- Department of Kinesiology, NeuroFit Lab, McMaster University, Hamilton, ON, Canada
Introduction: The COVID-19 pandemic brought on higher-than-normal levels of anxiety and depression, especially among graduate students whose academic trajectory was disrupted. However, not all graduate students were affected and therefore, it is important to identify potential protective factors.
Method: We recruited 61 graduate students whose research was directly impacted by the pandemic and examined their change in academic stressors since the onset of the pandemic. Hierarchical regression analyses were used to evaluate how perceived academic stressors brought on by the COVID-19 pandemic impacted anxiety, depression, and heart rate variability (HRV), and whether physical activity and trait resiliency independently buffered against the effects of stress.
Results: Graduate students who reported greater changes in academic stressors since the onset for the pandemic were more anxious and depressed. Moderate-intensity physical activity explained significant variance in anxiety whereas resiliency explained significant variance in both anxiety and depression. HRV was higher in males than females, aligning with sex differences in vulnerability to stress and mental illness.
Conclusion: Overall, the results suggest that resiliency and physical activity may offer unique protection against symptoms of anxiety and depression in graduate students experiencing increased academic stress during COVID-19. Institutions of higher education should consider investing in programs that encourage physical activity and promote resiliency by teaching mindfulness, stress management, and cognitive behavioral approaches.
Introduction
Although globally, the pandemic caused rates of anxiety and depression to increase by over thirty percent (Xiong et al., 2020), graduate students and other young to middle aged adults may have been disproportionally affected (Varma et al., 2021). Under normal circumstances, young to middle aged adults are at a particularly high risk of experiencing onset of mental illness. The majority of mental disorders onset during early to middle adulthood, with a median range of 25 to 53 years old for anxiety disorders and 25 to 45 years old for other mood disorders (Kessler et al., 2007). Furthermore, onset of mental illness is often triggered by stressful life events (McLaughlin et al., 2010). Graduate students whose median age at graduation ranges from 28 to 32 years (Statistics Canada, 2019), have reported higher-than-normal levels of anxiety and depression during the pandemic because of the uncertainty surrounding their academic trajectory, environmental changes, and disruption to laboratory-based research (Chirikov et al., 2020; Suart et al., 2021). These stressors may be especially present among students in human and health sciences, where research often involves in-person data collection which was directly impacted by lockdown protocols (Suart et al., 2021). Canada’s response to the pandemic included widespread closure of green spaces, national parks, recreational facilities, gyms, and dance studios, which negatively impacted physical activity participation and mental health (Marashi et al., 2021). It is important to understand how we can support the mental health of graduate students now and in the aftermath of the pandemic. The current study sought to examine the protective effects of physical activity and trait resiliency (Jacob et al., 2020; Rogowska et al., 2020; Kavčič et al., 2021; Marashi et al., 2021).
Regular engagement in moderate-to-vigorous physical activity (MVPA) has been shown to reduce the risk of stress-induced mental illness (Gerber and Pühse, 2009). Moderate intensity activity can be described as physical activity that is performed at 40-59% of heart rate reserve (HRR; max HR-rest HR) or at a rated perceived exertion (RPE) of five to six on a ten-point scale. Examples of moderate intensity activity include brisk walking, dancing, and raking the yard (MacIntosh et al., 2021). Vigorous intensity exercise can be described as physical activity that is performed at 60-84% of HRR or at a RPE of seven to eight on a ten-point scale. Examples of vigorous intensity exercise include jogging, running, carrying heavy loads upstairs, or participating in a strenuous fitness class (MacIntosh et al., 2021). A key physiological change induced by regular MVPA is increased cardiorespiratory fitness. Higher fit individuals tend to be less prone to anxiety and depression (Kandola et al., 2019), and the protective effects of cardiorespiratory fitness against depression seem to be stronger for groups experiencing higher perceived stress (Gerber et al., 2013). Cardiorespiratory fitness also correlates with heart rate variability (HRV), an index of autonomic nervous system functioning, and it may be through improved HRV that regular engagement in MVPA protects one against stress-induced mental illness (Levy et al., 1998; Sandercock et al., 2005; Hallman et al., 2017). HRV, defined as the beat-to-beat variability of the heart measured over time (McCraty and Shaffer, 2015), is influenced by the dynamic interaction between the two branches of the autonomic nervous system (McCorry, 2007). Resting HRV has been identified as an important biomarker of autonomic flexibility in response to environmental stressors (Mulcahy et al., 2019), and when higher fit individuals experience a stressor, they exhibit higher HRV than their untrained peers, indicating less stress reactivity (Klaperski et al., 2014; von Haaren et al., 2016).
