- 1Missouri School of Dentistry and Oral Health, A.T. Still University, Kirksville, MO, United States
- 2Department of Periodontology and Community Dentistry, University of Ibadan and University College Hospital, Ibadan, Nigeria
- 3Fellow, Consortium for Advanced Research Training in Africa (CARTA), Nairobi, Kenya
- 4Department of Child Oral Health, University of Ibadan and University College Hospital, Ibadan, Nigeria
- 5Department of Preventive Dentistry, Faculty of Dentistry, Lagos State University College of Medicine, Lagos, Nigeria
- 6Department of Oral Diagnostic Sciences, Faculty of Dentistry, Bayero University Kano, Kano, Nigeria
- 7Department of Oral Diagnostic Sciences, Aminu Kano Teaching Hospital, Kano, Nigeria
- 8Department of Oral Pathology, Radiology and Medicine, College of Dentistry, University of Iowa, Iowa City, IA, United States
- 9Iowa Institute for Oral Health Research, University of Iowa, Iowa City, IA, United States
- 10School of Public Health, University of Nevada, Reno, NV, United States
- 11Department of Oral and Maxillofacial Surgery, Lagos University Teaching Hospital, Lagos, Nigeria
- 12Department of Restorative Dentistry, Lagos University Teaching Hospital, Lagos, Nigeria
- 13Department of Preventive Dentistry, Aminu Kano Teaching Hospital, Kano, Nigeria
- 14Faculty of Dentistry, Bayero University, Kano, Nigeria
- 15Colgate-Palmolive Company, Piscataway, NJ, United States
- 16National Dental Association Foundation, Washington, DC, United States
- 17Division of Pediatric Surgery, Department of Surgery, University of Ibadan and University College Hospital, Ibadan, Nigeria
Introduction: Oral health disparities in Nigeria highlight the need to integrate basic oral health into Primary Health Care (PHC). Project OHE-NCHeW (Oral Health Education for Nurses and Community Health Workers) was developed to train PHC workers in providing basic oral health care, education, and referrals in underserved communities. This study explored the impact of the training program on participants' knowledge, referral practices, and patient outcomes, and gathered feedback to optimize the program for future implementation.
Methods: Using a qualitative phenomenological approach, five focus group discussions (FGDs) were conducted with participants to gather insights on knowledge acquisition, changes in referral practices, and barriers or facilitators to implementation. Audio recordings were transcribed verbatim and analyzed thematically using the CREATIVE framework. Additional feedback from trainers and observed patient impact were also considered.
Results: The trained PHC workers reported enhanced knowledge and confidence, resulting in improved patient education and referrals. Patients also noted better oral health literacy and increased trust in dental referrals. Facilitators viewed the program as valuable and feasible, emphasizing the importance of ongoing training, resource allocation, and policy integration to maintain the program's impact. Key barriers included insufficient resources, lack of supervision, and cultural beliefs.
Discussion: The pilot training enhanced PHC worker capacity and was positively perceived by trainers. Patients reportedly responded favorably, indicating potential impact. However, addressing identified systemic and resource barriers is crucial for sustainable integration. This study offers multi-perspective insights for optimizing oral health integration within PHC in similar settings.
Introduction
Oral diseases represent a significant global public health burden, impacting billions of individuals and contributing to substantial morbidity, pain, and economic costs (1). In Nigeria, Africa's most populous nation, oral health disparities are particularly acute, driven by factors including a severe shortage of dentists (estimated dentist-to-population ratio of 1:44,830 vs. WHO recommended 1:5,000) and their uneven distribution, with the majority concentrated in urban centers (2–4). This leaves vast populations, particularly in rural and underserved areas, with limited or no access to essential oral healthcare services (5).
Integrating oral health into Primary Health Care (PHC) is widely recognized as a cost-effective strategy to expand access to basic oral health services, promote prevention, and advance health equity, as advocated by the WHO (6–8). The existing PHC workforce in Nigeria, comprising nurses, community health workers (CHWs), and midwives, is well-positioned to deliver basic oral health interventions due to their reach within communities (9). However, previous studies in Nigeria and other settings have consistently reported inadequate oral health knowledge among these healthcare cadres (10–12) and have highlighted the need for structured training to equip them with the necessary skills and confidence (9, 13). Despite a willingness among some PHC workers to incorporate oral health into their duties, systemic barriers and a lack of adequate preparation remain challenges (11, 14, 15). To address this critical gap and strengthen the capacity of the Nigerian PHC workforce in oral health, Project OHE-NCHeW (Oral Health Education for Nurses and Community Health Workers) was developed (16). This comprehensive initiative designed a standardized, evidence-based curriculum and piloted its delivery among nurses and CHWs in three diverse states across two geopolitical zones in Nigeria. Unlike some previous, smaller-scale efforts, Project OHE-NCHeW aimed for a more standardized approach to facilitate broader implementation and evaluation (16).
To evaluate the sustainable potential of the Project OHE-NCHeW model for training PHC workers, it is vital to explore the views of major stakeholders about the training process. Moreover, stakeholders play critical roles in the success of educational programs (17, 18). Therefore, this specific manuscript presents a focused qualitative evaluation embedded within the Project OHE-NCHeW pilot phase. The primary objective of this study was to explore in-depth the experiences and perceptions of trained nurses and CHWs regarding their participation in the pilot training, their application of acquired knowledge and skills in practice, and the perceived barriers and facilitators encountered during the implementation of basic oral health interventions in their respective PHC settings. This qualitative exploration also incorporated feedback from trainers on the program's delivery and captured reported observations from patients regarding their encounter with trained PHC workers, providing a multi-stakeholder perspective on the feasibility and initial impact of integrating oral health through this training model. The findings from this study contribute crucial qualitative data to inform the refinement and future scaling of oral health training initiatives for PHC workers in Nigeria and similar low-resource contexts globally.
Materials and methods
Study design and setting
This study utilized a qualitative, phenomenological approach to evaluate the experiences and perceptions of the Nurses and CHWs who participated in the pilot training—Project OHE-NCHeW, in Lagos, Ibadan, and Kano, Nigeria, following project completion. We also reported on the experiences of the facilitators of the training and patients at the PHCs who benefited from the outcomes of the training. These locations were strategically selected due to their geographic, cultural, and socio-economic diversity, which provides valuable insights into the unique challenges faced by PHC workers across the country. Lagos, Nigeria's largest urban center, represents a metropolitan population with significant healthcare demand (19). Ibadan, the second-largest city in Nigeria, offers a mix of urban and peri-urban demographics, which provides a distinct perspective on regional healthcare access (20–22). Kano, in northern Nigeria, is characterized by its cultural richness and the need for tailored health interventions (23–25).
