- 1Department of Physiology, Faculty of Basic Medical Sciences Baze University, Abuja, Nigeria
- 2Department of Biochemistry and Forensic Science, Faculty of Natural and Applied Sciences, Abiola Ajimobi Technical University, Ibadan, Nigeria
- 3Department of Human Physiology, Faculty of Basic Medical Sciences, College of Health Sciences, Federal University Wukari, Wukari, Nigeria
- 4Department of Community Medicine, Kaduna State University, Kaduna, Nigeria
- 5Department of Biosciences and Biotechnology, University of Medical Sciences, Ondo, Nigeria
- 6Department of Medicinal Chemistry & Quality Control, National Institute for Pharmaceutical Research and Development (NIPRD), Abuja, Nigeria
- 7Department of Medical Laboratory Science, McPherson University, Seriki Sotayo, Ogun State, Nigeria
- 8Nigerian Institute of Medical Research Foundation, Yaba, Lagos State, Nigeria
- 9Clinical Sciences Department, Lead City University, Ibadan, Nigeria
Background: Diabetic nephropathy (DN) is one of the most frequent microvascular consequences of diabetes, accounting for a significant portion of morbidity and mortality in diabetic patients in Africa. This study aims to report on the prevalence of nephropathy among patients with diabetes mellitus patients in Africa and the risk factors.
Methods: This systematic review was reported using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standards, and the protocol was pre-registered in PROSPERO with the registration number CRD42024587467. The search was conducted across databases such as PubMed, Google Scholar, CINAHL and Scopus to retrieve studies published between January 2000 and August 2024. All statistical analyses were conducted using R software (version 4.4.2). The pooled prevalence of nephropathy in patients with diabetes was calculated with a 95% confidence interval (CI).
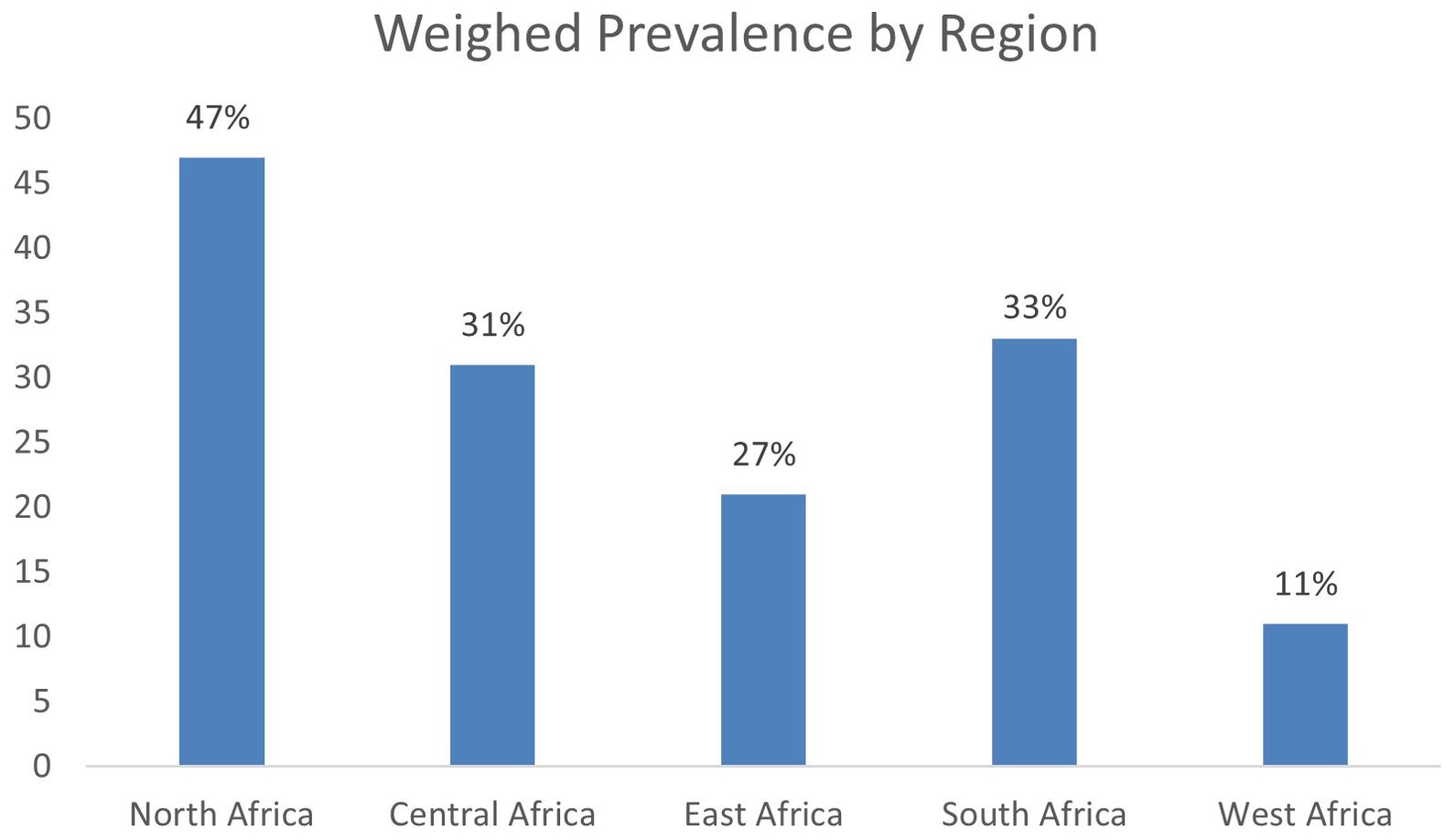
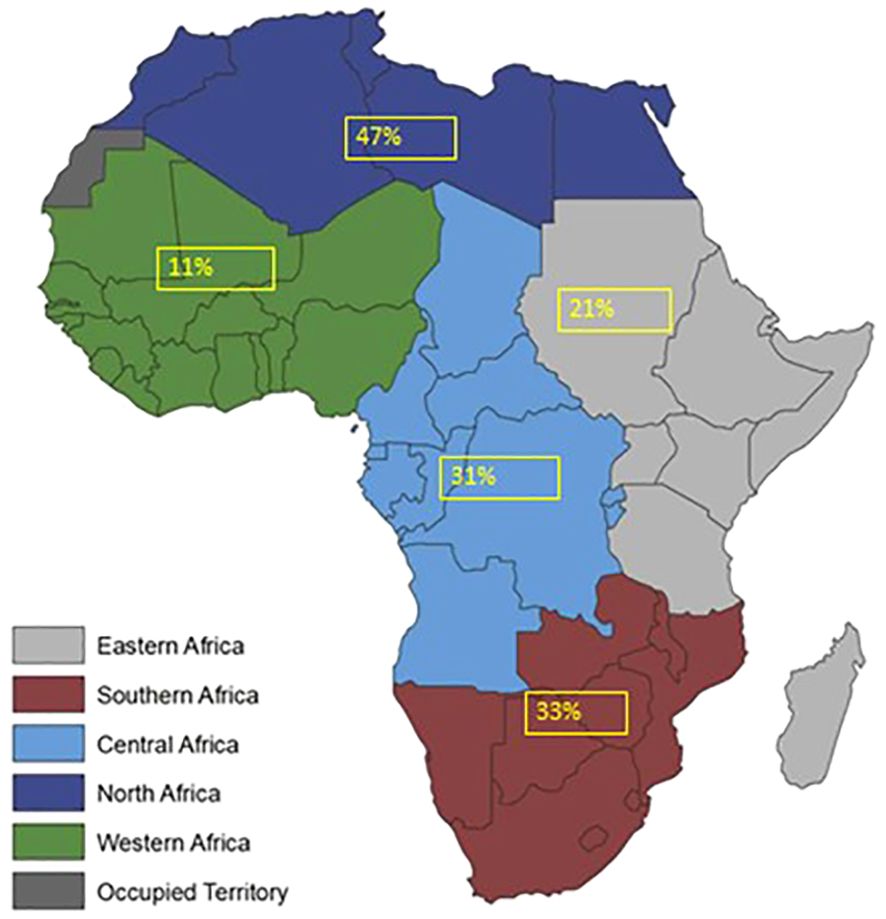
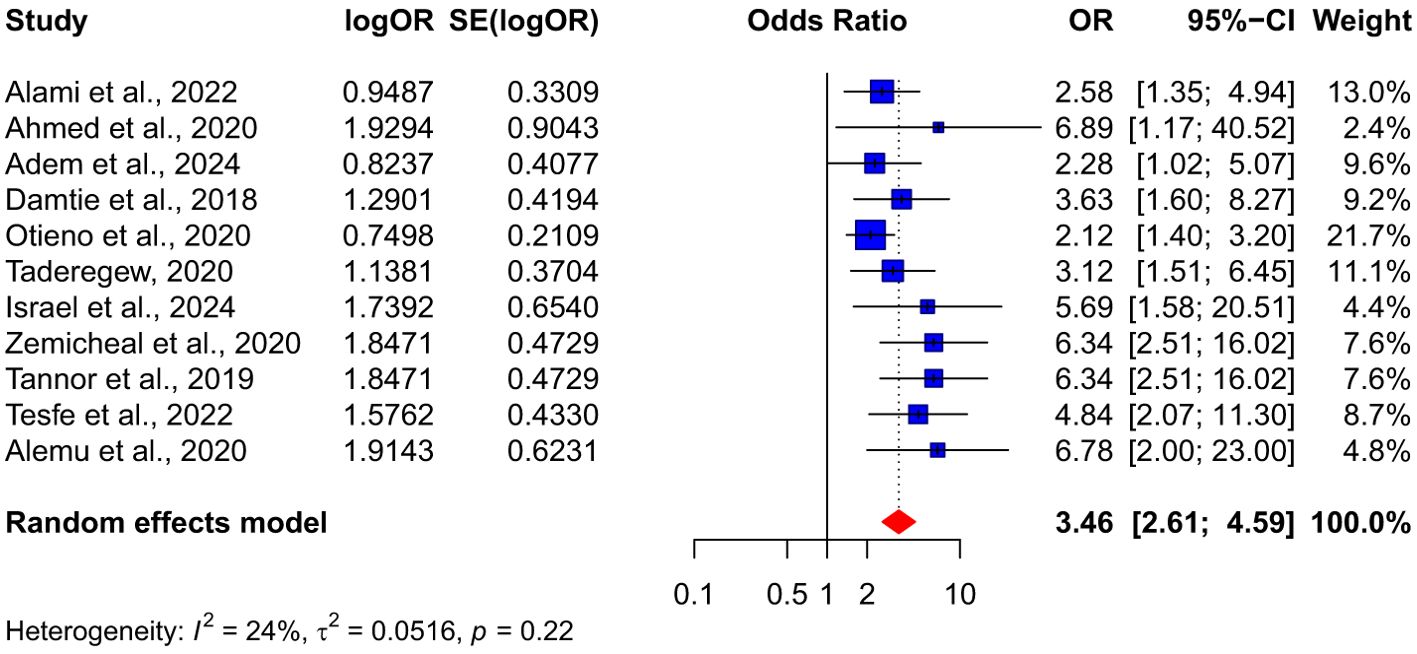
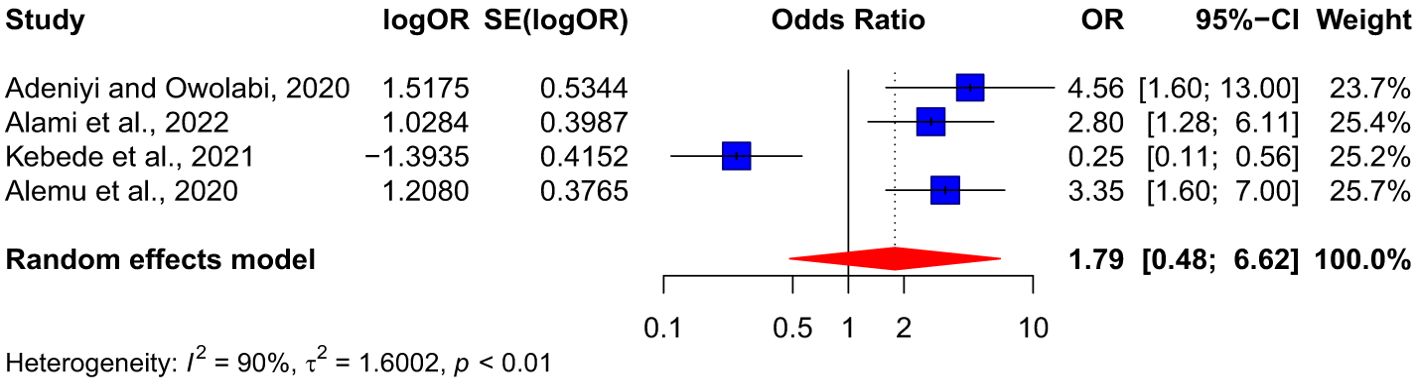
Results: Thirty-four (34) articles met the inclusion criteria. Only 28 studies were incorporated into the meta-analysis to determine the pooled prevalence of nephropathy among diabetes patients. The findings indicated a pooled prevalence of 21% (95%, CI: 16-28) of nephropathy among diabetes patients. Among type 1 and type 2 diabetes patients, the pooled prevalence of nephropathy is 46% (95%, CI: 18-77, I² = 98%) and 20% (95% CI: 14-27, I² = 98%), respectively. Weighted prevalence of 47%, 31%, 33% and 11% were reported in North Africa, Central Africa, South Africa and West Africa respectively. The result also showed that diabetes patients with hypertension are more than three times at risk of developing nephropathy compared to those without hypertension OR:3.46 (95% CI: 2.61-4.59).
