- Department of Pediatric Dentistry and Dental Public Health and Policy, School of Dentistry, Virginia Commonwealth University, Richmond, VA, United States
Introduction: Parents play an influential role in their children's lives, but little is known about how their healthcare experiences connect. This study examined the relationship between parent's healthcare use and their child's overall and preventive dental care use.
Methods: We pooled three years (2017–2019) of Medical Expenditure Panel Survey (MEPS) data and merged child (0–17 years) and parent data. Our outcomes included any dental visit, preventive visit, and receipt of sealant or fluoride. The primary exposure variable was the parents’ medical and dental care use, grouped into four categories. Descriptive and bivariate analyses were conducted, and multivariable logistic regression analyses were used to examine the associations.
Results: The study included data from 9,927 children. Overall, 50.1%, 42.3%, and 21.2% had any dental visit, preventive visit, and fluoride or sealant application, respectively, in the past 12 months. Among parents, 38.3% had both medical and dental visits, 5.8% had a dental but no medical, 36.7% had a medical but no dental, and 19.1% had neither. Children whose parents had medical and dental visits had more than five times the odds of having any dental visit (aOR = 5.49, 95% CI: 4.64, 6.52) and preventive dental visit (aOR = 5.41, 95% CI: 4.57, 6.39) and 3.64 times the odds of receiving sealant or fluoride application (95% CI: 2.93, 4.53) compared to those whose parents had no dental and medical visits.
Conclusions: Children's oral health utilization is strongly linked with parents’ healthcare use. It can be improved by educating parents and supporting their healthcare use.
Introduction
Despite advances in oral health care access and delivery in the past decade, one in five 6–11-year-olds and one in two 12–19-year-olds had experienced dental caries, and nearly one in five 6–8-year-olds and 12–19-year-olds (16.4% and 16.6%) had untreated caries, respectively (1). Untreated caries can result in pain, infections, expensive emergency department (ED) visits, and hospitalizations (2) and can negatively impact learning, school attendance, social interactions, and self-esteem (3). The foundation for good oral health starts early in childhood. Still, many children lack routine dental visits, and many do not receive preventive oral health services to support good oral health (4, 5). Acute and unplanned dental care accounts for a loss of 34 million school hours annually among US children (6).
Regular dental care can detect dental issues early and prevent disease progression. The two highly effective evidence-based preventive oral health services to prevent the onset and progression of dental caries among children include fluoride varnish (FV) and dental sealants (7, 8). Sealants are recommended for use on the molars in children and adolescents (9). Dental sealants reduce caries incidence by 80% over two years in the posterior teeth (10). However, despite being a national health objective, sealant receipt is low and disparate (11). During 2011–2016, sealant prevalence in 1st molars and 2nd molars was only 44% and 35%, respectively, among 12–19-year-old children (12), and it varied widely by sociodemographic factors (1).
FV, another proven preventive oral health service, can help remineralize the tooth enamel and protect teeth. It prevents nearly 40% of caries (13). Its use among children is recommended by the American Dental Association, the American Association of Pediatric Dentistry (AAP) (14), and the US Preventive Services Task Force (15). Additionally, the AAP suggests that primary care providers should apply FV on all infants’ and children's teeth at least once every six months, starting when the first tooth erupts and until the establishment of a dental home, but its prevalence remains low (14). A 2014 study using Medical Expenditure Panel Survey data found that only 14.2% of children aged ≤21 years received topical fluoride, sealants, or both (16).
Children and adolescents heavily depend on adults to meet their health needs, including oral health. Parents play a pivotal role in a child's life, and the well-being of children is intricately tied to their parents' physical, social, and emotional health and social circumstances (17). As the primary decision-makers for children, parents' personal choices, experiences, and interactions with health systems can significantly influence and impact the health services used by their children (18). Prior studies have shown an association between parents' healthcare use and children's receipt of well-child visits (19, 20). Evidence also shows a strong relationship between mothers' and children's use of healthcare for physician visits, emergency department use, hospitalizations, vaccination, and mental health visits (21, 22). Similarly, parents who have a negative experience with health care or have problems accessing care may also have difficulty getting care for their children. A recent study using 2016 National Health Interview Survey (NHIS) data found that children had two times the risk of lacking dental visits if the parent had no dental visit and nine times the risk of deferred care if the parent reported inability to afford dental care (23) compared to their counterparts. Similar results were found in another study using older NHIS data (24). However, the relationship between parents' healthcare use and dental care use among children is not known.
Previous studies had used only one measure of dental care use, whether a child had at least one dental visit within the past 12 months, and did not differentiate between dental use and preventive services used, such as sealant and fluoride treatments (23, 24). In this study, we addressed this gap using the Medical Expenditure Panel Survey (MEPS), a preferred survey for estimating health utilization, to significantly extend our understanding of the relationship between parent's medical and dental care use and their child's dental care use. We hypothesized that children whose parent had healthcare use (dental, medical, or both) would have higher odds of dental care use and show a dose-response. For example, dental care among children will be highest among children whose parents had used medical and dental care, followed by those whose parents had just used dental care. Our rationale for these hypotheses is based on the assumption that parents' interaction with the health system in medical or dental settings improves their knowledge about health conditions in general, oral health, and preventive services. By using healthcare services for themselves and understanding the benefits and risks, parents may be more inclined to use these services for their children, influencing children's use of dental care and preventive oral health services.
