- Department of Rehabilitation, Hangzhou Children’s Hospital, Hangzhou, Zhejiang, China
Background: Early intervention plays a crucial role in improving outcomes for children with autism spectrum disorder (ASD). The Early Start Denver Model (ESDM) and the Treatment and Education of Autistic and Communication-Handicapped Children (TEACCH) program are commonly used approaches. This study aimed to evaluate whether combining ESDM with TEACCH provides greater clinical benefits than ESDM alone in young children with ASD.
Methods: A retrospective observational study was conducted involving 264 children aged 24–60 months diagnosed with ASD. Participants were divided into two groups based on treatment period: the control group (n = 128) received ESDM-only therapy, while the observation group (n = 136) received ESDM combined with TEACCH over six months. Outcomes were assessed using the Autism Treatment Evaluation Checklist (ATEC) and the Psycho-Educational Profile, Third Edition (PEP-3). Baseline comparability was confirmed by the Chinese version of the Childhood Autism Rating Scale (CCARS).
Results: Both groups showed significant within-group improvement after intervention, but the combined observation group demonstrated greater gains. Post-treatment ATEC scores decreased from 84.56 ± 20.90 to 68.76 ± 17.96 versus 92.84 ± 18.20 to 84.91 ± 17.50 in controls (between-group difference = 16.32 ± 4.35; P < 0.001; Hedges’ g = 0.45). Cognitive scores on the PEP-3 improved by 11.31 points in the observation group compared to 8.15 in controls (P = 0.026). Reductions in maladaptive behaviors also favored the combined intervention (P = 0.036).
Conclusions: The integrated ESDM and TEACCH intervention was more effective than ESDM alone in enhancing cognitive development and reducing symptom severity in young children with ASD.
1 Introduction
Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition characterized by persistent deficits in social communication and interaction, alongside restricted, repetitive patterns of behavior, interests, or activities. The global prevalence of ASD has increased significantly over recent decades, currently estimated at approximately 1 in 100 children, according to the World Health Organization (1). The clinical heterogeneity of ASD presents substantial challenges in early diagnosis and individualized intervention, underscoring the necessity for evidence-based, multifaceted therapeutic approaches tailored to the developmental needs of affected children (2, 3).
Early intervention is widely recognized as a cornerstone in optimizing developmental outcomes in children with ASD (4). Among various early intervention models, the Early Start Denver Model (ESDM) and the Treatment and Education of Autistic and Communication-Handicapped Children (TEACCH) approach have both demonstrated effectiveness across multiple domains (5). ESDM is a comprehensive, play-based, and relationship-focused early behavioral intervention designed for children aged 12 to 48 months. Rooted in principles of applied behavior analysis (ABA), ESDM integrates developmental and behavioral techniques to promote social communication, cognitive, and language skills in naturalistic settings (6, 7). In contrast, the TEACCH program emphasizes structured teaching and environmental modifications to facilitate autonomy, predictability, and task engagement in individuals with ASD. TEACCH is particularly effective in enhancing adaptive behavior and reducing behavioral rigidity through visual supports, individualized routines, and structured learning environments. Although both the Early Start Denver Model (ESDM) and the Treatment and Education of Autistic and Communication-Handicapped Children (TEACCH) program have demonstrated positive outcomes in children with autism spectrum disorder (ASD), existing studies have primarily evaluated these interventions in isolation (8–10). To date, limited research has investigated the clinical effectiveness of combining ESDM and TEACCH within a single, integrated treatment framework (11, 12). In particular, there is a lack of controlled studies directly comparing outcomes between ESDM alone and ESDM combined with TEACCH, which hinders our understanding of the potential added value of such a combined approach (13).
In this context, the present study aims to evaluate the clinical efficacy of a combined intervention strategy incorporating both the Early Start Denver Model and the TEACCH program in children diagnosed with ASD. By assessing the outcomes of this integrated approach, the current research seeks to contribute empirical evidence to inform early intervention strategies and refine multidisciplinary treatment protocols for children with ASD. The findings are expected to enhance our understanding of the potential synergistic effects of combining developmental and structured teaching paradigms in early therapeutic interventions for ASD.
2 Methods
2.1 Study design
This retrospective observational study was conducted to evaluate the clinical efficacy of the ESDM alone and in combination with the TEACCH program in children diagnosed with ASD. The study population comprised patients treated in the Department of Rehabilitation of our institution between January 2021 and December 2024. Inclusion criteria were as follows: (1) a diagnosis of ASD confirmed by qualified developmental pediatricians based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria; (2) age between 24 and 60 months at the time of enrollment; (3) no prior systematic behavioral intervention before receiving treatment at our institution; and (4) complete baseline and follow-up assessment data. Exclusion criteria included: (1) comorbid neurological disorders such as epilepsy or cerebral palsy; (2) significant sensory impairments (e.g., blindness or deafness) that would interfere with behavioral assessment or therapy delivery; (3) Cognitive ability was assessed at baseline using the Chinese revision of the Wechsler Intelligence Scale for Children administered by certified clinical psychologists (14). Children with IQ <40 were excluded; and (4) any major psychiatric disorder other than ASD. Beginning in January 2021, ESDM was formally implemented as the standard intervention. Children with ASD who received ESDM-based therapy between January 2021 and December 2022 (n = 128) were assigned to the control group. From January 2023 onward, the TEACCH program was incorporated into the existing ESDM framework, and children treated between January 2023 and December 2024 (n = 136) were classified into the observation group. Informed consent was obtained from all subjects and/or their legal guardian(s). The study was reviewed and approved by the hospital’s ethics committee. All procedures followed relevant guidelines and adhered to the ethical principles of the Declaration of Helsinki. Participant data were anonymized prior to analysis to ensure confidentiality and privacy.