Conclusion: The current study showed the prevalence of nephropathy with a significant association with hypertension among diabetic mellitus patients. Higher prevalence in North Africa is likely due to Western cultural impacts on dietary consumption.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, identifier CRD42024587467.
1 Introduction
Diabetes mellitus (DM) is a chronic metabolic disorder characterized by either insulin deficiency due to the destruction of pancreatic islet beta cells or by insulin resistance, where the body fails to use the insulin available (1) effectively. With the global prevalence of DM reaching 10.5% among adults aged 20 to 79 impacting approximately 440 million people—diabetes has become a critical public health issue worldwide (2). Projections suggest that over 550 million people will be affected by 2035, intensifying the urgency for effective management and prevention of its complications (2, 3).
Diabetic nephropathy (DN), a microvascular complication of diabetes, significantly contributes to morbidity and mortality among individuals with diabetes (4–6). DN is a leading cause of end-stage renal disease (ESRD) globally, accounting for 12% to 55% of all ESRD cases (4, 7, 8). While it affects 30-40% of those with type 1diabetes and 10-20% of those with type 2 diabetes (9), the sheer prevalence of type 2 diabetes means that the majority of ESRD cases occur in this population. Additionally, age-related decline in kidney function and comorbid conditions, such as hypertension, further elevate the risk of kidney complications in type 2 diabetes patients, particularly in older adults (10).
While several studies have assessed chronic kidney disease (CKD) prevalence in African populations, results have varied across countries and patient groups, highlighting the complex interaction between diabetes and nephropathy in the region. Studies in Ethiopia (11–14), Nigeria (15, 16), Ghana (10, 17), Tanzania (18), and the Democratic Republic of Congo (19) report a range of CKD prevalence among people with diabetes, yet these data are often fragmented and inconsistent in methodology. Furthermore, risk factors, demographic influences, and regional variations within Africa remain underexplored comprehensively and systematically.
This systematic review and meta-analysis aim to fill this gap by determining the prevalence of nephropathy among diabetic patients across African nations. By synthesizing available evidence, we examined the region-specific risk factors that potentiate DN incidence among patients with DM in Africa, offering critical insights for regional healthcare planning and targeted interventions.
2 Methods
2.1 Protocol registration
This systematic review was reported using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standards. The protocol was pre-registered in PROSPERO with the registration number CRD42024587467.
2.2 Review question
What is the prevalence of nephropathy among patients with diabetes mellitus in Africa?
What are the factors contributing to the prevalence of nephropathy among patients with diabetes mellitus in Africa?
2.3 Main study outcomes
2.3.1 Primary outcome
1. Pooled prevalence estimates of diabetes nephropathy among diabetes mellitus patients
2. Risk factors associated with nephropathy in Africa
2.3.2 Secondary outcomes
1. Regional prevalence of nephropathy among diabetes patients
2. Prevalence of diabetes nephropathy by diabetes mellitus type
3. Prevalence of diabetes nephropathy based on gender of diabetes patients
2.4 Search strategy
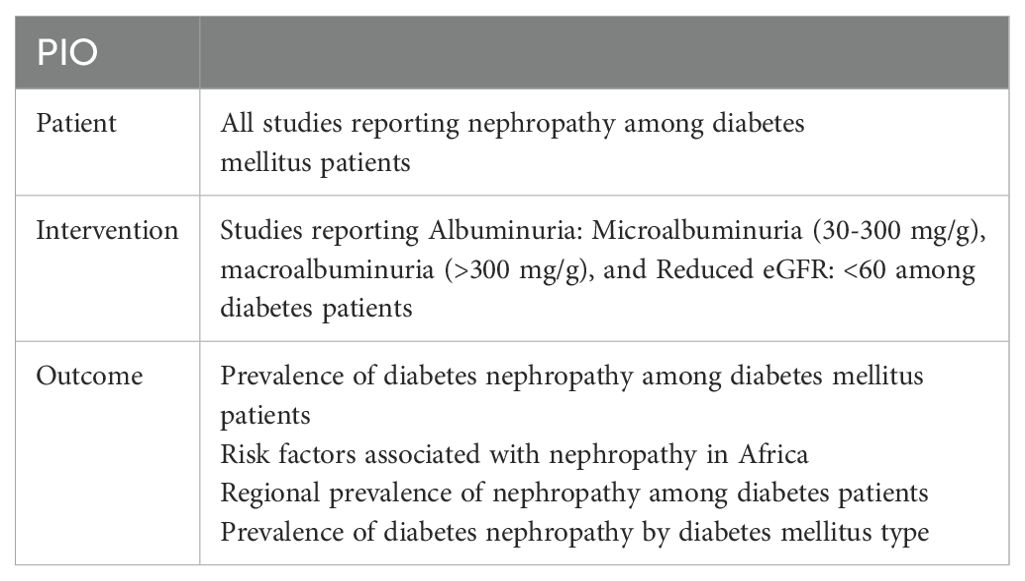
The PICO framework was utilized before searching for relevant articles to frame and structure the research concepts and develop the search terms. Each component of the PICO framework and the search terms are shown in Table 1. The search strategy involves utilizing specific keywords across various databases, such as PubMed, Google Scholar, CINAHL (Cumulative Index to Nursing and Allied Health Literature), and Scopus, to retrieve relevant literature.
The search across the databases involved careful formulation of search queries combined with Boolean operators like ‘AND’’ and ‘OR.’’ The search queries were thereafter submitted into the selected databases to retrieve studies published between January 1, 2000, and August 31st, 2024, on the prevalence of nephropathy among diabetes patients in Africa. The search included all studies published in African lingua franca. The search strategy is shown in Supplementary Table 1.
2.5 Inclusion and exclusion criteria
The systematic review included Cross-sectional studies, Cohort studies (prospective or retrospective), and Case-control studies. Studies that met the eligibility criteria were included and uploaded to Rayyan, a collaborative systematic literature review web tool (20). Before the article screening, the level of agreement between the reviewers was evaluated using kappa scores. Thereafter, two independent reviewers (G.I.G., P.I.A) removed duplicate articles and screened the titles and abstracts for suitability before the full-text screening. In contrast, the third reviewer (L.D.A) resolved conflicts through discussion or consultation. A similar approach was used for full-text screening. The list of excluded studies is provided in Supplementary Table 2.
2.6 Study selection and screening
The selection of studies was based on preset inclusion and exclusion criteria. In addition to the study designs already described will be included, studies conducted in hospital settings, community-based, studies with nephropathy directly related to diabetes as an outcome, population ≥100, studies that clearly define nephropathy, provide quantitative data on the prevalence of diabetes nephropathy, reports on the contributing/risk factors for nephropathy and prevalence, conducted among Africans were selected. Articles published in other languages aside from English were translated into English with the help of a translator, while articles not freely available were retrieved using a university subscription. Overall, the article selection followed a strict process to answer the research questions and achieve the objectives.
2.7 Data extraction
Data extraction was performed using a pre-tested form prepared in Microsoft Excel. The reviewers (G.I.G., P.I.A, L.D.A) extracted information including article title, first author’s surname, publication year, country, geographical region of the study, study setting, sample size, sample size by gender, study design, the mean age of participants, type of diabetes, duration of diabetes, nephropathy definition, number of confirmed nephropathy cases, risk factors, number of controlled and uncontrolled diabetes from the selected articles in the Supplementary Table 3.
2.8 Assessment of risk of bias in included studies
The methodology quality of the included studies was assessed by adapting the JBI critical appraisal checklist for studies reporting prevalence data (21). Two reviewers assessed methodological quality and risk of bias in the included studies, while a third reviewer resolved discrepancies. The nine-quality domain of the assessment checklist was ranked to score the included articles as either high, moderate, or low in Supplementary Table 4.