Materials and methods
Data source and study population
We pooled three years (2017–2019) of publicly available MEPS data. MEPS is an annual survey conducted by the Agency for Healthcare Research and Quality, providing a nationally representative sample of the U.S. civilian non-institutionalized population. It includes detailed information about individuals' healthcare use (including visits to a dentist), health insurance status, socioeconomic status, and family characteristics. A single respondent from the household provides information to an interviewer using computer-assisted personal interviewing. More information about MEPS can be found at http://www.meps.ahrq.gov. For a detailed description of the survey and its methodology, see Chowdhury et al. (25). For our study, we merged the household data with the dental visit data each year, and children and parent data were linked to create dyadic observational units.
The unit of analysis for our study was a child. We specifically focused on the youngest child in the family. Our final analytical sample included 9,927 children (weighted n = 36,691,423) aged 0–17, with complete information on dental utilization and parent healthcare utilization. We excluded children who resided alone, resided in separate households, or with grandparents (n = 1,677), those with non-positive weights (n = 368), and older children in the same family (n = 10,156).
Outcome variables
Our analysis included three outcome variables describing the children's dental care use for all children included in the study. Each outcome was categorized as a binary yes/no variable.
Any dental visit: Parents who reported that their child had visited general dentists, dental hygienists, dental technicians, dental surgeons, orthodontists, endodontists, or periodontists in the past 12 months were categorized as “yes” for any dental visit and “no” otherwise.
Preventive dental visit: In the MEPS questionnaire, participants were asked to select all the services they had used during a dental visit in the past 12 months. Parent reported for their child. We constructed the variable to identify children who received preventive dental services if the following procedures were recorded: cleaning, prophylaxis, polishing, periodontal recall, fluoride treatment, or sealant application, and categorized it as “yes” otherwise “no.”
FV/Sealant receipt: This outcome was coded as “yes” if the child received sealant, fluoride, or both. Otherwise, it was coded as “no.”
Main exposure variable
Parent's healthcare utilization: Our primary exposure variable was constructed using two variables describing medical and dental care use among parents and using the mother as a primary source (21, 22). We used the mother's complete healthcare data when available, and in cases where the mother's data was missing, the father's data was utilized (we used the mother's information for 9,484 children and father's information for 443 children) to construct this variable. A parent was considered to have a medical visit if they had at least one visit to any medical provider, including physicians and non-physicians (e.g., nurses, technicians), in an office-based setting. Similarly, a parent was considered to have a dental visit if they had at least one visit to a general dentist, dental hygienist, dental technician, dental surgeon, orthodontist, endodontist, or periodontist in the past 12 months. Using information from both variables, parent's healthcare utilization was categorized into four groups: had both a medical visit and a dental visit, had a dental visit only, had a medical visit only, and had no medical or dental visits.
Covariates
We selected the following child, parent, and family covariates based on the prior literature (23, 24): child age (0–5 years, 6–11 years, and 12–17 years), sex (male, female), race and ethnicity [Hispanic, non-Hispanic (NH) White, NH Black, NH Asian, and Other or Multiple races], dental insurance (private dental, public dental, private medical but no dental, and no insurance), number of children under 18 years old in the family (one, two or three, and four or more), and region (Northeast, Midwest, South, and West). The health status of children was assessed three times in a calendar year and was categorized as very good/excellent, good, and fair/poor based on the parent's reports of “excellent or very good” and “good” in at least two rounds, and “fair or poor” otherwise. We did not include the parent insurance variable in the model as it was correlated with the child's insurance variable and was also, in part, accounted for in our main exposure, the parent healthcare use variable.
For children whose mothers' healthcare data was not missing, the mothers' information was used for all parent-level variables. This included variables like parental education, categorized as less than high school, high school, bachelor's (some college or bachelor's), and master's or more; poverty status, categorized as poor (<100% FPL), near-poor (100%–200% FPL), middle income (>200%–400% FPL), and high income (>400% FPL); and employment status, categorized as unemployed, self-employed, or employed. If the mothers' information was missing, the fathers' information was used for these variables.
Data analysis
We utilized descriptive statistics to provide the demographic, socioeconomic characteristics, dental insurance, and health status associated with children's dental care utilization outcomes. Chi-square tests were used to assess bivariate relationships between outcomes and included variables. As all of our outcome variables were binary, we used multivariable logistic regression models, controlling for various child and parent-related covariates and adjusted odds ratios (aOR), and their corresponding 95% confidence intervals (CI) were calculated. All analyses were weighted and adjusted for the complex survey design using SAS, with survey weights to generate national estimates. Pooled variance structure was used to account for clustering in the panel data. Further details on survey weighting and adjusting for complex design are available on the MEPS website. A p-value of 0.05 was considered significant and non-missing data from each variable was utilized for analysis. IRB approval was not necessary as the data is publicly available and deidentified. We also conducted a sensitivity analysis to examine sealant and FV receipt among 6–17-year-olds to align the study population age with the sealant recommendation age (Supplementary Table 1).
Results
During 2017–2019, 38.3% of US children aged 0–17 years living with a parent, had at least one parent who had both medical and dental visits, 5.8% had only dental visits, 36.7% had only medical visits, and the remaining did not have either visit in the past 12 months (Table 1). Demographically, 40.8% of the children were aged 0–5 years, 51.9% were males, and 50.2% were NH White. Nearly half (48.8%) of children had private dental insurance, 88.1% had a report of excellent/very good health status, and 38.8% resided in the South region. At the family level, 36.7% of children lived in families with income greater than 400% of the federal poverty level, 51.5% had a parent with some college/bachelor's degrees, 69.1% had a employed/self-employed parent, and 56.7% had at least one sibling under 18 years old.