2.2 ESDM-based intervention in the control group
Children in the control group received intervention based exclusively on the ESDM, a relationship-focused, developmentally informed, and behaviorally based approach designed for young children with ASD. A multidisciplinary intervention team was assembled for each child, consisting of trained therapists, healthcare professionals, and primary caregivers. Each child underwent a comprehensive developmental assessment encompassing cognitive abilities, expressive and receptive language, motor coordination, and social engagement. Based on these assessments, individualized intervention plans were developed with clearly defined rehabilitation objectives. Intervention strategies involved identifying and leveraging the child’s interests to promote engagement, providing timely and responsive feedback during communication, and emphasizing the development of expressive language during social interactions. Positive behavior support techniques were used to encourage the acquisition and generalization of new behaviors and skills. Family involvement was an integral part of the intervention process; caregivers received training to reinforce therapeutic goals in daily life. Specific skill domains targeted during the intervention included imitation, comprehension, verbal communication, social reciprocity, play behaviors, and self-care abilities. Each child received 2-hour daily sessions, six days per week, over a six-month period.
2.3 Combined ESDM and TEACCH intervention in the observation group
Children in the observation group received the same ESDM-based intervention as the control group, supplemented by the TEACCH program, which emphasizes structured teaching and environmental adaptation. The TEACCH strategies used in this study were grounded in its core principles of structured teaching, visual clarity, routine building, and individualized task design aimed at fostering autonomy and behavioral regulation in children with ASD. The observation group also received intervention six days per week for six consecutive months, allowing for direct comparison with the ESDM-only control group to evaluate the potential synergistic effects of the combined approach. The combined intervention targeted five core components:
1. Structured Physical Environment: Therapy spaces were functionally divided into specific zones, including areas for play, group instruction, individual learning, storage, and meals, to enhance spatial predictability and reduce environmental confusion.
2. Visual Structure: Clear visual cues such as colors, shapes, and pictorial aids were used to organize materials and guide learning tasks. Instructional visuals, including sequences for daily routines (e.g., handwashing, table manners, greeting peers), supported comprehension and behavior regulation.
3. Establishment of Daily Routines: Children were guided to develop consistent routines in both learning and daily living contexts. Social behaviors such as greeting others and expressing gratitude were practiced to promote social normalization.
4. Activity Schedules: Individualized daily schedules were created using photos, icons, or simple text, depending on each child’s developmental level. These schedules were posted in both the child’s activity area and the central program board to ensure consistent guidance throughout the day.
5. Individual Work Systems: Tailored task systems were developed based on each child’s functional level, incorporating visual and environmental structure, routine, and task predictability to promote autonomy and task completion.
2.4 Intervention fidelity
Both the ESDM and TEACCH interventions were implemented in our institution following standardized clinical procedures derived from publicly available guidelines and professional training resources. All therapists involved had received structured training in the core principles and techniques of both programs through institution-approved professional development activities. Training was conducted using publicly available resources, including ESDM guidance documents from early intervention platforms such as Foundations (UK), and was overseen by senior clinicians with extensive experience in developmental therapy.
Fidelity to intervention protocols was supported through multiple mechanisms, including standardized session planning templates, family coaching modules, and regular peer or supervisory review of clinical records. The same team of therapists trained in both ESDM and TEACCH strategies provided services to both study groups. As the study was based on retrospective review of routine clinical care, therapists were unaware of any subsequent research use of their sessions, minimizing potential bias in treatment delivery.
2.5 Data collection and assessment tools
Baseline demographic and clinical data were retrospectively extracted from the electronic medical records of all participants. Variables collected included age, sex, parental education, household income, family history of neurodevelopmental disorders, and relevant perinatal factors. Information on comorbid medical or psychiatric conditions (e.g., epilepsy, attention-deficit/hyperactivity disorder, language delay) was also recorded when available. Cognitive ability was assessed at baseline using the Chinese revision of the Wechsler Intelligence Scale for Children administered by certified clinical psychologists (14).
In addition to demographic and clinical characteristics, standardized, validated instruments widely used in autism spectrum disorder (ASD) research and clinical practice were employed to evaluate baseline status and treatment outcomes. All assessment tools were administered in their Chinese-translated and culturally adapted versions, with established reliability and validity for the Chinese pediatric population. Trained clinicians or research staff performed the assessments following standardized protocols, and all scoring was verified by senior developmental specialists to ensure consistency and objectivity.