2.9 Dealing with missing data
For missing data in included studies, such as failure to report a particular outcome, such study was excluded from the analysis of such outcome. When a study has missing data and such data are unavailable, we conduct subgroup analyses to explore how missing data might influence results.
2.10 Statistical analysis
All statistical analyses were conducted using R software (version 4.4.2). The pooled prevalence of nephropathy in patients with diabetes was calculated with a 95% confidence interval (CI). When at least two studies from the same region reported nephropathy prevalence among diabetes patients, a weighted prevalence was used to determine the overall prevalence in each region. Odds ratios (OR) were utilized to explore potential risk factors, including underlying hypertension and a duration of diabetes greater than 10 years.
Statistical heterogeneity among studies was assessed using Cochran’s Q test and the I² statistic. A P-value of <0.1 for the Q test and an I² value greater than 50% indicated statistically significant heterogeneity. Given the anticipated heterogeneity, a random-effects model was employed to pool all outcomes, providing a more conservative estimate of prevalence. Kappa statistics were used to assess inter-rater agreement between reviewers during the study inclusion process.
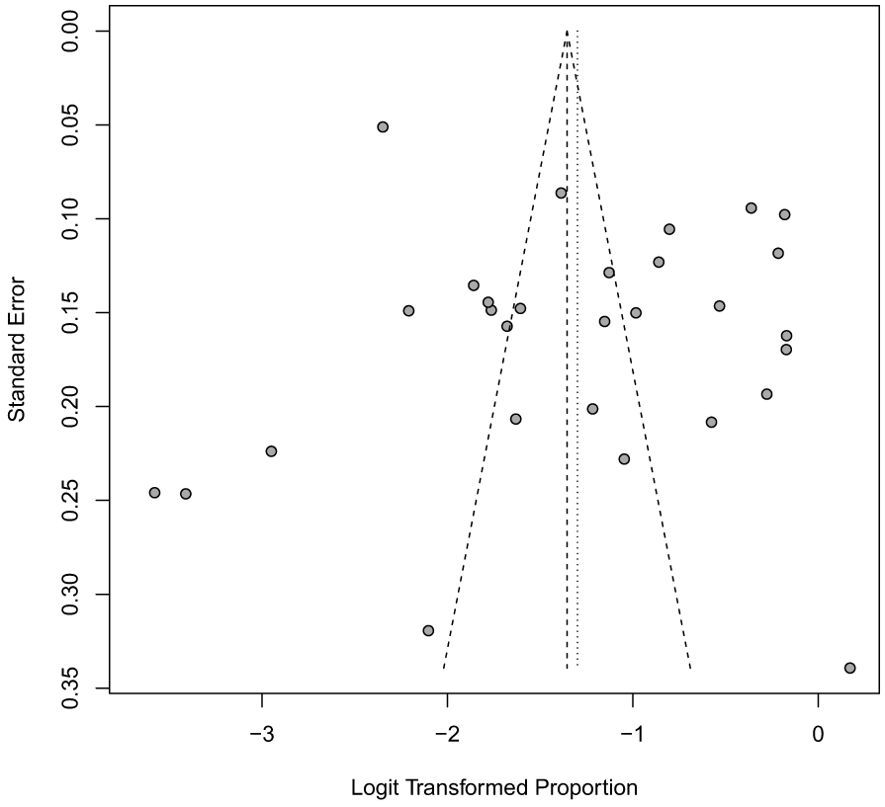
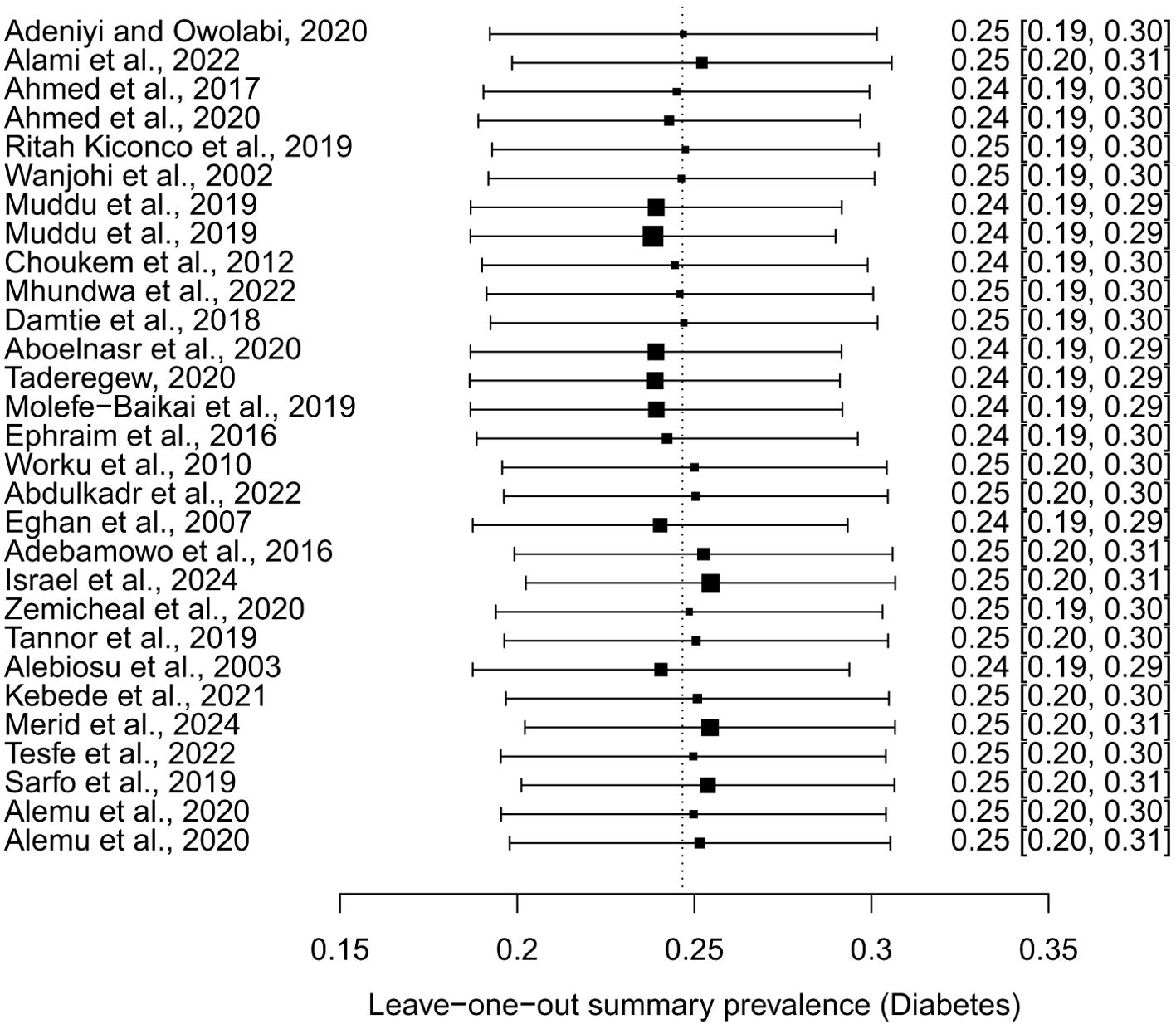
2.11 Publication bias and sensitivity analysis
Funnel plots were used to assess publication bias for the primary outcome. A leave-one-out analysis, systematically excluding each study, was performed to evaluate the robustness of the results and assess the impact of individual studies on the pooled prevalence.
3 Results
3.1 Selection of studies
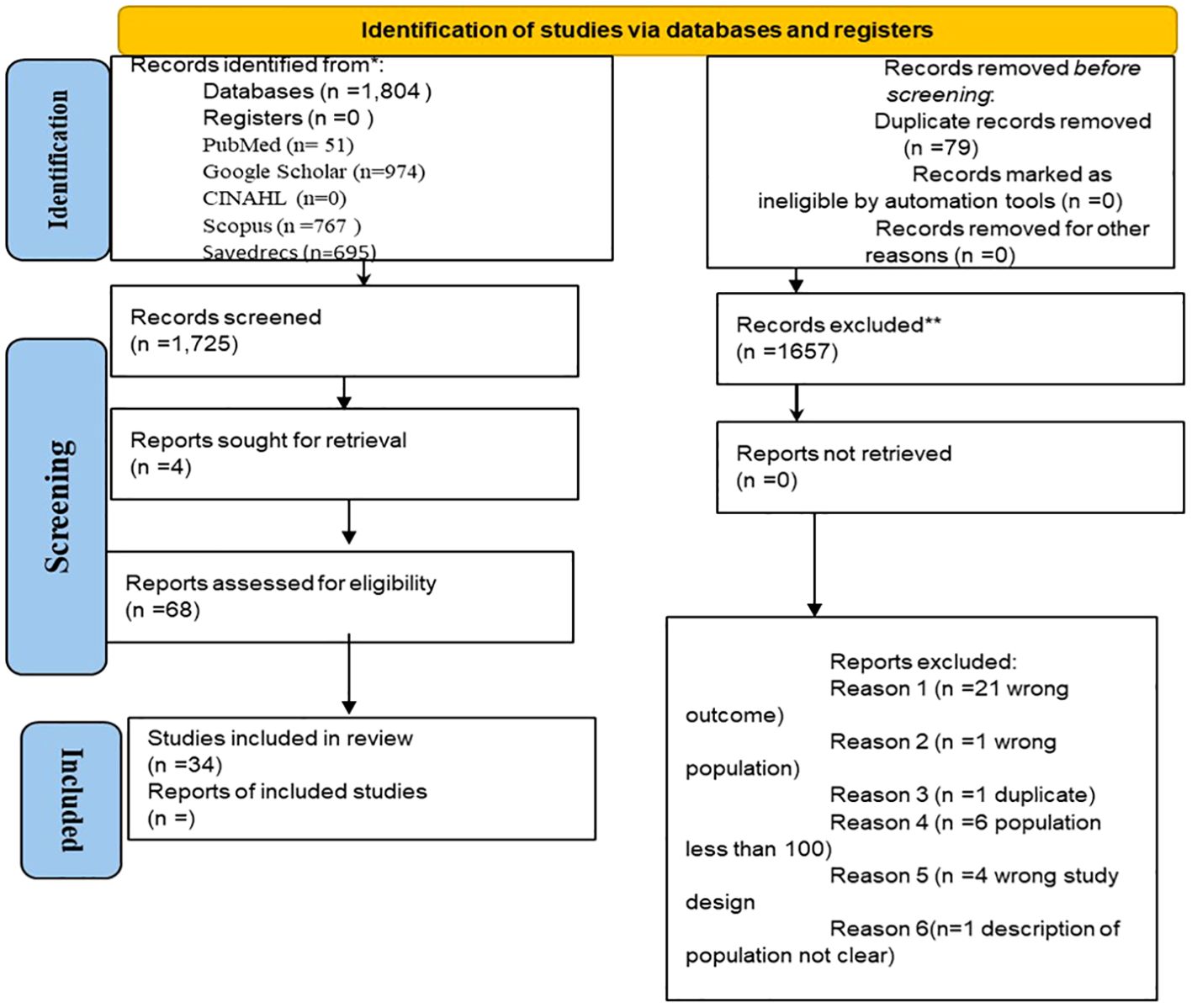
Electronic searches retrieved one thousand eight hundred and four (1,804) records (see Figure 1). Seventy-nine (79) duplicate records were removed, leaving 1,725 articles for screening. A total of 1,657 articles were excluded based on the title and abstract, while the full-text record of the remaining 68 studies was obtained for full-text evaluation. Based on population size, ambiguity of study design and the study outcome, 34 were excluded. The selected 34 articles met the inclusion criteria, clearly revealing the study population and prevalence of diabetic nephropathy (See Figure 1).