The pilot study employed a quasi-experimental design (pre- and post-with a non-equivalent control group) to assess the impact of the 5-day oral health training delivered on the knowledge level and referral practices of the participants (February to May 2024) (16). After completing the training, participants were asked to incorporate oral health education into their routine health promotion activities at their respective PHCs over 3 months. Full details of the training content and implementation process have been reported elsewhere (16). This study explores the perspectives of CHWs and nurses regarding the influence of the OHE-NCHeW training program on referral practices, knowledge dissemination, and clinical application using a qualitative approach. Additionally, insights were obtained from stakeholders and trainers to inform the refinement of training content and referral pathways. Patient interviews were also conducted across study sites to evaluate the perceived impact of the program from the service users' perspective, thereby contributing to a comprehensive assessment of program implementation and areas for optimization.
Participants
The sample of trainees (nurses and CHWs) was drawn from a predefined “sampling frame” of all 60 participants (20 per study site) who participated in the 5-day pilot training (16). This virtual platform was created during the training to support and facilitate resource sharing among the trainers and research participants. From this group, 34 participants (about of the trained PHC workers) were randomly selected and took part in the FGDs. The eligibility criteria and complete description of the participant sampling have been described elsewhere (16).
Additionally, six members of the study team who were involved in implementing Project OHE-NCHEW were invited to participate in an unstructured interview. Thirty out of the 503 patients who were referred to the dental centers from the PHCs where the trainees worked and conducted oral health promotion activities were also engaged. The assessment of patients' perspectives aimed to understand how well the training was translated into practice and how it affected patient experiences and outcomes.
Data collection
Data were collected using multiple qualitative methods to gain diverse perspectives on the pilot training. Course evaluation forms were administered immediately after the training to assess its impact and participant satisfaction (26). Completion of the evaluation form was voluntary and anonymous. For this manuscript, data derived from the open-ended questions on this form were utilized to provide qualitative insights into participants' experiences and suggestions (see Supplementary Material).
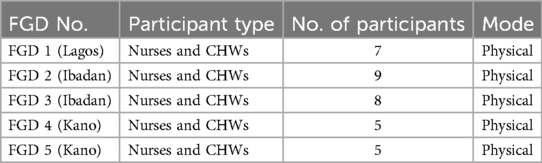
A total of five focus group discussions (FGDs) were conducted with the trainees at the host tertiary healthcare center, at the same site where the initial training occurred, to facilitate participant convenience and ensure robust participation (Table 1). These discussions included one in Lagos, two in Ibadan, and two in Kano, with 5–9 participants per group. Three licensed dentists facilitated the FGDs, consisting of two males and one female (AO, AO, and LFB), who had extensive research experience and were members of the study team. None of the facilitators had prior relationships with the participants or any conflicting interests or biases. The participants were assigned identification numbers to ensure anonymity and were compensated with a token equivalent to ∼$10 to cover transportation expenses to the interview site.
Each FGD lasted approximately 2 h and was audio-recorded with participants' consent. The discussions were guided by semi-structured interview guides, which were developed collaboratively by the research team based on the training objectives and a review of relevant literature (see Supplementary Material). The guides were tailored to assess the perceived impact of the training, identify areas for improvement, and explore the feasibility and sustainability of integrating oral health promotion into routine maternal and child health (MCH) services. Versions of the guides were adapted for linguistic and cultural relevance and translated into local languages (Hausa, Yoruba, and Fulfulde) to ensure participant comprehension and engagement. Complex terms were summarized and interpreted in local languages during the sessions. Although audio recordings were made for transcription and analysis, no field notes were taken during the discussions.
Additionally, an unstructured interview was conducted with six facilitators who delivered the pilot training immediately after the training sessions and was audio-recorded. The face-to-face interview, guided by a set of open-ended questions (see Supplementary Material), was largely conversational and aimed to capture the facilitators' experiences, challenges, and perspectives on the program's delivery and perceived impact.
Lastly, initial feedback was sought from a sample of patients who benefited from oral health promotion activities and required referrals following their interaction with trained PHC workers. This feedback was collected through phone calls made by trained project staff using a standardized phone script (see Supplementary Material). These calls aimed to capture patients' immediate perceptions of the oral health information or referrals received. While the script included some closed-ended questions, the primary goal of this evaluation was to gather qualitative insights, and the data collection method was not designed for rigorous quantitative analysis of patient outcomes.
Data analysis
Qualitative data analysis was conducted separately for each distinct data source. The qualitative data collected from the open-ended questions on the course evaluation forms were analyzed using a descriptive approach to summarize frequently mentioned comments and suggestions.
The transcripts obtained from the FGD audio recordings were transcribed verbatim and checked by two members of the research team. Analysis was done using the CREATIVE approach, adapted from Pitney and Parker (27). This framework involves the following steps: Considering the research questions and study purpose; Reading through transcripts to develop a comprehensive understanding of the data; Examining the data for significant insights related to the research questions; Assigning descriptive labels to data units to capture their essence; Thematizing the data to organize recurring patterns; Interpreting the themes in relation to the study's objectives; Verifying the findings to ensure accuracy and credibility; and Engaging in the writing process to present the analyzed findings systematically (27). Discrepancies in coding were resolved through team discussions (28). Trustworthiness was enhanced through prolonged engagement in the study settings to understand the context and participants, and comprehensive descriptions to provide detailed accounts that support the transferability of findings (29).
The audio recording of the unstructured interview with the trainers was transcribed verbatim. The transcripts were then reviewed to identify recurring perspectives and significant insights shared by the facilitators regarding their training delivery experience. Responses collected via the patient feedback phone script were reviewed to identify recurring perceptions and notable points from patients. Findings derived from the analysis of each of these data sources (PHC worker FGDs, trainer interviews, and patient feedback) were analyzed and are reported separately in the Results section to present the distinct perspectives of each stakeholder group on the Project OHE-NCHeW pilot training and its initial impact.
