- 1Department of Psychiatry, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia
- 2Department of Psychiatry, Radboud University Medical Center, Nijmegen, Netherlands
- 3Nijmegen Institute for Scientist-Practitioners in Addiction (NISPA), Nijmegen, Netherlands
- 4Donders Center for Medical Neuroscience, Donders Institute for Brain, Cognition and Behavior, Nijmegen, Netherlands
Gambling disorder (GD) has emerged as a significant concern in Indonesia, particularly due to the rise in internet-based gambling during the pandemic and the limited availability of treatment options and support services for affected individuals. This issue has had profound impacts on individuals, their families, and society as a whole. Research has demonstrated that cognitive-behavioral therapy (CBT) is an effective treatment for GD. Additionally, as a relatively novel intervention, several studies have explored the efficacy of repetitive transcranial magnetic stimulation (rTMS) in addiction management, specifically in reducing cravings. This study aims to determine the potential effectiveness and feasibility of combining these two modalities within the Indonesian population. A pilot study of 10 subjects will be conducted to evaluate the effectiveness and feasibility of multimodalistic therapy using rTMS and CBT for GD. South Oaks Gambling Screen (SOGS) will be used to determine the presence of pathological gambling, and the participants will be assessed periodically using SOGS, Gambling Symptoms Assessment Scale (G-SAS), Gambling Urge Scale (GUS), Gambling Related Cognitions Scale (GRCS), Clinical Global Impression (CGI), Self-Reporting Questionnaire-20 Item (SRQ-20), Patient Health Questionnaire-9 Item (PHQ-9), and cognitive assessment. The treatment regimen will consist of 15 sessions of rTMS and 12 sessions of CBT, administered over a 5-week period. The findings of this study will contribute to the development of an optimized rTMS protocol in combination with CBT for the treatment of GD in Indonesia.
Clinical trial registration: ClinicalTrials.gov https://clinicaltrials.gov/study/NCT06598501, identifier NCT06598501.
Introduction
Gambling disorder (GD), recognized as a behavioral addiction in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the International Classification of Diseases (ICD-11), is a complex and multifaceted condition characterized by persistent and recurrent problematic gambling behavior that leads to significant distress or impairment in daily functioning (1). The prevalence of GD varies globally, influenced by cultural, societal, and regulatory factors (2, 3). Indonesia has faced novel challenges due to the proliferation of online gambling platforms and online lending services during the COVID-19 pandemic, with 2% of the total population suffering from GD (4). This is linear to global prevalence (around 1.29%) with a rising trend observed within the last decade (2, 5). The increasing prevalence of GD in Indonesia is concerning as the lack of available treatment options and support services for individuals affected by GD continues to exacerbate the issue, leading to strained relationships, financial difficulties, and an increased risk of mental health problems such as depression and anxiety (6, 7).
Cognitive-behavioral therapy (CBT) has been demonstrated to be an effective treatment for GD, significantly reducing gambling-related symptoms and problematic behaviors while improving overall functioning and quality of life (8, 9). Another promising modality is repetitive transcranial magnetic stimulation (rTMS), a non-invasive brain stimulation method using electromagnetic induction to modulate brain activity and connectivity (10). Studies using rTMS in the left dorsolateral prefrontal cortex (DLPFC) showed significantly decreased craving symptoms, substance use and compulsive behavior in subjects with nicotine and other substance dependence (11, 12). The Food and Drug Administration (FDA) has approved rTMS as treatment modality for substance dependence but not for behavioral addiction, despite shared clinical features between substance use and gambling disorders. Brain connectivity alterations have also been implicated in GD, with preliminary rTMS data indicating safety and potential effectiveness (13, 14). Study by Hu et al. found a more favorable outcome in alcohol dependent patients who received both CBT and rTMS, acting on the DLPFC neural system to induce neuronal plasticity and expedite neural circuit recovery. Combination of both treatments may also enhance treatment retention and adherence, potentially mitigating the high recurrence rate of GD due to treatment discontinuation (15). Therefore, this study aims to assess the feasibility of the rTMS protocol combined with CBT in Indonesian GD clients.