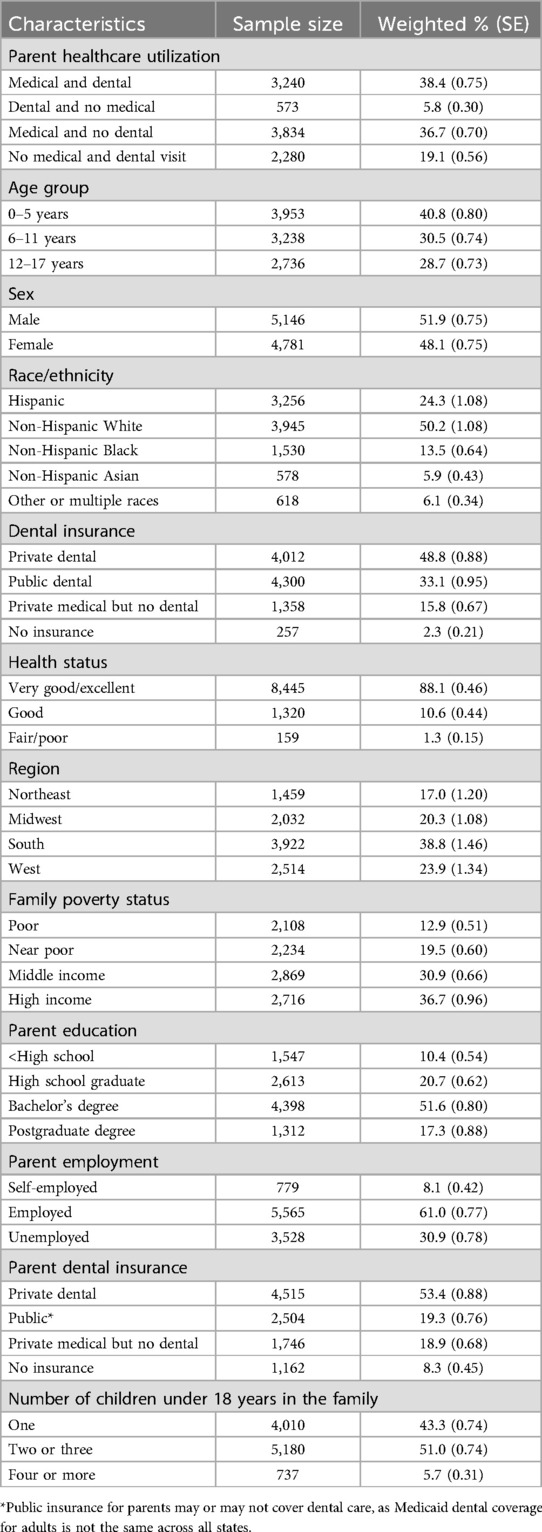
Table 1. Characteristics of the study population, Medical Expenditure Panel Survey, 2017–2019 (n = 9,927).
Bivariate analysis
Any dental visits
Overall, 50.1% of children had a dental visit in the past 12 months. Among children whose parents had both medical and dental visits, 70.1% had a dental visit. The percentage of dental visits reduced to 60.6% among children whose parents had a dental visit only, 38.6.% among those whose parents had a medical visit only, and 29.1% among children whose parents had neither medical nor dental visits (Figure 1).
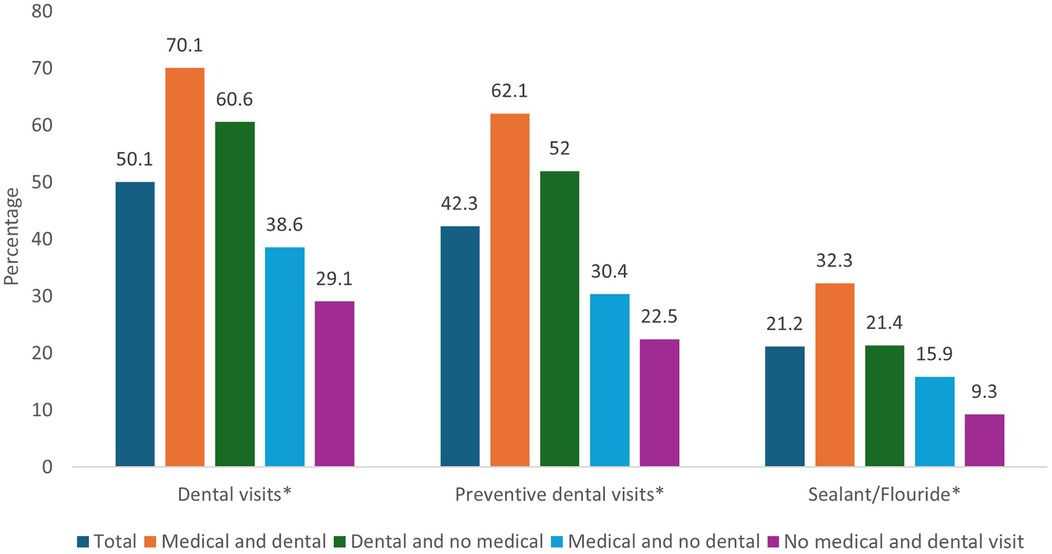
Figure 1. Dental care utilization outcomes among children stratified by parent's health care utilization, Medical Expenditure Panel Survey, 2017–2019. *Statistical significance at p-value <0.001.