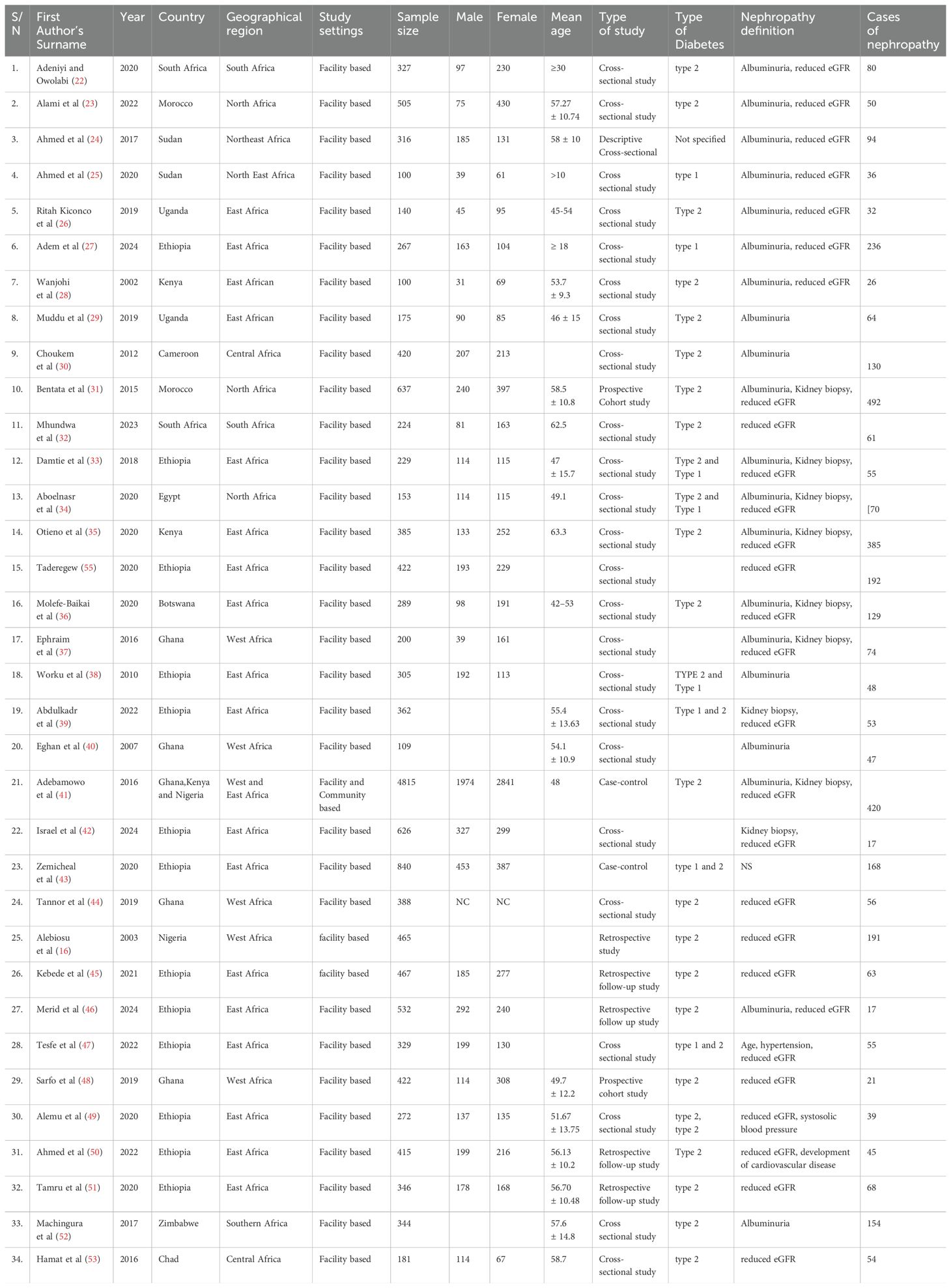
3.2 Characteristics of the articles included in this study
The characteristics of the articles included in this study were summarized in Tables 2, 3. The thirty-four (34) articles were published in 2002 and 2024. Of all the studies, 25 (73.5%) were cross-sectional designs (22–30, 32–40, 42, 44, 47, 49, 52, 53, 55), 5 (14.7%) were retrospective follow up (45, 46, 50, 51, 54), 2 (5.9%) were cohort (31, 48) and 2 (5.9%) case-control studies (41, 43) (See Table 3). Most of the included studies were facility-based studies.
The studies covered 12 different countries from the various geographical regions of Africa. More than half of the studies 18 (52.9%) were reported from the East Africa region. The captured East African countries included Ethiopia 13 (38.2%) (27, 33, 38, 39, 42, 43, 45–47, 49–51, 55), Uganda 2 (5.9%) (26, 29), Kenya 2 (5.9%) (28, 35) and Botswana 1 (2.9%) (36). West Africa and North Africa regions respectively had 5 (14.7%) of the studies performed in countries like Ghana 4 (11.8%) (37, 40, 44, 48) and Nigeria 1 (2.9%) (54) and North African countries like Morocco 2 (5.9%) (23, 31), Sudan 2 (5.9%) (24, 25) and Egypt 1 (2.9%) (34). Other regions covered in the selected articles are Southern Africa 3 (8.8%) with the record from South Africa 2 (5.9%) (22, 32), and Zimbabwe 1 (2.9%) (54), as well as Central Africa 2 (5.9%) region which had 1 (2.9%) (30) of the record from Cameroon and 1 (2.9%) (53) from Chad. A study conducted in sub-Saharan Africa (2.9% of total data) was drawn from three countries: Nigeria, Ghana, and Kenya.”
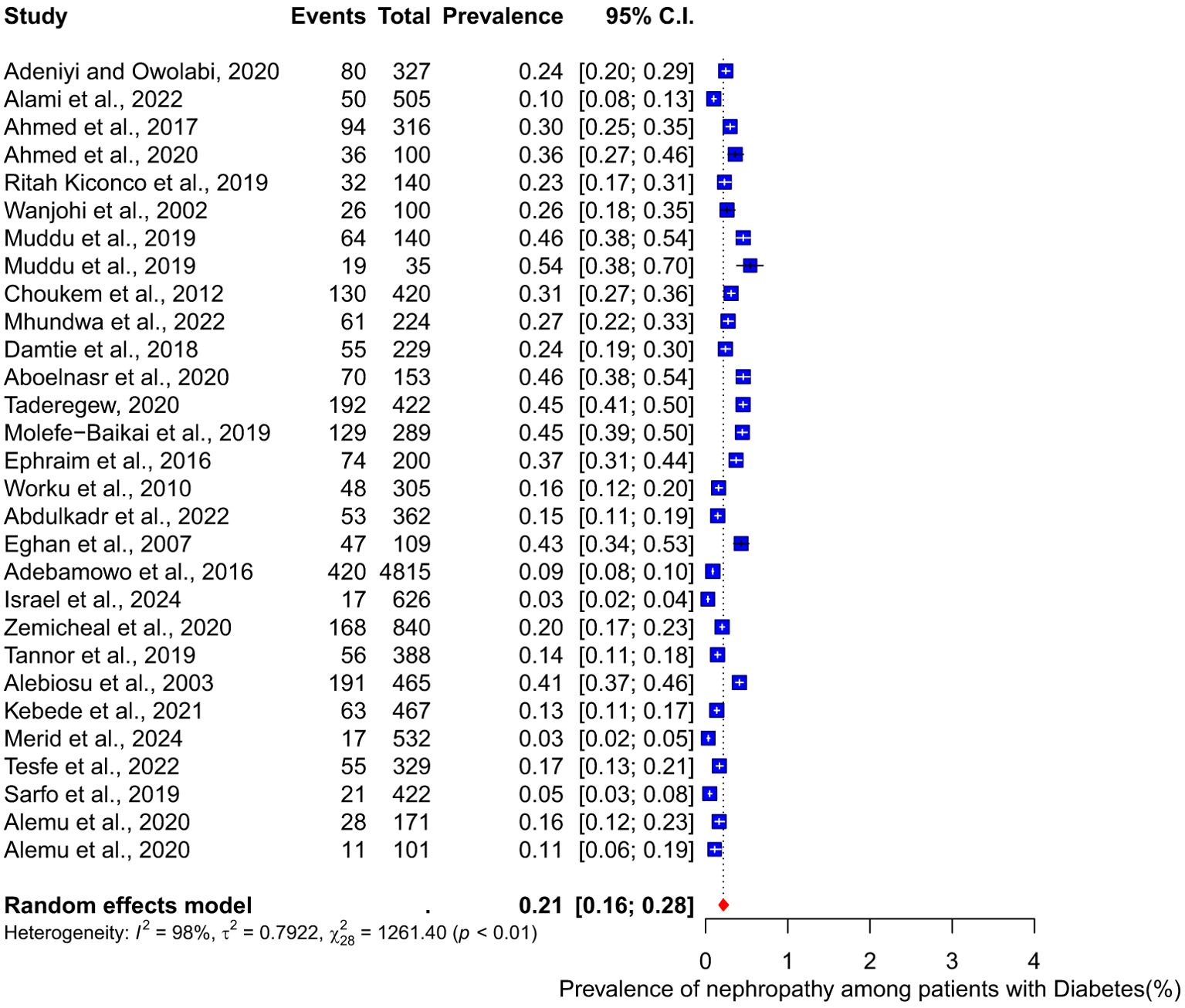
3.3 Prevalence of nephropathy among diabetes patients
This meta-analysis incorporated 28 studies to determine the pooled prevalence of nephropathy among diabetes patients. The findings indicated a pooled prevalence of 21% (95% CI 16-28) of nephropathy among diabetes patients with a substantial heterogeneity (I2 = 98%) (Figure 2).
