In training to become a registered psychologist in Australia, as with many other countries, there is a requirement for students to attend placements, where they work with clients in an apprenticeship model under the guidance of qualified supervisors. In the context of COVID-19, tertiary sector psychology educators responsible for facilitating these placements, which typically require face-to-face client work, have been challenged to arrange or maintain practica. During the pandemic, across Australia, most placements have been affected through cancellation, postponement, or modification (e.g., using telehealth, supported by the Australian Federal Government). In this paper we describe a collaborative initiative by members of the psychology profession across 15 providers of Australian postgraduate professional training programs. The initiative aimed to identify ways in which to develop and innovate psychological placement offerings, specifically using simulation-based learning. Although simulation-based learning in psychology training programs in Australia is a widely employed pedagogy for the scaffolding of theory into psychological practice, there is paucity of clear and comprehensive guidelines for the use of simulation to both optimize competency-based training and ensure public and student safety. The overarching aim of the group, and the focus of this paper, is to provide standardized guidelines for the inclusion of simulation-based learning in psychology training in Australia both during and post-COVID 19. Such guidelines may be equally valuable for psychology training programs globally.
Introduction
COVID-19 dramatically shifted how education and health services were delivered in Australia in 2020. While some tertiary education providers in Australia were already utilizing online delivery, not all had embraced this format. The sudden shift to online delivery caused several providers to reconsider training modalities for their professional psychology students. At present, there are no set standards or guidelines in Australia for simulated learning activities (SLA) in the context of professional psychology programs.
The Australian Postgraduate Psychology Education Simulation Working Group and the Aims and Objectives of This Paper
The following paper is a version of a document prepared by the Australian Postgraduate Psychology Education Simulation Working Group (APPESWG), consisting of representatives from 15 postgraduate psychology education providers across Australia. The paper covers the impact of the COVID-19 pandemic on higher education in Australia and specifically the implications for practical training components of postgraduate psychology training. We provide the background and context for training as a psychologist in Australia, review the literature regarding simulation-based learning and education (SBLE), and provide guidelines for the ethical SLA into postgraduate psychology training. Finally, we cover the processes of having these guidelines accepted by postgraduate psychology education providers across Australia and the relevant regulatory and accrediting bodies, alongside areas for potential research. The primary aim of this paper is to provide educators of psychology postgraduate training programs with guidance in the design and implementation of SLA.
COVID-19 and The Impact on Education in Australia
During the COVID-19 pandemic, tertiary education providers across Australia had to grapple with impact of physical distancing and health restrictions on psychology training placements. These impacts fell along a continuum from substantial delay through to being unable to progress which, in turn, has flow-on effects. The cessation of placements not only halts student progress but potentially leads to a backlog of students and a workforce shortage if training cannot continue for extended periods. Such outcomes are particularly problematic given the projected ongoing impacts of COVID-19 on psychological health and wellbeing over the coming years (Simon et al., 2020), placing increased demands on an already under-resourced psychology workforce. The integration of SLA combined with telehealth is one way that trainee psychologists can continue to gain clinical skills and accumulate required practice hours whilst adhering to the physical distancing requirements set by State and Federal governments. It is arguable that the training crisis of psychologists caused by the restrictions associated with COVID-19 has provided an opportunity to further investigate SBLE as a training tool for the psychology profession, and may also provide an avenue to remedy the contraction of postgraduate psychology training programs across the country.
A challenge of health professional training is finding the balance between providing an authentic experience so that newly qualified professionals are work ready vs. ensuring trainees learn skills in a safe way to protect the public. The use of SLA provides one medium to balance this risk, and as technology (i.e., video/graphics, artificial intelligence, and person machine integration) continues to improve, the use of these media to support this becomes a more viable option (Rudd et al., 2010; Graj et al., 2019). SLA can provide an avenue to increase capacity to train psychologists when placement availability may otherwise limit the number of graduates entering the workforce.
Postgraduate Psychology Training in Australia
Tertiary Education
Tertiary education providers in Australia are regulated and accredited by the Tertiary Education Quality and Standards Agency (TEQSA) and must adhere to the Australian Qualifications Framework (AQF; Australian Qualifications Framework Council, 2013, January). The AQF is the national policy for regulating education and training in Australia. The policy provides the standards for learning outcomes for each AQF level and qualification type in Australia. Postgraduate psychology programs are considered an AQF Level 9 qualification and are referred to as a coursework masters, as opposed to a master’s degree by research–a doctoral degree is a Level 10 qualification. All providers of postgraduate psychology training programs must be able to demonstrate that graduates of these programs have attained a level of advanced knowledge and skills in the field of psychology.
Psychology Programs
Tertiary education providers of psychology programs that lead to graduates being eligible for registration by the Australian Health Practitioner Regulation Agency (AHPRA), must be accredited by the Australian Psychology Accreditation Council (APAC). AHPRA is the national agency that implements the National Accreditation and Regulation Scheme and works with 15 different health practitioner boards, one of which is the Psychology Board of Australia (PsyBA; Australian Health Practitioner Regulation Agency, 2019). The title “psychologist” is protected under National Law in Australia with heavy penalties imposed for using the title when not qualified to do so (Health Practitioner Regulation Law (ACT), 2019). Psychologists are registered as either Provisional or [full] General and must have completed an approved sequence of training as specified by APAC (details below). Psychologists who have completed a specific sequence of postgraduate training and further professional development may be eligible for an Area of Practice Endorsement (AoPE; Psychology Board of Australia, 2019). There are currently nine different AoPEs, with the most common being Clinical Psychologist (Australian Health Practitioner Regulation Agency, 2019).
APAC accredits undergraduate and postgraduate psychology degrees (AQF Levels 7–9) and provides standards (Australian Psychology Accreditation Council, 2019a) and guidelines for evidence (Australian Psychology Accreditation Council, 2019b) that tertiary education providers must meet in order to attain or retain their accreditation status. Programs are typically accredited on a 6-year cycle and education providers must demonstrate appropriate evidence that they are meeting the APAC standards, or they may lose their accreditation status. At present this evidence consists of graduates meeting various competencies as determined by APAC at different levels.
There are currently four levels of APAC competencies that graduates are required to attain by the end of their degree. Level 1 are the Foundational Competencies, which are typically included in a 3-year undergraduate degree (AQF Level 7 Bachelor Degree). Level 2 are the Pre-Professional Competencies with programs at this level typically resulting in an Honors Degree (AQF Level 8), a fourth year, which is the minimum academic qualification to be eligible for provisional registration in Australia (Psychology Board of Australia, 2017) and entry into a postgraduate psychology training program (AQF Level 9). Level 3 are the Professional Competencies and Level 4 are the Professional Competencies for Specialized Areas of Practice. Levels 3 and 4 are typically 1 year in length each. Graduates of a Level 3 course of study can then apply to do a 1-year internship under the supervision of a PsyBA approved supervisor, alongside meeting other professional development requirements, and gain full general registration. Graduates of a Level 4 course of study can apply for a 2-year registrar program reflective of their specific degree (e.g., Clinical, Health, Neuropsychology) and under the supervision of a PsyBA approved supervisor, alongside completing numerous professional development requirements, apply for an AoPE. Colloquially in Australia a Level 3 APAC sequence is known as the 5 + 1 pathway, with degrees often having the title “Master of Professional Psychology” or similar. AoPE degrees typically have the named specialty in the title (e.g., “Master of Clinical Psychology,” “Master of Health Psychology”).
Alongside the numerous competencies that students need to meet in Level 3 and 4 programs is the requirement for a set number of hours of client-related activities and direct client contact. Students in a Level 3 course of study are expected to have accumulated at least 300 h of practicum skills and training. Graduates from a Level 4 course of study are required to accumulate at least 1,000 h of direct client and client-related activities, with a minimum of 400 h of the 1,000 coming from direct client activities.
The focus of the discussion in this paper is about the incorporation of SLA into APAC Level 3 and Level 4 degrees in a standardized empirically supported fashion. At present only Level 3 degrees have an allowance for the use of some SLA. We propose that using an evidence-based approach and the guidelines outlined in this paper, postgraduate psychology training programs can incorporate SLA into their programs in an ethical way. We suggest that the incorporation of SLA will improve trainee outcomes, ethical practice, client outcomes, and reduce the burden on training programs to find enough direct client-related hours for students, especially in the context of ongoing lockdowns and social distancing regulations.
Defining Simulated Learning
The Healthcare Simulation Dictionary (Lioce et al., 2020, p. 44) defines simulation as “a technique that creates a situation or environment to allow persons to experience a representation of a real event for the purpose of practice, learning, evaluation, testing, or to gain understanding of systems or human actions.” Gaba (2007) adds that simulation is a “technique … to replace or amplify real experiences with guided experiences that evoke or replicate substantial aspects of the real world in a fully interactive manner” (p. 126).
