- 1South Ethiopia Region Health Bureau Public Health Institute, Jinka, Ethiopia
- 2Gambella Teachers Education and Health Science College, Gambella, Ethiopia
- 3Department of Public Health, Arba Minch University, Arba Minch, Ethiopia
- 4South Ethiopia Region Health Bureau, Jinka, Ethiopia
- 5Department of Epidemiology and Biostatistics, School of public health, Wolaita Sodo University, Wolaita Sodo, Ethiopia
- 6Arbaminch General Hospital, Monitoring & Evaluation, Arbaminch, Ethiopia
Introduction: Food insecurity is a multidimensional issue that has been related with poor overall health, obesity and chronic diseases and not only related with increased prevalence of diabetes but also with increasing health care expenses. There is paucity of researches conducted to assess food insecurity and its associated factors among adult diabetic clients in Ethiopia. Hence this study was aimed to assess food insecurity and its associated factors among adult diabetic patients in Gambella town public hospitals.
Methods: A facility based cross sectional study was conducted among adult diabetic clients in Gambella town public hospital from May 1 to June 30, 2023. A systematic sampling technique was used to select a sample of 412 patients. Data were collected by trained data collectors using structured questionnaires. Data were checked for its completeness and consistence then entered into Epidata 4.6 and transported to SPSS version 26 for analysis. Bivariate analysis was done to make variables candidate for multivariate analysis at p-value <0.25. In multivariate analysis AOR with 95% CI were used to declare factors associated with food insecurity at p-value <0.05.
Results: The prevalence of food insecurity was found to be 59.5% (95% CI: 54.6%-64.3%). In multivariate analysis the variables age 18 to 24 years (AOR=0.093,95% CI:0.02-0.30), able to read and write (AOR=4.31, CI:1.246-11.250), employed (AOR=0.20; 95% CI: 0.063-0.63), low wealth status (AOR=3.02, CI:1.265-4.788) OR=2.46, CI:1.265-4.788), medium wealth status (AOR=1.88, CI:1.002-3.815). Family size (AOR=0.48; 95% CI: 0.27-0.87), and family history of diabetes (AOR=2.86, CI: 1.43- 5.72) were significantly associated with food insecurity. income and (AOR=1.88, CI:1.002-3.815)
Conclusion and recommendations: The prevalence of food insecurity among adult diabetic patients was high. Therefore, health professionals should give emphasis to encourage self-management for those who have family history of diabetes in order to screen the clients at early before the occurrence of DM complication and health care expenditure.
Introduction
Food insecurity refers to the limited and inconsistent availability, accessibility, utilization and stability of food. It is an important community health problem that remains mainly critical in place of chronic health conditions, like diabetes, that require dietary modification to manage (1).
Food insecurity has been associated with poor overall health, poor mental health, obesity and chronic diseases (2–4). In fact, adults who lack access to adequate food and nutrition are 2 to 3 times more likely to develop diabetes than those who do not. Food and nutrition insecurity are not only associated with increased prevalence of diabetes but also with increasing health care expenses. Diabetics with low FI and self-efficacy have more than twice health care utilization than food secure even after being stabilized in hospital, FI patients have double likelihood of being readmitted within 15 days of discharge and this is potentially harmful and can result in severe diabetes-related complications (5).
Diabetic patients often do not present to the hospital until they have severe complications related to previously undiagnosed diabetes, particularly those who do not have the economic means to see a physician regularly. FI is an important target for diabetes prevention and management since it is associated with poor glycemic control, higher rates of complications and hospitalization, and poor adherence to treatment. FI screening among individuals with diabetes could help healthcare workers to identify patients’ difficulties in adhering to treatment and dietary recommendations (6)
Globally, the prevalence of moderate and severe FI was predictable at 28.9%, with significant numbers of the people (2.33 billion) experiencing hunger in 2023. That means they did not have access to adequate food. It was also estimated that about 10.7% of the world’s population that means about 864 million people were food insecure at severe level. The prevalence of moderate or severe food insecurity in Africa was over twice as high as the global average in 2023 (58.0 percent), whereas the prevalence is closer to the global estimate in Asia, Latin America and the Caribbean, and Oceania (24.8, 28.2, and 26.8 percent, respectively) (7). According to the world food program (WFP) report 10.2 million people are severely food insecure including the 3 million people who are internally displaced in Ethiopia in 2025 (8). There are numerous studies that have described FI as an independent risk issue for poor intermediate health outcomes and may be associated with chronic disease in adults with low-income, including obesity, insulin resistance, T2DM, and cardiovascular diseases (9, 10). FI can compound diabetes management challenges by directly or indirectly influencing the three pillars of optimal glycemic control: nutrition therapy, physical activity, and self-management (11). Although genetic factors had a big influence on the development of diabetes and environmental factors also contributed to illness (12). FI is related with inadequate income as well as higher housing costs, higher rates of joblessness and nations with market taxes (13).
In Ethiopia; diabetic mellitus is a main community health problem in the modern era. Alongside more than half of diabetic patients not practicing the perceived healthy nutritive based approach, gathering with family and friends and eating out of home were the major reasons for not being in line with this (14). Food Security was essential in the managing of diabetic mellitus cases and its complications. Particularly, diets with low glycemic index, little total cholesterol reduce the risk of diabetic patients from developing complications. Adult diabetic patients should continue their food treatment throughout their whole course of diabetic care. There are three types of domains of food insecurity such as worry about not getting enough food, inadequate food quality and inadequate food quantity and it has been recognized as a theoretically modifiable risk factor that can be related with both the development of T2DM (15) and poor glycemic control (15).
Even if the previous research has identified a number of factors associated with both FI and diabetes, the factors that explain the relationship between FI and glycemic control remain unclear and there was also paucity of researches conducted in Ethiopia regarding to food insecurity and its associated factors among adult diabetic patients (15). The objective of this study was to assess food insecurity and its associated factors among adult diabetic patients in Gambella Town Public Hospitals, South Western Ethiopia. Addressing FI may help tackle the burgeoning challenge of diabetes in Ethiopia particularly in Gambella town.
Methods
Study design and period
A facility-based cross-sectional study was conducted from May 1 to June 30, 2023.
