- 1Clinical Psychology Department, Nursing Department, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2Social Work Department, Shanghai Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 3General Surgery,Nursing Department, Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 4General Psychiatry Department, Nursing Department, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
Introduction: This systematic review summarizes the recommendations related to psychosocial interventions for anxiety disorders included in existing guidelines and compares their differences.
Methods: Computer-based searches were conducted to identify relevant guidelines on psychosocial interventions for anxiety disorders from domestic and international guideline websites, professional association websites, and other relevant databases. The guidelines’ quality was evaluated using the Appraisal of Guidelines for Research and Evaluation II (AGREE II) tool.
Results: Fourteen guidelines from nine countries were included, with AGREE II scores ranging between 64.4%–96.3%. The specific recommendations were synthesized into a single evidence map, revealing that cognitive behavioral therapy demonstrated strong support for treating generalized anxiety, panic, and social anxiety disorders. Conversely, eye movement desensitization and reprocessing, exposure therapy, and virtual reality exposure therapy were not recommended for panic disorder. Additionally, no guidelines provided any recommendations for psychosocial interventions for separation anxiety disorder.
Discussion: Guidelines on psychosocial interventions for adult anxiety disorders vary remarkably concerning their quality and recommended suggestions. Future guideline development or updates should strictly adhere to standardized development processes. Additionally, researchers should double their efforts to continuously explore and validate the efficacy of various psychosocial interventions in anxiety populations.
Sytematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD420250654358, PROSPERO, identifier CRD420250654358.
1 Introduction
Anxiety disorders predominantly consist of generalized anxiety disorder, panic disorder, agoraphobia, specific phobia, social anxiety disorder, separation anxiety disorder, and selective mutism. These conditions are characterized by excessive fear, worry, and associated behavioral disturbances (1). Over the past three decades, China has undergone unprecedented economic development and social transformation. This profound shift has exposed the population to a range of challenges spanning work, education, cultural perceptions, and social norms. Notably, this societal context may be linked to the rising prevalence of anxiety disorders. Currently, anxiety disorders rank as the mental illness with the highest lifetime prevalence rate in China, at 7.57% (2). Globally, anxiety disorders also remain highly prevalent. The World Health Organization report demonstrates that approximately 301 million people suffer from anxiety disorders (3). Moreover, anxiety disorders frequently present alongside other mental or physical health conditions. Among psychiatric comorbidities, major depressive disorder is the most prevalent, as noted by Penninx, Pine, Holmes and Reif (1), and can increase the severity of anxiety disorders to a certain extent. Given that individuals with anxiety disorders typically experience persistent fear and worry, the condition is often associated with impairments across critical domains such as personal life, family functioning, social participation, and career development. Without timely intervention, it may further lead to functional deficits in areas including academic performance, cognitive functioning, decision-making capabilities, and attention span—ultimately impairing these individuals’ ability to carry out daily activities.
Presently, the treatment modalities for anxiety disorders largely include pharmaceutical treatment, psychosocial interventions, physical rehabilitation therapies, and management of comorbid diseases. Among these, selective serotonin reuptake inhibitors are regarded as the first-line recommendation for clinical treatment (4). However, long-term use of selective serotonin reuptake inhibitors can lead to adverse reactions, such as lethargy and decreased appetite; studies have confirmed that more than 50% of patients with anxiety are non-responsive to pharmacological treatment (5). Therefore, psychosocial interventions—classified as first-line treatment—have assumed an increasingly critical role in anxiety management. Certain guidelines (6, 7) indicate that psychosocial interventions can replace or partially substitute pharmacological therapy, with their primary objectives being to alleviate core symptoms, such as anxiety, tension, and fear; thereby, improving patients’ quality of life. Compared to routine care, various psychosocial interventions, such as cognitive behavioral therapy (CBT; Papola et al. (8)) and psychodynamic therapy (9), can enhance patients’ coping skills and psychosocial functioning while preventing relapses. It is important to note that psychosocial interventions do not share identical goals. For instance, CBT typically centers on symptom reduction, whereas acceptance- and mindfulness-based interventions—such as Acceptance and Commitment Therapy (ACT)—place greater emphasis on enhancing psychological flexibility and values-based living, rather than directly eliminating symptoms. Additionally, research has examined differences in efficacy among various psychosocial interventions for mixed anxiety disorders. For example, one randomized controlled trial (10), randomly assigned 128 participants diagnosed with at least one anxiety disorder subtype (e.g., generalized anxiety disorder, social anxiety disorder) to either the ACT group or the CBT group. Results revealed that participants in both groups exhibited similar overall reductions in anxiety levels before and after treatment. This study suggests that goal-oriented psychosocial interventions with different foci may all exert positive effects on individuals with mixed anxiety disorders, and their beneficial impacts are not limited to a specific type of anxiety disorder.
To date, clinical research has not reported any serious side effects of psychosocial interventions. Their gentle and sustainable characteristics provide universally applicable and safe treatment options for patients with diverse pathological features. In addition to alleviating anxiety symptoms across cognitive, emotional, and social functional domains, these interventions support long-term rehabilitation and improve both clinical efficacy and quality of life. Therefore, psychosocial interventions should be prioritized as core approaches by clinical practitioners in the treatment protocols for anxiety disorders.
Numerous authoritative organizations worldwide have published clinical practice guidelines for anxiety disorder treatment, which include several psychosocial interventions to assist healthcare providers and patients in making appropriate healthcare decisions in specific clinical contexts. However, these guidelines differ significantly across countries and organizations, and may even offer conflicting recommendations (11). This undermines the value of the guidelines for clinical practice and reduces the compliance of healthcare providers and patients with the recommended interventions. Furthermore, the quality of clinical guidelines is highly contingent on the rigor of their development process. Should deficiencies exist in this process—such as in evidence synthesis, consensus development, or conflict of interest management—it may directly undermine the guidelines’ reliability and applicability. Conducting a systematic review of guidelines within this field is therefore essential. Currently, the Appraisal of Guidelines for Research & Evaluation II (AGREE-II) (12) is widely recognized and adopted as the gold standard for guideline quality assessment in the international evidence-based medicine community. This tool delivers an objective, reproducible, and standardized evaluation of guideline quality across six core domains: Scope and Purpose, Stakeholder Involvement, Rigor of Development, Clarity of Presentation, Applicability, and Editorial Independence—thereby providing a scientific basis for determining guideline quality.
In summary, this study aims to collate international guidelines on anxiety disorders and conduct a systematic review to examine whether the existing guidelines include content on psychosocial interventions, while comparing the methodological quality and recommendations of specific psychosocial interventions mentioned in these guidelines. The goal is to provide a basis and reference for the development of subsequent relevant guidelines and practical decision-making to improve the clinical outcomes for patients with anxiety disorders.
