- 1Department of Radiology, Affiliated Hospital of North Sichuan Medical College, Nanchong, China
- 2Key Laboratory of Digital-Intelligent Disease Surveillance and Health Governance, North Sichuan Medical College, Nanchong, Sichuan, China
- 3Department of Medical Imaging Function, Xi’an Electric Power Central Hospital, Xi’an, Shaanxi, China
- 4School of Medical Imaging, North Sichuan Medical College, Nanchong, China
- 5Mental Health Center, Affiliated Hospital of North Sichuan Medical College, Nanchong, China
Prior research has predominantly adopted variable-centered approaches to demonstrate significant correlations between psychological capital and death anxiety. However, few studies have investigated the heterogeneity of these constructs among patients with pancreatic cancer. To address this gap, we employed a random sampling method to recruit 513 patients with pancreatic cancer. Latent profile analysis was conducted to examine their psychological capital and death anxiety profiles, followed by univariate analysis and multinomial logistic regression to identify influencing factors. The results revealed three distinct profiles: high psychological capital–low death anxiety, moderate psychological capital–moderate death anxiety, and low psychological capital–high death anxiety. Key determinants included Gender, age, place of residence, and cancer stage. These findings enhance our understanding of the psychological recovery trajectory in pancreatic cancer patients, enabling clinicians to develop targeted interventions based on distinct psychological profiles to improve mental health outcomes.
1 Introduction
Pancreatic cancer is one of the malignant tumors with the lowest five-year survival rates, which is less than 10% (1, 2). It ranks as the seventh leading cause of cancer-related mortality worldwide (3), claiming nearly half a million lives annually (4), with particularly high mortality rates in developed countries such as the United States (5, 6). Despite advancements in multidisciplinary treatments—including surgical intervention, chemotherapy, and nutritional support (7, 8)—the disease’s insidious progression and limited therapeutic efficacy continue to inflict severe physical and psychological suffering (9). Notably, over 30% of patients exhibit clinically significant death anxiety at diagnosis (10), while more than 50% experience depressive tendencies during treatment (11). Death anxiety refers to the fear, worry, or unease of patients about death-related events of themselves or others (12). Death anxiety not only includes specific manifestations such as fear of the death process (13), worry about the unknown after death (14), and anxiety about the loss of the meaning of life (15), but also may be accompanied by physiological manifestations such as palpitations (16), asphyxia (17), and cognitive avoidance (18). Previous studies have found that death anxiety can exacerbate depression (19), sleep disorders (20), social withdrawal (21), and treatment termination in cancer patients (22). For example, in the study by Gui et al. (23), it was explored that family support could effectively alleviate the death anxiety of breast cancer patients. However, few studies have paid attention to the death anxiety of pancreatic cancer patients. This neglect is deplorable. According to data released by the National Cancer Center in 2024, the 5-year survival rate of pancreatic cancer in China is only 7.2% (24). Compared with other adenocarcinomas or cancers, with effective treatment at early detection, the 5-year survival rate is relatively high, and patients have a longer survival expectancy (25–27). On the other hand, the research of pancreatic cancer focuses more on treatment methods and pathological mechanisms (28, 29), while the research on the psychological level of death anxiety of pancreatic cancer patients is relatively few, and there is a lack of effective intervention measures. Therefore, by studying the heterogeneity of death anxiety in patients with pancreatic cancer, this study developed measures for different categories of pancreatic cancer patients to help them reduce death anxiety, improve their quality of life, and prolong their survival.
In recent years, a large number of researchers have begun to pay attention to the correlation between psychological capital and death anxiety (30–32). Psychological Capital refers to an individual’s positive psychological resources, including resilience, self-efficacy, and adaptive coping mechanisms (33, 34), and is a critical determinant of treatment outcomes in pancreatic cancer (35). Characterized by its high lethality, rapid physical deterioration, treatment-related toxicities, and relatively low overall survival rates (36–38), this disease context may be mitigated by psychological capital, which buffers psychological trauma and fosters treatment resilience. Preliminary evidence suggests that enhanced psychological resources in pancreatic cancer patients often correlate with better treatment adherence (39, 40). Specifically, patients with higher psychological capital demonstrate greater tolerance for aggressive treatment regimens, reduced engagement in health-damaging behaviors, and improved tolerance during completion of neoadjuvant therapy (41, 42). However, previous studies have never explored the relationship between psychological capital and death anxiety in patients with pancreatic cancer, and even fewer studies have analyzed the heterogeneity of psychological capital and death anxiety in patients with pancreatic cancer and their influencing factors.
Recent cross-sectional studies have gradually elucidated the complex relationship between psychological capital and death anxiety in pancreatic cancer patients (35, 43, 44). However, these studies exhibit significant limitations in methodology and theoretical depth. For instance, while prior research highlights negative correlations between death anxiety and dimensions of psychological capital—such as hope, self-efficacy, resilience, and optimism (45, 46)—the underlying mechanisms remain underexplored. Specifically, hope has been shown to buffer death anxiety through goal-directed thinking and positive attribution patterns, enabling patients to reinterpret disease outcomes (47, 48). Optimism mitigates catastrophic cognitions by framing mortality as a universal human experience (49). In terms of emotional regulation, self-efficacy enhances perceived control over treatment processes (50, 51), while resilience reduces emotional exhaustion by fostering acceptance of disease progression (52). For example, Marinelli et al. (53) found that advanced pancreatic cancer patients with high self-efficacy reported significantly lower death anxiety scores than those with low self-efficacy. Collectively, these findings suggest that robust psychological capital confers resilience against death anxiety (54). From a neurobiological perspective, psychological capital interventions have been linked to strengthened prefrontal cortex regulation of the limbic system, inhibition of amygdala hyperactivation, and reduced cortisol levels (55–57). Such neuroendocrine modulation disrupts the fear-stress-anxiety cycle, underscoring the therapeutic potential of psychological capital in clinical settings.
However, some scholars argue that death anxiety can also undermine psychological capital (58, 59). Death anxiety triggers persistent worry and rumination, diverting cognitive resources toward imagined mortality scenarios (60, 61). This state undermines individuals’ ability to cope with real-world challenges, eroding self-efficacy (62, 63). From an existential perspective, death anxiety may provoke profound angst about the meaning of life (64–66). Specifically, when individuals succumb to self-denigration over perceived wasted potential, the hope dimension of psychological capital is directly impaired, leaving them unable to sustain goal-directed optimism.
The inconsistent findings regarding the relationship between death anxiety and psychological capital may partially stem from limitations in research perspectives. Previous studies have predominantly employed variable-centered approaches to examine associations between psychological constructs, yet this methodology often overlooks individual heterogeneity. Pancreatic cancer patients may exhibit distinct patterns of psychological capital and death anxiety based on their unique experiences, coping strategies, and disease trajectories (13, 34). Neglecting this heterogeneity risks overgeneralized conclusions and constrains the development of targeted interventions.
Furthermore, research investigating influential factors of psychological capital and death anxiety in pancreatic cancer patients remains relatively scarce. Existing studies have primarily focused on demographic characteristics, presenting a unidimensional perspective (45, 67). Perceived stress, defined as an individual’s subjective cognitive appraisal of stressors, emphasizes personal interpretation of challenging events (68, 69). Pancreatic cancer patients frequently endure intense psychological stress, which may undermine self-efficacy by fostering doubts about recovery capabilities (70, 71). Concurrently, heightened stress levels may induce physiological symptoms such as palpitations and insomnia, potentially misinterpreted as harbingers of imminent mortality, thereby exacerbating death anxiety (72, 73). Beyond perceived stress, social support emerges as another potential determinant, encompassing material assistance, emotional comfort, information sharing, and sense of belonging within social networks (74, 75). Prognostic guidance and rehabilitation protocols from specialized medical teams can effectively correct patients’ cognitive biases regarding mortality (76, 77). Nevertheless, previous research has rarely explored how perceived stress and social support influence psychological capital and death anxiety in this population.
This study therefore addresses two primary questions: 1) What distinct subgroups exist regarding psychological capital and death anxiety among pancreatic cancer patients? 2) Which factors influence these psychological constructs across different subgroups? Latent Profile Analysis (LPA), a person-centered statistical approach, provides a robust framework for identifying subgroups with similar psychological characteristics (78). By applying LPA to pancreatic cancer patients, this research reveals distinct psychological capital and death anxiety profiles while exploring each subgroup’s defining attributes. Subsequently, we examine how demographic characteristics, perceived stress, and social support differentially impact these psychological constructs across identified latent classes. This dual approach not only enhances our understanding of psychological heterogeneity but also establishes foundations for personalized interventions. Healthcare professionals conducting psychological counseling should consider patients’ distinct psychological profiles while emphasizing individualized management of perceived stress and social support systems.
2 Method
2.1 Sample sources
This study aimed to use Latent Profile Analysis (LPA) to investigate the heterogeneity of psychological capital and death anxiety among pancreatic cancer patients. The Ethics Committee of North Sichuan Medical College approved the study. Data collection was conducted in several Grade A tertiary hospitals in Nanchong City and Xi’an City. Prior to data collection, all participants were informed of the study’s purpose, procedures, potential risks, benefits, and the voluntary nature of participation. Following the obtainment of informed consent, participants completed either paper or electronic questionnaires. Given the relatively long nature of the questionnaire, completion of all items required approximately 8 minutes.
Inclusion Criteria. (1) Patients were diagnosed with pancreatic ductal adenocarcinoma through pathological or imaging examinations and staged as I-IV according to the AJCC 8th Edition staging system (79). (2) Patients were aged over 18, had no significant cognitive impairment, and were capable of signing informed consent independently. (3) Patients had an expected survival period of at least 3 months, as assessed by tumor oncologists. (4) Patients were native Chinese speakers with no significant language barriers or reading difficulties.
Exclusion Criteria. (1) Patients with severe cognitive impairments, such as dementia, delirium, or active mental illnesses. (2) Patients who had undergone systematic psychological intervention or adjustment of psychotropic medications within the past 4 weeks. (3) Patients requiring long-term bed rest or completely lacking self-care ability. (4) Patients who had participated in other clinical trials involving psychological assessment within the past 3 months.