Ethical considerations
Prior to their involvement in the qualitative study, informed consent was obtained from all participants, including trainers, trainees (nurses and CHWs), and patients. Ethical approval for the study was obtained from the Institutional Review Boards at the University of Iowa (IRB-01/202312517); the University of Ibadan/University College Hospital, Ibadan (UI/EC/23/0724); the University of Lagos/Lagos University Teaching Hospital, Lagos (ADM/DSCST/HREC/APP/6454) and Bayero University Kano/Aminu Kano Teaching Hospital, Kano (NHREC/28/01/2020/AKTH/EC/3739), Nigeria.
Results
Summary of the course evaluation responses
Post-course evaluation feedback from trainees highlighted the training's strengths and areas for improvement. Participants appreciated the training's detailed, practical content, the trainers' expertise, and the interactive format featuring Q&A sessions and outcome-focused quizzes. They praised the simplicity and clarity of the materials, the availability of reference modules, and the effective communication methods.
To enhance future sessions, participants suggested more frequent training (quarterly or biannually), expanding the program to include traditional birth attendants (TBAs), voluntary health workers, nursing administrators, and community health officers. They recommended incorporating practical demonstrations at dental clinics, offering residential training formats, increasing the use of teaching aids, and extending the curriculum to cover broader aspects of dental care. Participants also emphasized raising program awareness via social media and expanding the program's reach into communities. This feedback affirms the program's impact while identifying opportunities for refinement to maximize its reach and effectiveness.
Focus group discussion with trainees
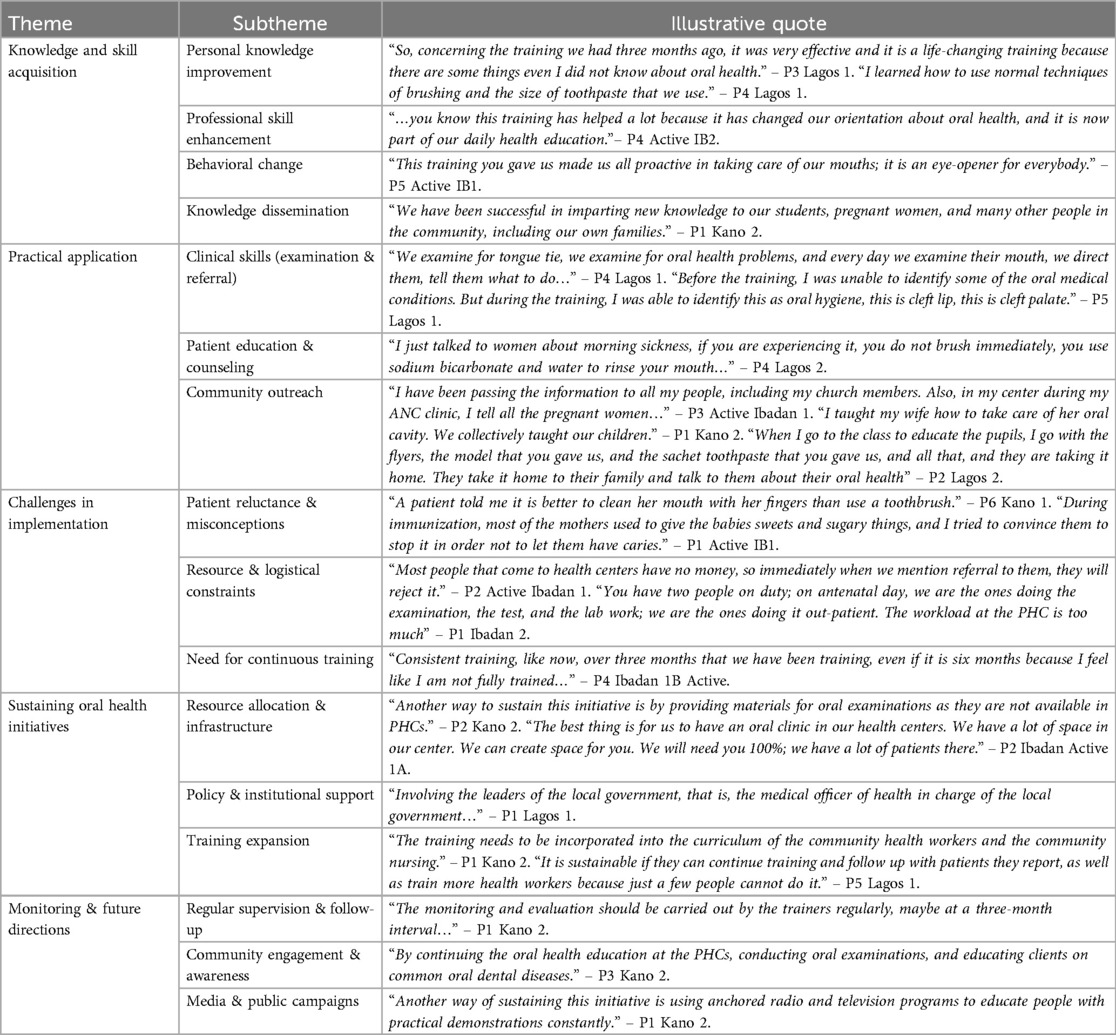
We identified five themes that summarized the participants' perspectives regarding the recently completed training (Table 2); (1) Knowledge and Skill Acquisition, demonstrating improved personal and professional understanding of oral health; (2) Practical Application, showcasing real-world implementation in clinical and community settings; (3) Challenges in Implementation, identifying barriers such as patient misconceptions and resource limitations; (4) Sustaining Oral Health Initiatives, offering recommendations for program sustainability; and (5) Monitoring and Future Directions, emphasizing the need for continued evaluation and community engagement. The table below presents these themes alongside derived subthemes and illustrative quotes, providing a structured overview of participants' experiences and insights.
Feedback from trainers
Overall, trainers described their experiences as positive, highlighting high trainee responsiveness and eagerness to apply their knowledge in practice. Speaker P2 noted, “The interactiveness of the students; the whole point of these lectures is to see that not only were they interested, but they were also interested in coming and using it in interactions with their clients.” Trainers emphasized the value of pre-implementation activities, such as tailoring content to the local context through culturally relevant examples and adapting materials from the WHO manual. Speaker P3 explained, “The first thing was to relate the topic to what they have done initially and what they have on the ground in their centers. So, based on that, we are able to tailor the lecture to suit what they are already doing.”
