- 1School of Social Work, Colorado State University, Fort Collins, CO, United States
- 2Kent School of Social Work and Family Science, University of Louisville, Louisville, KY, United States
- 3Graduate School of Social Work, University of Denver, Denver, CO, United States
- 4Clinical Sciences, College of Veterinary Medicine, Colorado State University, Fort Collins, CO, United States
- 5Department of Psychological & Brain Sciences, University of Louisville, Louisville, KY, United States
Background: Animal cruelty is a recognized correlate of interpersonal violence within family systems, yet children’s exposure to this form of harm remains absent from most standardized assessments of childhood adversity. Guided by the Dimensional Model of Adversity and Psychopathology, this study examined the co-occurrence of exposure to animal cruelty with other threat-related adverse childhood experiences (ACEs) and how these patterns relate to adult mental health.
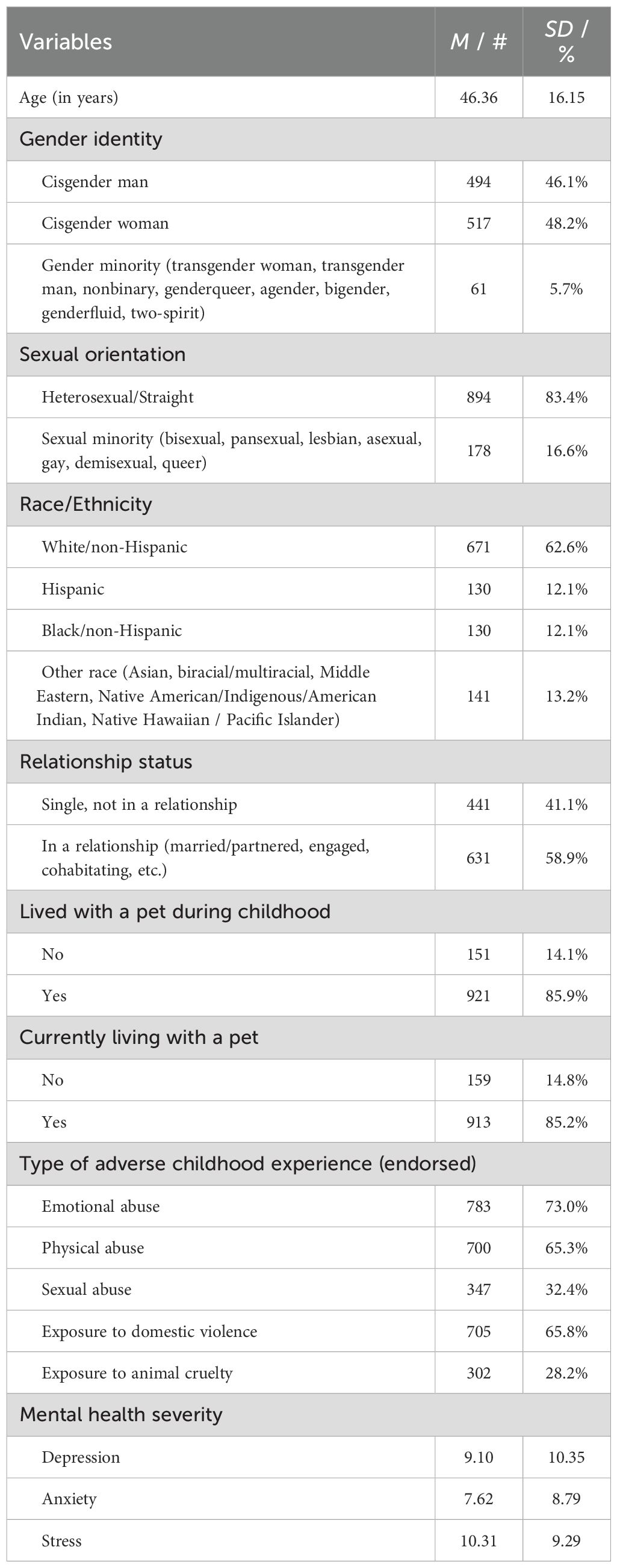
Methods: Our sample included 1,072 U.S. adults recruited online through Prolific, a licensed participant recruitment firm, using its representative U.S. sample option. Participants reported on childhood experiences of emotional abuse, physical abuse, sexual abuse, exposure to domestic violence, and exposure to animal cruelty, along with current symptoms of depression, anxiety, and stress. Latent class analysis identified subgroups based on adversity profiles. Associations between class membership and sociodemographic factors were examined, and differences in mental health outcomes across classes were estimated adjusting for these covariates.
Results: A three-class model best fit the data: low adversity (29.6%), interpersonal violence only (34.8%), and interpersonal violence and animal cruelty (35.6%). Membership in the latter was more likely among younger participants, those with a minoritized gender modality, those with a minoritized sexual orientation, and Hispanic or Black individuals compared to white participants. The class interpersonal violence and animal cruelty reported the highest depression, anxiety, and stress scores, followed by the interpersonal violence only group, with the low adversity group reporting the lowest scores (all ps <.001; moderate-to-large effects).
Conclusion: Future research should test whether including animal cruelty in person-centered models of adversity improves identification of high-risk subgroups, and explore how such inclusion can inform multispecies approaches to violence prevention and intervention.
1 Introduction
A growing body of research highlights the intersection of animal cruelty and interpersonal violence within family systems (1). Studies have documented that violence toward animals frequently co-occurs with child maltreatment (including emotional, physical, and sexual abuse), as well as children’s exposure to intimate partner violence (1–7). In the context of family violence, cruelty toward animals is not an isolated or random act of harm. Instead, it may be used intentionally as a tactic of coercive control or punishment, contributing to an atmosphere of fear and instability within the household (8–10). For example, in families experiencing intimate partner violence, 50–75% of women report that their partner has harmed or threatened to harm a pet as part of a broader pattern of intimidation, control, and emotional abuse (1).
Children living in such environments may directly witness the intentional harm of companion animals by caregivers or siblings, and witnessing these acts can have attendant psychological consequences (8–11). Exposure to animal cruelty, particularly when the child is emotionally bonded to the pet, has been linked to short and long-term mental health problems (6, 12–14). For instance, Girardi and Pozzulo (15) found that exposure to aggression toward pets in childhood was associated with elevated anxiety and depression symptoms in early adulthood, particularly among those who reported medium levels (compared to low levels) of bonding with their childhood pets. Similarly, Hawkins et al. (16) found that among children aged 7 to 12 years, exposure to animal cruelty amplified the effect of exposure to IPV on generalized internalizing symptoms as well as anxiety, depression, and posttraumatic stress symptoms. In addition to these psychological impacts, childhood exposure to animal cruelty, particularly when it occurs within the broader context of family violence, has been linked to an increased risk of later cruelty toward animals and other forms of antisocial behavior (17–19). These findings underscore the importance of recognizing animal cruelty exposure as both a form of adversity and a potential early marker of broader psychosocial risk.
Although exposure to animal cruelty may contribute to children’s psychological distress and long-term wellbeing (15, 20), it remains absent from most standardized assessments of childhood adversity. Thus, it is not included in widely used instruments such as the World Health Organization’s Adverse Childhood Experiences – International Questionnaire (20–22) or the original Adverse Childhood Experiences (ACE) questionnaire developed by the CDC (23). This exclusion limits opportunities to systematically detect these experiences and understand their intersection and co-occurrence with other forms of adversity. As a result, even though research has demonstrated that exposure to animal cruelty is often linked with other adverse childhood experiences and concomitant health outcomes, it continues to be overlooked in child welfare and population health research (1). Notably, the United Nations Committee on the Rights of the Child recently recognized in General Comment No. 26 (24) that children should be protected from witnessing violence toward animals, affirming the developmental risks posed by such exposure and underscoring the need for its inclusion in child rights and protection frameworks (24).
1.1 Exposure to animal harm as threat-based adversity
Recent theoretical developments in childhood adversity research underscore the importance of distinguishing among qualitatively different dimensions of early adversity. The Dimensional Model of Adversity and Psychopathology (25) proposes that distinct dimensions—such as threat (e.g., experiences involving harm or the threat of harm) and deprivation (e.g., absence of expected cognitive and social inputs)—confer risk for psychopathology through different neurodevelopmental mechanisms. Threat-based adversities, including physical and sexual abuse, emotional abuse, and exposure to interpersonal violence, have been linked to altered fear learning, heightened emotional reactivity, and dysregulation of biological stress systems (26–28). Although this model has largely been applied to interpersonal harm, exposure to animal cruelty, particularly when it involves closely bonded animals considered family members, may function similarly (6, 7, 16). Witnessing or learning about violence toward a companion animal can elicit anticipatory fear, helplessness, and relational distress, which are core features of threat-based experiences (6, 25).
From a developmental and biopsychosocial perspective, such experiences may disrupt multiple systems central to emotional regulation and relational security. Because childhood exposure to animal cruelty often occurs within broader contexts of family or community violence that normalize interpersonal harm and undermine safety, empathy, and moral agency, this exposure may further reinforce maladaptive fear learning and anticipatory threat responses (6, 7, 11, 13, 16, 29). Biologically, repeated exposure to animal cruelty and concomitant forms of violence may sensitize stress-response systems such as the hypothalamic–pituitary–adrenal (HPA) axis, contributing to chronic hyperarousal and maladaptive fear learning (25, 30–32). Psychologically, witnessing or losing a bonded companion animal due to harm could evoke traumatic grief and guilt, reinforce internalized helplessness, and impair attachment security (6, 7, 11, 13, 16, 33, 34). Collectively, these pathways illustrate how animal cruelty exposure may operate as a form of threat-based adversity that heightens vulnerability to internalizing distress, particularly when the harm involves a companion animal to which the child is bonded.
1.2 Profiles of childhood adversity
Research using person-centered approaches demonstrates that patterns of childhood adversity often cluster in distinct and meaningful ways (35–37). Latent class analysis (LCA), in particular, has been used to identify subgroups of individuals with shared adversity profiles (38). For example, in a community-based sample of young adults, Shin et al. (36) identified four latent classes of ACE exposure patterns (Low ACEs, Household Dysfunction/Community Violence, Emotional ACEs, and High/Multiple ACEs). Accounting for socioeconomic status and gender, they found that individuals in the High/Multiple ACEs class reported significantly higher levels of psychological difficulties. Similarly, in a nationally representative sample of U.S. older adults (37), Kim et al. (37) identified four distinct ACE profiles (Low Adversity, High Adversity, Child Abuse, and Parental Substance Use). Membership in the High Adversity and Child Abuse classes was associated with elevated risk for poor mental health outcomes in later life. These results, along with other studies, suggest that distinct adversity profiles are differentially associated with adult outcomes including depression, anxiety, posttraumatic stress symptoms, substance use, emotion regulation difficulties, and disrupted interpersonal functioning (36, 37, 39, 40).
Although variable-centered studies have demonstrated associations between exposure to animal cruelty and other forms of adversity, person-centered approaches have not yet considered animal cruelty within the broader classification of adverse childhood experiences. As a result, it remains unclear how exposure to this form of violence clusters with other types of adversity in childhood, what contextual factors are associated with its occurrence, and how it may relate to long-term psychological and relational outcomes. This omission is notable, particularly in light of recent evidence demonstrating that animal cruelty is not only prevalent in family violence contexts but may operate as a form of trauma with distinct psychological consequences (6, 7, 13, 16). Understanding these associations is especially important given the central role that companion animals often play in children’s emotional lives and the potential for these experiences to shape later wellbeing (41).
