- 1Mental Health Center of Yangtze University, Jingzhou, Hubei, China
- 2Mental Health Institute of Yangtze University, Jingzhou, Hubei, China
- 3Department of Psychiatry, Jingzhou Rongjun Special Care Hospital, Jingzhou, Hubei, China
- 4Department of Psychiatry, Jingzhou Mental Health Center, Jingzhou, Hubei, China
Objective: To explore the network structure of emotional resilience and anxiety-depressive symptoms in adolescents and identify gender differences in these networks.
Method: A convenience sample of students from 21 middle schools in Jingzhou City was recruited for an online questionnaire survey. Emotional resilience, anxiety, and depression symptoms were assessed using the Adolescents’ Emotional Resilience Questionnaire, Generalized Anxiety Disorder Scale (GAD-7), and Patient Health Questionnaire (PHQ-9), respectively. Network analysis was performed to construct a model of emotional resilience dimensions (GP: generate positive emotion, RN: recover from negativity) and anxiety-depressive symptoms, with key features identified via expected influence (EI) and bridge expected influence (bEI). Gender differences were tested using the Network Comparison Test.
Results: A total of 17,499 adolescents were included. The prevalence of anxiety (GAD-7 ≥ 10) was 7.43% in males and 13.32% in females; depression (PHQ-9 ≥ 10) prevalence was 9.89% in males and 16.33% in females. Core symptoms included “uncontrollable worry,” “depressed mood,” and “psychomotor problems,” while four bridge symptoms were identified: “GP,” “RN,” “restlessness,” and “depressed mood. “ Network structure (M=0.144, p < 0.001) and global strength (S=0.354, p < 0.001) differed significantly by gender.
Conclusion: Adolescents need to develop emotional resilience in a balanced manner, and targeted interventions on core (e.g., “uncontrollable worry”, “psychomotor problems”) and bridge symptoms (e.g., “GP,” “RN,” “restlessness” and “depressed mood”) in the context of anxiety and depression are crucial for preventing these conditions in youth.
1 Introduction
The 2022 World Mental Health Report by the World Health Organization points out that over one billion people globally suffer from mental disorders, with depression and anxiety being the most common conditions (1). Depression and anxiety are common mental health disorders among adolescents. It is estimated that 6.2% of adolescents worldwide have depression disorders and 6.5% have anxiety disorders (2, 3). According to a meta-analysis of Chinese middle school adolescents, the detection rate of depressive symptoms was found to be 24.3% (4), and that of anxiety symptoms was 28.0% (5). Generalized anxiety disorder is characterized by persistent feelings of worry, restlessness, irritability, sleep disturbances, and nervousness, accompanied by symptoms such as palpitations, dry mouth, and sweating (6). Overall, anxiety disorders are the most common form of mental disorders among young people (7). A study on the prevalence and related disability burden of mental disorders among Chinese children and adolescents found that anxiety disorders represent the largest burden of mental disorders (8). Anxiety disorders not only significantly increase the risk of suicide among youth (9) but are also closely associated with the occurrence of substance use disorders and depression (10). Depression, a common and serious mental health disorder, is characterized by symptoms including low mood, anhedonia, lack of energy, and sleep disturbances (11). Global statistics show that 34% of adolescents are at risk of developing clinical depression (12). Depressive symptoms not only affect the mental health of adolescents but can also lead to declining academic performance, impaired cognitive function, and interpersonal relationship issues. Notably, studies have indicated a sharp rise in depression rates among young people, particularly within female populations (13, 14).
Most disorders among children and adolescents globally show significant gender differences (15). Significant changes in estrogen levels in adolescent girls may act as a trigger for the onset of depression (16). A recent study highlighted the unique challenges faced by adolescent girls, such as the influence of gender norms, academic pressure, and difficulties in peer relationships, making an important empirical contribution to understanding gender inequality in emotional distress and anxiety. It draws attention to the complex and interwoven nature of girls’ lived experiences (17). A meta-analysis by Salk et al. indicated that females generally report higher rates of depression diagnoses and symptoms than males, with gender differences peaking during adolescence, a trend observed universally across the globe (18). Similarly, studies within Chinese children and adolescents have found higher prevalence rates of depressive and anxiety disorders among girls compared to boys, highlighting significant gender differences (8, 19–21). Additionally, the comorbidity rate of depression and anxiety is higher in girls than in boys, with adolescents experiencing both conditions showing more severe depressive symptoms and behavioral issues (21). These findings underscore the critical role of adolescence in the emergence and progression of mental health problems, as well as the differential impact of gender on this process. A recent study on the network of psychological symptoms among Chinese high school students found that depression was the core symptom for boys, while anxiety was central for girls, indicating significant gender differences (22). However, recent meta-analyses reveal low treatment rates for mental disorders among children and adolescents, particularly for depression and anxiety disorders (23). Evidence suggests that targeted and directed prevention are more effective than universal prevention (14). Therefore, we hope that this study can provide some new insights into the prevention and early intervention of emotional problems in adolescents of different genders.
Resilience can be viewed as a defense mechanism, which enables people to thrive in the face of adversity, and improving resilience may be an important target for the treatment and prophylaxis of disease (24). The concept of resilience has evolved over time, yet there is considerable variation in how it is defined and measured across studies. Psychological resilience encompasses a broad range of dimensions; in the gradual refinement of this construct, some researchers argue that emotional resilience—although a significant component of psychological resilience—should be further distinguished from it (25, 26). The ability to generate positive emotions and recover quickly from negative emotional experiences is known as emotional resilience (26). This concept contains two key aspects, composed of two fundamental components: first, the ability to generate positive emotion when faced with negative emotional stimuli (GP); second, the ability to rapidly recover from negative emotional experiences even after they have been felt (RN). Some researchers suggest that GP and RN may relate to emotion regulation through distinct mechanisms (27). Previous studies have found that individuals with high emotional resilience recover more quickly from negative emotions and demonstrate better adaptive functioning and psychological well-being (28). Furthermore, Ong and colleagues found that positive emotional experiences help highly resilient individuals recover effectively from stress (29). When facing stressful events, positive emotions can enhance coping abilities, thereby improving psychological resilience and promoting mental and physical health (30). A longitudinal prospective sequential experimental cohort study on Canadian public safety personnel found that suicidal ideation and planning decreased directly after receiving Emotional Resilience Skills Training (31). However, it remains unknown whether GP or RN is more effective in reducing suicidal ideation.
By reviewing and synthesizing the literature on early research related to emotional resilience, it can be found that only a limited number of studies have provided conceptual definitions of emotional resilience. For example, a study involving 266 Chinese adolescents found that emotional resilience is negatively correlated with symptoms of depression and anxiety, and this negative correlation is partially mediated by positive emotions. The results highlight the role of emotional resilience in alleviating psychological problems and promoting mental health among Chinese adolescents (32). But very few studies have explored the relationship between emotional resilience and the dimensions of anxiety and depression symptoms, nor have they identified intervention targets (33). Previous studies have mostly relied on total scale scores to assess the relationship between resilience and anxiety or depression, overlooking the heterogeneity and complexity among the internal components of psychological variables, which makes it difficult to identify precise intervention targets. Furthermore, traditional statistical methods have limitations in handling the dynamic interactions among multidimensional variables, potentially obscuring the underlying associations between symptoms. In recent years, network analysis (NA) methods have become increasingly prevalent in the field of psychology. Network theory views mental disorders as the result of direct interactions between symptoms, with symptoms causally linked through biological, psychological, and social mechanisms. Symptoms act as nodes within psychopathological networks, with causal interactions between symptoms serving as connections between nodes (34). Numerous studies have utilized NA to explore the underlying mechanisms of mental disorders and identify symptoms that have more significant impacts (35–37). A previous study employed the NA method to explore the relationships among resilience, anxiety, and depression among clinical nurses at the item level (38). From a network perspective, symptoms are not interchangeable indicators. They are entities within a causal network, where their role depends on their position within that network. Theorists argue that highly “central” symptoms are more likely to propagate symptom activation throughout the network compared to those at the periphery (39). Therefore, these central symptoms are considered to play crucial roles in the onset and remission of mental disorders (39, 40).
Previous research has not explored, from a network perspective, the dimensions of adolescents’ emotional resilience and their relationships with anxiety and depression symptoms, nor is the influence of gender on the topological structure of the emotion resilience-symptom network well understood. To address this gap, this study innovatively applies network analysis to an integrated model of adolescent emotional resilience and anxiety-depression symptoms, aiming to answer the following key questions (1): How do the two dimensions of emotional resilience form a dynamically interconnected network with anxiety and depression symptoms? Which core nodes serve as “bridges” within this network? (2) Are there differences in network connectivity strength and core node distribution between male and female adolescents? Can these differences inform gender-specific interventions? By using network analysis to precisely delineate the mechanisms linking emotional resilience with anxiety and depression, this study aims to identify targeted intervention points for adolescent mental health problems, providing empirical support for developing personalized prevention and intervention strategies based on network characteristics.
2 Methods
2.1 Participants and study procedure
This is a study on the mental health status of adolescents, conducted by Jingzhou Mental Health Center in collaboration with the local Education Bureau from September 18 to October 8, 2023. The study adopted a convenience sampling method, distributing questionnaires in 21 middle and high schools in Jingzhou, China, with a methodology similar to previous studies (41). Data were collected through the “Questionnaire Star” platform embedded in WeChat. A QR code linked to the study introduction, invitation, and questionnaire entrance was designed and distributed. The research center provided the QR codes to cooperating schools and invited teachers at these schools to organize student and parent participation. After providing electronic written informed consent, participants used smartphones to scan the QR code and access the data collection form and questionnaire. A total of 19,686 questionnaires were distributed. Those who failed the attention-check questions, or whose completion times were excessively long or short, were excluded, resulting in 17,499 valid responses (an effective rate of 88.89%). This study has been approved by the Ethics Committee of Jingzhou Mental Health Center.
2.2 Measures
The Chinese version of the Patient Health Questionnaire-9 (PHQ-9) has demonstrated good reliability and validity in both general populations and youth samples (42, 43). This questionnaire was used to assess depressive symptoms over the past two weeks. The severity of anxiety symptoms was measured using the Chinese version of the 7-item Generalized Anxiety Disorder Scale (GAD-7) (44, 45), which has been validated among Chinese adolescents (46). Both scales use a 4-point Likert scoring system, where 0 indicates “not at all” and 3 indicates “nearly every day.” Following previous research (47, 48), a total score of 10 or higher on either the PHQ-9 or GAD-7 is considered “test-positive,” indicating possible presence of depression or anxiety. In this study, the Cronbach’s alpha coefficients for the PHQ-9 and GAD-7 were 0.91 and 0.93, respectively.