Effective elements of the program included interactive sessions, local songs, familiar scenarios, and visual teaching aids. Speaker P2 shared, “The activities, I think the activities…and even the pictures. A lot of the modules had pictures so that they could see.” Speaker P4 added, “I think one of the improvements I noticed was relating those pictures to cases that they had seen before, and they had most likely mismanaged.” Challenges included the need for more visual aids and practical tools, as mentioned by Speaker P1: “I felt I needed more pictures so that they could see the cases more clearly. To overcome this, we downloaded pictures and shared them with the participants using mobile tablets.” Adapting to local challenges, such as finding alternatives for infant oral hygiene, demonstrated the importance of context-specific solutions.
Trainers observed significant impacts of the program, including improvements in trainees' oral health practices and their ability to link lessons across modules. Speaker P3 highlighted the importance of follow-up support, suggesting, “If they do not have the support of their direct superiors, there is little they cannot actually do on their own.” Proposed enhancements included creating a WhatsApp group for reminders and incorporating oral health into the broader healthcare system to address staffing shortages.
Assessment of oral health education impact on patients attending PHCs
Patient perspectives on the oral health education and referrals provided by the trained PHC workers were gathered through follow-up phone calls. Most patients expressed satisfaction with PHC workers, reporting they received clear and comprehensive information about visiting dental centers. This contributed to high referral follow-through, reflecting the training's effectiveness. Patients overwhelmingly described the information provided by PHC workers as clear or very clear, which enhanced their understanding of what to expect at dental centers and increased trust. The principal themes and illustrative points derived from this patient feedback are presented in Table 3.
Discussion
This qualitative study provides valuable insights into the feasibility and challenges of integrating basic oral health services into Primary Health Care (PHC) in Nigeria through the pilot implementation of the Project OHE-NCHeW training program. The study focused on task shifting, a leading strategy where tasks are transferred from highly qualified healthcare professionals to CHWs and nurses to address healthcare worker shortages and improve access to services (30). By capturing multi-stakeholder perspectives from trained PHC workers, trainers, and initial patient feedback, our findings highlight the program's immediate successes, the persistent systemic barriers, and critical considerations for future scale-up and sustainability.
Enhanced knowledge acquisition and practical application at the PHC level
Study findings indicate that the Project OHE-NCHeW training effectively enhanced the oral health knowledge and skills of participating nurses and CHWs. PHC workers reported a significant shift in their orientation towards oral health, describing the training as an “eye-opener” and leading to behavioral changes in their practices. While the training was for all participating PHC workers, some of the most prominent examples of practical application emerged from their work with expectant mothers and young children. This aligns with previous studies demonstrating that targeted training can significantly improve the oral health knowledge of non-dental healthcare professionals, especially in low-resource settings where dental professionals are scarce (15, 31–36). The acquisition of skills, such as identifying oral conditions and providing basic oral hygiene education, empowered these workers to actively integrate oral health into their routine activities. This newfound awareness was also extended to community outreach, with participants actively disseminating oral health information in markets, churches, and schools.
In some cases, trainees educated family members and church congregations, thereby amplifying the reach of the training beyond their immediate work environment. This direct application of acquired knowledge, evidenced by workers actively using flyers, models, and even personal examples in their education efforts, highlights the immense potential of a well-trained PHC workforce to bridge critical gaps in oral healthcare access, consistent with the World Health Organization's advocacy for oral health integration into PHC (7, 37). Oral health education programs for non-dental practitioners have been successful in many settings, improving confidence in examining the mouth (35, 38) and referring to oral health providers (36). The universally acknowledged contribution of PHC workers to healthcare is entrenched in policy statements and related research that recognize them as a key link between professional care providers, such as physicians and patients (36, 39, 40). The USAID Health Care Improvement Project suggests that CHWs should receive ongoing training every 6 months to develop new skills, reinforce pre-service training, and ensure prior skills are being properly practiced (41). Informing non-dental healthcare workers about the intersection of oral care with medicine and providing them with clear guidance on how they can protect and promote patients' oral health may facilitate consideration of oral health in their practice (35, 36).
Insights from trainers and patient experiences
The perspectives of the trainers further validated the program's design and delivery, with trainers perceiving the modules as valuable and feasible for PHC workers, which is crucial for successful program implementation (42, 43). Patient feedback, collected through phone calls, corroborated the effectiveness of the PHC workers' enhanced communication skills. Most patients reported receiving clear and comprehensive information, which enhanced their understanding and contributed to reported referral follow-through. This positive patient reception is critical, as patient understanding and acceptance are key determinants of health intervention success (44).
Persistent barriers to sustainable integration
Despite these successes, our study identified significant barriers to the sustained implementation of oral health services, mirroring challenges reported in similar initiatives in developing countries (45, 46). Financial constraints emerged as a significant deterrent for patients, who often could not afford transportation to referral centers or the fees associated with specialist dental care, echoing findings across the globe (47–49). Thus, integrating more affordable or subsidized dental services within PHCs could improve affordability and care access. Patient misconceptions and reluctance to adopt new practices also presented challenges (50–54). This highlights the broader challenges in altering patient attitudes toward preventive care, which should be a central focus for future health promotion interventions. Logistical challenges within the PHC settings, including staff shortages, heavy workloads, and insufficient basic resources, were frequently cited by PHC workers. These resource limitations are commonly reported obstacles to PHC strengthening in Nigeria and other low-income countries, impeding the effective integration of new services (55–58). Furthermore, negative past experiences (59, 60) and rural accessibility issues further hindered follow-up care. Thus, while the training program successfully improved patient education and referrals at PHCs, addressing structural barriers such as cost, accessibility, and patient perceptions will be essential for sustaining the program's impact.