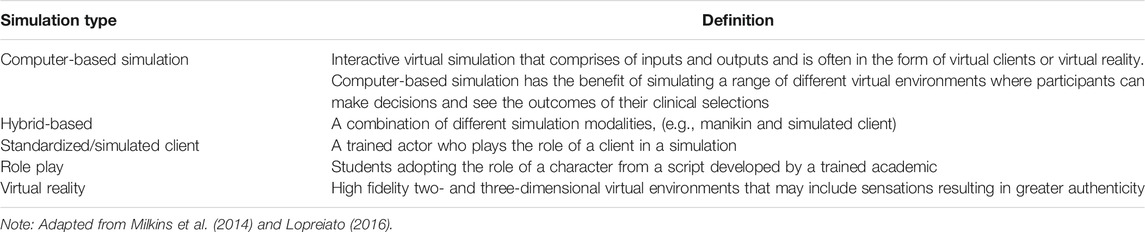
Simulation-based learning and education approaches are varied but may include computer-based simulation (e.g., use of avatars), standardized or simulated clients who are trained to act as real clients by simulating the symptoms and behaviors of an illness, manikins, virtual reality, objective structured clinical examinations (OSCEs), and role plays (Bearman et al., 2013). Table 1 contains a comprehensive outline of various simulated learning activities relevant to professional psychology training.
Benefits of Simulation-Based Learning and Education
“There is a huge disconnection between knowing something in abstract and being able to make that knowledge actionable.” (Galarneau, 2005, p. 3).
Although Australian postgraduate psychology courses have utilized SBLE for over a decade, to date there has not been a systematic uptake or benchmarking of this teaching approach at a national level. The reasons for this include financial and workload impacts associated with implementation, limited empirical evidence regarding its efficacy in the Australian context, and current APAC standards limiting this approach for accrual of placement hours in Level 3 and 4 postgraduate psychology training programs. However, given the unique and unprecedented challenges experienced due to the COVID-19 pandemic, there has been renewed interest in this pedagogical approach to ensure high quality learning experiences and outcomes that facilitate progression towards achievement of graduate competencies irrespective of access to traditional placement experiences. In the current global context, SBLE allows educators to continue the vital education and development of psychologists, addressing some of the barriers associated with placement loss. SBLE provides several additional opportunities (detailed below), both as an educational approach and a framework for competency-based assessment (McNaughton et al., 2008; Butler et al., 2009; Kameg et al., 2010; Maas and Flood, 2011; Stegmann et al., 2012; Milkins et al., 2014; Nestel et al., 2017).
Bridging the Gap. By integrating SBLE in psychology, courses trainers can address the disconnect between knowing and making knowledge actionable, as identified by Galarneau (2005). Research indicates that SBLE increases students’ confidence and competence by providing a bridge between classroom theory and workplace practice (Cybulski et al., 2010; Rudd et al., 2010).
Supporting a Safe Learning Experience. Simulation provides a structured, learner-centered environment where students can learn and practice skills without causing harm to clients (Bearman et al., 2013). Risk to students can also be mitigated by providing opportunities to practice risk management skills before placement (Graj et al., 2019), identify and discuss professional and ethical issues raised in SLA, and gain confidence with peers before the additional pressures of real-world practice are added.
Ensuring Curriculum Control. While placement provides an excellent opportunity for learning and socialization into the workplace environment, it is difficult to control the quality of a student’s experience and the breadth of client presentations they encounter. SBLE builds in a degree of curriculum control not provided within workplace contexts, supporting equality in students’ learning experience and ensuring all students can access a breadth of health disorders and symptoms including low prevalence presentations in their studies before they are fully qualified.
Supporting Sustainability. While cost has been identified as a barrier to SBLE, once developed, many SLA are sustainable. Those delivered online or using virtual methodologies are far less susceptible to the global challenges that are currently faced by services offering direct client contact (Rudd et al., 2010).
Developing Appropriate Illness Scripts. SLA may be useful in the development of appropriate or typical illness scripts. An illness script or schema is a collection of knowledge that embodies the common characteristics of a condition, providing a basis for typical to which atypical can be later quantified (Custers, 2015; Strasser and Gruber, 2015). Custers (2015) notes that illness scripts are developed by both doing and observing, making this ideal for use in SLA. Importantly, illness scripts are difficult to shift once developed so exposing students to typical cases under controlled environments helps to manage the potentially challenging influence of atypical scripts presented early in training.
Teaching High Stakes, Low Frequency Events. SLA comes into its own when teaching the skills necessary to manage high stakes (risky), low frequency (unusual) clinical events. These events, by their very nature, may not occur during placement, but ensuring that students have the skills to manage them is essential to ensure workforce ready graduates.
Student Engagement and Outcomes. Students trained with SBLE are additionally engaged, better prepared and more competent, resulting in greater ability to meet the demands of a range of placements and client presentations spanning a continuum of complexities, and thereby develop more appropriate workforce skills (Cybulski et al., 2010; Sheen et al., 2015). SBLE is also a recognized work integrated learning activity and thus has direct application to the development of employability skills (Orrell, 2011).
Current Use of Simulated Learning
The use of SBLE in training and assessment is a widely used and accepted practice in a number of health-related fields, such as nursing and medicine (Kühne et al., 2018) and there is a large volume of research on SBLE in health professional education (Cook et al., 2011). Nursing and medicine have successfully used SBLE in several ways (e.g., use of high-fidelity manikins that enable students to acquire clinical skills in respiratory assessment, heart rate, and blood pressure (Mutter et al., 2020), with some tasks implemented using integrated scenarios to foster clinical decision making and reasoning (Cantrell et al., 2017). There are also multiple forms of SLA, including simulated and standardized clients, virtual reality, manikins, role-play, computer simulation and voice simulation. Simulated clients are actors who role-play the client (Chur-Hansen and Burg, 2006); standardized clients are also trained to provide consistent responses to the students (Kühne et al., 2018).
SBLE has been utilized as a modality in other health professions for at least 2 decades with multiple systematic reviews and meta-analyses having been conducted on the effectiveness of this method of training (e.g., McGaghie et al., 2010; Cook et al., 2013; Gegenfurtner et al., 2014; Vandyk et al., 2018) with best practice training guides published for use of SBLE in healthcare training (Motola et al., 2013). SBLE has been trialed in social work (e.g., Dodds et al., 2018) and psychiatry (e.g., Ajaz et al., 2016) with promising results. SBLE has been successfully used to train front of house staff (i.e., reception and administrators) in specialty psychosis services for how to interact with effectively with clients (e.g., Baumeister et al., 2015). Physiotherapy and occupational therapy have also successfully utilized simulation in training (see for example, Bennett et al., 2017; Tuttle and Horan, 2019).
Of note, most of the learning theories and pedagogical foundations for using SBLE are couched in psychological theories (e.g., Rutherford-Hemming, 2012). The use of actors and standardized clients is common in SLA (e.g., Keltner et al., 2011; Alexandera and Dearsley, 2013; Masters et al., 2015; Edwards et al., 2016; Kühne et al., 2018; Meghani and Ferm, 2019), with best practice standards also published for the actors themselves (Lewis et al., 2017).
Simulation-Based Learning and Education in Professional Psychology Training
In Australia, SBLE for psychology has involved the use of a range of SLA, from general techniques such as role plays and the use of OSCEs through to competency training in areas such as mental state assessments and empathy skills training (Beccaria, 2013; Sheen et al., 2016). The media used in psychology SLA can include live or recorded actors, or decision-making virtual reality scenes. Alongside the benefits of SBLE, the importance of telehealth and its role in training the next generation of psychologists is recognized (Simpson et al., 2014), especially given the COVID-19 pandemic. While SBLE can be expensive, it does enhance trainee and client safety (Oberhauser and Dreyer, 2017) through increased opportunity for competency development prior to engaging with true clients.
Although SBLE is emerging in the field of postgraduate psychology training (e.g., Nel, 2010; Edwards et al., 2016), there is limited research in this area (Kühne et al., 2018). In response to this, a scoping review explored barriers and facilitators to using simulated clients in clinical psychology education. Considerations raised in the review included cost, finding people with both acting skills and psychological knowledge, authenticity of portrayal, the importance of careful planning of scenarios, and the effects on actors simulating mental health conditions (Kühne et al., 2018). Traditionally, psychology education has tended to use methods such as clinical placements and written exams rather than SBLE (Sheen et al., 2020); however, SLA are beginning to become more widely considered in postgraduate psychology education and there recent studies testing the efficacy of SLA for psychology trainees.
An interprofessional study involving medical, nursing and clinical psychology students found that knowledge, confidence and attitudes towards clients, professional roles, interprofessional working and intervention approaches improved after working through simulated scenarios and debriefs (Attoe et al., 2019). Students appreciated being able to collaborate with other professionals and reported that the experience had helped them develop better ways of communication, and that they had increased in clinical skills and confidence. Other benefits that they identified were developing empathy, self-awareness and resilience when dealing with clients (Attoe et al., 2019).
Another study assessed the efficacy of a simulation course in helping mental health professionals–including clinical psychologists–work with families and networks of clients with a mental illness (Kowalski et al., 2018). The interprofessional course involved participating in and observing several scenarios, with trained actors portraying clients and members of their network. The results indicated that confidence and attitudes towards tasks associated with the professional role improved after the simulation course. Participants commented on the safety that they felt in the SLA, the opportunity for professional development, and the importance of reflection (Kowalski et al., 2018).