Study area
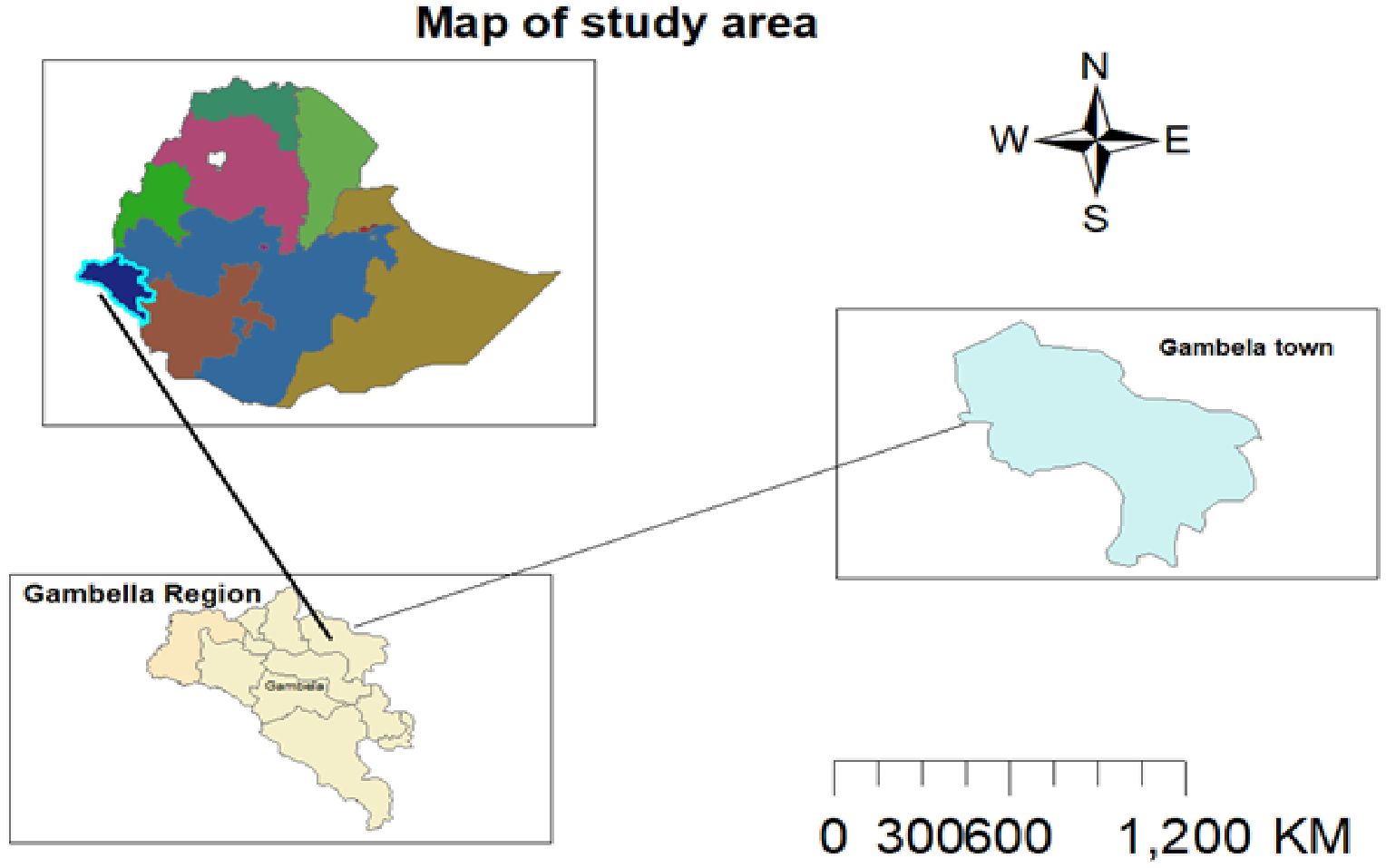
The study took place in Gambella town’s public general and primary hospitals. Gambella town is located 768 kilometers southwest of Addis Ababa, the capital city of Ethiopia. The town is situated at the confluence of the Baro River and its tributary, the Jejebie. It has a latitude and longitude of 8°15’N 34°35’E and an elevation of 526 meters above sea level, featuring a hot climate. According to a 2023 report by the town health office, Gambella has a population of 67,451, comprising various ethnic groups, predominantly the Nuer, Agnuhak, and Majang. There are also settlers from other highlands of the country (Figure 1).
The study population consisted of adult diabetic patients attending DM clinics during the data collection period. Adult DM patients aged 18 and above visiting diabetic clinics during the study period were included whereas severely ill patients and pregnant mothers were excluded from the study.
Sample size determination
The sample size was calculated using a single population proportion formula, assuming a 50.7% proportion of food insecurity (FI) among DM clients based on a previous study (15). With a 95% confidence level and a 5% margin of error, the calculated sample size was 384. Accounting for a 10% non-response rate, the final sample size was 422. The sample size for secondary objectives was lower, so the larger sample size was used.
Sampling technique
The study involved two public hospitals having a total of 1350 DM clients: 900 from Gambella General Hospital and 450 from Gambella Primary Hospital. A systematic random sampling technique was used after proportional allocation based on client flow. Diabetic clinic services are provided five days a week. The sampling interval was calculated by dividing the average monthly flow of diabetic clients by the sample size. For Gambella General Hospital, K=900/281 = 3; for Gambella Primary Hospital, K=450/141 = 3. The initial number was randomly selected from one to three by lottery, resulting in two.
Data collection technique and quality control
Data was collected through face-to-face interviews using structured questionnaires adapted from various literature sources. The questionnaire covered socio-economic, anthropometric and diabetic-related knowledge questions, diet, and the Household Food Insecurity Access Scale (HFIAS). Data collection was performed by four skilled diploma nurses and two BSc midwifery supervisors from Gambella town public hospitals. To maintain data quality, a two- day training session was conducted for data collectors and supervisors. The questionnaire was prepared in English, translated to Amharic, and back-translated to English to ensure consistency. The questionnaire was pretested on 5% of the sample size at a nearby health center, and data completeness was checked daily by the supervisor.
Operational definitions for the study variables
Adequate glycemic control: When the FBS measurements 70 mg/dL - 126 mg/dL.
Inadequate glycemic control: When FBS measurements ≥126 mg/dL.
Diabetic knowledge: Patients who answered below the average of 23 DM knowledge assessment questions were labeled as having poor knowledge; those who scored above average were labeled as having good knowledge (15).
Food-secure: Q1a=0 or Q1a=1) and Q2 - Q9 = 0 (15)
Mild Food Insecurity: Q1a=2 or 3, or Q2a=1,2, or 3 or Q3a or Q4a=1 and Q5-Q9 = 0 (6)
Moderate Food Insecurity: Q3a or Q4a=2 or 3, or Q5a or Q6a=1 or 2, and Q7- Q9 = 0 (16)
Severe Food Insecurity: Q5a or Q6a=3, or Q7a, or Q8a, or Q9a=1,2 or 3 (17)
Wealth index: scores were given based on the number and kinds of consumer goods and housing characteristics. These scores were derived using principal component analysis and classified into low, middle and high wealth index (18).