Recommendations for sustaining and scaling oral health initiatives
The suggestions from PHC workers and patients offer a roadmap for optimizing the Project OHE-NCHeW model and similar future initiatives. Participants' recommendations for allocating dedicated resources for oral examinations at PHCs, establishing specialized oral clinics within existing PHC facilities, and simplifying referral processes are aligned with calls for strengthening PHC infrastructure and capacity (61–63) The emphasis on continuous training, workforce expansion to include other cadres like Traditional Birth Attendants (TBAs), and the integration of oral health into existing curricula are crucial for building a sustainable oral health workforce, a strategy supported by studies on task-shifting and health worker capacity building (4, 64, 65). Furthermore, suggestions for institutional support, policy integration, and robust monitoring and evaluation mechanisms highlight the critical role of health system governance and multi-sectoral collaboration for successful program sustainability (66, 67). The proposal for public awareness campaigns through various media and the provision of incentives for patients reflects strategies known to enhance patient engagement and uptake of health services in low-resource contexts (68, 69). Furthermore, a problematic referral system, characterized by feedback gaps and cumbersome processes, undermined the continuum of care, a barrier also documented in broader health system strengthening efforts (70, 71). This highlights the need for improved coordination between PHC and secondary care levels to ensure seamless patient journeys and maximize the impact of referrals. The need for continuous training and re-training, voiced by PHC workers who felt the initial training was insufficient to achieve complete competence, underscores the importance of ongoing professional development and supportive supervision for new skill adoption (72).
Strengths and limitations
A key strength of the training is its comprehensive and interactive approach. Participants consistently noted that the use of case studies, images, and quizzes helped reinforce their learning. Trainers effectively adapted the content to the local context, making the material more relatable and actionable. Additionally, the program's structure, which combines theoretical lessons with practical applications, enables trainees to develop a solid understanding of key oral health concepts. These strengths were further reflected in the participants' ability to apply their new knowledge to patient interactions and community education. Furthermore, unlike other studies, which focused predominantly on urban populations or PHC workers from only one state or subregion (15, 33), our sampling strategy enabled the recruitment of a more diverse geographic distribution of PHC workers from three states in Nigeria from both the northern and southwestern regions of the country. The inclusion of expanded modules, culturally relevant materials, and case scenarios also distinguishes this program from previous ones.
Our study's qualitative design, while providing rich, in-depth perspectives from multiple stakeholders, inherently limits the direct generalizability of findings beyond the specific pilot sites in Nigeria. The findings represent the perceptions of participants at a specific point in time, and long-term outcomes regarding sustained practice changes among PHC workers and direct patient health improvements were not within the scope of this qualitative evaluation. Furthermore, the patient feedback was collected via a convenience sample of phone calls, which might introduce selection bias. Future research should include quantitative measures of impact (e.g., changes in oral health status, referral completion rates), long-term follow-up, and explore the generalizability of these findings across diverse geographical and socio-economic contexts within Nigeria.
Implications for practice and policy
Health ministries and policymakers should consider allocating more resources for oral health training programs, especially in underserved areas. The program's success could be scaled up by leveraging trained PHC workers to train peers. Moreover, in light of the anticipated increase in awareness and oral health-seeking behavior from patients, resulting from the program, the current dental care financing mechanisms in low- and middle-income countries that inadequately shield the public from the economic burden of dental treatment should transition more, from out-of-pocket payments to prepayment and risk-pooling systems to better protect households from significant health expenses and reduce the financial strain of healthcare costs.
Conclusion
The Project OHE-NCHeW pilot training improved PHC workers' oral health knowledge and patient referrals. Despite positive feedback, systemic challenges—costs, resources, and referral gaps—must be addressed for long-term success. The multi-stakeholder insights gained from this qualitative evaluation provide actionable recommendations essential for optimizing the impact and scalability of oral health integration initiatives within Nigeria's broader public health framework, ultimately contributing to better oral health outcomes and overall well-being in underserved communities.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval for the study was obtained from the Institutional Review Boards at the University of Iowa (IRB-01/202312517); the University of Ibadan/University College Hospital, Ibadan (UI/EC/23/0724); the University of Lagos/Lagos University Teaching Hospital, Lagos (ADM/DSCST/HREC/APP/6454) and Bayero University Kano/Aminu Kano Teaching Hospital, Kano (NHREC/28/01/2020/AKTH/EC/3739), Nigeria. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AO: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing. FL: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing. OS: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing. OU: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing. AOy: Conceptualization, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. AA: Conceptualization, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. MO: Formal analysis, Writing – original draft, Writing – review & editing. OF: Project administration, Writing – review & editing. AW: Project administration, Writing – original draft, Writing – review & editing. AD: Project administration, Writing – original draft, Writing – review & editing. EI: Project administration, Writing – review & editing. Y-IA-K: Project administration, Writing – review & editing. IAden: Project administration, Writing – review & editing. AM: Project administration, Writing – review & editing. ABa: Project administration, Writing – review & editing. IAdet: Project administration, Writing – review & editing. KM: Project administration, Writing – review & editing. BS: Writing – review & editing. CD: Writing – review & editing. DH: Writing – review & editing. JB: Writing – review & editing. TL: Project administration, Writing – review & editing. ABu: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This pilot training was supported jointly by Colgate-Palmolive and the National Dental Association Foundation Grant ID 18748400 – L833500 PI, AO).
Conflict of interest
BS, CD, and DH are current employees of the Colgate-Palmolive Company.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) ABu, AB declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. Generative AI tools were used to assist with the manuscript outline and to improve grammar and statement structure. The intellectual content, analysis, and conclusions are entirely that of the authors.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/froh.2025.1597243/full#supplementary-material
References
1. Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, et al. Oral diseases: a global public health challenge. Lancet. (2019) 394(10194):249–60. doi: 10.1016/S0140-6736(19)31146-8
2. Ajao H. Oral health workforce planning in Nigeria. Otolaryngol Head Neck Surg. (2018) 4:1–6. doi: 10.24966/OHNS-010X/100018
3. Uguru N, Onwujekwe O, Ogu UU, Uguru C. Access to oral health care: a focus on dental caries treatment provision in Enugu Nigeria. BMC Oral Health. (2020) 20(1):1–13. doi: 10.1186/s12903-020-01135-1
4. Foláyan MO, Ishola AG, Bhayat A, El Tantawi M, Ndembi N. Strengthening health systems to tackle oral diseases in Africa: Africa centers for disease control and prevention’s role. Front Public Health. (2025) 13:1539805. doi: 10.3389/fpubh.2025.1539805
5. Adeniyi AA, Sofola OO, Kalliecharan RV. An appraisal of the oral health care system in Nigeria. Int Dent J. (2012) 62(6):292–300. doi: 10.1111/j.1875-595X.2012.00122.x
6. Prasad M, Manjunath C, Murthy AK, Sampath A, Jaiswal S, Mohapatra A. Integration of oral health into primary health care: a systematic review. J Family Med Prim Care. (2019) 8(6):1838–45. doi: 10.4103/jfmpc.jfmpc_286_19
7. Petersen PE, Kwan SYL. The 7th WHO global conference on health promotion - towards integration of oral health, Nairobi, Kenya, 26-30 October 2009. Community Dent Health. (2010) 27:129–36.