The percentage of dental visits was over 50% among children in age categories 6–11 (60.8%) or 12–17 (61.9%) years, as well as among NH White (54.5%), NH Asian (50.1%), or other races (50.5%) compared to their counterparts (Table 2). There was a difference of 27.0 percentage points in any dental visit between children with private dental insurance (56.9%) and those without any insurance (29.9%). More than 50% of children residing in the West (53.6%), Midwest (50.6%), or Northeast (50.4%) regions had a dental visit (Table 2). The dental visit percentage was higher among children from families with income greater than 400% of the federal poverty level (60.7%), whose parents had a postgraduate degree or more (62.5%), or those who lived in families with 2–3 children (50.6%) compared to their counterparts.
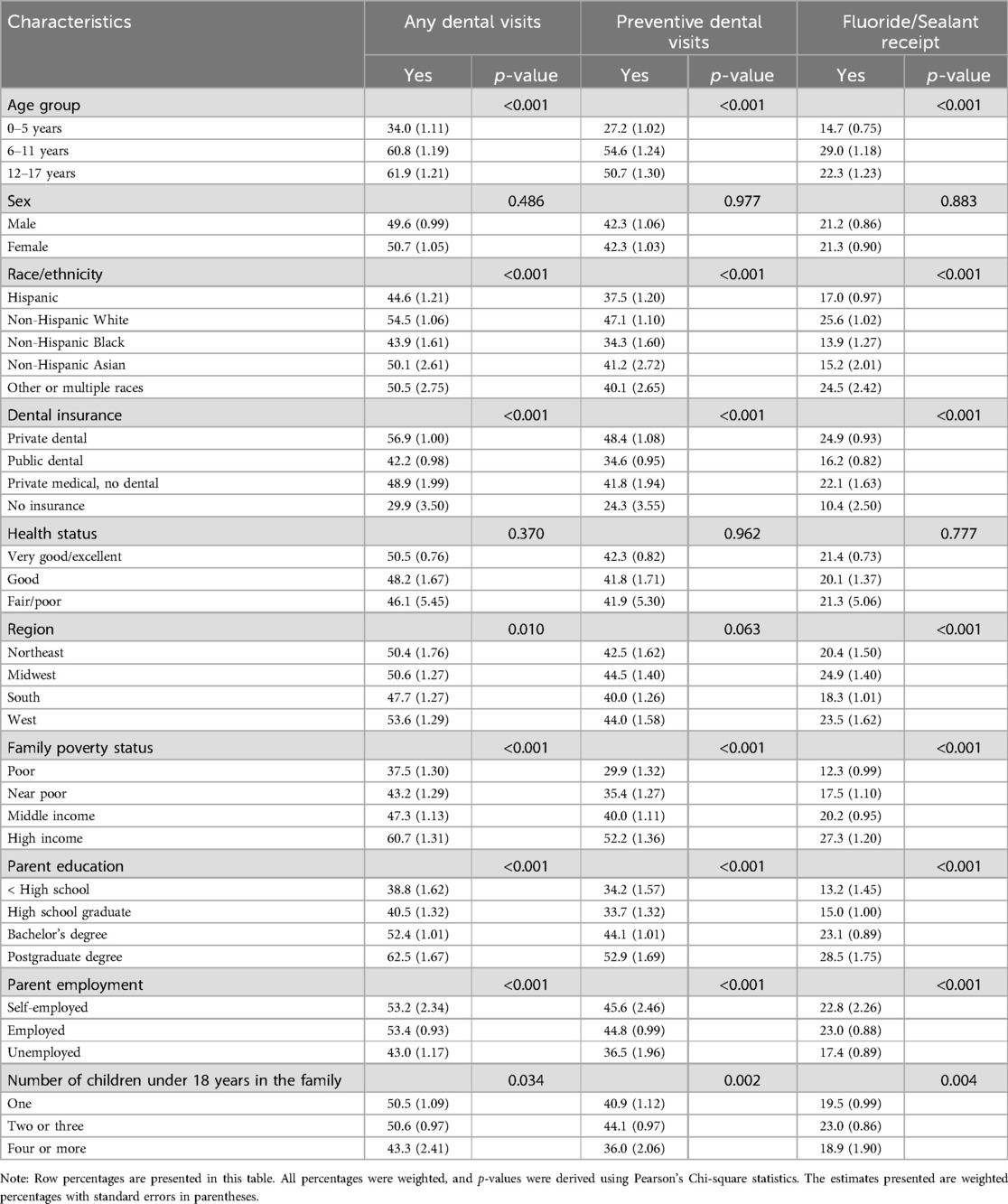
Table 2. Bivariate associations between children's dental utilization outcomes and included children, family, and parent characteristics, Medical Expenditure Panel Survey, 2017–2019.
Preventive dental visits
Among this study population, 42.3% of children had preventive dental visits in the past 12 months. When stratified, this outcome followed a similar pattern as “any dental visit” outcome. Preventive dental visits were highest among children whose parents had both medical and dental visits (62.1%) and lowest among those whose parents had no medical or dental visits (22.5%) (Figure 1).
Preventive dental visits were higher among children aged 6–11 (54.6%), NH White (47.1%), those from high-income families (52.2%), or who had a higher educated parent (52.9%) or employed parent (44.80%) compared to their counterparts (Table 2). Children with private dental insurance (48.4%), and those living in families with 2–3 children (44.1%) had a higher prevalence of preventive dental visits than others.
FV/sealant receipt
Only 21.2% had FV/sealant application in the past 12 months (Figure 1). FV/Sealant receipt was 32.3%, 21.4%, 15.9%, and 9.3% among children whose parents had both medical and dental visits, had only dental visits, had only medical visits, and had no medical or dental visits, respectively (Figure 1).
Among 6–17-year-olds, the percentage of FV/sealant receipt had a similar pattern: 38.8%, 27.0%, 18.9%, and 10.1% among children whose parents had both medical and dental visits, had dental visits only, had medical visits only, and had neither medical or dental visit, respectively (data not shown).