Methods
Study design
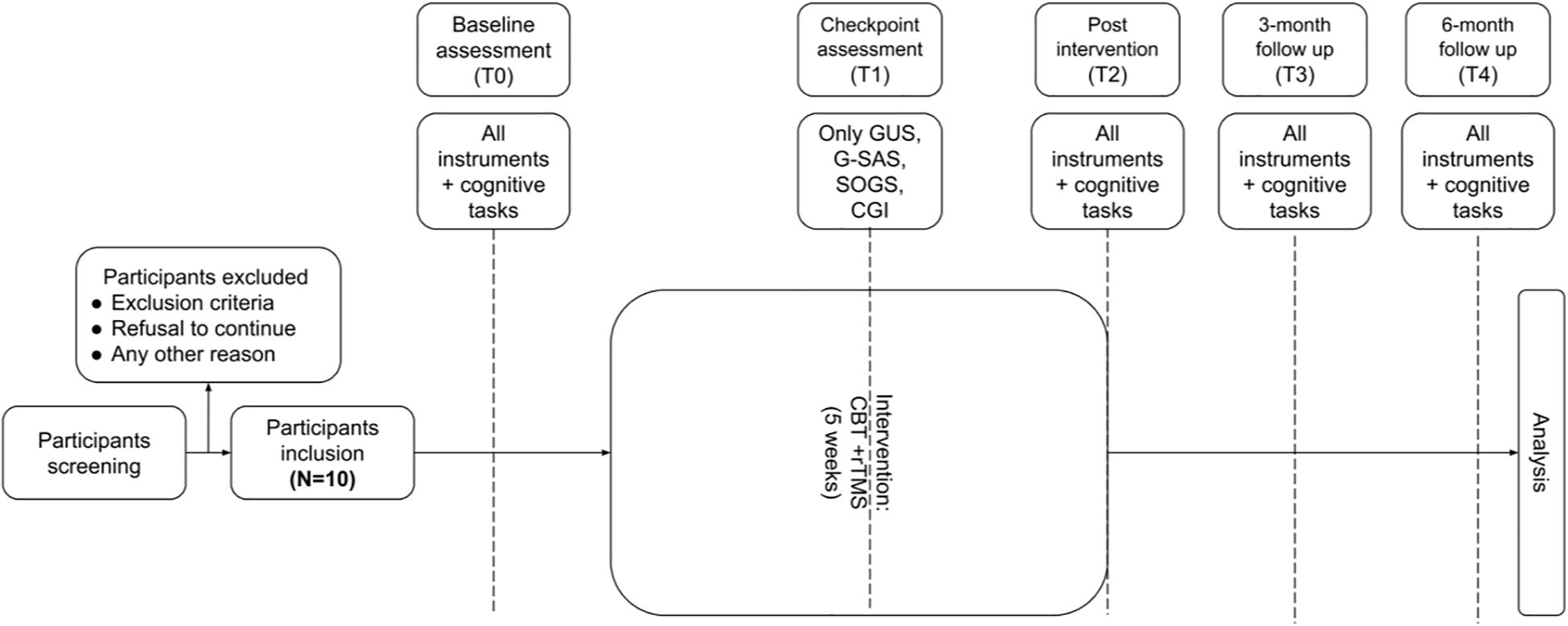
This study is a pilot and feasibility study employing a one-arm design. The research protocol adheres to the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) checklist (Supplementary File 1). After initial screening, participants will undergo complete baseline assessment (T0) and will be given treatment consisting of 15 rTMS sessions, three sessions per week, for a total of 5 weeks. A total of 12 cognitive behavioral therapy (CBT) sessions with psychiatrists will be given at once after baseline assessment, once every two rTMS sessions, and once post-treatment. Each CBT session will last for approximately 60 minutes, which will be divided into 3 phases: (1) preparation, (2) work and (3) summary.
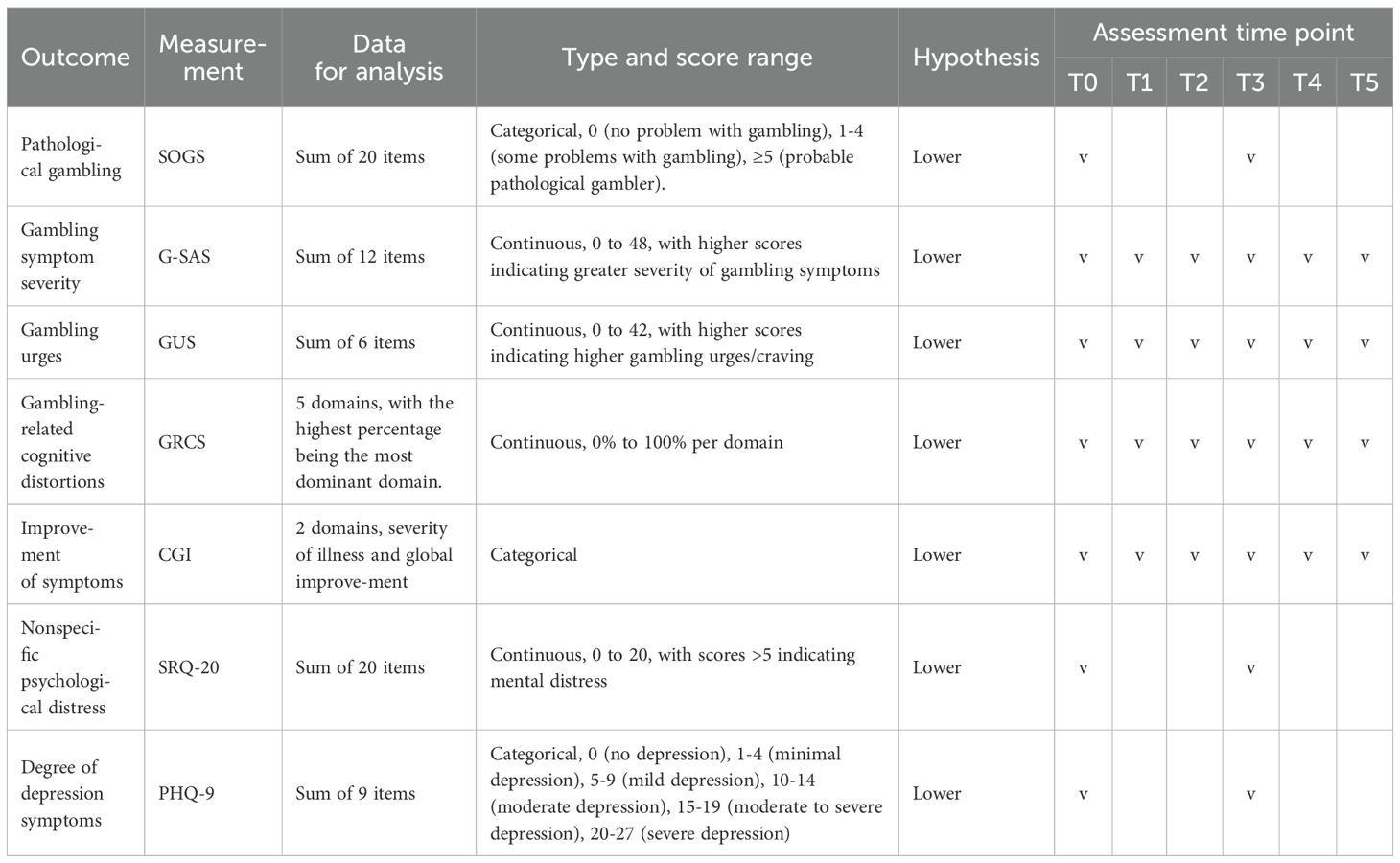
Interim assessment during treatment will be done after the seventh rTMS session (T1). This will be followed by a post-treatment assessment (T2) immediately after the last rTMS session, and two follow-up assessments at 3 months (T3) and 6 months (T4) after treatment. For T0, a complete psychiatric interview, cognitive assessment, a demographic questionnaire and 7 instruments will be used, which consist of South Oaks Gambling Screen (SOGS), Gambling Symptom Assessment Scale (G-SAS), Gambling Urge Scale (GUS), Gambling Related Cognition Scale (GRCS), Self-Reporting Questionnaire-20 Item (SRQ-20), Patient Health Questionnaire-9 Item (PHQ-9), and Clinical Global Impression – Severity and Improvement Scale (CGI) (Table 1). During T1, SOGS, G-SAS, GUS and CGI will be reassessed and during T2, T3 and T4 all 7 instruments and cognitive assessment will be given to every subject (Figure 1). All therapy sessions, as well as assessments at T0, T1, and T2, will be conducted at Cipto Mangunkusumo General Hospital. Assessments at T3 and T4 will be administered either at the hospital or via online platforms to accommodate participants.
Participants and settings
Participants will be recruited through social media platforms, using an online survey to screen potential research subjects. This survey will be administered using the REDCap online survey application (16). The respondents will fill in a demographic questionnaire along with SOGS to assess the presence of pathological gambling. Subjects with pathological gambling (SOGS score ≥ 5) will be contacted by the researcher and explained about the research procedures.
Inclusion criteria will be those: (1) screened with pathological gambling (SOGS score ≥ 5), (2) aged 18–74 years old, (3) comprehend Bahasa Indonesia, (4) consented to participate and receive treatment. Individuals who have (1) history of psychotic disorder and personality disorder according to ICD-11, (2) severe neurological disorder comorbidities, which cause seizure or loss of consciousness, (3) intellectual disability, (4) history of neurostimulation, (5) history of medical implant, (6) currently