8. Patro SK. Editorial: integration of oral health care within the healthcare system. Front Oral Health. (2024) 5:1387141. doi: 10.3389/froh.2024.1387141
9. Braimoh M, Ogunbodede E, Adeniyi A. Integration of oral health into primary health care system: views of primary health care workers in Lagos state, Nigeria. J Public Health Afr. (2014) 5(1):328. doi: 10.4081/jphia.2014.328
10. Okoroafor SC, Christmals CD. Task shifting and task sharing implementation in Africa: a scoping review on rationale and scope. Healthcare. (2023) 11(8):1200. doi: 10.3390/healthcare11081200
11. Amedari MI, Ogunbodede EO, Owotade FJ, Afolabi TO, Amedari IK, Mudasiru TO, et al. A mixed methods study of the oral health knowledge and practice of community health practitioners. Niger J Health Sci. (2024) 23(2):7–15.
12. Dedeke AA, Galvin SR, Sofola O. Community health workers (CHWs) as oral health navigators in a local government area in Lagos state: a pilot intervention. Afr J Oral Health. (2022) 11(1):13–21.
13. Amedari MI. Primary oral health care in Nigeria; four decades after the Alma Ata declaration. PAMJ One Health. (2020) 2(13). doi: 10.11604/pamj-oh.2020.2.13.24357
14. Braimoh OB, Umanah AU. Basic package of oral care: a veritable tool for promotion of primary oral health care by community health officers. Odontostomatol Trop. (2014) 37(147):51–6.25975068
15. Adeniyi AA, Ajieroh V, Sofola OO, Asiyanbi O, Oyapero A. A pilot test of an oral health education module for community health workers in Ikeja LGA, Lagos state. Afr J Oral Health. (2017) 7(1):8–16. doi: 10.4314/ajoh.v7i1.162231
16. Oladayo AM, Lawal FB, Sofola OO, Uti OG, Oyapero A, Aborisade A, et al. Study protocol for a pilot quasi-experimental study on oral health education for nurses and community health workers in Nigeria. Front Public Health. (2024) 12:1398869. doi: 10.3389/fpubh.2024.1398869
17. Sadovska V, Rastorgueva N, Migliorini P, Melin M. Engagement of stakeholders in action-oriented education for sustainability: a study of motivations and benefits and development of a process model. J Agric Educ Ext. (2024) 1–23.
18. Truong TD, Dinh H-VT, Ha XV, Nguyen HT, Dau LM, Tran NG. The role of key stakeholders in building effective professional learning communities (PLCs) in Vietnamese primary schools. Soc Sci Humanit Open. (2025) 11:101212. doi: 10.1016/j.ssaho.2024.101212
19. Aliyu AA, Amadu L. Urbanization, cities, and health: the challenges to Nigeria - a review. Ann Afr Med. (2017) 16(4):149–58. doi: 10.4103/aam.aam_1_17
20. Adewoyin IB, Falegan AV, Yusuff BS. Beyond the inner city: understanding the preference for peri-urban areas in Ibadan, Nigeria. Int J Environ Res Earth Sci. (2024).
21. Adelekan IO. Urban dynamics, everyday hazards and disaster risks in Ibadan, Nigeria. Environ Urban. (2020) 32(1):213–32. doi: 10.1177/0956247819844738
22. Ojewale LY, Mukumbang FC. Access to healthcare services for people with non-communicable diseases during the COVID-19 pandemic in Ibadan, Nigeria: a qualitative study. BMC Health Serv Res. (2023) 23(1):1231. doi: 10.1186/s12913-023-10278-0
23. Aliyu TK, Titus OS, Bernard OT, Alade OT, Ehizele AO, Foláyan MO. Cultural themes related to oral health practices, beliefs, and experiences in Nigeria: a scoping review. Oral. (2025) 5(2):23. doi: 10.3390/oral5020023
24. Hood S, Campbell B, Baker K. Culturally Informed Community Engagement: Implications for Inclusive Science and Health Equity [Internet]. Research Triangle Park, NC: RTI Press (2023). doi: 10.3768/rtipress.2023.op.0083.2301
25. Abah AJ, Etiaba E, Onwujekwe O. Communicating health information at the community level in Nigeria: examining common practices and challenges. J Commun Healthc. (2025):1–10. doi: 10.1080/17538068.2025.2487380
26. Mossey P, Muthu MS, Yan S, Campodonico M, Orenuga L. Oral health in comprehensive cleft care educational resources for non-oral health professionals. World Dental Federation (2021).
27. Pitney WA, Parker J. Qualitative Research in Physical Activity and the Health Professions. Champaign, IL: Human Kinetics (2009).