The Adolescents’ Emotional Resilience Questionnaire (AERQ) is an 11-item self-report measure of emotional resilience. See Supplementary Table S1 for details. The questionnaire assesses two dimensions: the ability to generate positive emotion (GP) and the ability to recover from negative emotional experiences (RN). It is suitable for adolescents aged 11 to 20. A six-point Likert scale is used, ranging from 1 (“completely disagree”) to 6 (“completely agree”), with five items reverse-scored. The total emotional resilience score is obtained by summing the scores of the two dimensions. Higher scores indicate greater emotional resilience. The questionnaire has demonstrated good internal consistency and discriminant validity in previous studies, and is used to assess adolescents’ emotional resilience (27). In this study, the Cronbach’s alpha coefficient for the AERQ was 0.84; the internal consistency coefficients for the subscales were as follows: GP, 0.90; RN, 0.79.
2.3 Statistical analyses
2.3.1 Network estimation
In psychometrics, accurate estimation of the number of dimensions has long been a challenging issue. Exploratory Graph Analysis (EGA), proposed by Golino and Epskamp (49), is an emerging dimension detection method in recent years. Based on the graphical lasso algorithm and using the EBIC criterion to determine the regularization parameter, EGA can assess the dimensional structure of items within psychological constructs. Overall, evidence suggests that compared to factor analysis—regarded as the “gold standard” for dimension assessment—EGA performs better in accurately detecting the correct number of dimensions in psychological scales, particularly when the sample size is large (50). In this study, we employed Exploratory Graph Analysis (EGA) to estimate the dimensionality of the GAD-7, PHQ-9, and AERQ, and evaluated model stability using the bootstrap method (bootEGA). In the final model, 27 nodes were distributed across four communities (Supplementary Figure S1), which was largely consistent with our pre-specified dimensional structure (one dimension for anxiety, one for depression, and two for emotional resilience, totaling four dimensions). The PHQ-9 and GAD-7 are designed to assess specific symptom clusters (corresponding to depressive and anxiety symptoms, respectively), with each item directly reflecting a unique, clinically identifiable symptom. Using individual items as nodes enables the capture of fine-grained associations between symptoms, aligning with the core objective of network analysis to explore interactions at the symptom level. Some scholars argue that resilience factors act as independent, additive network nodes that can weaken the connections between symptoms or the self-sustaining nature of symptoms, thereby preventing maladaptive shifts in the system (51). For the AERQ, our focus lies on the broader dimensions of emotional resilience represented by its subscales. The AERQ subscales are empirically derived constructs with demonstrated internal consistency. Therefore, using subscale total scores as nodes better reflects our interest in the question of “how resilience dimensions interact with specific anxiety and depression symptoms,” rather than focusing on individual resilience items.
Network analysis of the dimensions of emotional resilience and anxiety and depressive symptoms was conducted using the R software (Version 4.4.0), with the network model estimated via the EBICglasso method (36). Network visualization was performed using the “qgraph” package in R. Expected Influence (EI) was calculated to identify central (i.e., influential) symptoms within the network. Compared to traditional centrality indices (e.g., node strength), this approach is more suitable for networks containing both positive and negative edges (52). Nodes with higher Expected Influence in the network are considered more important. The bridge function from the R package networktools (Version 1.5.2) was used to compute bridge Expected Influence (bEI) in order to identify bridge symptoms. Compared to bridges with lower expected influence, those with higher bEI reflect a greater risk of spreading activation from one community to others (53). To identify bridge symptoms, an 80% threshold of the bridge Expected Influence value was used as the cutoff (54). In addition, the mgm package was used to estimate the predictability of each node. Predictability refers to the extent to which the variance of a given node can be predicted by the variances of its neighboring nodes in the network, and is represented visually by the area of the ring around each node in the network plot.
2.3.2 Network stability
To assess the accuracy and stability of the observed network model, the R package bootnet (Version 1.6) (36) was used to perform 1000 bootstrap samples for each node. Using non-parametric bootstrapping, a new dataset with 95% confidence intervals (CIs) was generated to evaluate the accuracy of edge weights (40). Lower overlap of the confidence intervals indicates higher accuracy in edge weight estimation. The stability of centrality indices—Expected Influence and bridge Expected Influence—was assessed using the correlation stability (CS) coefficient. A CS coefficient greater than 0.25 suggests acceptable stability for node centrality, while a coefficient greater than 0.5 indicates good stability (36). Finally, non-parametric bootstrapping based on 95% confidence intervals was used to estimate the differences between each pair of edges or nodes. A confidence interval that includes zero indicates a statistically significant difference between the paired edges or nodes.
2.3.3 Network comparison
Considering the moderating role of gender on anxiety and depressive symptoms in adolescents (55), the present study aimed to investigate whether there are differences in network characteristics between genders. The R package NetworkComparisonTest (Version 2.2.2) (56) was used to perform 1000 permutations to assess global network strength (the sum of absolute values of all edge weights) and network structure (the distribution of edge weights). Additionally, the Benjamini-Hochberg procedure was applied to evaluate the strength of each edge between the two networks while controlling for multiple comparisons.
3 Results
This study included a total of 17,499 adolescents, among whom 8,932 (51.04%) were male and 8,567 (48.96%) were female. There were 4,432 students from Grade 7 (25.33%), 3,317 from Grade 8 (18.96%), 3,176 from Grade 9 (18.15%), 2,118 from Grade 10 (12.10%), 2,546 from Grade 11 (14.55%), and 1,910 from Grade 12 (10.91%). The average age was 14.32 (± 1.63) years.
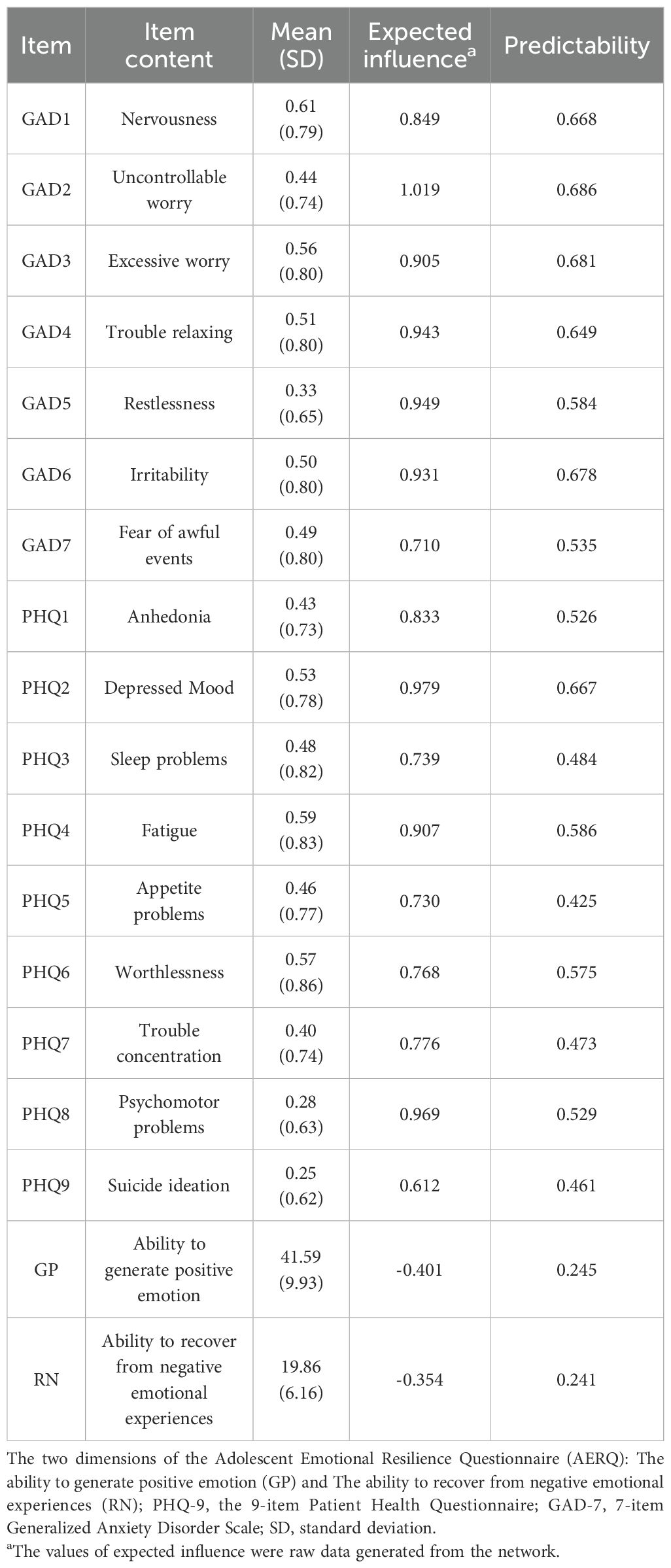
There was a gender difference in the positive rate for anxiety (GAD-7 ≥ 10): 7.43% for males and 13.32% for females. A similar trend was observed for depression (PHQ-9 ≥ 10), with positive rates of 9.89% for males and 16.33% for females. The scores for each item on the GAD-7 and PHQ-9 scales, as well as the two dimensions of the AERQ, are shown in Table 1.
3.1 Network structure
The network structure of emotional resilience dimensions and anxiety and depressive symptoms for all participants is shown in Figure 1. Regarding the basic characteristics of the final network, first, 135 out of a possible 153 edges (88.24%) were non-zero, reflecting considerable interconnectivity between symptoms. The predictability of each symptom is depicted by ring-shaped pie charts (Figure 1, Table 1). The average node predictability was 0.539, indicating that 53.9% of the variance of nodes within the network can be explained by their neighboring nodes.