or expecting pregnancy, (7) fulfilling diagnostic criteria of substance use disorder in the last 6 months will be excluded. Participants may withdraw from the study at any time. Participants will be dropped out from the study if they miss more than two consecutive rTMS sessions. To enhance participant adherence to the treatment regimen, an appointed research associate will be tasked with issuing text message reminders to each participant one day prior to their scheduled treatment. During the study, all participants with previously prescribed medications will be permitted to continue their treatment regimen, with all medications thoroughly screened and closely monitored.
Development and implementation of the rTMS protocol
The rTMS protocol is developed by the Department of Psychiatry, Faculty of Medicine, Universitas Indonesia, Indonesia and Faculty of Medical Sciences, Radboud University Medical Center, Netherlands. The left LPFC has been shown to be central through functional connectivity in behavioral addiction previously (17). More specifically, alterations in the DLPFC have been implicated in GD through multiple structural and functional imaging studies (18, 19). Response inhibition trials demonstrate decreased activation of the DLPFC and other structures among GD participants (20, 21). In contrast, increased activation was seen during gambling cues and reversal learning tasks (22, 23). Subsequently, enhancing metabolism in the DLPFC had been posited to improve GD symptoms and affect regulation. Similar success was demonstrated in prior transcranial direct current stimulation (tDCS) leading to improved craving and cognitive inhibition (24). Thus, this protocol selects the left DLPFC as the site of stimulation. The protocol parameters are 120% RMT intensity; the stimulation is set to 10 Hz, each train will last for 4 seconds, with 11 seconds of inter-train interval (ITI), and a total of 75 trains thus in total delivering 3,000 waves. Previous rTMS studies have attempted using varying intensity ranging 80-110% and frequency ranging 1-15Hz (24). The frequency 10 Hz was selected. In line with the safety guideline for rTMS, the current protocol capped the intensity at 120% and 4s trains for 10Hz stimulation (25). The rTMS will be delivered using a Neurosoft stimulation system equipped with a 100-mm figure-8 coil (Supplementary File 2). The coil will be positioned tangentially to the scalp using a flexible coil holder, with the handle oriented posteriorly and laterally at a 45-degree angle from the midline. This coil orientation allows for targeted stimulation of the DLPFC, a superficial cortical region, while also modulating functionally connected deeper brain structures (26). All rTMS sessions will be conducted by two trained psychiatrists. Treatment will be scheduled by appointment three times per week (Monday, Wednesday, and Friday or Tuesday, Thursday, and Saturday) over a five-week period.