Among all children, the receipt of FV/sealant was lowest among 0–5-year children (14.7%), NH Black (13.9%), those living in poor income households (12.3%), those with unemployed parent (17.4%) or those whose parent had less than high school educated parents (13.2%). Children who had public insurance (16.2%) or children who had no insurance (10.4%), those who lived in households with four or more kids (18.9%), and those who lived in the South region (18.3%) had a lower percentage of FV/sealant receipt than their counterparts.
Multivariable logistic regression analysis
Any dental visits
Children's dental care use was strongly associated with their parent's medical and dental care use. Children whose parent had both medical and dental visits, had only dental visit or had only medical visit had 5.49 (95% CI: 4.64, 6.52), 3.77 (95% CI: 2.96, 4.78), and 1.51 (95% CI: 1.29, 1.77) times odds, respectively, of having dental visit than children whose parent had no medical and dental visit after controlling for all covariates (Table 3).
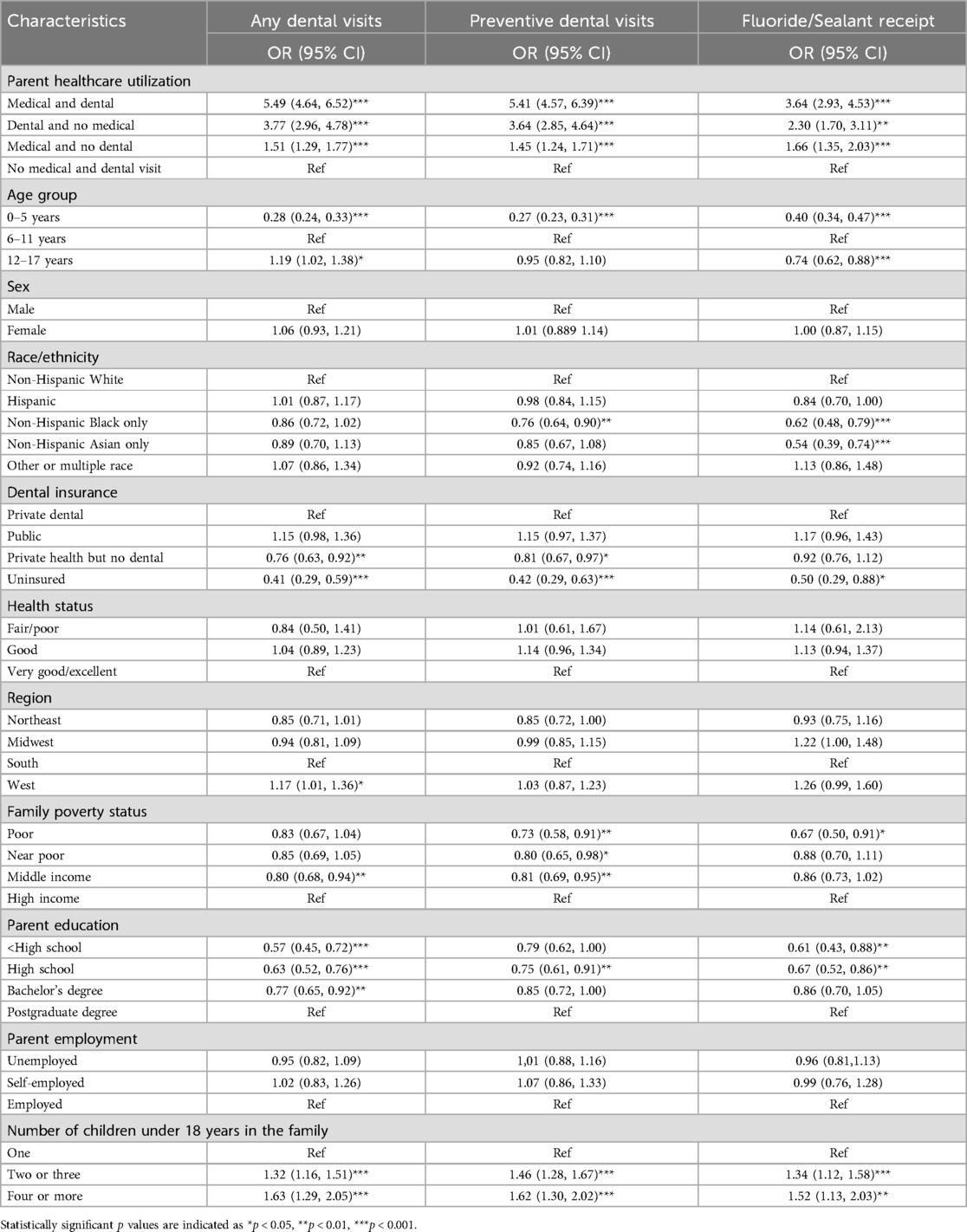
Table 3. Adjusted logistic regression model examining the association between parents’ healthcare utilization and children's dental services utilization outcomes, Medical Expenditure Panel Survey, 2017–2019.
In the adjusted model, we also found that younger children, those without dental insurance, those who had parents with a bachelor's or less education, were less likely to have a dental visit compared to their respective counterparts. Children residing in the West region and those living in households with one or more siblings had higher odds of dental visits than children living in the South region and those living in single-child households, respectively.