2 Materials and methods
2.1 Study design and registration
This systematic review followed the updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) statement and was recorded on PROSPERO (CRD420250654358), with our protocol being released later (13).
2.2 Literature search strategy
In this investigation, we systematically scoured domestic and international guideline websites, professional association websites, and relevant databases. Domestic and international guideline websites included UpToDate, BMJ Best Practice, Guidelines International Network, National Institute for Health and Care Excellence, Scottish Intercollegiate Guidelines Network, New Zealand Guidelines Group, Agency for Healthcare Research and Quality, Registered Nurses’ Association of Ontario, and Medsci Guidelines.
Professional association websites included the American Psychiatric Association, Anxiety and Depression Association of America, United States Preventive Services Task Force, Royal Australian and New Zealand College of Psychiatrists (RANZCP), NSW Ministry of Health, Australian Department of Health and Aged Care, World Federation of Societies of Biological Psychiatry (WFSBP), Chinese Medical Association, and Chinese Association of Integrative Medicine.
Databases included PubMed, Web of Science, Embase, CINAHL, Cochrane Library, Joanna Briggs Institute Database, Wanfang Data Knowledge Service Platform, China National Knowledge Infrastructure, Chinese Biomedical Literature Service System, and Chongqing VIP database. Both MeSH and free-text terms were combined and adopted. English search keywords included “anxiety disorders/anxiety” and “guideline*/consensus*/recommendation*.” Chinese search keywords included “anxiety/anxiety disorders” and “guideline*/consensus*/recommendation*.” The extent of the search went from the creation of the database to January 2025.
2.3 Inclusion and exclusion criteria
Guideline screening was independently conducted by two researchers (Huang and Jin). Inclusion criteria comprised articles published in Chinese or English that addressed psychosocial interventions for anxiety disorders. Exclusion criteria comprised duplicate records or superseded guidelines and guideline interpretations, translations, or post-implementation evaluations. Different reports from the same study can be found in the Supplementary Material (List of Different Reports from the Same Study).
2.4 Literature screening and data extraction
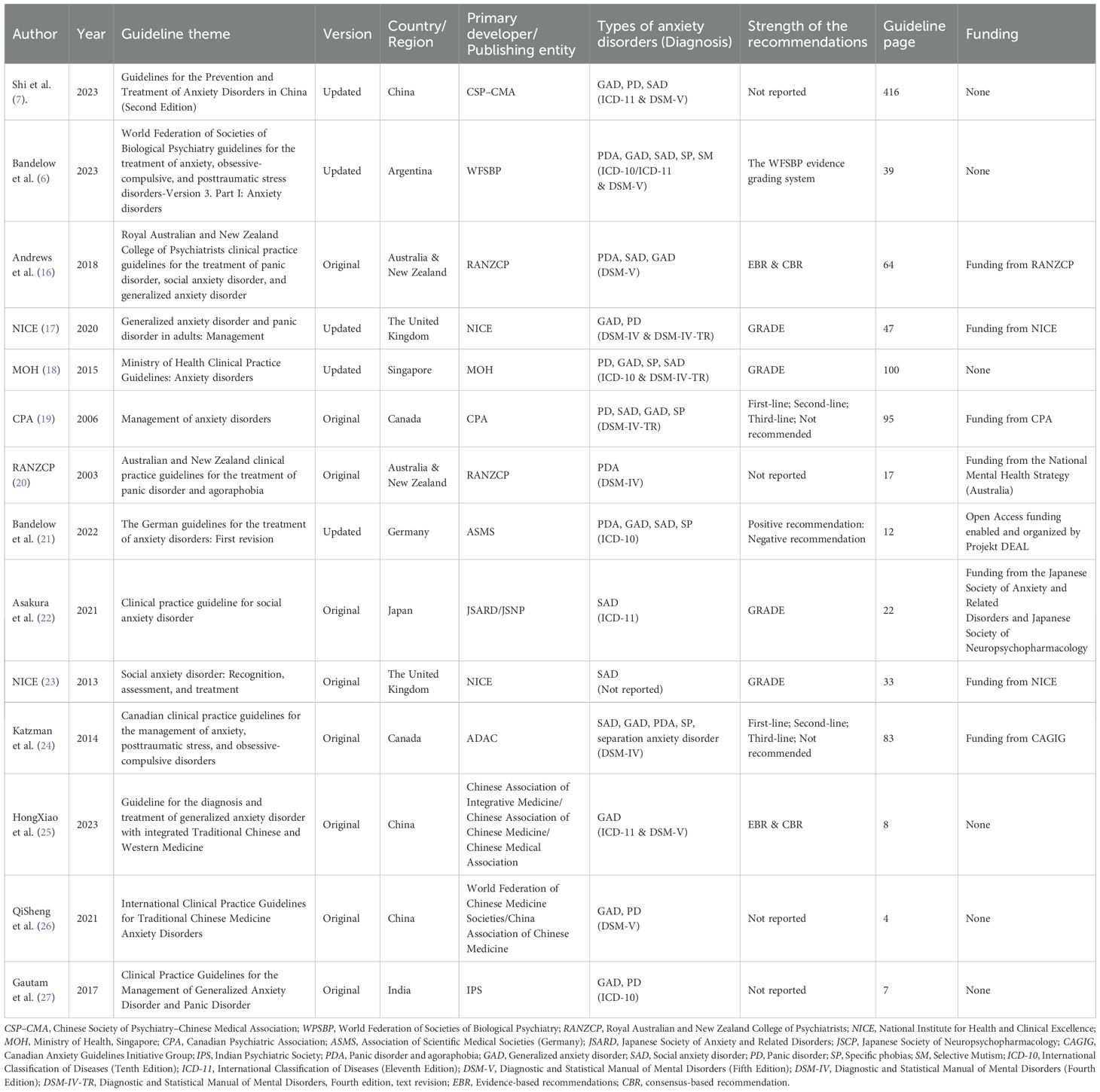
Two researchers, trained in the standardized evidence-based approach, systematically hunted for relevant literature. Studies were logged into the NoteExpress software to eliminate duplicates. Using the Population & Clinical Areas, Interventions, Comparators, Attributes of CPGs, and Recommendation characteristics (PICAR) (14, 15) framework (Table 1), two researchers independently screened titles and abstracts based on the inclusion and exclusion criteria. Finally, the full text was read for rescreening. Data were extracted using a specially designed basic information extraction table and a content extraction table, and then cross checked. The basic information extraction form for the guidelines included authors, guideline title, type, country/region, target population, and development/update date. The recommendation content extraction form included types of anxiety disorders addressed in the guideline, recommended specific psychosocial interventions, and recommendation strength.