Data processing and analysis
After checking for completeness and consistency, data was cleaned, coded, and entered into Epidata version 4.6, then exported to SPSS version 26 for analysis. Descriptive statistics was used to show frequency distribution and principal component analysis (PCA) for wealth index was also performed. Bivariate analysis identified candidate variables for multivariate analysis at p-values <0.25. Adjusted Odds Ratios (AOR) with 95% Confidence Intervals (CI) and p-values <0.05 were used to identify statistically significant factors associated with food insecurity. Multicollinearity was checked using Variance Inflation Factor (VIF). Model goodness-of-fit was assessed using Hosmer-Lemeshow’s test, which yielded a result of 0.084, indicating a good fit.
Ethical approval
ethical clearance was obtained from the Institutional Review Board of Arba Minch University College of Medicine and Health Science (Protocol No: MT1443/2023). Official permission was secured from Gambella town public hospitals. Participants were provided verbal consent before interviews, and confidentiality was maintained throughout the study. Participants were informed that refusal to consent or withdrawal from the study would not affect their access to healthcare.
Results
Socio-economic characteristics
In this study the overall response rate was found to be 412 (97.6%) among these 221 (53.6%) were females and the mean age ± SD was 43.1 ( ± 12.2) years and 287 (60.9%) respondents were urban dwellers. 296 (71.8%) of the respondents were married and 289 (70.1%) of the participants had <5 family sizes. Moreover, concerning occupation almost half of the respondents (51.2%) were housewives. Last but not least, one hundred forty-nine of the study participants (36.2%) were in the lowest wealth status (Table 1).
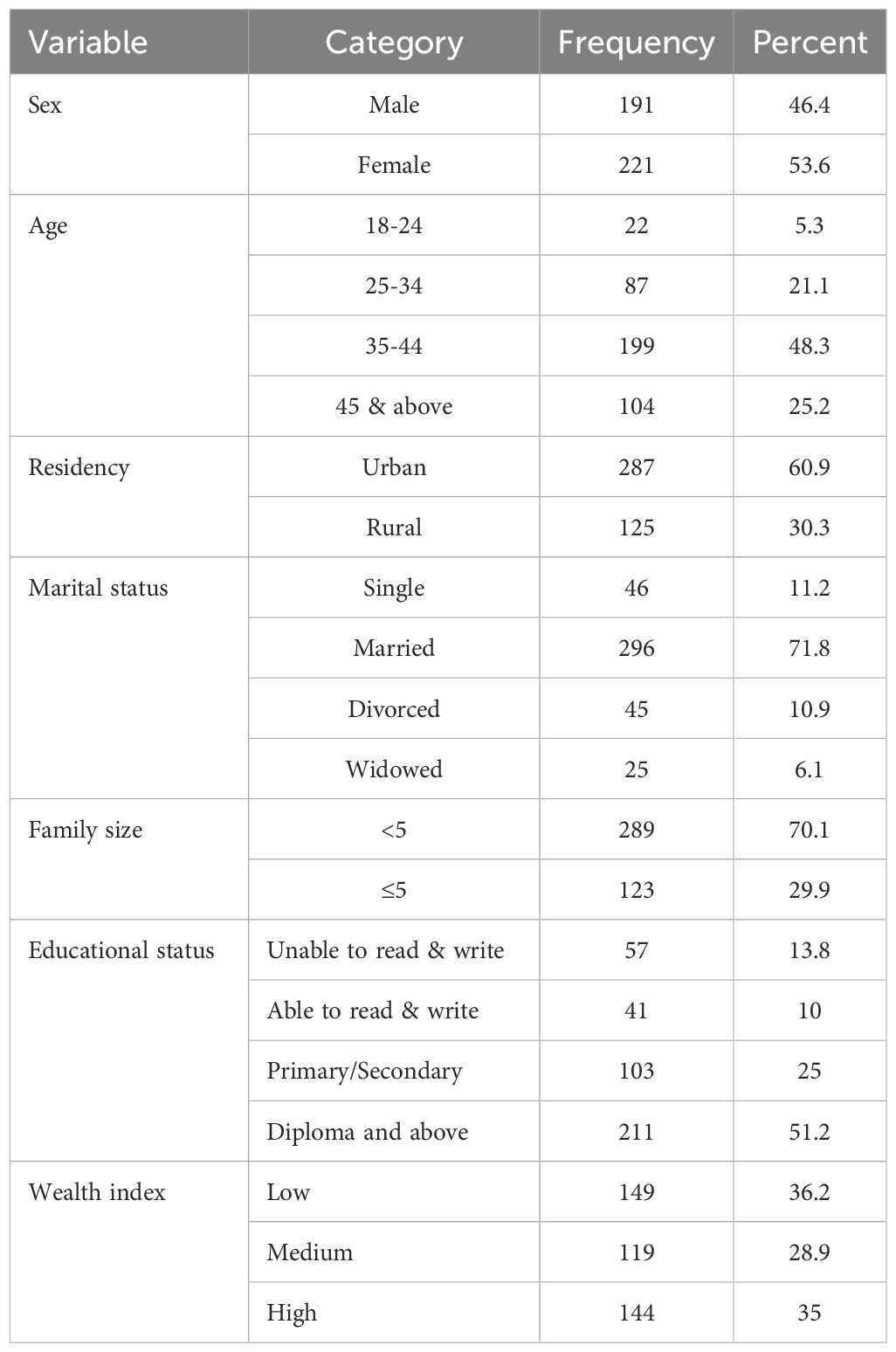
Table 1. Socio-economic characteristics of diabetic clients who had medical follow up in Gambella town public hospitals, Southwestern Ethiopia, 2023.
Health and anthropometric characteristics of diabetic patients
In this study, 350 (85%) of the respondents had a disease duration of <5 years and 153 (37.1%) of the respondents had DM related comorbidities. Of the DM patients, 331(80.3%) were taking oral treatment and 64 (15.5%) of them were using insulin medications. Two hundred ninety-two (70.9%) of the respondents did not get education related to DM and 336 (81.5%) of the respondents reported that they don’t know the presences of DM association. 322 (78.2%) of the respondents had faced inadequate glycemic control. Moreover, in this study 275 (66.7%) of the respondents had inadequate knowledge related to DM. (Table 2).