All participants will be screened with a 16-question safety checklist for any contraindications and potential risk factors (i.e. sleep deprivation, metal implants, seizure threshold lowering substances consumption) to rTMS procedure (Supplementary File 3) (25). After being declared safe, each participant will have their left DLPFC measured individually using the BeamF3 method (27). This technique involves measuring the nasion-inion distance, tragus-tragus distance, and head circumference to approximate the site of the left DLPFC using a software package, providing a heuristic yet reliable and cost-effective alternative to magnetic resonance imaging-guided neuronavigation. Measurements will be taken with participants wearing a personalized headcap to ensure consistency across sessions (27, 28). Resting motor threshold (RMT) will be identified visually by observing the twitch of the right pollicis brevis muscle (29). Five observable twitches of the muscle in the lowest setting after ten consecutive stimuli will determine the RMT. Prior to each stimulation session, the safety checklist will be re-administered to confirm that no new contraindications or risk factors have emerged. During each session, participants may report any discomfort and after each session they will complete an adverse event assessment. This assessment will focus on pain (including onset, location, quality, duration, and severity), twitching, tingling or redness at the stimulation site and beyond, tinnitus, mood changes, hearing alterations, and other adverse effects (Supplementary File 4). Both the safety checklist and adverse event assessment are adapted from Radboud University’s internal assessments checklist and prior guideline for rTMS applications (25).
Administering the CBT for GD
The CBT for GD module that will be utilized in this study was adapted from Indonesia Drug Addiction and Relapse Prevention Program (Indo-DARPP) CBT module for substance use disorders, with modifications based on established gambling-specific CBT frameworks (30–34).The CBT module for this study consists of 12 sessions, each lasting approximately 30–45 minutes. Sessions will be held individually in person and delivered once for every two rTMS session, depending on participant availability. The CBT module addresses a range of topics relevant to GD, including: (1) the definition, symptoms, and underlying mechanisms of GD; (2) individualized gambling-related harms; (3) reasons to stop gambling; (4) stages of change; (5) gambling triggers; (6) the gambling cycle; (7) gambling craving and extinction strategies; (8) development of alternative, non-gambling routines; (9) financial management skills; (10) rebuilding interpersonal relationships affected by gambling behavior; (11) emotional regulation strategies; and (12) relapse prevention planning.
Instruments for study outcomes
This study will employ four instruments to assess gambling related outcomes (SOGS, G-SAS, GUS, GRCS), two instruments to evaluate mental health symptoms (PHQ-9 and SRQ-20), and one clinician-rated instrument to assess symptom severity and improvement over the course of treatment (CGI). The selected gambling-related instruments have demonstrated strong reliability and validity. These instruments are widely used internationally and available in Bahasa Indonesia to capture various dimensions of gambling behavior (35–38). Specifically, the SOGS will be used not only to screen for pathological gambling but also to gather information on participants’ preferred gambling activities, the presence of gambling culture within their family or social environment, and sources of gambling funds (35). The G-SAS will assess fluctuations in gambling symptoms severity, while the GUS will measure gambling cravings experienced throughout the study (36, 37). The GRCS will identify cognitive distortions related to gambling among participants (38). Regarding mental health outcomes, the PHQ-9 will assess depressive symptoms, and the SRQ-20 will evaluate general psychological distress (39, 40). The CGI will provide insights to progress made by the participants based on clinical judgment (41).
Participant characteristics
The subsequent demographic information will be gathered through a self-administered questionnaire: age, sex, ethnicity, educational level, marital status, employment status, monthly earnings, most recent gambling experience, age of initial gambling experience, frequency of gambling per month, initial exposure to gambling, presence of other individuals with gambling issues in the patient’s circle, preferred gambling platforms, types of devices used, varieties of gambling engaged in, typical duration of gambling on weekdays and weekends, minimum and maximum wagers ever placed, total monetary losses from gambling, motives behind gambling, negative consequences from gambling, attempts to seek help, history of substance use, substance consumption during gambling, and, if applicable, experience of rehabilitation programs due to substance use.
Sample size
Based on convention in previous safety studies of medical interventions, the study sample ranged below 20 subjects (Murshed, 2019) (42). A study assessing pre-screening rTMS questionnaires in adults previously used 15 subjects (Keel et al., 2001) while a European feasibility study used 10 subjects (43, 44). Therefore, the current feasibility study will also use a sample size of 10 subjects.
Because this study is a pilot and feasibility study, we used references from previous studies related to the potential of rTMS as a therapy for gambling addiction. However, previous research has not examined the efficacy and combination of therapy, and no research has succeeded in determining standards for these variables. Therefore, we refer to studies of the safety and feasibility of rTMS.