Trait resiliency can be conceptualized as the ability to rebound from a stressful event (Luthar et al., 2000), and as with physical activity, is predictive of better mental health outcomes and less stress reactivity in response to stressful events (Souza et al., 2007). Perhaps, not surprising, people with higher cardiorespiratory fitness also tend to score higher on measures of trait resiliency (Silverman and Deuster, 2014), which begs the question: how uniquely related are physical activity and trait resiliency to a graduate student’s stress response? Characterizing the unique contribution of physical activity and trait resiliency to graduate student well-being is critical for identifying intervention strategies during and post-pandemic.
Considering the paucity of research exploring the impact of COVID-19 on the mental and physical health of graduate students, the objective of the current study was to explore changes in perceived academic stressors brought on by the COVID-19 pandemic. We expected that increases in perceived stress would predict higher symptoms of anxiety and depression, and lower HRV. A second objective of the study was to test whether physical activity and trait resiliency buffered the effect of stress and to quantify the unique variance captured by each.
Materials and methods
The study followed a cross-sectional design. All participants were provided with an information sheet outlining the study protocol and were instructed to complete each step as follows. Participants filled out an online questionnaire using the platform LimeSurvey. Resting heart rate and HRV were measured each morning for one week using a mobile application. All steps were done asynchronously and unsupervised.
Participants
Based on prior research (Chalmers et al., 2014; Papasavvas et al., 2016), a small-to-moderate effect size was expected (Cohen’s f = 0.20) and a total of approximately 67 participants would be required, as estimated by G*Power (Faul et al., 2007) with ß = 0.90; α = 0.05. Participants were recruited through social media advertisements (Twitter, Facebook, Instagram, Reddit) and by email to graduate student associations across Canada.
Participants were eligible if they were 18 years of age or older, currently enrolled in full-time studies in a thesis-based graduate degree program and could confirm that their research efforts had been affected by COVID-19 restrictions such that they experienced significant disruption and/or delay to their research program. To hone in on the unique experience of thesis-based graduate studies, professional and non-research based students were deemed ineligible. Participants were recruited and participated in the study between the period of November 2020 and April 2021 during which Canadian residents were facing the second and third waves of the COVID-19 pandemic, which included extensive closures. Additionally, to control for the effect of confounding variables, participants were required to confirm that they were free from diagnosis of diabetes type 1 or 2, cardiovascular or cerebrovascular disease, infectious disease, or acute illness; that they were non-smokers, had a BMI of 35 or less, were not taking prescription drugs to treat anxiety, depression, or blood pressure, and were not currently using illicit drugs. The fulfilment of these criteria was confirmed verbally over the phone. This study received ethics clearance from McMaster Research Ethics Board (MREB #5100). Written informed consent for participation was required for this study in accordance with the national legislation and the institutional requirements. Participants were compensated $25 CAD for their participation.
Materials
Questionnaires
The online survey collected demographic information on the participants including biological sex, gender, age, faculty of study, and income. The survey also included the following questionnaires.
Change in academic stress
Change in perceived stress related to academics since the onset of the COVID-19 pandemic was measured using an adapted version of the Graduate Stress Inventory-Revised (GSI-R) (Rocha-Singh, 1994). Its items are categorized into three domains of graduate student experience: (1) university environment, (2) academic and professional responsibilities, and (3) financial and familial responsibilities. Normally, the GSI-R is rated on a “not at all stressful” to “extremely stressful” 7-point Likert scale. Given the unprecedented circumstances, there were no existing psychometric tools designed to measure the impact of COVID-19 on graduate-school-related stress. Therefore, in the current study, we adapted the GSI-R to capture a difference in perceived stress from 6-months prior to COVID-19 to the onset of COVID-19. Specifically, participants were asked to rate how much stress they have perceived in “…relation to the following events encountered in graduate school since the onset of COVID-19 relative to 6-months prior to COVID-19”. Responses included “much less” (−2), “less” (−1), “the same” (0), “more” (+ 1) and “much more” (+ 2). Item scores were summed for a maximum of 50 and minimum of −50. In the current study sample, Cronbach’s α = 0.87, indicating good internal consistency (George and Mallery, 2019).