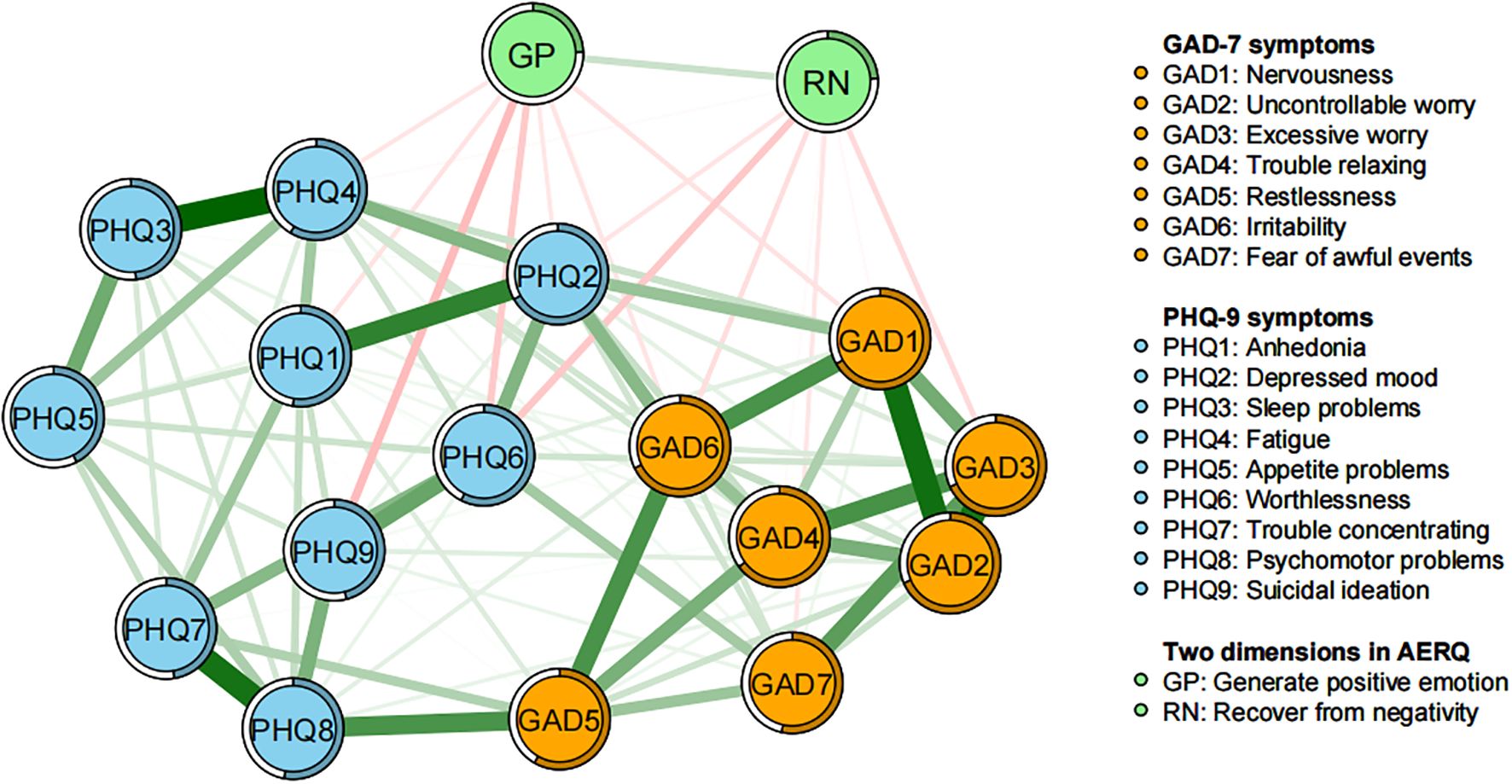
Figure 1. Network structure of emotional resilience and symptoms of anxiety and depression in adolescents. In the diagram, symptom nodes with stronger connections are closer to each other. The orange nodes denote the GAD-7 items; the sky-blue nodes denote the PHQ-9 items; the light green nodes denote the two dimensions of the AERQ. The dark green lines represent positive correlations, and the red lines represent negative correlations. To simplify the graph, edges with an absolute weight below 0.03 are not displayed. The edge thickness represents the strength of the association between symptom nodes.
“Uncontrollable worry” (GAD2), “depressed mood” (PHQ2), “psychomotor problems” (PHQ8), and “restlessness” (GAD5) occupy central positions in the node Expected Influence metrics, showing significant connectivity and predictive power (Figure 2, Table 1). This indicates that these individual symptoms are crucial and have the most substantial impact for understanding the structure of the emotional resilience and anxiety-depression network model. They may represent core symptoms requiring intervention, suggesting that improving these core symptoms could be more effective in alleviating the entire symptom network. This approach aligns with clinical strategies that prioritize addressing key symptoms.
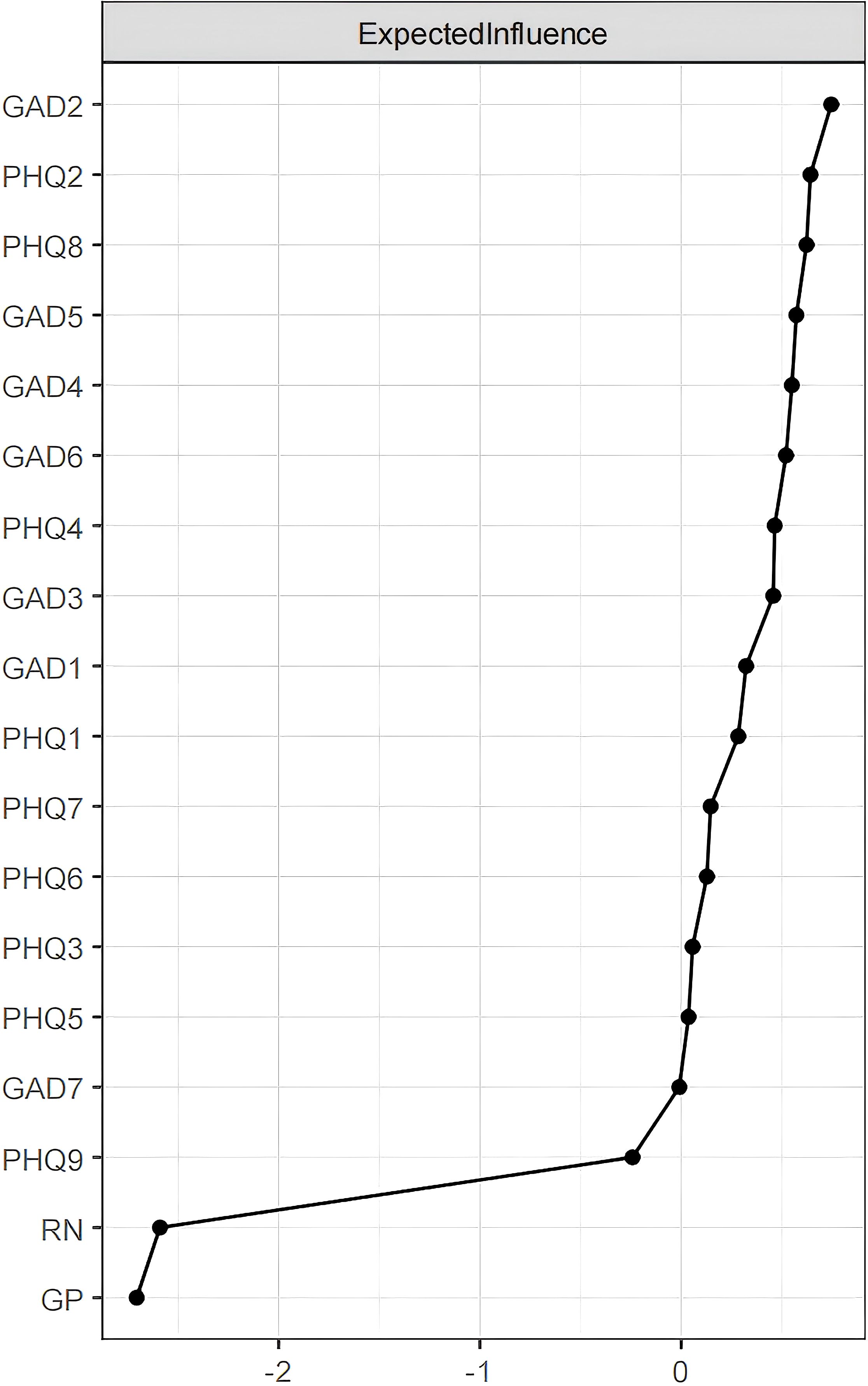
Figure 2. Centrality indices of the network structure for emotional resilience and symptoms of anxiety and depression in adolescents: Expected Influence. Centrality indices are shown as standardized z-scores.
As shown in Figure 1, the two dimensions of emotional resilience are negatively correlated with most anxiety and depression symptoms. The top three symptoms that have the strongest negative correlations with the ability to generate positive emotion (GP) are: “suicidal ideation” (PHQ9), “worthlessness” (PHQ6), and “nervousness” (GAD1) (with weights of -0.082, -0.069, and -0.049, respectively). For the ability to recover from negative emotional experiences (RN), the top three symptoms with the strongest negative correlations are: “worthlessness” (PHQ6), “excessive worry” (GAD3), and “irritability” (GAD6) (with weights of -0.071, -0.056, and -0.052, respectively).
The study identified four bridge symptoms: “generate positive emotion,” “recover from negativity,” “restlessness,” and “depressed mood” (Figures 3, 4). These bridge symptoms play a critical role in connecting different parts of the network, indicating their significance in the interaction between emotional resilience and anxiety and depression symptoms.