A recent Australian study explored the differences between simulation-based and case-based learning for clinical psychology trainees (Sheen et al., 2020). While trainees in the simulation-based condition rated their confidence higher than those in the case-based condition, their improvements in clinical competence, as assessed in an OSCE, were not significantly different. Qualitative feedback indicated that the trainees preferred the simulation-based option to the case-based option, as they felt the case-based learning did not prepare them for the OSCE (Sheen et al., 2020). However, trainees had concerns about the realism and practical aspects (such as time needed to devote to SLA tasks) of the simulation option.
A study from the United States focused specifically on the use of virtual simulated clients (Washburn et al., 2020). Virtual simulated clients can provide practice scenarios before students begin to interact with real clients, as well as overcoming many of the time and cost concerns of using trained actors. In this study, students in masters’ psychology and social work courses were allocated to one of three conditions, with each condition having a different combination of practice opportunities with virtual clients, and assessments with virtual or actor clients. The results after the final assessment indicated that having opportunities to practice clinical assessment with virtual clients increased the students’ self-efficacy and diagnostic accuracy (Washburn et al., 2020).
A common assessment method in health professional education is the OSCE, which involves students interacting with simulated clients to demonstrate their clinical skills (Roberts et al., 2020). These have been used for many years in medical education; however, psychology has been slower to adopt OSCEs for assessment, with some recent Australian studies conducted to explore the responses of postgraduate clinical and health psychology students to the OSCE (e.g., Sheen et al., 2015; Roberts et al., 2017; Roberts et al., 2020).
One paper detailed the development of an exam to assess clinical competence, which refers to the ability of students to apply knowledge in practice (Masters et al., 2015). Clinical psychology students completed the exam, which involved observing and conducting a therapy session with a standardized client, and a discussion with the examination committee. Students responded with apprehension and anxiety, although this decreased over time. They also reported growing in confidence and self-efficacy following the exam. The researchers noted challenges in developing the exam, such as finding the right people to play the standardized clients and meeting the time and financial costs (Masters et al., 2015).
In another study, students and staff provided feedback on the OSCEs that were used in three postgraduate psychology units (Sheen et al., 2015). Most students reported feeling positively towards the OSCE, although some noted feeling insufficiently prepared. Students commented on the realism of the OSCE and the ability to put theory into practice. A main disadvantage was feeling stressed going into the OSCE. This student stress has been reported in other research (i.e., Roberts et al., 2017; Roberts et al., 2020). Staff in Sheen et al. (2015) commented that the reliability and validity of the OSCE was higher than for other assessment methods, as well as providing a safe place for students to practice their skills; however, a disadvantage was the increased time and cost required to run the OSCE (Sheen et al., 2015). In response to the limited research on student perceptions of the OSCE, these were assessed in a postgraduate psychology course taken by clinical and health psychology masters students (Roberts et al., 2020). Based on a pilot study (Roberts et al., 2017), the researchers designed a new process for students, which included written and verbal feedback from the simulated client, a mentoring session with a registered psychologist, increased preparation, and the opportunity to reflect on the experience. Overall, students found the OSCE very beneficial for several reasons, including receiving feedback from the client, developing skills and being able to observe and reflect on their own clinical practice. Some students felt that they did not have enough practice and formative feedback prior to summative OSCE assessment, and some did not like the implemented method of receiving feedback immediately after the OSCE (Roberts et al., 2020).
SLA needs to demonstrate reliability and validity to achieve the desired outcomes for students. Within a study of internet-based cognitive behavioral therapy (CBT) education, a sub-study focused on the actors recruited to be the standardized clients (Edwards et al., 2016). The results indicated that the standardized clients were successful in script adherence and character fidelity. The accurate portrayal of the correct psychological disorder was lower than other aspects, yet still acceptable. The assessment of performance drift indicated that portrayals were consistent over time. The researchers suggest that ongoing performance assessment of standardized clients is a necessary component in SBLE (Edwards et al., 2016).
In conclusion, SBLE has been widely used and researched across a range of disciplines including nursing, medicine, and allied health professions. Use of, and research on, SLA in Australia has emerged more recently in psychology, with a focus on clinical and health psychology. The limited research that has been conducted regarding SLA and professional psychology training has provided evidence that SLA has a variety of benefits to learning, including increased improvements in inter-professional learning, improved empathy, self-awareness, diagnostic accuracy, competence, and student satisfaction and confidence in the area of applied and clinical psychology. Cost and stress involved in preparing for OSCEs have been noted as barriers to carrying out OSCEs in postgraduate studies. Some factors which may mitigate against these barriers include providing written and verbal feedback from the simulated client, mentoring pre- and post-assessment with registered psychologists affiliated with the program, increased time for preparation and provision of formative feedback, and time to reflect on the SLA.
Guidelines for Incorporating Simulated Learning Activities in Professional Psychology Training Standards of Best Practice and Criteria for Simulated Learning Activities
The primary aim of this paper is to provide educators of psychology postgraduate training programs with guidance in the design and implementation of SLA. As previously detailed, SBLE has been widely and successfully utilized in training and assessment across several health-related disciplines. The International Nursing Association for Clinical Simulation and Learning (INASCL) have developed 11 standards of best practice in the design and implementation of SLA (INASCL Standards Committee, 2016). These include key processes to consider such as performing a needs assessment, designing scenarios, having appropriate pre- and de-briefing processes, and pilot testing the SLA before full implementation. These standards provide a useful step-by-step guide for educators considering the varying aspects of implementing SLA in their training programs.
The Association of Standardized Patient Educators (ASPE; Lewis et al., 2017) has also developed standards of best practice relating to the involvement of standardized patients/clients in the SBLE. The standards include a set of core values (safety, quality, professionalism, accountability, and collaboration) and provide guidance across five domains (safe work environment, case development, training of standardized clients, program management, and professional development). The ASPE standards of best practice (Lewis et al., 2017) are intended to be used alongside the standards developed by INSACL (INASCL Standards Committee, 2016). Together, the two documents provide overarching standards of best practice in the design and implementation of SLA within the SBLE. Although originating from the fields of nursing and medical training, these standards are generalizable to the context of professional psychology training.
Another focus of the current paper is to provide consistency within the discipline of psychology regarding the criteria of SLA in a training context. Although the two documents cited above provide broad guidance regarding the design and implementation of SLA, it is useful for educators to develop a specific set of principles to guide their design of specific SLA. This allows educators to determine if a particular SLA fits the commonly adopted criteria of SLA within the context of postgraduate psychology training.
Consequently, we propose criteria for SLA within psychology, based on standards from the INACSL (INASCL Standards Committee, 2016) and ASPE (Lewis et al., 2017). In developing these criteria, we were cognizant that postgraduate psychology training in Australia encompasses a wide range of programs and different applied areas of practice (refer to Australian Psychology Accreditation Council, 2019a Standards; and Kavanagh, 2015 for an indepth coverage of postgraduate psychology training in Australia). As such we developed the principles to be sufficiently flexible to be adapted to different program levels and areas of practice. We propose nine key criteria for what constitutes an SLA within postgraduate psychology training.
Criterion 1: Competency Based
All SLA should be directly linked with the development and/or assessment of specific trainee professional competencies. That is, each SLA should specifically focus on aspects of competencies within the specific psychology training program in which it is introduced.
Criterion 2: Opportunity for New Learning
SLA should be designed to scaffold learning, building on existing skills and knowledge while extending new learning with minimal risk or concern of causing harm. As such, the scope and complexity of SLA should be commensurate with the professional development stage of the trainee and needs to provide opportunity for new learning or an extension of previously acquired skillsets. As such the activity should not be overly simplistic or difficult and should provide an appropriate level of challenge for trainees to develop new learning.
Criterion 3: Parallels Real Life Psychology Practice
The SLA needs to have authenticity, and represent aspects of real professional situations, activities and/or interactions that the trainee will encounter in their psychology careers within their area of practice. These should be realistic and authentically mirror real-world situations and practice in a way that enhances relevance. In other words, the SLA should be ecologically valid in the development of skills, procedures, and knowledge, identification of learning needs, and the assessment of real competencies.
Criterion 4: Trainee Active Participation
SLA should have an emphasis on experiential and active learning principles embedded into the activity–as compared to didactic presentations, passive observation, or rote learning of material. Trainees involved in the SLA should play active and engaged roles, and not simply be observers.
Criterion 5: Structured Processes
The SLA needs to be designed and implemented in a structured and controlled manner, which allows risk to be better contained, and learning to be more targeted. This includes the use of standardized clients and provision of clear instructions to all involved, including the trainee undertaking the SLA, supervisors overseeing the activity and any simulated/standardized clients. The scope, complexity and areas of targeted learning should be clearly presented, ethical considerations of confidentiality, safety, and mechanisms to opt out for the person in the simulated client role. Procedures should be appropriately documented to provide clear instructions in the entire SBLE process.
Criterion 6: Supervised
The implementation of the SLA needs to be supervised by suitably qualified staff able to monitor trainee learning, oversee the appropriate implementation of simulated learning, ensure sufficient safeguards are in place and review the outcome of the activity.
Criterion 7: Reviews and Feedback on Trainee Performance
SLA needs to have inbuilt processes whereby the work of the trainee can be reviewed, even if the SLA does not constitute a formal assessment component of their training. As such, the activity may require the use of audio-visual recording and/or suitably qualified reviewers to be present during SLA. Training protocols and assessment guidelines should also be available for reviewers to provide a standardized assessment process. Trainees should be provided with feedback regarding their performance, which can be either summative or formative in nature. Within a structured SLA, feedback should also be structured, allowing clear linkage to the development of competencies.