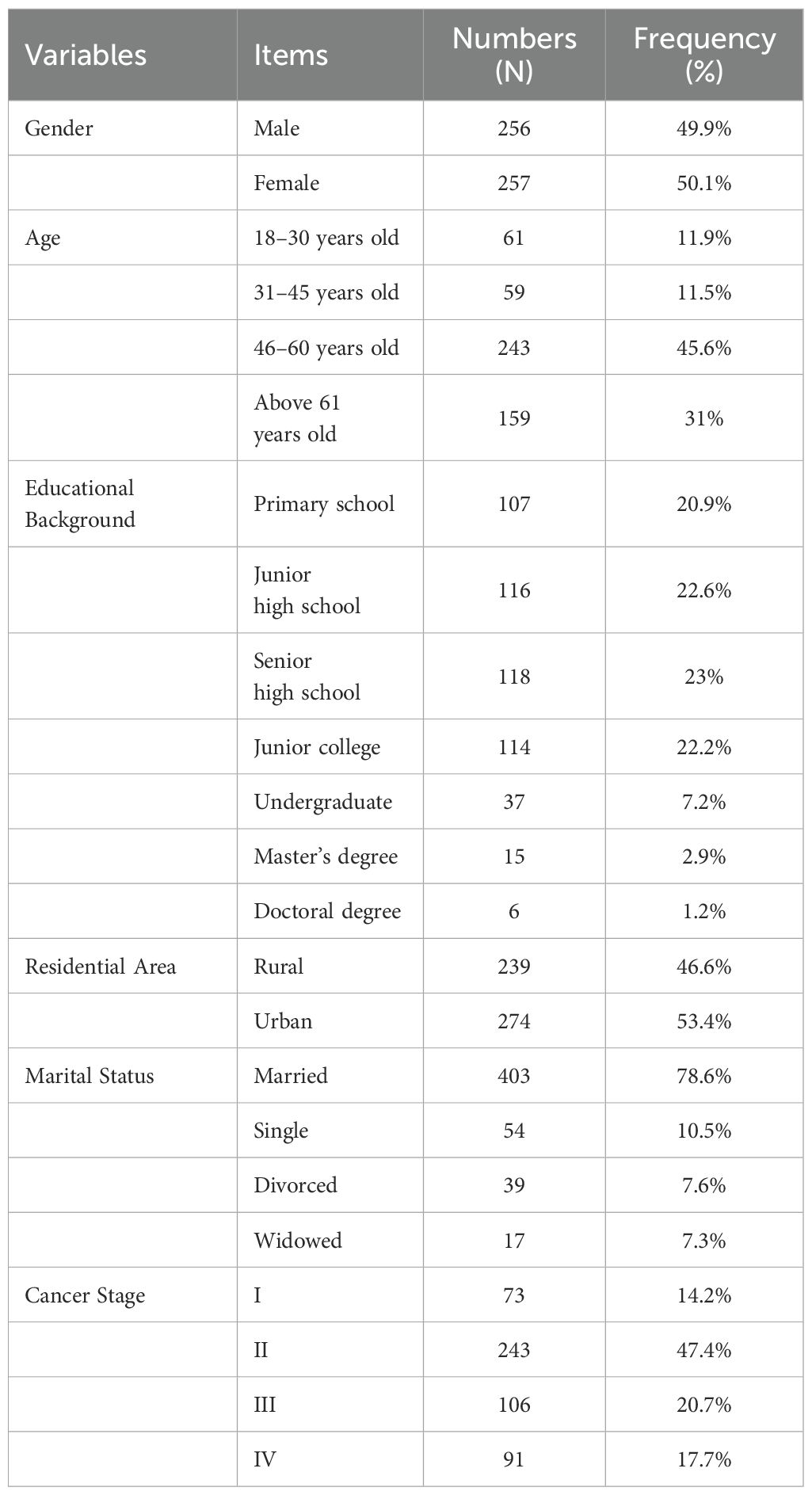
Data collection took place between June 2024 and December 2024. A total of 550 questionnaires were distributed, with 526 returned. During data cleaning, 13 questionnaires were excluded due to short time to fill (N=3), incomplete questionnaire filling (N=6), and too consistent responses (N=4). Given that 6 points of incomplete data had been excluded, there were no missing data at the item level in the remaining 513 questionnaires, and the list deletion method was used in descriptive and correlation analyses, which is recommended for low missing rates to minimize bias (80). For LPA and regression models, under the missing at random assumption, full information maximum likelihood estimation was used to account for any residual missing, ensuring unbiased parameter estimates (81). This resulted in 513 valid questionnaires, yielding an effective response rate of 93.27%. The sample included 256 male and 257 female patients. Detailed demographic information is provided in Table 1.
2.2 Measurement tools
2.2.1 Psychological Capital Scale
The Psychological Capital Scale used in this study was adapted from Zhang (82), consisting of 26 items across four dimensions: self-efficacy, resilience, hope, and optimism. This scale has been widely used among Chinese populations (83, 84) and has demonstrated strong cultural adaptability and reliability. For instance, Zhou et al. (85) employed this scale to measure psychological capital among Chinese nurses. The 26-item version was selected to assess psychological capital in patients with pancreatic cancer. Responses were collected using a 7-point Likert scale (1=“strongly disagree,” 7=“strongly agree”), with higher scores indicating more substantial psychological capital. The Cronbach’s α coefficient for this scale in the current study was 0.952.
2.2.2 Death Anxiety Scale
The Death Anxiety Scale was adapted from Templer (86), comprising 15 items across four dimensions: affective (6 items), stress and suffering (4 items), time awareness (2 items), and cognitive (3 items). This scale has been widely applied to measure death anxiety among Chinese cancer populations (67, 87) and was translated into Chinese and validated for cultural adaptability and reliability by Che et al. (88). All 15 items were used to assess death anxiety in pancreatic cancer patients. Responses were collected using a 7-point Likert scale (1=“strongly disagree,” 7=“strongly agree”), with higher scores indicating greater death anxiety. The Cronbach’s α coefficient for this scale was 0.882.
2.2.3 Social Support Scale
The Social Support Scale was adapted from Zimet et al. (89), consisting of 12 items across three dimensions: support from others, friends, and family. This scale has been widely used to measure social support among Chinese populations (120, 121) and has been translated into Chinese, validated for cultural adaptability, and tested for reliability by Yang et al. (90). All 12 items were used to assess social support in patients with pancreatic cancer. Responses were collected using a 7-point Likert scale (1=“strongly disagree,” 7=“strongly agree”), with higher scores indicating greater social support. The Cronbach’s α coefficient for this scale was 0.75.
2.2.4 Perceived Stress Scale
The Perceived Stress Scale was adapted from Cohen et al. (91), comprising 14 items. This scale was translated into Chinese, validated for cultural adaptability, and tested for reliability by Yang and Huang (92). All 14 items were used to assess perceived stress among pancreatic cancer patients. Responses were collected using a 7-point Likert scale (1=“strongly disagree,” 7=“strongly agree”), with higher scores indicating greater perceived stress. The Cronbach’s α coefficient for this scale was 0.857.
3 Result
3.1 Common method bias test
Following the approach used by Podsakoff et al. (93), we employed an anonymous data collection method to gather self-reported data from participants, thereby reducing potential biases in the responses. Subsequently, we utilized Harman’s single-factor test to examine common method bias. The results indicated that, without rotation, a total of 12 factors with eigenvalues greater than one were extracted. The first factor explained 24.114% of the variance, which did not exceed the critical threshold of 40%. This suggests that the study is free from issues related to common method bias.
3.2 Descriptive statistics and correlation analysis
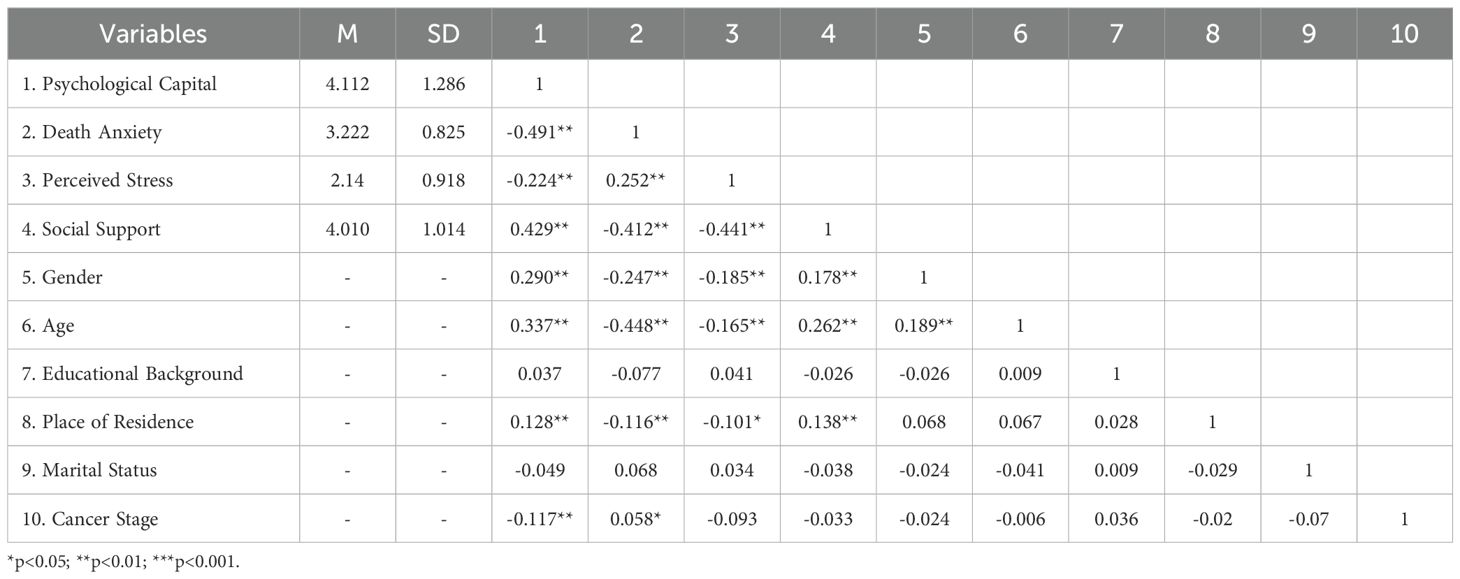
We conducted descriptive statistics and correlation analyses on psychological capital, death anxiety, social support, perceived stress, and demographic information among pancreatic cancer patients, as shown in Table 2. The results revealed the following significant correlations: psychological capital was negatively correlated with death anxiety (r=-0.491, P < 0.001) and perceived stress (r=-0.224, P < 0.001), and positively correlated with social support (r=0.429, P < 0.001). Death anxiety was negatively correlated with social support (r=-0.412, P < 0.001) and positively correlated with perceived stress (r=0.252, P < 0.001). Social support was negatively correlated with perceived stress (r=-0.441, P < 0.001). From a demographic perspective, gender was significantly correlated with psychological capital, death anxiety, perceived stress, and social support. Residence was also significantly correlated with psychological capital, death anxiety, perceived stress, and social support. Cancer stage was significantly correlated with psychological capital and death anxiety.