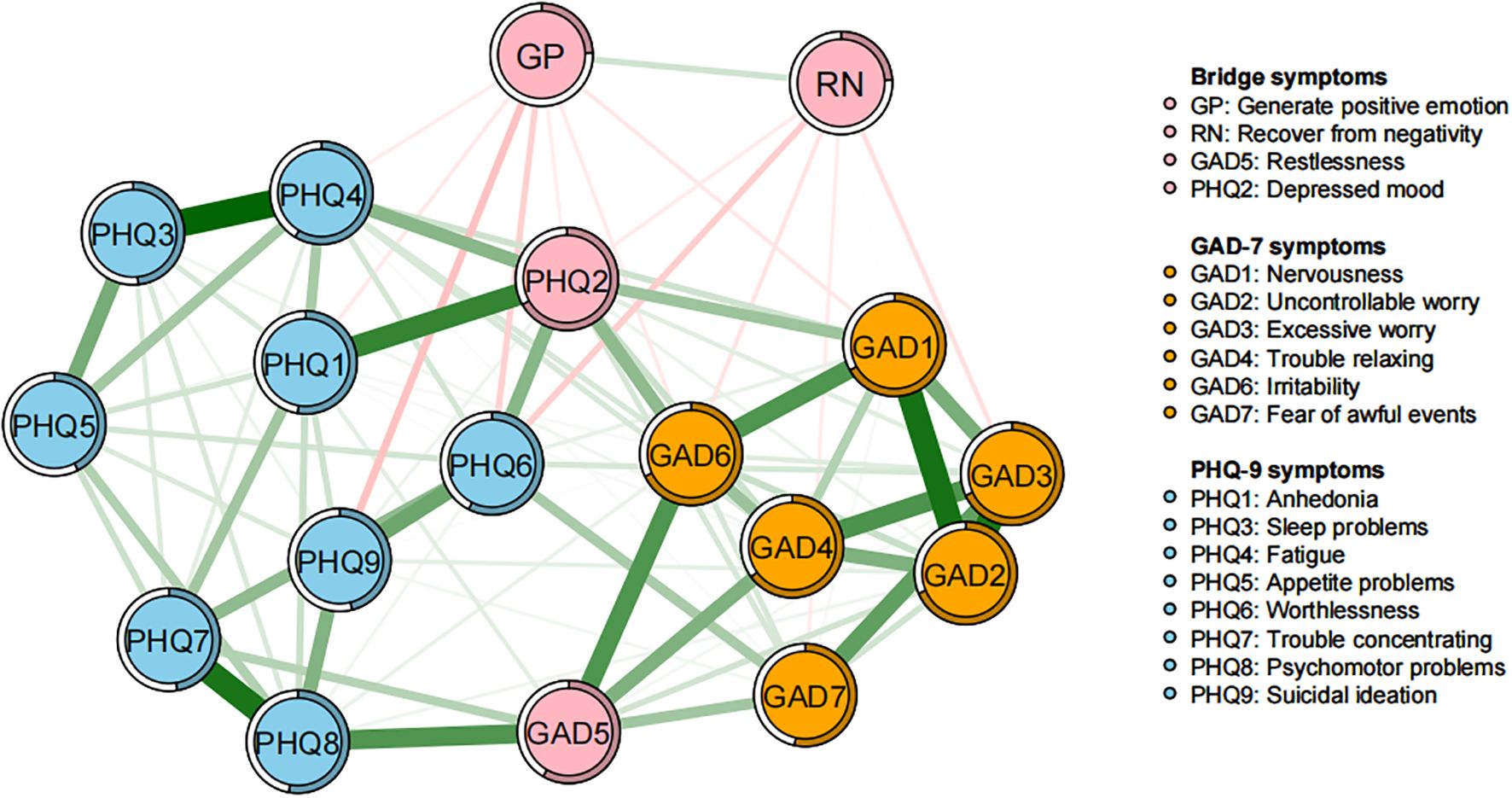
Figure 3. Bridge network structure of emotional resilience and symptoms of anxiety and depression in adolescents. In the diagram, symptom nodes with stronger connections are closer to each other. The orange nodes denote the GAD-7 items; the sky-blue nodes denote the PHQ-9 items; the light pink nodes denote the Bridge symptoms. To simplify the graph, edges with an absolute weight below 0.03 are not displayed.
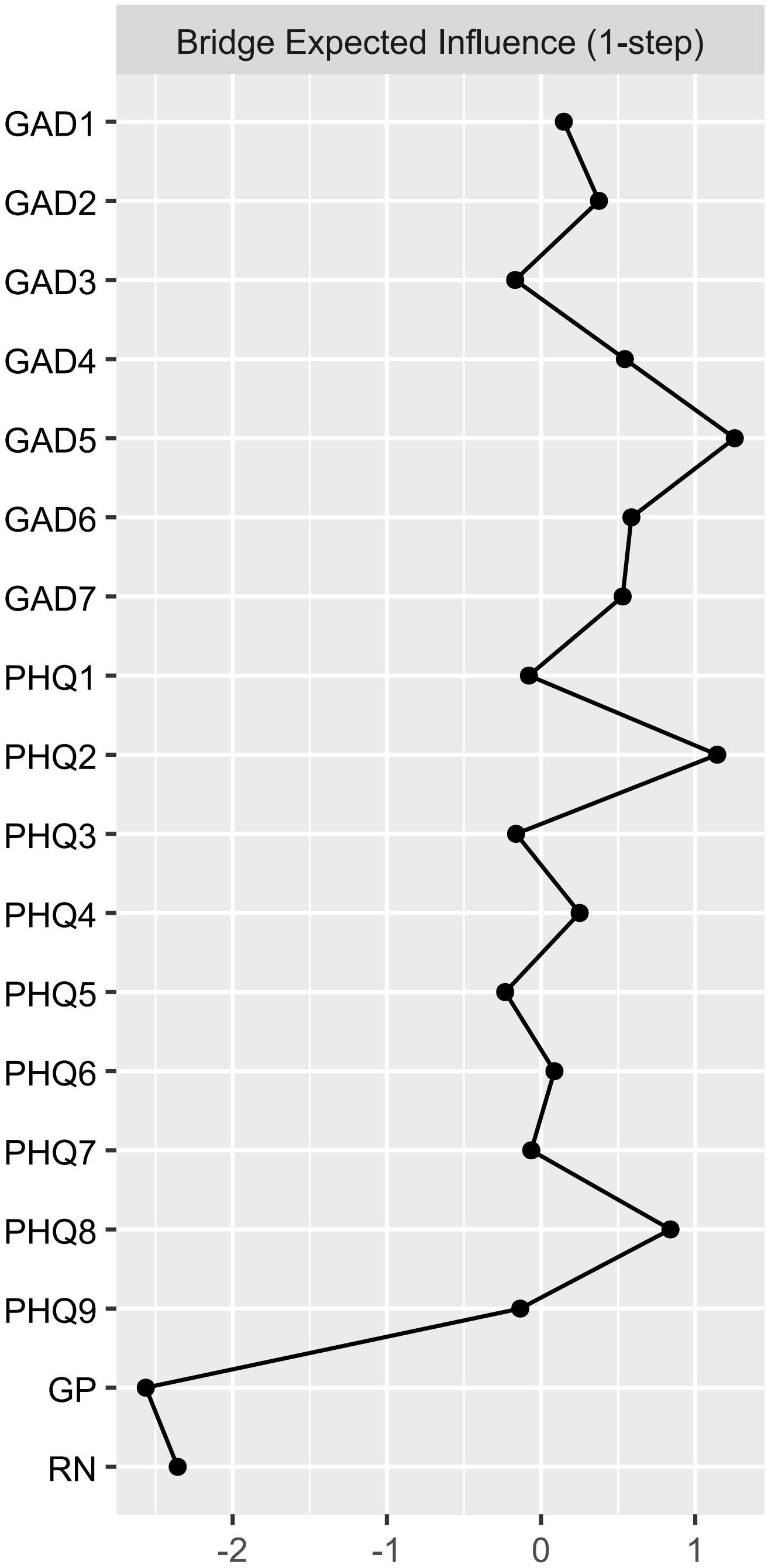
Figure 4. Bridge expected influence (1-step) of the Network Structure of Adolescent Emotional Resilience, Anxiety, and Depression Symptoms. Centrality indices are shown as standardized z-scores.
3.2 Network stability and accuracy
Both the Expected Influence and bridge Expected Influence values demonstrated excellent stability (with CS coefficients of 0.75), indicating that the network structure would not substantially change even when 75% of the sample was removed (Figure 5). Additionally, the 95% confidence intervals (CIs) obtained through bootstrapping were narrow, suggesting reliable estimates for the edge weights (Supplementary Figure S2). Non-parametric bootstrap results also showed that most comparisons of node EI and bEI were statistically significant (Supplementary Figures S3, S4).
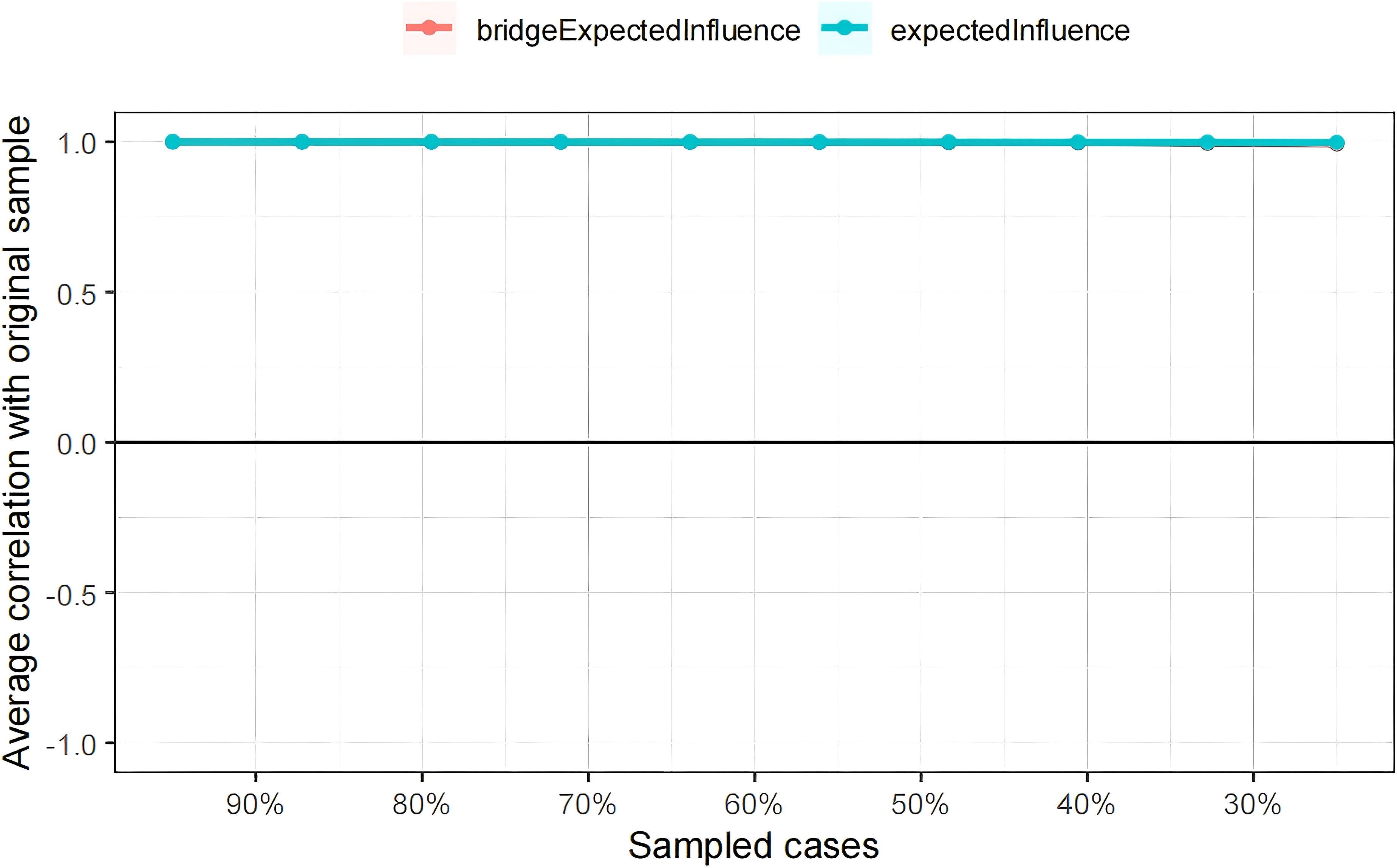
Figure 5. Stability of centrality and bridge centrality indices using case-dropping bootstrap. The x-axis represents the percentage of cases of the original sample used at each step. The y-axis represents the average of correlations between the centrality indices in the original network and the centrality indices from the re-estimated networks after excluding increasing percentages of cases. The line indicates the correlations of EI and bEI.