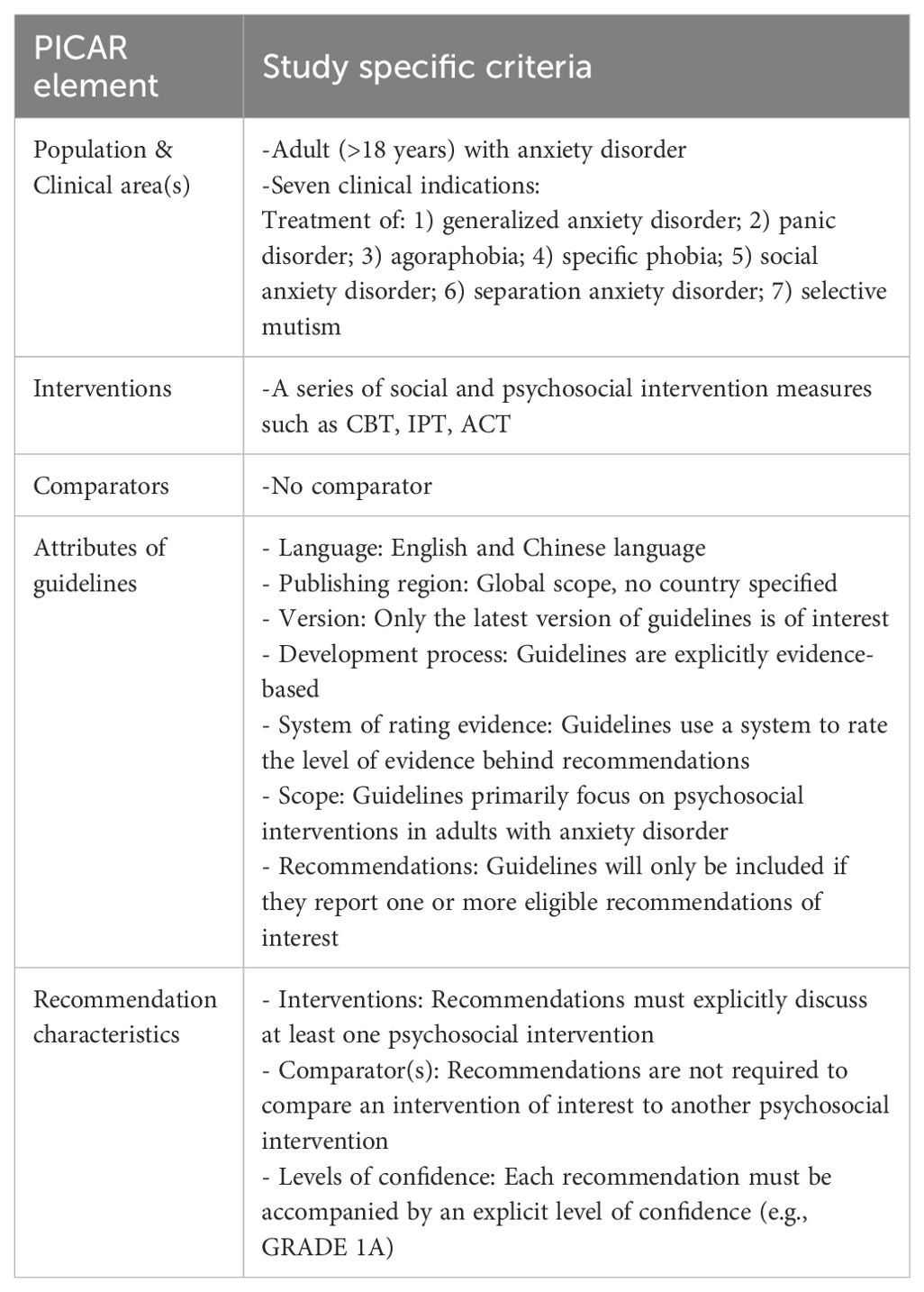
Table 1. Eligibility criteria pertaining to the population & clinical areas, interventions, comparators, attributes of CPGs, and recommendation characteristics (PICAR) framework.
2.5 Quality evaluation of included guidelines
In this study, we utilized the Appraisal of Guidelines for Research and Evaluation II (AGREE II (12);) to examine and determine the methodological quality of the guidelines that had been included. Four researchers (Huang, Jin, Luo, and Cai) independently conducted the evaluations after receiving training on AGREE II scoring criteria. Each included guideline was rated item-by-item according to the AGREE II criteria, with researchers documenting their rationales for each score. To determine the inter-rater reliability, the intraclass correlation coefficient (ICC (28);) was utilized. The descriptions for the ICC values were presented in the following manner: ICC < 0.40 indicated low consistency, 0.40 ≤ ICC < 0.75 indicated average consistency, and ICC ≥ 0.75 indicated high consistency.
AGREE II comprises 23 articles that are divided into 6 domains, consisting of “Scope and Purpose,” “Stakeholder Involvement,” “Rigor of Development,” “Clarity of Presentation,” “Applicability,” and “Editorial Independence.” Every item is evaluated using a scale ranging from 1 to 7. A rating of 1 signifies total non-conformance, whereas a rating of 7 represents full conformance. The standardized scores for each area are identified as the ratio of the highest possible score for that area expressed as a percentage. The calculation for the standardized score is [(actual score – minimum possible score)/(maximum possible score – minimum possible score)] x 100%. A higher score implies a higher standard of the guideline in that area. According to the standardized scores of each field in the guidelines, the recommendations are divided into three levels: Recommended: Six areas with scores ≥60% are rated as level A, Recommended with modifications: There are ≥3 fields with a score of ≥30%; however, <60% of the fields are rated as level B, and Not recommended: Fields with scores <30% and ≥3 are rated as level C.
2.6 Integration of the recommendations in the guidelines
Two researchers integrated the recommended situations into the guidelines extracted from the content extraction form of the guidelines’ recommendations. Among them, the recommended situations were classified into “strong recommendation,” “recommendation,” “unclear recommendation,” “non-recommendation,” and “not mentioned.” Additionally, we constructed a bubble chart to display the recommended situations of psychosocial interventions for various kinds of anxiety disorders stated in each guideline. Different types of anxiety disorders were presented on the Y-axis, and different types of psychosocial interventions were presented on the X-axis. Four colored spheres, namely green (strong recommendation), blue (recommendation), red (non-recommendation), and yellow (unclear recommendation), were used to distinguish between and visualize the recommended situations of the psychosocial interventions for different types of anxiety disorders.