Statistical analysis
Statistical analysis will be conducted to evaluate the treatment response using generalized linear mixed model. The Statistical Package for the Social Sciences (SPSS) software version 25.0 will be used for this analysis. The raw data obtained in this study only be accessible to the authors. Subgroup analysis will not be conducted in this study.
Data monitoring
Collected data within the study encompass socio-demographic information, psychometric assessments, and rTMS measurements, all of which will be securely stored and accessible solely to the research team. This study does not involve the collection of biological specimens. Participants will undergo assessments both before and after each rTMS session to monitor any adverse effects (such as headaches, fatigue, mood alterations, etc.) resulting from the intervention. Should any adverse effects be noted, participants will be promptly referred to appropriate medical professionals for comprehensive evaluation and treatment. Any subsequent medical expenses not already covered will be fully provided for by the investigators.
Discussion
This will be the first study to examine the effectiveness and feasibility of rTMS treatment modality for GD in Indonesia. GD therapeutic options are still limited, with no pharmacotherapy proven effective. Opioid antagonists have been suggested as potential therapy, but the results were inconclusive (45). Although CBT is widely used for treating GD with effectiveness of improving gambling related symptoms and overall quality of life, the improvements may not be immediate and often require months to show its desired effects (46). rTMS treatment modality has the added benefit of neuromodulation and inducing neuroplasticity in the targeted brain region (14). A decrease of striatal dopamine transporter (DAT) availability is observed in individuals with GD compared to healthy controls. This reduced availability of dopamine was found to be inversely correlated with gambling frequency and reward-based decision-making in individuals with GD (47). Thus, restoring dopamine function is hypothesized to benefit addiction treatment (48).
A study by Strafella et al. discovered that rTMS targeted to the left mid-dorsolateral prefrontal cortex was able to induce the release of dopamine in the striatal region, potentially benefiting many clinical aspects (49). Reduced cognitive control in GD may be linked to abnormal activity in the DLPFC, anterior cingulate cortex (ACC), and orbitofrontal cortex (OFC). Impaired DLPFC function is associated with deficits in working memory, which affects decision-making in GD (50). Stimulation using rTMS targeting glutamatergic and dopaminergic systems through the DLPFC showed potential for treatment (44). Previous rTMS studies have targeted both the right and left DLPFC, with improvements in craving and cognitive control observed in studies targeting the left rather than right DLPFC, suggesting a preference for the left DLPFC. Furthermore, high frequency rTMS is also preferred as several studies using high frequency rTMS showed notable improvements while low frequency rTMS reported no significant changes (14).
These findings do not undermine CBT as the preferred therapy for GD but emphasize the potential advantages of a multimodal treatment approach. Combining CBT with other modalities, such as pharmacotherapy and neurostimulation, may improve treatment outcomes for GD clients.
Ethics statement
The study protocol was approved by the Research Ethical Committee of Faculty of Medicine, Universitas Indonesia (approval number: KET-1499/UN2.F1/ETIK/PPM.00.02/2023). All protocol modifications will be informed to the Research Ethical Committee of Faculty of Medicine, Universitas Indonesia.
Author contributions
KS: Funding acquisition, Conceptualization, Supervision, Writing – review & editing, Writing – original draft. LS: Writing – original draft, Methodology. BM: Methodology, Conceptualization, Writing – original draft. EH: Conceptualization, Writing – review & editing. KK: Writing – original draft. AA: Writing – original draft. AS: Methodology, Conceptualization, Writing – original draft. PE: Writing – original draft, Conceptualization. ID: Writing – review & editing, Methodology, Conceptualization. TB: Writing – review & editing, Methodology, Conceptualization.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This work was supported by the National Research and Innovation Agency of Indonesia (Grant Number 34/IV/KS/05/2023 and 22/PKS/WR III-DISTP/UI/20) and Mining Industry Indonesia (MIND ID) (Grant Number 016/CSR/PK/IX/2024). The funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1658195/full#supplementary-material
Abbreviations
ACC, Anterior Cingulate Cortex; CBT, Cognitive-Behavioral Therapy; CGI, Clinical Global Impression; DAT, Dopamine Transporter; DLPFC, Dorsolateral Prefrontal Cortex; DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; FDA, Food and Drug Administration; G-SAS, Gambling Symptoms Assessment Scale; GD, Gambling Disorder; GRCS, Gambling Related Cognitions Scale; GUS, Gambling Urge Scale; ICD-11, International Classification of Diseases 11th Revision; INDO-DARPP, Indonesia Drug Addiction and Relapse Prevention Program; ITI, Inter-Train Interval; OFC, Orbitofrontal Cortex; PHQ-9, Patient Health Questionnaire-9 Item; RMT, Resting Motor Threshold; rTMS, Repetitive Transcranial Magnetic Stimulation; SOGS, South Oak Gambling Scale; SPIRIT, Standard Protocol Items: Recommendations for Interventional Trials; SPSS, Statistical Package for the Social Sciences; SRQ-20, Self-Reporting Questionnaire-20 Item; tDCS, Transcranial Direct Current Stimulation.
References
1. Gambling disorder and comorbid behavioral addictions: Demographic, clinical, and personality correlates. Available online at: https://www.sciencedirect.com/science/article/abs/pii/S0165178119319341 (Accessed May 6, 2025).