1. Chinese version of Childhood Autism Rating Scale (CCARS) (15): Prior to intervention, all children underwent diagnostic evaluation using the CCARS, a clinician-administered instrument designed to differentiate children with ASD from those with other developmental disorders and to assess the severity of autism-related behaviors. The scale includes 15 items covering multiple symptom domains, including verbal and non-verbal communication, sensory responses, emotional regulation, and relationship to people. Each item is rated on a 4-point Likert scale (1 to 4), yielding a total score ranging from 15 to 60. According to standard cutoff thresholds, scores <30 indicate no ASD, 30–36 suggest mild-to-moderate ASD, and 37–60 reflect severe ASD.
2. Autism Treatment Evaluation Checklist (ATEC) (16): To evaluate treatment effectiveness, the ATEC was administered both before and after the intervention. Originally developed by Rimland and Edelson, the ATEC is a parent-reported scale designed to monitor changes in core ASD symptoms over time. The checklist consists of 77 items grouped into four subscales: Speech/Language/Communication (0–28 points), Sociability (0–40 points), Sensory/Cognitive Awareness (0–36 points), and Health/Physical/Behavior (0–75 points), for a total possible score of 0–179. Higher total and subscale scores reflect greater symptom severity. The scale is especially useful for longitudinal monitoring of therapeutic response.
3. Psycho-Educational Profile, Third Edition (PEP-3) (17): The PEP-3, was used to assess the developmental functioning and behavioral characteristics of children with ASD across multiple domains. Originally developed by Schopler and colleagues and revised in 2005, the PEP-3 is designed to identify uneven cognitive and behavioral profiles commonly seen in ASD. The PEP-3 includes three main components: (1) direct assessment of developmental and behavioral subtests, (2) caregiver report, and (3) composite scores. Domains assessed include communication, motor skills, maladaptive behavior, and social reciprocity. Lower scores are indicative of more pronounced developmental delays and more severe autistic symptoms.
2.6 Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, USA). Data were first examined for normality using the Kolmogorov–Smirnov test. Continuous variables were expressed as mean ± standard deviation (SD) if normally distributed, or as median with interquartile range (IQR) for non-normally distributed data. Categorical variables were summarized as frequencies and percentages. Between-group comparisons for continuous variables were conducted using independent samples t-tests or the Mann–Whitney U test, as appropriate. Categorical variables were analyzed using the chi-square test or Fisher’s exact test. Within-group comparisons before and after the intervention were performed using paired t-tests or Wilcoxon signed-rank tests, depending on the data distribution. Effect sizes (Cohen’s d) were calculated for primary and key secondary outcomes to aid clinical interpretation. Given the multiple comparisons across PEP-3 subdomains, the Benjamini–Hochberg false discovery rate (FDR) procedure was applied to control