Anxiety
Anxiety was measured using the Generalized Anxiety Disorder 7-item (GAD-7) Scale (Spitzer et al., 2006). The GAD-7 is a validated tool used to measure anxiety symptoms associated with generalized anxiety disorder (GAD) and asks participants to score each of the seven DSM-IV criteria of GAD, on a scale from 0 to 3 (0 = not at all, 3 = nearly every day). Item scores were summed for a maximum score of 21 (none/minimal, 0-4; mild, 5-9; moderate, 10-14; severe, 15-21; Spitzer et al., 2006). In the current study sample, Cronbach’s α = 0.91, indicating excellent internal consistency (George and Mallery, 2019).
Depression
Depression was measured using a modified version of the Patient Health Questionnaire-9 (PHQ-9) (Gilbody et al., 2007). The PHQ-9 is a validated tool used to monitor depressive symptoms and asks participants to score each of the nine DSM-IV criteria of Major Depressive Disorder (MDD), on a scale from 0 to 3 (0 = not at all, 3 = nearly every day; Gilbody et al., 2007). Due to concerns surrounding disclosure of sensitive information, the ninth item regarding suicidal thoughts and self-harm was omitted. Item scores were summed for a maximum score of 24 (none/minimal, 0-4; mild, 5-9; moderate, 10-14; moderately severe, 15-19; severe, 20-24). In the current study sample, Cronbach’s α = 0.85, indicating good internal consistency (George and Mallery, 2019).
Resiliency
Resiliency was operationalized using the 14-item Resilience Scale (RS-14) (Wagnild, 2009). The RS-14 measures five characteristics of resiliency: (1) purpose, (2) perseverance, (3) equanimity, (4) self-reliance, and (5) existential aloneness (Wagnild, 2009). The RS–14 employs a 7-point Likert scale (1 = strongly disagree, 7 = strongly agree). Item scores were summed for a maximal score of 98 (low, < 64; moderate, 65-81; moderately high, 82-90; high, > 90). In the current study sample, Cronbach’s α = 0.88, indicating good internal consistency (George and Mallery, 2019).
Physical activity
Self-reported physical activity and sedentary behavior was measured using the International Physical Activity Questionnaire (IPAQ) (Wanner et al., 2016). Specifically, participants were asked to denote the number of minutes per week that they typically engage in moderate physical activity (e.g., carrying light loads or bicycling at a regular pace) and vigorous physical activity (e.g., heavy lifting, digging, aerobics or fast bicycling). Minutes per week of total MVPA as well as moderate physical activity and vigorous physical activity were calculated.
Heart rate variability
HRV is typically measured using an electrocardiogram (ECG); however, readily accessible measurements using smartphone photoplethysmography (PPG) (Dobbs et al., 2019) show acceptable agreement with gold standard measures (Plews et al., 2017). In our study, HRV was measured using the mobile application, HRV4Training (HRV4T)1. HRV4T is a validated tool that utilizes photoplethysmography to detect volumetric changes in blood peripheral circulation by illuminating the skin and measuring changes in light absorption. The mobile application calculates the time difference between successive heart beats in milliseconds and automatically computes the root mean square of successive differences between R-R intervals (rMSSD) by squaring each data point, computing the average of those squared data points, and taking the square root of that average (Shaffer and Ginsberg, 2017). Although no measure of HRV is known to clearly indicate sympathetic activity, both rMSSD and high frequency (HF) HRV are shown to reflect parasympathetic activity (Thayer and Lane, 2000; Kleiger et al., 2005). We used rMSSD because it is relatively free of respiratory influences (Hill et al., 2009) and is shown to be the most accurate index in the context of short-term R-R interval readings (i.e., 5 min or less) (Munoz et al., 2015).
Participants used the HRV4T application to calculate rMSSD by placing their index finger over their smartphone’s camera and LED flash for a five-minute reading. They did this upon waking, while lying in a supine position and breathing normally, for seven consecutive days and the average rMSSD reading across those seven days was used in the analysis. To mitigate issues related to accuracy of readings, participants were instructed to ensure that their daily HRV reading was deemed “Optimal” by the application before it was stored. An “Optimal” reading is defined by the application developers as being “…clean with either no ectopic beats or issues due to motion artifacts or a very limited amount of noise that could be dealt with by our artifact removal algorithms1”. “Optimal” readings were confirmed by the researcher during data export. At the end of the week, participants forwarded their heart rate and HRV data directly from the HRV4T application to the researcher.