2. Gabellini E, Lucchini F, and Gattoni ME. Prevalence of problem gambling: A meta-analysis of recent empirical research (2016-2022). J Gambl Stud. (2023) 39:1027–57. doi: 10.1007/s10899-022-10180-0, PMID: 36586057
3. Quigley L. Gambling disorder and stigma: opportunities for treatment and prevention. Curr Addict Rep. (2022) 9:410–9. doi: 10.1007/s40429-022-00437-4, PMID: 36093357
4. Sinambela YSY. Uji Validitas dan Reliabilitas Instrumen South Oaks Gambling Screen (SOGS) versi Indonesia. = Validity and Reliability Study of The Indonesian South Oaks Gambling Screen Tool. Indonesia: Universitas Indonesia Library. Fakultas Kedokteran Universitas Indonesia (2022). Available online at: https://lib.ui.ac.id (Accessed May 6, 2025).
5. Calado F and Griffiths MD. Problem gambling worldwide: An update and systematic review of empirical research (2000–2015). J Behav Addict. (2016) 5:592–613. doi: 10.1556/2006.5.2016.073, PMID: 27784180
6. Thurm A, Satel J, Montag C, Griffiths MD, and Pontes HM. The relationship between gambling disorder, stressful life events, gambling-related cognitive distortions, difficulty in emotion regulation, and self-control. J Gambl Stud. (2023) 39:87–101. doi: 10.1007/s10899-022-10151-5, PMID: 35921002
7. Fong TW. The biopsychosocial consequences of pathological gambling. Psychiatry (Edgmont). (2005) 2:22–30., PMID: 21179626
8. Gooding P and Tarrier N. A systematic review and meta-analysis of cognitive-behavioural interventions to reduce problem gambling: Hedging our bets? Behav Res Ther. (2009) 47:592–607. doi: 10.1016/j.brat.2009.04.002, PMID: 19446287
9. Ribeiro EO, Afonso NH, and Morgado P. Non-pharmacological treatment of gambling disorder: a systematic review of randomized controlled trials. BMC Psychiatry. (2021) 21:105. doi: 10.1186/s12888-021-03097-2, PMID: 33596853
10. Liu Q and Yuan T. Noninvasive brain stimulation of addiction: one target for all? Psychoradiology. (2021) 1:172–84. doi: 10.1093/psyrad/kkab016, PMID: 38666219
11. Abdelrahman AA, Noaman M, Fawzy M, Moheb A, Karim AA, and Khedr EM. A double-blind randomized clinical trial of high frequency rTMS over the DLPFC on nicotine dependence, anxiety and depression. Sci Rep. (2021) 11:1640. doi: 10.1038/s41598-020-80927-5, PMID: 33452340
12. Zhang JJQ, Fong KNK, Ouyang R, Siu AMH, and Kranz GS. Effects of repetitive transcranial magnetic stimulation (rTMS) on craving and substance consumption in patients with substance dependence: a systematic review and meta-analysis. Addiction. (2019) 114:2137–49. doi: 10.1111/add.14753, PMID: 31328353
13. Sauvaget A, Bulteau S, Guilleux A, Leboucher J, Pichot A, Valrivière P, et al. Both active and sham low-frequency rTMS single sessions over the right DLPFC decrease cue-induced cravings among pathological gamblers seeking treatment: A randomized, double-blind, sham-controlled crossover trial. J Behav Addict. (2018) 7:126–36. doi: 10.1556/2006.7.2018.14, PMID: 29463098
14. Zucchella C, Mantovani E, Federico A, Lugoboni F, and Tamburin S. Non-invasive brain stimulation for gambling disorder: A systematic review. Front Neurosci. (2020) 14:729/full. doi: 10.3389/fnins.2020.00729/full
15. Hu X, Zhang T, Ma H, Zhou X, Wang H, Wang X, et al. Repetitive transcranial magnetic stimulation combined with cognitive behavioral therapy treatment in alcohol-dependent patients: A randomized, double-blind sham-controlled multicenter clinical trial. Front Psychiatry. (2022) 13:935491. doi: 10.3389/fpsyt.2022.935491, PMID: 36299538
16. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J BioMed Inform. (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208, PMID: 31078660
17. Siste K, Pandelaki J, Miyata J, Oishi N, Tsurumi K, Fujiwara H, et al. Altered resting-state network in adolescents with problematic internet use. J Clin Med. (2022) 11:5838. doi: 10.3390/jcm11195838, PMID: 36233704
18. Spagnolo PA, Gómez Pérez LJ, Terraneo A, Gallimberti L, and Bonci A. Neural correlates of cue- and stress-induced craving in gambling disorders: implications for transcranial magnetic stimulation interventions. Eur J Neurosci. (2019) 50:2370–83. doi: 10.1111/ejn.14313, PMID: 30575160