for Type I error inflation. To further account for potential baseline confounding, analysis of covariance (ANCOVA) models were performed, adjusting for baseline scores, age, and sex. In addition, propensity score weighting (inverse probability of treatment weighting, IPTW) was conducted using key demographic and clinical variables (age, sex, baseline CCARS, baseline ATEC, and baseline PEP-3 cognition scores) to perform sensitivity analyses. Both adjusted analyses and IPTW confirmed the robustness of the main results. All statistical tests were two-tailed, with a P-value < 0.05 considered statistically significant. For analysis with FDR correction, q-values < 0.05 were regarded as statistically significant.
3 Results
3.1 Baseline characteristics
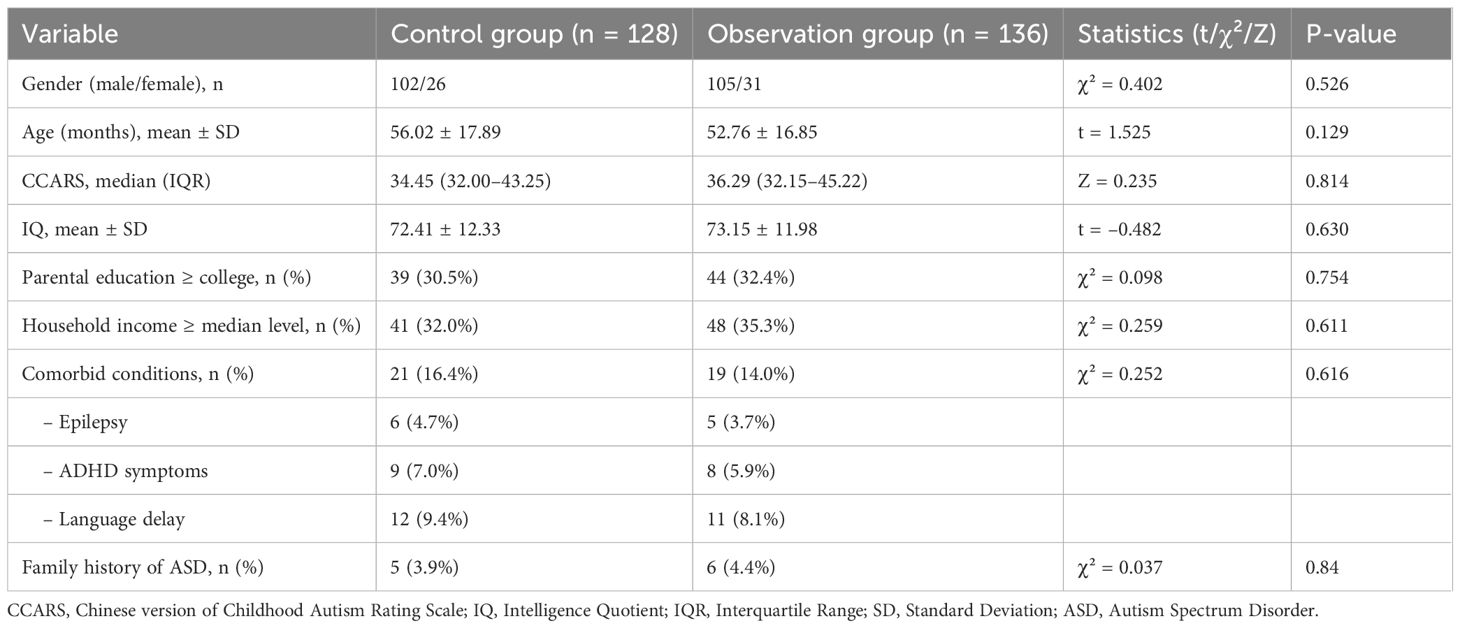
A total of 264 children were included (128 in the control group and 136 in the observation group). The two groups were comparable at baseline with respect to sex distribution (P = 0.526), age (P = 0.129), and CCARS scores (P = 0.814). No significant differences were observed in baseline IQ, socioeconomic indicators (parental education, household income), or the prevalence of comorbid conditions, including epilepsy, ADHD symptoms, and language delay. Family history of ASD was rare and similarly distributed between groups. Overall, baseline demographic and clinical characteristics were balanced, supporting comparability prior to intervention (Table 1).
To further account for potential confounding, adjusted analyses were performed. Covariance models controlling for baseline values and demographic variables confirmed the absence of significant baseline differences. In addition, sensitivity analyses using propensity score weighting yielded consistent results, supporting the robustness of baseline comparability between groups (Supplementary Table 1).
3.2 Changes in ATEC scores
Analysis of within‐group changes in ATEC scores demonstrated statistically significant reductions following intervention in both cohorts. In the control group (n = 128), mean ATEC scores decreased from 92.84 ± 18.20 at baseline to 84.91 ± 17.50 after treatment (t = 3.553, P = 0.001). The observation group (n = 136) exhibited an even greater decline, with scores falling from 84.56 ± 20.90 pre-treatment to 68.76 ± 17.96 post-treatment (t = 6.687, P < 0.001). Between‐group comparisons revealed no significant difference at baseline (mean difference 8.28 ± 5.20; t = 1.865, P = 0.065), confirming comparable starting points. However, post-treatment ATEC scores were significantly lower in the observation group than in controls (mean difference 16.32 ± 4.35; t = 3.647, P < 0.001), indicating superior improvement in the combined ESDM+TEACCH intervention (Table 2). At post-treatment, the between-group effect size for ATEC total favored ESDM+TEACCH (Hedges’ g = 0.45, 95% CI 0.20–0.69) (Supplementary Table 2).
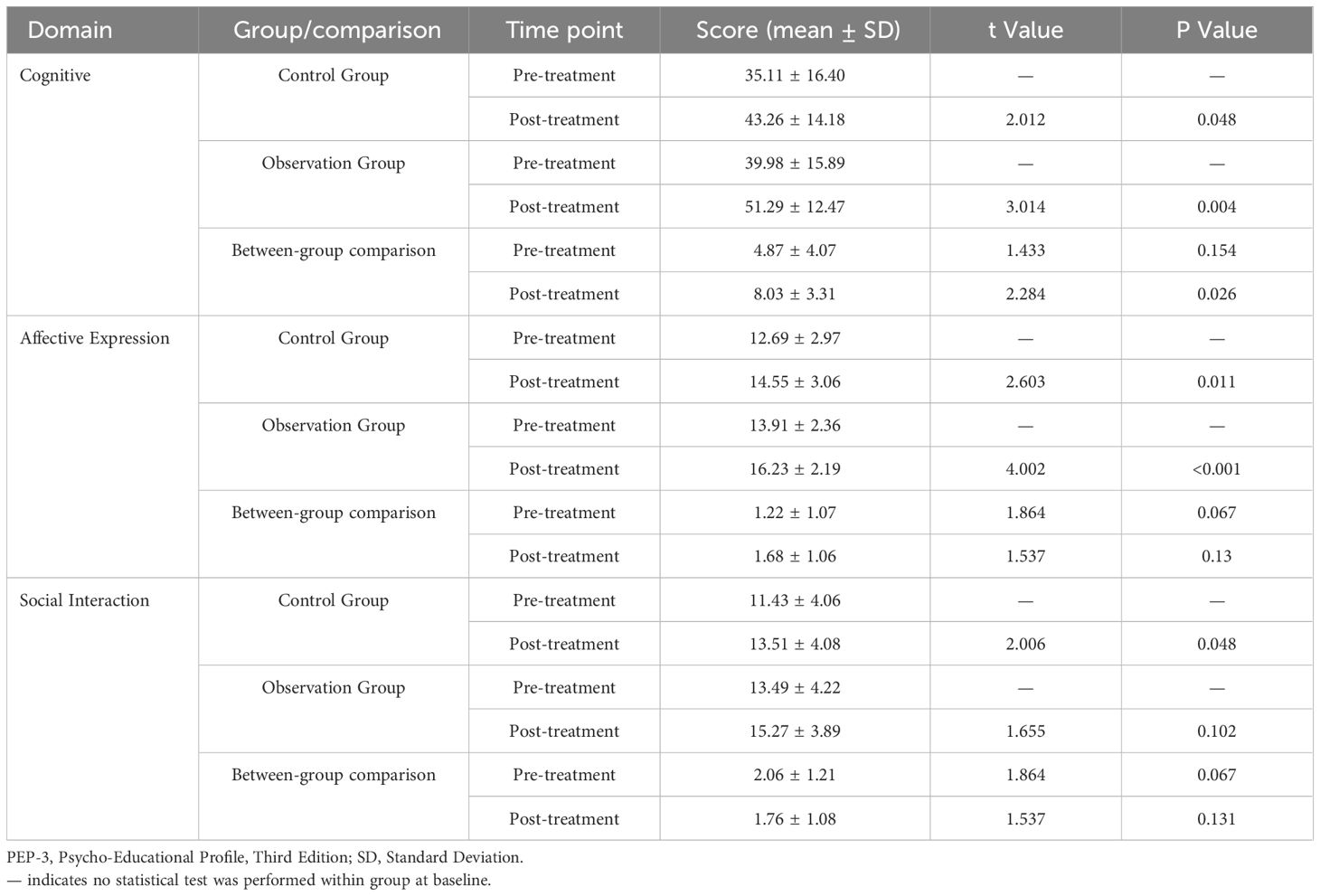
3.3 PEP-3 domain score improvements