3.3 Latent profile analysis
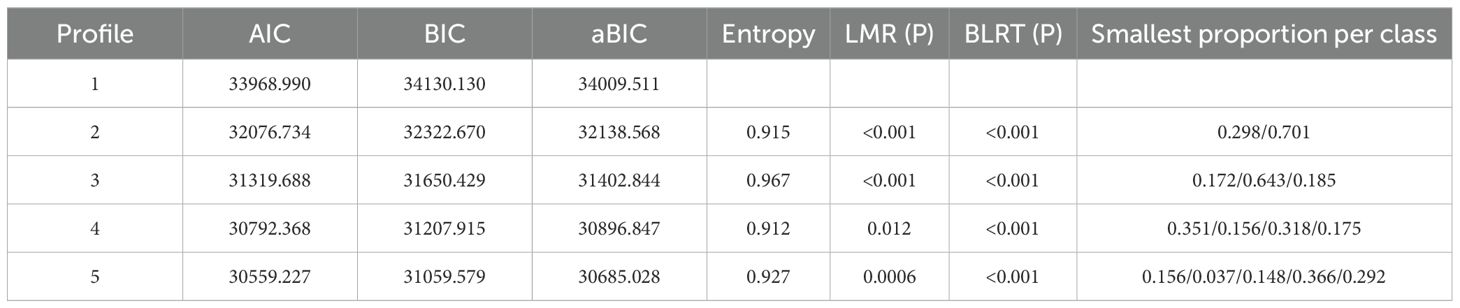
This study employed the LPA method to evaluate potential models with 1 to 5 latent profiles, aiming to determine the optimal fitting model, as detailed in Table 3. Analyses were conducted using Mplus version 8.3 (94) with robust maximum likelihood estimation to handle potential non-normality and provide bias-corrected standard errors. Models were estimated using 500 random starts and 100 final-stage optimizations to ensure convergence on global maxima. As the number of profiles increased, the information criteria AIC, BIC, and aBIC consistently decreased, indicating improved model fit. Furthermore, the Lo-Mendell-Rubin likelihood ratio test (LMRT) and the bootstrapped likelihood ratio test (BLRT) values remained significant. However, upon further comparison, we found that the Entropy value for the 3-profile model was significantly higher than those for the 2-, 4-, and 5-profile models. Entropy is primarily used to assess the accuracy of latent class assignment in a model, with values closer to 1 indicating better classification quality. Therefore, the 3-profile model was deemed more reasonable.
3.4 Subgroup classification
The latent profile analysis identified three subgroups, as illustrated in Figure 1. The first subgroup was labeled as “high psychological capital-low death anxiety,” accounting for 17.15% of the sample. The second subgroup was labeled as “moderate psychological capital-moderate death anxiety,” representing 64.33% of the sample. The third subgroup was named “low psychological capital-high death anxiety,” comprising 18.52% of the sample. This indicates that most pancreatic cancer patients exhibit some degree of death anxiety and psychological capital.

Figure 1. Potential profile results of psychological capital and death anxiety. The 1–4 items are the four dimensions of psychological capital, namely self-efficacy, resilience, hope, and optimism. The 5–19 items were death anxiety.
3.5 Single-factor analysis of psychological capital and death anxiety subgroups
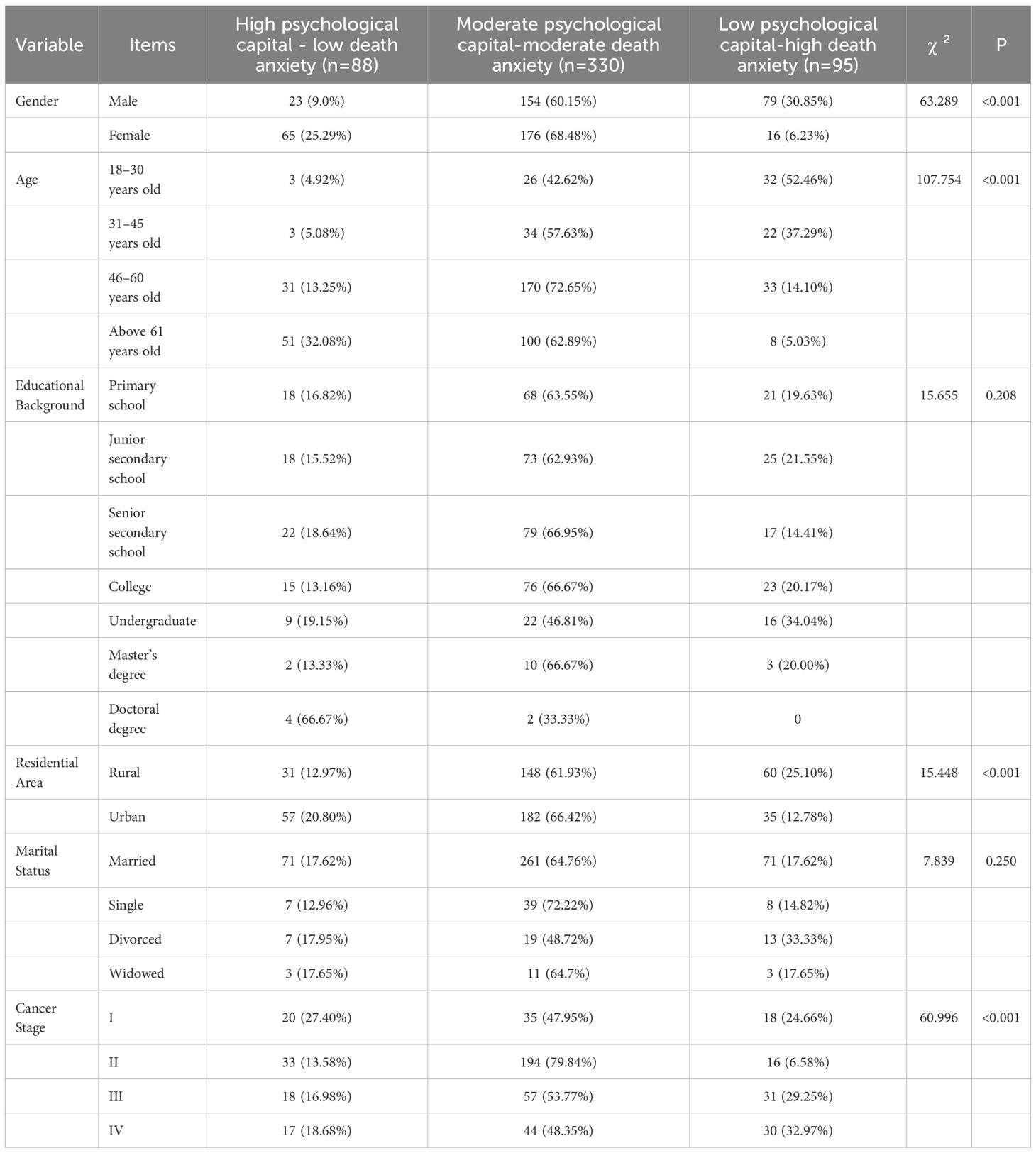
We compared the three psychological capital and death anxiety subgroups in terms of demographic characteristics, social support, and perceived stress using single-factor analysis. The results demonstrated significant differences in psychological capital and death anxiety across gender, age, residence, and cancer stage (P < 0.001). In contrast, no significant differences were found for education (P=0.208) or marital status (P=0.250). Further details are provided in Table 4.
3.6 Logistic regression analysis of factors influencing the latent categories of psychological capital and death anxiety
We treated the latent categories of psychological capital and death anxiety in pancreatic cancer patients as the dependent variables, using the variables with statistical significance from the single-factor analysis as independent variables. The “low psychological capital-high death anxiety” group was used as the reference category. Prior to regression, multicollinearity was assessed using Variance Inflation Factors (VIF), with all values ranging from 1.017 to 1.329 (mean VIF=1.137), well below the threshold of 5, indicating no multicollinearity issues (95). Unordered multinomial logistic regression analysis was conducted to examine the relationships.
Comparison of the high psychological capital-low death anxiety group with the reference group. The probability of males belonging to this group was significantly lower than that of females (OR=0.073, 95% CI=[0.030, 0.182], P < 0.001), suggesting that females are more likely to maintain high psychological capital and alleviate death anxiety. The probabilities of belonging to this group were significantly lower for the 18 - 30 (OR=0.011, P < 0.001), 31 - 45 (OR=0.053, P < 0.001), and 46 - 60 (OR=0.195, P=0.002) age groups compared to the above 61 years old age group, indicating that younger individuals exhibited lower psychological capital and higher death anxiety, possibly related to life stress or health risk perception. Rural residents had a significantly lower probability of belonging to this group compared to urban residents (OR=0.44, 95% CI=[0.196, 0.986], P=0.046). Stage II patients were significantly more likely to belong to this group than early-stage patients (OR=8.27, 95% CI=[2.56, 26.713], P < 0.001). Each unit increase in social support significantly increased the likelihood of belonging to this group by 6.6-fold (OR=6.602, P < 0.001), highlighting the reinforcing effect of social support on psychological capital.
Comparison of the moderate psychological capital-moderate death anxiety group with the reference group: The probability of males belonging to this group was also significantly lower than that of females (OR=0.18, 95% CI=[0.086, 0.378], P < 0.001), showing consistent gender differences across both groups. The probabilities for the 18 - 30 (OR=0.053, P < 0.001) and 31 - 45 (OR=0.172, P=0.002) age groups were significantly lower than that of the older age group, while the 46–60 age group showed no significant difference (P=0.106). Stage II patients were 10.07 times more likely to belong to this group than early-stage patients (OR=10.07, 95% CI=[4.089, 24.801], P < 0.001), indicating that disease progression exacerbates the co-occurrence of psychological capital and death anxiety. Increased social support significantly enhanced the likelihood of belonging to this group (OR=2.722, 95% CI=[1.893, 3.915], P < 0.001). However, this effect was weaker compared to the “high psychological capital-low death anxiety” group. Further details are provided in Tables 5–10.