1.3 Current study
The present study applied a person-centered approach to examine how exposure to animal cruelty co-occurs with interpersonal threat-based adversity in childhood. Using LCA, we sought to identify distinct profiles of threat-related adversities that include both interpersonal abuse and animal cruelty. Perceived social support and other sociodemographic correlates were included as covariates, given extensive evidence that supportive relationships are associated with improved mental health following adversity and that demographic characteristics such as age, gender, sexual orientation, race and ethnicity are related to both adversity exposure and psychological outcomes (42–47). Guided by the dimensional model of adversity and psychopathology (25), we hypothesized that animal cruelty would cluster with other forms of interpersonal adversity, reflecting its role as a threat-related experience. We further hypothesized that classes characterized by high levels of both interpersonal abuse and animal cruelty would be associated with greater psychosocial difficulties in adulthood compared to low-adversity classes.
2 Methods
2.1 Participants and procedure
Data were collected from 1,147 U.S. adults aged 18 years or older who participated in the Pets, Attachment, and Mental Health Study, an online survey administered between 6/2/25 and 6/3/25. This study was designed to examine relationships among human–animal attachment, childhood experiences, and adult mental health across a demographically diverse sample of U.S. adults. Participants completed standardized measures of ACEs, pet-related experiences, attachment, and psychological functioning.
The national sample was recruited through Prolific, a licensed online participant recruitment firm that maintains panels of pre-screened participants. Prolific uses verified demographic screening and quota sampling to approximate U.S. census distributions on age, gender, and ethnicity, and its representative-sample option draws participants to match these targets. To ensure data quality, Prolific employs multiple verification procedures (e.g., IP and device fingerprinting, CAPTCHA checks, and periodic attention-screening) and removes accounts that fail quality audits or show fraudulent activity. Peer-reviewed comparisons have shown that Prolific responses demonstrate higher data quality and/or lower rates of inattentive or random responding than other online platforms such as Amazon Mechanical Turk or CrowdFlower (41).
Informed consent was obtained on the first page of the online survey. Participants were provided with information about the study and asked to indicate their willingness to participate before proceeding. The Prolific study description and consent form informed participants that the survey included questions about potentially sensitive or distressing experiences so they could make an informed decision about participation. Participants were paid, via the Prolific platform, $7.50 for completion of the survey and up to an additional $3.00 to complete the pet-related survey items. The present study utilized a subset of variables from the broader survey, which included multiple constructs related to human–animal interaction, early-life experiences, and wellbeing. To minimize priming and social-desirability bias, participants were informed that the survey focused on “childhood and adult experiences, including relationships with pets,” rather than specifically on ACEs or trauma outcomes. Items assessing childhood experiences were embedded among other measures of attachment and wellbeing. All surveys were administered in English. This research was approved by the Institutional Review Board at Colorado State University.
2.2 Measures
2.2.1 Adverse childhood experiences
ACEs were assessed using items from the World Health Organization’s ACE-International Questionnaire (21). Eleven items assessed four categories of adversity experienced before the age of 18: 1) Emotional abuse (e.g., being yelled at, insulted, or threatened with abandonment), 2) Physical abuse (e.g., being slapped, kicked, or hit with an object), 3) Sexual abuse (e.g., unwanted sexual touching or intercourse), and 4) Exposure to domestic violence (e.g., witnessing yelling or physical assault between household members). Participants indicated the frequency of exposure to each of the 11 items on a five-point scale ranging from never to always. For the current study, each item was dichotomized to indicate whether the participant was exposed (=1, rarely, sometimes, most of the time, always) or not exposed (=0, never). If any of the dichotomous items corresponding to the four types of ACEs were endorsed, then that exposure was also represented in the four types of ACEs (1=exposed), whereas if all items for the corresponding type of ACE never occurred, the score would be 0 (see Table 1).
2.2.2 Childhood exposure to animal cruelty
Two additional items assessing forms of childhood exposure to animal cruelty (i.e., Did you see or hear a parent, guardian, or other adult household member hurt a pet on purpose? Did you see or hear a sibling or another child in your household hurt a pet on purpose)? were added for the purposes of this study and are not part of the original ACE-IQ. These items were adapted from the Pet Treatment Survey (48). Each item was rated on a five-point Likert scale from Never to Always. To align with the scoring of the four types of ACEs, items were dichotomized to reflect whether participants had ever been exposed to either form of animal cruelty (0 = Never, 1 = Ever).
2.2.3 Depression, anxiety, and stress
We assessed depression, anxiety, and stress using the Depression, Anxiety, and Stress Scale–21 (DASS-21 (49, 50);. Each of the DASS-21 subscales included 7 items that indicate the frequency of symptoms as experienced over the past week. The items were scored on a four-point scale ranging from “never” to “almost always.” We calculated subscale scores for depression, anxiety, and stress by summing the item scores and then multiplying them by two for each subscale. This allows for subscale scores to be compared to established cut-off scores indicating the severity of symptoms. Conventional scoring of the DASS-21 indicates that depression, anxiety, and stress scores are considered to be within a normal severity range if they fall between 0-9, 0-7, and 0-14, respectively. Mild scores range from 10-13, 8-9, and 15-18; moderate scores range from 14-20, 10-14, and 19-25; severe scores range from 21-27, 15-19, and 26-33; and extremely severe scores are greater than or equal to 28, 20, and 34, respectively (49). Internal consistency in the current study was good for depression (ω = 0.96), anxiety (ω = 0.94), and stress (ω = 0.94).
2.2.4 Covariates
2.2.4.1 Social support
Perceived social support was assessed using the Multidimensional Scale of Perceived Social Support (51). The MSPSS includes 12 items about whether the participant perceives available support from significant others, family, and friends. Items are ranked on a seven-point scale ranging from “very strongly disagree” to “very strongly agree.” We used the total perceived social support score, which is the mean of responses to all 12 items in this study. Internal consistency of the MSPSS total score was good (ω=0.95).
2.2.4.2 Sociodemographic correlates
Age (continuous), gender modality, sexual orientation, race, ethnicity, relationship status, perceived social support (continuous), childhood pet ownership and current pet ownership were included as sociodemographic covariates. Based on theoretical conceptualizations, we examined whether covariates were associated with latent class membership and with differences in stress, anxiety, and/or depression scores. Gender modality was dummy-coded into three groups: cisgender man, cisgender woman, and gender minority, with cisgender man as the reference group. Sexual orientation was dummy-coded into heterosexual and sexual minority with heterosexual as the reference group. Race and ethnicity were recoded into four dummy variables to address small cell sizes and ensure sufficient statistical power: white/non-Hispanic, Hispanic, Black/non-Hispanic, and another race group (including those who selected Asian, biracial/multiracial, Middle Eastern, Native American/Indigenous/American Indian, or Native Hawaiian/Pacific Islander; see the Discussion section for a review of the limitations of this approach). White/non-Hispanic was used as the reference group. Relationship status, lived with a pet during childhood, and currently living with a pet were dichotomized to indicate whether participants were single/not in a relationship (=0, reference group) or in a relationship (=1, married, partnered, engaged, cohabitating, etc.), did (=1) or did not live with a pet in childhood (=0, reference group), and currently did (=1) or did not live with a pet (=0, reference group).
2.3 Analytic strategy
Data cleaning and assumption checks were conducted in SPSS version 30. All other analyses were conducted in Mplus version 8.10. Checks for multicollinearity for the dependent variables were satisfied, as all VIF values were < 10 and conditional index values were < 15. Missing data was minimal (less than 1%) and handled using full information maximum likelihood (FIML) estimation. To avoid having different sample sizes for the LCA and the regression analyses, we conducted analyses with an analytic sample of 1,072 participants. This removed participants who were missing on all of the ACE indicators (n = 11, <1% missing) and participants who were missing on any predictor (n = 75), which would result in them being excluded from the LCA and/or regression analyses, respectively. Participants who were missing on DASS (n = 11) were the same participants missing on all ACE indicators. Most of the missing data was due to missing on any predictor. Examining missingness on each of the predictors separately, 30 participants were missing on race/ethnicity, 21 were missing on current pet ownership, 21 were missing on childhood pet ownership, 20 were missing on gender identity, 17 were missing on sexual orientation, 16 were missing on relationship status, four participants were missing on age, and one was missing on perceived social support. Missingness on these variables was negligible (<3%). We examined descriptive statistics for the ACEs indicators, covariates, additional sociodemographic variables, and DASS-21 subscales. Bivariate correlations were tested for the DASS-21 subscales.
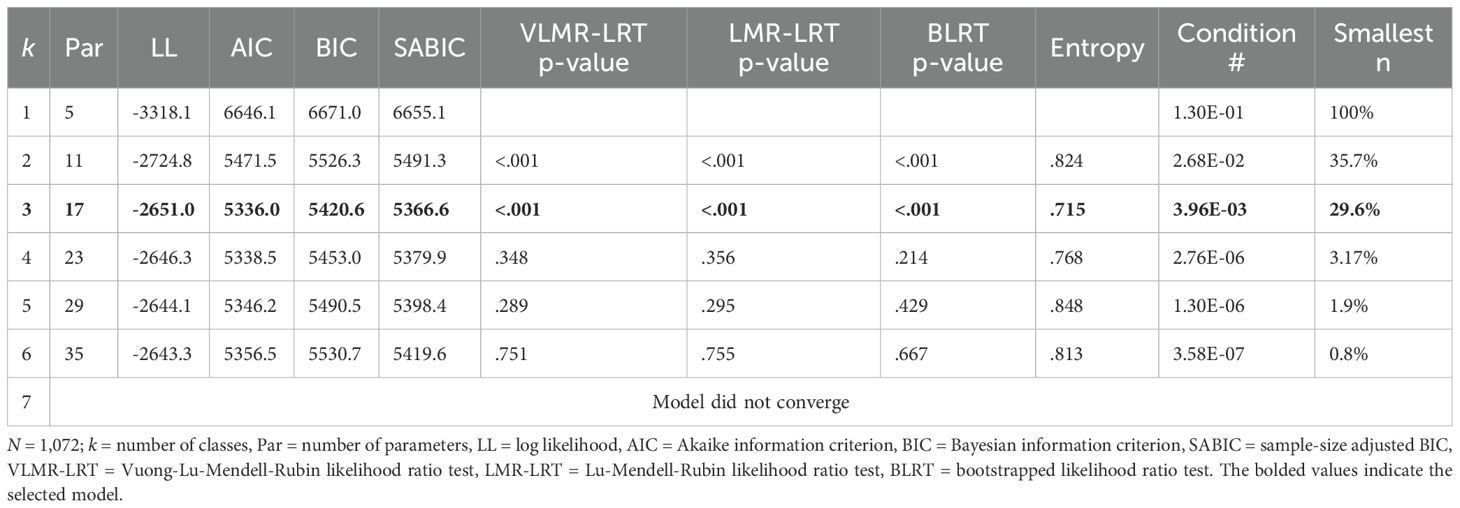
We conducted latent class analysis to identify unobserved subgroups based on participants’ adversity profiles (52). Models with one to six classes were estimated. We evaluated model fit using standard criteria, including the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), sample-size adjusted BIC (SABIC), likelihood ratio tests (Lo–Mendell–Rubin (LMR) LRT, Vuong–Lo–Mendell–Rubin (VLMR) LRT), and bootstrap LRT (BLRT). Lower values on the AIC, BIC, and SABIC indicate better model fit. The LRTs test whether the additional model complexity of a k + 1 class is a significant improvement in model fit compared to a k class model, with a significant p-value indicating significant improvement in fit and the k + 1 class should be retained. Additional considerations included entropy, average posterior probabilities (AvePP), minimum class size, and interpretability of the resulting profiles. Entropy greater than 0.80 is an indication of “good” classification of individuals into latent classes and AvePP greater than 0.70 is indicative of good class separation (53, 54). We compared potential candidate models (e.g., three-, four-, and five-class solutions) using the item probabilities, class sizes, and interpretability of the subgroups.