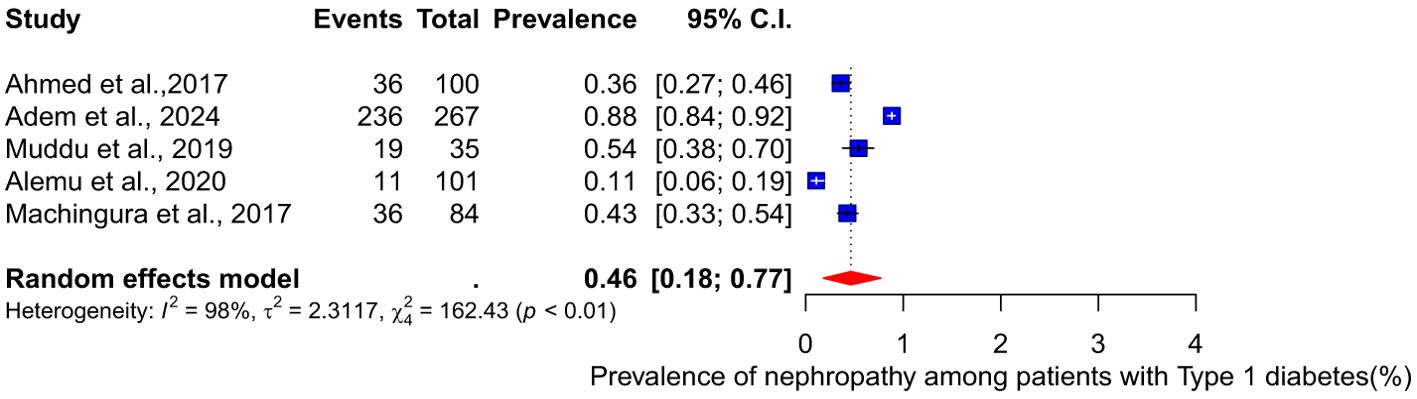
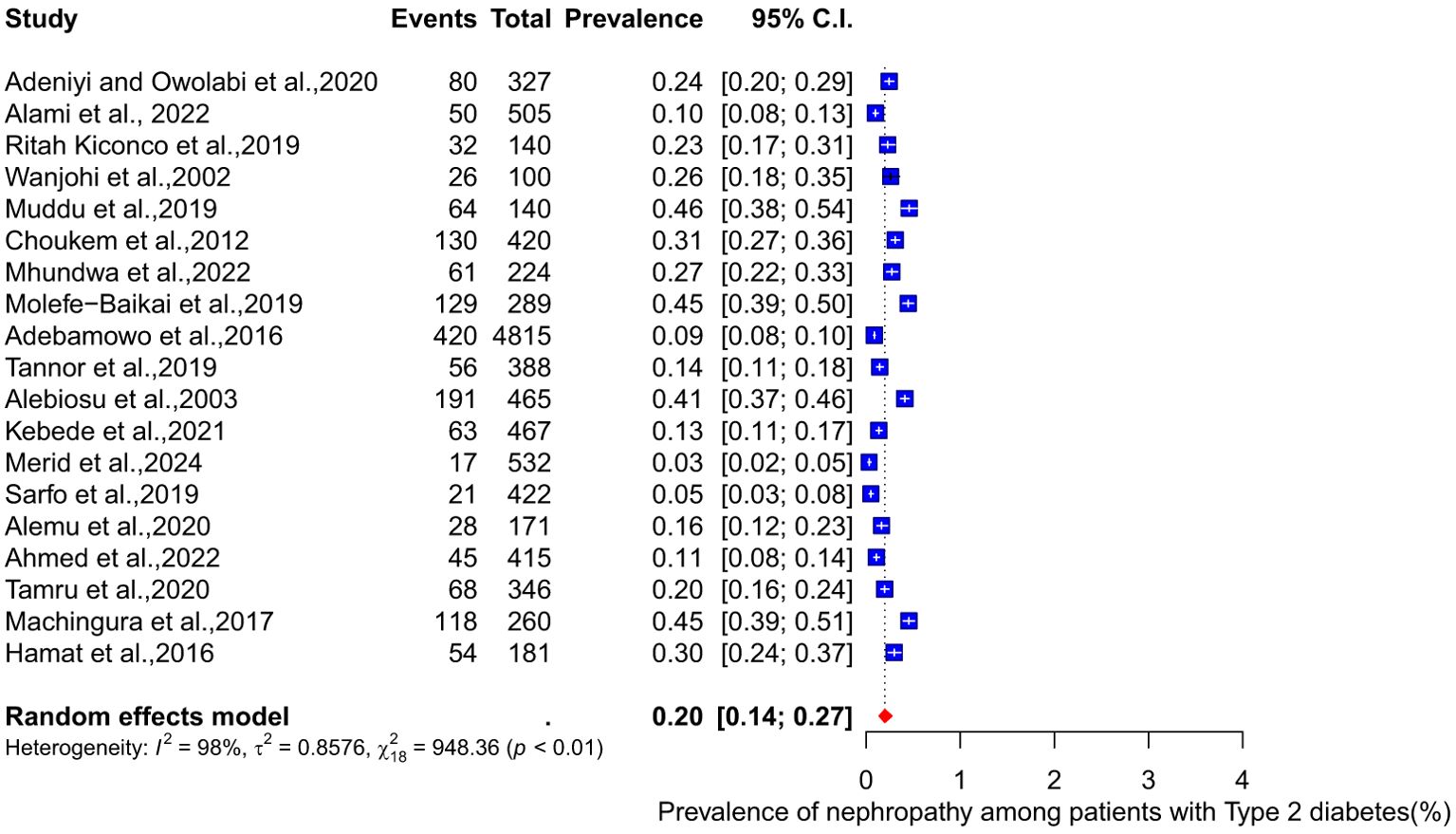
3.4 Prevalence of nephropathy based on type of diabetes
The pooled prevalence of nephropathy among patients with different types of diabetes (type 1 and type 2) was conducted. Among type 1 diabetes patients, the pooled prevalence of nephropathy is 46% (95% CI: 18-77, I² = 98%) (see Figure 3). For type 2 diabetes patients, the meta-analysis of eighteen studies shows a pooled prevalence of 20% (95% CI: 14-27, I² = 98%) (Figure 4).
3.5 Prevalence of nephropathy by gender
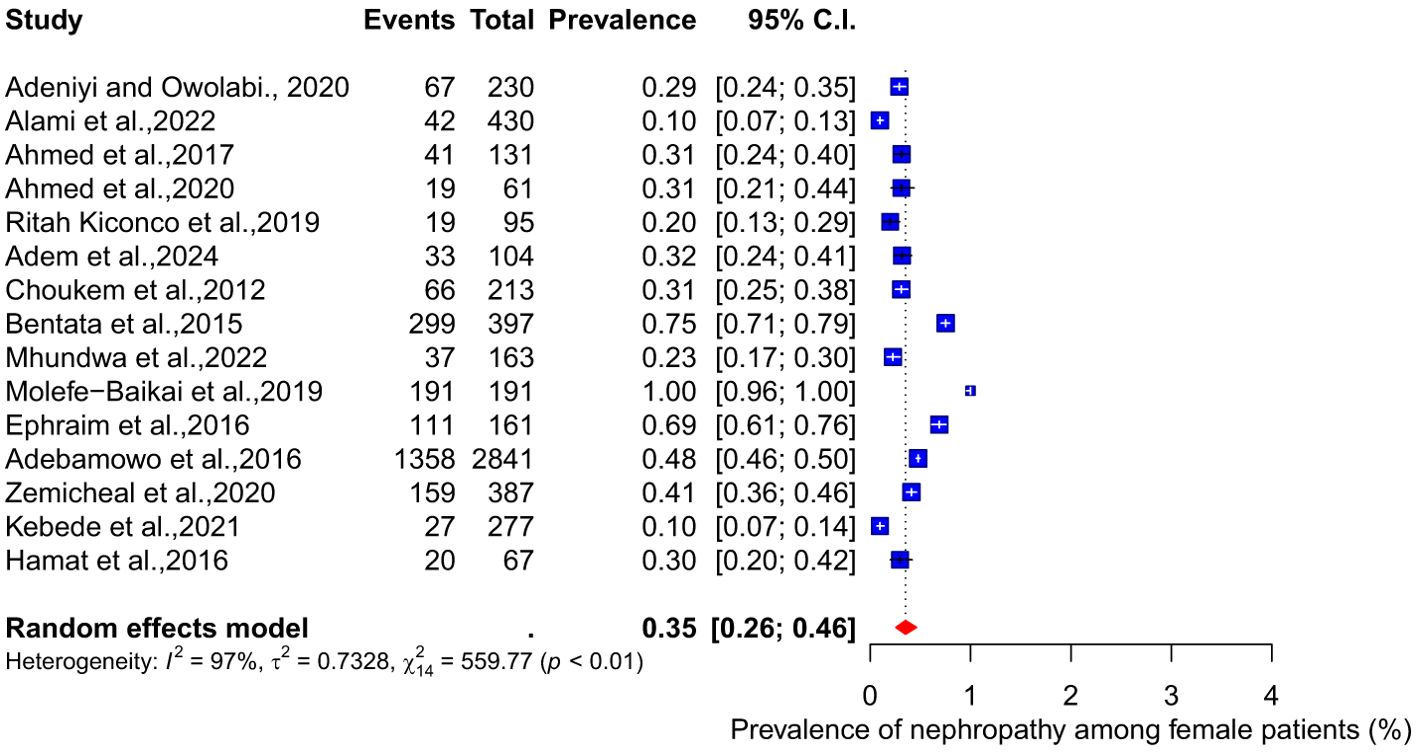
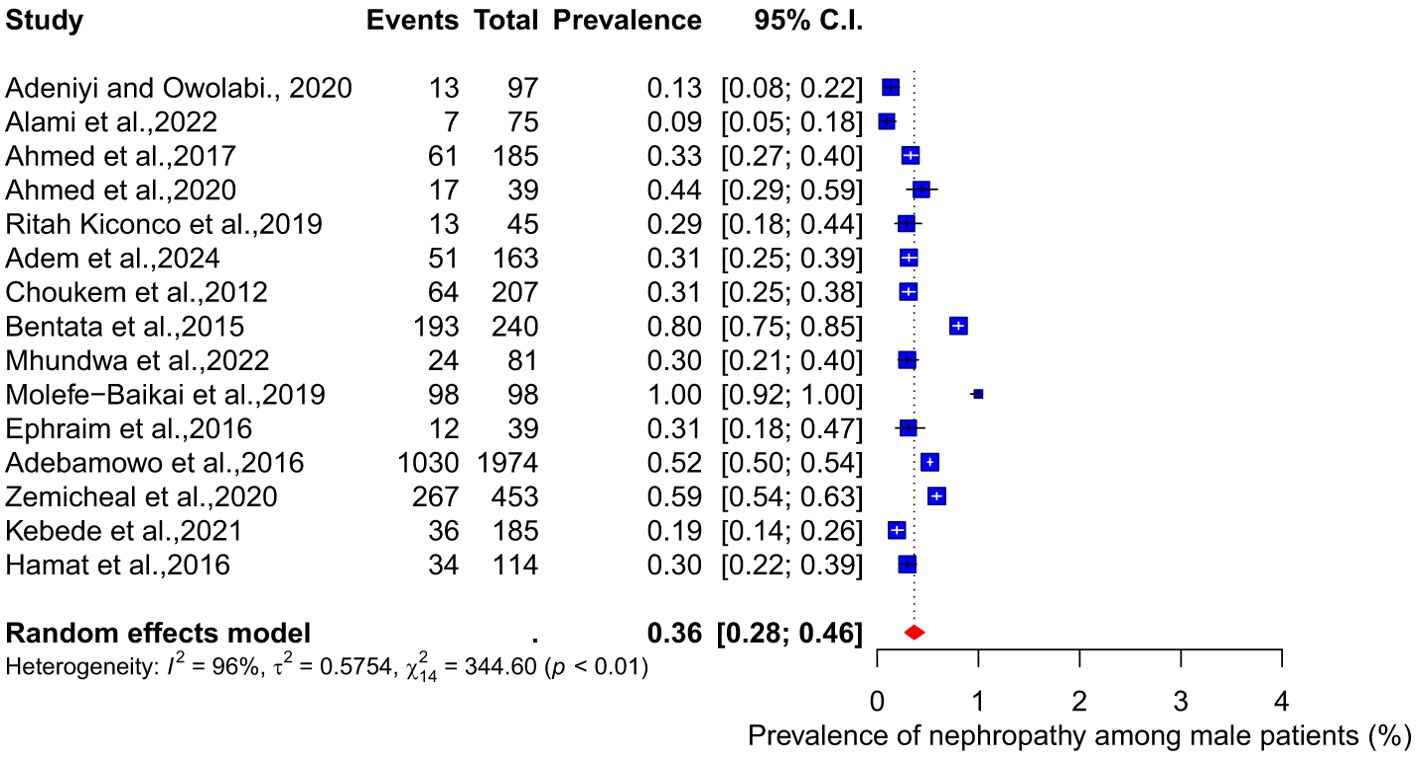
There were no significant differences in the pooled prevalence of nephropathy between male and female diabetes patients. The meta-analysis results show a pooled prevalence of 35% (95% CI: 26-45, I² = 97%) among female diabetes patients, while the pooled prevalence among male diabetes patients is 36% (95% CI: 28-46, I² = 96%) (see Figures 5, 6).
3.6 Prevalence of nephropathy by region
The weighted prevalence of nephropathy among diabetes patients varies across African regions. In North Africa, three studies with a total sample size of 1,295 reported a weighted prevalence of 47%. In Central Africa, two studies involving 601 participants indicated a prevalence of 31%. Eighteen studies conducted in East Africa, with a combined sample size of 5,453, found a prevalence of 21%. In South Africa, the weighted prevalence reported by four studies was 33%. Lastly, four studies in West Africa, with a total sample size of 6,090, showed a prevalence of 11% (see Figures 7, 8).
3.7 Association between hypertension and nephropathy among diabetes patients
The results of the meta-analysis showed a significant association between hypertension and nephropathy among diabetes patients. The pooled effect size from 11 studies indicated that diabetes patients with hypertension are more than three times at risk of developing nephropathy compared to those without hypertension OR:3.46 (95% CI: 2.61-4.59). Furthermore, the analysis identified no substantial heterogeneity, evidenced by an I2 value of 24% (see Figure 9).
3.8 Association between duration of diabetes and nephropathy
The pooled effect size from four studies indicated that having diabetes for more than 10 years does not have a significant association with developing nephropathy, with OR: 1.79 (95% CI: 0.48–6.62) (See Figure 10). However, the results had substantial heterogeneity, as indicated by an I² value of 90%.
3.9 Publication bias and sensitivity analysis
The funnel plot indicated significant asymmetry (Figure 11). However, a leave-one-out analysis of the prevalence of nephropathy among diabetes patients was conducted to assess the impact of individual studies on the pooled prevalence. The results showed that the weighted prevalence remained consistent with the original summary prevalence. This suggests that the conclusion drawn from this meta-analysis should be interpreted with caution (See Figure 12).
3.10 Risk of bias assessment for the included studies
The thirty-four (34) included articles were assessed for risk of bias and methodological quality by adapting the JBI critical appraisal checklist for studies reporting prevalence data. Each checklist was assigned a score of 1, and the overall score was 9. The articles were appraised, and each study obtained a maximum score of 9. On the quality scale, a score between ≤5 was deemed ‘high risk’’, six was deemed ‘moderate risk’’ and a score of ≥7 was deemed ‘low risk’’. Only 4(11.8%) of the articles were deemed to have a ‘high risk’’ of bias, whereas 26(76.5%) of the articles fell into the ‘low risk’’ bias. Finally, 4(11.8%) of the articles were determined to have a moderate risk of bias with a score of 6 out of 9 (Supplementary Table 4).
4 Discussion
The prevalence of nephropathy among diabetes mellitus patients in Africa, as well as the risk factors associated with its development, are underreported. Diabetic nephropathy is one of the most prevalent and dangerous diabetes mellitus complications. However, there has been a paucity of reliable statistics on its prevalence among diabetes mellitus patients and the risk factors contributing to its development in African regions. This paucity of data could be associated with a lack of serious documentation or renal registries (56). The main objectives of this study were to evaluate the prevalence of nephropathy among diabetes mellitus patients in Africa and further understand the contributing factors to the development of nephropathy. The current study identified 34 relevant articles published from 2000 to 2024 on the prevalence of nephropathy among diabetes mellitus patients in Africa and various risk factors enhancing its development.
The pooled prevalence of diabetes nephropathy reported was from 28 eligible studies, and as clearly observed in the result, the pooled prevalence of diabetes nephropathy was 21% (95% CI 16-28), indicating a substantial burden of diabetes nephropathy in Africa. This prevalence is higher than reported in the systematic review and meta-analysis conducted (57) in Asia. The significant heterogenicity (I² = 98%) observed in the study highlights the variation in study populations and geographical locations.