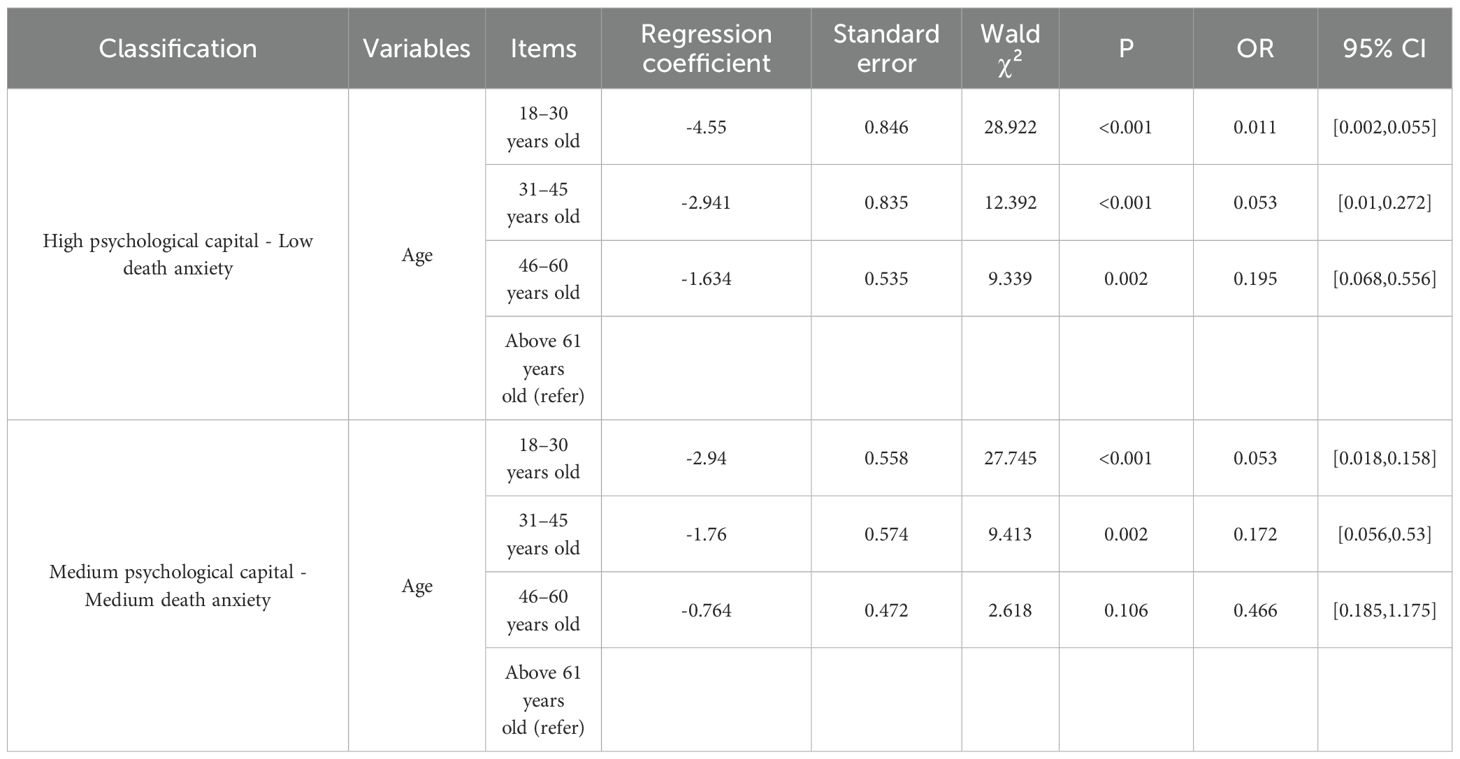
Table 5. Logistic regression analysis of factors influencing the latent categories of psychological capital and death anxiety (age).
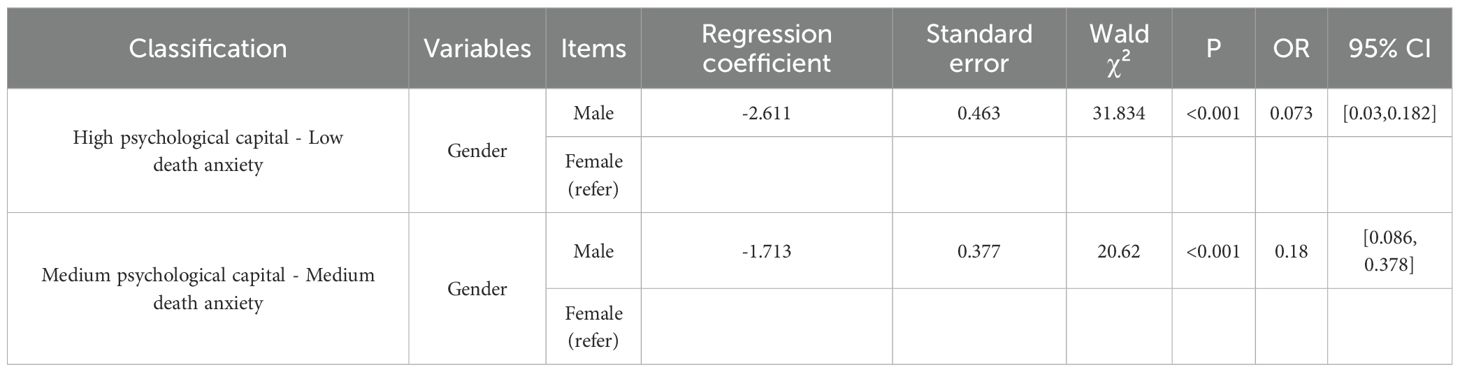
Table 6. Logistic regression analysis of factors influencing the latent categories of psychological capital and death anxiety (gender).
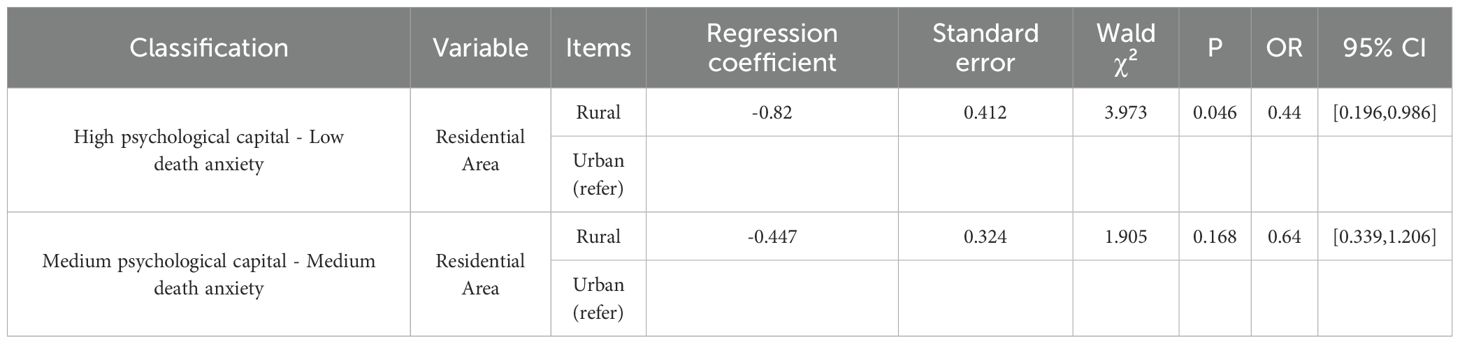
Table 7. Logistic regression analysis of factors influencing the latent categories of psychological capital and death anxiety (residential area).
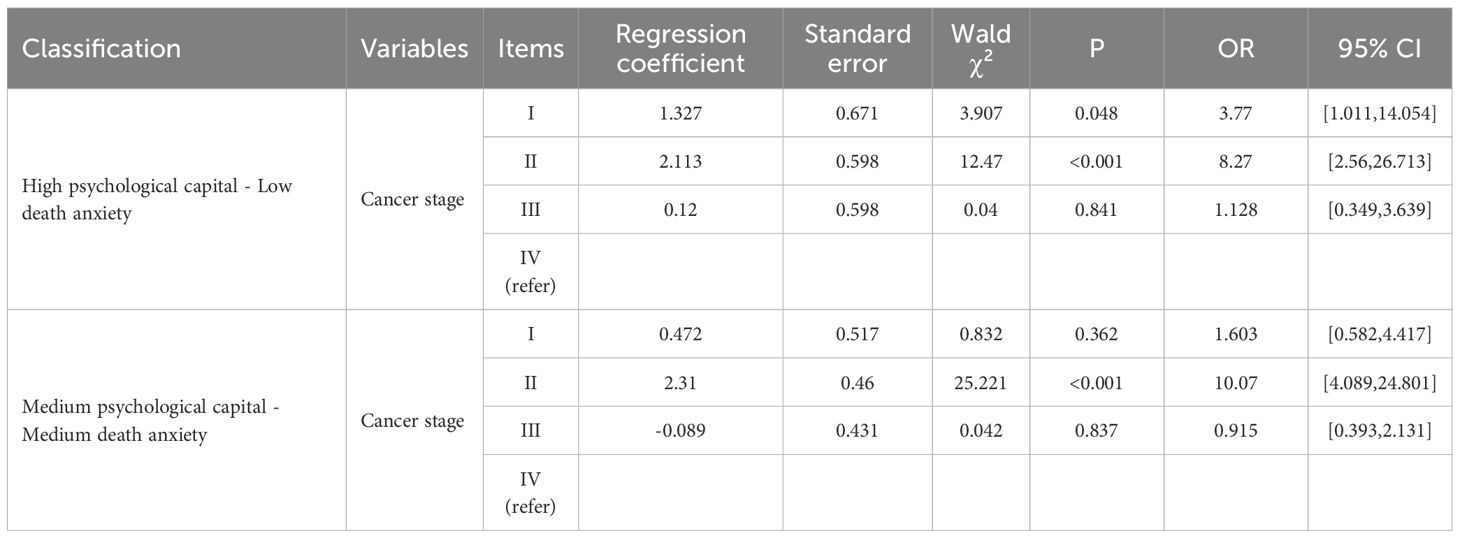
Table 8. Logistic regression analysis of factors influencing the latent categories of psychological capital and death anxiety (cancer stage).
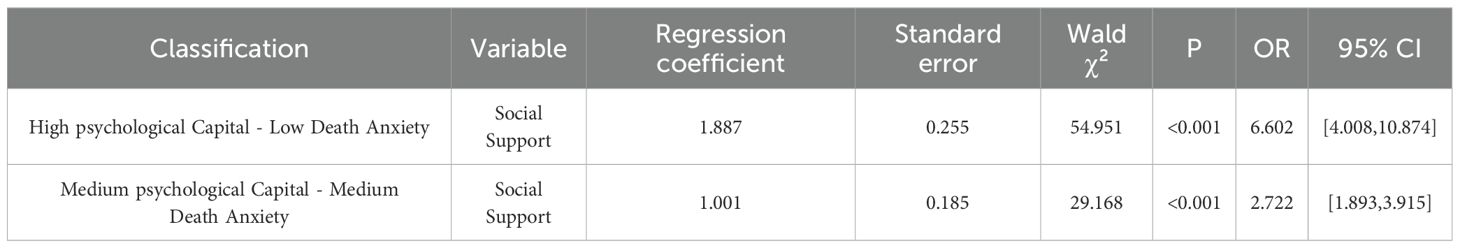
Table 9. Logistic regression analysis of factors influencing the latent categories of psychological capital and death anxiety (social support).

Table 10. Logistic regression analysis of factors influencing the latent categories of psychological capital and death anxiety (perceived stress).
4 Discussion
4.1 Latent profile analysis
This study employed the LPA method to investigate the heterogeneity of psychological capital and death anxiety among pancreatic cancer patients. Participants were categorized into three latent profiles: high psychological capital-low death anxiety, moderate psychological capital-moderate death anxiety, and low psychological capital-high death anxiety. The moderate psychological capital-moderate death anxiety group had the highest sample proportion. These findings partially align with previous studies. For instance, Teng et al. (96) identified similar classification patterns based on psychological factors in a study on nurses’ psychological capital. However, that study only focused on the heterogeneity of psychological capital and did not explore the distinct grouping characteristics of death anxiety among pancreatic cancer patients. The present study further advances the understanding of this specific patient population by providing detailed profiles of proportions and characteristics.
