037/h0054651
41. MacLeod CM. Half a century of research on the Stroop effect: an integrative review. Psychol Bull. (1991) 109:163–203. doi: 10.1037/0033-2909.109.2.163
42. Baraniuk JN, Thapaliya K, Inderyas M, Shan ZY, and Barnden LR. Stroop task and practice effects demonstrate cognitive dysfunction in long COVID and myalgic encephalomyelitis/chronic fatigue syndrome. Sci Rep. (2024) 14:26796. doi: 10.1038/s41598-024-75651-3
43. Scheffler F, Phahladira L, Hendrikse CB, du Plessis S, Asmal L, Luckhoff HK, et al. The associations of cannabis and methamphetamine use with cognitive performance over the first 2 years of treatment in schizophrenia spectrum disorders. Early intervention Physiatry. (2022) 16:12030–1239.
44. Scott JC, Slomiak ST, Jones JD, Rosen AFG, Moore TM, and Gur RC. Association of cannabis with cognitive functioning in adolescents and young adults a systematic review and meta-analysis. JAMA. Psychiatry. (2018) 75:585–95. doi: 10.1001/jamapsychiatry.2018.0335
45. Duperrouzel JC, Granja K, Pacheco-Colón I, and Gonzalez R. Adverse effects of cannabis use on neurocognitive functioning: A systematic review of meta- analytic studies. J Dual Diagnosis. (2020) 16:43–57. doi: 10.1080/15504263.2019.1626030
46. Gonzalez R, Pacheco-Colón I, Duperrouzel JC, and Hawes SW. Does cannabis use cause declines in neuropsychological functioning? A review of longitudinal studies. J Int Neuropsychol Soc. (2017) 23:893–902. doi: 10.1017/S1355617717000789
Keywords: methamphetamine, cannabis, cognitive functions, MoCA, WASI, Stroop test
Citation: Afifi SY, Alghamdi ASS, Sallam A, Almuqahwi MSA, Al-sayegh IA, Alzahrani FMO, Al-Zain Al–Dain AN, Al-Zain Al-Deen AN, ALabdulhadi AA and Ali MI (2025) Cognitive functions among Saudi patients with methamphetamine and cannabis use disorder. Front. Psychiatry 16:1621261. doi: 10.3389/fpsyt.2025.1621261
Received: 30 April 2025; Accepted: 31 July 2025;
Published: 22 August 2025.
Edited by:
Giorgio Di Lorenzo, University of Rome Tor Vergata, ItalyReviewed by:
Rana Hamimy, Cairo University, EgyptHaydy Hassan, Suez Canal University, Egypt
Sana Maidoumi, Cadi Ayyad University, Morocco
Copyright © 2025 Afifi, Alghamdi, Sallam, Almuqahwi, Al-sayegh, Alzahrani, Al-Zain Al–Dain, Al-Zain Al-Deen, ALabdulhadi and Ali. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shrief Y. Afifi, c2FkMTk5NDE5ODlAZ21haWwuY29t
 Shrief Y. Afifi
Shrief Y. Afifi Abdulkhaliq S. S. Alghamdi2
Abdulkhaliq S. S. Alghamdi2 Farah M. O. Alzahrani
Farah M. O. Alzahrani