Statistical analysis
Data were analyzed using IBM SPSS (Version 26). Descriptive statistics were computed for all study variables. Normality was assessed using visual inspection of histograms, and skewness and kurtosis based on recommendations by Kim (2013). Missing values were analyzed for pattern of missing data using Little’s MCAR test. For all statistical analyses, a p value (2-tailed) < 0.05 was considered significant.
Sex differences in demographics were assessed with parametric and non-parametric t tests. Bivariate correlations were conducted for all study variables examined in the main analyses.
Separate hierarchical regression analyses were conducted for anxiety, depression, and HRV to first determine how changes in perceived academic stress affected mental health and to then determine the independent contribution of physical activity (moderate and vigorous) and trait resiliency. Age and biological sex were included as covariates.
Multicollinearity was assessed using tolerance and variance inflation factor (VIF). Homogeneity of variance and normality of residuals were assessed by plotting residuals against the predicted values. Independence of residuals was assessed using the Durbin-Watson test. In step 1, age and biological sex (coded: 0 = males; 1 = females) were entered to control for the age-related depletion of HRV as well as the established differences between males and females for anxiety and depression (Gater et al., 1998) and perceived stress (Brougham et al., 2009). In step 2, change in perceived academic stressors was entered, and in step 3, trait resiliency, moderate physical activity, and vigorous physical activity were entered stepwise.