Based on social cognitive theory, psychological capital is viewed as an expression of individual behavior in different states (97). These states reflect an individual’s behavior at a specific moment and are a manifestation of their psychological capital. Psychological capital comprises elements such as self-efficacy, optimism, hope, and resilience. The varying combinations and levels of these elements result in diverse psychological states among patients when facing pancreatic cancer. Death anxiety, as a strong negative emotion, interacts with psychological capital. Patients with different traits exhibit varying dimensions of psychological capital when coping with the disease, leading to differences in the degree of death anxiety. These combinations of traits and states are manifested in real-life situations.
Among the three identified latent profiles, the “low psychological capital-high death anxiety” group represented a relatively small proportion. In contrast, the “moderate psychological capital-moderate death anxiety” group was significantly more representative. This suggests that the combination of moderate psychological capital and moderate death anxiety is a relatively common phenomenon in the pancreatic cancer patient population. Most patients do not possess extremely high psychological capital to cope with the disease effectively, nor do they have extremely low psychological capital, leading to complete despair. Instead, they hover between the two extremes, reflecting the complex psychological states of patients as they face the disease.
4.2 Analysis of influencing factors for different potential profiles
4.2.1 Gender
This study found that gender is a core variable distinguishing the combination of states of psychological capital and death anxiety. In the “high psychological capital-low death anxiety” group, males had a significantly lower probability of belonging to this group compared to females. This result is consistent with previous research suggesting that females tend to have higher psychological resilience than males (98, 99). Social role theory posits that women tend to assume more emotional support roles in both family and society, potentially accumulating psychological resources through more frequent emotional expression and social interactions (100). Additionally, neuroendocrinological studies suggest that estrogen’s regulatory role in stress responses may enhance women’s ability to buffer death anxiety (101). However, this advantage may come at a cost, as women’s heightened vigilance to health threats may increase the risk of death anxiety (102). Nevertheless, the present study found that women still exhibited higher psychological capital, suggesting that they effectively transformed potential anxiety through social support networks.
Notably, gender differences remained significant in the “moderate psychological capital-moderate death anxiety” group, albeit with a reduced effect size, indicating that the protective effect of gender on psychological capital diminishes as death anxiety levels increase. When external pressures exceed the capacity of the social support system, the influence of gender differences on psychological resources may weaken (103).
4.2.2 Age
Significant nonlinear trends characterized the relationship between age and psychological capital-death anxiety. The probability of 18 - 30-year-olds belonging to the “high psychological capital-low death anxiety” group was only 0.011 of that of older individuals. From a developmental psychology perspective, young adults face multiple transitional pressures, such as career orientation and economic independence, which may deplete short-term psychological capital (104). Additionally, the U-shaped curve theory of death anxiety suggests that young individuals’ conceptualization of death is less mature, and sudden health events (e.g., a cancer diagnosis) may trigger existential fear (105). In contrast, the 46–60 age group exhibited transitional characteristics, possibly reflecting the accumulation of psychological resources through life experiences, albeit still constrained by responsibilities such as childcare and care for the elderly. Notably, the oldest group (61 years and above) had the highest probability of belonging to the high psychological capital group, consistent with the paradox of aging theory. Older adults may alleviate anxiety by accepting death and reconstructing meaning (106). However, this advantage may be influenced by sample selection bias, as late-stage cancer patients are often older and may not have been fully included in the study.
4.2.3 Residence
Residence significantly influenced the patterns of psychological capital and death anxiety. The probability of rural residents belonging to the “high psychological capital-low death anxiety” group was only 44% of that of urban residents, highlighting the profound impact of structural health inequalities. This may be attributed to the insufficient coverage of mental health services in rural areas, which is only one-third of that in urban areas (107), and the stigma that deters help-seeking behavior (108). Interestingly, urban-rural differences were not statistically significant in the “moderate psychological capital-moderate death anxiety” group, suggesting that structural factors may be buffered by individual resilience when psychological capital and anxiety are balanced.
4.2.4 Cancer stage
The influence of cancer stage on psychological capital revealed significant phase-specific characteristics. The probability of Stage II patients belonging to the “high psychological capital-low death anxiety” group was 8.27 times higher than that of early-stage patients. According to post-traumatic growth theory, the initial shock of a disease diagnosis (Stage I) may disrupt psychological equilibrium. In contrast, Stage II patients, after initial adaptation, may reactivate psychological capital through meaning-seeking (e.g., reevaluating life values) and regaining control (109). However, late-stage patients (Stage III/IV) did not show significant associations, possibly due to the nonlinear depletion of psychological resources. When disease progression exceeds individual coping thresholds, psychological capital may collapse even with social support (110). Notably, Stage II patients had a 10.07-fold increased risk of belonging to the “moderate psychological capital-moderate death anxiety” group, suggesting that mid-disease psychological adaptation is a dynamic balancing process rather than a unidirectional improvement.
4.2.5 Social support
According to the social support buffering theory, social support networks not only alleviate stress but also actively construct psychological resources. Instrumental support may enhance a sense of disease control, emotional support promotes positive emotions, and affiliational support (e.g., peer groups) reconstructs self-concept through social identification (111). Notably, the effect of social support on the “moderate psychological capital-moderate death anxiety” group weakened to an OR of 2.722, consistent with the law of diminishing marginal utility. When death anxiety reaches moderate levels, the transformation efficiency of the support system may decrease. This suggests that interventions should be designed in layers: for high-anxiety groups, structured support should be prioritized, while for moderate-anxiety groups, the quality of support networks should be optimized. Digital support tools may overcome the spatial and temporal limitations of traditional support, but their effectiveness requires further evidence-based validation.
This study revealed that social support is a core driver for enhancing psychological capital and alleviating death anxiety, with its effect exceeding the influence of demographic and clinical variables. This finding corroborates the universality of the social support buffering theory (112). Social support operates through its instrumental, emotional, and affiliational dimensions. Instrumental support directly reduces objective stress loads and enhances disease control (113); emotional support regulates anxiety responses by modulating neural circuits (114); and affiliational support reconstructs social identities, transforming patients into survivors and strengthening psychological resilience (115). However, in the “moderate psychological capital-moderate death anxiety” group, the effect size of social support weakened to OR=2.722 (95% CI=[1.893, 3.915], p < 0.001), aligning with the stress-support dynamic balance model (116). This suggests the need for layered intervention strategies: for high-anxiety groups, prioritize structured instrumental support, while for moderate-anxiety groups, focus on enhancing the quality of emotional support.
4.2.6 Perceived stress
This study found that the individual perceived stress level had no significant predictive power for the latent profile of psychological capital and death anxiety. This seemingly counterintuitive result in fact profoundly reflects the psychological adaptation mechanism in the unique disease context of advanced pancreatic cancer. Pancreatic cancer itself constitutes an overwhelming and persistent threat to survival due to its high degree of malignancy, poor prognosis (117), and often accompanied by severe pain and digestive dysfunction. In this context, the patient’s cognitive assessment of the disease itself and the primary stress response triggered by it may become the influencing factors that dominate the patient’s psychological state (118). In contrast, the intensity and salience of general perceived stressors in daily life may be weakened or decentralized in the face of extreme survival crises. In other words, when individuals are exposed to the ultimate stress situation of advanced pancreatic cancer, their perception of stress is fundamentally reconstructed. The importance of daily stressors is relatively diminished, and the disease itself and the threats related to its existential meaning become the overwhelming cognitive focus. This cognitive reappraisal process may be the core psychological mechanism responsible for the insignificant effect of general perceived stress on deep psychological profiles. At the same time, individuals may develop specific psychological resilience or emotional numbness in the long-term process of coping with extreme disease stress (119), which alters their sensitivity to stress and further cushions the impact of perceived stress on deep psychological structures.
However, this result may also be limited by the study design and measurement tools. Factors such as the size of the sample, the selection criteria of the study subjects, and the sensitivity of the measurement instrument may affect the stability of the results. Future studies with larger sample sizes and more rigorous study designs are needed to verify the robustness of this finding. At the same time, it is necessary to further analyze whether perceived stress may act as a regulatory mechanism to affect the relationship between them, which will help to better understand the psychological adaptation process of pancreatic cancer patients. In clinical practice, while paying attention to the physiological symptoms of patients, clinical medical staff should pay attention to the assessment and intervention of psychological capital, improve the psychological resilience of patients through psychological support and psychological intervention, so as to improve their overall quality of life.
4.3 Practical implications
From a practical perspective, this study offers valuable guidance for psychological interventions in patients with pancreatic cancer. First, the results indicate that psychological capital and social support are key factors in alleviating death anxiety. Therefore, clinical psychological interventions should focus on enhancing psychological capital and building social support systems. Specifically, interventions such as psychological counseling, support groups, and family therapy can be employed to strengthen patients’ psychological capital and improve their social support networks. Particularly for patients in the “low psychological capital-high death anxiety” category, more personalized and intensified psychological support measures are recommended to alleviate their death anxiety and improve their quality of life.
This study also provides a stratified practical strategy for psychological interventions in pancreatic cancer patients. Through latent profile analysis, the study categorizes patients into three groups, each with distinct psychological characteristics and clinical needs. For example, patients in the “high psychological capital-low death anxiety” group may require less professional psychological intervention. In contrast, those in the “moderate psychological capital-moderate death anxiety” group may need stable psychological support and follow-up services. In contrast, patients in the “low psychological capital-high death anxiety” group should be prioritized for psychological interventions. This classification strategy can help clinicians more accurately identify high-risk patients and develop personalized psychological intervention plans tailored to their needs.
The data further show that each unit increase in social support significantly increases the probability of patients belonging to the “high psychological capital-low death anxiety” group. This suggests that healthcare institutions should actively help patients construct their social support networks, including family, friends, and community resources. Especially in rural areas with relatively scarce resources, healthcare institutions should strengthen collaboration with community resources to provide patients with more external support. Additionally, younger patients (18–45 years) may face higher life pressures and health risk perceptions and should receive special attention regarding their mental health needs.
The study found that females, urban residents, and Stage II patients exhibited significantly better psychological health, likely due to their greater access to high-quality medical resources and social support. Therefore, policymakers should focus on the mental health issues of rural residents and early-stage patients to ensure the equitable distribution of mental health resources. Furthermore, this study emphasizes the importance of interdisciplinary collaboration, suggesting the integration of psychology, sociology, and clinical medicine to establish a comprehensive system for managing mental health. Through cross-departmental collaboration, high-risk individuals can be screened more effectively, and timely psychological interventions can be provided to improve the overall survival quality and mental health of pancreatic cancer patients.