Preventive dental visits
Children whose parents had medical and dental visits had 5.41 times odds of having a preventive dental visit (95% CI: 4.57, 6.39) than children whose parents had no healthcare visits. Similarly, children whose parents had only a dental visit had 3.64 times the odds (95% CI: 2.85, 4.64), and those whose parents had only a medical visit had 1.45 times the odds (95% CI: 1.24, 1.71) of a preventive dental visit compared to children whose parents had no medical or dental visits (Table 3).
Results in the preventive visit model were similar to “any dental visit” model for other included covariates, with a few exceptions. NH Black children had 24% lower odds (aOR = 0.76, 95% CI 0.64, 0.90) of preventive dental visits than NH White children. Children living in middle-income, near poor or poor had lower odds of preventive visits than those living in high-income. Region, adolescent age group (12–17 years), less than high school and bachelor's degree were not found to be significantly associated with the preventive dental care use in the model.
FV/sealant receipt
The multivariable logistic regression model in Table 3 for sealant/FV receipt showed that children whose parents had both medical and dental visits, had only dental visits, or had only medical visits had 3.64 (95% CI: 2.93, 4.53), 2.30 (95% CI: 1.70, 3.11), and 1.66 (95% CI: 1.35, 2.03) times odds of FV/sealant receipt compared to children whose parents had no medical or dental visit (Table 3). Receipt of FV/sealant was lower among 0–5- and 12–17-year-old children compared to 6–11-year-olds. NH Black, NH Asian children, those who had parents with high school or less education, those who lived in poor-income households, and those who were uninsured had lower odds of FV/sealant receipt. Children living in families with two or more children had higher odds of FV/sealant receipt.
The sensitivity analysis for sealant/FV receipt among 6–17-year-olds showed results in a similar direction and stronger magnitude than among 0–17-year-olds for all variables (Supplementary Appendix Table 1).
Discussion
During 2017–2019, among 0–17-year-old children, one in two (50.1%) had a dental visit, 42.3% had a preventive dental visit, and only 21.2% received an FV/sealant application. Nearly 85% of children who had any dental visit had received preventive services (42.3%). Still, only half of those who received preventive services received FV/sealant (21.2%), which varied by parent healthcare use. Dental visit, preventive dental visit, and sealant/FV application among children whose parent had both Medical or dental visits were 9.5–10.9 percentage points, 16.4–31.7 percentage points, and 23.0–41.0percentage points higher compared to children whose parents only had a dental visit, had only a medical visit or had no medical or dental visit, respectively in the unadjusted data. Adjusted regression models showed similar results with nearly 3–5 times the odds of any dental visit, preventive visit, and sealant/FV receipt among children whose parents had both medical and dental visits, 1.8–2.8 times the odds among those whose parents had dental visit only and 1.3–1.5 times the odds among those whose parents had medical visit only compared to children whose parents had no dental or medical visits. The data finding supports our dose-response hypothesis for all outcomes.
Among our study population, 19% of parents did not have dental or medical visits in the past 12 months, and more than 1/3rd had a medical visit but not a dental visit. Given the positive association between parent's and child's dental visits and that more than 50% of parents did not have a dental visit in the past 12 months, it is necessary to improve parent's utilization of dental care, not only to support their oral health but also to improve dental care use among their children, especially for preventive care and evidence-based dental services. Sealants and fluoride varnish are proven effective in arresting and preventing caries (7, 13) and reducing the burden of dental caries in the long term. The improvement in preventive care and FV/sealant use among children whose parents had dental care use was nearly twice or more compared to children whose parents had no dental and medical care use, showing evidence of parents' role in influencing their child's preventive dental care use.
One way to support dental care utilization among adults is to provide coverage through Medicaid. Many adults lack dental insurance, and cost remains a prime barrier to dental care access and utilization (26). Several states have expanded dental coverage in the past few years, but many still do not cover dental services beyond emergency services (27). A study found a 5-percentage-point reduction in the prevalence of untreated caries among children after Medicaid-enrolled adults had access to dental coverage for at least one year (28).
We found that parents' medical care use alone was also strongly associated with children's dental care use. One explanation for this could be the increased awareness and knowledge among parents who seek health care. These parents may be better able to navigate health systems and prioritize their children's health, including oral health, due to their exposure to the health system. To further support parents in investing in their child's oral health, discussing oral health at regular adult medical visits could be valuable. Primary care providers can conduct oral health screening, provide fluoride varnish, and refer young children to a dentist (29), but this is not a practice during adult visits. Furthermore, it's important to note that parents are role models for children and can inculcate healthy behaviors and knowledge in the family unit, and thus, children may adopt similar behaviors as they grow.
Additional findings show that receipt of FV/sealants was lower among 0–5-year-olds and 12–17-year-olds compared to 6–11-year-olds. In the 0–5 age group, FV mainly drives the results as these children do not have permanent molars that are eligible for sealants. The sensitivity analysis showed that 12–17-year-olds, a group eligible for both FV and sealants, also had lower odds of FV/sealant receipt compared to 6–11-year-olds. Molars are the most susceptible teeth for dental caries (30). Sealants are typically recommended for permanent first and 2nd molars (6 years of age and above), and fluoride can be applied since the first tooth erupts (6 months of age and above). Our findings highlight the need to target and improve evidence-based oral health services delivery to both younger and older age groups while maintaining the oral health of 6–11-year-olds. School oral health programs are effective community oral health programs that can deliver FV and sealants to elementary school-age children who otherwise would not receive them. Still, these programs are not available to all and are uncommon among higher grades and in the preschool/Head Start population. Expanding these programs and educating parents and children about the benefits of preventive oral health services could help to improve oral health among these age groups. Additionally, increasing the delivery of FV among young children by primary care providers could be another way to increase the utilization of effective oral health services.