Next, to examine subgroup differences in covariates, depression, anxiety, and stress, we used the Bolck-Croon-Hagenaars (BCH) approach (55). This approach is recommended as it allows for the examination of covariates and distal outcomes in the same model while preventing the latent classes from shifting while accounting for individual classification error. The first step of the BCH approach creates BCH weights that account for classification error into subgroups. The final step of the BCH approach allows for the testing of covariates and distal outcomes. To test for subgroup differences based on covariates, we regressed the latent class variable on the covariates (age, gender modality, sexual orientation, race/ethnicity, and living with a pet during childhood) and used Wald tests to determine the significance of each association, separately. Finally, we used Wald tests to evaluate whether there were significant mean differences in depression, anxiety, and stress across subgroups, adjusting for covariates (age, gender modality, sexual orientation, currently living with a pet, relationship status, social support, and race/ethnicity). We explored more specific pair-wise differences using the model constraint function in Mplus.
3 Results
3.1 Univariate and bivariate statistics
The most frequently endorsed type of ACE was emotional abuse (73.0%), followed by exposure to domestic violence (65.8%) and physical abuse (65.3%). Less frequently endorsed were sexual abuse (32.4%) and exposure to animal cruelty (28.2%). The dependent variables, depression, anxiety, and stress, were all positively correlated. Depression was moderately to strongly associated with anxiety (r = 0.72, p <.001) and stress (r = 0.78, p <.001), and anxiety was strongly associated with stress (r = 0.81, p <.001). Although the average score for stress was within the normal range (M = 10.31, SD = 9.29), the scores of depression (M = 9.10, SD = 10.35) and anxiety (M = 7.62, SD = 8.79) indicated that the average scores in this sample were mild in severity.
3.2 Latent class enumeration
The LCA produced models with one to six latent classes. The fit statistics across these models suggested that the three-class model fit our data best (see Table 2). The AIC, BIC, and SABIC were all lowest in the three-class model. The LRTs also provide support for this model, as the three-class model was a significant improvement in fit compared to the two-class model, but the added complexity of the four-class model did not significantly improve fit above and beyond the three-class model. Although less than ideal, the entropy of the three-class model was adequate (entropy = 0.72). Further, the average posterior probabilities ranged from 0.71 to 0.91, which indicate that there is adequate separation between classes and precision.
We used the probability of endorsing each of the five types of ACEs to label the three subgroups (see Figure 1). The first subgroup contained 29.6% of the sample and was characterized by low probability (< 0.30) of endorsing all five types of adversity. Therefore, we labeled this subgroup the low adversity subgroup. The second subgroup was labeled the interpersonal violence only subgroup (34.8%) as it was characterized by high probability (> 0.70) of endorsing emotional abuse, physical abuse, and exposure to domestic violence and low probability of endorsing sexual abuse and exposure to animal cruelty. The last subgroup (35.6%) was labeled interpersonal violence and animal cruelty as this group had high probability of endorsing all of the following: emotional abuse, physical abuse, sexual abuse, exposure to domestic violence, and exposure to animal cruelty. We included sexual abuse endorsement as the probability in this subgroup was 0.69, which we considered close enough to the cut-off to be characteristic exposure.
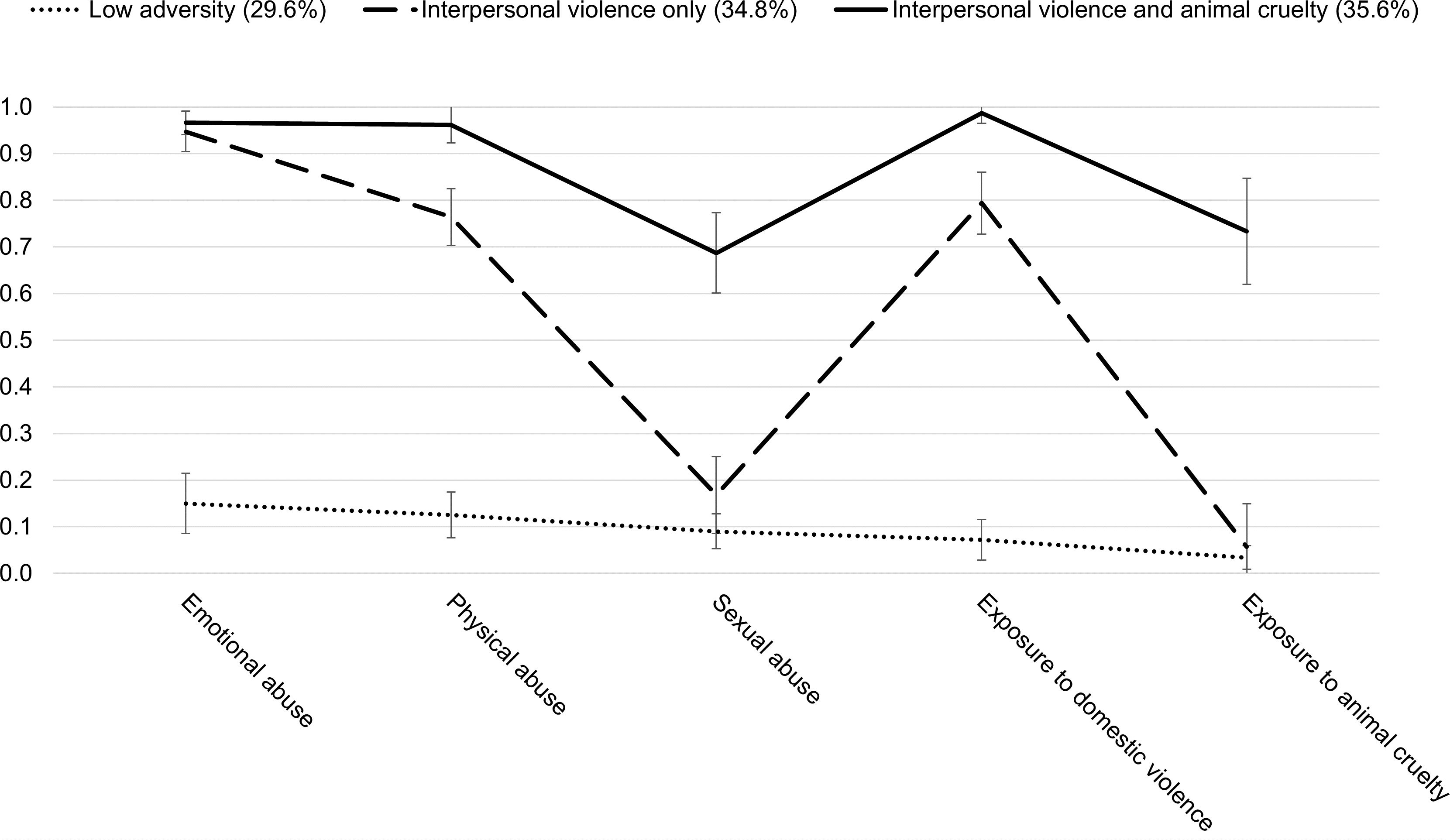
Figure 1. Item probability plot for the 3-class model (N = 1,072). The error bars represent 95% confidence intervals.
3.3 Sensitivity analysis
Although not included in the current study, we also conducted a sensitivity analysis of the latent class enumeration process using the ordinal frequency response scales (never, rarely/sometimes, most of the time/always). These results did not provide clear defining patterns of frequency of ACE exposures, and thus models using the ordinal response scale were not carried forward. We provide further detail in the Supplementary Materials.
3.4 Differences in subgroup membership by sociodemographic characteristics
Our comparisons of posterior class probabilities indicated significant differences in subgroup membership based on age, gender modality, sexual orientation, and race/ethnicity (see Table 3). However, living with a pet during childhood was not significantly associated with subgroup membership, x2(2) = 3.47, p = .177. Age was significantly associated with subgroup membership, x2(2) = 8.00, p = .018. Specifically, compared to membership in the low adversity subgroup, as age increased, the likelihood of being in the interpersonal violence and animal cruelty subgroup decreased (OR = 0.98, 95% CI: 0.97, 0.99). There was no significant association between membership in the interpersonal violence only subgroup compared with the low adversity subgroup based on age.
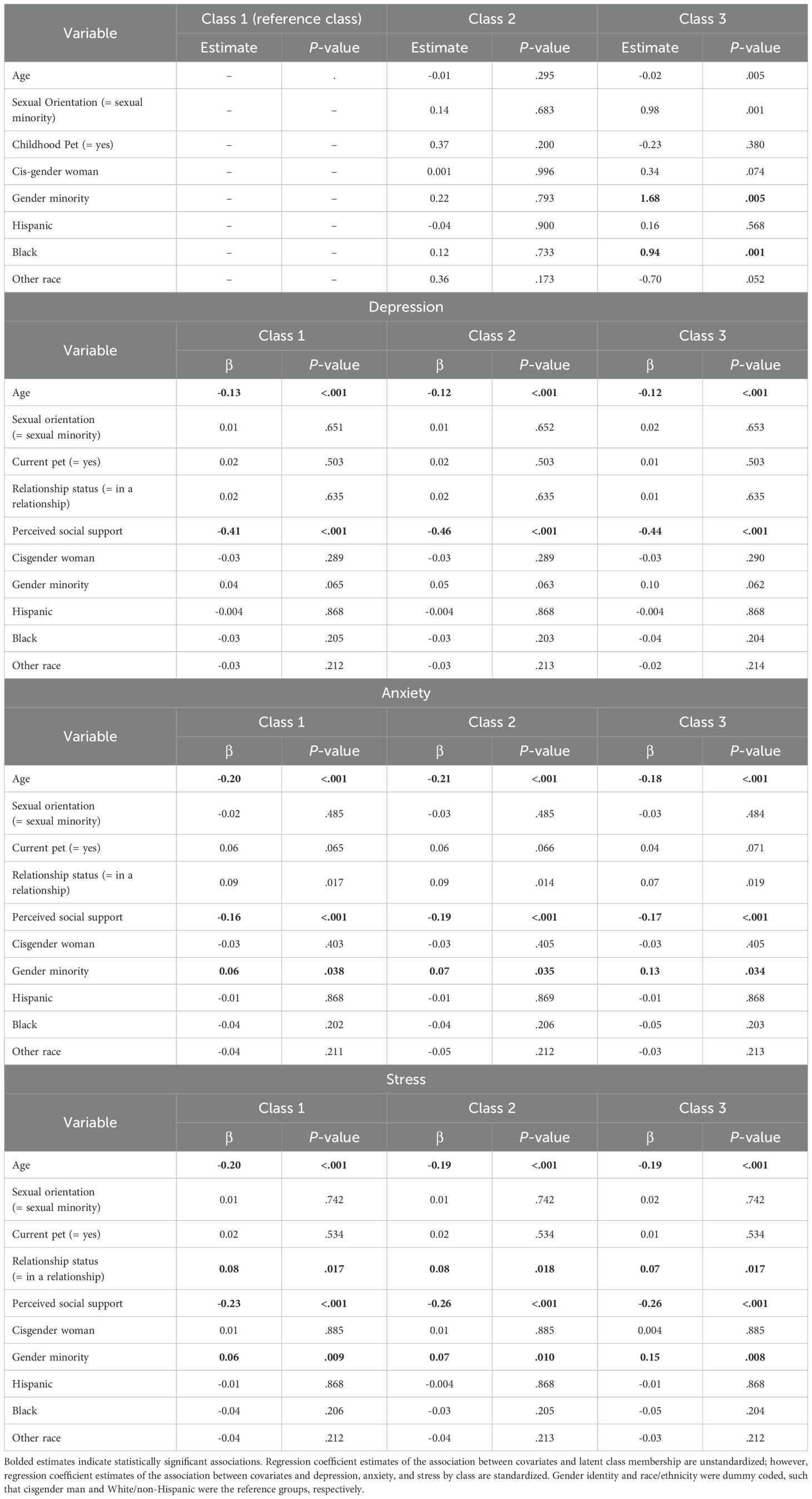
Table 3. Associations between covariates and latent classes and between covariates and stress, anxiety, and depression by latent class membership.