4.4 Limitations
Although this study incorporated randomization at the recruitment centers and random selection from lists of eligible patients at participating hospitals, it primarily employed convenience sampling. The data were exclusively collected from multiple tertiary grade A hospitals in Nanchong and Xi’an, which inherently limited the geographic, socioeconomic, and cultural diversity. For instance, the urban bias in the sample may have overestimated the protective effect of urban residency on psychological capital, as rural patients often face greater barriers, such as limited access to mental health services and stigmatization. Therefore, the generalizability of the findings is restricted and may not fully represent pancreatic cancer patients in either Chinese or international contexts, where regional disparities in healthcare resources could influence patients’ psychological states. Future studies should adopt multicenter, stratified random sampling across diverse settings, including rural and international locations, to enhance external validity and validate subgroup proportions.
The cross-sectional design further precluded causal inferences between variables, such as whether social support directly enhances psychological capital or whether bidirectional effects exist. The inability to track temporal dynamics further complicates this limitation. For example, the higher psychological capital observed in stage II patients may reflect post-diagnosis adaptation rather than a causal relationship, yet unmeasured variables, such as the timing of chemotherapy or surgery, were not controlled for, potentially leading to confounded results. Similarly, the single-time-point latent profile analysis classification cannot capture within-individual changes in subgroup membership. To address these limitations, future research is recommended to adopt longitudinal designs with repeated measurements and causal models, such as cross-lagged panel analysis or propensity score matching, which could integrate treatment timelines and thereby distinguish acute from chronic effects on death anxiety.
Moreover, this study did not comprehensively assess potential confounding factors, including cultural norms, religious beliefs, and work-family conflicts. These omissions introduced biased estimates in multivariate analyses, as single-variable results already indicated demographic influences, but without deeper exploration of mediating pathways. The lack of biomarkers or physiological indicators further reduced the ability to link psychosocial findings to potential disease mechanisms, such as how heightened death anxiety might accelerate pancreatic cancer progression through neuroendocrine dysregulation. Future studies should employ structural equation modeling to test mediating/moderating factors, use mixed methods for qualitative analyses of cultural/familial factors, and integrate multi-omics data with longitudinal tracking to develop dynamic biopsychosocial predictive models. These approaches not only enhance subgroup classification but also provide precise interventions based on patients’ evolving needs.
5 Conclusion
This study reveals the heterogeneous interplay between psychological capital and death anxiety among pancreatic cancer patients through latent profile analysis, identifying three distinct subgroups characterized by varying levels of psychological resilience and existential distress. The significant negative correlation between psychological capital and death anxiety, coupled with the protective role of social support, underscores the critical importance of psychosocial resources in mitigating emotional burden. Notably, demographic disparities—such as younger age, male gender, rural residency, and advanced cancer stages—highlight the need for culturally sensitive interventions tailored to vulnerable populations. While the findings advance theoretical frameworks by integrating dynamic interactions between psychological states and socio-environmental factors, limitations in sample diversity and cross-sectional design necessitate longitudinal and multicentric validation. Future research should prioritize biopsychosocial models that link psychological interventions (e.g., narrative therapy for death anxiety) with biomarkers of stress and immune function, ultimately fostering precision medicine strategies to enhance holistic care for pancreatic cancer patients.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Committee of North Sichuan Medical College. The studies were conducted in accordance with the local legislation and institutional requirements. All procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The participants provided their written informed consent to participate in this study.
Author contributions
DY: Data curation, Investigation, Project administration, Software, Visualization, Writing–original draft, Writing – review & editing. TS: Conceptualization, Data curation, Investigation, Validation, Writing – original draft, Writing – review & editing. GG: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. LWL: Conceptualization, Data curation, Investigation, Project administration, Writing – original draft, Writing – review & editing. ZZ: Conceptualization, Data curation, Investigation, Supervision, Writing – original draft, Writing – review & editing. LL: Conceptualization, Formal analysis, Investigation, Project administration, Supervision, Writing – original draft, Writing – review & editing. NL: Data curation, Investigation, Project administration, Software, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, and/or publication of this article. This study was supported by the Sichuan Science and Technology Program [Grant No. 2024ZYD0272,2024 NSFSC2017].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1627422/full#supplementary-material
References
1. Kleeff J, Michalski C, Friess H, and Büchler MW. Pancreatic cancer: from bench to 5-year survival. Pancreas. (2006) 33:111–8. doi: 10.1097/01.mpa.0000229010.62538.f2
2. Li J, Li Y, Chen C, Guo J, Qiao M, and Lyu J. Recent estimates and predictions of 5-year survival rate in patients with pancreatic cancer: A model-based period analysis. Front Med. (2022) 9:1049136. doi: 10.3389/fmed.2022.1049136
3. Khalaf N, El-Serag HB, Abrams HR, and Thrift AP. Burden of pancreatic cancer: from epidemiology to practice. Clin Gastroenterol Hepatol. (2021) 19:876–84. doi: 10.1016/j.cgh.2020.02.054
4. Ajina R and Weiner LM. T-cell immunity in pancreatic cancer. Pancreas. (2020) 49:1014–23. doi: 10.1097/MPA.0000000000001621
5. Huang J, Lok V, Ngai CH, Zhang L, Yuan J, Lao XQ, et al. Worldwide burden of, risk factors for, and trends in pancreatic cancer. Gastroenterology. (2021) 160:744–54. doi: 10.1053/j.gastro.2020.10.007
6. Ilic M and Ilic I. Epidemiology of pancreatic cancer. World J Gastroenterol. (2016) 22:9694. doi: 10.3748/wjg.v22.i44.9694
7. Bibby N, Rajai A, and O’Reilly DA. From prehab to rehab: Nutritional support for people undergoing pancreatic cancer surgery. J Hum Nutr Dietetics. (2023) 36:493–503. doi: 10.1111/jhn.13040
8. Mękal D, Sobocki J, Badowska-Kozakiewicz A, Sygit K, Cipora E, Bandurska E, et al. Evaluation of nutritional status and the impact of nutritional treatment in patients with pancreatic cancer. Cancers. (2023) 15:3816. doi: 10.3390/cancers15153816
9. Ruze R, Song J, Yin X, Chen Y, Xu R, Wang C, et al. Mechanisms of obesity-and diabetes mellitus-related pancreatic carcinogenesis: a comprehensive and systematic review. Signal transduction targeted Ther. (2023) 8:139. doi: 10.1038/s41392-023-01376-w
10. Yaman G, Kayikçioğlu E, and Hocaoğlu Ç. Examination of mental symptoms, anger, and death anxiety in elderly cancer patients. Turk Geriatri Dergisi. (2023) 26. doi: 10.29400/tjgeri.2023.357
11. Akizuki N, Shimizu K, Asai M, Nakano T, Okusaka T, Shimada K, et al. Prevalence and predictive factors of depression and anxiety in patients with pancreatic cancer: a longitudinal study. Japanese J Clin Oncol. (2016) 46:71–7. doi: 10.1093/jjco/hyv169
12. Mercês C, Souto J, Zaccaro KRL, de Souza JF, Primo CC, and Brandão MAG. Death anxiety: concept analysis and clarification of nursing diagnosis. Int J Nurs Knowl. (2020) 31:218–27. doi: 10.1111/2047-3095.12260
13. Lehto R and Stein KF. Death anxiety: An analysis of an evolving concept. Hanover, Pennsylvania: Springer Publishing Company. (2009). doi: 10.1891/1541-6577.23.1.23.
14. Benton JP, Christopher AN, and Walter MI. Death anxiety as a function of aging anxiety. Death Stud. (2007) 31:337–50. doi: 10.1080/07481180601187100
15. Dursun P, Alyagut P, and Yılmaz I. Meaning in life, psychological hardiness and death anxiety: individuals with or without generalized anxiety disorder (GAD). Curr Psychol. (2022) 41:3299–317. doi: 10.1007/s12144-021-02695-3
16. Alijaniha F, Noorbala A, Afsharypuor S, Naseri M, Fallahi F, Mosaddegh M, et al. Relationship between palpitation and mental health. Iranian Red Crescent Med J. (2016) 18:e22615. doi: 10.5812/ircmj.22615
17. Yıldız E, Taskin Yilmaz F, and Karagözoğlu Ş. The relationship between spiritual care needs and death anxiety in turkish patients with chronic obstructive pulmonary disease. J Religion Health. (2025), 1–14. doi: 10.1007/s10943-025-02284-9
18. Yan Y, Chen Y, Ou M, Gong Y, Yang R, Liu X, et al. The mediating role of meaning in life between experiential avoidance and death anxiety among cancer patients: a cross-sectional study. BMC Cancer. (2024) 24:663. doi: 10.1186/s12885-024-12433-0
19. Menzies RE, Sharpe L, and Dar-Nimrod I. The relationship between death anxiety and severity of mental illnesses. Br J Clin Psychol. (2019) 58:452–67. doi: 10.1111/bjc.12229
20. Menzies RE, Brown J, and Marchant J. To die, to sleep”: A systematic review and meta-analysis of the relationship between death anxiety and sleep. J Anxiety Disord. (2025) 103001. doi: 10.1016/j.janxdis.2025.103001
21. Zuccala M, Modini M, and Abbott MJ. The role of death fears and attachment processes in social anxiety: A novel hypothesis explored. Aust J Psychol. (2021) 73:381–91. doi: 10.1080/00049530.2021.1917307
22. Kolva E, Rosenfeld B, Pessin H, Breitbart W, and Brescia R. Anxiety in terminally ill cancer patients. J Pain symptom Manage. (2011) 42:691–701. doi: 10.1016/j.jpainsymman.2011.01.013
23. Gui G, Yang D, Liu Y, Yao Y, Xie X, Liu R, et al. How family support alleviates death anxiety in breast cancer patients: the mediating role of meaning in life. Front Public Health. (2025) 13:1567485. doi: 10.3389/fpubh.2025.1567485
24. Han B, Zheng R, Zeng H, Wang S, Sun K, Chen R, et al. Cancer incidence and mortality in Chin. J Natl Cancer Cent. (2024) 4:47–53. doi: 10.1016/j.jncc.2024.01.006
25. Kenner BJ. Early detection of pancreatic cancer: the role of depression and anxiety as a precursor for disease Vol. 47. Amsterdam, The Netherlands: LWW (2018) p. 363–7.