Criterion 8: Opportunity for Trainee Reflection
The SLA should cause trainees to explicitly reflect on their experience and learning within the SLA, including the extent to which this material relates to the development of their professional competencies. Trainees should also be encouraged to provide balanced reflection that includes both areas of strength and areas of improvement, and how their learning can inform their future practice.
Criterion 9: Opportunity for Stakeholder Feedback
The SLA should also have feedback mechanisms for all stakeholders, including program authority, supervisors, assessors, simulated/standardized clients, and trainees. The feedback process allows for ongoing adjustments and improvements to be made so that the SLA remains fit for purpose.
Ethical Considerations
SLA are designed to replicate psychological practice; however, the use of SLA in professional psychology training raises some unique ethical issues relative to other learning activities. A key difference between a simulated and real psychological practice experience is that, for the most part, in professional psychological practice ethical considerations prioritize public safety and the client. In contrast, while the goal may be to ensure students are competent to work safely and ethically in the real practice setting, in SLA academics have an ethical responsibility to both consider and protect the psychological safety of students participating in the SLA and the integrity of the learning activity. This is especially the case where SLA involve student dyad role-plays of therapist and client.
Ethical psychological practice principles must guide all stages of an SLA, including at the design, implementation, and review phases, and consider all parties involved. Considering the needs of students who may be personally activated (i.e., distressed) by the SLA themes is integral to safe and ethical simulation design, and provides for proactive support and management of such situations prior to engaging in client work where such activation may also occur. All those involved in an SLA have both separate and overlapping responsibilities (detailed below) and these should be understood by all parties.
Academic Staff Responsibilities
The responsibility of academic staff is in developing and setting up the guidelines and parameters for the SLA (including guidelines designed to prioritize student safety first and student competency-based learning second), develop comprehensive scenarios plays for suitable SLA, including role-plays, and to ensure a framework for student safety is in place. These frameworks and guidelines should span issues including the nature and expectations of the various roles in SLA (e.g., what is the role of the therapist, the client, and the supervisor in a simulation?), as well as ensuring there are clear protocols on ensuring confidentiality and safety, especially if the person in the client role shares lived experiences. Protocols for responding to both “clients” and “therapists” who struggle or become distressed during the SLA should include an opt-out process. Note that the academic may also be the clinical supervisor.
Clinical Supervisor
The responsibility of the clinical supervisor is to support the learning experience of the student-peers and apply the principles of ethical psychological practice during the SLA, including boundary setting clear and transparent processes for the roles of all parties should be established prior to the commencement of the simulation. Supervisors are also responsible for the safe practice of student SLA, to intervene (if the therapist has not already) during the SLA to ensure safety of the client, to debrief with the client and therapist before feedback/reflective practice. Supervisors need to model ethical conduct in the design and delivery of SLA.
Simulated Client’s Responsibilities
The role and responsibility of the simulated client is to support the learning experience of their student-peers and apply the principles of ethical psychological practice principles during the SLA, including boundary setting. Specifically, simulated clients need to be aware of personal boundaries, refrain from choosing client issues that may represent their own personal issues and conflicts, and to choose the issues that will also support the student-therapist’s learning experience.
Simulated Therapist’s Responsibilities
The simulated therapist is responsible for engaging in the SLA in a professional manner consistent with that employed when working with “true clients,” including application of ethical psychological practice principles. They are also responsible for responding appropriately if the client is struggling with the simulation, which may involve terminating the simulation and providing access to supports. The simulated therapist is also responsible for prioritizing the simulated client’s safety through the SLA.
Ethical SLA design serves as a powerful teaching tool for ethical psychological practice. Table 2 highlights key ethical considerations relevant to the design, implementation, and review phases of the SLA. Note that the table provides a non-exhaustive list of considerations and recommendations, and references to sections of the Australian Psychological Society (APS) Code of Ethics [the Code] (Australian Psychological Society, 2007) are in parentheses. The table focuses on the Code to provide examples, but there are many Ethical Guidelines which would also be of relevance.
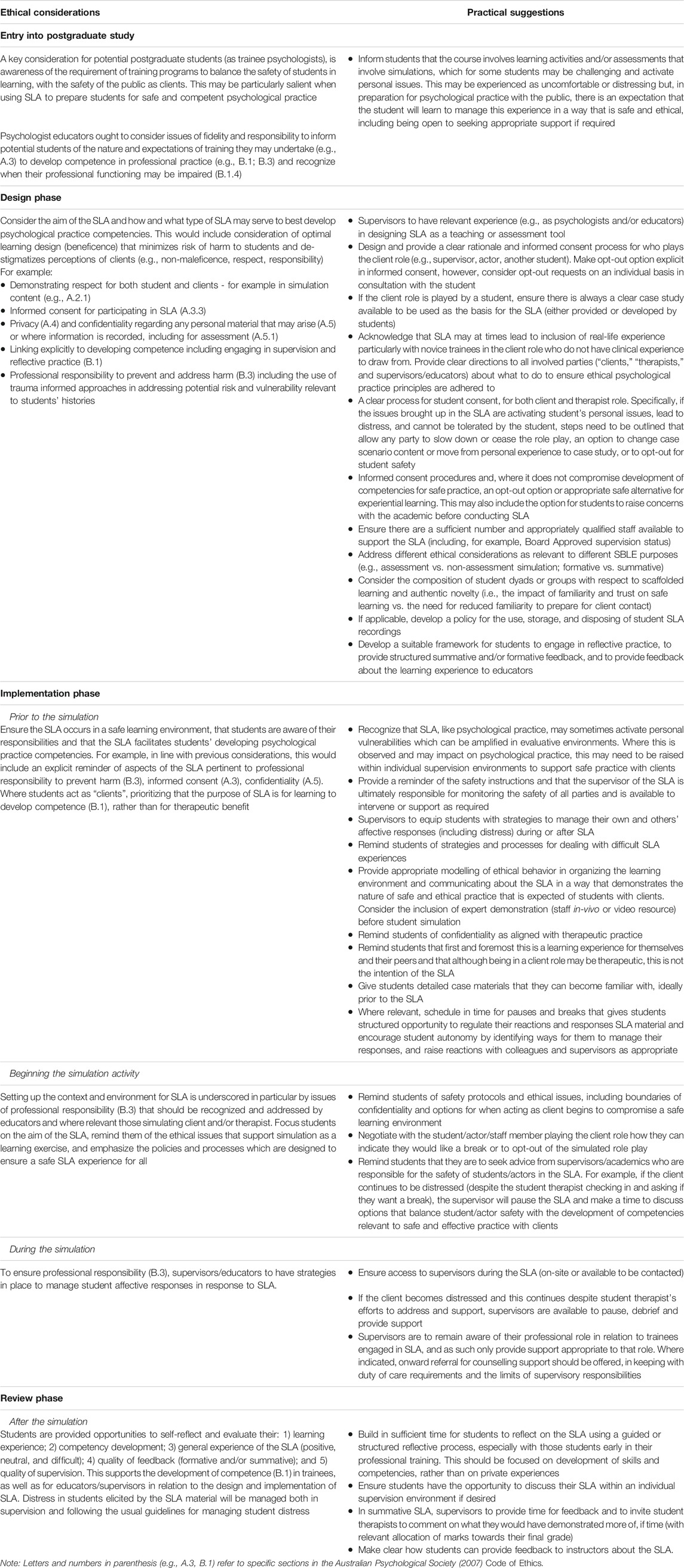
TABLE 2. Ethical considerations and practical suggestions for employing ethical psychological practice principles at each phase of the SLA.
Examples of Implementation of SBLE
Throughout the course of 2020, tertiary education providers of postgraduate psychology training courses were invited to take part in regular national meetings to discuss and address common issues resulting from the impact of COVID-19 on student training. As part of the discussions about the use of SLA in this context, teaching staff involved in postgraduate psychology training were invited to provide information about the SLA they already use as well as their experiences on the use of SLA. Examples of simulations were offered from 17 providers of postgraduate psychology training courses. All contributors were asked if they would like to be acknowledged in any materials developed from their contributions; the names of the contributors outside of APPESWG are listed in the acknowledgements section.
Based on the examples provided, we propose that SLA may be particularly beneficial in the early phases of postgraduate psychology training, commonly in role-play with other students, with an emphasis on preparatory skills development and competency demonstration in advance of service delivery to members of the public. These examples (below) describe a range of activities relevant to SLA which may have different purposes, although may occur within the same SLA.
Simulation Observation
Trainees observe simulations of psychological practice, which can be live (e.g., lecturer demonstrations or role plays) or virtual. To encourage active learning, students may be encouraged to incorporate the observed material into skill relevant practice such as case formulation and treatment planning and write a reflection or engage in peer supervision to discuss the observations made.