3.3 Network comparison tests
Network comparisons of gender differences in emotional resilience with anxiety and depressive symptoms are presented in Figure 6. Further analyses revealed significant gender differences in both network structure invariance (M=0.144, p < 0.001) and global strength (females: 8.415, males: 8.061; S=0.354, p < 0.001) (Supplementary Figure S5), suggesting that emotional resilience has a more pronounced inhibitory effect on anxiety and depression in females. Results of edge invariance tests indicated that there were multiple edges with significantly stronger strength in the female group (p < 0.05), including those within the anxiety-depression dimensions: “Uncontrollable worry” (GAD2) and “excessive worry” (GAD3), “worthlessness” (PHQ6) and “suicidal ideation” (PHQ9); that within the emotional resilience dimension: GP-RN; and that across dimensions: RN and “worthlessness” (PHQ6). This result reflects greater connectivity and stronger inhibitory effects of emotional resilience in these dimensions among females. Centrality invariance tests showed gender differences in bridge Expected Influence for nodes RN and “restlessness” (GAD5) (p < 0.05). Specifically, GAD5 exhibited a stronger bridging role in the female network, while RN had a more significant inhibitory effect on anxiety and depression in females. In addition, most other nodes did not show significant differences between the gender-based networks (p ≥ 0.05).
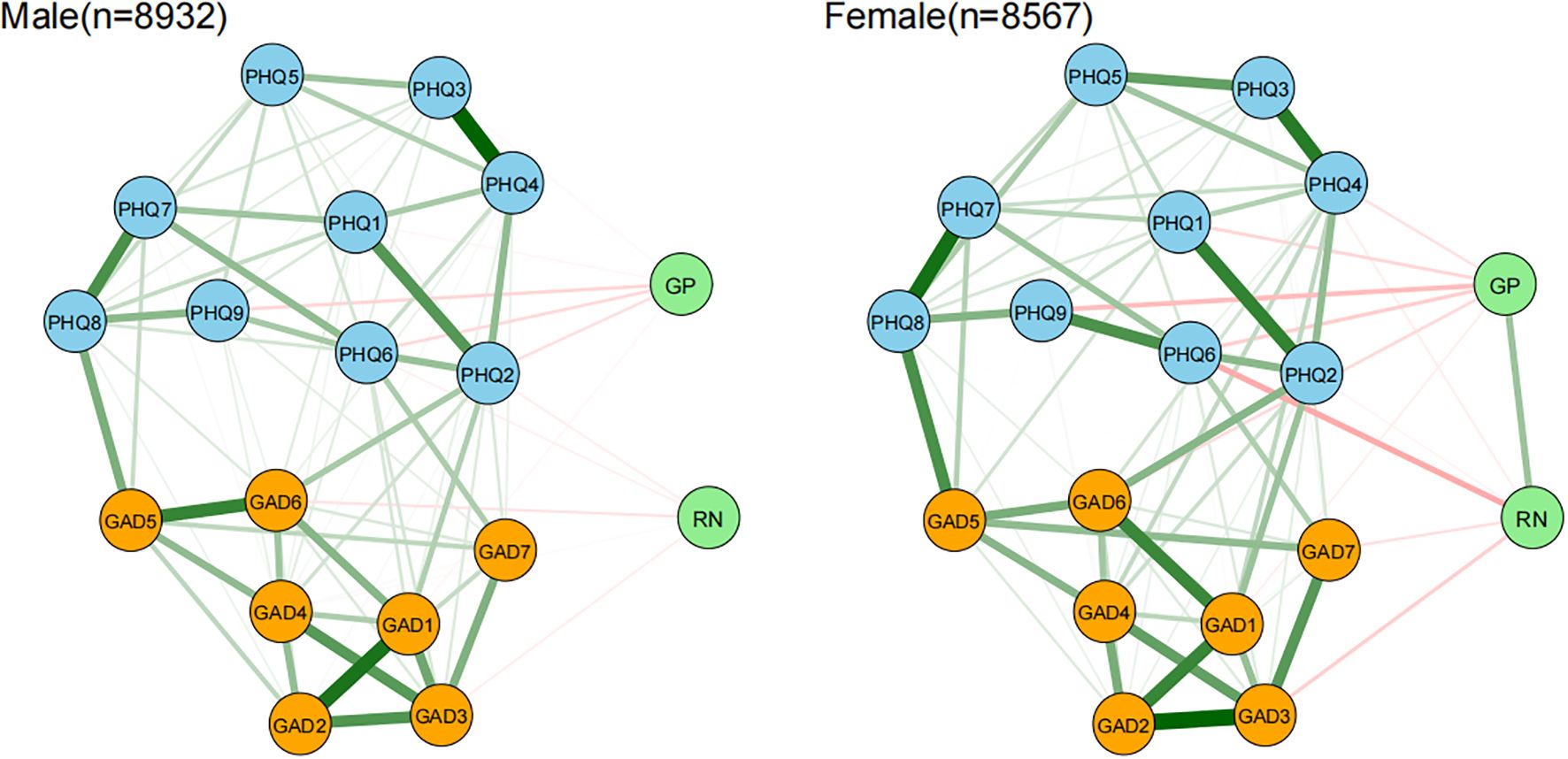
Figure 6. Network comparison of emotional resilience and symptoms of anxiety and depression between adolescent males and females. In the diagram, symptom nodes with stronger connections are closer to each other. The orange nodes denote the GAD-7 items; the sky-blue nodes denote the PHQ-9 items; the light green nodes denote the two dimensions of the AERQ. To simplify the graph, edges with an absolute weight below 0.03 are not displayed.
4 Discussion
This study is the first to apply network analysis methods to explore the dynamic associations between emotional resilience and anxiety and depressive symptoms among adolescents. “Uncontrollable worry” emerged as the most central symptom in the entire network, followed by “depressed mood,” “psychomotor problems,” and “restlessness.” Therefore, the activation or persistence of these symptoms may trigger or sustain the dynamic development of other anxiety and depressive symptoms. Additionally, in this sample, the bridge symptoms connecting emotional resilience with anxiety and depressive symptoms can be categorized into two types: protective factors (“recover from negativity,” “generate positive emotion”) and risk factors (“restlessness,” “depressed mood”). This study reveals the complex dynamic interplay between emotional resilience and symptoms of anxiety and depression among adolescents, highlights the role of gender differences, and offers a novel perspective and empirical support for understanding the network mechanisms underlying adolescent mental health.
Notably, “uncontrollable worry” and “depressed mood” exhibited the highest Expected Influence values in the network, which is consistent with findings from a study by Su et al. based on a large sample of early adolescents in China (N=15,391) (57). This consistency suggests that these two emotional symptoms may serve as key hubs within the anxiety-depression network across different adolescent age groups, playing a central role in symptom transmission and persistence.
“Uncontrollable worry” exhibits the strongest connectivity and predictive power in the network. The metacognitive model of generalized anxiety disorder places worrying, meta-worry (“worry about worry”) and corresponding underlying metacognitive beliefs (i.e., beliefs about worry) as central in the maintenance of symptoms (58). Psychological resilience has an inhibitory effect on worry-related factors (59), providing a target for clinical interventions.
In this study, “depressed mood” was observed as a core and bridge symptom within the network among non-clinical adolescents. This finding resonates with the centrality characteristics of depressive mood observed by Beard et al. (60) in clinical samples, suggesting a developmental stage correspondence—both studies indicate that depressive mood exhibits significant centrality characteristics regardless of whether the sample consists of clinical or non-clinical populations. This aligns with existing research indicating that depressive mood serves as a central pathological mechanism in depression (61).
Another bridge symptom identified in this study is “restlessness.” Interestingly, in our sample, both “psychomotor problems” and “restlessness” were also core symptoms within the network. Additionally, the bridging effect of “restlessness” was stronger in females, consistent with previous studies (37, 62), suggesting that physiological anxiety symptoms (such as psychomotor agitation) may be a critical pathway for the transdiagnostic transmission of emotional disorders in females. The findings of this study align with previous research indicating gender differences in somatic experiences; for example, Ruchkin and Schwab-Stone noted in a longitudinal study of urban adolescents that females exhibit higher levels of somatic symptoms and somatic anxiety compared to males (63). These gender differences may stem from interactions between biological susceptibility, psychological coping mechanisms, and sociocultural pressures. From a clinical perspective, given their transdiagnostic nature, targeted interventions for bridge symptoms are likely to be effective for both co-occurring disorders. This suggests that interventions focused on regulating psychomotor activity—such as mindfulness-based therapies, relaxation exercises, or behavioral activation therapy—would be particularly effective, especially for patients with comorbid conditions. Recent research indicates that behavioral activation therapy has shown stronger effects compared to Acceptance and Commitment Therapy (64).
The two dimensions of emotional resilience (GP, RN) served as bridge nodes in the network and demonstrated broad negative associations with both anxiety and depressive symptoms. These findings align with prior research (38, 65–67), which has established resilience as a protective factor against the development of anxiety and depression. Notably, GP exerted the strongest inhibitory effect on “suicidal ideation,” whereas RN showed the most robust negative association with “worthlessness.” Moreover, the negative association between RN and “worthlessness” was stronger in females, suggesting that females’ emotional recovery ability may be more susceptible to the influence of self-evaluation. When emotional recovery capacity is insufficient, females are more likely to fall into depression following setbacks in self-worth. Cognitive reappraisal can mitigate the impact of depressive symptoms on emotional reactivity in adolescents, particularly showing significant effects in emotional recovery (68). Resilient individuals also utilize positive emotions to recover from negative emotional experiences (69). Higher emotional resilience enables individuals to experience greater positive emotions, which fosters more oppositional and negative attitudes toward suicidal ideation. Positive emotions not only buffer the negative impacts of crises but also reduce depressive feelings and suicidal thoughts, promoting psychological growth (70), aligning with the broaden-and-build theory of positive emotions. This theory posits that over time, the broadening effects initiated by positive emotions build enduring personal resources (71, 72). Emotional recovery ability refers to the capacity to rapidly bounce back from negative emotional experiences; by accelerating the resolution of negative emotions, it helps alleviate core depressive symptoms such as low self-evaluation.