In our study, we found that the FV/Sealant receipt was lower among NH Asian and NH Black children compared to NH White children, uninsured children, and children whose parents had high school or less education compared to their counterparts. These findings concur with the published literature (24). However, our study found that children with public insurance were not significantly different from private insured children in having any dental visit, preventive dental visit and FV/Sealant receipt in the adjusted analysis. This is an encouraging finding suggesting improved oral health and health equity among children with public insurance. One of the potential reasons for these findings may be the use of sealant and dental care use measures as national health objectives and the endorsement of oral evaluation, topical fluoride, and sealant receipt in the CMS child core set measures and by the National Quality Forum (11, 31).
We also found that families with more than one child used any dental care, preventive dental care, and received FV/sealant more frequently than those with only one child. One explanation for this finding may be the older child's oral health experience and familiarity with the health system, which may encourage timely and preventive oral health use and maintenance of good oral health.
To our knowledge, this is the first study investigating parents' healthcare use and its connection with their child's dental care use and quantifying the influence of parents' combined use of medical and dental care on their child's dental visit and preventive oral health service use. However, some limitations should be acknowledged. As this is a cross-sectional study, we do not have information on the timing of parent's and children's healthcare visits and cannot ascertain temporality or causality. Although MEPS is the best national data available to study healthcare utilization and has a robust panel design, the dental services used for children are reported by adult respondents and may suffer from reporting errors or bias. Although we controlled for several covariates, there may be some unmeasured confounders such as cultural beliefs or trust that could influence the results. Future studies should examine ways to improve dental care use among adults, identify reasons for differences in receiving preventive care services among children, and investigate ways to improve the delivery of these services in all age groups.
Conclusions
This study provides estimates of dental utilization among children and its relationship with parents' healthcare use using robust MEPS data. Children's oral health utilization is strongly linked with parent's healthcare use and has a dose-response relationship. Although 2 out of 5 reported receipt of preventive services, only 1 in 5 children received evidence-based preventive services, including sealants or fluoride varnish, and there was a 3–5-fold difference in these dental care use outcomes based on parents' healthcare use. Oral health utilization among children remains low, especially for evidence-based preventive services. The information from this study suggests that improving healthcare use among parents can have important implications for children's dental care use.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://meps.ahrq.gov/mepsweb/data_stats/download_data_files.
Ethics statement
The Institutional Review Board (IRB) of the researchers' institutions recognize that the analysis of de-identified, publicly available data does not constitute human subjects research as defined in federal regulations, and as such does not require IRB review.
Author contributions
SN: Conceptualization, Investigation, Methodology, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing. RL: Data curation, Formal analysis, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
SN is supported by the National Institute of Dental and Craniofacial Research of the National Institutes of Health under the award number K08DE032443. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/froh.2025.1541045/full#supplementary-material
References
1. Centers for Disease Control and Prevention. Oral Health Surveillance Report: Trends in Dental Caries and Sealants, Tooth Retention, and Edentulism, United States: 1999–2004 to 2011–2016. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services (2019).
2. Claiborne DM, Kelekar U, Shepherd JG, Naavaal S. Emergency department use for nontraumatic dental conditions among children and adolescents: NEDS 2014–2015. Community Dent Oral Epidemiol. (2021) 49(6):594–601. doi: 10.1111/cdoe.12631
3. Rebelo MAB, Rebelo Vieira JM, Pereira JV, Quadros LN, Vettore MV. Does oral health influence school performance and school attendance? A systematic review and meta-analysis. Int J Paediatr Dent. (2018) 29(2):138–48. doi: 10.1111/ipd.12441
4. Wei L, Griffin SO, Robison VA. Disparities in receipt of preventive dental services in children from low-income families. Am J Prev Med. (2018) 55(3):e53–60. doi: 10.1016/j.amepre.2018.04.039
5. Griffin SO, Wei L, Gooch BF, Weno K, Espinoza L. Vital signs: dental sealant use and untreated tooth decay among U.S. school-aged children. MMWR Morb Mortal Wkly Rep. (2016) 65(41):1141–5. doi: 10.15585/mmwr.mm6541e1
6. Naavaal S, Kelekar U. School hours lost due to acute/unplanned dental care. Health Behav Policy Rev. (2018) 5(2):66–73. doi: 10.14485/HBPR.5.2.7
7. Griffin S, Naavaal S, Scherrer C, Griffin PM, Harris K, Chattopadhyay S. School-based dental sealant programs prevent cavities and are cost-effective. Health Aff (Millwood). (2016) 35(12):2233–40. doi: 10.1377/hlthaff.2016.0839
8. Scherrer C, Naavaal S, Lin M, Griffin SO. COVID-19 pandemic impact on US childhood caries and potential mitigation. J Dent Res. (2022) 101(10):1147–54. doi: 10.1177/00220345221090183
9. Wright JT, Crall JJ, Fontana M, Gillette EJ, Nový BB, Dhar V, et al. Evidence-based clinical practice guideline for the use of pit-and-fissure sealants: a report of the American Dental Association and the American Academy of Pediatric Dentistry. J Am Dent Assoc. (2016) 147(8):672–82.e12. doi: 10.1016/j.adaj.2016.06.001
10. Community Preventive Services Task Force. Preventing Dental Caries: School-Based Dental Sealant Delivery Programs. Atlanta: US Department of Health and Human Services, Community Preventive Service Task Force (2016).
11. Department of Health and Human Services. Healthy people 2030-Oral condition. Office of Disease Prevention and Health Promotion.