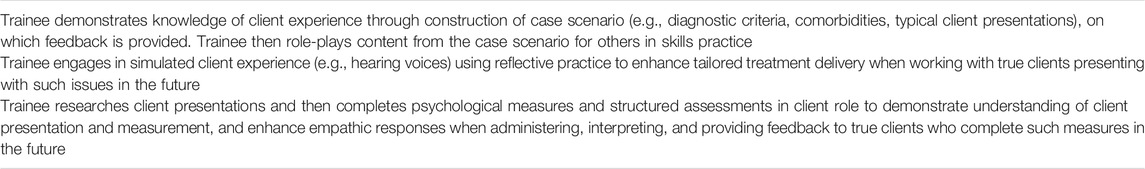
Experiential Client Perspective
Trainees engage in a simulated client experience. This may include learning a client role based on details from a case study (typically for a role-play), or it may be an immersive experience intended to build empathy and perspective taking. While there is less emphasis on the client role in simulations, SLA can also be structured to enhance competency development when adopting the client perspective. See Table 3 for examples of experiential client perspectives embedded within postgraduate psychology training in Australia.
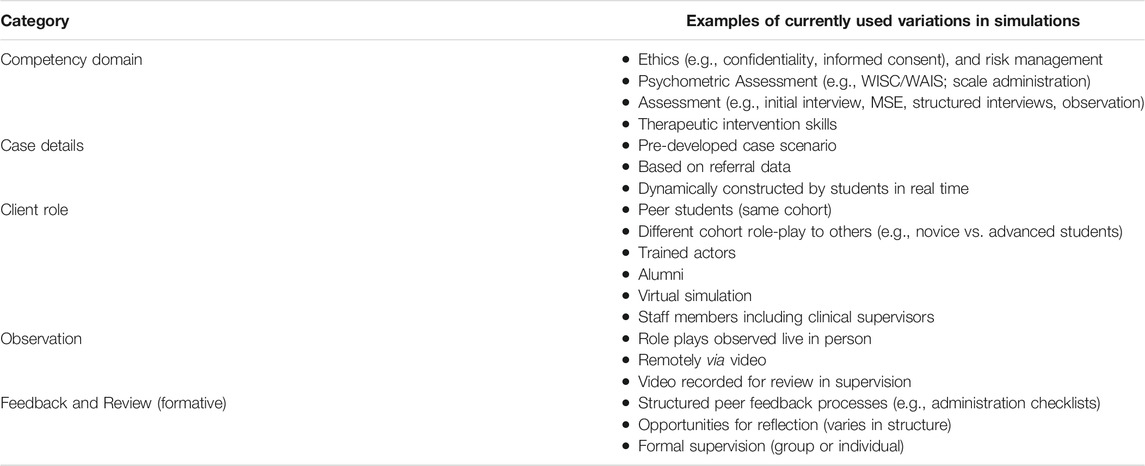
Structured Skills Practice
These SLA provide an opportunity for training and skills rehearsal, typically in the format of role plays with student peers. Structured case-based learning is still used, with the client role informed by material from existing clients, ensuring case materials are deidentified to ensure confidentiality, or with constructed case details that are provided to students. Where appropriate, variability and flexibility allow students to learn and experiment safely in the therapist role. Feedback is formative, reflective practice often embedded, and may include structured review within formal supervision sessions. It may also build towards a competency based summative assessment. See Table 4 for examples of structured skills practice currently employed across postgraduate psychology programs in Australia.
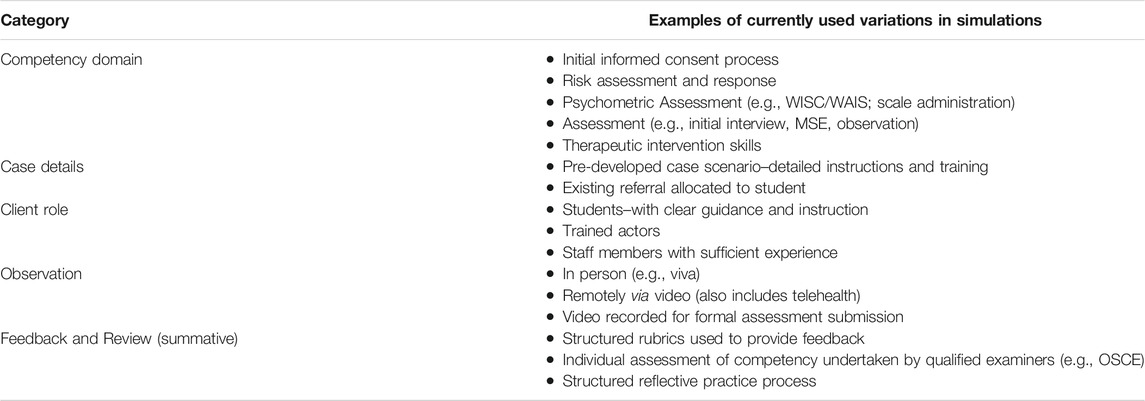
Competency Demonstrations
These SLA are summative assessments of competency, including across the domains of ethical practice, psychological assessment, and therapy identified above, and often designed to replicate the practitioner experience as authentically as possible. They tend to be more structured and standardized to ensure fairness of assessment across trainees and commonly used as gatekeeper tasks to ensure safe and competent practice before service delivery to the public, with student resubmissions if competency is not met. Formal feedback is embedded and may also include reflective practice components. See Table 5 for examples of competency demonstrations currently used in Australian postgraduate psychology training programs.
SLA currently in use differ according to the intended learning outcomes, resources, and purpose of courses and programs of study; however, the key methods currently in use are summarized below (Table 4) in relation to the most common purposes of skill development and competency demonstration (Table 5) and may provide ideas for future SLA design.
Potential Issues in Implementation of SLA
While there are clear benefits of SLA, the proposed increased integration of SLA as defined by these guidelines in postgraduate psychology training is not without controversy, with some understandable reservations held by trainers and trainees alike. The subsequent section attempts to directly respond to the key issues typically expressed about the use of formalized SLA in postgraduate psychology training programs. Discussion is based on evidence and best practice outlined in these guidelines, the views of Australian professional psychology trainers consulted regarding their experience of simulations as part of the national initiative, and a survey of students participating in postgraduate psychology training programs, conducted by members of APPESWG. This student survey sought to understand students’ attitudes towards the use of SBL in postgraduate psychology training programs. It comprised responses from 84 students (71 female, 13 male) enrolled in Master of Psychology programs with most in their fifth year of training (APAC Level 3) from across all Australian states and territories. Students were undertaking training in five different areas of psychology with most participants completing a Master of Professional Psychology (APAC Level 3) or a Master of Clinical Psychology (APAC Level 4 AoPE) (Oxlad et al., 2020).
The Worth of SLA
Effective SLA require a lot of work and educators and students are often already overloaded, so the question arises “Are SLA activities really worth it?.” Using best practice guidelines in the design, implementation, and assessment of SLA does require additional work by educators–as does any new assessment process. It was an objective of APPESWG to improve the training of postgraduate psychology students and reduce the burden on individual educators when devising innovative training and assessment processes. To do so, this paper provides benchmarked guidelines for best practice in SLA.
There is empirical evidence to suggest that SLA can increase student competency and confidence, resulting in better performance on placement and better breadth of experience particularly with low frequency high risk situations (Roberts et al., 2017). This accords with the views offered by educators from Australian postgraduate psychology training programs to the national initiative, highlighting that positive feedback is often received from both the student performing the role of client and the student performing the role of the therapist in the context of SLA activities. This feedback is especially likely if SLA are well designed and implemented, consistent with the principles outlined above, as opposed to adoption on a more an ad-hoc basis.
Students surveyed about their experiences of SBLE reported that they felt SLA to be valid way to develop assessment and intervention skills, to “ease into” client work and to enhance competency. Both empirical and anecdotal evidence therefore suggests that simulation-based client work not only instils confidence in trainee psychologists but that this can translate into competency attainment, safely and effectively, before trainees enter placements, which is a universal goal of early professional psychology training. From this perspective SLA are likely to be “worth it” in supporting students to develop required competencies for client work and ensuring protection of the public.
A final issue for consideration highlighted through our consultation of postgraduate psychology educators was whether institutions would commit to adequate resourcing of SLA, especially when used in the context of formative assessment for the development of specific professional competencies (i.e., separate from trainee placements). Example concerns included costs associated with the use of actors and examiners in the context of OSCEs. These issues relating to individual institutional support for SLA activities, while recognized as important potential barriers to more widespread use of SLA, are beyond the scope of this document and thus included as a topic for future inquiry and consideration.
How to Fit SLA into Already Full Curricula
Professional psychology training program curricula are already full, which leads to the concern and question of “how can we fit it in?” Integrating SLA into pre-existing postgraduate psychology training program curricula can be challenging and ideally will occur as part of a broader curriculum review. The best way to achieve SLA integration within postgraduate training programs will depend on the structure and resourcing at different institutions. Some helpful considerations in this paper include the overview of different modes of SLA (e.g., virtual, trained actors, role plays) and examples of different SLA. These modes and examples will aid in selecting the best fit between SLA and institutional needs when considering how to add the benefits of SLA to existing course loads.