There were significant differences in subgroup membership based on gender modality, x2(4) = 12.81, p = .012. Cisgender men and cisgender women had higher odds of being in the low adversity subgroup (OR = 3.28, p <.001 and OR = 2.73, p = .001, respectively) and the interpersonal violence only subgroup (OR = 2.45 and 2.06, ps <.001, respectively) compared to those with a minoritized gender modality. In contrast, individuals with a minoritized gender modality were more likely to be in the interpersonal violence and animal cruelty subgroup compared to cisgender men (OR = 4.79, p <.001) and cisgender women (OR = 3.40, p <.001).
We also found significant differences in subgroup membership based on sexual orientation, x2(2) = 14.45, p = .001. Individuals with a minoritized sexual orientation had higher odds of being in the interpersonal violence and animal cruelty subgroup, relative to heterosexual individuals (OR = 2.50, p <.001). In contrast, the odds of being in the interpersonal violence only (OR = 0.64, p = .001) and low adversity subgroups (OR = 0.53, p <.001) were lower for individuals who held minoritized sexual identities in comparison to heterosexual individuals.
There were also significant differences in subgroup membership based on race/ethnicity, x2(6) = 22.11, p = .001. Relative to white individuals, Hispanic and Black individuals had lower odds of being in the low adversity subgroup (OR = 0.94, p = .001 and OR = 0.54, p = .002, respectively) and the interpersonal violence only subgroup (OR = 0.89, p = .007 and OR = 0.65, p = .012, respectively). Individuals in the other racial/ethnic identity group had higher odds of being in the low adversity subgroup (OR = 1.03, p = .001) and the interpersonal violence only subgroup (OR = 1.88, p = .004) compared to white individuals. The pattern reversed for the interpersonal violence and animal cruelty subgroup. Hispanic (OR = 1.19, p = .003) and Black individuals (OR = 2.42, p = .002) had higher odds of being in this subgroup compared to white individuals. Those with another racial/ethnic identity had lower odds of being in this subgroup compared to white individuals (OR = 0.42, p = .015).
3.5 Associations between covariates and depression, anxiety, and stress
Across classes, age was negatively associated with depression (βs range: -0.12 to -0.13, ps <.001), anxiety (βs range: -0.18 to -0.21, ps <.001), and stress (βs range: -0.19 to -0.20, ps <.001). Similarly, social support was negatively associated with depression (βs range: -0.41 to -0.46, ps <.001), anxiety (βs range: -0.16 to -0.19, ps <.001), and stress (βs range: -0.23 to -0.26, ps <.001) across all classes. On average, individuals who were in a relationship reported higher stress (βs range: 0.07 to 0.08, ps <.05) and anxiety (βs range: 0.07 to 0.09, ps <.05) across classes compared to those who were single. Those with a minoritized gender modality had higher anxiety across classes (βs range: 0.06 to 0.13, ps <.05) and higher stress across classes (βs range: 0.06 to 0.15, ps <.05) compared to cisgender men. No other associations between predictors and outcome variables were significant (see Table 3).
3.6 Differences in depression, anxiety, and stress across classes
There were significant differences in mean scores for depression, anxiety, and stress across classes. Figure 2 displays the standardized means of depression, anxiety, and stress. There were significant differences across classes in depression scores, x2(2) = 75.43, p <.001. The low adversity and the interpersonal violence only classes reported lower depression scores than those in the interpersonal and animal cruelty class (d = 0.73 and d = 0.61, ps <.001, respectively). There was no significant difference in depression scores between the low adversity and the interpersonal violence only classes (d = 0.12, p = .075).
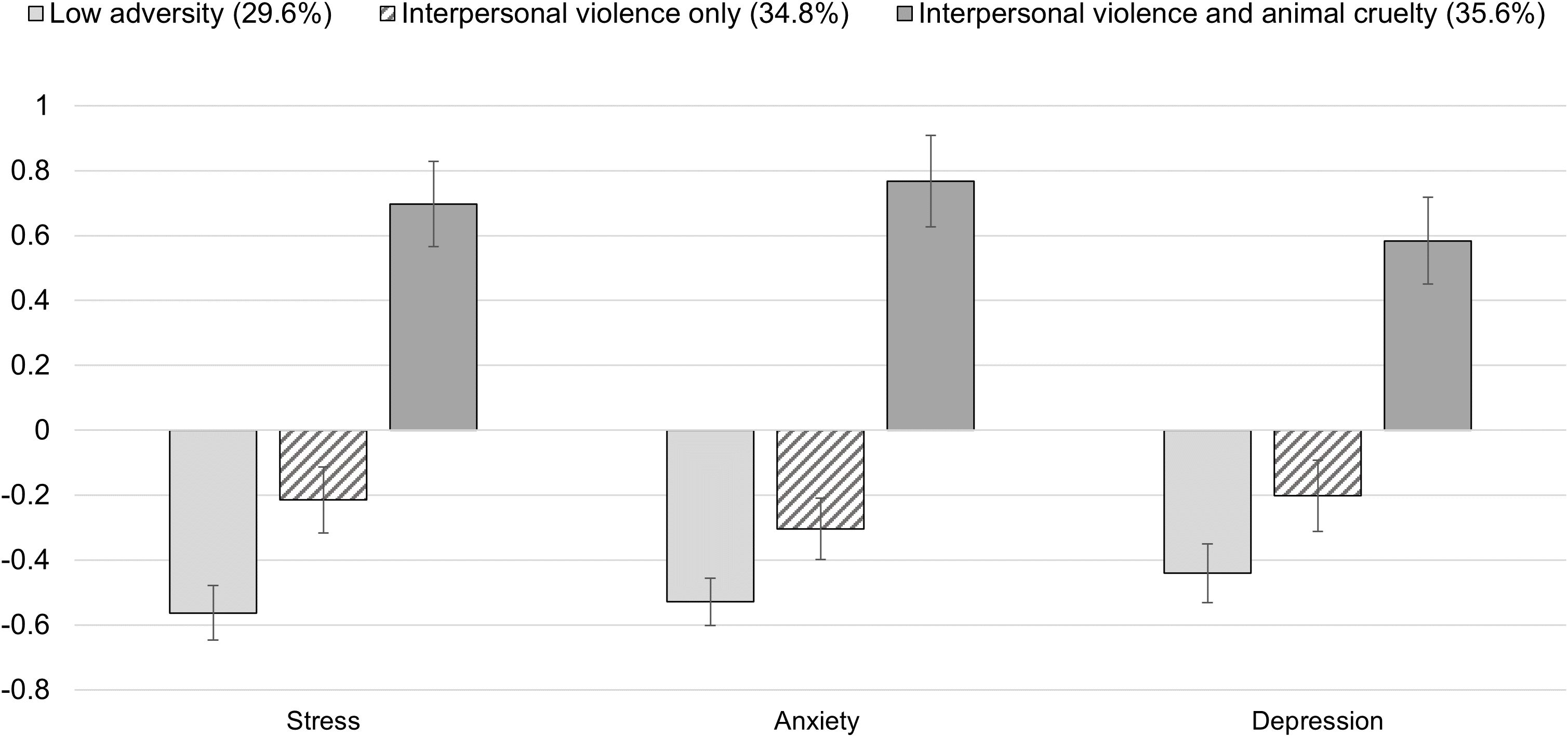
Figure 2. Mean Scores of Depression, Anxiety, and Stress Across Subgroups (N = 1,072). Y-axis values represent standard deviations from the sample mean. Error bars represent 95% confidence intervals.
All classes differed significantly from each other in their anxiety scores, x2(2) = 162.95, p <.001. The low adversity class had lower anxiety scores compared with the interpersonal only (d = 0.19, p = .003) and the interpersonal violence and animal cruelty classes (d = 1.13, p <.001). The interpersonal violence and animal cruelty class reported higher anxiety scores than the interpersonal violence only class (d = 0.95, p <.001).
Lastly, classes differed in their stress scores, x2(2) = 150.82, p <.001. All classes differed significantly from one another in the anticipated directions. The low adversity class had lower stress scores than the interpersonal violence only (d = 0.28, p <.001) and the interpersonal violence and animal cruelty classes (d = 1.03, p <.001). The interpersonal violence and animal cruelty class also reported higher stress scores than the interpersonal violence only class (d = 0.75, p <.001).
4 Discussion
This study extends the ACEs literature by integrating childhood exposure to animal cruelty into a person-centered analysis of threat-based adversities. Using LCA, we identified three distinct classes: low adversity, interpersonal violence only, and interpersonal violence with animal cruelty. The emergence of a class characterized by high co-occurrence of human- and animal-directed violence underscores the importance of applying a multispecies lens to the study of childhood adversity and developmental risk, particularly given prior research suggesting that exposure to animal cruelty is associated with compromised socioemotional functioning among children and adults (7, 16, 56, 57). Furthermore, our findings correspond to the threat dimension within the Dimensional Model of Childhood Adversity which frames experiences involving harm or threat of harm as conferring risk for psychopathology through mechanisms such as increased emotional reactivity and dysregulation of stress-response systems (25).
In our sample, 28.2% of participants reported childhood exposure to animal cruelty. This aligns with the lower range of prevalence estimates from U.S. samples where children are affected by intimate partner violence, in which studies have reported that 25–57% of children witness threats or harm to companion animals (1, 2, 6, 58). In contrast, general population and college samples show markedly lower rates. For example, Carlisle-Frank et al. (59) found that only 4% of college students recalled witnessing harm to a pet, and similar single-digit rates have been documented among broader community samples (8, 17, 60). Our findings suggest that animal cruelty exposure, while not ubiquitous, is elevated in settings of complex family violence and that prevalence may vary across population subgroups, such as those defined by demographic factors like age.