Furthermore, the prevalence of nephropathy varied between the two types of diabetes mellitus studied. In type 1, the pooled prevalence was significantly higher, 46% (18-77, I² = 98%), than the 20% (95% CI: 14-27, I² = 98%) prevalence observed among type 2 diabetes patients. A report by Wu et al. (58) stated that adults with Type 2 diabetes mellitus had a prevalence of 38.3% from 2007-2012, whereas Elhafeez et al. (59) reported that the pooled prevalence among type 2 diabetes mellitus patients was 24.7% (95% CI 23.6–25.7%). Contrary to these reports, our findings from the review and meta-analysis of 28 articles published between 2002 and 2024 showed a higher prevalence of diabetes nephropathy among type 1 diabetes patients. This disparity may be attributed to differences in disease duration, glycaemic control, and genetic predisposition. The higher prevalence in type 1 diabetes patients underscores the need for intensified monitoring and early intervention. To further elaborate on the factors that might contribute to heterogeneity observed in the results, it is important to emphasize variation in the geographical location and countries of the 28 studies represented in the analysis. Additionally, the characteristics of the study population, including variations in age, sex, ethnicity, genetic variably and socioeconomic status, contributed to the heterogeneity (60–62). The study design also varied, with both cross-sectional and cohort studies included. Furthermore, differences in methodology, such as data collection tools, added to the heterogeneity. The duration and severity of the disease also impacted on the prevalence of diabetic nephropathy (61), contributing to the variations observed. Lastly, differences in prevalence between type 1 and type 2 diabetes patients also played a significant role in heterogeneity. To address possible bias, a funnel plot which may indicate that studies with significant results are overrepresented in literature, while those with non-significant results are underrepresented was conducted. The funnel plot revealed significant asymmetry, suggesting potential publication bias. To address this concern, a leave-one-out sensitivity analysis was performed, which removed each study individually from the meta-analysis and recalculated the pooled prevalence. The results showed that the weighted prevalence remained consistent with the original summary prevalence, indicating that no single study had a disproportionate influence on the overall estimate. While this finding provides reassurance about the robustness of the results, caution is still warranted when interpreting the findings.
A 5-year retrospective study by Zhang et al. (63) stated that the prevalence of nephropathy and changes in renal activity was greater in women than men, indicating gender differences in the prevalence of nephropathy in Type 2 diabetes. Moreover, it was noted that women showed a more pronounced loss in renal function with an increase in follow-up duration. In men, the prevalence of nephropathy in type 2 diabetes mellitus patients was substantially linked with age, insulin resistance, and hypertension. Age and the length of diabetes were associated in female patients.
Our study’s findings show no significant differences in the pooled prevalence of nephropathy between male and female diabetes mellitus patients. According to the meta-analysis, the pooled prevalence of diabetes among female patients is 35% (95% CI: 26-45, I² = 97%), whereas the pooled prevalence among male patients is 36% (95% CI: 28-46, I² = 96%).
Equally observed in this study was a differential variation in the geographical distribution of diabetes nephropathy prevalence among diabetes mellitus patients in Africa. The main observation was the highest prevalence in North Africa, followed by South Africa, while the lowest was in West Africa despite having the highest recorded sample size. The disparity in the regions can be attributed to genetic factors (64) and systemic factors like Western cultural influences, population changes, low-quality healthcare, and personal factors such as poverty, educational status, perceptions about the disease, diet, and lifestyle, such as exercise (65). The Western cultural influences on North Africa are on a high scale compared to those in West Africa because of their geographical proximity, which contrasts what is obtainable in the West African region. Studies have also reported difficulties in educating lifestyle intervention programs due to existing patients’ habits, including cultural diet and eating patterns, being more evident in West Africa than in North Africa (60). Population changes have to do with the migration of people from rural to urban cities, where they consume pre-packed foods and are more susceptible to the disease. Most West Africans are rural dwellers, where consumption of pre-packed foods is not typical and where a sedentary lifestyle is absent compared to other regions of Africa (65).