Both groups demonstrated improvements across PEP-3 domains following intervention. In the cognitive domain, the control group’s mean score increased from 35.11 ± 16.40 to 43.26 ± 14.18 (P = 0.048), while the observation group rose from 39.98 ± 15.89 to 51.29 ± 12.47 (P = 0.004). Post-treatment between-group comparison favored the observation cohort (difference 8.03 ± 3.31; P = 0.026). Affective expression improved from 12.69 ± 2.97 to 14.55 ± 3.06 in controls (P = 0.011) and from 13.91 ± 2.36 to 16.23 ± 2.19 in the observation group (P < 0.001). Although the between-group difference was not significant (P = 0.130), trends favored combined intervention. Social interaction scores rose significantly in the control group (11.43 ± 4.06 to 13.51 ± 4.08; P = 0.048) and non-significantly in the observation group (13.49 ± 4.22 to 15.27 ± 3.89; P = 0.102). The post-treatment between-group difference (1.76 ± 1.08) did not reach statistical significance (P = 0.131) (Table 3).
3.4 PEP-3 domain score comparisons
Both groups showed significant post-treatment improvements in motor and imitation domains: fine motor (Control: P = 0.014; Observation: P = 0.041), gross motor (Control: P = 0.003; Observation: P = 0.019), and imitation (Control: P = 0.009; Observation: P = 0.001). Reductions in problem behaviors favored the observation group (P = 0.036). Changes in language expression, language understanding, affective expression, social interaction, and behavioral traits did not reach significance (P > 0.05). Baseline scores were comparable across all domains (Table 4). Because multiple comparisons were conducted across PEP-3 subdomains, the Benjamini–Hochberg false discovery rate (FDR) procedure was applied. After adjustment, improvements in the cognitive domain and reductions in problem behaviors remained statistically significant, whereas several borderline results did not survive correction. Detailed uncorrected P-values and FDR-adjusted q-values are provided in Supplementary Table 3.
3.5 ATEC and PEP-3 score difference comparison
The observation group showed significantly greater median improvement in total ATEC scores (12.00 vs. 3.00; P < 0.001) and in PEP-3 cognition (9.00 vs. 5.00; P = 0.004) and problem behavior (2.00 vs. 0.00; P < 0.001) compared with controls. Changes in all other PEP-3domains did not differ significantly between groups (P > 0.05) (Table 5). Rank-biserial effect sizes supported these findings (r = 0.223 for ATEC, r = 0.180 for PEP-3 cognition, and r = 0.259 for problem behavior), consistent with greater improvement in the ESDM+TEACCH group (Supplementary Table 4).

Table 5. Comparison of ATEC and PEP-3 score differences between control and observation groups pre- and post-treatment.
3.6 Power calculation
To evaluate the adequacy of the sample size for detecting meaningful differences in primary and secondary outcomes, a post-hoc power analysis was performed. Under a two-sided α = 0.05 and assuming 80% power, the minimum detectable effect (MDE) for this study was calculated as Cohen’s d ≈ 0.345, which corresponds to approximately 6.12 points for ATEC and 4.60 points for PEP-3 cognition. The observed between-group differences at follow-up were ATEC ≈ 16.15 points and PEP-3 cognition ≈ 8.03 points, both of which exceed the MDE thresholds, indicating that the sample size provided at least 80% power to detect significant differences for the primary endpoints.