Notably, our rates for other adversities—emotional abuse (73%), physical abuse (65%), sexual abuse (32%), and witnessing domestic violence (66%)—are substantially higher than those observed in general U.S. adult populations. These elevated rates likely reflect differences in item wording and sampling approach. Compared to single-item ACE measures used in surveillance studies, our multi-item indicators may have lowered the threshold for endorsement, while online, self-selected participation through Prolific could increase willingness to disclose sensitive experiences. Data from CDC’s Behavioral Risk Factor Surveillance System indicate much lower prevalence, with estimates around 34-35% for emotional abuse, 16–23% for physical abuse, 11-13% for sexual abuse, and 15-17% for witnessing domestic violence (47, 61, 62). Other large-scale studies, such as Felitti et al. (23) and Ports et al. (63), similarly report lower base rates (63, 64). In our study, emotional abuse included an item for being “yelled, screamed, or sworn at,” which may have resulted in more endorsements than the ACE study item “swear at, insult, or put you down.” Similarly, physical abuse included an item for having been “spanked, slapped, kicked, punched, or beat up,” whereas the ACE study item includes “hit, beat, kick, or physically hurt you.” The inclusion of spanking as an indicator of physical abuse may have also lowered the threshold for this type of adversity, as rates of spanking in the U.S. are as high as 49% (65).
Discrepancy in measurement and differences in samples have been shown to result in disparate rates of reporting of emotional abuse. [e.g., 6.9% vs. 83% (66)]. High rates of emotional, physical, and sexual abuse and exposure to domestic violence similar to ours have been found among low-income mothers (60%, 42.4%, 43.5%, 46.4%, respectively (67)). There is also evidence that rates of ACEs have increased over the course of 14 years [2009-2022 (68)], which may indicate a trend in greater recognition of ACEs and of certain parenting behaviors (e.g., spanking) as harmful; this may help to explain why our rates are higher than previous studies. Further, our study relied on a binary assessment of exposure to ACEs (i.e., exposed vs. not exposed), which may over-estimate exposure. For example, in the current sample, emotional abuse and physical abuse endorsement are closer to 50% if those who experienced these rarely are not considered exposed. Future studies should take into consideration the frequency of exposure to ACEs and the thresholds of adversity that increase risk for negative mental and physical health outcomes. This study should also be replicated to examine the co-occurrence of animal cruelty with other forms of childhood adversity in samples with potentially different prevalence rates.
The elevated mental health symptoms observed in the interpersonal violence and animal cruelty class are consistent with prior variable-centered studies showing that animal cruelty exposure amplifies the effects of other forms of family violence on psychological distress (15, 16). These findings also align with the Dimensional Model of Adversity and Psychopathology (25), which posits that threat-based adversities (experiences involving harm or the threat of harm) are associated with heightened emotional reactivity, dysregulated stress physiology, and altered fear learning; all processes that may contribute directly to the elevated risk for anxiety, depression, and stress observed in this sample (25, 30–32). Witnessing harm to an animal, particularly one with whom a child has an emotional bond, represents a distinct adversity that can elicit fear, helplessness, grief, and disruption of attachment relationships, while also potentially compounding the psychological impact of other forms of violence or maltreatment. Beyond internalizing difficulties, witnessing or experiencing animal cruelty in childhood has also been linked to externalizing outcomes. Prior work indicates that such exposure is associated with cruelty perpetration, broader antisocial behavior, and later justice-system contact (69); future longitudinal research should test whether ACE profiles that include animal cruelty predict these outcomes above and beyond classes characterized by interpersonal forms of violence alone.
The sociodemographic differences in latent class membership, including the overrepresentation of individuals with minoritized gender identities, sexual orientations, and certain racial/ethnic backgrounds in the interpersonal violence and animal cruelty subgroup, parallel prior evidence that marginalized populations face disproportionate exposure to violence (70–72) and systemic barriers to safety and care (73, 74). Although individuals in the “other” racial/ethnic identity group had higher probabilities of being in the low adversity and interpersonal violence only subgroups, interpretation is limited by the heterogeneity of this category. Prior research has documented that some groups, such as Native American individuals, tend to experience higher rates of adversity, whereas others, such as Asian individuals, often report lower rates (75). Grouping these identities together may have obscured meaningful differences in the findings. Future studies should aim to explore these identities separately and with an intersectional lens (e.g., the intersection of race and gender) in order to better ascertain racial/ethnic variation in patterns of ACEs exposure. Although we found that animal cruelty often co-occurred with other forms of violence (76–82), prior research suggests this overlap reflects broader structural risks (e.g., poverty, racism, cumulative adversity) that differentially burden marginalized communities (83–87). This is further corroborated by a study by Reese et al. (85) that found that race, gender, and age were not associated with animal cruelty. Rather, they found that neighborhood conditions in terms of economic stress, vacancy and blight, and crime appear to be most strongly associated with animal cruelty in urban Detroit. Recognizing these patterns underscores the need to interpret the co-occurrence of human- and animal-directed harm in light of social and structural inequities, rather than attributing it to inherent features of individuals or groups.
4.1 Implications
From a clinical perspective, these findings emphasize the importance of integrating animal welfare considerations into trauma-informed assessment and intervention. The identification of three distinct adversity classes, and particularly the elevated depression, anxiety, and stress symptoms in the interpersonal violence and animal cruelty class, suggests that animal cruelty can signal severe, multifaceted trauma. Clinicians should anticipate complex presentations involving disruptions in trust and attachment, heightened physiological arousal, and grief or guilt tied to harm of companion animals (33). Comprehensive screening protocols should explicitly include questions about animal-directed harm, particularly in contexts where pets are present, to improve detection of complex household violence. Treatment approaches combining evidence-based trauma therapies such as Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) and Eye Movement Desensitization and Reprocessing (EMDR) with interventions addressing grief, guilt, and relational disruptions related to pet loss or harm are recommended (84, 88).
We also recognize ongoing debate regarding the potential harms and unintended consequences of routine ACEs screening. Scholars have cautioned that universal or poorly contextualized screening may lead to stigma, retraumatization, or inadequate follow-up care if it is not paired with appropriate support (89–91). Accordingly, our recommendations align with calls for targeted, trauma-informed assessment rather than broad population-level screening. Within this context, questions about pets and their wellbeing may provide a more relationally sensitive means of understanding family dynamics and safety (6). Pets often function as emotional and relational agents within families, and discussing their wellbeing can surface information about caregiving, attachment, and household stress that individuals may be hesitant to disclose through more direct questioning. Qualitative studies show that children experiencing domestic violence frequently describe pets as sources of comfort or emotional security amid household conflict, and that harm or threats toward animals can reveal underlying coercion or relational distress (6, 8, 92). Integrating pet-related inquiry within trauma-informed frameworks—paired with clear referral pathways and ethical safeguards—may therefore offer clinicians a compassionate, non-confrontational approach to exploring complex family processes. Further research should examine this approach empirically to determine its validity, feasibility, and boundaries, and how it can be embedded within broader cross-sector efforts to identify and respond to multispecies forms of household violence.
At the systems level, cross-sector collaboration between child welfare, domestic violence services, and animal protection organizations can strengthen early detection and coordinated responses (93). Implementation planning should establish feasible cross-reporting pathways, safeguard data-sharing, and provide workforce training that equips professionals across sectors (including veterinary and animal-services staff) to recognize and respond to suspected maltreatment. At the same time, safeguards are essential to avoid disproportionate surveillance of marginalized families, who are already more likely to experience system involvement and punitive responses (94, 95). Clear guidelines, accountability measures, and meaningful community input can help ensure that cross-reporting enhances safety without reinforcing or exacerbating existing inequities (95). These safeguards are particularly important given sociodemographic differences in class membership, which highlight the need for culturally responsive practices. The overrepresentation of individuals with minoritized gender identities, sexual orientations, and racial/ethnic backgrounds in the interpersonal violence and animal cruelty class underscores how systemic discrimination and structural inequities compound exposure to complex household violence (95, 96). To address these inequities, clinicians and service providers should approach assessment with cultural humility, awareness of barriers to safety and care, and readiness to respond to the cumulative impact of interpersonal and systemic trauma. Community-based outreach, training in cultural competence, and co-designed screening protocols can enhance trust, mitigate unintended harms, and increase relevance for the populations most affected (97).
At the prevention and policy levels, education about the co-occurrence of human- and animal-directed violence, stigma reduction around disclosure, and multisector service coordination remain essential (93, 98). A tiered intervention framework that combines universal education with targeted services for higher-risk subgroups may be especially effective. Future research should examine whether safety planning that explicitly includes animal companions and acknowledges multispecies family systems improves engagement and outcomes. Finally, while advocacy groups often highlight “the Link” between animal cruelty and interpersonal violence in broad terms, our findings point to the need for more nuanced, evidence-based communication. In this sample, animal cruelty co-occurred with other adversities only in the highest-risk subgroup, suggesting that its predictive value is context-dependent. Prevention messaging should therefore emphasize the conditions under which animal cruelty is most strongly associated with other forms of violence, rather than overgeneralizing across contexts (34, 93).
Another implication concerns ongoing debates in the ACEs literature regarding construct proliferation (i.e., the ever-expanding list of indicators now included under the ACE umbrella) and the conflation of exposure with symptomatology, which can blur conceptual boundaries and inflate associations with later outcomes (99–101). Some scholars argue that continual ACE expansion risks diluting the construct’s theoretical coherence and utility for prevention and policy, while others emphasize the importance of incorporating contextually and developmentally salient forms of adversity that have been historically overlooked. Our analytic approach addresses these concerns by restricting LCA indicators to threat-based exposure events and modeling psychopathology (depression, anxiety, and stress) as distal outcomes, maintaining a conceptual separation between adversity and sequelae. Including animal-cruelty exposure thus represents a theory-driven refinement—situating it within the threat dimension of the Dimensional Model of Adversity and Psychopathology rather than as an unbounded expansion of ACEs. We also recommend that future research test model sensitivity to indicator inclusion, avoid undifferentiated ACE “sum scores,” and continue advancing mechanism-focused frameworks that distinguish adversity exposures from their psychological and biological outcomes.
4.2 Limitations and future directions
Several limitations warrant consideration. One limitation is that ACEs were assessed using a subset of WHO ACE-IQ items limited to interpersonal violence, supplemented with two animal cruelty items developed for this study. Although this approach aligned with our focus on threat-based adversities, it excluded other important domains, such as neglect and household dysfunction, limiting our ability to capture the full spectrum of adversity. Another limitation is that all data were retrospective and self-reported, which may introduce recall bias and misclassification. Additionally, the cross-sectional design precludes conclusions about temporal ordering or causal relationships between adversity class membership and mental health outcomes.
Although the sample was nationally recruited through Prolific, a paid online research platform that approximates U.S. census distributions on key demographics, several features of the sample may limit generalizability. Most participants reported current (85%) or past (86%) experience with companion animals, which may reduce representativeness for individuals without such experiences. The sample was also predominantly white, cisgender, and heterosexual, potentially constraining generalizability and limiting representation of populations disproportionately affected by adversity, including racially minoritized and LGBTQ+ groups (102–104). These intersecting identities can shape both exposure to adverse experiences and access to supportive relationships—including with animals—through structural inequities such as discrimination, housing insecurity, or barriers to pet ownership. Future research should aim to recruit more diverse samples and explore whether the protective or mediating roles of human–animal relationships differ across cultural contexts and systems of marginalization. As previously discussed, participants who self-select into compensated online studies may also differ from the general population in their comfort disclosing sensitive experiences, and those with strong connections to animals may have been especially motivated to participate, potentially resulting in overrepresentation of pet owners.