Age, gender, duration of diabetes, hypertension, and poor glycaemic control are among the various factors reported to contribute to the severity of diabetes mellitus by orchestrating the development of diabetes commodities.
In this study, we highlighted hypertension as a critical risk factor for nephropathy among diabetes patients. The meta-analysis revealed a significant association between hypertension and nephropathy among diabetes patients. This finding suggests that hypertension significantly increases the risk of developing nephropathy by more than threefold. The low heterogeneity (I² = 24%) among the 11 studies included in this analysis lends credibility to this Association. The strong link between hypertension and nephropathy underscores the importance of blood pressure management among diabetes mellitus patients. Contrary to common observation, our analysis did not show any significant association between the duration of diabetes and the risk of developing nephropathy (OR: 1.79, 95% CI: 0.48-6.62). However, substantial heterogeneity (I² = 90%) among the four studies included in this analysis might be attributed to variations in the study populations, thus suggesting that this finding should be interpreted cautiously.
4.1 Strengths
This systematic review includes an extensive search strategy covering multiple database sources, which reduces publication bias and ensures relevant studies are captured. Reproducible methodology, including predefined inclusion and exclusion criteria, enhances the reliability of the study. Also, the rigorous quality assessment using established tools like PRISMA risk analysis scoring to evaluate the quality of each included study, thereby increasing the credibility of the conclusion. Conducting a meta-analysis to provide a quantitative summary of the findings across studies. Identifying and analyzing sources of heterogeneity was also strength in this study.
4.2 Limitations
Not all countries in Africa had representative articles in the included studies. Many studies were excluded based on the exclusion criteria. Risk factors within each country responsible for their prevalence were not considered.
4.3 Conclusion and recommendation
The current study looked at the prevalence of nephropathy among diabetic mellitus (DM) patients and the risk variables in different parts of Africa. West Africa had the lowest prevalence of nephropathy among people with diabetes, whereas North Africa had the highest frequency of the condition. Consequently, investigations on nutritional determinants, patient adherence to diet adjustments, Western cultural impacts on African dietary consumption, and knowledge of nephropathy management among diabetes mellitus patients should be prioritized in Africa to lessen the burden of the disease. The possibility of West African dietary habits as a contributory factor to the lower burden of nephropathy in West Africa is worthy of investigation and will serve as a guideline for other continents with higher incidences of diabetes mellitus nephropathy.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
GA-G: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. PA: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. LA: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. AMO: Visualization, Writing – review & editing. IO: Visualization, Writing – review & editing. OO: Visualization, Writing – review & editing. AAO: Visualization, Writing – review & editing. OPO: Project administration, Resources, Writing – review & editing. OA: Data curation, Formal Analysis, Methodology, Software, Supervision, Validation, Writing – review & editing. FA: Data curation, Formal Analysis, Methodology, Software, Supervision, Validation, Writing – review & editing. OS: Project administration, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Financial funding was obtained from the Nigerian Institute of Medical Research (NIMR) Foundation with Grant ID: NF-GMTP-24-152809.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcdhc.2025.1551088/full#supplementary-material
References
1. Eizirik DL, Pasquali L, Cnop M. Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failure. Nat Rev Endocrinol. (2020) 16:349–62. doi: 10.1038/s41574-020-0355-7
2. Ogurtsova K, da Rocha Fernandes JD, Huang Y, Linnenkamp U, Guariguata L, Cho NH, et al. IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. (2017) 128:40–50. doi: 10.1016/j.diabres.2017.03.024
3. Atlas D. International diabetes federation. In: IDF Diabetes Atlas, 7th edn. International Diabetes Federation, Brussels, Belgium (2015).
4. Roglic G. WHO global report on diabetes: a summary. Int J Noncommunicable Dis. (2016) 1:3. doi: 10.4103/2468-8827.184853
5. Association, A. D. Standards of medical care in diabetes2017 Abridged for primary care providers. Clin Diabetes. (2017) 35:5–26. doi: 10.2337/cd16-0067
6. Association, A. H. Kidney Disease and Diabetes. Mount Laurel, NJ, USA (2016). Available online at: https://www.heart.org/en/health-topics/diabetes/diabetes-complications-and-risks/kidney-disease--diabetes.
7. Atkins RC, Zimmet P. Diabetic kidney disease: act now or pay later. Nephrol Dialysis Transplant. (2010) 25:331–3. doi: 10.1093/ndt/gfp757
8. Wang G, Ouyang J, Li S, Wang H, Lian B, Liu Z, et al. The analysis of risk factors for diabetic nephropathy progression and the construction of a prognostic database for chronic kidney diseases. J Trans Med. (2019) 17:264–312. doi: 10.1186/s12967-019-2016-y
10. Addo J, Smeeth L, Leon DA. Hypertensive target organ damage in Ghanaian civil servants with hypertension. PloS One. (2009) 4:e6672. doi: 10.1371/journal.pone.0006672
12. Organization W.H. Guidelines for the Prevention, Management and Care of Diabetes Mellitus. Geneva, Switzerland: Organization W.H. (2006).
13. Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys Ther. (2008) 88:1254–64. doi: 10.2522/ptj.20080020
15. Bamgboye EL. End-stage renal disease in Sub- Saharan Africa. Ethn Dis. (2006) 16 2 Suppl 2:S2–5-9.
16. Alebiosu. Clinical diabetic nephropathy in a tropical African population. WAJM. (2003) 22(2):152–5.
17. Osafo C, Mate-Kole M, Affram K, Adu D. Prevalence of chronic kidney disease in hypertensive patients in Ghana. Ren Fail. (2011) 33:388–92. doi: 10.3109/0886022X.2011.565140
18. Janmohamed MN, Kalluvya SE, Mueller A, Kabangila R, Smart LR, Downs JA, et al. Prevalence of chronic kidney disease in diabetic adult out-patients in Tanzania. BMC Nephrol. (2013) 14(183):1–5. doi: 10.1186/1471-2369-14-183
19. Sumaili EK, Cohen EP, Zinga CV, Krzesinski JM, Pakasa NM, Nseka NM. High prevalence of undiagnosed chronic kidney disease among at-risk population in Kinshasa, the Democratic Republic of Congo. BMC Nephrol. (2009) 10:18. doi: 10.1186/1471-2369-10-18
20. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan — a web and mobile app for systematic reviews. Systematic Rev. (2016) 5:210. doi: 10.1186/s13643-016-0384-4
21. Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and incidence data. Int J Evid Based Healthc. (2015) 13:147–53. doi: 10.1097/XEB.0000000000000054
22. Adeniyi OV, Owolabi EO. Cross-sectional study of diabetes kidney disease in the Eastern Cape, South Africa. Medicine. (2020) 99:e23303. doi: 10.1097/MD.0000000000023303
23. El Alami H, Haddou I, Benaadi G, Lkhider M, El Habchi D, Wakrim L, et al. Prevalence and risk factors of chronic complications among patients with type 2 diabetes mellitus in Morocco: a cross-sectional study. Pan Afr Med J. (2022) 41(1):1–18. doi: 10.11604/pamj.2022.41.182.25532
24. Ahmed MH, Elwali ES, Awadalla H, Almobarak AO. The relationship between diabetic retinopathy and nephropathy in Sudanese adult with diabetes: population-based study. Diabetes Metab Syndrome: Clin Res Rev. (2017) 11:S333–6. doi: 10.1016/j.dsx.2017.03.011
25. Ahmed H, Elshaikh T, Abdullah M. Early diabetic nephropathy and retinopathy in patients with type 1 diabetes mellitus attending Sudan childhood diabetes centre. J Diabetes Res. (2020) 2020:7181383. doi: 10.1155/2020/7181383
26. Kiconco R, Rugera SP, Kiwanuka GN. Microalbuminuria and traditional serum biomarkers of nephropathy among diabetic patients at Mbarara regional referral Hospital in south western Uganda. J Diabetes Res. (2019) 2019:3534260. doi: 10.1155/2019/3534260
27. Adem M, Mekonen W, Ausman A, Ahmed M, Yimer A. Prevalence of chronic kidney disease and its associated factors among diabetes mellitus patients in Dessie Referral Hospital, South Wollo, Ethiopia. Sci Reports. (2024) 14:9229. doi: 10.1038/s41598-024-59184-3
28. Wanjohi FW, Otieno FC, Ogola EN, Amayo EO. Nephropathy in patients with recently diagonised type 2 diabetes mellitus in black Africans. East Afr Med J. (2002) 79:399–404. doi: 10.4314/eamj.v79i8.8824
29. Muddu M, Mutebi E, Ssinabulya I, Kizito S, Mulindwa F, Kiiza CM. Utility of albumin to creatinine ratio in screening for microalbuminuria among newly diagnosed diabetic patients in Uganda: a cross sectional study. Afr Health Sci. (2019) 19:1607–16. doi: 10.4314/ahs.v19i1.36
30. Choukem SP, Dzudie A, Dehayem M, Halle MP, Doualla MS, Luma H, et al. Comparison of different blood pressure indices for the prediction of prevalent diabetic nephropathy in a sub-Saharan African population with type 2 diabetes. Pan Afr Med J. (2012) 11:1–8.
31. Bentata Y, Chemlal A, Karimi I, El Alaoui F, Haddiya I, Abouqal R. Diabetic kidney disease and vascular comorbidities in patients with type 2 diabetes mellitus in a developing country. Saudi J Kidney Dis. Transplantation. (2015) 26:1035–43. doi: 10.4103/1319-2442.164602
32. Mhundwa W, Joubert G, Mofokeng TR. The prevalence of chronic kidney disease among type 2 diabetes mellitus patients in central South Africa. South Afr Family Practice. (2023) 65:1–6. doi: 10.4102/safp.v65i1.5663
33. Damtie S, Biadgo B, Baynes HW, Ambachew S, Melak T, Asmelash D, et al. Chronic kidney disease and associated risk factors assessment among diabetes mellitus patients at a tertiary hospital, Northwest Ethiopia. Ethiopian J Health Sci. (2018) 28. doi: 10.4314/ejhs.v28i6.3
34. Aboelnasr MS, Shaltout AK, AlSheikh MR, Abdelhameed AH, Elrefaey W. Diabetic kidney disease in patients newly diagnosed with type-2 diabetes mellitus: incidence and associations. Saudi J Kidney Dis. Transplantation. (2020) 31:191–9. doi: 10.4103/1319-2442.279940
35. Otieno FC, Ogola EN, Kimando MW, Mutai K. The burden of unrecognised chronic kidney disease in patients with type 2 diabetes at a county hospital clinic in Kenya: implications to care and need for screening. BMC nephrology. (2020) 21:1–1. doi: 10.1186/s12882-020-1705-3
36. Molefe-Baikai OJ, Molefi M, Cainelli F, Rwegerera GM. The prevalence of microalbuminuria and associated factors among patients with type 2 diabetes mellitus in Botswana. Nigerian J Clin practice. (2018) 21:1430–7. doi: 10.4103/njcp.njcp_224_18
37. Ephraim RK, Arthur E, Owiredu WK, Adoba P, Agbodzakey H, Eghan BA. Chronic kidney disease stages among diabetes patients in the Cape Coast Metropolis. Saudi J Kidney Dis. Transplantation. (2016) 27:1231–8. doi: 10.4103/1319-2442.194658
38. Worku D, Hamza L, Woldemichael K. Patterns of diabetic complications at jimma university specialized hospital, southwest Ethiopia. Ethiopian J Health Sci. (2010) 20(1):33–9.