3 Results
3.1 Study selection
The database investigation initially retrieved 2,087 works, which were reduced to 117 after the elimination of duplicates and the exclusion of irrelevant records by title and abstract. A full-text assessment was conducted for these 117 works. Following the application of the inclusion and exclusion criteria (Supplementary Figure 1), numerous articles were excluded. Finally, 14 guidelines from 12 organizations were incorporated into this research (6, 7, 16–27).
3.2 Characteristics of the guidelines
The characteristics of the incorporated guidelines are presented in Table 2. The publication years of these guidelines spanned from 2003 to 2023 in China (n = 3), Argentina (n = 1), Australia and New Zealand (n = 2), the UK (n = 2), Singapore (n = 1), Canada (n = 2), Germany (n = 1), Japan (n = 1), and India (n = 1); 35.7% of these guidelines were updated versions. None of the 14 guidelines included all types of anxiety. Of these, generalized anxiety disorder was included in 10 guidelines, social anxiety disorder in 9, specific phobia in 5, panic disorder in 6, panic disorder with agoraphobia in 4, SM in one, and separation anxiety disorder in two. Four guidelines used the Grading of Recommendations Assessment, Development, and Evaluation system, whereas four guidelines did not report on the strength of the recommendations. The funding information was reported in eight guidelines.
3.3 Quality of the guidelines
Supplementary Table 2 presents the AGREE II scores for all 14 guidelines. The average AGREE II scores for the guidelines corresponding to the six domains were: “Scope and Purpose” – 94.1%, “Stakeholder Involvement” – 83.9%, “Rigor of Development” – 77.5%, “Clarity of Presentation” – 92.3%, “Applicability” – 77.9%, and “Editorial Independence” – 70.4%. Ten guidelines from seven organizations, namely WFSBP, RANZCP, National Institute for Health and Care Excellence, Ministry of Health (MOH), Canadian Psychiatric Association (CPA), Association of Scientific Medical Societies (Germany) (ASMA), Japanese Society of Anxiety and Related Disorders (JSARD)/Japanese Society of Neuropsychopharmacology (JSNP), and Canadian Anxiety Guidelines Initiative Group, were regarded as “recommended” (6, 16–24). Four remaining guidelines were scored as “recommended with modifications” (7, 25–27), whereas no guideline was regarded as “non-recommendation.” The ICC value for the assessment results using AGREE II was 0.854, indicating that the internal agreement of the four assessors was relatively consistent. Supplementary Figure 2 illustrates the overall quality score of AGREE II for each guideline. Supplementary Figure 3 compares scores across the six domains for every guideline.
3.4 Recommendations for psychosocial interventions for adults with anxiety disorder
Supplementary Table 3 summarizes the recommendations for psychosocial interventions for patients with anxiety in the 14 guidelines. Accordingly, Figure 1 visualizes and displays the recommended situations of the guidelines. Among them, several recommendations on psychosocial interventions were available for generalized anxiety disorder, panic disorder, and social anxiety disorder. Conversely, recommendations for specific phobias, agoraphobia, and selective mutism were noticeably fewer. During the guideline review, no recommendations for psychosocial interventions for separation anxiety disorder were identified. The WFSBP noted that, since separation anxiety disorder primarily affected children and adolescents, research on separation anxiety disorder in adults was limited; therefore, no recommendations could be made.
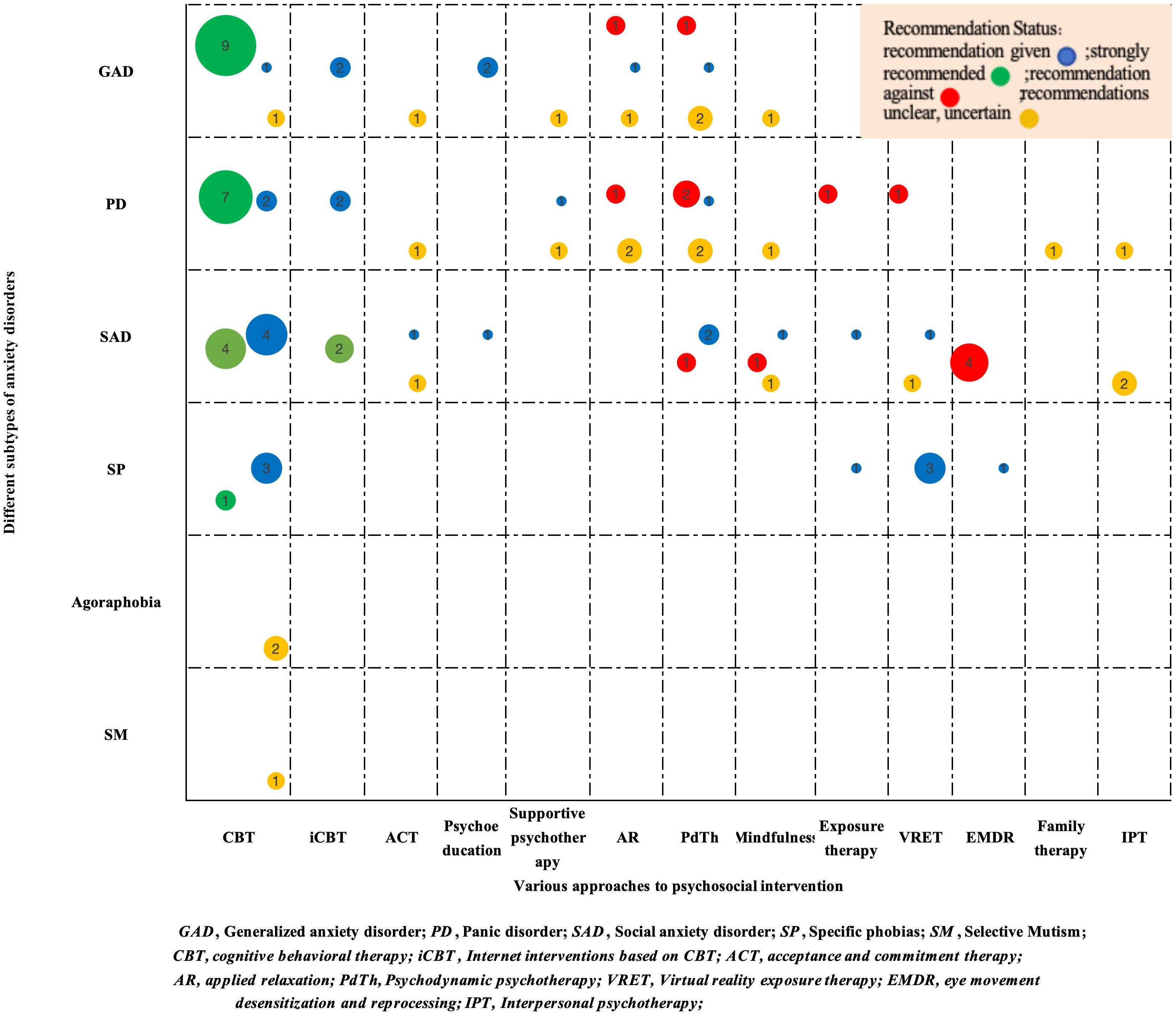
Figure 1. Evidence map of recommended psychosocial interventions in clinical practice guidelines for anxiety disorders.