A further consideration is that our analytic approach grouped racial and ethnic identities into broad categories due to sample size considerations. While this was necessary for statistical power, it may obscure important differences in adversity exposure and mental health outcomes across more specific racial and ethnic subgroups. Prior research demonstrates meaningful heterogeneity in ACE prevalence and sequelae across diverse populations (47, 105). Future studies should prioritize sufficient representation to allow for disaggregated analyses that more accurately capture the experiences of historically marginalized communities and contains sufficient power for exploring intersecting identities.
Another limitation concerns measurement of animal cruelty; the items did not include contextual features such as severity, frequency, perpetrator relationship, or emotional closeness to the harmed animal, all of which likely shape psychological impact (6, 7, 16). Future measurement work should evaluate item performance of the animal cruelty items alongside other ACEs, assess invariance across sociodemographic groups, and incorporate gradient scoring (e.g., severity, chronicity, relational proximity).
Finally, our assessment of ACEs dichotomized items into ever exposed or never exposed. Although this approach has been used in prior LCA studies (37, 106–108), it may overestimate exposure to ACEs that occurred infrequently in childhood and limit the ability to analyze outcomes based on frequency of exposure. We also chose to include sexual abuse exposure as a defining characteristic of the interpersonal violence and animal cruelty subgroup due to a 0.69 probability of endorsement; however, distributions of exposure may differ in other samples due to the sample-specific nature of LCA. Future research should replicate the current study and explore whether classes of individuals based on patterns of frequency of exposure to ACEs can be identified to support the presence of these subgroups in the larger population and to determine whether additional subgroups can be identified.
Future research can build on these findings in several ways. Longitudinal studies are needed to examine whether the adversity profiles identified here predict trajectories of mental health, social functioning, and relational outcomes across developmental stages. Expanding adversity measurement to include both threat- and deprivation-based domains would allow for a more comprehensive understanding of how adversity impacts multispecies households. More nuanced and precise animal cruelty measurement (e.g., severity, frequency, relational context) could also clarify how different features of cruelty exposures contribute to psychological outcomes (13). Additionally, qualitative studies could further illuminate children’s lived experiences of animal cruelty within the ecology of family violence, providing insight into meaning-making, coping, and recovery, and informing intervention strategies. Although prior work has emphasized overlap between intimate partner violence and animal cruelty (6, 11, 16), few studies have examined how animal cruelty interacts with broader constellations of childhood adversity.
A key priority for future research is to test whether ACE profiles that include animal cruelty exposure predict externalizing outcomes (e.g., cruelty perpetration, delinquency, arrests) and multi-system contact (e.g., child welfare, juvenile justice, behavioral health) linked to broader antisocial behavior (2, 109–111). Prospective designs using latent transition analysis (LTA) could examine movement between classes over time and clarify directionality of effects. Incorporating multi-informant data (e.g., caregiver reports, administrative records) would strengthen causal inference, reproducibility, and generalizability. Finally, intervention studies should test whether integrating animal welfare considerations into trauma-informed care, including safety planning for pets and grief-focused supports, improves engagement, safety, and outcomes for survivors of complex household violence. Together, such work would advance our understanding of animal cruelty as a meaningful component of childhood adversity and inform multispecies approaches to prevention, assessment, and intervention.
5 Conclusion
Exposure to violence directed toward animals in the home is an important and under-recognized form of childhood adversity. A majority (60%–80%) of U.S. children live with a companion animal (112, 113), and many consider these animals to be members of the family (114). Moreover, a substantial proportion of individuals report witnessing or being aware of harm to animals during childhood (2, 8). By integrating exposure to animal cruelty into a person-centered model of ACEs, this study demonstrates how patterns of violence can span across species boundaries. Understanding these patterns is essential in creating more inclusive models of adversity and developing prevention and intervention strategies that reflect the realities of children’s lives in multispecies families. Our findings underscore the value of incorporating animal cruelty exposure into ACE assessments, advancing translational efforts that align trauma-informed clinical care with coordinated responses across child welfare, domestic violence, and animal-protection systems.
Data availability statement
The datasets generated and analyzed for this study are not publicly available due to participant confidentiality and ethical restrictions under the approved Colorado State University IRB protocol. Qualified researchers may request access to de-identified data from the corresponding author (Dr. Shelby E. McDonald,c2hlbGJ5LmUubWNkb25hbGRAY29sb3N0YXRlLmVkdQ==) contingent upon appropriate data-use agreements and institutional approval.
Ethics statement
This study involving humans was approved by Colorado State University Institutional Review Board. The study was conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SM: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing, Writing – original draft. CT: Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing. NN: Writing – original draft, Writing – review & editing. LK: Methodology, Writing – original draft, Writing – review & editing. TA: Writing – original draft, Writing – review & editing. JF: Visualization, Writing – review & editing. SJ: Visualization, Writing – review & editing. GG: Writing – review & editing. LR: Writing – review & editing. CB: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This work was supported by the Human-Animal Bond in Colorado (HABIC) Center at Colorado State University.
Acknowledgments
We thank Dr. Stacey Freedenthal, Dr. Jen Currin-McCulloch, and Megan Scaggs for their support in refining and developing the overarching protocol for the study from which these data were obtained.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1701584/full#supplementary-material
References
1. Tomlinson CA, Murphy JL, Matijczak A, Califano A, Santos J, and McDonald SE. The link between family violence and animal cruelty: A scoping review. Soc Sci (Basel). (2022) 11:514. doi: 10.3390/socsci11110514
2. Ascione FR. Battered women’s reports of their partners’ and their children’s cruelty to animals. J Emotional Abuse. (1997) 1:119–33. doi: 10.1300/J135v01n01_06
3. Barrett BJ, Fitzgerald A, Peirone A, Stevenson R, and Cheung CH. Help-seeking among abused women with pets: evidence from a Canadian sample. Violence Victims. (2018) 33:604–26. doi: 10.1891/0886-6708.VV-D-17-00072
4. Faver CA and Strand EB. To leave or to stay?: battered women’s concern for vulnerable pets. J Interpers Violence. (2003) 18:1367–77. doi: 10.1177/0886260503258028
5. Fitzgerald AJ, Barrett BJ, Stevenson R, and Cheung CH. Animal maltreatment in the context of intimate partner violence: A manifestation of power and control? Violence Against Women. (2019) 25:1806–28. doi: 10.1177/107780121882499
6. McDonald SE, Collins EA, Nicotera N, Hageman TO, Ascione FR, Williams JH, et al. Children’s experiences of companion animal maltreatment in households characterized by intimate partner violence. Child Abuse Neglect. (2015) 50:116–27. doi: 10.1016/j.chiabu.2015.10.005
7. McDonald SE, Graham-Bermann SA, Maternick A, Ascione FR, and Williams JH. Patterns of adjustment among children exposed to intimate partner violence: a person-centered approach. Journ Child Adol Trauma. (2016) 9:137–52. doi: 10.1007/s40653-016-0079-y
8. DeGue S and DiLillo D. Is animal cruelty a “Red flag” for family violence?: investigating co-occurring violence toward children, partners, and pets. J Interpers Violence. (2009) 24:1036–56. doi: 10.1177/0886260508319362
9. Flynn CP. Examining the links between animal abuse and human violence: Animal Abuse and Criminology. Crime Law Soc Change. (2011) 55:453–68. doi: 10.1007/s10611-011-9297-2
10. Hartman CA, Hageman T, Williams JH, and Ascione FR. Intimate partner violence and animal abuse in an immigrant-rich sample of mother–child dyads recruited from domestic violence programs. J Interpers Violence. (2018) 33:1030–47. doi: 10.1177/0886260515614281
11. Collins EA, Cody AM, McDonald SE, Nicotera N, Ascione FR, and Williams JH. A template analysis of intimate partner violence survivors’ Experiences of animal maltreatment: implications for safety planning and intervention. Violence Against Wom. (2018) 24:452–76. doi: 10.1177/1077801217697266
12. Arkow P. Recognizing and responding to cases of suspected animal cruelty, abuse, and neglect: what the veterinarian needs to know. Vet Med: Res Rep. (2015) 6:349–59. doi: 10.2147/VMRR.S87198
13. McDonald SE, Cody AM, Collins EA, Stim HT, Nicotera N, Ascione FR, et al. Concomitant exposure to animal maltreatment and socioemotional adjustment among children exposed to intimate partner violence: a mixed methods study. Journ Child Adol Trauma. (2018) 11:353–65. doi: 10.1007/s40653-017-0176-6
14. Wauthier LM and Williams JM. Understanding and conceptualizing childhood animal harm: A meta-narrative systematic review. Anthrozoös. (2022) 35:165–202. doi: 10.1080/08927936.2021.1986262
15. Girardi A and Pozzulo JD. Childhood experiences with family pets and internalizing symptoms in early adulthood. Anthrozoos. (2015) 28:421–36. doi: 10.1080/08927936.2015.1052274
16. Hawkins RD, McDonald SE, O’Connor K, Matijczak A, Ascione FR, and Williams JH. Exposure to intimate partner violence and internalizing symptoms: The moderating effects of positive relationships with pets and animal cruelty exposure. Child Abuse Neglect. (2019) 98:104166. doi: 10.1016/j.chiabu.2019.104166
17. Currie CL. Animal cruelty by children exposed to domestic violence. Child Abuse Neglect. (2006) 30:425–35. doi: 10.1016/j.chiabu.2005.10.014
18. McEwen FS, Moffitt TE, and Arseneault L. Is childhood cruelty to animals a marker for physical maltreatment in a prospective cohort study of children? Child Abuse Negl. (2014) 38:533–43. doi: 10.1016/j.chiabu.2013.10.016
19. Thompson KL and Gullone E. Prosocial and antisocial behaviors in adolescents: An investigation into associations with attachment and empathy. Anthrozoos. (2008) 21:123–37. doi: 10.2752/175303708X305774
20. Pace CS, Muzi S, Rogier G, Meinero LL, and Marcenaro S. The Adverse Childhood Experiences – International Questionnaire (ACE-IQ) in community samples around the world: A systematic review (part I). Child Abuse Neglect. (2022) 129:105640. doi: 10.1016/j.chiabu.2022.105640
21. World Health Organization. Adverse Childhood Experiences International Questionnaire (ACE-IQ) (2018). Geneva: WHO. Available online at: https://cdn.who.int/media/docs/default-source/documents/child-maltreatment/ace-questionnaire.pdf?sfvrsn=baed215c_2 (Accessed June 15, 2025).
22. World Health Organization Team – Violence Prevention (PVL). Adverse Childhood Experiences International Questionnaire (ACE-IQ) (2020). Geneva: WHO. Available online at: https://www.who.int/publications/m/item/adverse-childhood-experiences-international-questionnaire-(ace-iq) (Accessed June 15, 2025).
23. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am J Prev Med. (1998) 14:245–58. doi: 10.1016/S0749-3797(98)00017-8
24. United Nations Committee on the Rights of the Child. General Comment No. 26 on Children’s rights and the envrionment with a special focus on climate change (2023). Available online at: https://www.ohchr.org/en/documents/general-comments-and-recommendations/crccgc26-general-comment-no-26-2023-childrens-rights?utm_source=chatgpt.com. Report No.: CRC/C/GC/26 (Accessed June 15, 2025).