Gender difference analyses revealed that the female symptom network exhibited higher global strength and several gender-specific connections. Notably, females showed stronger connectivity between GP and RN, suggesting a greater reliance on the synergistic effects of emotional resilience to resist symptom development. In the female network, stronger connections were observed for GAD2–GAD3 and PHQ6–PHQ9, which may be linked to a higher tendency among females to engage in rumination—internally processing emotions through repetitive thinking or self-critical behaviors (73, 74). This aligns with Nolen-Hoeksema’s theory of gender differences in rumination, which posits that females are more prone to repetitive worry, partially explaining why they are at higher risk for depression and anxiety (75, 76). Our findings contrast with those of Cai et al. (77), who investigated the network structure of depressive and anxiety symptoms in adolescents (n = 1057) during the later phase of the COVID-19 pandemic and found no significant gender effect on network structure. This discrepancy may stem from differences in sample timing, population characteristics, or modeling approaches.
Recent meta-analytic results indicate that psychotherapy leads to significant improvements in overall functioning among adolescents with anxiety (78), and is also effective in preventing subclinical symptoms from developing into more severe depression. Psychological interventions have shown broad applicability across different populations (79). This study provides important implications for adolescent mental health interventions: for adolescents primarily presenting core symptoms such as “uncontrollable worry” and “depressed mood,” targeted intervention strategies can be designed. For example, cognitive behavioral therapy (CBT) techniques such as “worry behavior prevention” can be combined with mindfulness training to reduce hyperarousal. Given females’ higher tendency toward rumination and greater emotional connectivity, interventions targeting worry, meta-worry, and underlying metacognitive beliefs—such as employing “metacognitive therapy” to interrupt excessive focus on worry—may have a significant impact on both anxiety and depressive symptoms in individuals with generalized anxiety disorder (58).
In addition, psychological interventions should prioritize enhancing GP and RN in adolescents, particularly female adolescents, to strengthen their resilience to depression and anxiety and break the vicious cycle of negative cognition and emotion. One study found that higher resilience can act as a protective factor against mood disorders (80). Notably, interventions such as resilience training and CBT have been shown to effectively enhance psychological resilience (81). Mindfulness training has been proven to improve resilience (82), with stronger effects observed in females than in males (83). Another study indicated that emotional resilience in females demonstrates a more pronounced inhibitory effect on negative emotional symptoms. According to the mindfulness-based stress reduction model, after engaging in positive cognitive evaluation, individuals experience an expanded attentional scope, reframe their understanding of stressful events, and ultimately increase their resilience levels (84). It is recommended that mindfulness strategies be tailored based on gender differences: females may benefit more from emotion awareness training, while males may respond better to active interventions such as mindful yoga or tai chi, which align with their externalizing coping styles (85). Furthermore, a recent systematic review found that interventions combining CBT with mindfulness techniques appear to have a positive impact on individual resilience (86). Researchers have also suggested that educators and policymakers should encourage adolescents to engage in regular physical activity. Exercise not only directly reduces emotional distress such as anxiety and improves overall well-being but also indirectly promotes mental health by fostering resilience (87, 88). Physical activity is an effective factor in enhancing stress resistance, with particularly significant effects observed in females (89).
Both internal assets and external resources may serve as key factors in enhancing resilience (90). Strengthening collaboration among schools, families, and communities can better support adolescent mental health. A study involving 163 children aged 8 to 10 found that mindfulness instruction in schools or other settings helps improve children’s emotional resilience (91), and therefore the application of this teaching approach should be encouraged. Research indicates that school-based universal interventions focusing on resilience enhancement are promising and can at least short-term alleviate symptoms of depression and anxiety in adolescents, especially when using cognitive behavioral therapy (CBT)-based approaches (92). A study by Rudolph et al. (93) showed that adolescent females who participated in a single-session emotional mindset course (E-MIND) experienced improved emotional states, increased self-efficacy in emotion regulation, and enhanced use of coping strategies. Single-session interventions are low-cost, time-efficient, and easy to implement, making them suitable for resource-limited settings. If integrated into school health education and combined with parental and teacher involvement, the effectiveness may be further enhanced. Internationally validated school-based mental health programs such as My FRIENDS Youth have been shown to significantly improve adolescent emotional resilience (94, 95). Through cognitive behavioral training, this program effectively alleviates emotional symptoms in adolescents, particularly showing notable benefits for anxiety reduction in females, offering an adaptable model for reducing the burden of mental disorders in other countries. Additionally, a systematic review and meta-analysis by Schäfer et al. (96) found that online and mobile interventions are as effective as face-to-face interventions. Digital resilience interventions hold potential for addressing future mental health challenges; they can promote psychological well-being, enhance resilience components, and possibly help maintain good psychological functioning or enable rapid recovery following periods of stress. Based on these findings, it is recommended to develop digital interventions aimed at enhancing psychological resilience.
However, several limitations should be noted. First, due to the cross-sectional design, the causal direction among symptoms cannot be inferred. Future studies could further examine the causal relationships between variables using cross-lagged panel models or intervention designs. Second, the sample was drawn from a single region and recruited via convenience sampling, which may introduce regional, cultural, and selection biases. Specifically, although convenience sampling provided practical advantages for this study—such as ease of data collection and resource efficiency—it may have led to an overrepresentation of easily accessible groups, such as adolescents from specific schools, thereby limiting the generalizability of the findings to the broader target population. This could reduce the external validity of the results across diverse cultural contexts, geographical populations, and non-clinical adolescents. Therefore, future research should replicate and validate these findings in diverse cultural and regional settings, with particular attention to gender differences in resilience and emotional symptoms within collectivistic cultures. Additionally, probability sampling methods are recommended to enhance sample representativeness and the external validity of the findings. Third, data were collected using self-report questionnaires, which may be subject to potential biases such as recall bias and response bias. These limitations suggest that future research combining longitudinal designs, cross-cultural comparisons, and multimodal assessment approaches (e.g., incorporating objective physiological indicators or observer ratings) would help overcome the current constraints and provide more universally applicable theoretical foundations for the precise intervention of adolescent emotional health.
In summary, this study based on network analysis reveals the dynamic associations between emotional resilience and anxiety and depressive symptoms in adolescents, as well as the gender differences underlying these relationships. Core symptoms such as “uncontrollable worry” and “psychomotor problems,” along with bridge symptoms including “GP,” “RN,” “restlessness,” and “depressed mood,” represent potential intervention targets. The findings indicate that gender differences should be fully considered in adolescent mental health interventions, necessitating more targeted strategies. For females, interventions should focus on strengthening RN and blocking the cross-system transmission of somatic anxiety symptoms, while for males, cognitive behavioral therapy and active mindfulness training may be particularly effective. Moreover, multi-institutional collaboration is needed, with governments, schools, and healthcare institutions working together to explore effective measures to enhance adolescents’ emotional resilience. This would contribute to more effective prevention and intervention of emotional problems and promote psychological health during adolescence.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Ethics Committee of Jingzhou Mental Health Center. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
CL: Conceptualization, Data curation, Investigation, Methodology, Visualization, Writing – original draft. X-XP: Data curation, Investigation, Methodology, Validation, Writing – original draft. BL: Resources, Supervision, Validation, Writing – review & editing. LZ: Data curation, Investigation, Writing – original draft. M-YL: Formal Analysis, Investigation, Writing – original draft. Y-JZ: Conceptualization, Investigation, Writing – original draft. X-FZ: Data curation, Funding acquisition, Investigation, Supervision, Writing – review & editing. S-CN: Methodology, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This research was funded by a grant from the Jingzhou Association for Science and Technology (Grant Number: JZCXZK202209).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1651506/full#supplementary-material.
Supplementary Figure 1 | Dimensionality results from EGA (left) and item stability of the GAD-7, PHQ-9, and AERQ (right).
Supplementary Figure 2 | Bootstrapped confidence intervals of edge weights.
Supplementary Figure 3 | Bootstrapped stability test for ‘expected influence’.
Supplementary Figure 4 | Bootstrapped stability test for’bridge expected influence’.
Supplementary Figure 5 | Difference in global strength and maximum of difference between adolescent males and females. There was a significant difference in network global strength between females and males (females: 8.415, males: 8.061; S=0.354, p < 0.001), as well as in network structural invariance (M=0.144, p < 0.001).