For generalized anxiety disorder, nine guidelines strongly recommended CBT as a first-line treatment. Two additional guidelines indicated that internet interventions based on CBT (iCBT) could be recommended to reduce waiting times before initiating face-to-face CBT or as an adjunct to standard CBT. Psychoeducation was recommended for patients with generalized anxiety disorder in two guidelines. Although acceptance and commitment therapy, supportive psychotherapy, and mindfulness were mentioned in the guidelines, these psychosocial interventions were classified as “recommended with uncertainty” or “unclear recommendation” due to insufficient high-quality evidence to validate their effectiveness. The WFSBP did not recommend relaxation or psychodynamic therapy for generalized anxiety disorder, whereas few guidelines included these interventions. Similarly, relaxation and psychodynamic therapy were frequently classified as “recommended with uncertainty” or “unclear recommendation” due to limited evidence.
For panic disorder, seven guidelines strongly recommended CBT as a first-line treatment. Similar to generalized anxiety disorder, two guidelines recommended iCBT as an adjunct to CBT. Few guidelines mentioned supportive psychotherapy, acceptance and commitment therapy, family therapy, interpersonal therapy, and mindfulness; however, these methods were classified as “recommended with uncertainty” or “unclear recommendation” due to limited evidence. There were significant differences in the recommendations for psychodynamic psychotherapy and applied relaxation among the guidelines. Among them, the Association of Scientific Medical Societies recommends psychodynamic psychotherapy as an intervention for panic disorder, RANZCP (16) and Shi and Wenyuan (7) label it as an “unclear recommendation,” and the WFSBP and Canadian Psychiatric Association (CPA) refrain from recommending it. CPA advises against using applied relaxation as an approach for panic disorder, whereas the WFSBP and RANZCP (20) label it as an “unclear recommendation.” Two guidelines do not recommend exposure therapy and virtual reality exposure therapy for panic disorder. The WFSBP, RANZCP (16), CPA, and RANZCP (20) do not recommend eye movement desensitization and reprocessing for managing panic disorder.
For social anxiety disorder, four guidelines strongly recommended CBT as a first-line treatment. The WFSBP and ADAC recommended iCBT as an adjunct to CBT. Separate guidelines recommended psychoeducation and exposure therapy. Currently, the quality of evidence for acceptance and commitment therapy, virtual reality exposure therapy, and interpersonal psychotherapy is inconsistent, leading existing guidelines to avoid clear recommendations or acknowledging their potential benefits. There are differences in recommendations for psychodynamic psychotherapy and mindfulness among various guidelines. Guidelines from Association of Scientific Medical Societies (21) and National Institute for Health and Clinical Excellence (23) recommend psychodynamic psychotherapy for social anxiety disorder, whereas WFSBP did not recommend it. Shi and Wenyuan (7) suggest using mindfulness therapy to treat social anxiety disorder. The recommendation for RANZCP (16) is unclear, whereas the National Institute for Health and Clinical Excellence (23) does not recommend mindfulness as a routine treatment for social anxiety disorder.
For specific phobias, the existing guidelines recommended four psychosocial interventions: CBT, exposure therapy, virtual reality exposure therapy, and eye movement desensitization and reprocessing. Some guidelines suggested CBT for agoraphobia and selective mutism; however, due to inconsistent evidence, CBT was classified as “recommended with uncertainty” or “unclear recommendation.” Currently, no guidelines recommend psychosocial interventions for separation anxiety disorder.
4 Discussion
4.1 Principal findings
AGREE II evaluation results indicate that the 14 guidelines included in this study were of high quality, with those from JSARD/JSNP (22), RANZCP (16), and MOH (18) ranking among the top performers. Specifically, “Scope and Purpose” and “Clarity of Presentation” attained remarkable scores, reflecting well-defined clinical issues, clear target populations, and unambiguous presentation of recommendations facilitating evidence accessibility for clinicians. Some guidelines have standardized scores of less than 60% in the four domains of “Stakeholder Involvement,” “Rigor of Development,” “Applicability,” and “Editorial Independence.” The rationale is that, in “Stakeholder Involvement,” some guidelines (27) did not include patients as stakeholders in the development process. In “Rigor of Development,” some guidelines (27) did not provide detailed descriptions of the methods for retrieving evidence and the strength of the evidence. In “Applicability,” although some guidelines (25) describe implementation strategies, there is a lack of evidence on potential obstacles in the application. In “Editorial Independence,” during the compilation process, a few guidelines (7, 26) did not elaborate on the conflicts of interest and the project funding details among those involved in developing the guidelines. Thus, when formulating or revising the guidelines for psychosocial interventions for anxiety disorders in the future, involving stakeholders, considering patient preferences and values, and developing recommendations scientifically and rigorously while factoring in the barriers to the clinical implementation of evidence is necessary. This way, the recommendations can be genuinely and effectively utilized in clinical practice.
The evidence map in this report provides an overview of the psychosocial interventions for patients with anxiety disorders. Our evidence mapping analysis revealed that: 1) CBT is supported by robust clinical trial evidence as the first-line psychosocial intervention for generalized anxiety disorder, panic disorder, and social anxiety disorder. 2) Significant evidence gaps exist regarding the efficacy of applied relaxation and psychodynamic psychotherapy for generalized anxiety disorder and panic disorder, necessitating methodologically rigorous clinical trials to establish their therapeutic value. 3) The existing evidence fails to support the use of eye movement desensitization and reprocessing, exposure therapy, or virtual reality exposure therapy in the management of panic disorder. Future research should explore contextual and cultural factors that may influence treatment outcomes. 4) To study the therapeutic efficacy of psychodynamic psychotherapy and interpersonal psychotherapy for social anxiety disorder, mindfulness-based approaches and high-caliber randomized controlled trials are essential. 5) Limited evidence exists for CBT in agoraphobia and SM, with uncertain intervention efficacy requiring further study.