Managing Student Apprehension Toward Training and Assessment Approaches
The increasing focus on the students’ experiences in postgraduate psychology training programs leads to the question of “how can we manage student apprehension towards training and assessment approaches?” Students commonly respond with apprehension to changes to their training programs where they perceive they must undertake something new or additional; however, in a recent survey of student perceptions of SLA, students responded favorably when asked whether increased use of SLA would be beneficial. Students perceived the benefits of SLA to include providing an opportunity to learn and apply skills in a safe environment and receive feedback where they were not placing the public at risk. SLA also provided them with a means with which to enhance their confidence in such skills. While some students indicated no drawbacks to the increased use of SLA, others raised concerns such as SLA being stressful, increased workload, and whether it would take away time from actual client work. Despite such concerns, most students reported many potential benefits. Indeed, students noted that when it comes to additional SLA, they would value the opportunity to further apply their skills and integrate their learning into practice, to be exposed to diverse client presentations, and to receive feedback about their performance from multiple sources, which is consistent with our proposal of best practice guidelines for SLA. Postgraduate programs educators noted that in their experience, while students may initially perceive SLA as not as beneficial as real-life client work, this attitude changes very quickly when they experience the value and benefits, and enjoy the freedom to learn the paradigms afforded them. Emphasizing these aspects of SLA when presenting these activities to students (i.e., scaffolding learning activities) is recommended, as well as explicitly and pre-emptively addressing the concerns students may typically hold about SLA.
Providing Realistic Learning Experiences and Ethical and Safe SBLE/SLA
There are several approaches to SLA, utilizing different models for the identity of the client (e.g., known peer from same institution, unknown peer from same institution, cross institution collaborations, virtual client, actor as client, etc.), as well as the nature of case characterization (e.g., embellished vs. real life), with a view to promoting a safe but realistic opportunity for SBLE.
Supporting Effective Client Portrayals to Maximize Student Learning Experiences
Important considerations when setting up SLA include ensuring that the person acting as the client can sustain a realistic and logically consistent characterization for the duration of the SLA, while also balancing this with understandable concerns for student/actor safety. To achieve the best results, it is essential that SLA are structured processes that employ the use of standardized clients, that clear instructions and training have been provided, and that supervisors oversee the standardized clients and the activity. Both educator feedback and the trainee survey also highlight the importance of SLA being planned and structured to maximize learning potential so that trainees can mentally prepare in advance. This is as true for the client as it is for the therapist. In fact, feedback received by educators from trainees indicates that trainees acting in the role of client are often surprised at how much they learn by researching their own case with a view to presenting as authentically as possible in their role of the client. By increasing focus on this aspect of SLA activities, it is possible that not only is therapist skill development supported, but also students’ understanding of psychopathology and different client presentations.
Some interesting insights, specific to the use of known peers as clients in SLA, from the trainee survey (Oxlad et al., 2020) are worth noting. For example, some trainees may find it difficult to approach a peer to work with for the purposes of engaging in SLA, where pairs are not assigned a priori by educators. Others may struggle to demonstrate the same degree of motivation and commitment to engage in SLA, placing their paired peer in a difficult situation that may ultimately inhibit their capacity to derive full benefit from these activities. Trainees also expressed concerns that when portraying the client their peer may inadvertently make the cases easier or more difficult than necessary, for example, by divulging too much or too little information. As such, SLA may achieve better outcomes when, consistent with the principles outlined in the guidelines for best-practice SLA, educators provide adequate training and instructions for those acting as client and embed monitoring mechanisms and supervisory oversight into SLA. Similarly, it may be important to assign client/therapist pairs. Another perspective is that such challenges may also present an opportunity to practice assertiveness skills and ethical practice such as discussing concerns regarding practice/behavior with and about a peer.
Variation in Efficacy of SLA Across Competency Domains
One of the benefits of SLA is that they can be tailored to address areas of underdeveloped competencies in postgraduate psychology trainees. Whether or not these activities convey differential advantages for specific competency domains is yet to be explored and thus discussed in areas for future consideration in research.
Standardizing SLA
Some educators might ask “is SLA really that different from what we already do?.” While the concept of SBLE is not new, what this paper sets out to establish are a number of features and guidelines for best-practice SLA, with benchmarking across postgraduate psychology programs and institutions. To our knowledge, this has not yet been attempted in the field of postgraduate psychology training programs, either in Australia, or internationally.
Competency Development
In the context of developing competencies, the question could be posed that if trainees are struggling to develop their competence in a specific area, are they not better having more actual client work experience than simulated client experience? Underscoring the rationale and evidence for the integration of SLA in postgraduate psychology training, as outlined earlier in this paper is the notion that such paradigms afford trainees the opportunity to cultivate competencies in a safe and scaffolded manner before transferring these skills to real-life client work. Consistent with the concerns raised by both educators and trainees through our work, we agree that SLA should not take away from a trainee’s opportunity for real-life client work. However, we would argue where a trainee has been identified as lagging in specific competency development, these remedial needs are best nurtured and assessed in the context of SLA, with criteria for satisfactory performance able to be standardized across trainees. In this way, simulated client experience is a more appropriate safe first step in a trainee developing the minimal requisite skills to work with real-life clients, as opposed to a substitute for actual client work. This affords not only protections to the trainee and supervisor, but also upholds the interests of public safety.
Guidelines for the Assessment of SLA
We understand that educators and trainees alike share reservations about the way in which SLA are best assessed, and how this feedback might be used to inform trainee competency development, including implications for evaluations in which trainee performance is deemed to not meet competency based on SLA. These concerns are addressed in these guidelines.
Contribution of SLA to Direct Client Hours Accrual
The issue of whether SLA should contribute to and how many hours can be counted as direct client hours as defined by the Australian Psychology Accreditation Council (APAC; Australian Psychology Accreditation Council, 2019a) is an important consideration. Currently SLA is allowed for Level 3 APAC accredited masters programs and we recommend this to also be considered for Level 4 APAC accredited courses as well.
Future Directions
Recognition of Simulation-Based Learning and Education by Accrediting Bodies
As already articulated throughout this paper, SBLE research demonstrates that well designed SLA are not an inferior substitute to placements. SBLE presents numerous benefits including enhanced training in typical and atypical client presentations, improvements in trainee engagement and confidence, and more authentic formative and summative assessments of competencies. We expect that greater use of SLA that comply with our guidelines will lead to improvements in public safety, the trainee experience, and attainment of competencies. These guidelines can also serve as a standardized protocol for future SBLE research. We therefore recommend greater recognition of SLA as an integral part of postgraduate psychology training by relevant accrediting bodies (i.e., APAC).
At this point in time, the guidelines have been endorsed by the Heads of Departments and Schools of Psychology Association (HODSPA) in Australia, to be circulated to postgraduate psychology training program staff. Representatives of APPESWG are also preparing to make a submission to APAC for their consideration of the guidelines. The typical process by APAC for making changes to standards and guidelines is engaging in stakeholder consultation (e.g., education providers, professional associations) on their proposed modifications–a top-down approach. Given that over one third of the postgraduate psychology training providers of APAC Level 3 and 4 qualifications contributed to the guidelines, APPESWG is hoping that a ground up approach of stakeholders presenting recommendations, may facilitate the incorporation of the SLA and SBLE guidelines and recommendation in to APAC’s standards and guidelines in a timelier fashion (i.e., months not years).
Future pandemics and other crises are possible, if not likely, as in between inception of this process and final publication, parts of Australia have experienced some of the harshest lockdowns in the world, with currently 18 million people (72% of the population) in another snap lockdown as of June 2021. Therefore, SBLE approaches are necessary to avoid deficits in trainee client contact hours, development of competencies, and in the mental health workforce that would otherwise occur due to inaccessibility or limited availability of external placement opportunities.
Collaboration Across Universities
The benefits of SBLE are contingent on the quality, reliability, and validity of simulations. Thus, the primary purpose of this document is to present guidelines for best practice in SBLE, which we hope will provide consistency in SBLE standards in postgraduate psychology training. We acknowledge that these standards will require a degree of institutional support from tertiary education providers; likely be contingent on the development and implementation of standardized evaluation frameworks showing that SLA are not only highly effective for learning but can be conducted in a safe and ethical way. Consistency in SBLE standards across universities will therefore require greater collaboration across providers. Cross-institutional collaboration will mean better benchmarking, more SBLE research, and the sharing of SLA resources and costs (e.g., training of simulated clients and educators, and the development of simulation material). Cross-institutional collaboration will also see SBLE becoming a standardized approach with graduates across different programs having similar knowledge and skills.
Research
Although the evidence base for the use of SBLE is strong in other disciplines, such as medicine, there is much less research into SBLE in psychology training. To date, most SBLE studies in psychology have been qualitative and as such, more research, including quantitative and mixed methods, is needed to support our assertion that SLA are important additions and preparatory adjuncts to traditional training methods such as placements. We therefore recommend a program of research beginning with pilot studies that compare programs with and without SBLE to examine whether SLA led to improvements in the trainee experience and learning outcomes. This can then be followed by cross-institutional trials that examine the efficacy of SLA that comply with our guidelines. Longitudinal studies to examine the predictive validity of simulations and research examining the reliability and validity of SLA when used in summative assessments are also required. Whether or not SLA convey differential advantages for the development of certain competency domains over others may also be of interest to trainers with a view to better targeting the investment of institutional resources. Finally, as new technologies such as virtual reality and augmented reality become more affordable and accessible, further research into their use in SLA might lead to improvements in standardization and authenticity of simulations.