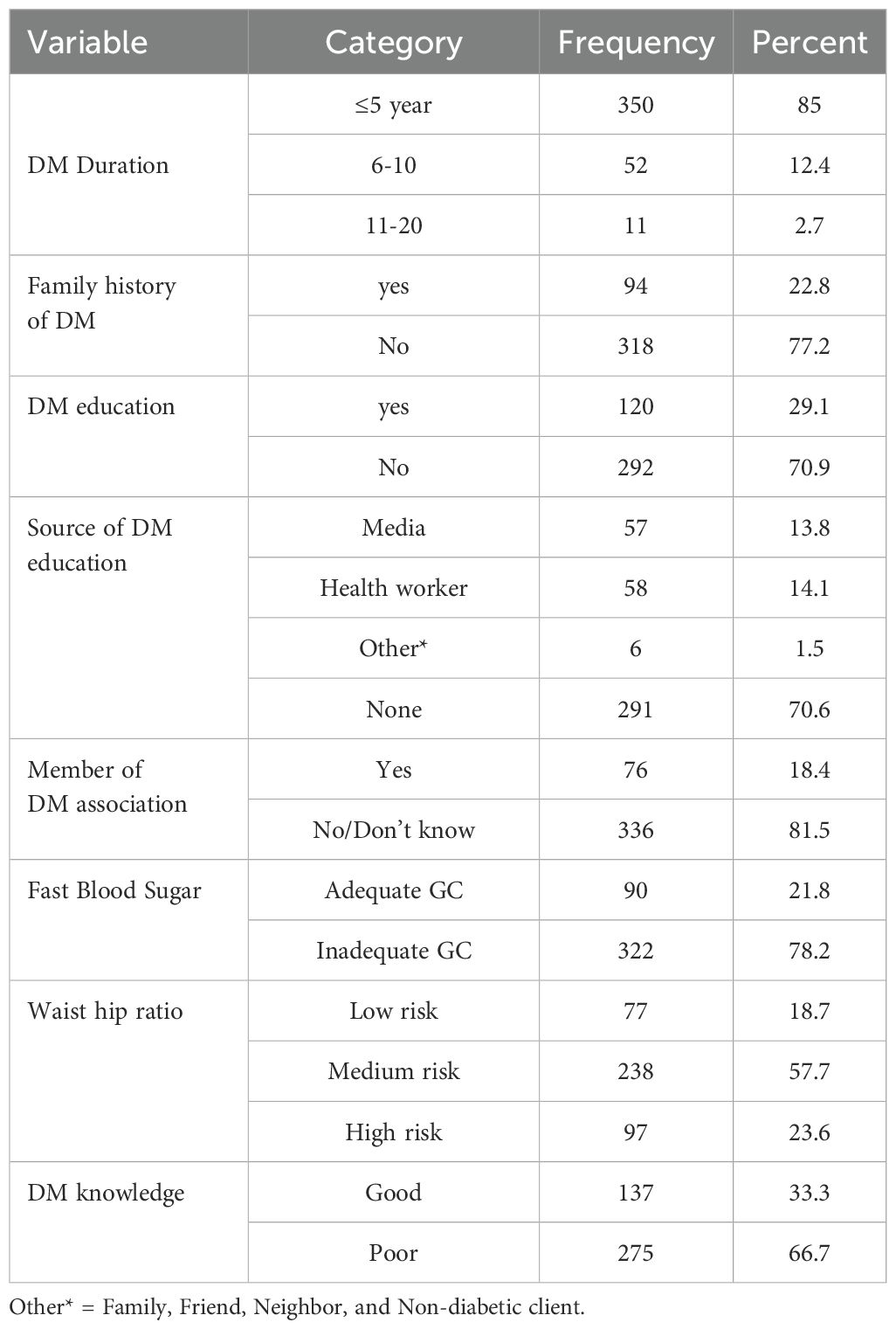
Table 2. Health and anthropometric characteristics of diabetic clients who had medical follow up in Gambella town public hospitals, Southwestern Ethiopia, 2023.
Diet related characteristics
In this study it was reported that two hundred fifty-three (61.4%) of the study participants consumes food outside their home and 247 (60%) of them reported as their consumption was ≤ 4 days per week. 318 (77.8%) the respondents did not fast before diabetic diagnosis and for one hundred twenty (29.1%) of the participants the most fasting hours was 7-10. In addition to this, 373 (90.5%) of the respondents worried about the high cost of food (Table 3).
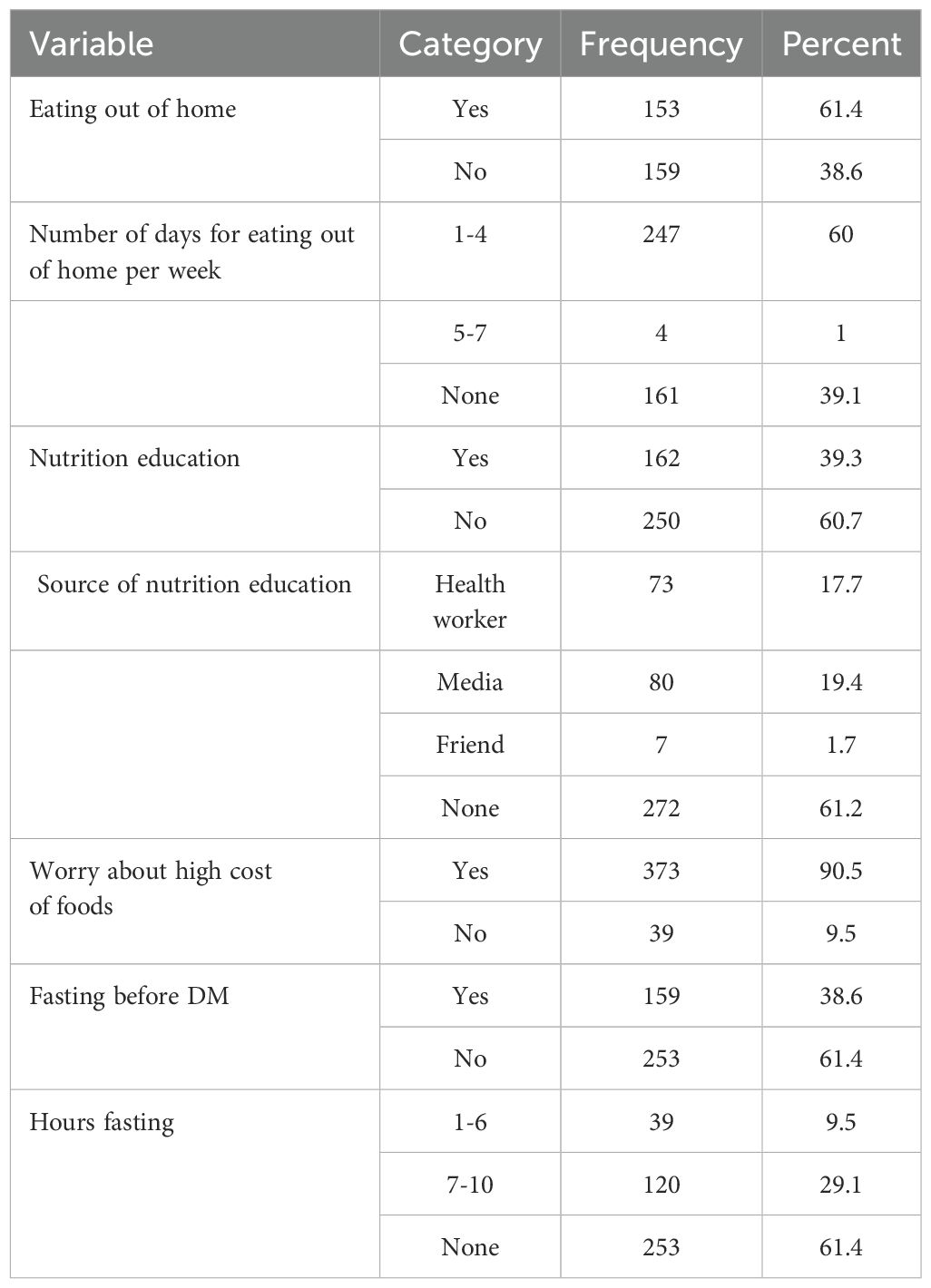
Table 3. Diet related characteristics of diabetic clients who had medical follow up in Gambella town public hospitals, Southwestern Ethiopia, 2023.