4.2 Strengths, limitations, and comparison with other studies
Presently, no systematic review of psychosocial intervention guidelines for adult patients with anxiety has been retrieved. However, during the literature review process, researchers found two related studies (11, 29) on complementary and alternative therapies for patients with anxiety. In the inclusion section of the guidelines, Zhao, Kennedy, Xu, Conduit, Wang, Zhang, Wang, Yue, Huang, Wang, Xu, Fu and Zheng (11) included ten guidelines (published 2003–2022) in their review, whereas Ng and Jain (29) included 11 guidelines (published 2011–2020) in their review. There were 6 overlapping guidelines between this study and the two aforementioned studies (16, 18, 20, 21, 24, 27), accounting for 42.9% of all guidelines included in this study. This finding indicates that the evidence base of this study is largely consistent with the core guideline framework widely recognized in the field. Notably, this study identified 8 unique guidelines that were not included in the two prior reviews. Of these, 2 were newly published between 2021 and 2023 (6, 22), 3 were China-specific guidelines (7, 25, 26), and 3 were previously overlooked guidelines (17, 19, 23). The inclusion of these unique guidelines provides new evidence and perspectives for the present study. In the recommended population section, the article (29) does not provide clear recommendations for specific subtypes of anxiety disorders, and some recommendations are aimed at cancer survivors, breast cancer survivors, and common mental health disorders. In the recommendation section, only a small part of the article mentions psychosocial interventions and only reviews mindfulness and the application of relaxation. Bandelow, Michaelis and Wedekind (5) conducted a systematic study of treatment recommendations for anxiety disorders based on guidelines and only mentioned CBT as the psychosocial intervention.
Compared with previous studies, our review offers the following advantages. We conducted a relatively systematic and comprehensive search of domestic and international guideline websites, professional association websites, and relevant databases, incorporating more and newer guidelines. The entire process, from literature screening to the integration of recommended opinions, was independently conducted by 2–4 researchers, enabling this study to reach comprehensive and reliable conclusions. This study adopted innovative forms such as radar charts and evidence graphs to visually demonstrate the quality and recommended opinions of social psychosocial intervention guidelines for adult anxiety disorders, while further refining the social psychosocial intervention methods applicable or not applicable to different anxiety disorders. In addition, this study identified gaps in existing guideline recommendations, such as the lack of social and psychosocial intervention recommendations for adult dissociative anxiety disorder, uncertainty in recommendations for mindfulness therapy or psychodynamic therapy, which can provide clear guidance for future research.
However, our research has some limitations. First, it only included guidelines in Chinese and English, and did not search for grey literature, which cannot fully cover all recommendations for social and psychosocial interventions for adult anxiety disorder patients worldwide, and may lead to biased results. Second, this study may involve cultural biases, such as differences in the recognition and value of some intervention measures such as mindfulness therapy and psychodynamics across countries. Future research can enhance global applicability through cultural adaptation adjustment or cross-cultural comparative studies.
4.3 Implications for guideline updates/developments and clinical applications
To date, many countries have developed clinical practice guidelines for anxiety disorders and have pointed out that psychosocial interventions are an important component of the treatment regimen for anxiety disorders. The WHO Mental Health Action Plan (2023-2030) (30) explicitly proposed to “expand the coverage of mental health services, with particular attention to low - and middle-income countries.” However, the fairness of global medical guidelines still faces significant regional differences, with the “guideline practice gap” resultant from resource constraints in low - and middle-income countries being particularly prominent. For example, only 15% of patients with anxiety disorder in sub Saharan Africa can receive standardized treatment, which is far lower than the 70% in high-income countries (31). Studies (32–34) have indicated that in the past decade, the number of people seeking help for anxiety disorders has increased significantly. However, most of their treatment and care are not evidence-based. A cross-sectional survey (35) on doctors’ implementation of clinical practice guidelines has shown that approximately 30% of doctors believe that the guidelines are too complex, making it difficult to find the necessary information and use it in clinical practice. This suggests that researchers should strictly follow the steps for creating guidelines, such as the development process recommended by the American College of Physicians (36), to support clinicians in providing excellent healthcare and closing the existing gap between what the evidence suggests and what is done in practice. Future research may also consider developing practical guidelines for psychosocial interventions for anxiety disorders, which can be directly used by interest groups. At the same time, low-cost intervention programs—such as developing a visual social and psychosocial intervention training manual to enhance the social and psychosocial intervention capabilities of grassroots medical staff in low - and middle-income countries, and reducing per capita costs through group social and psychosocial intervention models—can be explored to further promote accessible and executable standardized interventions for populations in low - and middle-income countries, to narrow the global gap in health equity in anxiety treatment.
The existing guidelines have cumulatively provided 13 psychosocial interventions for anxiety disorders. In specific clinical practice, the preferences and motivations of patients determine the choice of intervention methods. Single or combined psychosocial intervention measures can be provided according to the patient’s needs. Concurrently, the accessibility, cost, and safety of the treatment should be considered. For example, effective face-to-face CBT requires a large number of professionally trained psychotherapists to implement and manage it, and the global shortage of professional psychotherapists might limit the effectiveness of psychotherapy.
Moreover, a study cited in Williams et al. (37) indicates that merely 10%–50% of patients obtain proper treatment within healthcare systems. The primary causes of this situation include shortages in mental health resources, extended waiting periods, and insufficient awareness regarding available treatment alternatives. With the latest advances in digital technology, there has been significant development and growth in digital interventions for treating anxiety disorders. While digital interventions bring benefits to patients with anxiety disorders, they effectively address gaps in the implementation of clinical guidelines and expand the coverage of evidence-based nursing. Patients who were previously reluctant or unable to undergo psychosocial interventions now have an alternative in the form of a sequence of structured iCBT (38, 39). The MindDoc APP designed by Kuester et al. (40) improves patient compliance and anxiety symptoms as well as quality of life through a lightweight psychosocial intervention module. Additionally, digital interventions enhance cost-efficiency and allow for a personalized approach to meet the unique requirements of each patient (41). Another example is that in some developing countries, medical resources are limited, and the high cost of psychosocial interventions makes it difficult for patients to receive long-term treatment. Therefore, clinical practitioners can provide such patients with less expensive and more accessible interventions, such as supportive psychotherapy and psychoeducation, to improve the patient’s symptoms.
Following clinical practice, psychosocial interventions with strong recommendations should be prioritized; however, the continuous updating and iteration of guidelines will inform change in the quality of evidence. Therefore, interventions currently defined as “unclear recommendations” should not be completely negated in clinical practice. Rigorous randomized controlled trials can be designed in the future to collect evidence on the efficacy of such psychosocial interventions, determine the quality of the evidence, and provide corresponding evidence.