25. McLaughlin KA, Sheridan MA, and Lambert HK. Childhood adversity and neural development: Deprivation and threat as distinct dimensions of early experience. Neurosci Biobehav R. (2014) 47:578–91. doi: 10.1016/j.neubiorev.2014.10.012
26. Busso DS, McLaughlin KA, and Sheridan MA. Dimensions of adversity, physiological reactivity, and externalizing psychopathology in adolescence: deprivation and threat. Psychosom Med. (2017) 79:162–71. doi: 10.1097/PSY.0000000000000369
27. Lambert HK, King KM, Monahan KC, and McLaughlin KA. Differential associations of threat and deprivation with emotion regulation and cognitive control in adolescence. Dev Psychopathol. (2017) 29:929–40. doi: 10.1017/S0954579416000584
28. Sheridan MA and McLaughlin KA. Dimensions of early experience and neural development: deprivation and threat. Trends Cognit Sci. (2014) 18:580–5. doi: 10.1016/j.tics.2014.09.001
29. McDonald SE, Tomlinson CA, Applebaum JW, Moyer SW, Brown SM, Carter S, et al. Human–animal interaction and perinatal mental health: A narrative review of selected literature and call for research. Int J Environ Res Public Health. (2021) 18:10114. doi: 10.3390/ijerph181910114
30. Heim C, Newport DJ, Mletzko T, Miller AH, and Nemeroff CB. The link between childhood trauma and depression: Insights from HPA axis studies in humans. Psychoneuroendocrino. (2008) 33:693–710. doi: 10.1016/j.psyneuen.2008.03.008
31. Jovanovic T and Ressler KJ. How the neurocircuitry and genetics of fear inhibition may inform our understanding of PTSD. Am J Psychiat. (2010) 167:648–62. doi: 10.1176/appi.ajp.2009.09071074
32. McLaughlin KA, Sheridan MA, Gold AL, Duys A, Lambert HK, Peverill M, et al. Maltreatment exposure, brain structure, and fear conditioning in children and adolescents. Neuropsychopharmacol. (2016) 41:1956–64. doi: 10.1038/npp.2015.365
33. Whipple EE. The human–animal bond and grief and loss: implications for social work practice. Families Society. (2021) 102:518–28. doi: 10.1177/10443894211015132
34. Wauthier L and Williams JM. A qualitative study of children’s accounts of cruelty to animals: uncovering the roles of trauma, exposure to violence, and attachment. J Interpers Violence. (2022) 37:NP6405–38. doi: 10.1177/0886260520928640
35. Brown SM, Rienks S, McCrae JS, and Watamura SE. The co-occurrence of adverse childhood experiences among children investigated for child maltreatment: A latent class analysis. Child Abuse Neglect. (2019) 87:18–27. doi: 10.1016/j.chiabu.2017.11.010
36. Shin SH, McDonald SE, and Conley D. Patterns of adverse childhood experiences and substance use among young adults: A latent class analysis. Addict Behav. (2018) 78:187–92. doi: 10.1016/j.addbeh.2017.11.020
37. Kim Y, Kim K, Chartier KG, Wike TL, and McDonald SE. Adverse childhood experience patterns, major depressive disorder, and substance use disorder in older adults. Aging Ment Health. (2021) 25:484–91. doi: 10.1080/13607863.2019.1693974
38. Lanza ST and Rhoades BL. Latent class analysis: an alternative perspective on subgroup analysis in prevention and treatment. Prev Sci. (2013) 14:157–68. doi: 10.1007/s11121-011-0201-1
39. Bridges-Curry Z and Newton TL. Patterns of trauma exposure, emotion dysregulation, and mental health symptoms: A latent class analysis. J Aggress Maltreat Trauma. (2022) 31:285–303. doi: 10.1080/10926771.2021.1970673
40. Romm KF and Berg CJ. Patterns of adverse childhood experiences and problematic health outcomes among US young adults: A latent class analysis. Subst Use Addict J. (2024) 45:191–200. doi: 10.1177/29767342231218081
41. Palan S and Schitter C. Prolific.ac—A subject pool for online experiments. J Behav Exp Finance. (2018) 17:22–7. doi: 10.1016/j.jbef.2017.12.004
42. Cohen S and Wills TA. Stress, social support, and the buffering hypothesis. psychol Bull. (1985) 98:310–57. doi: 10.1037/0033-2909.98.2.310
43. Lakey B and Cohen S. Social support theory and measurement. In: Social support measurement and intervention: A guide for health and social scientists. Oxford University Press, New York (2000). p. 29–52.
44. Rueger SY, Malecki CK, Pyun Y, Aycock C, and Coyle S. A meta-analytic review of the association between perceived social support and depression in childhood and adolescence. Psychol Bull. (2016) 142:1017–67. doi: 10.1037/bul0000058
45. Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. (2011) 52:145–61. doi: 10.1177/0022146510395592
46. McLaughlin KA, Greif Green J, Gruber MJ, Sampson NA, Zaslavsky AM, and Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Arch Gen Psychiat. (2012) 69:1151–60. doi: 10.1001/archgenpsychiatry.2011.2277
47. Merrick MT, Ford DC, Ports KA, and Guinn AS. Prevalence of adverse childhood experiences from the 2011–2014 behavioral risk factor surveillance system in 23 states. JAMA Pediatr. (2018) 172:1038–44. doi: 10.1001/jamapediatrics.2018.2537
48. Ascione FR. Pet treatment survey (Unpublished rating scale). Denver, CO: University of Denver (2011).
49. Lovibond SH and Lovibond PF. Manual for the depression anxiety stress scales (1995). Psychology Foundation of Australia, Sydney, N.S.W., ©1995. Available online at: https://cir.nii.ac.jp/crid/1370294643851494273 (Accessed June 15, 2025).
50. Antony MM, Bieling PJ, Cox BJ, Enns MW, and Swinson RP. Psychometric properties of the 42-item and 21-item versions of the depression anxiety stress scales in clinical groups and a community sample. Psychol Assessment. (1998) 10:176–81. doi: 10.1037/1040-3590.10.2.176
51. Zimet GD, Powell SS, Farley GK, Werkman S, and Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. (1990) 55:610–7. doi: 10.1207/s15327752jpa5503&4_17
52. Masyn KE and Little TD. Latent class analysis and finite mixture modeling. In: The Oxford Handbook of Quantitative Methods in Psychology. New York, NY: Oxford University Press (2013). p. 551–611. (Oxford Library of Psychology; vol. 2).
53. Nagin DS and Kerner HJ. Group-based modeling of development. Ann Am Acad Pol Soc Sci. (2005) 602:259–79. doi: 10.4159/9780674041318
54. Nylund-Gibson K and Choi AY. Ten frequently asked questions about latent class analysis. Trans Issues psychol Sci. (2018) 4:440–61. doi: 10.1037/tps0000176
55. Asparouhov T and Muthén B. Auxiliary variables in mixture modeling: three-step approaches using mplus. Struct Equation Model. (2014) 21:329–41. doi: 10.1080/10705511.2014.915181
56. McDonald SE, Dmitrieva J, Shin S, Hitti SA, Graham-Bermann SA, Ascione FR, et al. The role of callous/unemotional traits in mediating the association between animal abuse exposure and behavior problems among children exposed to intimate partner violence. Child Abuse Neglect. (2017) 72:421–32. doi: 10.1016/j.chiabu.2017.09.004
57. Murphy JL, Voorhees EV, O’Connor KE, Tomlinson CA, Matijczak A, Applebaum JW, et al. Positive engagement with pets buffers the impact of intimate partner violence on callous-unemotional traits in children. J Interpers Violence. (2022) 37:NP17205–26. doi: 10.1177/08862605211028301
58. Volant AM, Johnson JA, Gullone E, and Coleman GJ. The relationship between domestic violence and animal abuse: an Australian study. J Interpers Violence. (2008) 23:1277–95. doi: 10.1177/0886260508314309
59. Carlisle-Frank P, Frank JM, and Nielsen L. Selective battering of the family pet. Anthrozoos. (2004) 17:26–42. doi: 10.2752/089279304786991864
60. Gullone E and Clarke JP. Animal abuse, cruelty, and welfare: An Australian perspective. In: The international handbook of animal abuse and cruelty: Theory, research, and application West Lafayette, Indiana (2008). p. 305–34.
61. Gilbert LK, Breiding MJ, Merrick MT, Thompson WW, Ford DC, Dhingra SS, et al. Childhood adversity and adult chronic disease an update from ten states and the district of Columbia, 2010. Am J Prev Med. (2015) 48:345–9. doi: 10.1016/j.amepre.2014.09.006
62. Swedo EA, Aslam MV, Dahlberg LL, Niolon PH, Guinn AS, Simon TR, et al. Prevalence of adverse childhood experiences among U.S. Adults — Behavioral risk factor surveillance system, 2011–2020. MMWR Morbid Mortal Wkly Rep. (2023) 72:707–15. doi: 10.15585/mmwr.mm7226a2
63. Ports KA, Ford DC, Merrick MT, and Guinn AS. Chapter 2 - ACEs: Definitions, measurement, and prevalence. In: Asmundson GJG and Afifi TO, editors. Adverse childhood experiences. London, UK: Academic Press (2020). p. 17–34. Available online at: https://www.sciencedirect.com/science/article/pii/B9780128160657000021 (Accessed August, 1, 2025).
64. Hines DA, Douglas EM, and Mahmood S. The effects of survey administration on disclosure rates to sensitive items among men: A comparison of an internet panel sample with a RDD telephone sample. Comput Hum Behav. (2010) 26:1327–35. doi: 10.1016/j.chb.2010.04.006
65. Finkelhor D, Turner H, Wormuth BK, Vanderminden J, and Hamby S. Corporal punishment: current rates from a national survey. J Child Fam Stud. (2019) 28:1991–7. doi: 10.1007/s10826-019-01426-4
66. Mathews B and Dube S. Childhood emotional abuse is becoming a public health priority: Evidentiary support for a paradigm change. Child Prot Pract. (2025) 4:100093. doi: 10.1016/j.chipro.2024.100093
67. Krause JT, Murray-Perdue SA, Tomlinson CA, and Brown SM. The influence of cumulative and dimensional childhood adversity on maternal sleep quality. J Family Psychol. (2025). doi: 10.1037/fam0001322
68. Kumar S, Campbell JA, Wang X, Xu Y, Nagavally S, and Egede LE. Trends in prevalence of adverse childhood experiences by sociodemographic factors in the United States: Behavioral Risk Factor Surveillance System 2009–2022. BMC Public Health. (2024) 24:2615–13. doi: 10.1186/s12889-024-20125-4
69. Ladny RT and Meyer L. Traumatized witnesses: review of childhood exposure to animal cruelty. Journ Child Adol Trauma. (2020) 13:527–37. doi: 10.1007/s40653-019-00277-x
70. McCown CM, Platt LF, Burgess C, Johnson AJ, and Lund EM. Violence Against Queer and TGNC People of Color. Switzerland: Springer International Publishing AG (2020) p. 203–17.