Magnitude of food insecurity among adult diabetic patients
The overall magnitude of food insecurity in this study was found to be 59.5% (54.6% - 64.3%). The level of FI classified as Food Secure (40.5%), mildly FI (7.3%), moderately FI (22.8%), and severely FI (29.4%), (Figure 2). In this study concerning the domain of Food Insecurity it was reported that two hundred forty five (59.5%) of the participants worry about not getting enough food, 236(57.5%) unable to eat preferred foods, 263(63.8%) has limited variety of foods, 213(51.7%) feed unwanted food, 266(64.6%) eat a smaller meal, 235(57%) eat fewer meals in a day, 68(16.5%) has no any kind food in house, 139(26.1%) go to sleep at night hungry, and 71(17.2%) go hungry a day and night (Table 4).
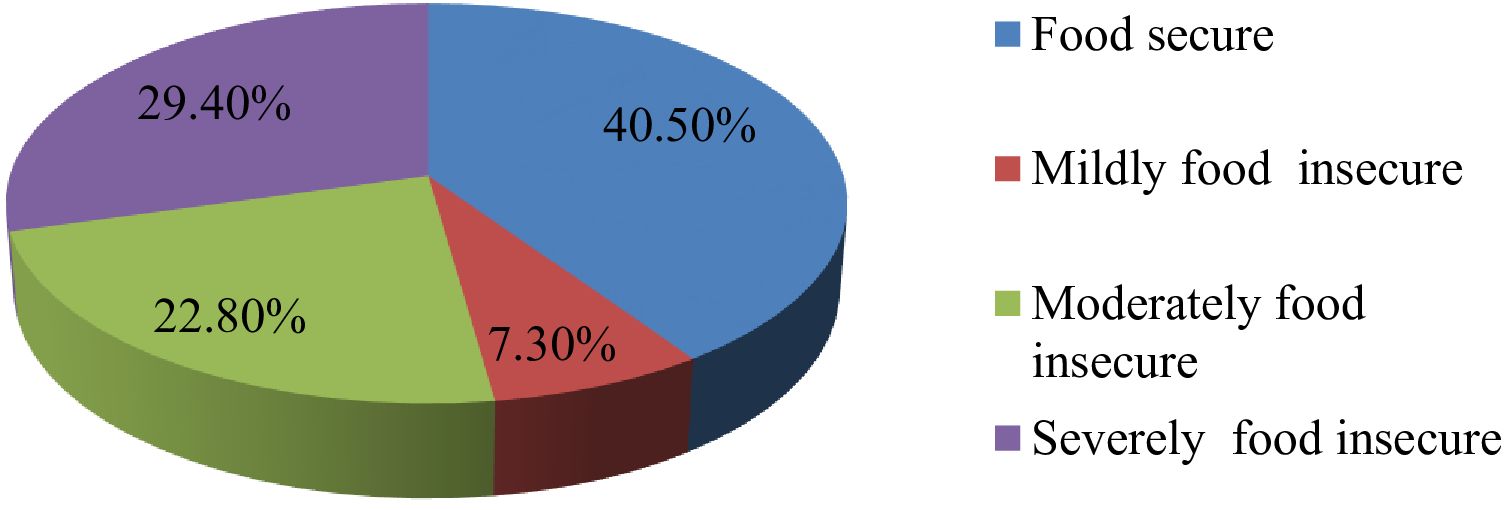
Figure 2. Levels of food insecurity among adult diabetic’s wgo had medical follow up in Gambella town in public hospitals, Southwestern Ethiopia, 2023.
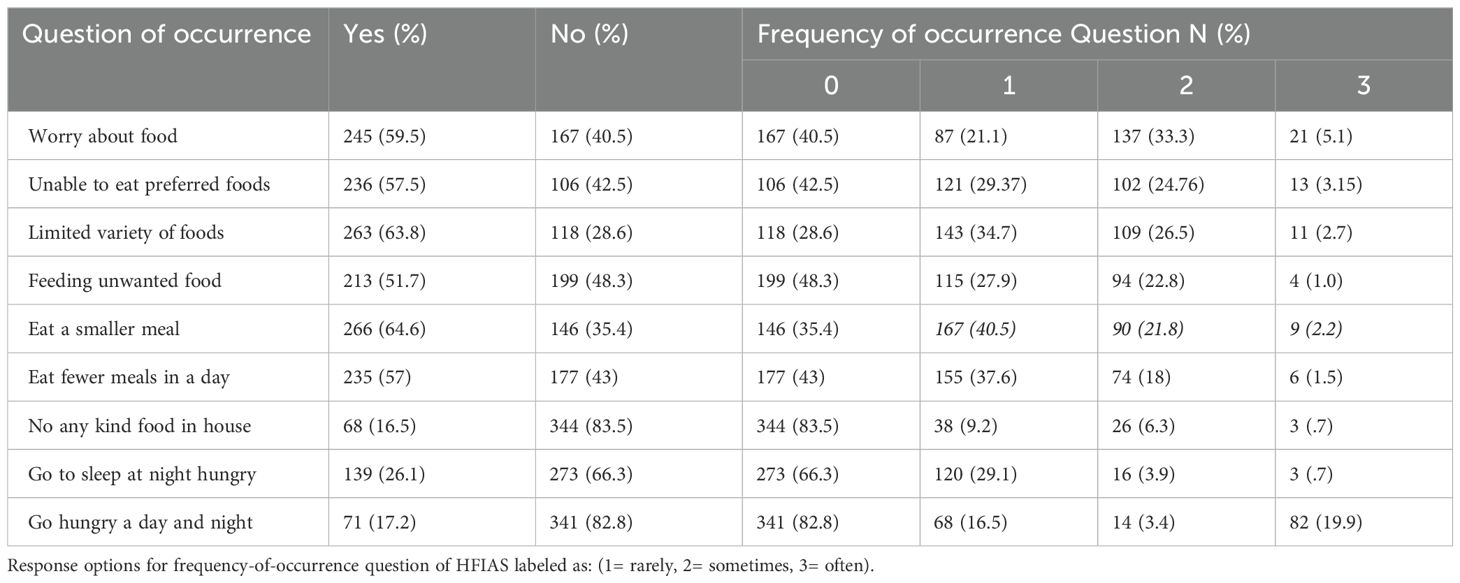
Table 4. Magnitude of food insecurity among adult diabetic clients who had medical follow up in Gambella town public hospitals, Southwestern Ethiopia, 2023.