5 Conclusions
Specific disparities in the quality of guidelines correlate with psychosocial interventions for anxiety disorders in adults, especially in “Rigor of Development,” “Editorial Independence,” and “Applicability.” Among the different guidelines, there are a few differences in the advice provided regarding psychosocial interventions. Therefore, while formulating or updating guidelines, researchers must strictly adhere to the development process. While providing high-quality evidence for the adult anxiety disorder population, they should ensure that the guidelines are consistent with the emerging evidence. Additionally, future research should focus on discovering the significant impact of specific psychosocial interventions, such as CBT, and pay attention to interventions classified under “unclear recommendations.” Moreover, in clinical practice, scientific and efficient psychosocial interventions should be enforced. This can decrease the difference between the guidelines and practical operations, help those with anxiety disorders improve their emotional experiences, and increase their quality of life.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author/s.
Author contributions
CH: Writing – original draft, Writing – review & editing. XL: Writing – original draft. YL: Writing – original draft. CL: Writing – original draft. JiC: Writing – original draft. YW: Writing – original draft. JuC: Writing – review & editing. ZS: Writing – review & editing. XJ: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This work was supported by the Research Project of Shanghai Nursing Association in 2024, CH (Grant number 2024QN-B03); Shanghai Nursing Association Excellent Youth Nurse Training Program, CH (this project does not have a grant number); Shanghai Municipal Health Commission’s Clinical Research Special Youth Project, XL (Grant number 20204Y0363); and Shanghai Jiao Tong University School of Medicine: Nursing Development Program, XJ (Grant number SJTUHLXK2023).
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1677705/full#supplementary-material.
References
1. Penninx BW, Pine DS, Holmes EA, and Reif A. Anxiety disorders. Lancet. (2021) 397:914–27. doi: 10.1016/S0140-6736(21)00359-7
2. Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, et al. Prevalence of mental disorders in China: A cross-sectional epidemiological study. Lancet Psychiatry. (2019) 6:211–24. doi: 10.1016/S2215-0366(18)30511-X
3. World Health Organization. Mental disorders (2019). Available online at: https://www.who.int/zh/news-room/fact-sheets/detail/mental-disorders (Accessed July 14, 2025).
4. Baldwin DS, Anderson IM, Nutt DJ, Allgulander C, Bandelow B, den Boer JA, et al. Evidence-based pharmacological treatment of anxiety disorders, post-traumatic stress disorder and obsessive–compulsive disorder: A revision of the 2005 guidelines from the British Association for Psychopharmacology. J Psychopharmacol. (2014) 28:403–39. doi: 10.1177/0269881114525674
5. Bandelow B, Michaelis S, and Wedekind D. Treatment of anxiety disorders. Dial Clin Neurosci. (2017) 19:93–107. doi: 10.31887/DCNS.2017.19.2/bbandelow
6. Bandelow B, Allgulander C, Baldwin DS, Costa DLDC, Denys D, Dilbaz N, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for treatment of anxiety, obsessive–compulsive and posttraumatic stress disorders—Version 3. Part I: Anxiety disorders. World J Biol Psychiatry. (2023) 24:79–117. doi: 10.1080/15622975.2022.2086295
7. Shi SX and Wu W. Guidelines for the prevention and treatment of anxiety disorders in China. 2nd ed. Beijing, China: Medical Electronic Audiovisual Publishing House (2023).
8. Papola D, Miguel C, Mazzaglia M, Franco P, Tedeschi F, Romero SA, et al. Psychotherapies for generalized anxiety disorder in adults: A systematic review and network meta-analysis of randomized clinical trials. JAMA Psychiatry. (2024) 81:250–9. doi: 10.1001/jamapsychiatry.2023.3971
9. Mayo-Wilson E, Dias S, Mavranezouli I, Kew K, Clark DM, Ades AE, et al. Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. Lancet Psychiatry. (2014) 1:368–76. doi: 10.1016/S2215-0366(14)70329-3
10. Arch JJ, Eifert GH, Davies C, Plumb Vilardaga JC, Rose RD, and Craske MG. Randomized clinical trial of cognitive behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for mixed anxiety disorders. J Consult Clin Psychol. (2012) 80:750–65. doi: 10.1037/a0028310
11. Zhao FY, Kennedy GA, Xu P, Conduit R, Wang YM, Zhang WJ, et al. Identifying complementary and alternative medicine recommendations for anxiety treatment and care: A systematic review and critical assessment of comprehensive clinical practice guidelines. Front Psychiatry. (2023) 14:1290580. doi: 10.3389/fpsyt.2023.1290580
12. Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. AGREE II: Advancing guideline development, reporting and evaluation in health care. CMAJ. (2010) 182:E839–42. doi: 10.1503/cmaj.090449
13. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
14. Johnston A, Kelly SE, Hsieh SC, Skidmore B, and Wells GA. Systematic reviews of clinical practice guidelines: A methodological guide. J Clin Epidemiol. (2019) 108:64–76. doi: 10.1016/j.jclinepi.2018.11.030
15. Mancin S, Sguanci M, Andreoli D, Soekeland F, Anastasi G, Piredda M, et al. Systematic review of clinical practice guidelines and systematic reviews: A method for conducting comprehensive analysis. MethodsX. (2024) 12:102532. doi: 10.1016/j.mex.2023.102532
16. Andrews G, Bell C, Boyce P, Gale C, Lampe L, Marwat O, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of panic disorder, social anxiety disorder and generalised anxiety disorder. Aust N Z J Psychiatry. (2018) 52:1109–72. doi: 10.1177/0004867418799453
17. National Institute for Health and Clinical Excellence. Generalised anxiety disorder and panic disorder in adults (2020).
19. Canadian Psychiatric Association. Clinical practice guidelines. Management of anxiety disorders. Can J Psychiatry. (2006) 51:9S–91S.
20. Royal Australian and New Zealand College of Psychiatrists Clinical Practice Guidelines Team for Panic Disorder and Agoraphobia. Australian and New Zealand clinical practice guidelines for the treatment of panic disorder and agoraphobia. Aust N Z J Psychiatry. (2003) 37:641–56. doi: 10.1080/j.1440-1614.2003.01254.x
21. Bandelow B, Werner AM, Kopp I, Rudolf S, Wiltink J, and Beutel ME. The German Guidelines for the treatment of anxiety disorders: First revision. Eur Arch Psychiatry Clin Neurosci. (2022) 272:571–82. doi: 10.1007/s00406-021-01324-1
22. Asakura S, Yoshinaga N, Yamada H, Fujii Y, Mitsui N, Kanai Y, et al. Japanese Society of Anxiety and Related Disorders/Japanese Society of Neuropsychopharmacology: Clinical practice guideline for social anxiety disorder (2021). Neuropsychopharmacol Rep. (2023) 43:288–309. doi: 10.1002/npr2.12365
23. National Institute for Health and Clinical Excellence. Social anxiety disorder: Recognition, assessment and treatment (2013).