4 Discussion
The present study evaluated the effectiveness of combining ESDM with the TEACCH program in young children with ASD. ATEC total scores decreased significantly in both the control and observation groups, with a larger reduction in the latter. On the PEP-3, significant within-group gains were observed for cognition (control: P = 0.048; observation: P = 0.004), fine and gross motor skills, and imitation (all P ≤ 0.041). In contrast, changes in language expression/understanding and social interaction in the observation group did not reach statistical significance (e.g., social interaction P = 0.102). Post-treatment between-group comparisons favored the observation group for cognition (P = 0.026), whereas differences in social interaction were not significant (P = 0.131). Because multiple subdomains were assessed, we applied the Benjamini–Hochberg FDR procedure; after correction, improvements in cognition and reductions in problem behaviors remained significant, while several borderline findings did not survive adjustment.
Regarding developmental domains assessed using the PEP-3, both groups exhibited significant within-group improvements. However, the observation group demonstrated more pronounced gains in cognitive development. Cognition scores increased from approximately 40 to 51 points in the observation group, compared to a more modest increase from 35 to 43 points in the control group. This between-group difference was statistically significant and clinically relevant, given the role of early cognitive ability in predicting adaptive functioning and academic success in ASD. In addition, the combined-treatment group exhibited significantly greater improvements in maladaptive behaviors than the control group. While both groups showed improvements, the observation group achieved significantly larger median improvement. TEACCH is known to manage problem behaviors by promoting environmental structure and visual organization. The incorporation of ESDM techniques, including positive reinforcement and teaching alternative behaviors, likely reinforced these effects by improving communication and reducing frustration. This integrated approach may have created a more supportive and responsive learning environment (4, 18). Notably, the combined intervention also yielded greater reductions in ATEC total scores compared to ESDM alone, further supporting its superior efficacy in alleviating core ASD symptoms. Other developmental domains, such as language expression and comprehension, social interaction, and affective expression, improved similarly in both groups without statistically significant between-group differences. These results suggest that TEACCH alone may be effective in promoting communication and social-emotional development in early ASD intervention. The absence of additional benefit from ESDM in these domains may be due to limited study duration, ceiling effects, or insufficient sensitivity of the assessment tools. Nonetheless, the combined approach showed a broader pattern of improvement, particularly in cognitive functioning and symptom reduction, underscoring the potential advantage of multifaceted interventions (19, 20).
Comparison with previous research provides further support for the current findings. ESDM has been widely studied and recognized for its effectiveness in enhancing cognitive and language outcomes in young children with ASD. Studies such as those by Dawson et al. and Zhou et al. have demonstrated substantial IQ gains and improvements in language development following intensive ESDM intervention (18, 21). These findings parallel the significant cognitive improvements observed in the observation group in our study. Additionally, prior research has shown that ESDM can reduce autism symptom severity, aligning with the greater improvements in ATEC scores noted in the combined-treatment group (22). Conversely, TEACCH has a more varied evidence base. Meta-analyses and empirical studies have suggested that while TEACCH may offer moderate benefits in reducing problem behaviors and enhancing social engagement, its impact on cognitive and language development tends to be more limited. The findings from our study support this interpretation, as the control group showed measurable but smaller gains in cognition and no significant advantage in language or social interaction. This suggests that the structured teaching principles of TEACCH, particularly in managing maladaptive behaviors, may complement the developmental focus of ESDM, resulting in a more comprehensive intervention strategy (23).
Our results extend existing literature by demonstrating that integrating two evidence-based programs with distinct emphases can result in additive benefits. While previous studies, such as the TADPOLE trial, found comparable outcomes among different behavioral interventions, our findings suggest that combining programs with complementary strengths, namely ESDM’s developmental-behavioral framework together with TEACCH’s structured teaching, can yield superior outcomes, particularly in cognitive functioning and behavioral regulation. From a clinical perspective, the study supports the utility of integrated intervention models in early ASD treatment. Practitioners should consider blending strategies from ESDM and TEACCH to address the diverse needs of autistic children. TEACCH provides a predictable, low-stress learning environment, while ESDM promotes engagement, communication, and learning through play-based interaction (24, 25). Together, these approaches can create a responsive and enriched setting conducive to development across multiple domains. Training educators and therapists in both methods may enhance program effectiveness and allow for individualized application based on each child’s profile. Moreover, the observed improvements suggest that early implementation of a combined intervention may enhance school readiness and long-term developmental outcomes. Parental involvement in applying consistent strategies at home can further reinforce gains made in therapy settings, emphasizing the importance of family-centered care (26, 27). Given the robust improvements in cognition and symptom severity, integrating TEACCH into existing ESDM-based programs may represent a feasible and effective approach in clinical practice.