19. Neural correlates of cognitive control in gambling disorder: a systematic review of fMRI studies. Available online at: https://www.sciencedirect.com/science/article/abs/pii/S0149763416304596?via%3Dihub (Accessed May 11, 2025)., PMID: 28456569
20. van Holst RJ, van Holstein M, van den Brink W, Veltman DJ, and Goudriaan AE. Response Inhibition during Cue Reactivity in Problem Gamblers: An fMRI Study. PloS One. (2012) 7:e30909. doi: 10.1371/journal.pone.0030909, PMID: 22479305
21. Fujimoto A, Tsurumi K, Kawada R, Murao T, Takeuchi H, Murai T, et al. Deficit of state-dependent risk attitude modulation in gambling disorder. Transl Psychiatry. (2017) 7:e1085–5. doi: 10.1038/tp.2017.55, PMID: 28375207
22. Goudriaan AE, de Ruiter MB, van den Brink W, Oosterlaan J, and Veltman DJ. Brain activation patterns associated with cue reactivity and craving in abstinent problem gamblers, heavy smokers and healthy controls: an fMRI study. Addict Biol. (2010) 15:491–503. doi: 10.1111/j.1369-1600.2010.00242.x, PMID: 20840335
23. Brevers D, Noël X, He Q, Melrose JA, and Bechara A. Increased ventral-striatal activity during monetary decision making is a marker of problem poker gambling severity. Addict Biol. (2016) 21:688–99. doi: 10.1111/adb.12239, PMID: 25781641
24. Del Mauro L, Vergallito A, Gattavara G, Juris L, Gallucci A, Vedani A, et al. Betting on non-invasive brain stimulation to treat gambling disorder: A systematic review and meta-analysis. Brain Sci. (2023) 13:698. doi: 10.3390/brainsci13040698, PMID: 37190663
25. Rossi S, Antal A, Bestmann S, Bikson M, Brewer C, Brockmöller J, et al. Safety and recommendations for TMS use in healthy subjects and patient populations, with updates on training, ethical and regulatory issues: Expert Guidelines. Clin Neurophysiology. (2021) 132:269–306. doi: 10.1016/j.clinph.2020.10.003, PMID: 33243615
26. Ueno S and Sekino M. Figure-eight coils for magnetic stimulation: from focal stimulation to deep stimulation. Front Hum Neurosci. (2021) 15:805971. doi: 10.3389/fnhum.2021.805971, PMID: 34975440
27. Beam W, Borckardt JJ, Reeves ST, and George MS. An efficient and accurate new method for locating the F3 position for prefrontal TMS applications. Brain Stimul. (2009) 2:50–4. doi: 10.1016/j.brs.2008.09.006, PMID: 20539835
28. Mir-Moghtadaei A, Caballero R, Fried P, Fox MD, Lee K, Giacobbe P, et al. Concordance between beamF3 and MRI-neuronavigated target sites for repetitive transcranial magnetic stimulation of the left dorsolateral prefrontal cortex. Brain Stimul. (2015) 8:965–73. doi: 10.1016/j.brs.2015.05.008, PMID: 26115776
29. Badran BW, Ly M, DeVries WH, Glusman CE, Willis A, Pridmore S, et al. Are EMG and visual observation comparable in determining resting motor threshold? A reexamination after twenty years. Brain Stimulation: Basic Translational Clin Res Neuromodulation. (2019) 12:364–6. doi: 10.1016/j.brs.2018.11.003, PMID: 30448078
30. Yamada C, Siste K, Hanafi E, Ophinni Y, Beatrice E, Rafelia V, et al. Relapse prevention group therapy via video-conferencing for substance use disorder: protocol for a multicentre randomised controlled trial in Indonesia. BMJ Open. (2021) 11:e050259. doi: 10.1136/bmjopen-2021-050259, PMID: 34489288
31. Battersby M, Oakes J, Tolchard B, Forbes A, and Pols R. Cognitive behavioral therapy for problem gamblers. In: Zangeneh M, Blaszczynski A, and Turner NE, editors. the Pursuit of Winning: Problem Gambling Theory, Research and Treatment. Springer US, Boston, MA (2008). p. 179–97. doi: 10.1007/978-0-387-72173-6_11
32. Oakes J, Gardiner P, McLaughlin K, and Battersby M. A pilot group cognitive behavioural therapy program for problem gamblers in a rural Australian setting. Int J Ment Health Addiction. (2012) 10:490–500. doi: 10.1007/s11469-010-9294-1
33. Tolchard B and Battersby MW. Cognitive behaviour therapy for problem gamblers: A clinical outcomes evaluation. Behav Change. (2013) 30:12–23. doi: 10.1017/bec.2013.2
34. Higuchi S, Matsushita S, and Furuno S. Gambling Disorder STEP-G Recovery Support Manual (2021). Available online at: https://kurihama.hosp.go.jp/research/pdf/tool_book_gamble_stepg.pdf (Accessed August 16, 2025).