26. Koopmann BD, Omidvari AH, Lansdorp-Vogelaar I, Cahen DL, Bruno MJ, and de Kok IM. The impact of pancreatic cancer screening on life expectancy: A systematic review of modeling studies. Int J Cancer. (2023) 152:1570–80. doi: 10.1002/ijc.34379
27. Zhang R, Wang J, Zhang P, Zhang Z, and Miao R. Pancreatic cancer progression and mortality predicted by depression and anxiety: a systematic review and meta-analysis protocol. Front Psychiatry. (2024) 14:1266502. doi: 10.3389/fpsyt.2023.1266502
28. Haeberle L and Esposito I. Pathology of pancreatic cancer. Trans Gastroenterol Hepatol. (2019) 4:50. doi: 10.21037/tgh.2019.06.02
29. Kolbeinsson HM, Chandana S, Wright GP, and Chung M. Pancreatic cancer: a review of current treatment and novel therapies. J Invest Surg. (2023) 36:2129884. doi: 10.1080/08941939.2022.2129884
30. Afrashteh MY, Majzoobi MR, Janjani P, and Forstmeier S. The relationship between the meaning of life, psychological well-being, self-care, and social capital, with depression and death anxiety in the elderly living in nursing homes: The mediating role of loneliness. Heliyon. (2024) 10(9). doi: 10.1016/j.heliyon.2024.e30124
31. Lei R, Zhang M, Gui G, Yang D, and He L. How perceived risk of recurrence strengthens health management awareness in stroke patients: the chain mediating role of risk fear and health literacy. Front Public Health. (2025) 13:1524492. doi: 10.3389/fpubh.2025.1524492
32. Salehi R and Rabiee M. investigating the role of Self-Compassion and Psychological Capital (hope, resilience, Self-efficacy and Optimism) in predicting depression and death anxiety in Patients with Cancer. Rooyesh-e-Ravanshenasi J (RRJ). (2020) 9:103–14.
33. Çavuş MF and Gökçen A. Psychological capital: Definition, components and effects. Br J Education Soc Behav Sci. (2015) 5:244–55. doi: 10.9734/BJESBS/2015/12574
34. Luthans F and Youssef-Morgan CM. Psychological capital: An evidence-based positive approach. Annu Rev organizational Psychol organizational Behav. (2017) 4:339–66. doi: 10.1146/annurev-orgpsych-032516-113324
35. Wang Y, Bao S, and Chen Y. How does social media use influence the mental health of pancreatic cancer patients: a chain mediating effect of online social support and psychological resilience. Front Public Health. (2023) 11:1166776. doi: 10.3389/fpubh.2023.1166776
36. Chen J, Chen L, Yu J, Xu Y, Wang X, Zeng Z, et al. Meta-analysis of current chemotherapy regimens in advanced pancreatic cancer to prolong survival and reduce treatment-associated toxicities. Mol Med Rep. (2019) 19:477–89. doi: 10.3892/mmr.2018.9638
37. Hu ZI and O’Reilly EM. Therapeutic developments in pancreatic cancer. Nat Rev Gastroenterol Hepatol. (2024) 21:7–24. doi: 10.1038/s41575-023-00840-w
38. Yeo TP, Hruban RH, Leach SD, Wilentz RE, Sohn TA, Kern SE, et al. Pancreatic cancer. Curr problems Cancer. (2002) 26:176–275. doi: 10.1067/mcn.2002.129579
39. Chung V, Sun V, Ruel N, Smith TJ, and Ferrell BR. Improving palliative care and quality of life in pancreatic cancer patients. J Palliative Med. (2022) 25:720–7. doi: 10.1089/jpm.2021.0187
40. Wong SS, George TJ, Godfrey M, Le J, and Pereira DB. Using photography to explore psychological distress in patients with pancreatic cancer and their caregivers: a qualitative study. Supportive Care Cancer. (2019) 27:321–8. doi: 10.1007/s00520-018-4330-y
41. Klute KA, Lukas L, Hwang S, Gwon Y, Krishnan M, Grem J, et al. Abstract C001: A pilot study of palliadelic treatment with psilocybin to reduce psychological distress and improve quality of life in patients with advanced pancreatic adenocarcinoma. Cancer Res. (2024) 84:C001–1. doi: 10.1158/1538-7445.PANCA2023-C001
42. Pichardo R, Jacob B, Jamil M, Jamil D, Raslan S, Rose CM, et al. Patient-reported and clinical outcomes among patients with pancreatic cancer. Am Soc Clin Oncol. (2024) 42:e23200–e23200. doi: 10.1200/JCO.2024.42.16_suppl.e23200
43. Choi JW, Park E-C, Kim TH, and Han E. Mental disorders and suicide risk among cancer patients: a nationwide cohort study. Arch suicide Res. (2022) 26:44–55. doi: 10.1080/13811118.2020.1779156
44. Elberg Dengsø K, Thomsen T, Christensen BM, Sørensen CL, Galanakis M, Dalton SO, et al. Physical and psychological symptom burden in patients and caregivers during follow-up care after curative surgery for cancers in the pancreas, bile ducts or duodenum. Acta Oncol. (2023) 62:782–93. doi: 10.1080/0284186X.2023.2185541
45. Cui CY, Wang Y, Zhang Y, Chen S, Jiang N, and Wang L. The development and validation of the psychological capital questionnaire for patients with Cancer the psychological capital questionnaire. BMC Cancer. (2021) 21:1–8. doi: 10.1186/s12885-021-08960-9
46. Xu H, Liu X, and Zeng P. The mediating role of social support in the relationship between psychological capital and depression among Chinese emergency physicians. Psychol Res Behav Manage. (2022), 977–90. doi: 10.2147/PRBM.S360611
47. Befecadu FBP, Perrenoud B, Behaghel G, Jaques C, Pautex S, Rodrigues MGDR, et al. Experience of hope in adult patients with advanced chronic disease and their informal caregivers: a qualitative systematic review protocol. JBI evidence synthesis. (2022) 20:2025–31. doi: 10.11124/JBIES-21-00364
48. Loučka M, Althouse AD, Arnold RM, Smith TJ, Smith KJ, White DB, et al. Hope and illness expectations: A cross-sectional study in patients with advanced cancer. Palliative Med. (2024) 38:131–9. doi: 10.1177/02692163231214422
49. Gawronski KA, Kim ES, Langa KM, and Kubzansky LD. Dispositional optimism and incidence of cognitive impairment in older adults. Psychosomatic Med. (2016) 78:819–28. doi: 10.1097/PSY.0000000000000345
50. Merluzzi TV, Pustejovsky JE, Philip EJ, Sohl SJ, Berendsen M, and Salsman JM. Interventions to enhance self-efficacy in cancer patients: a meta-analysis of randomized controlled trials. Psycho-Oncology. (2019) 28:1781–90. doi: 10.1002/pon.5148
51. Zhang M, Chan SW-C, You L, Wen Y, Peng L, Liu W, et al. The effectiveness of a self-efficacy-enhancing intervention for Chinese patients with colorectal cancer: a randomized controlled trial with 6-month follow up. Int J Nurs Stud. (2014) 51:1083–92. doi: 10.1016/j.ijnurstu.2013.12.005
52. Zanatta F, Maffoni M, and Giardini A. Resilience in palliative healthcare professionals: a systematic review. Supportive Care Cancer. (2020) 28:971–8. doi: 10.1007/s00520-019-05194-1
53. Marinelli V, Danzi OP, Mazzi MA, Secchettin E, Tuveri M, Bonamini D, et al. PREPARE: PreoPerative Anxiety REduction. One-year feasibility RCT on a brief psychological intervention for pancreatic cancer patients prior to major surgery. Front Psychol. (2020) 11:362. doi: 10.3389/fpsyg.2020.00362
54. Del Piccolo L, Marinelli V, Mazzi MA, Danzi OP, Bonamini D, Secchettin E, et al. Prevalence of depression in a cohort of 400 patients with pancreatic neoplasm attending day hospital for major surgery: role on depression of psychosocial functioning and clinical factors. Psycho-Oncology. (2021) 30:455–62. doi: 10.1002/pon.5607
55. Buchheim A, Viviani R, Kessler H, Kächele H, Cierpka M, Roth G, et al. Changes in prefrontal-limbic function in major depression after 15 months of long-term psychotherapy. PloS One. (2012) 7:e33745. doi: 10.1371/journal.pone.0033745
56. Riedel P, Heil M, Bender S, Dippel G, Korb FM, Smolka MN, et al. Modulating functional connectivity between medial frontopolar cortex and amygdala by inhibitory and excitatory transcranial magnetic stimulation. Hum Brain Mapp. (2019) 40:4301–15. doi: 10.1002/hbm.24703
57. Yao Y, Ge L, Yu Q, Du X, Zhang X, Taylor-Piliae R, et al. The effect of Tai Chi Chuan on emotional health: potential mechanisms and prefrontal cortex hypothesis. Evidence-Based Complementary Altern Med. (2021) 2021:5549006. doi: 10.1155/2021/5549006
58. Li Y, Dong W, Tang H, Guo X, Wu S, Lu G, et al. Correlates of death anxiety for patients with cancer: A systematic review and meta-analysis. J Clin Nurs. (2024) 33:1933–47. doi: 10.1111/jocn.17021
59. Nia HS, Lehto RH, Ebadi A, and Peyrovi H. Death anxiety among nurses and health care professionals: A review article. Int J Community based Nurs midwifery. (2016) 4:2.
60. Eisma MC, de Lang TA, and Boelen PA. How thinking hurts: Rumination, worry, and avoidance processes in adjustment to bereavement. Clin Psychol Psychother. (2020) 27:548–58. doi: 10.1002/cpp.2440
61. Zia T and Aslam N. Rumination, death anxiety and coping among students after terrorist attacks in universities. Bahria J Prof Psychol. (2018) 17:17.