Several limitations should be acknowledged. First, the retrospective, non-randomized design with sequential group assignment across different time periods introduces a risk of temporal confounding. Although baseline demographic and clinical characteristics were comparable, unmeasured changes in clinical practices, therapist experience, or environmental context (e.g., post-COVID factors) may have influenced outcomes. Adjusted analyses using ANCOVA and sensitivity analyses based on propensity score weighting were conducted to mitigate these biases, and results remained consistent. Nevertheless, residual confounding cannot be fully excluded. Second, intervention fidelity was not formally quantified. Although therapists were trained and supervised in both ESDM and TEACCH protocols, and session records were regularly reviewed, the absence of prospective fidelity scoring (e.g., video review or inter-rater reliability) limits the ability to assess consistency of implementation across participants. Third, several baseline covariates such as socioeconomic status, comorbidities, and family history were retrospectively extracted from clinical records and may have been incompletely documented, which reduced our capacity to fully adjust for potential confounders. Fourth, outcome evaluation partly relied on parent-reported measures (e.g., ATEC), which are susceptible to expectancy and reporting bias, particularly in the absence of blinding. While standardized tools like the PEP-3 were also used, caregiver perceptions may have influenced observed differences. Therapists and caregivers were not blinded to intervention type, which may have introduced additional bias. Fifth, the relatively short follow-up period precludes conclusions about the long-term durability of treatment effects. Additionally, not all developmental domains showed significant between-group differences, which may reflect limited intervention duration, ceiling effects of assessment tools, or insufficient statistical power. Finally, concurrent implementation of both ESDM and TEACCH requires substantial time and institutional resources, potentially limiting feasibility in low-resource settings. Future research should prioritize randomized controlled trials with prospective fidelity monitoring, blinded assessments, and longer-term follow-up. Stratified analyses may also help identify subgroups that derive the greatest benefit from integrated interventions.
5 Conclusions
In conclusion, the combined application of the ESDM and the TEACCH program demonstrated superior efficacy in improving cognitive development and reducing autism symptom severity in young children with ASD compared to ESDM alone. These findings support the clinical value of integrated intervention models in enhancing early developmental outcomes for children on the autism spectrum.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Hangzhou Children’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
LM: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Resources, Software, Supervision, Writing – original draft, Writing – review & editing. QL: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Resources, Software, Writing – original draft, Supervision. YX: Conceptualization, Methodology, Data curation, Formal Analysis, Investigation, Resources, Software, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We sincerely thank all the people who participated in this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1669476/full#supplementary-material
References
1. Hodges H, Fealko C, and Soares N. Autism spectrum disorder: definition, epidemiology, causes, and clinical evaluation. Transl Pediatr. (2020) 9:S55–s65. doi: 10.21037/tp.2019.09.09
2. Wood JJ, Kendall PC, Wood KS, Kerns CM, Seltzer M, Small BJ, et al. Cognitive behavioral treatments for anxiety in children with autism spectrum disorder: A randomized clinical trial. JAMA Psychiatry. (2020) 77:474–83. doi: 10.1001/jamapsychiatry.2019.4160
3. Özkan E, Belhan Çelik S, Yaran M, and Bumin G. Joint attention-based occupational therapy intervention in preschoolers with autism spectrum disorder: A randomized controlled trial. Am J Occup Ther. (2023) 77. doi: 10.5014/ajot.2023.050177
4. Fuller EA, Oliver K, Vejnoska SF, and Rogers SJ. The effects of the early start Denver model for children with autism spectrum disorder: A meta-analysis. Brain Sci. (2020) 10. doi: 10.3390/brainsci10060368
5. Geoffray MM, Oreve MJ, Jurek L, Sonie S, Schroder C, Delvenne V, et al. Early Start Denver Model effectiveness in young autistic children: a large multicentric randomised controlled trial in two European countries. BMJ Ment Health. (2025) 28. doi: 10.1136/bmjment-2024-301424
6. Kasari C, Shire S, Shih W, Landa R, Levato L, and Smith T. Spoken language outcomes in limited language preschoolers with autism and global developmental delay: RCT of early intervention approaches. Autism Res Jun. (2023) 16:1236–46. doi: 10.1002/aur.2932
7. Wang Z, Zheng L, Yang L, Yin S, Yu S, Chen K, et al. Structural and functional whole brain changes in autism spectrum disorder at different age stages. Eur Child Adolesc Psychiatry May. (2025) 34:1589–602. doi: 10.1007/s00787-024-02585-6
8. Suprihatin S and Indina T. Evaluating the Outcome of Structured Teaching Intervention for Children with Autism. Paris, France: Atlantis Press (2019) p. 286–9.
9. Virues-Ortega J, Julio FM, and Pastor-Barriuso R. The TEACCH program for children and adults with autism: A meta-analysis of intervention studies. Clin Psychol Review. (2013) 33:940–53. doi: 10.1016/j.cpr.2013.07.005
10. Eapen V, Črnčec R, and Walter A. Clinical outcomes of an early intervention program for preschool children with Autism Spectrum Disorder in a community group setting. BMC Pediatrics. (2013) 13:3. doi: 10.1186/1471-2431-13-3
11. Oswald TM, Winder-Patel B, Ruder S, Xing G, Stahmer A, and Solomon M. A pilot randomized controlled trial of the ACCESS program: A group intervention to improve social, adaptive functioning, stress coping, and self-determination outcomes in young adults with autism spectrum disorder. J Autism Dev Disord May. (2018) 48:1742–60. doi: 10.1007/s10803-017-3421-9
12. Brierley NJ, McDonnell CG, Parks KMA, Schulz SE, Dalal TC, Kelley E, et al. Factor structure of repetitive behaviors across autism spectrum disorder and attention-deficit/hyperactivity disorder. J Autism Dev Disord. (2021) 51:3391–400. doi: 10.1007/s10803-020-04800-0
13. Srinivasan S, Patel S, Khade A, Bedi G, Mohite J, Sen A, et al. Efficacy of a novel augmentative and alternative communication system in promoting requesting skills in young children with Autism Spectrum Disorder in India: A pilot study. Autism Dev Lang Impair. (2022) 7:23969415221120749. doi: 10.1177/23969415221120749
14. Gong Y and Cai T. The Chinese revision of the Wechsler intelligence scale for children. Chin J Clin Psychol. (1994) 2:1–6.