71. Santacrose DE, Kia-Keating M, and Lucio D. A systematic review of socioecological factors, community violence exposure, and disparities for Latinx youth. J Traumatic Stress. (2021) 34:1027–44. doi: 10.1002/jts.22733
72. Sheats KJ, Irving SM, Mercy JA, Simon TR, Crosby AE, Ford DC, et al. Violence-related disparities experienced by black youth and young adults: opportunities for prevention. Am J Prev Med. (2018) 55:462–9. doi: 10.1016/j.amepre.2018.05.017
73. Clark KD, Jewell J, Sherman ADF, Balthazar MS, Murray SB, and Bosse JD. Lesbian, gay, bisexual, transgender and queer people’s experiences of stigma across the spectrum of inpatient psychiatric care: A systematic review. Int J Ment Health Nurs. (2025) 34:e13455. doi: 10.1111/inm.13455
74. Feagin J and Bennefield Z. Systemic racism and U.S. health care. Soc Sci Med. (2014) 103:7–14. doi: 10.1016/j.socscimed.2013.09.006
75. Richards TN, Schwartz JA, and Wright E. Examining adverse childhood experiences among Native American persons in a nationally representative sample: Differences among racial/ethnic groups and race/ethnicity-sex dyads. Child Abuse Neglect. (2021) 111:104812. doi: 10.1016/j.chiabu.2020.104812
76. Arluke A, Levin J, Luke C, and Ascione FR. The relationship of animal abuse to violence and other forms of antisocial behavior. J Interpers Violence. (1999) 14:963–75. doi: 10.1177/088626099014009004
77. Baxendale S, Lester L, Johnston R, and Cross D. Risk factors in adolescents’ involvement in violent behaviours. J Aggress Conflict Peace Res. (2015) 7:2–18. doi: 10.1108/JACPR-09-2013-0025
78. Boat BW, Pearl E, Barnes JE, Richey L, Crouch D, Barzman D, et al. Childhood cruelty to animals: psychiatric and demographic correlates. J Aggress Maltreat Trauma. (2011) 20:812–9. doi: 10.1080/10926771.2011.610773
79. Gullone E and Robertson N. The relationship between bullying and animal abuse behaviors in adolescents: The importance of witnessing animal abuse. J Appl Dev Psychol. (2008) 29:371–9. doi: 10.1016/j.appdev.2008.06.004
80. Henry B and Sanders C. Bullying and animal abuse: is there a connection? Soc Anim. (2007) 15:107–26. doi: 10.1163/156853007X187081
81. Miller C. Childhood animal cruelty and interpersonal violence. Clin Psychol Rev. (2001) 21:735–49. doi: 10.1016/S0272-7358(00)00066-0
82. Vaughn MG, Fu Q, DeLisi M, Beaver KM, Perron BE, Terrell K, et al. Correlates of cruelty to animals in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Psychiatr Res. (2009) 43:1213–8. doi: 10.1016/j.jpsychires.2009.04.011
83. Burchfield KB. The nature of animal crime: scope and severity in Chicago. Crime Delinquency. (2018) 64:1904–24. doi: 10.1177/0011128717719515
84. Hankerson SH, Moise N, Wilson D, Waller BY, Arnold KT, Duarte C, et al. The intergenerational impact of structural racism and cumulative trauma on depression. Am J Psychiatry. (2022) 179:434–40. doi: 10.1176/appi.ajp.21101000
85. Reese LA, Vertalka JJ, and Richard C. Animal cruelty and neighborhood conditions. Anim (Basel). (2020) 10:2095. doi: 10.3390/ani10112095
86. Warner BD. The role of attenuated culture in social disorganization theory. Criminology. (2003) 41:73–98. doi: 10.1111/j.1745-9125.2003.tb00982.x
87. White G and Quick LD. Animal cruelty, domestic violence, and social disorganization in a suburban setting. Deviant Behav. (2019) 40:930–41. doi: 10.1080/01639625.2018.1445442
88. Stone SD. Trauma approaches to healing animal companion loss. 1st ed. United Kingdom: Routledge (2024) p. 137–56.
89. Finkelhor D. Screening for adverse childhood experiences (ACEs): Cautions and suggestions. Child Abuse Neglect. (2018) 85:174–9. doi: 10.1016/j.chiabu.2017.07.016
90. McLennan JD, MacMillan HL, Afifi TO, McTavish J, Gonzalez A, and Waddell C. Routine ACEs screening is NOT recommended. Paediatr Child Health. (2019) 24:272–3. doi: 10.1093/pch/pxz042
91. McLennan JD, Gonzalez A, MacMillan HL, and Afifi TO. Routine screening for adverse childhood experiences (ACEs) still doesn’t make sense. Child Abuse Negl. (2024) 106708:1–7.
92. Callaghan JEM, Fellin LC, Mavrou S, Alexander JH, Deligianni-Kouimtzi V, Papathanassiou M, et al. Part of the family: children’s experiences with their companion animals in the context of domestic violence and abuse. J Fam Viol. (2025) 40:863–77. doi: 10.1007/s10896-023-00659-8
93. Diemer K, Gallant D, Mosso Tupper N, Hammond K, Ramamurthy A, Humphreys C, et al. Exploring the linkages between animal abuse, domestic abuse, and sexual offending: A scoping review. Health Soc Care Community. (2024) 2024:1–19. doi: 10.1155/2024/1170505
94. Baughman C, Coles T, Feinberg J, and Newton H. The surveillance tentacles of the child welfare system. Columbia J Race Law. (2021) 11:501–32. doi: 10.52214/cjrl.v11i3.8743
95. Maldonado Fabela K. The child welfare system as a social determinant of health. Sociol Compass. (2024) 18:1–19. doi: 10.1111/soc4.13210
96. Voith LA, Lee H, Russell KN, and Korsch-Williams AE. Understanding how relational health effects intimate partner violence perpetration among low-income, black, indigenous, men of color exposed to adverse childhood experiences: an exploratory study. Int J Environ Res Public Health. (2021) 18:3890. doi: 10.3390/ijerph18083890
97. Nadeem E, Greswold W, Torres LZ, and Johnson HE. Trauma-informed care in school-based health centers: A mixed methods study of behavioral health screening and services. School Psychol. (2023) 38:355–69. doi: 10.1037/spq0000591
98. Mota-Rojas D, Monsalve S, Lezama-García K, Mora-Medina P, Domínguez-Oliva A, Ramírez-Necoechea R, et al. Animal abuse as an indicator of domestic violence: one health, one welfare approach. Anim (Basel). (2022) 12:977. doi: 10.3390/ani12080977
99. Danese A. Annual Research Review: Rethinking childhood trauma-new research directions for measurement, study design and analytical strategies. J Child Psychol Psychiatry. (2020) 61:236–50. doi: 10.1111/jcpp.13160
100. Lacey RE and Minnis H. Practitioner Review: Twenty years of research with adverse childhood experience scores – Advantages, disadvantages and applications to practice. J Child Psychol Psychiatry. (2020) 61:116–30. doi: 10.1111/jcpp.13135
101. Krushas AE, Kulig TC, and Goslar M. Advancing the study of adverse childhood experiences: an examination of measurement and latent classes. Justice Q. (2025), 1–37. doi: 10.1080/07418825.2025.2451311
102. Craig SL, Austin A, Levenson J, Leung VWY, Eaton AD, and D’Souza SA. Frequencies and patterns of adverse childhood events in LGBTQ+ youth. Child Abuse Neglect. (2020) 107:104623. doi: 10.1016/j.chiabu.2020.104623
103. Maguire-Jack K, Lanier P, and Lombardi B. Investigating racial differences in clusters of adverse childhood experiences. Am J Orthopsychiatry. (2020) 90:106–14. doi: 10.1037/ort0000405
104. Mersky JP, Choi C, Plummer Lee C, and Janczewski CE. Disparities in adverse childhood experiences by race/ethnicity, gender, and economic status: Intersectional analysis of a nationally representative sample. Child Abuse Neglect. (2021) 117:105066. doi: 10.1016/j.chiabu.2021.105066
105. Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, et al. Adverse childhood experiences expanding the concept of adversity. Am J Prev Med. (2015) 49:354–61. doi: 10.1016/j.amepre.2015.02.001
106. Guo N, Luk TT, Zhao SZ, and Weng X. Associations between patterns of adverse childhood experiences and adult chronic conditions: A population-based study. Child Abuse Negl. (2025) 169:107628. doi: 10.1016/j.chiabu.2025.107628
107. Herberholz ES, Wolchok RE, Rogers JM, Selenou-Yemgang S, Beckwith BD, Smith KE, et al. Latent classes of adverse childhood experiences (ACEs) and adult substance-use problems and psychosocial outcomes: complex and heterogeneous associations. Int J Ment Health Addict. (2025). doi: 10.1007/s11469-025-01527-w
108. Merians AN, Baker MR, Frazier P, and Lust K. Outcomes related to adverse childhood experiences in college students: Comparing latent class analysis and cumulative risk. Child Abuse Neglect. (2019) 87:51–64. doi: 10.1016/j.chiabu.2018.07.020
109. Walters GD. Testing the direct, indirect, and moderated effects of childhood animal cruelty on future aggressive and non-aggressive offending. Aggress Behav. (2014) 40:238–49. doi: 10.1002/ab.21514
110. Walters GD and Noon A. Family context and externalizing correlates of childhood animal cruelty in adjudicated delinquents. J Interpers Violence. (2015) 30:1369–86. doi: 10.1177/0886260514540328
111. Walters GD. A developmental antecedent-reciprocal effects model of the animal cruelty-later offending relationship. Aggress Violent Behav. (2025) 82:102053. doi: 10.1016/j.avb.2025.102053
112. Purewal R, Christley R, Kordas K, Joinson C, Meints K, Gee N, et al. Companion animals and child/adolescent development: A systematic review of the evidence. Int J Env Res Pub He. (2017) 14:234. doi: 10.3390/ijerph14030234
113. Melson GF. Child development and the human-companion animal bond. Am Behav Sci. (2003) 47:31–9. doi: 10.1177/0002764203255210
Keywords: animal cruelty, adverse childhood experiences, interpersonal violence, mental health, latent class analysis, childhood adversity, violence prevention
Citation: McDonald SE, Tomlinson C, Nicotera N, Kogan LR, Abell T, Ford J, Jafarian S, Girish G, Rodriguez LS and Bright CL (2025) Integrating animal cruelty exposure into person-centered models of childhood adversity: latent classes and associations with depression, anxiety, and stress. Front. Psychiatry 16:1701584. doi: 10.3389/fpsyt.2025.1701584
Received: 08 September 2025; Accepted: 20 October 2025;
Published: 07 November 2025.
Edited by:
Domenico De Berardis, ASL 4, ItalyReviewed by:
Crispin Mbamba, University at Albany, SUNY, United StatesAmber Soluri (krushas), University of Nevada Las Vegas Greenspun College of Urban Affairs, United States
Copyright © 2025 McDonald, Tomlinson, Nicotera, Kogan, Abell, Ford, Jafarian, Girish, Rodriguez and Bright. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shelby E. McDonald, c2hlbGJ5LmUubWNkb25hbGRAY29sb3N0YXRlLmVkdQ==
 Shelby E. McDonald
Shelby E. McDonald Camie Tomlinson
Camie Tomlinson Nicole Nicotera3
Nicole Nicotera3 Lori R. Kogan
Lori R. Kogan