References
1. Cuijpers P, Javed A, and Bhui K. The WHO World Mental Health Report: a call for action. Br J Psychiatry. (2023) 222:227–9. doi: 10.1192/bjp.2023.9
2. Erskine HE, Baxter AJ, Patton G, Moffitt TE, Patel V, Whiteford HA, et al. The global coverage of prevalence data for mental disorders in children and adolescents. Epidemiol Psychiatr Sci. (2016) 26:395–402. doi: 10.1017/S2045796015001158
3. Polanczyk GV, Salum GA, Sugaya LS, Caye A, and Rohde LA. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. (2015) 56:345–65. doi: 10.1111/jcpp.12381
4. Tang X, Tang S, Ren Z, and Wong DFK. Prevalence of depressive symptoms among adolescents in secondary school in mainland China: A systematic review and meta-analysis. J Affect Disord. (2019) 245:498–507. doi: 10.1016/j.jad.2018.11.043
5. Zhang Y, Bao X, Yan J, Miao H, and Guo C. Anxiety and depression in chinese students during the COVID-19 pandemic: A meta-analysis. Front Public Health. (2021) 9. doi: 10.3389/fpubh.2021.697642
6. Tyrer P and Baldwin D. Generalised anxiety disorder. Lancet. (2006) 368:2156–66. doi: 10.1016/S0140-6736(06)69865-6
7. Rapee RM, Creswell C, Kendall PC, Pine DS, and Waters AM. Anxiety disorders in children and adolescents: A summary and overview of the literature. Behav Res Ther. (2023) 168:104376. doi: 10.1016/j.brat.2023.104376
8. Dong W, Liu Y, Bai R, Zhang L, and Zhou M. The prevalence and associated disability burden of mental disorders in children and adolescents in China: a systematic analysis of data from the Global Burden of Disease Study. Lancet Regional Health - Western Pacific. (2025) 55. doi: 10.1016/j.lanwpc.2025.101486
9. Foley DL, Goldston DB, Costello EJ, and Angold A. Proximal psychiatric risk factors for suicidality in youth: the Great Smoky Mountains Study. Arch Gen Psychiatry. (2006) 63:1017–24. doi: 10.1001/archpsyc.63.9.1017
10. Pine DS, Cohen P, Gurley D, Brook J, and Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry. (1998) 55:56–64. doi: 10.1001/archpsyc.55.1.56
11. Correia AS and Vale N. Tryptophan metabolism in depression: A narrative review with a focus on serotonin and kynurenine pathways. Int J Mol Sci. (2022) 23. doi: 10.3390/ijms23158493
12. Shorey S, Ng ED, and Wong CHJ. Global prevalence of depression and elevated depressive symptoms among adolescents: A systematic review and meta-analysis. Br J Clin Psychol. (2022) 61:287–305. doi: 10.1111/bjc.12333
13. Moreno-Agostino D, Wu Y-T, Daskalopoulou C, Hasan MT, Huisman M, and Prina M. Global trends in the prevalence and incidence of depression:a systematic review and meta-analysis. J Affect Disord. (2021) 281:235–43. doi: 10.1016/j.jad.2020.12.035
14. Thapar A, Eyre O, Patel V, and Brent D. Depression in young people. Lancet. (2022) 400:617–31. doi: 10.1016/S0140-6736(22)01012-1
15. Kieling C, Buchweitz C, Caye A, Silvani J, Ameis SH, Brunoni AR, et al. Worldwide prevalence and disability from mental disorders across childhood and adolescence: evidence from the global burden of disease study. JAMA Psychiatry. (2024) 81:347–56. doi: 10.1001/jamapsychiatry.2023.5051
16. Albert PR. Why is depression more prevalent in women? J Psychiatry Neurosci. (2015) 40:219–21. doi: 10.1503/jpn.150205
17. Demkowicz O, Jefferson R, Nanda P, Foulkes L, Lam J, Pryjmachuk S, et al. Adolescent girls’ explanations of high rates of low mood and anxiety in their population: a co-produced qualitative study. BMC Womens Health. (2025) 25:49. doi: 10.1186/s12905-024-03517-x
18. Salk RH, Hyde JS, and Abramson LY. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. psychol Bulletin. (2017) 143:783–822. doi: 10.1037/bul0000102
19. Bai R, Dong W, Peng Q, and Bai Z. Trends in depression incidence in China, 1990-2019. J Affect Disord. (2022) 296:291–7. doi: 10.1016/j.jad.2021.09.084
20. Li F, Cui Y, Li Y, Guo L, Ke X, Liu J, et al. Prevalence of mental disorders in school children and adolescents in China: diagnostic data from detailed clinical assessments of 17,524 individuals. J Child Psychol Psychiatry. (2021) 63:34–46. doi: 10.1111/jcpp.13445
21. Wang Y, Zhang X, Li Y, Qin H, and Li X. Gender differences in the prevalence, correlated factors and comorbidity of depression in adolescents: a cross-sectional study in Shanghai, China. Front Public Health. (2024) 12. doi: 10.3389/fpubh.2024.1436413
22. Zhang Z, Qiu A, Zhang X, Zhao Y, Yuan L, Yi J, et al. Gender differences in the mental symptom network of high school students in Shanghai, China: a network analysis. BMC Public Health. (2024) 24:2719. doi: 10.1186/s12889-024-20130-7
23. Wang S, Li Q, Lu J, Ran H, Che Y, Fang D, et al. Treatment rates for mental disorders among children and adolescents. JAMA Network Open. (2023) 6. doi: 10.1001/jamanetworkopen.2023.38174
24. Davydov DM, Stewart R, Ritchie K, and Chaudieu I. Resilience and mental health. Clin Psychol Rev. (2010) 30:479–95. doi: 10.1016/j.cpr.2010.03.003
25. Conway AM and McDonough SC. Emotional resilience in early childhood: developmental antecedents and relations to behavior problems. Ann N Y Acad Sci. (2006) 1094:272–7. doi: 10.1196/annals.1376.033
26. Davidson RJ. Affective style, psychopathology, and resilience: brain mechanisms and plasticity. Am Psychol. (2000) 55:1196–214. doi: 10.1037/0003-066X.55.11.1196
27. Wang Y, Xu W, and Luo F. Emotional resilience mediates the relationship between mindfulness and emotion. psychol Rep. (2016) 118:725–36. doi: 10.1177/0033294116649707
28. Zhang Q, Zhou L, and Xia J. Impact of COVID-19 on emotional resilience and learning management of middle school students. Med Sci Monitor. (2020) 26. doi: 10.12659/MSM.924994
29. Ong AD, Bergeman CS, Bisconti TL, and Wallace KA. Psychological resilience, positive emotions, and successful adaptation to stress in later life. J Pers Soc Psychol. (2006) 91:730–49. doi: 10.1037/0022-3514.91.4.730
30. Tugade MM, Fredrickson BL, and Barrett LF. Psychological resilience and positive emotional granularity: examining the benefits of positive emotions on coping and health. J Pers. (2004) 72:1161–90. doi: 10.1111/j.1467-6494.2004.00294.x
31. Nisbet J, Maguire KQ, Teckchandani TA, Shields RE, Andrews KL, Afifi TO, et al. Suicidal ideation, planning, and attempts changes among diverse canadian public safety personnel after the emotional resilience skills training. Suicide Life Threat Behav. (2025) 55:e13168. doi: 10.1111/sltb.13168
32. Zhu Z, Sang B, Liu J, Zhao Y, and Liu Y. Associations between emotional resilience and mental health among chinese adolescents in the school context: the mediating role of positive emotions. Behav Sci (Basel). (2025) 15. doi: 10.3390/bs15050567
33. Yang T, He Y, Wu L, Ren L, Lin J, Wang C, et al. The relationships between anxiety and suicidal ideation and between depression and suicidal ideation among Chinese college students: A network analysis. Heliyon. (2023) 9:e20938. doi: 10.1016/j.heliyon.2023.e20938
34. Borsboom D. A network theory of mental disorders. World Psychiatry. (2017) 16:5–13. doi: 10.1002/wps.20375
35. van Rooijen G, Isvoranu AM, Meijer CJ, van Borkulo CD, Ruhé HG, and de Haan L. A symptom network structure of the psychosis spectrum. Schizophr Res. (2017) 189:75–83. doi: 10.1016/j.schres.2017.02.018
36. Epskamp S, Borsboom D, and Fried EI. Estimating psychological networks and their accuracy: A tutorial paper. Behav Res Methods. (2018) 50:195–212. doi: 10.3758/s13428-017-0862-1
37. Peng P, Chen Q, Liang M, Liu Y, Chen S, Wang Y, et al. A network analysis of anxiety and depression symptoms among Chinese nurses in the late stage of the COVID-19 pandemic. Front Public Health. (2022) 10:996386. doi: 10.3389/fpubh.2022.996386
38. Zhou Y, Gao W, Li H, Yao X, Wang J, and Zhao X. Network analysis of resilience, anxiety and depression in clinical nurses. BMC Psychiatry. (2024) 24:719. doi: 10.1186/s12888-024-06138-8
39. Cramer AO, Waldorp LJ, van der Maas HL, and Borsboom D. Comorbidity: a network perspective. Behav Brain Sci. (2010) 33:137–50; discussion 50-93. doi: 10.1017/S0140525X09991567
40. Borsboom D and Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. (2013) 9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608
41. Luo H, Lie Y, and Prinzen FW. Surveillance of COVID-19 in the general population using an online questionnaire: report from 18,161 respondents in China. JMIR Public Health Surveill. (2020) 6:e18576. doi: 10.2196/18576
42. Leung DYP, Mak YW, Leung SF, Chiang VCL, and Loke AY. Measurement invariances of the PHQ-9 across gender and age groups in Chinese adolescents. Asia Pac Psychiatry. (2020) 12:e12381. doi: 10.1111/appy.12381
43. Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2014) 36:539–44. doi: 10.1016/j.genhosppsych.2014.05.021
44. Chi G and Wang L. The association of sports participation with depressive symptoms and anxiety disorder in adolescents. Front Public Health. (2022) 10:860994. doi: 10.3389/fpubh.2022.860994
45. Wang M, Mou X, Li T, Zhang Y, Xie Y, Tao S, et al. Association between comorbid anxiety and depression and health risk behaviors among chinese adolescents: cross-sectional questionnaire study. JMIR Public Health Surveill. (2023) 9:e46289. doi: 10.2196/46289
46. Sun J, Liang K, Chi X, and Chen S. Psychometric properties of the generalized anxiety disorder scale-7 item (GAD-7) in a large sample of chinese adolescents. Healthcare (Basel). (2021) 9. doi: 10.3390/healthcare9121709
47. Aktürk Z, Hapfelmeier A, Fomenko A, Dümmler D, Eck S, Olm M, et al. Generalized Anxiety Disorder 7-item (GAD-7) and 2-item (GAD-2) scales for detecting anxiety disorders in adults. Cochrane Database Syst Rev. (2025) 3:Cd015455. doi: 10.1002/14651858.CD015455
48. Wu Y, Levis B, Riehm KE, Saadat N, Levis AW, Azar M, et al. Equivalency of the diagnostic accuracy of the PHQ-8 and PHQ-9: a systematic review and individual participant data meta-analysis. Psychol Med. (2020) 50:1368–80. doi: 10.1017/S0033291719001314
49. Golino HF and Epskamp S. Exploratory graph analysis: A new approach for estimating the number of dimensions in psychological research. PloS One. (2017) 12:e0174035. doi: 10.1371/journal.pone.0174035
50. Golino H, Shi D, Christensen AP, Garrido LE, Nieto MD, Sadana R, et al. Investigating the performance of exploratory graph analysis and traditional techniques to identify the number of latent factors: A simulation and tutorial. Psychol Methods. (2020) 25:292–320. doi: 10.1037/met0000255
51. Kalisch R, Cramer AOJ, Binder H, Fritz J, Leertouwer I, Lunansky G, et al. Deconstructing and reconstructing resilience: A dynamic network approach. Perspect Psychol Sci. (2019) 14:765–77. doi: 10.1177/1745691619855637