Results
Data screening and assumptions
Sixty-eight participants were recruited for the study, five participants did not submit their data or follow up with emails, and therefore, 63 participants completed the entire protocol. Two participants were removed from analyses: one withdrew their data, and the other withdrew because of a family emergency. The final sample consisted of 61 participants.
Data were screened for missing data; 0.5% was missing (BMI, n = 2; Year of Study n = 1; Income Since COVID, n = 2; Income Pre COVID, n = 2). The pattern of missingness was missing completely at random (MCAR), according to Little’s MCAR test. Therefore, no replacement strategy was employed, and listwise deletion was used for missing values. Dependent variables (anxiety and depression) had skewness and kurtosis within an acceptable range and all assumptions for linear regression were met (Field, 2013).
Demographics
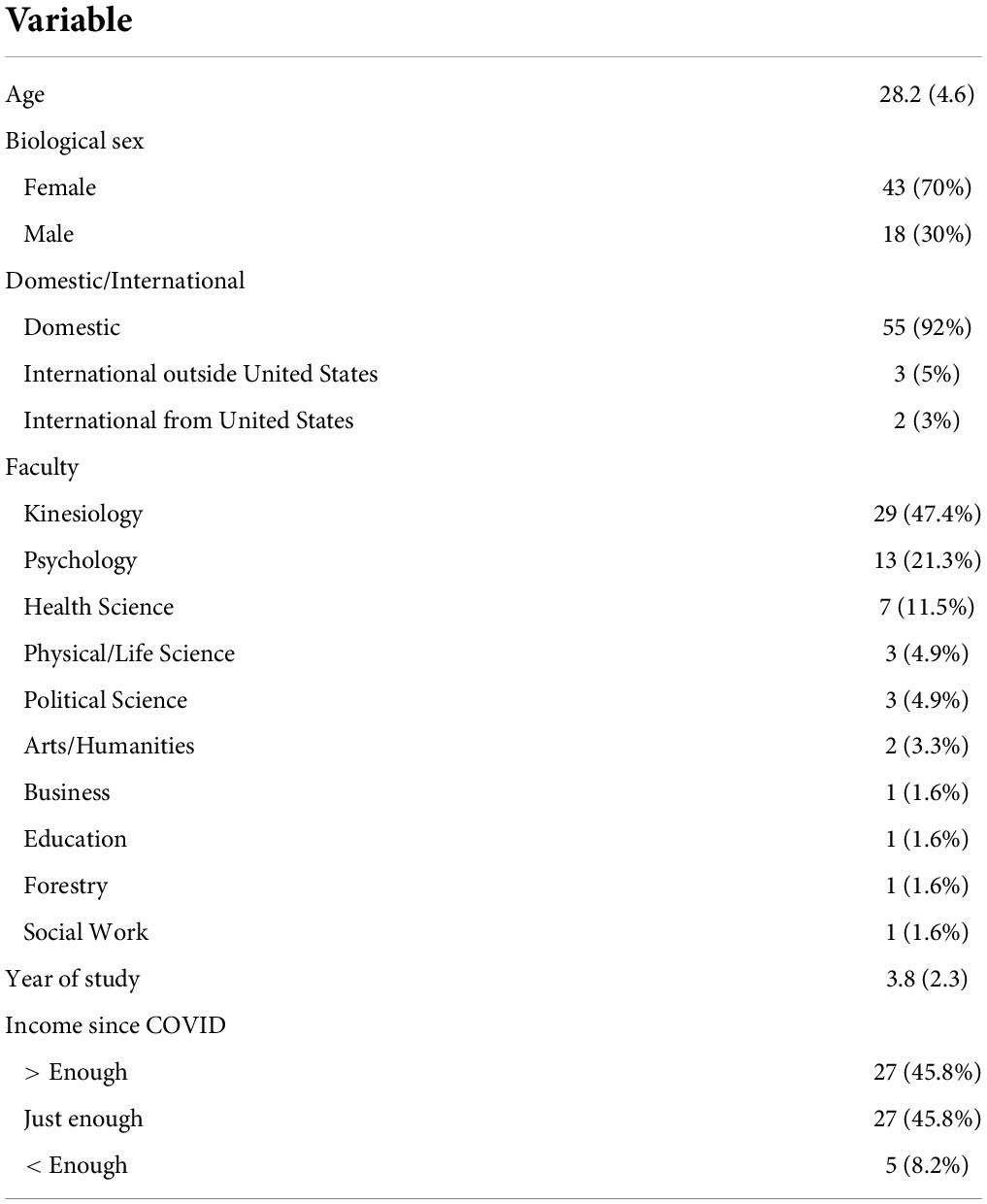
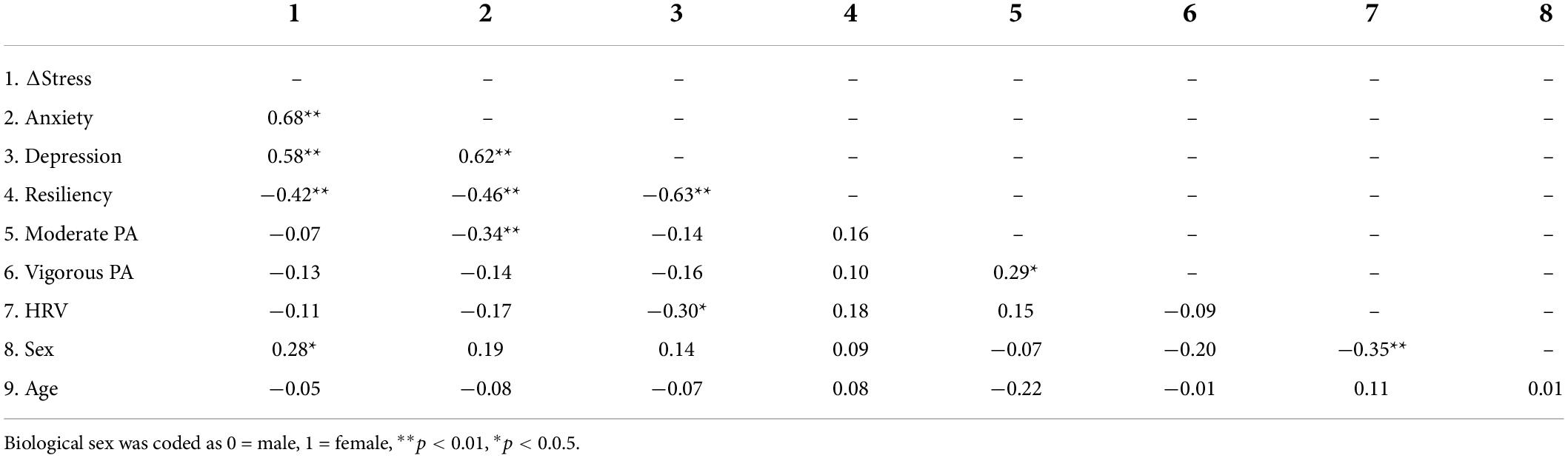
The demographics are presented in Tables 1, 2, and bivariate Spearman correlations for main study variables are displayed in Table 3. Participants were graduate students between the ages of 22 and 46 years with a mean age of 28.2 years. All females identifying as women and all males identifying as men. Most participants were domestic students (92%) enrolled in a kinesiology (47.5%), Psychology (21.3%), or Health Science (11.5%) program and rated their current financial status as “earning just enough” (45.8%) or “earning more than enough” (45.8%). Therefore, it was a relatively homogenous sample.