35. Siste K, Sinambela YSY, Hanafi E, Murtani BJ, Putri KG, Damayanti R, et al. Construct validity and reliability of the south oaks gambling screen among the Indonesian population. J Korean Acad Child Adolesc Psychiatry. (2025) 36:163–71. doi: 10.5765/jkacap.250021, PMID: 40631655
36. Kim SW, Grant JE, Potenza MN, Blanco C, and Hollander E. The Gambling Symptom Assessment Scale (G-SAS): A reliability and validity study. Psychiatry Res. (2009) 166:76–84. doi: 10.1016/j.psychres.2007.11.008, PMID: 19200607
37. Smith DP, Pols RG, Battersby MW, and Harvey PW. The Gambling Urge Scale: Reliability and validity in a clinical population. Addict Res Theory. (2013) 21:113–22. doi: 10.3109/16066359.2012.696293
38. Raylu N and Oei TPS. The Gambling Related Cognitions Scale (GRCS): development, confirmatory factor validation and psychometric properties. Addiction. (2004) 99:757–69. doi: 10.1111/j.1360-0443.2004.00753.x, PMID: 15139874
39. Prasetio CE, Triwahyuni A, and Prathama AG. Psychometric properties of self-report questionnaire-20 (SRQ-20) Indonesian version. Jurnal Psikologi. (2022) 49:69–86. doi: 10.22146/jpsi.69782
40. Dian CN, Effendy E, and Amin MM. The validation of Indonesian version of patient health questionnaire-9. Open Access Macedonian J Med Sci. (2022) 10:193–8. doi: 10.3889/oamjms.2022.9293
41. Busner J and Targum SD. The clinical global impressions scale. Psychiatry (Edgmont). (2007) 4:28–37.
42. Murshed H. Chapter 12 - statistical considerations in radiation oncology. In: Murshed H, editor. Fundamentals of Radiation Oncology, 3rd ed. United States: Academic Press (2019). p. 201–17. Available online at: https://www.sciencedirect.com/science/article/pii/B978012814128100012X (Accessed June 2, 2025).
43. Keel JC, Smith MJ, and Wassermann EM. A safety screening questionnaire for transcranial magnetic stimulation. Clin Neurophysiology. (2001) 112:720. doi: 10.1016/S1388-2457(00)00518-6, PMID: 11332408
44. Pettorruso M, Martinotti G, Montemitro C, De Risio L, Spagnolo PA, Gallimberti L, et al. Multiple sessions of high-frequency repetitive transcranial magnetic stimulation as a potential treatment for gambling addiction: A 3-month, feasibility study. Eur Addict Res. (2019) 26:52–6. doi: 10.1159/000504169, PMID: 31665732
45. Victorri-Vigneau C, Spiers A, Caillet P, Bruneau M, Challet-Bouju G, and Grall-Bronnec M. Opioid antagonists for pharmacological treatment of gambling disorder: are they relevant? Curr Neuropharmacol. (2018) 16:1418–32. doi: 10.2174/1570159X15666170718144058, PMID: 28721822
46. Higueruela-Ahijado M, López-Espuela F, Caro-Alonso PÁ, Novo A, and Rodríguez-Martín B. Efficacy of cognitive-behavioral therapy in improving the quality of life of people with compulsive gambling, a systematic review. Arch Psychiatr Nursing. (2023) 43:127–42. doi: 10.1016/j.apnu.2022.12.014, PMID: 37032006
47. Pettorruso M, Martinotti G, Cocciolillo F, De Risio L, Cinquino A, Di Nicola M, et al. Striatal presynaptic dopaminergic dysfunction in gambling disorder: A 123 I-FP-CIT SPECT study. Addict Biol. (2019) 24:1077–86. doi: 10.1111/adb.12677, PMID: 30226290
48. Clark L, Averbeck B, Payer D, Sescousse G, Winstanley CA, and Xue G. Pathological choice: the neuroscience of gambling and gambling addiction. J Neurosci. (2013) 33:17617–23. doi: 10.1523/JNEUROSCI.3231-13.2013, PMID: 24198353
49. Strafella AP, Paus T, Barrett J, and Dagher A. Repetitive transcranial magnetic stimulation of the human prefrontal cortex induces dopamine release in the caudate nucleus. J Neurosci. (2001) 21:RC157. doi: 10.1523/JNEUROSCI.21-15-j0003.2001, PMID: 11459878
Keywords: gambling disorder, craving, cognitive-behavioral therapy, repetitive transcranial magnetic stimulation, multimodal therapy
Citation: Siste K, Sen LT, Murtani BJ, Hanafi E, Kusuma KS, Aryani A, Schellekens A, van Eijndhoven P, Dalhuisen I and Biemans T (2025) Utilizing repetitive transcranial magnetic stimulation in the management of gambling disorder in Indonesia: protocol for a pilot and feasibility study. Front. Psychiatry 16:1658195. doi: 10.3389/fpsyt.2025.1658195
Received: 02 July 2025; Accepted: 18 August 2025;
Published: 05 September 2025.
Edited by:
Yi-lang Tang, United States Department of Veterans Affairs, United StatesReviewed by:
Katia Nunes Sá, Bahiana School of Medicine and Public Health, BrazilCarmen Concerto, Gaspare Rodolico Hospital, Italy
Copyright © 2025 Siste, Sen, Murtani, Hanafi, Kusuma, Aryani, Schellekens, van Eijndhoven, Dalhuisen and Biemans. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kristiana Siste, a3Npc3RlQHlhaG9vLmNvbQ==
 Kristiana Siste
Kristiana Siste Lee Thung Sen1
Lee Thung Sen1 Belinda Julivia Murtani
Belinda Julivia Murtani Enjeline Hanafi
Enjeline Hanafi Kevin Surya Kusuma
Kevin Surya Kusuma Astria Aryani
Astria Aryani Arnt Schellekens
Arnt Schellekens Philip van Eijndhoven
Philip van Eijndhoven