39. Abdulkadr M, Merga H, Mizana BA, Terefe G, Dube L. Chronic kidney disease and associated factors among diabetic patients at the diabetic clinic in a police hospital, Addis Ababa. Ethiopian J Health Sci. (2022) 32(2):307–12. doi: 10.4314/ejhs.v32i2.11
40. Eghan BA, Frempong MT, Adjei-Poku M. Prevalence and predictors of microalbuminuria in patients with diabetes mellitus. Ethnicity disease. (2007) 17:726–30.
41. Adebamowo SN, Adeyemo AA, Tekola-Ayele F, Doumatey AP, Bentley AR, Chen G, et al. Impact of Type 2 Diabetes on impaired Kidney Function in sub-saharan african Populations. Front endocrinology. (2016) 7:50. doi: 10.3389/fendo.2016.00050
42. Israel E, Borko UD, Mota K, Tesfaw M, Feleke T, Abraham A, et al. Out of sight: chronic kidney diseases among diabetic patients attending care and follow up. Findings from pastoralist health facilities of Southern Ethiopia. Front Public Health. (2024) 12:1326011. doi: 10.3389/fpubh.2024.1326011
43. Mariye Zemicheal T, Bahrey Tadesse D, Tasew Atalay H, Teklay Weldesamuel G, Gebremichael GB, Tesfay HN, et al. Determinants of diabetic nephropathy among diabetic patients in general public hospitals of tigray, Ethiopia, 2018/19. Int J Endocrinology. (2020) 2020:6396483. doi: 10.1155/2020/6396483
44. Tannor EK, Sarfo FS, Mobula LM, Sarfo-Kantanka O, Adu-Gyamfi R, Plange-Rhule J. Prevalence and predictors of chronic kidney disease among Ghanaian patients with hypertension and diabetes mellitus: A multicenter cross-sectional study. J Clin hypertension. (2019) 21:1542–50. doi: 10.1111/jch.13672
45. Kebede SA, Tusa BS, Weldesenbet AB, Tessema ZT, Ayele TA. Incidence of diabetic nephropathy and its predictors among type 2 diabetes mellitus patients at university of gondar comprehensive specialized hospital, Northwest Ethiopia. J Nutr Metab. (2021) 2021:6757916. doi: 10.1155/2021/6757916
46. Merid F, Getahun F, Esubalew H, Gezahegn T. Incidence and predictors of diabetic nephropathy among type 2 diabetes mellitus patients, southern Ethiopia. J Nutr Metab. (2024) 2024:6976870. doi: 10.1155/2024/6976870
47. Tesfe D, Adugna M, Nigussie ZM, Woldeyohanins AE, Kifle ZD. The proportion of chronic kidney disease and its associated factors among adult diabetic patients at Tibebe Ghion Specialized Hospital, Bahir Dar, Ethiopia. Metab Open. (2022) :15:100198. doi: 10.1016/j.metop.2022.100198
48. Sarfo FS, Mobula LM, Sarfo-Kantanka O, Adamu S, Plange-Rhule J, Ansong D, et al. Estimated glomerular filtration rate predicts incident stroke among Ghanaians with diabetes and hypertension. J Neurological Sci. (2019) 396:140–7. doi: 10.1016/j.jns.2018.11.017
49. Alemu H, Hailu W, Adane A. Prevalence of chronic kidney disease and associated factors among patients with diabetes in northwest Ethiopia: a hospital-based cross-sectional study. Curr Ther Res. (2020) 92:100578. doi: 10.1016/j.curtheres.2020.100578
50. Ahmed MA, Ferede YM, Takele WW. Incidence and predictors of chronic kidney disease in type-II diabetes mellitus patients attending at the Amhara region referral hospitals, Ethiopia: a follow-up study. PloS One. (2022) 17:e0263138. doi: 10.1371/journal.pone.0263138
51. Tamru K, Aga F, Berhanie E, Aynalem YA, Shiferaw WS. Incidence of diabetic nephropathy in patients with type 2 diabetes mellitus at a tertiary healthcare setting in Ethiopia. Diabetes Metab Syndrome: Clin Res Rev. (2020) 14:1077–83. doi: 10.1016/j.dsx.2020.06.028
52. Machingura PI, Chikwasha V, Okwanga PN, Gomo E. Prevalence of and factors associated with nephropathy in diabetic patients attending an outpatient clinic in Harare, Zimbabwe. Am J Trop Med hygiene. (2017) 96:477. doi: 10.4269/ajtmh.15-0827
53. Hamat I, Abderraman GM, Cisse MM, Youssouf M, Djafar MS, Mbainguinam D, et al. Profile of diabetic nephropathy at the National Reference General Hospital of N’Djamena (Chad). Pan Afr Med J. (2016) 24:193–. doi: 10.11604/pamj.2016.24.193.8415
54. Alebiosu CO, Odusan O, Jaiyesimi A. Morbidity in relation to stage of diabetic nephropathy in type-2 diabetic patients. J Natl Med association. (2003) 95:1042.
55. Taderegew MM. Assessment of renal impairment using estimated glomerular filtration rate among type 2 diabetes mellitus patients in North-East Ethiopia: a cross-sectional study. J Diabetes Metab Disord. (2020) 19:1473–81. doi: 10.1007/s40200-020-00680-4
56. Noubiap JJ, Naidoo J, Kengne AP. Diabetic nephropathy in Africa: A systematic review. World J Diabetes. (2015) 6:759–73. doi: 10.4239/wjd.v6.i5.759
57. Suriyong P, Ruengorn C, Shayakul C, Anantachoti P, Kanjanarat P. Prevalence of chronic kidney disease stages 3–5 in low-and middle-income countries in Asia: A systematic review and meta-analysis. PloS One. (2022) 17:e0264393. doi: 10.1371/journal.pone.0264393
58. Wu B, Bell K, Stanford A, Kern DM, Tunceli O, Vupputuri S, et al. Understanding CKD among patients with T2DM: prevalence, temporal trends, and treatment patterns—NHANES 2007–2012. BMJ Open Diabetes. (2016) 4(1):e000154. doi: 10.1136/bmjdrc-2015-000154
59. ElHafeez SA, Bolignano D, D’Arrigo G, Dounousi E, Tripepi G, Zoccali C. Prevalence and burden of chronic kidney disease among the general population and high-risk groups in Africa: a systematic review. BMJ Open. (2018) 8:e015069. doi: 10.1136/bmjopen-2016-015069
60. Chowdhury T. A, Kumar S, Barnett AH, Bain SC. Nephropathy in type 1 diabetes: the role of genetic factors. Diabet Med. (1995) 12(12):1059–67. doi: 10.1111/j.1464-5491.1995.tb00422.x
61. Al-Zahrani N, AlSwat HK, AlQarni AM, Alzahrani SS, Boubshait LA, Alassaf LA, Alsalman Z. Prevalence and risk factors of diabetic nephropathy among Saudi type-1 diabetic patients in Taif City, Saudi Arabia. Diabetes Metab Syndr Obes. (2023) 3609–16. doi: 10.2147/DMSO.S432700
62. Rizvi S, Raza ST, Mahdi F. (2014). Association of genetic variants with diabetic nephropathy. World J Diabetes 5(6):809–16. doi: 10.4239/wjd.v5.i6.809
63. Zhang F, Han Y, Zheng G, Li W. Gender differences in the incidence of nephropathy and changes in renal function in patients with type 2 diabetes mellitus: A retrospective cohort study. Diabetes Metab Syndr. Obes. (2024) 17:943–57. doi: 10.2147/DMSO.S451628
64. Bekele H, Asefa A, Getachew B, Belete AM. Barriers and strategies to lifestyle and dietary pattern interventions for prevention and management of TYPE-2 diabetes in Africa, systematic review. J Diabetes Res. (2020) 2020:7948712. doi: 10.1155/2020/7948712
Keywords: nephropathy, Africa, diabetes mellitus, hypertension, prevalence
Citation: Adebayo-Gege GI, Adegbola PI, Adedayo LD, Oyefabi AM, Oyeyemi IT, Olubukola O, Oke AA, Okeke OP, Abodunrin OR, Akinsolu FT and Sobande OO (2025) Prevalence of nephropathy among patients with diabetes mellitus in Africa: a systematic review and meta-analysis. Front. Clin. Diabetes Healthc. 6:1551088. doi: 10.3389/fcdhc.2025.1551088
Received: 10 January 2025; Accepted: 01 April 2025;
Published: 25 April 2025.
Edited by:
Taner Bayraktaroğlu, Zonguldak Bulent Ecevit University, TürkiyeReviewed by:
Lamija Ferhatbegovic (Pojskic), University of Zenica, Bosnia and HerzegovinaShivani Sharma, Mercer University, United States
Copyright © 2025 Adebayo-Gege, Adegbola, Adedayo, Oyefabi, Oyeyemi, Olubukola, Oke, Okeke, Abodunrin, Akinsolu and Sobande. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peter Ifeoluwa Adegbola, cGV0ZXIuYWRlZ2JvbGFAdGVjaC11LmVkdS5uZw==
 Grace I. Adebayo-Gege1
Grace I. Adebayo-Gege1 Peter Ifeoluwa Adegbola
Peter Ifeoluwa Adegbola Ifeoluwa Temitayo Oyeyemi
Ifeoluwa Temitayo Oyeyemi Adewale Adegboyega Oke
Adewale Adegboyega Oke Oluchukwu Perpetual Okeke
Oluchukwu Perpetual Okeke Olunike Rebecca Abodunrin
Olunike Rebecca Abodunrin Folahanmi Tomiwa Akinsolu
Folahanmi Tomiwa Akinsolu Olajide Odunayo Sobande
Olajide Odunayo Sobande