Associated factors with FI among adult diabetic patients
Based on bivariate analysis variables like sex, age, residence, marital status, family size, educational status, occupational status, wealth status, duration of DM, comorbidity, DM medication, family history of DM, education on DM, Source of DM education, member of DM association, fasting before DM diagnosis, WHR, knowledge on DM, nutrition education, and worry about high costs were candidate variables at p<0.25.
In multivariate analysis, age, able to read and write, occupational status of house wife, low and medium in wealth status, and having family history of DM were significantly associated with FI at p value<0.05. The odds of food insecurity were reduced by 90.7% (AOR=0.093, CI:0.02-0.30), 78% (AOR= 0.22, CI:0.086-0.465) and 63% (AOR= 0.37, CI: 0.19-0.76) among age group 18-24, 25-34, and 35-44, respectively than age group 44 and above. The odds of FI was 4.31 times higher among able to read and write as compared to diploma and above (AOR=4.31, CI:1.246-11.250). The odd of FI was reduced by 80% (AOR=0.20; 95% CI: 0.063-0.63), and 88% (AOR=0.12, CI: 0.039- 0.43) among employed and merchant study participants respectively as compared to those who are housewife. The odds of FI was 3.02 and 1.88 times higher among low- and medium-income respondents than high income (AOR=3.02, CI:1.265-4.788) and (AOR=1.88, CI:1.002-3.815) respectively. Moreover, the odds of FI was about 2.8 times higher among participants having family history of diabetic compared to their counter parts (AOR=2.86, CI: 1.43- 5.72) (Table 5). Furthermore, the odds of FI was reduced by 52% (AOR=0.48; 95% CI: 0.27-0.87) among study participants with less than 5 family members as compared to those who have more than or equal to 5 family members.
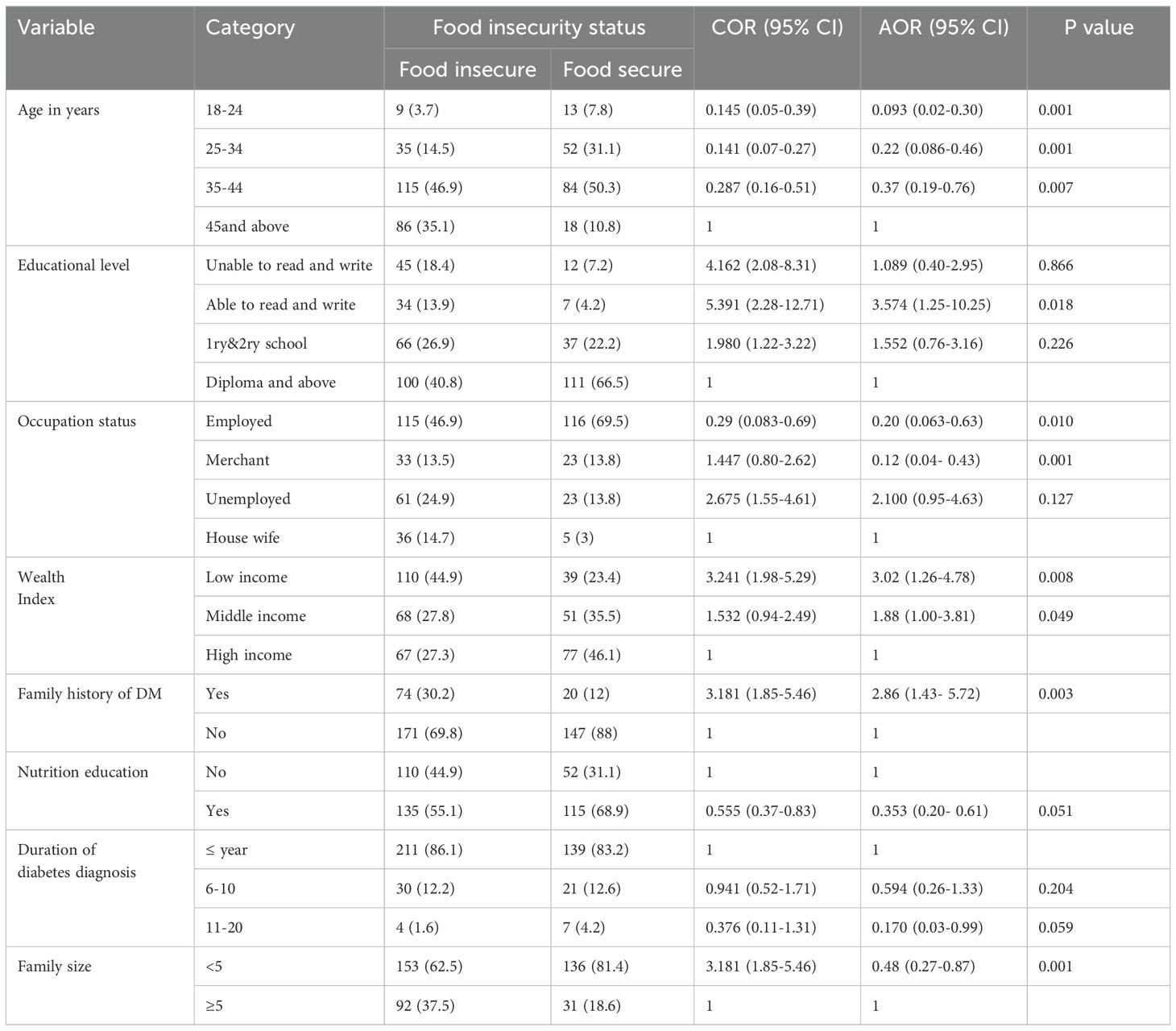
Table 5. Factors associated with food insecurity among adult diabetic clients who had medical follow up in Gambella town public hospitals, Southwestern Ethiopia, 2023.