28. Church S, Dunn M, Prokopy L. Benefits to qualitative data quality with multiple coders: two case studies in multi-coder data analysis. J Rural Soc Sci. (2019) 34(1).37559698
29. Ahmed SK. The pillars of trustworthiness in qualitative research. J Med Surg Public Health. (2024) 2:100051. doi: 10.1016/j.glmedi.2024.100051
30. Orkin AM, Rao S, Venugopal J, Kithulegoda N, Wegier P, Ritchie SD, et al. Conceptual framework for task shifting and task sharing: an international Delphi study. Hum Resour Health. (2021) 19(1):61. doi: 10.1186/s12960-021-00605-z
31. Gallagher JE, Mattos Savage GC, Crummey SC, Sabbah W, Varenne B, Makino Y. Oral health workforce in Africa: a scarce resource. Int J Environ Res Public Health. (2023) 20(3):2328. doi: 10.3390/ijerph20032328
32. Bhadauria US, Priya H, Purohit B, Kharbanda OP, Khurana C, Das D, et al. Effectiveness of an oral health training program for nursing professionals in India: an interventional study. Public Health Nurs. (2021) 38(6):1135–9. doi: 10.1111/phn.12953
33. Adeniyi AA, Oyapero A, Ajieroh V, Sofola O, Asiyanbi O. Effect of health education intervention conducted by primary health care workers on oral health knowledge and practices of nursing mothers in Lagos state. J Public Health Africa. (2018) 9(2):833. doi: 10.4081/jphia.2018.833
34. Põld A, Kientega DF, Garé J, Listl S. A mixed methods evaluation of the effectiveness of an oral health training program for disability care workers in Burkina Faso. BMC Oral Health. (2024) 24(1):33. doi: 10.1186/s12903-023-03837-8
35. Park SE, Donoff RB, Saldana F. The impact of integrating oral health education into a medical curriculum. Med Princ Pract. (2017) 26(1):61–5. doi: 10.1159/000452275
36. Shimpi N, Schroeder D, Kilsdonk J, Chyou PH, Glurich I, Penniman E, et al. Medical providers’ oral health knowledgeability, attitudes, and practice behaviors: an opportunity for interprofessional collaboration. J Evid Based Dent Pract. (2016) 16(1):19–29. doi: 10.1016/j.jebdp.2016.01.002
37. Petersen PE, Baez RJ, Ogawa H. Global application of oral disease prevention and health promotion as measured 10 years after the 2007 world health assembly statement on oral health. Community Dent Oral Epidemiol. (2020) 48(4):338–48. doi: 10.1111/cdoe.12538
38. Laniado N, Cloidt M, Altonen B, Badner V. Interprofessional oral health collaboration: a survey of knowledge and practice behaviors of hospital-based primary care medical providers in New York city. Adv Med Educ Pract. (2021) 12:1211–8. doi: 10.2147/AMEP.S332797
39. Findley SE, Matos S, Hicks AL, Campbell A, Moore A, Diaz D. Building a consensus on community health workers’ scope of practice: lessons from New York. Am J Public Health. (2012) 102(10):1981–7. doi: 10.2105/AJPH.2011.300566
40. Kok MC, Vallières F, Tulloch O, Kumar MB, Kea AZ, Karuga R, et al. Does supportive supervision enhance community health worker motivation? A mixed-methods study in four African countries. Health Policy Plan. (2018) 33(9):988–98. doi: 10.1093/heapol/czy082
41. Crigler L, Hill K, Furth R, Bjerregaard D. Community health worker assessment and improvement matrix (CHW AIM): a toolkit for improving community health worker programs and services. Published by the USAID Health Care Improvement Project (2011).
42. Ndambo MK, Munyaneza F, Aron MB, Nhlema B, Connolly E. Qualitative assessment of community health workers’ perspective on their motivation in community-based primary health care in rural Malawi. BMC Health Serv Res. (2022) 22(1):179. doi: 10.1186/s12913-022-07558-6
43. Toki D. Community health workers and trainers perspectives on education and practice: a qualitative case study in the context of maternal and child health in Rwanda (Doctoral dissertation). The University of Western Ontario (Canada) (2021).
44. Sharkiya SH. Quality communication can improve patient-centred health outcomes among older patients: a rapid review. BMC Health Serv Res. (2023) 23(1):886. doi: 10.1186/s12913-023-09869-8
45. Manongi RN, Marchant TC, Bygbjerg IC. Improving motivation among primary health care workers in Tanzania: a health worker perspective. Hum Resour Health. (2006) 4:1–7. doi: 10.1186/1478-4491-4-6
46. Ansah JP, Chiu C-T. Projecting the chronic disease burden among the adult population in the United States using a multi-state population model. Front Public Health. (2023) 10:1082183. doi: 10.3389/fpubh.2022.1082183
47. Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. (2013) 38(5):976–93. doi: 10.1007/s10900-013-9681-1
48. Kim J, Roy I, Martinez-Mier EA, Shukla A, Weir P. Impact of lack of transportation on access to dental care. Heliyon. (2024) 10(23):e40657. doi: 10.1016/j.heliyon.2024.e40657
49. Cohen LK, Gift HC. Disease Prevention and Oral Health Promotion: Socio-Dental Sciences in Action. London: FDI (1995).
50. Kikwilu E, Frencken J, Mulder J, Masalu J. Barriers to restorative care as perceived by dental patients attending government hospitals in Tanzania. Community Dent Oral Epidemiol. (2009) 37(1):35–44. doi: 10.1111/j.1600-0528.2008.00446.x
51. Edward M, Agyapong D, Paul IK, Idris I, Boris GK, Kengo NE, et al. Oral health in Tanzania: unmasking its neglected dimension. Public Health Chall. (2024) 3(3):e70000. doi: 10.1002/puh2.70000
52. Varenne B, Petersen PE, Fournet F, Msellati P, Gary J, Ouattara S, et al. Illness-related behaviour and utilization of oral health services among adult city-dwellers in Burkina Faso: evidence from a household survey. BMC Health Serv Res. (2006) 6:164. doi: 10.1186/1472-6963-6-164
53. Lo EC, Lin HC, Wang ZJ, Wong MC, Schwarz E. Utilization of dental services in southern China. J Dent Res. (2001) 80(5):1471–4. doi: 10.1177/00220345010800051701
54. Dany SS, Naik C, Tangade P, Satpathy AK. Felt and normative needs for oral health and utilization of services. Int J Prev Clin Dent Res. (2017) 4(4):258–61. doi: 10.5005/jp-journals-10052-0120
55. Oleribe OO, Momoh J, Uzochukwu BS, Mbofana F, Adebiyi A, Barbera T, et al. Identifying key challenges facing healthcare systems in Africa and potential solutions. Int J Gen Med. (2019) 12:395–403. doi: 10.2147/IJGM.S223882
56. Ogah PO, Uguru N, Okeke C, Mohammed N, Ogbe O, Ashiver WG, et al. Primary health care in Nigeria: best practices and quality of care in Nigeria. BMC Health Serv Res. (2024) 24(1):963. doi: 10.1186/s12913-024-11406-0
57. Hanson K, Brikci N, Erlangga D, Alebachew A, De Allegri M, Balabanova D, et al. The lancet global health commission on financing primary health care: putting people at the centre. Lancet Glob Health. (2022) 10(5):e715–72. doi: 10.1016/S2214-109X(22)00005-5
58. Harnagea H, Couturier Y, Shrivastava R, Girard F, Lamothe L, Bedos CP, et al. Barriers and facilitators in the integration of oral health into primary care: a scoping review. BMJ Open. (2017) 7(9):e016078. doi: 10.1136/bmjopen-2017-016078
59. Muneer MU, Ismail F, Munir N, Shakoor A, Das G, Ahmed AR, et al. Dental anxiety and influencing factors in adults. Healthcare. (2022) 10(12):2352. doi: 10.3390/healthcare10122352
60. Wang M-C, Vinall-Collier K, Csikar J, Douglas G. A qualitative study of patients’ views of techniques to reduce dental anxiety. J Dent. (2017) 66:45–51. doi: 10.1016/j.jdent.2017.08.012
61. Lehmann U, Sanders D. Policy brief: community health workers: what do we know about them? The state of the evidence on programmes, activities, costs and impact on health outcomes of using community health workers. Evidence and Information for Policy (2007), 2.