24. Katzman MA, Bleau P, Blier P, Chokka P, Kjernisted K, Van Ameringen M, et al. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive–compulsive disorders. BMC Psychiatry. (2014) 1:S1. doi: 10.1186/1471-244X-14-S1-S1
25. HongXiao J, Xue L, DongQing Y, Zhiyuan H, QunSong W, Jian W, et al. Guideline for the diagnosis and treatment of generalized anxiety disorder with integrated traditional Chinese and western medicine. Mod Chin Clin Med. (2023) 30:21–7 + 35. doi: 10.3969/j.issn.2095-6606.2023.06.005
26. QiSheng T, Miao Q, and WenJun S. International clinical practice guidelines for traditional Chinese medicine anxiety disorders. World Chin Med. (2021) 16:1188–91. doi: 10.3969/j.issn.1673-7202.2021.08.002
27. Gautam S, Jain A, Gautam M, Vahia VN, and Gautam A. Clinical practice guidelines for the management of generalised anxiety disorder (GAD) and panic disorder (PD). Indian J Psychiatry. (2017) 59:S67–73. doi: 10.4103/0019-5545.196975
28. Yu HM, Luo YH, and Sa J. Intraclass correlation coefficient and software procedures. Chin J Health Stat. (2011) 28:497–500. doi: CNKI:SUN:ZGWT.0.2011-05-007
29. Ng JY and Jain A. Complementary and alternative medicine mention and recommendations in guidelines for anxiety: A systematic review and quality assessment. Psychiatry Res. (2022) 309:114388. doi: 10.1016/j.psychres.2022.114388
30. World Health Organization. Comprehensive mental health action plan 2013–2030. Geneva, Switzerland: World Health Organization (2021). Available online at: https://iris.who.int/handle/10665/345301.
31. World Health Organization. World health statistics 2024: Monitoring health for the SDGs, Sustainable Development Goals. Geneva, Switzerland: World Health Organization (2024). Available online at: https://iris.who.int/handle/10665/376869.
32. Fernández A, Haro JM, Martinez-Alonso M, Demyttenaere K, Brugha TS, Autonell J, et al. Treatment adequacy for anxiety and depressive disorders in six European countries. Br J Psychiatry. (2007) 190:172–3. doi: 10.1192/bjp.bp.106.023507
33. Sullivan G, Craske MG, Sherbourne C, Edlund MJ, Rose RD, Golinelli D, et al. Design of the coordinated anxiety learning and management (CALM) study: Innovations in collaborative care for anxiety disorders. Gen Hosp Psychiatry. (2007) 29:379–87. doi: 10.1016/j.genhosppsych.2007.04.005
34. van Dijk MK, Oosterbaan DB, Verbraak MJPM, and van Balkom AJLM. The effectiveness of adhering to clinical-practice guidelines for anxiety disorders in secondary mental health care: The results of a cohort study in the Netherlands. J Eval Clin Pract. (2013) 19:791–7. doi: 10.1111/j.1365-2753.2012.01851.x
35. Taba P, Rosenthal M, Habicht J, Tarien H, Mathiesen M, Hill S, et al. Barriers and facilitators to the implementation of clinical practice guidelines: A cross-sectional survey among physicians in Estonia. BMC Health Serv Res. (2012) 12:455. doi: 10.1186/1472-6963-12-455
36. Qaseem A, Snow V, Owens DK, Shekelle P, and Clinical Guidelines Committee of the American College of Physicians. The development of clinical practice guidelines and guidance statements of the American College of Physicians: Summary of methods. Ann Intern Med. (2010) 153:194–9. doi: 10.7326/0003-4819-153-3-201008030-00010
37. Williams C, McClay CA, Martinez R, Morrison J, Haig C, Jones R, et al. Online CBT life skills programme for low mood and anxiety: Study protocol for a pilot randomized controlled trial. Trials. (2016) 17:220. doi: 10.1186/s13063-016-1336-y
38. Apolinário-Hagen J, Drüge M, and Fritsche L. Cognitive behavioral therapy, mindfulness-based cognitive therapy and acceptance commitment therapy for anxiety disorders: Integrating traditional with digital treatment approaches. Adv Exp Med Biol. (2020) 1191:291–329. doi: 10.1007/978-981-32-9705-0_17
39. Stefanopoulou E, Lewis D, Taylor M, Broscombe J, and Larkin J. Digitally delivered psychological interventions for anxiety disorders: A comprehensive review. Psychiatr Q. (2019) 90:197–215. doi: 10.1007/s11126-018-9620-5
40. Kerber A, Beintner I, Burchert S, and Knaevelsrud C. Effects of a self-guided transdiagnostic smartphone app on patient empowerment and mental health: Randomized controlled trial. JMIR Ment Health. (2023) 10:e45068. doi: 10.2196/45068
Keywords: anxiety disorder, guidelines, psychosocial intervention, systematic review, recommendations
Citation: Huang C, Liu X, Liu Y, Luo C, Cai J, Wang Y, Chen J, Shi Z and Jin X (2025) Psychosocial interventions for anxiety disorders in adults: evidence mapping and guideline appraisal. Front. Psychiatry 16:1677705. doi: 10.3389/fpsyt.2025.1677705
Received: 01 August 2025; Accepted: 01 October 2025;
Published: 20 October 2025.
Edited by:
Tamara Melnik, Federal University of São Paulo, BrazilReviewed by:
Aline Rocha, Federal University of São Paulo, BrazilThiago Sampaio, Instituto do Coração (InCor) – Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, Brazil
Copyright © 2025 Huang, Liu, Liu, Luo, Cai, Wang, Chen, Shi and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jue Chen, Y2hlbmp1ZTIwODhAMTYzLmNvbQ==; Zhongying Shi, c3NjLjFAMTYzLmNvbQ==; Xiaochao Jin, YW5ncnlhbGV4QHNpbmEuY29t
†These authors have contributed equally to this work
 Chuxian Huang
Chuxian Huang Xiao Liu
Xiao Liu Yue Liu1†
Yue Liu1† Chen Luo
Chen Luo Zhongying Shi
Zhongying Shi