62. Hoelterhoff M and Chung MC. Resilience against death anxiety in the face of trauma; the role of self-efficacy. Compr Psychiatry. (2013) 54:e24. doi: 10.1016/j.comppsych.2013.07.027
63. Zheng R, Bloomer MJ, Guo Q, and Lee SF. New graduate nurses’ coping with death and the relationship with death self-efficacy and death anxiety: A multicentre cross-sectional study. J advanced Nurs. (2021) 77:795–804. doi: 10.1111/jan.14621
64. Evram G and Çakici Eş A. Investigation of personal factors affecting existential anxiety: A model testing study. Curr Psychol. (2020) 39:1535–42. doi: 10.1007/s12144-020-00947-2
65. Farkas A. Existential concerns in anton chekhov’s short stories. Acta Universitatis Sapientiae Philologica. (2022) 14:83–95. doi: 10.2478/ausp-2022-0007
66. Tomer A. Death anxiety in adult life—theoretical perspectives. Death Stud. (1992) 16:475–506. doi: 10.1080/07481189208252594
67. Gong Y, Yan Y, Yang R, Cheng Q, Zheng H, Chen Y, et al. Factors influencing death anxiety among Chinese patients with cancer: a cross-sectional study. BMJ Open. (2022) 12:e064104. doi: 10.1136/bmjopen-2022-064104
68. Chan SF and La Greca AM. Perceived stress scale (PSS). In: Encyclopedia of behavioral medicine. Hanover, Pennsylvania: Springer (2020). p. 1646–8. doi: 10.1007/978-3-030-39903-0_773
69. Lee E-H. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res. (2012) 6:121–7. doi: 10.1016/j.anr.2012.08.004
70. Bettison TM, Nahm CB, Gill AJ, Mittal A, Malhi GS, and Samra JS. Understanding the pathophysiology of psychological distress and pancreatic cancer: a systematic review. Pancreas. (2018) 47:376–81. doi: 10.1097/MPA.00000000000001016
71. Wu H-C, Yang C-Y, and Chen Y-C. The role of self-efficacy in the recovery trajectory of mental health consumers. Br J Soc work. (2021) 51:907–26. doi: 10.1093/bjsw/bcab025
72. Birch JN and Vanderheyden WM. The molecular relationship between stress and insomnia. Advanced Biol. (2022) 6:2101203. doi: 10.1002/adbi.202101203
73. Ziegler MG. Psychological stress and the autonomic nervous system. In: Primer on the autonomic nervous system. United Kingdom: Elsevier (2012). p. 291–3. doi: 10.1016/B978-0-12-386525-0.00061-5
74. Iqbal S. Social networks and mental health: exploring the threads of support. Policy J Soc Sci Rev. (2024) 2:64–72. doi: 10.63075/pjssr.v2i02.18
75. Park HY. Emotional support and palliative care for distressed patients suffering from pancreatic cancer. Korean J Gastroenterol. (2019) 74:95–100. doi: 10.4166/kjg.2019.74.2.95
76. Cristian A and Green J. Patient safety and quality improvement in rehabilitation medicine. Phys Med Rehabil Clinics. (2012) 23:221–30. doi: 10.1016/j.pmr.2012.02.001
77. Saposnik G, Redelmeier D, Ruff CC, and Tobler PN. Cognitive biases associated with medical decisions: a systematic review. BMC Med Inf decision making. (2016) 16:1–14. doi: 10.1186/s12911-016-0377-1
78. Gabriel AS, Campbell JT, Djurdjevic E, Johnson RE, and Rosen CC. Fuzzy profiles: Comparing and contrasting latent profile analysis and fuzzy set qualitative comparative analysis for person-centered research. Organizational Res Methods. (2018) 21:877–904. doi: 10.1177/1094428117752466
79. Hwang JK, Page BJ, Flynn D, Passmore L, McCaul E, Brady J, et al. Validation of the eighth edition TNM lung cancer staging system. J Thorac Oncol. (2020) 15:649–54. doi: 10.1016/j.jtho.2019.11.030
80. Baraldi AN and Enders CK. An introduction to modern missing data analyses. J school Psychol. (2010) 48:5–37. doi: 10.1016/j.jsp.2009.10.001
81. Ferguson SL, Moore G, and Hull DM. Finding latent groups in observed data: A primer on latent profile analysis in Mplus for applied researchers. Int J Behav Dev. (2020) 44:458–68. doi: 10.1177/0165025419881721
82. Zhang K. Positive psychological capital: measurement and relationship with mental health. Stud Psychol Behav. (2010) 8:58.
83. Cao X, Zhang H, Li P, and Huang X. The influence of mental health on job satisfaction: mediating effect of psychological capital and social capital. Front Public Health. (2022) 10:797274. doi: 10.3389/fpubh.2022.797274
84. Wang Y, Chang Y, Fu J, and Wang L. Work-family conflict and burnout among Chinese female nurses: the mediating effect of psychological capital. BMC Public Health. (2012) 12:915. doi: 10.1186/1471-2458-12-915
85. Zhou H, Peng J, Wang D, Kou L, Chen F, Ye M, et al. Mediating effect of coping styles on the association between psychological capital and psychological distress among Chinese nurses: a cross-sectional study. J Psychiatr Ment Health Nurs. (2017) 24:114–22. doi: 10.1111/jpm.12350
86. Templer DI. The construction and validation of a Death Anxiety Scale. J Gen Psychol. (1970) 82(2):165–77. doi: 10.1080/00221309.1970.9920634
87. Feng Y, Liu X, Lin T, Luo B, Mou Q, Ren J, et al. Exploring the relationship between spiritual well-being and death anxiety in patients with gynecological cancer: a cross-section study. BMC Palliat Care. (2021) 20:78. doi: 10.1186/s12904-021-00778-3
88. Che SL, Li X, Zhu M, and Ng WI. The Death Literacy Index: translation, cultural adaptation, and validation of the Chinese version. Front Public Health. (2023) 11:1140475. doi: 10.3389/fpubh.2023.1140475
89. Zimet GD, Dahlem NW, Zimet SG, and Farley GK. The multidimensional scale of perceived social support. J Pers Assess. (1988) 52:30–41. doi: 10.1207/s15327752jpa5201_2
90. Yang X, Xue M, Pauen S, and He H. Psychometric properties of the chinese version of multidimensional scale of perceived social support. Psychol Res Behav Manag. (2024) 17:2233–41. doi: 10.2147/prbm.S463245
91. Cohen S, Kamarck T, and Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
92. Yang TZ and Huang HT. An epidemiological study on stress among urban residents in social transition period. Zhonghua Liu Xing Bing Xue Za Zhi. (2003) 24:760–4.
93. Podsakoff PM, MacKenzie SB, Lee JY, and Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. (2003) 88:879–903. doi: 10.1037/0021-9010.88.5.879
94. Muthén B and Muthén L. Mplus: A general latent variable modeling program. Muthén Muthén. (2019).
96. Teng M, Wang J, Jin M, Yuan Z, He H, Wang S, et al. Psychological capital among clinical nurses: A latent profile analysis. Int Nurs Rev. (2024) 71:786–93. doi: 10.1111/inr.12918
97. Nolzen N. The concept of psychological capital: a comprehensive review. Manage Rev Q. (2018) 68:237–77. doi: 10.1007/s11301-018-0138-6
98. Cadete N and Ruggunan S. Self-perceptions and benefits of psychological resilience among women academics in the context of working in South African higher education institutions (SA-HEIs): A mixed-method approach. SAGE Open. (2024) 14:21582440241256770. doi: 10.1177/21582440241256770
99. O’Rourke N. Psychological resilience and the well-being of widowed women. Ageing Int. (2004) 29:267–80. doi: 10.1007/s12126-996-1002-x
100. Eagly AH and Wood W. Social role theory. In: Handbook of theories of social psychology. New York, US: Sage Publications, vol. 2. (2012). p. 458–76.
101. Kajantie E and Phillips DI. The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology. (2006) 31:151–78. doi: 10.1016/j.psyneuen.2005.07.002
102. Garcia-Retamero R and Cokely ET. Designing visual aids that promote risk literacy: A systematic review of health research and evidence-based design heuristics. Hum Factors. (2017) 59:582–627. doi: 10.1177/0018720817690634
103. Cohen S and Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. (1985) 98:310–57. doi: 10.1037/0033-2909.98.2.310
104. Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. (2000) 55:469–80. doi: 10.1037/0003-066X.55.5.469
105. Fortner BV and Neimeyer RA. Death anxiety in older adults: a quantitative review. Death Stud. (1999) 23:387–411. doi: 10.1080/074811899200920
106. Wong PTP and Yu TTF. Existential suffering in palliative care: an existential positive psychology perspective. Medicina (Kaunas). (2021) 57:924. doi: 10.3390/medicina57090924
107. Ziller EC, Anderson NJ, and Coburn AF. Access to rural mental health services: service use and out-of-pocket costs. J Rural Health. (2010) 26:214–24. doi: 10.1111/j.1748-0361.2010.00291.x
108. Li J-Y. Acculturation and social stigma: Mental health communicative action and help-seeking behaviors among chinese immigrants in the United States. Int J Strategic Communication. (2021) 15:487–503. doi: 10.1080/1553118X.2021.1984918
109. Tedeschi RG and Calhoun LG. Posttraumatic growth: conceptual foundations and empirical evidence. psychol Inq. (2004) 15:1–18. doi: 10.1207/s15327965pli1501_01
110. Carver CS and Antoni MH. Finding benefit in breast cancer during the year after diagnosis predicts better adjustment 5 to 8 years after diagnosis. Health Psychol. (2004) 23:595–8. doi: 10.1037/0278-6133.23.6.595
111. Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. (2011) 52:145–61. doi: 10.1177/0022146510395592
112. Bekiros S, Jahanshahi H, and Munoz-Pacheco JM. A new buffering theory of social support and psychological stress. PloS One. (2022) 17:e0275364. doi: 10.1371/journal.pone.0275364
113. Lepore SJ and Revenson TA. Social constraints on disclosure and adjustment to cancer. Soc Pers Psychol Compass. (2007) 1:313–33. doi: 10.1111/j.1751-9004.2007.00013.x
114. Eisenberger NI, Taylor SE, Gable SL, Hilmert CJ, and Lieberman MD. Neural pathways link social support to attenuated neuroendocrine stress responses. Neuroimage. (2007) 35:1601–12. doi: 10.1016/j.neuroimage.2007.01.038
115. Haslam SA, McMahon C, Cruwys T, Haslam C, Jetten J, and Steffens NK. Social cure, what social cure? The propensity to underestimate the importance of social factors for health. Soc Sci Med. (2018) 198:14–21. doi: 10.1016/j.socscimed.2017.12.020
116. Berkman LF. Social support, social networks, social cohesion and health. Soc Work Health Care. (2000) 31:3–14. doi: 10.1300/J010v31n02_02
117. Zhao Z and Liu W. Pancreatic cancer: A review of risk factors, diagnosis, and treatment. Technol Cancer Res Treat. (2020) 19:1533033820962117. doi: 10.1177/1533033820962117
118. O’Leary A. Stress, emotion, and human immune function. Psychol Bull. (1990) 108:363–82. doi: 10.1037/0033-2909.108.3.363
119. McFarlane AC. The long-term costs of traumatic stress: intertwined physical and psychological consequences. World Psychiatry. (2010) 9:3–10. doi: 10.1002/j.2051-5545.2010.tb00254.x
120. Xiang G, Teng Z, Li Q, et al. The influence of perceived social support on hope: A longitudinal study of older-aged adolescents in China[J]. Child Youth Serv Rev. (2020) 119:105616.
121. Ye Z, Yang X, Zeng C, Wang Y, Jetten Z, Li X, et al. Resilience, social support, and coping as mediators between COVID‐19‐related stressful experiences and acute stress disorder among college students in China. Appl Psychol Health Well Being. (2020) 12(4):1074–94. doi: 10.1016/j.socscimed.2017.12.020
Keywords: pancreatic cancer, psychological capital, death anxiety, perceived stress, social support, latent profile analysis
Citation: Yang D, She T, Gui G, Li L, Zhou Z, Liu L and Liu N (2025) Psychological capital and death anxiety in pancreatic cancer patients: a latent profile analysis. Front. Psychiatry 16:1627422. doi: 10.3389/fpsyt.2025.1627422
Received: 12 May 2025; Accepted: 21 August 2025;
Published: 10 September 2025.
Edited by:
Carmelo Mario Vicario, University of Messina, ItalyCopyright © 2025 Yang, She, Gui, Li, Zhou, Liu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nian Liu, bGl1bmlhbkBuc21jLmVkdS5jbg==; Lu Liu, bGl1bHVkb2N0b3I4OEBuc21jLmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Dajun Yang
Dajun Yang Tianyu She3†
Tianyu She3† Gui Gui
Gui Gui Lu Liu
Lu Liu Nian Liu
Nian Liu