62. Barnett T, Hoang H, Stuart J, Crocombe L. Non-dental primary care providers’ views on challenges in providing oral health services and strategies to improve oral health in Australian rural and remote communities: a qualitative study. BMJ Open. (2015) 5(10):e009341. doi: 10.1136/bmjopen-2015-009341
63. Poudel P, Griffiths R, Wong VW, Arora A, Flack JR, Khoo CL, et al. Perceptions and practices of general practitioners on providing oral health care to people with diabetes-a qualitative study. BMC Fam Pract. (2020) 21:1–11. doi: 10.1186/s12875-020-1102-9
64. Reinders J-J. Task shifting, interprofessional collaboration and education in oral health care (2018).
65. Choudhary P, Huda I, Pandey A, Kumar N, Nabi AT, Raj R. Insights of primary health care providers regarding opportunistic screening of oral cancer/precancers in Patna, Bihar. J Family Med Prim Care. (2020) 9(5):2400–4. doi: 10.4103/jfmpc.jfmpc_301_20
66. Tseng Y-H, Griffiths F, De Kadt J, Nxumalo N, Rwafa T, Malatji H, et al. Integrating community health workers into the formal health system to improve performance: a qualitative study on the role of on-site supervision in the South African programme. BMJ Open. (2019) 9(2):e022186. doi: 10.1136/bmjopen-2018-022186
67. Deconinck H, Hallarou M, Criel B, Donnen P, Macq J. Integrating acute malnutrition interventions into national health systems: lessons from Niger. BMC Public Health. (2016) 16:1–7. doi: 10.1186/s12889-016-2903-6
68. Wallace C, McCosker A, Farmer J, White C. Spanning communication boundaries to address health inequalities: the role of community connectors and social media. J Appl Commun Res. (2021) 49(6):632–50. doi: 10.1080/00909882.2021.1934513
69. Desai JR, Vazquez-Benitez G, Taylor G, Johnson S, Anderson J, Garrett JE, et al. The effects of financial incentives on diabetes prevention program attendance and weight loss among low-income patients: the we can prevent diabetes cluster-randomized controlled trial. BMC Public Health. (2020) 20:1–11. doi: 10.1186/s12889-020-09683-5
70. Seyed-Nezhad M, Ahmadi B, Akbari-Sari A. Factors affecting the successful implementation of the referral system: a scoping review. J Family Med Prim Care. (2021) 10(12):4364–75. doi: 10.4103/jfmpc.jfmpc_514_21
71. Abrahim O, Linnander E, Mohammed H, Fetene N, Bradley E. A patient-centered understanding of the referral system in Ethiopian primary health care units. PLoS One. (2015) 10(10):e0139024. doi: 10.1371/journal.pone.0139024
Keywords: primary healthcare (PHC), oral health disparities, CREATIVE framework, nurses, community health worker (CHW), oral health education/promotion
Citation: Oladayo AM, Lawal FB, Sofola OO, Uti OG, Oyapero A, Aborisade A, Olujitan M, Fagbule OF, Williams AT, Dedeke A, Idiga E, Abdul-Kabir Adegoke Y-I, Adeniji Oluwagbenga I, Mele AB, Baffa AS, Adetula I, Musa KS, Stewart B, Daep CA, Hines D, Beard J, Lawal TA and Butali A (2025) Integrating oral health into primary healthcare: lessons from project OHE-NCHeW (oral health education for nurses and community health workers) in Nigeria. Front. Oral Health 6:1597243. doi: 10.3389/froh.2025.1597243
Received: 20 March 2025; Accepted: 6 June 2025;
Published: 20 June 2025.
Edited by:
Giuseppe Minervini, Università della Campania Luigi Vanvitelli, ItalyReviewed by:
Katherine France, University of Pennsylvania, United StatesStanley Chibuzor Onwubu, Durban University of Technology, South Africa
Copyright: © 2025 Oladayo, Lawal, Sofola, Uti, Oyapero, Aborisade, Olujitan, Fagbule, Williams, Dedeke, Idiga, Abdul-Kabir Adegoke, Adeniji Oluwagbenga, Mele, Baffa, Adetula, Musa, Stewart, Daep, Hines, Beard, Lawal and Butali. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abimbola M. Oladayo, YWJpbWJvbGFvbGFkYXlvQGF0c3UuZWR1
 Abimbola M. Oladayo
Abimbola M. Oladayo Folake B. Lawal
Folake B. Lawal Oyinkansola O. Sofola
Oyinkansola O. Sofola Omolara G. Uti
Omolara G. Uti Afolabi Oyapero
Afolabi Oyapero Adetayo Aborisade
Adetayo Aborisade Mojisola Olujitan
Mojisola Olujitan Omotayo F. Fagbule
Omotayo F. Fagbule Adeola T. Williams
Adeola T. Williams Aderonke Dedeke
Aderonke Dedeke Ejiro Idiga2
Ejiro Idiga2 Yahya-Imam Abdul-Kabir Adegoke
Yahya-Imam Abdul-Kabir Adegoke Amina Sani Baffa
Amina Sani Baffa Bernal Stewart
Bernal Stewart Carlo Amorin Daep
Carlo Amorin Daep Azeez Butali
Azeez Butali