Conclusion
SLBE is an essential training method that has been demonstrated to scaffold clinical competency whilst ensuring public safety. It also provides an additional training option in the response to various challenges in the placement context including but not limited to, restrictions in the context of a global pandemic such as COVID-19, as well as low prevalence presentations that trainees may not come across in their placement settings. SLBE provides an authentic and controlled learning environment and this paper provides clear evidence as well as guidelines for its inclusion in postgraduate psychology training programs.
Australian Postgraduate Psychology Simulation Education Working Group (APPESWG)
Members of APPESWG are Josephine Paparo (*Chair, Australian College of Applied Psychology and Macquarie University), Gavin Beccaria (University of Southern Queensland), Doreen Canoy (Central Queensland University), Anna Chur-Hansen (University of Adelaide), Janet Conti (Western Sydney University), Helen Correia (Murdoch University), Amanda Dudley (Deakin University), Chien Hoong Gooi (University of New South Wales), Sabine Hammond (ISN Psychology and Australian Catholic University), Phil Kavanagh (University of Canberra), Melissa Monfries (RMIT University), Kimberley Norris (University of Tasmania), Melissa Oxlad (University of Adelaide), Rosanna Rooney (Curtin University), Alyssa Sawyer (University of Adelaide), Jade Sheen (Deakin University), Monica Thielking (Swinburne University), Sophia Xenos (RMIT University), Keong Yap (Australian Catholic University).
Author Contributions
All members of APPESWG have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
APPESWG would like to thank the educators who, in addition to those on the Working Group, provided examples of simulated learning activities currently used in postgraduate psychology training in Australia. The contributions of Maryanne Cheng (Curtin University) are also acknowledged.
References
Ajaz, A., David, R., and Bhat, M. (2016). The PsychSimCentre: Teaching Out-Of-Hours Psychiatry to Non-psychiatrists. Clin. Teach. 13 (1), 13–17. doi:10.1111/tct.12382
Alexander, L., and Dearsley, A. (2013). Using Standardized Patients in an Undergraduate Mental Health Simulation. Int. J. Ment. Health 42 (2-3), 149–164. doi:10.2753/IMH0020-7411420209
Attoe, C., Lavelle, M., Sherwali, S., Rimes, K., and Jabur, Z. (2019). Student Interprofessional Mental Health Simulation (SIMHS): Evaluating the Impact on Medical and Nursing Students, and Clinical Psychology Trainees. J. Ment. Health Train. 14 (1), 46–58. doi:10.1108/JMHTEP-06-2018-0037
Australian Health Practitioner Regulation Agency (2019). Australian Health Practitioner Regulation Agency. 2018/2019 Annual Report. Available at: www.ahpra.gov.au/annualreport (Accessed January 12, 2021).
Australian Psychology Accreditation Council (2019a). Accreditation Standards for Psychology Programs. Version 1.2. Melbourne, Australia: Author.
Australian Psychology Accreditation Council (2019b). Accreditation Standards for Psychology Programs: Evidence Guide. Version 1.1. Author.
Australian Qualifications Framework Council (2013). Australian Qualfications Framework South Australia: Australian Qualifications Framework Council (a council of the Ministers responsible for tertiary education, skills and employment). 2nd ed.
Baumeister, D., Gill, E., O’Neill, B., Perera, R., and Jolley, S. (2015). Simulation-based Training for "Front-Of-House" Staff in Psychosis Services. Psychosis 7 (4), 302–311. doi:10.1080/17522439.2015.1020334
Bearman, M., Nestel, D., and Andreatta, P. (2013). “Simulation-based Medical Education,” in Oxford Textbook of Medical Education. Editor K. Walsh (Oxford, England: Oxford University Press), 186–197. doi:10.1093/med/9780199652679.003.0016
Beccaria, G. (2013). The Viva Voce as an Authentic Assessment for Clinical Psychology Students. Aust. J. Career Develop. 22 (3), 139–142. doi:10.1177/1038416213498713
Bennett, S., Rodger, S., Fitzgerald, C., and Gibson, L. (2017). Simulation in Occupational Therapy Curricula: A Literature Review. Aust. Occup. Ther. J. 64 (4), 314–327. doi:10.1111/1440-1630.12372
Butler, K. W., Veltre, D. E., and Brady, D. (2009). Implementation of Active Learning Pedagogy Comparing Low-Fidelity Simulation versus High-Fidelity Simulation in Pediatric Nursing Education. Clin. Simulation Nurs. 5 (4), e129–e136. doi:10.1016/j.ecns.2009.03.118
Cantrell, M. A., Franklin, A., Leighton, K., and Carlson, A. (2017). The Evidence in Simulation-Based Learning Experiences in Nursing Education and Practice: An Umbrella Review. Clin. Simulation Nurs. 13 (12), 634–667. doi:10.1016/j.ecns.2017.08.004
Chur-Hansen, A., and Burg, F. (2006). Working with Standardised Patients for Teaching and Learning. Clin. Teach. 3 (4), 220–224. doi:10.1111/j.1743-498X.2006.00128.x
Cook, D. A., Hamstra, S. J., Brydges, R., Zendejas, B., Szostek, J. H., Wang, A. T., et al. (2013). Comparative Effectiveness of Instructional Design Features in Simulation-Based Education: Systematic Review and Meta-Analysis. Med. Teach. 35 (1), e867–e898. doi:10.3109/0142159X.2012.714886
Cook, D. A., Hatala, R., Brydges, R., Zendejas, B., Szostek, J. H., Wang, A. T., et al. (2011). Technology-Enhanced Simulation for Health Professions Education. JAMA 306 (9), 978–988. doi:10.1001/jama.2011.1234
Custers, E. J. F. M. (2015). Thirty Years of Illness Scripts: Theoretical Origins and Practical Applications. Med. Teach. 37 (5), 457–462. doi:10.3109/0142159X.2014.956052
Cybulski, J., Holt, D., Segrave, S., O’Brien, D., Munro, J., Corbitt, B., et al. (2010). Building Academic Staff Capacity for Using eSimulations in Professional Education for Experience Transfer. Sydney, Australia: Australian Learning and Teaching Council.
Dodds, C., Heslop, P., and Meredith, C. (2018). Using Simulation-Based Education to Help Social Work Students Prepare for Practice. Soc. Work Educ. 37 (5), 597–602. doi:10.1080/02615479.2018.1433158
Edwards, K. S., Parish, S. J., Rosen, R. C., Garvert, D. W., Spangler, S. L., and Ruzek, J. I. (2016). A Standardized Patient Methodology to Assess Cognitive-Behavioral Therapy (CBT) Skills Performance: Development and Testing in a Randomized Controlled Trial of Web-Based Training. Train. Educ. Prof. Psychol. 10 (3), 149–156. doi:10.1037/tep0000119
Gaba, D. M. (2007). The Future Vision of Simulation in Healthcare. Simulation Healthc. 2 (2), 126–135. doi:10.1097/01.SIH.0000258411.38212.32
Galarneau, L. L. (2005). Authentic Learning Experiences through Play: Games, Simulations and the Construction of Knowledge. doi:10.2139/ssrn.810065
Gegenfurtner, A., Quesada-Pallarès, C., and Knogler, M. (2014). Digital Simulation-Based Training: A Meta-Analysis. Br. J. Educ. Technol. 45 (6), 1097–1114. doi:10.1111/bjet.12188
Graj, E., Sheen, J., Dudley, A., Sutherland‐smith, W., and McGillivray, J. (2019). Enhancing Student Competency in Risky Clinical Environments: Evaluating an Online Education Program. Aust. Psychol. 54 (1), 68–79. doi:10.1111/ap.12364
Health Practitioner Regulation Law (ACT), (2019). Available at: https://www.legislation.act.gov.au/a/db_39269/. (Accessed January 12, 2021).
INASCL Standards Committee (2016). INACSL Standards of Best Practice: SimulationSM Simulation Design. Clin. Simulation Nurs. 12, S5–S12. doi:10.1016/j.ecns.2016.09.005
Kameg, K., Howard, V. M., Clochesy, J., Mitchell, A. M., and Suresky, J. M. (2010). The Impact of High Fidelity Human Simulation on Self-Efficacy of Communication Skills. Issues Ment. Health Nurs. 31 (5), 315–323. doi:10.3109/01612840903420331
Kavanagh, P. S. (2015). Psychology Regulation, Education, and Representation in Australia. Int. J. Ment. Health 44 (1-2), 4–10. doi:10.1080/00207411.2015.1009742
Keltner, N. L., Grant, J. S., and McLernon, D. (2011). Use of Actors as Standardized Psychiatric Patients. J. Psychosoc Nurs. Ment. Health Serv. 49 (5), 34–40. doi:10.3928/02793695-20110329-02
Kowalski, C., Attoe, C., Ekdawi, I., Parry, C., Phillips, S., and Cross, S. (2018). Interprofessional Simulation Training to Promote Working with Families and Networks in Mental Health Services. Acad. Psychiatry 42 (5), 605–612. doi:10.1007/s40596-017-0840-z
Kühne, F., Ay, D. S., Otterbeck, M. J., and Weck, F. (2018). Standardized Patients in Clinical Psychology and Psychotherapy: A Scoping Review of Barriers and Facilitators for Implementation. Acad. Psychiatry 42 (6), 773–781. doi:10.1007/s40596-018-0886-6
Lewis, K. L., Bohnert, C. A., Gammon, W. L., Hölzer, H., Lyman, L., Smith, C., et al. (2017). The Association of Standardized Patient Educators (ASPE) Standards of Best Practice (SOBP). Adv. Simul 2 (1), 10. doi:10.1186/s41077-017-0043-4
Lioce, L., Lopreiato, J. O., Dowing, D., Chang, T. P., Robertson, J. M., Anderson, M., et al. the Terminology and Concepts Working Group (2020). Healthcare Simulation Dictionary. 2nd ed. Rockville, USA: Agency for Healthcare Research and Quality. doi:10.23970/simulationv2
Lopreiato, J. O. (2016). Healthcare Simulation Dictionary. Rockville, USA: Agency for Healthcare Research and Quality. Available at: https://www.ahrq.gov/sites/default/files/publications/files/sim-dictionary.pdf (Accessed January 12, 2021).