52. Robinaugh DJ, Millner AJ, and McNally RJ. Identifying highly influential nodes in the complicated grief network. J Abnorm Psychol. (2016) 125:747–57. doi: 10.1037/abn0000181
53. Jones PJ, Ma R, and McNally RJ. Bridge centrality: A network approach to understanding comorbidity. Multivariate Behav Res. (2021) 56:353–67. doi: 10.1080/00273171.2019.1614898
54. Garabiles MR, Lao CK, Xiong Y, and Hall BJ. Exploring comorbidity between anxiety and depression among migrant Filipino domestic workers: A network approach. J Affect Disord. (2019) 250:85–93. doi: 10.1016/j.jad.2019.02.062
55. Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, and Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A meta-analysis. JAMA Pediatr. (2021) 175:1142–50. doi: 10.1001/jamapediatrics.2021.2482
56. van Borkulo CD, van Bork R, Boschloo L, Kossakowski JJ, Tio P, Schoevers RA, et al. Comparing network structures on three aspects: A permutation test. Psychol Methods. (2023) 28:1273–85. doi: 10.1037/met0000476
57. Su Z, Yang X, Hou J, Liu S, Wang Y, and Chen Z. Gender differences in the co-occurrence of anxiety and depressive symptoms among early adolescents: A network approach. J Psychiatr Res. (2024) 179:300–5. doi: 10.1016/j.jpsychires.2024.09.024
58. Nordahl H, Vollset T, and Hjemdal O. An empirical test of the metacognitive model of generalized anxiety disorder. Scand J Psychol. (2023) 64:263–7. doi: 10.1111/sjop.12884
59. Chen H, Gao J, Dai J, Mao Y, Wang Y, Chen S, et al. Generalized anxiety disorder and resilience during the COVID-19 pandemic: evidence from China during the early rapid outbreak. BMC Public Health. (2021) 21:1830. doi: 10.1186/s12889-021-11877-4
60. Beard C, Millner AJ, Forgeard MJ, Fried EI, Hsu KJ, Treadway MT, et al. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol Med. (2016) 46:3359–69. doi: 10.1017/S0033291716002300
61. Fried EI, Epskamp S, Nesse RM, Tuerlinckx F, and Borsboom D. What are ‘good’ depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J Affect Disord. (2016) 189:314–20. doi: 10.1016/j.jad.2015.09.005
62. Kaiser T, Herzog P, Voderholzer U, and Brakemeier EL. Unraveling the comorbidity of depression and anxiety in a large inpatient sample: Network analysis to examine bridge symptoms. Depress Anxiety. (2021) 38:307–17. doi: 10.1002/da.23136
63. Ruchkin V and Schwab-Stone M. A longitudinal study of somatic complaints in urban adolescents: the role of internalizing psychopathology and somatic anxiety. J Youth Adolesc. (2014) 43:834–45. doi: 10.1007/s10964-013-9966-9
64. Fernández-Rodríguez C, González-Fernández S, Coto-Lesmes R, and Pedrosa I. Behavioral activation and acceptance and commitment therapy in the treatment of anxiety and depression in cancer survivors: A randomized clinical trial. Behav Modif. (2021) 45:822–59. doi: 10.1177/0145445520916441
65. Brailovskaia J, Schönfeld P, Zhang XC, Bieda A, Kochetkov Y, and Margraf J. A cross-cultural study in Germany, Russia, and China: are resilient and social supported students protected against depression, anxiety, and stress? psychol Rep. (2017) 121:265–81. doi: 10.1177/0033294117727745
66. Ni F, Zheng Y, Qian S, Shen G, Yan WJ, Wu YW, et al. Mental toughness in adolescents: bridging family relationships and depression across personality traits. BMC Psychol. (2024) 12:213. doi: 10.1186/s40359-024-01702-z
67. Ibrahim D, Altahir AM, Abdalla D, Elkhidir I, Abdelmagid T, SirElkhatim D, et al. How do emotional intelligence, resilience, and parental employment affect anxiety and depression levels among Sudanese adolescents? Discov Ment Health. (2024) 4:36. doi: 10.1007/s44192-024-00096-z
68. Shapero BG, Stange JP, McArthur BA, Abramson LY, and Alloy LB. Cognitive reappraisal attenuates the association between depressive symptoms and emotional response to stress during adolescence. Cognit Emot. (2019) 33:524–35. doi: 10.1080/02699931.2018.1462148
69. Tugade MM and Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J Pers Soc Psychol. (2004) 86:320–33. doi: 10.1037/0022-3514.86.2.320
70. Fredrickson BL, Tugade MM, Waugh CE, and Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. J Pers Soc Psychol. (2003) 84:365–76. doi: 10.1037/0022-3514.84.2.365
71. Fredrickson BL. What good are positive emotions? Rev Gen Psychol. (1998) 2:300–19. doi: 10.1037/1089-2680.2.3.300
72. Fredrickson BL. The role of positive emotions in positive psychology. The broaden-and-build theory of positive emotions. Am Psychol. (2001) 56:218–26. doi: 10.1037/0003-066X.56.3.218
73. Johnson DP and Whisman MA. Gender differences in rumination: A meta-analysis. Pers Individ Dif. (2013) 55:367–74. doi: 10.1016/j.paid.2013.03.019
74. Li CE, DiGiuseppe R, and Froh J. The roles of sex, gender, and coping in adolescent depression. Adolescence. (2006) 41:409–15.
75. Nolen-Hoeksema S. Emotion regulation and psychopathology: the role of gender. Annu Rev Clin Psychol. (2012) 8:161–87. doi: 10.1146/annurev-clinpsy-032511-143109
76. Ando A, Giromini L, Ales F, and Zennaro A. A multimethod assessment to study the relationship between rumination and gender differences. Scand J Psychol. (2020) 61:740–50. doi: 10.1111/sjop.12666
77. Cai H, Bai W, Liu H, Chen X, Qi H, Liu R, et al. Network analysis of depressive and anxiety symptoms in adolescents during the later stage of the COVID-19 pandemic. Transl Psychiatry. (2022) 12:98. doi: 10.1038/s41398-022-01838-9
78. Dickson SJ, Kuhnert R-L, Lavell CH, and Rapee RM. Impact of psychotherapy for children and adolescents with anxiety disorders on global and domain-specific functioning: A systematic review and meta-analysis. Clin Child Family Psychol Review. (2022) 25:720–36. doi: 10.1007/s10567-022-00402-7
79. Buntrock C, Harrer M, Sprenger AA, Illing S, Sakata M, Furukawa TA, et al. Psychological interventions to prevent the onset of major depression in adults: a systematic review and individual participant data meta-analysis. Lancet Psychiatry. (2024) 11:990–1001. doi: 10.1016/S2215-0366(24)00316-X
80. Liu D, Wang Y, Xie P, Deng H, Qiu L, Liu W, et al. Rumination and depression in chinese adolescents with mood disorders: the mediating role of resilience. J Clin Psychiatry. (2023) 84. doi: 10.4088/JCP.22m14682
81. Imran A, Tariq S, Kapczinski F, and de Azevedo Cardoso T. Psychological resilience and mood disorders: a systematic review and meta-analysis. Trends Psychiatry Psychother. (2024). doi: 10.47626/2237-6089-2022-0524
82. Galante J, Dufour G, Vainre M, Wagner AP, Stochl J, Benton A, et al. A mindfulness-based intervention to increase resilience to stress in university students (the Mindful Student Study): a pragmatic randomised controlled trial. Lancet Public Health. (2018) 3:e72–81. doi: 10.1016/S2468-2667(17)30231-1
83. Zhang J, Zheng S, Hu Z, and Wang J. Effects of mindfulness on depression in college students: mediating role of psychological resilience and moderating role of gender. BMC Psychol. (2024) 12. doi: 10.1186/s40359-023-01468-w
84. Garland E, Gaylord S, and Park J. The role of mindfulness in positive reappraisal. Explore. (2009) 5:37–44. doi: 10.1016/j.explore.2008.10.001
85. Rojiani R, Santoyo JF, Rahrig H, Roth HD, and Britton WB. Women benefit more than men in response to college-based meditation training. Front Psychol. (2017) 8:551. doi: 10.3389/fpsyg.2017.00551
86. Joyce S, Shand F, Tighe J, Laurent SJ, Bryant RA, and Harvey SB. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open. (2018) 8. doi: 10.1136/bmjopen-2017-017858
87. Peng B, Chen W, Wang H, and Yu T. How does physical exercise influence self-efficacy in adolescents? A study based on the mediating role of psychological resilience. BMC Psychol. (2025) 13:285. doi: 10.1186/s40359-025-02529-y
88. Wu J, Shao Y, Zang W, and Hu J. Is physical exercise associated with reduced adolescent social anxiety mediated by psychological resilience?: evidence from a longitudinal multi-wave study in China. Child Adolesc Psychiatry Ment Health. (2025) 19:17. doi: 10.1186/s13034-025-00867-8
89. Fallon IP, Tanner MK, Greenwood BN, and Baratta MV. Sex differences in resilience: Experiential factors and their mechanisms. Eur J Neurosci. (2020) 52:2530–47. doi: 10.1111/ejn.14639
90. Rogers EM, Melde C, Williams J, Heinze J, and McGarrell E. Adolescent mental health and resilience before and during the COVID-19 pandemic. J Adolesc Health. (2024) 75:43–50. doi: 10.1016/j.jadohealth.2024.02.023
91. Treves IN, Li CE, Wang KL, Ozernov-Palchik O, Olson HA, and Gabrieli JDE. Mindfulness supports emotional resilience in children during the COVID-19 pandemic. PloS One. (2023) 18:e0278501. doi: 10.1371/journal.pone.0278501
92. Dray J, Bowman J, Campbell E, Freund M, Wolfenden L, Hodder RK, et al. Systematic review of universal resilience-focused interventions targeting child and adolescent mental health in the school setting. J Am Acad Child Adolesc Psychiatry. (2017) 56:813–24. doi: 10.1016/j.jaac.2017.07.780
93. Rudolph KD, Troop-Gordon W, Skymba HV, Modi HH, Ye Z, Clapham RB, et al. Cultivating emotional resilience in adolescent girls: Effects of a growth emotion mindset lesson. Child Dev. (2024) 96:389–406. doi: 10.1111/cdev.14175
94. Maalouf FT, Alrojolah L, Ghandour L, Afifi R, Dirani LA, Barrett P, et al. Building emotional resilience in youth in Lebanon: a school-based randomized controlled trial of the FRIENDS intervention. Prev Science. (2020) 21:650–60. doi: 10.1007/s11121-020-01123-5
95. Kozina A. School-based prevention of anxiety using the “My FRIENDS” emotional resilience program: Six-month follow-up. Int J Psychol. (2020) 55 Suppl 1:70–7. doi: 10.1002/ijop.12553
Keywords: emotional resilience, anxiety, depression, network analysis, gender differences, adolescents
Citation: Liu C, Pi X-X, Liu B, Zhang L, Luo M-Y, Zhang Y-J, Zhang X-F and Nie S-C (2025) Network characteristics of emotional resilience, anxiety, and depression among Chinese adolescents and their gender differences. Front. Psychiatry 16:1651506. doi: 10.3389/fpsyt.2025.1651506
Received: 21 June 2025; Accepted: 02 September 2025;
Published: 16 September 2025.
Edited by:
Eduardo Fernández-Jiménez, European University of Madrid, SpainReviewed by:
Frank Quansah, University of Education, Winneba, GhanaMarcin Moroń, University of Silesia in Katowice, Poland
Copyright © 2025 Liu, Pi, Liu, Zhang, Luo, Zhang, Zhang and Nie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Suo-Cheng Nie, MzU5MjgzOTY3QHFxLmNvbQ==; Xin-Feng Zhang, NDk2Mzc1NjlAcXEuY29t
†These authors have contributed equally to this work
 Chang Liu
Chang Liu Xiao-Xia Pi3,4†
Xiao-Xia Pi3,4†