Discussion
This study aimed to assess the magnitude and associated factors of food insecurity among diabetic patients in Gambella town public hospitals, Southwest Ethiopia. The results revealed that 59.5% (54.6% - 64.3%) of adult diabetic patients experienced FI. This finding is consistent with studies conducted in South Africa (63.6%) (19) Iran (59.7%) (20) the United States (56%) (20). However, it is higher than the prevalence reported in Addis Ababa (50.7%) (20) and Canada (19.5%). This may be potentially due to differences in poverty and income. That means people who live in Addis Ababa have high income rates as compared to Gambella region in general. In addition, there is a limited employment opportunity in Gambella region as compared to Addis Ababa that may limits the accessibility of sufficient nutritious food. Conversely, it is lower than the prevalence reported in Burkina Faso (71%) (21) and Jordan (78%) (22) which may be attributed to variations in geographical location, socio-economic status, study settings, and sample sizes.
Younger age groups were less likely to experience food insecurity compared to older age groups, aligning with findings from the National Health Interview Survey 2016 (23) and a similar study in Nigeria (24). This could be due to younger diabetic patients have higher chance of employment and get income providing a high chance of getting adequate food among younger diabetic patients. In addition, younger patients likely to have health insurance coverage because of higher employment that increases the chance of obtaining health services.
Participants who could read and write were 3.57 times more likely to be food insecure compared to those with diploma or higher. This is consistent with studies conducted at Nekemte Referral Hospital (16) and in Southwest Iran (25), suggesting that education creates self-awareness regarding a healthy and quality diet. Higher education also leads to higher employment or better job opportunities and better salaries this may lower the food insecurity among educated as compared to uneducated diabetic patients. Moreover, more educated diabetic patients may have good social networks that may increases access to information resources and in generally the support.
Housewives were more likely to experience food insecurity compared to employed individuals. This finding aligns with studies in South Africa (26) and Europe (27), indicating that housewives may rely on cash crops rather than edible crops and housewife entirely depend on their husbands for financial support. This financial dependence aggravates the food insecurity level at household level. Housewife may have limited control on the resources that are available in their home this can leads to difficulty for them to obtain nutritious food by them. housewives may have limited level of education as compared to government employee and merchant this may limit access to basic information about healthy diets, and available resources.
This study also showed that the odds of food insecurity were higher among low- and medium-income households than high income households respectively, which is consistent with studies in Canada (27), California and Chicago (28). This might be due to those who have low or middle income may face to buy necessary food items this may leads to food insecurity at their household. Often, they face difficult to make choices among different competing needs for instance between buying food items, for rent, transportation, health services and education.
Moreover, participants with a family history of DM were more likely to experience food insecurity compared to those without. This aligns with WHO findings indicating that offspring of individuals with T2DM have a higher risk of food insecurity (29). Study participants with family history of DM may have other members in their house who are diabetic which may lead them to financial catastrophe because it makes them to pay high costs for health services/drugs, monitoring materials like glucose meters and for diabetic related complications and at the end this leads to them to have less money for food. In addition, restricted type of foods is recommended for diabetic patients these recommended food types are costly as compared to other types of foods therefore this may affect food insecurity at the household level.
Furthermore, the odds of FI was reduced among study participants who have less than 5 family members as compared to those who have more than or equal to 5 family members. This might be because family’s with small number of members have low dependency ratio this reduces the burden among productive group in the family. They may also pay low cost/low expenses for food, education, transport, rent, and health care if they have family size. Having fewer family size could leads to greater per capital income because there are fewer family members who need support in the households this may decreases food insecurity at the household level.
Limitations of the study
The HFIAS questions relied on the respondents’ memory of events over the previous four weeks, which could introduce response and recall bias. Additionally, the cross-sectional design cannot establish a cause-and-effect relationship. Moreover, we have included so many independent variables in this study to identify the associated factors this may leads to in the interpretation and communication of the finding. For this reason, we have tried to focus on the most important variables in detail.
Conclusion
The proportion of food insecurity among adult diabetic patients in Gambella town public hospitals is high. Predictors of food insecurity include age, rural residence, literacy, housewife occupation, low and medium wealth status, non-membership in DM associations, nutritional education, longer DM duration, and family history of DM. Health professionals should emphasize self-management for individuals with a family history of DM to prevent complications and reduce healthcare costs. Encouraging participation in DM associations can enhance access to nutritional education and counseling. Moreover, higher officials should work to improve household income alongside other stakeholders.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Arba Minch University College of Medicine and Health Science (Protocol No: MT1443/2023). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
ZG: Writing – original draft, Writing – review & editing. YH: Writing – review & editing. MT: Formal Analysis, Methodology, Writing – review & editing. DM: Writing – review & editing. YC: Writing – review & editing. TT: Writing – review & editing. MG: Writing – review & editing. ES: Writing – review & editing. MW: Writing – review & editing. LT: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We want to express our heartfelt gratitude to Arba Minch University College of Medicine and Health Sciences and Gambella Teachers Education and Health Science College for providing ethical clearance and funding this research, respectively. We would also like to extend our thanks and appreciation to Gambella Town Public Hospitals, study participants, data collectors and supervisors for their tremendous contribution to achieve the data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Reeder N, Tapanee P, Persell A, and Tolar-Peterson T. Food insecurity, depression, and race: Correlations observed among college students at a university in the Southeastern United States. Int. J. Environ. Res. Public Health. (2020) 17:8268.
2. Haering SA and Syed SB. Community food security in United States cities: A survey of the relevant scientific literature. Center for a Livable Future. Baltimore, USA: Johns Hopkins Bloomberg School of Public Health (2009). Available at: https://wwwjhsphedu/sebin/s/c/FS_Literature%20Bookletpdf.
3. Gordon B. The impact of food insecurity on glycemic control among individuals with type 2 diabetes. BioMed. (2022) 2:170–80. doi: 10.3390/biomed2020016
4. Lee JS and Frongillo EA Jr. Nutritional and health consequences are associated with food insecurity among US elderly persons. J. Nutr. (2001) 131:1503–9.
5. Krupsky KL, Sliwa S, Seligman H, Brown AD, Liese AD, Demissie Z, et al. Adolescent health risk behaviors, adverse experiences, and self-reported hunger: Analysis of 10 states from the 2019 youth risk behavior surveys. J. hunger Environ. Nutr. (2024) 19:523–39. doi: 10.1080/19320248.2022.2088263
6. Zeleke Negera G and Charles Epiphanio D. Prevalence and predictors of nonadherence to diet and physical activity recommendations among type 2 diabetes patients in southwest Ethiopia: A cross-sectional study. Int. J. endocrinology. (2020) 2020:1512376.