12. Naavaal S, Tatro K, Scherrer C. Second molar sealants among US adolescents and their association with select sociodemographic factors and first molar sealants: a cross-sectional study using National Health and Nutrition Examination Survey data. J Am Dent Assoc. (2024) 155(10):836–44. doi: 10.1016/j.adaj.2024.07.010
13. Marinho VC, Worthington HV, Walsh T, Clarkson JE. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. (2013) 2013(7):Cd002279. doi: 10.1002/14651858.CD002279.pub2
14. Clark MB, Slayton RL. Fluoride use in caries prevention in the primary care setting. Pediatrics. (2014) 134(3):626–33. doi: 10.1542/peds.2014-1699
15. Moyer VA. Prevention of dental caries in children from birth through age 5 years: US preventive services task force recommendation statement. Pediatrics. (2014) 133(6):1102–11. doi: 10.1542/peds.2014-0483
16. Griffin SO, Barker LK, Wei L, Li CH, Albuquerque MS, Gooch BF, et al. Use of dental care and effective preventive services in preventing tooth decay among U.S. children and adolescents–Medical Expenditure Panel Survey, United States, 2003–2009 and National Health and Nutrition Examination Survey, United States, 2005–2010. MMWR Suppl. (2014) 63(2):54–60.25208259
17. Schor EL. Family pediatrics: report of the task force on the family. Pediatrics. (2003) 111(6 Pt 2):1541–71. doi: 10.1542/peds.111.S2.1541
18. Institute of Medicine Committee on the Consequences of Uninsurance. Care Without Coverage: Too Little, Too Late. Washington, DC: National Academies Press (US) (2002).
19. Angier H, Kaufmann J, Heintzman J, O'Malley J, Moreno L, Giebultowicz S, et al. Association of parent preventive care with their child’s recommended well-child visits. Acad Pediatr. (2022) 22(8):1422–8. doi: 10.1016/j.acap.2022.03.019
20. Goedken AM, Urmie JM, Polgreen LA. Factors related to receipt of well-child visits in insured children. Matern Child Health J. (2014) 18(3):744–54. doi: 10.1007/s10995-013-1301-2
21. Minkovitz CS, O'Campo PJ, Chen YH, Grason HA. Associations between maternal and child health status and patterns of medical care use. Ambul Pediatr. (2002) 2(2):85–92. doi: 10.1367/1539-4409(2002)002%3C0085:ABMACH%3E2.0.CO;2
22. Kornides M, Head KJ, Feemster K, Zimet GD, Panozzo CA. Associations between HPV vaccination among women and their 11–14-year-old children. Hum Vaccin Immunother. (2019) 15(7-8):1824–30. doi: 10.1080/21645515.2019.1625642
23. Edelstein BL, Rubin MS, Clouston SAP, Reusch C. Children’s dental service use reflects their parents’ dental service experience and insurance. J Am Dent Assoc. (2020) 151(12):935–43. doi: 10.1016/j.adaj.2020.08.018
24. Isong IA, Zuckerman KE, Rao SR, Kuhlthau KA, Winickoff JP, Perrin JM. Association between parents’ and children’s use of oral health services. Pediatrics. (2010) 125(3):502–8. doi: 10.1542/peds.2009-1417
25. Chowdhury SR, Machlin SR, Gwet KL. Sample Designs of the Medical Expenditure Panel Survey Household Component, 1996–2006 and 2007–2016. Methodology Report #33. Rockville, MD: Agency for Healthcare Research and Quality (2019).
26. CareQuest Institute of Oral health. Uninsured and in Need: 68.5 Million Lack Dental Insurance, More May Be Coming. Boston, MA: CareQuest-CareQuest Institute for Oral Health, Inc (2023).
27. Center for Health Care Strategies. Medicaid adult dental benefits: an overview (2019). Available at: https://www.chcs.org/media/Adult-Oral-Health-Fact-Sheet_091519.pdf (Accessed February 27, 2025).
28. Lipton BJ, Finlayson TL, Decker SL, Manski RJ, Yang M. The association between medicaid adult dental coverage and children’s oral health. Health Aff (Millwood). (2021) 40(11):1731–9. doi: 10.1377/hlthaff.2021.01135
29. Okah AY, Reddy M, Williams K, Talib N, Onikul R. Promoting oral health in primary care—closing the dental referral loop. Pediatrics. (2019) 144(2_MeetingAbstract):726. doi: 10.1542/peds.144.2MA8.726
30. Griffin SO, Wei L, Naavaal S, Fleming E. The contribution of different permanent tooth types to untreated caries: implications for public health surveillance and prevention. J Am Dent Assoc. (2021) 152(4):269–76.e2. doi: 10.1016/j.adaj.2021.01.003
Keywords: oral health utilization, preventive dental care use, children and adolescents, parent health behavior, Medical Expenditure Panel Survey (MEPS)
Citation: Naavaal S and Lamsal R (2025) Understanding the relationship between children's oral health utilization and parent's use of healthcare services. Front. Oral Health 6:1541045. doi: 10.3389/froh.2025.1541045
Received: 13 December 2024; Accepted: 29 April 2025;
Published: 13 May 2025.
Edited by:
Rahul Siram Naidu, The University of the West Indies St. Augustine, Trinidad and TobagoReviewed by:
Augusto R. Elias Boneta, University of Puerto Rico, Puerto RicoTumader Khouja, University of Florida, United States
Copyright: © 2025 Naavaal and Lamsal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shillpa Naavaal, bmFhdmFhbHNAdmN1LmVkdQ==
 Shillpa Naavaal
Shillpa Naavaal Rashmi Lamsal
Rashmi Lamsal