15. Li Y, Huo Y, Zhang Y, Qiu X, Ma C, Yin A, et al. Reliability and validity analysis of the parent version of the childhood autism rating scale. J Educ Biol. 12:421.
16. Mahapatra S, Vyshedsky D, Martinez S, Kannel B, Braverman J, Edelson SM, et al. Autism treatment evaluation checklist (ATEC) norms: A "Growth chart" for ATEC score changes as a function of age. Children (Basel). (2018) 5. doi: 10.3390/children5020025
17. Shek DT and Yu L. Construct validity of the Chinese version of the psycho-educational profile-3rd edition (CPEP-3). J Autism Dev Disord. (2014) 44:2832–43. doi: 10.1007/s10803-014-2143-5
18. Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, et al. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics. (2010) 125:e17–23. doi: 10.1542/peds.2009-0958
19. Asta L and Persico AM. Differential predictors of response to early start Denver model vs. Early intensive behavioral intervention in young children with autism spectrum disorder: A systematic review and meta-analysis. Brain Sci. (2022) 12. doi: 10.3390/brainsci12111499
20. Godel M, Robain F, Kojovic N, Franchini M, Wood de Wilde H, and Schaer M. Distinct patterns of cognitive outcome in young children with autism spectrum disorder receiving the early start Denver model. Front Psychiatry. (2022) 13:835580. doi: 10.3389/fpsyt.2022.835580
21. Zhou B, Xu Q, Li H, Zhang Y, Wang Y, Rogers SJ, et al. Effects of parent-implemented early start Denver model intervention on Chinese toddlers with autism spectrum disorder: A non-randomized controlled trial. Autism Res Apr. (2018) 11:654–66. doi: 10.1002/aur.1917
22. Wang SH, Zhang HT, Zou YY, Cheng SM, Zou XB, and Chen KY. Efficacy and moderating factors of the Early Start Denver Model in Chinese toddlers with autism spectrum disorder: a longitudinal study. World J Pediatr Aug. (2023) 19:741–52. doi: 10.1007/s12519-022-00555-z
23. Yang Y, Wang H, Xu H, Yao M, and Yu D. Randomized, controlled trial of a mixed early start Denver model for toddlers and preschoolers with autism. Autism Res Aug. (2023) 16:1640–9. doi: 10.1002/aur.3006
24. Asta L, Di Bella T, La Fauci Belponer F, Bruschetta M, Martines S, Basile E, et al. Cognitive, behavioral and socio-communication skills as predictors of response to Early Start Denver Model: a prospective study in 32 young children with Autism Spectrum Disorder. Front Psychiatry. (2024) 15:1358419. doi: 10.3389/fpsyt.2024.1358419
25. Tateno Y, Kumagai K, Monden R, Nanba K, Yano A, Shiraishi E, et al. The efficacy of early start Denver model intervention in young children with autism spectrum disorder within Japan: A preliminary study. Soa Chongsonyon Chongsin Uihak. (2021) 32:35–40. doi: 10.5765/jkacap.200040
26. Contaldo A, Colombi C, Pierotti C, Masoni P, and Muratori F. Outcomes and moderators of Early Start Denver Model intervention in young children with autism spectrum disorder delivered in a mixed individual and group setting. Autism. (2020) 24:718–29. doi: 10.1177/1362361319888344
Keywords: autism spectrum disorder, early start Denver model, TEACCH program, cognitive development, behavioral intervention
Citation: Ma L-L, Lv Q-Q and Xiao Y (2025) Efficacy of the early start Denver model combined with the TEACCH program in children with autism spectrum disorder. Front. Psychiatry 16:1669476. doi: 10.3389/fpsyt.2025.1669476
Received: 19 July 2025; Accepted: 30 October 2025;
Published: 18 November 2025.
Edited by:
Antonio Narzisi, Stella Maris Foundation (IRCCS), ItalyReviewed by:
Cecilia Montiel Nava, The University of Texas Rio Grande Valley, United StatesFrancisco Alcantud-Marín, University of Valencia, Spain
Copyright © 2025 Ma, Lv and Xiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ling-Ling Ma, TGluZ0xpbmdNMTIzQGhvdG1haWwuY29t
 Ling-Ling Ma
Ling-Ling Ma Qian-Qian Lv
Qian-Qian Lv Yao Xiao
Yao Xiao