7. WHO FIUW. The State of Food Security and Nutrition in the World 2024 Financing to end hunger, food insecurity and malnutrition in all its forms. (2024).
9. Gearhardt A N, Davis C, Kuschner R, and D. Brownell K. The addiction potential of hyperpalatable foods. Curr. Drug Abuse Rev. (2011) 4:140–5. doi: 10.2174/1874473711104030140
10. Organization WH. The state of food security and nutrition in the world 2019: safeguarding against economic slowdowns and downturns. Food & Agriculture Org (2019).
11. Nsimbo K, Erumeda N, and Pretorius D. Food insecurity and its impact on glycaemic control in diabetic patients attending Jabulani Dumani community health centre, Gauteng province, South Africa. Afr. J. Primary Health Care Family Med. (2021) 13:1–6. doi: 10.4102/phcfm.v13i1.2906
12. Mohammed MA and Sharew NT. Adherence to dietary recommendation and associated factors among diabetic patients in Ethiopian teaching hospitals. Pan Afr. Med. J. (2019) 33. doi: 10.11604/pamj.2019.33.260.14463
13. Cheng S, Kamano J, Kirui N, Manuthu E, Buckwalter V, Ouma K, et al. Prevalence of food insecurity in patients with diabetes in western Kenya. Diabetic Med. (2013) 30:e215–e22. doi: 10.1111/dme.2013.30.issue-6
14. Kushel MB, Gupta R, Gee L, and Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J. Gen. Internal Med. (2006) 21:71–7.
15. Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, and Wee CC. Food insecurity and metabolic control among US adults with diabetes. Diabetes Care. (2013) 36:3093–9. doi: 10.2337/dc13-0570
16. Tezera R, Sahile Z, Yilma D, Misganaw E, Amare E, and Haidar J. Food security status of patients with type 2 diabetes and their adherence to dietary counselling from selected hospitals in Addis Ababa, Ethiopia: A cross-sectional study. PloS One. (2022) 17:e0265523. doi: 10.1371/journal.pone.0265523
17. Mukai N, Doi Y, Ninomiya T, Hata J, Hirakawa Y, Fukuhara M, et al. Cut-off values of fasting and post-load plasma glucose and HbA1c for predicting Type 2 diabetes in community-dwelling Japanese subjects: the Hisayama Study. Diabetes Med. (2012). doi: 10.1111/j.1464-5491.2011.03378.x
18. WHO. Noncommunicable Disease Surveillance, Monitoring and Reporting. WHO (2024). Available at: https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps.
19. Kabakov E, Norymberg C, Osher E, Koffler M, Tordjman K, Greenman Y, et al. Prevalence of hypertension in type 2 diabetes mellitus: impact of the tightening definition of high blood pressure and association with confounding risk factors. J. cardiometabolic syndrome. (2006) 1:95–101. doi: 10.1111/j.1559-4564.2006.05513.x
20. Kharisma V and Abe N. Food insecurity and associated socioeconomic factors: Application of Rasch and binary logistic models with household survey data in three megacities in Indonesia. Soc. Indic. Res. (2020) 148:655–79. doi: 10.1007/s11205-019-02210-z
21. Coates J, Swindale A, and Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for measurement of food access: indicator guide: version 3. (2007).
22. Thomas MK, Lammert LJ, and Beverly EA. Food insecurity and its impact on body weight, type 2 diabetes, cardiovascular disease, and mental health. Curr. Cardiovasc. Risk Rep. (2021) 15:1–9.
23. Tabrizi JS, Nikniaz L, Sadeghi-Bazargani H, Farahbakhsh M, and Nikniaz Z. Socio-demographic determinants of household food insecurity among Iranian: a population-based study from northwest of Iran. Iranian J. Public Health. (2018) 47:893.
24. Shalowitz M, Eng J, McKinney C, Krohn J, Lapin B, Wang C, et al. Food security is related to adult type 2 diabetes control over time in a United States safety net primary care clinic population. Nutr. diabetes. (2017) 7:e277–e. doi: 10.1038/nutd.2017.18
25. Janzadeh H, Mozaffari-Khosravi H, and Javadi M. The association of food insecurity, inflammation, and several socioeconomic factors with type 2 diabetes: A case-control study. J. Nutr. Food security. (2020) 5:38–46.
26. Mendoza JA, Haaland W, D'Agostino RB, Martini L, Pihoker C, Frongillo EA, et al. Food insecurity is associated with high risk glycemic control and higher health care utilization among youth and young adults with type 1 diabetes. Diabetes Res. Clin. practice. (2018) 138:128–37. doi: 10.1016/j.diabres.2018.01.035
27. Bawadi HA, Ammari F, Abu-Jamous D, Khader YS, Sa B, and Tayyem RF. Food insecurity is related to glycemic control deterioration in patients with type 2 diabetes. Clin. Nutr. (2012) 31:250–4.
28. Fekadu G, Bula K, Bayisa G, Turi E, Tolossa T, and Kasaye HK. Challenges and factors associated with poor glycemic control among type 2 diabetes mellitus patients at Nekemte Referral Hospital, Western Ethiopia. J. Multidiscip. healthcare. (2019), 963–74. doi: 10.2147/JMDH.S232691
Keywords: food insecurity, diabetic patients, cross-sectional study design, Gambella town, Ethiopia
Citation: Girma Z, Teka M, Misker D, Chisha Y, Gujo MM, Shibru E, Wakeyo MU, Timiketu L, Toma T M and Haile Y (2025) Assessment of food insecurity and its associated factors among adult diabetic patients in Gambella town public hospital, South Western Ethiopia, 2023. Front. Clin. Diabetes Healthc. 6:1493312. doi: 10.3389/fcdhc.2025.1493312
Received: 12 January 2025; Accepted: 09 June 2025;
Published: 08 September 2025.
Edited by:
Margarida Liz Martins, Coimbra School of Health Technology, PortugalReviewed by:
Hui Liew, University of Nebraska at Kearney, United StatesAncah Caesarina Novi Marchianti, University of Jember, Indonesia
Copyright © 2025 Girma, Teka, Misker, Chisha, Gujo, Shibru, Wakeyo, Timiketu, Toma and Haile. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zeleke Girma, emVsZWtlZ2lybWE0QGdtYWlsLmNvbQ==
 Zeleke Girma
Zeleke Girma Mehari Teka2
Mehari Teka2 Yilma Chisha
Yilma Chisha Mintesinot Melka Gujo
Mintesinot Melka Gujo Mamud Umer Wakeyo
Mamud Umer Wakeyo Temesgen Mohammed Toma
Temesgen Mohammed Toma Yosef Haile
Yosef Haile