Maas, N. A., and Flood, L. S. (2011). Implementing High-Fidelity Simulation in Practical Nursing Education. Clin. Simulation Nurs. 7 (6), e229–e235. doi:10.1016/j.ecns.2010.04.001
Masters, K. S., Beacham, A. O., and Clement, L. R. (2015). Use of a Standardized Patient Protocol to Assess Clinical Competency: The University of Colorado Denver Comprehensive Clinical Competency Examination. Train. Educ. Prof. Psychol. 9 (2), 170–174. doi:10.1037/tep0000079
McGaghie, W. C., Issenberg, S. B., Petrusa, E. R., and Scalese, R. J. (2010). A Critical Review of Simulation-Based Medical Education Research: 2003â"2009. Med. Educ. 44 (1), 50–63. doi:10.1111/j.1365-2923.2009.03547.x
McNaughton, N., Ravitz, P., Wadell, A., and Hodges, B. D. (2008). Psychiatric Education and Simulation: A Review of the Literature. Can. J. Psychiatry 53 (2), 85–93. doi:10.1177/070674370805300203
Meghani, D. T., and Ferm, B. R. (2019). Development of a Standardized Patient Evaluation Exam: An Innovative Model for Health Service Psychology Programs. Train. Educ. Prof. Psychol. 15, 37–44. doi:10.1037/tep0000291
Milkins, L., Moore, C., and Spiteri, J. (2014). Simulation Based Education: Professional Entry Student Education and Training. St Leonards, Australia: Health Education and Training Institute. Available at: http://hdl.voced.edu.au/10707/440746. (Accessed January 12, 2021).
Motola, I., Devine, L. A., Chung, H. S., Sullivan, J. E., and Issenberg, S. B. (2013). Simulation in Healthcare Education: A Best Evidence Practical Guide. AMEE Guide No. 82. Med. Teach. 35 (10), e1511–e1530. doi:10.3109/0142159X.2013.818632
Mutter, M. K., Martindale, J. R., Shah, N., Gusic, M. E., and Wolf, S. J. (2020). Case-Based Teaching: Does the Addition of High-Fidelity Simulation Make a Difference in Medical Students' Clinical Reasoning Skills?. Med.Sci.Educ. 30 (1), 307–313. doi:10.1007/s40670-019-00904-0
Nestel. D, M. Kelly, B. Jolly, and M. Watson (Editors) (2017). Healthcare Simulation Education: Evidence, Theory and Practice (Oxford, England: John Wiley & Sons). doi:10.1002/9781119061656
Nel, P. W. (2010). The Use of an Advanced Simulation Training Facility to Enhance Clinical Psychology Trainees' Learning Experiences. Psychol. Learn. Teach. 9 (2), 65–72. doi:10.2304/plat.2010.9.2.65
Oberhauser, M., and Dreyer, D. (2017). A Virtual Reality Flight Simulator for Human Factors Engineering. Cogn. Tech. Work 19 (2), 263–277. doi:10.1007/s10111-017-0421-7
Orrell, J. (2011). Good Practice Report: Work-Integrated Learning. Sydney, Australia: Australian Learning and Teaching Council. Available at: https://ltr.edu.au/resources/GPR_Work_Integrated_Learning_Orrell_2011.pdf. (Accessed January 12, 2021).
Oxlad, M., D'Annunzio, J., Sawyer, A., and Paparo, J. (2020). Simulation Based Learning in Postgraduate Professional Pscyhology Training Programs: Student Perceptions of Experiences and Introduction of Extended Simulation Based Learning. unpublished manuscript.
Psychology Board of Australia (2019). Registration Standard: Area of Practice Endorsements. Available at: https://www.psychologyboard.gov.au/News/2019-11-18-new-registration-standard-and-guidelines.aspx. (Accessed January 12, 2021).
Psychology Board of Australia (2017). Registration Standard: Provisional Registration. Available at: https://www.psychologyboard.gov.au/Standards-and-Guidelines/Registration-Standards.aspx. (Accessed January 12, 2021).
Roberts, R., Chur-Hansen, A., Winefield, H., Patten, S., Ward, H., and Dorstyn, D. (2017). Using OSCEs with Simulation to Maximise Student Learning and Assess Competencies in Psychology: A Pilot Study. FoHPE 18 (2), 61–75. doi:10.11157/fohpe.v18i2.140
Roberts, R. M., Oxlad, M., Dorstyn, D., and Chur‐hansen, A. (2020). Objective Structured Clinical Examinations with Simulated Patients in Postgraduate Psychology Training: Student Perceptions. Aust. Psychol. 55 (5), 488–497. doi:10.1111/ap.12457
Rudd, C., Dobozy, E., and Smith, P. (2010). Use of Simulated Learning Environments in Clinical Psychology Curricula. Canberra, Australia: Health Workforce Australia.
Rutherford-Hemming, T. (2012). Simulation Methodology in Nursing Education and Adult Learning Theory. Adult Learn. 23 (3), 129–137. doi:10.1177/1045159512452848
Sheen, J., McGillivray, J., Gurtman, C., and Boyd, L. (2015). Assessing the Clinical Competence of Psychology Students through Objective Structured Clinical Examinations (OSCEs): Student and Staff Views. Aust. Psychol. 50 (1), 51–59. doi:10.1111/ap.12086
Sheen, J., Sutherland‐Smith, W., Thompson, E., Youssef, G. J., Dudley, A., King, R., et al. (2020). Evaluating the Impact of Simulation‐based Education on Clinical Psychology Students' Confidence and Clinical Competence. Clin. Psychol., 1–12. doi:10.1111/cp.12209
Sheen, J., Sutherland-Smith, W., Dudley, A., Boyd, L., and McGillivray, J. (2016). “Enhancing Psychology Students,” in clinical competence in risky environments through SBE Unknown conference name, Dublin, Ireland, 26th–28th October.
Simon, N. M., Saxe, G. N., and Marmar, C. R. (2020). Mental Health Disorders Related to COVID-19-Related Deaths. JAMA 324 (15), 1493–1494. doi:10.1001/jama.2020.19632
Simpson, S. G., Rochford, S., Livingstone, A., English, S., and Austin, C. (2014). Tele‐web Psychology in Rural South Australia: The Logistics of Setting Up a Remote University Clinic Staffed by Clinical Psychologists in Training. Aust. Psychol. 49 (4), 193–199. doi:10.1111/ap.12049
Stegmann, K., Pilz, F., Siebeck, M., and Fischer, F. (2012). Vicarious Learning during Simulations: Is it More Effective Than Hands-On Training?. Med. Educ. 46 (10), 1001–1008. doi:10.1111/j.1365-2923.2012.04344.x
Strasser, J., and Gruber, H. (2015). Learning Processes in the Professional Development of Mental Health Counselors: Knowledge Restructuring and Illness Script Formation. Adv. Health Sci. Educ. 20 (2), 515–530. doi:10.1007/s10459-014-9545-1
Tuttle, N., and Horan, S. A. (2019). The Effect of Replacing 1 Week of Content Teaching with an Intensive Simulation-Based Learning Activity on Physiotherapy Student Clinical Placement Performance. Adv. Simul 4 (1), 14. doi:10.1186/s41077-019-0095-8
Vandyk, A. D., Lalonde, M., Merali, S., Wright, E., Bajnok, I., and Davies, B. (2018). The Use of Psychiatry-Focused Simulation in Undergraduate Nursing Education: A Systematic Search and Review. Int. J. Ment. Health Nurs 27 (2), 514–535. doi:10.1111/inm.12419
Keywords: simulation-based learning, professional psychology, competency-based training, Australian psychologists, psychology training and education
Citation: (2021) A New Reality: The Role of Simulated Learning Activities in Postgraduate Psychology Training Programs. Front. Educ. 6:653269. doi: 10.3389/feduc.2021.653269
Received: 14 January 2021; Accepted: 13 July 2021;
Published: 09 August 2021.
Edited by:
Geneviève Pagé, University of Quebec in Outaouais, CanadaReviewed by:
Daniela Dumulescu, Babeş-Bolyai University, RomaniaMelissa Christine Davis, Edith Cowan University, Australia
Copyright © 2021 Australian Postgraduate Psychology Simulation Education Working Group (APPESWG). This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Josephine Paparo, am9zZXBoaW5lLnBhcGFyb0BhY2FwLmVkdS5hdQ==
 Australian Postgraduate Psychology Simulation Education Working Group (APPESWG)
Australian Postgraduate Psychology Simulation Education Working Group (APPESWG)