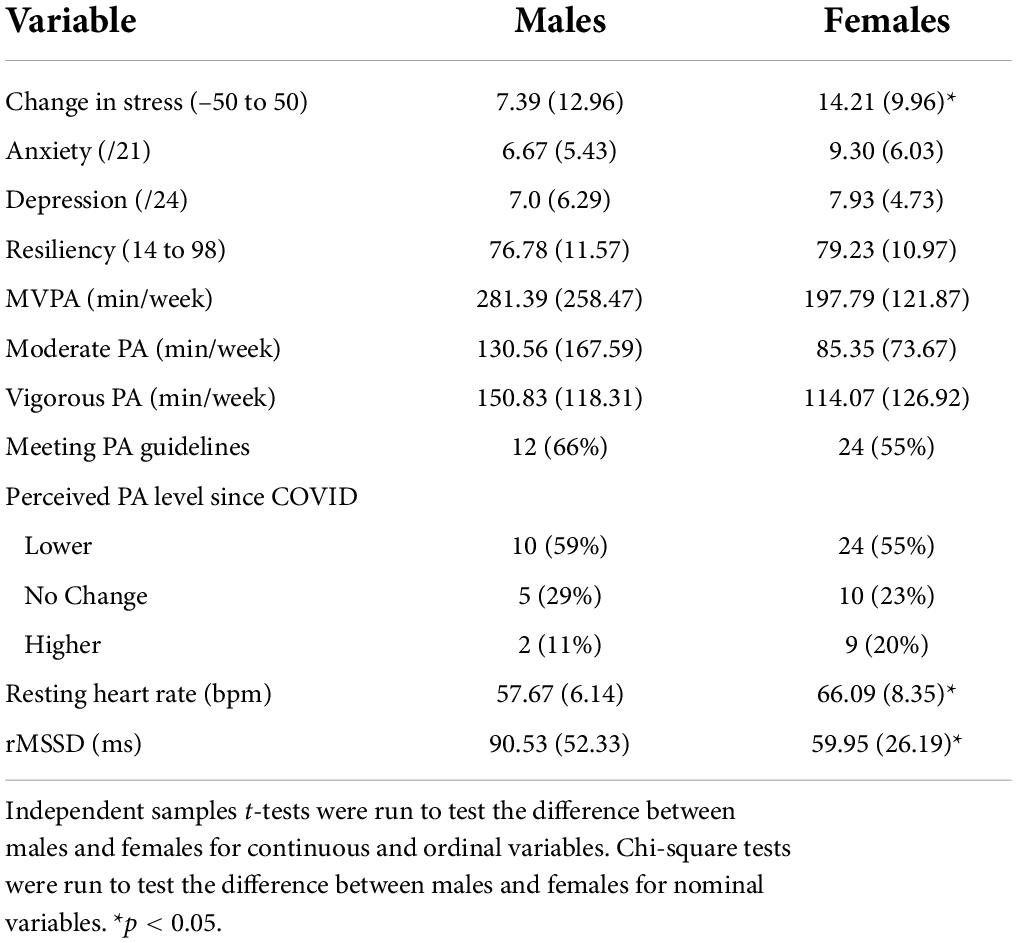
Participants were experiencing more academic stress since the onset of the pandemic. Notably, females reported a greater increase academic stress than males. On average, anxiety and depressive symptoms were mild (Kroenke and Spitzer, 2002; Spitzer et al., 2006), resiliency was moderate (Wagnild, 2016), and there were no sex differences in anxiety, depression, or resiliency scores.
The sample was highly physically active with a mean moderate-to-vigorous physical activity (MVPA) of 223.6 min (> 3 h) per week, which exceeds that of the recommended 150 minutes (2.5 hours) per week (Ross et al., 2020). Just over half of respondents reported meeting the guidelines; however, nearly sixty percent reported that their physical activity level had dropped since the start of the pandemic. There were no sex differences in either measure of physical activity.
Resting heart rate was considered normal (Nanchen, 2018) and females exhibited higher resting heart rate than males. HRV indicated by rMSSD was in the ideal range and males exhibited a higher HRV than females (Heiss et al., 2021).
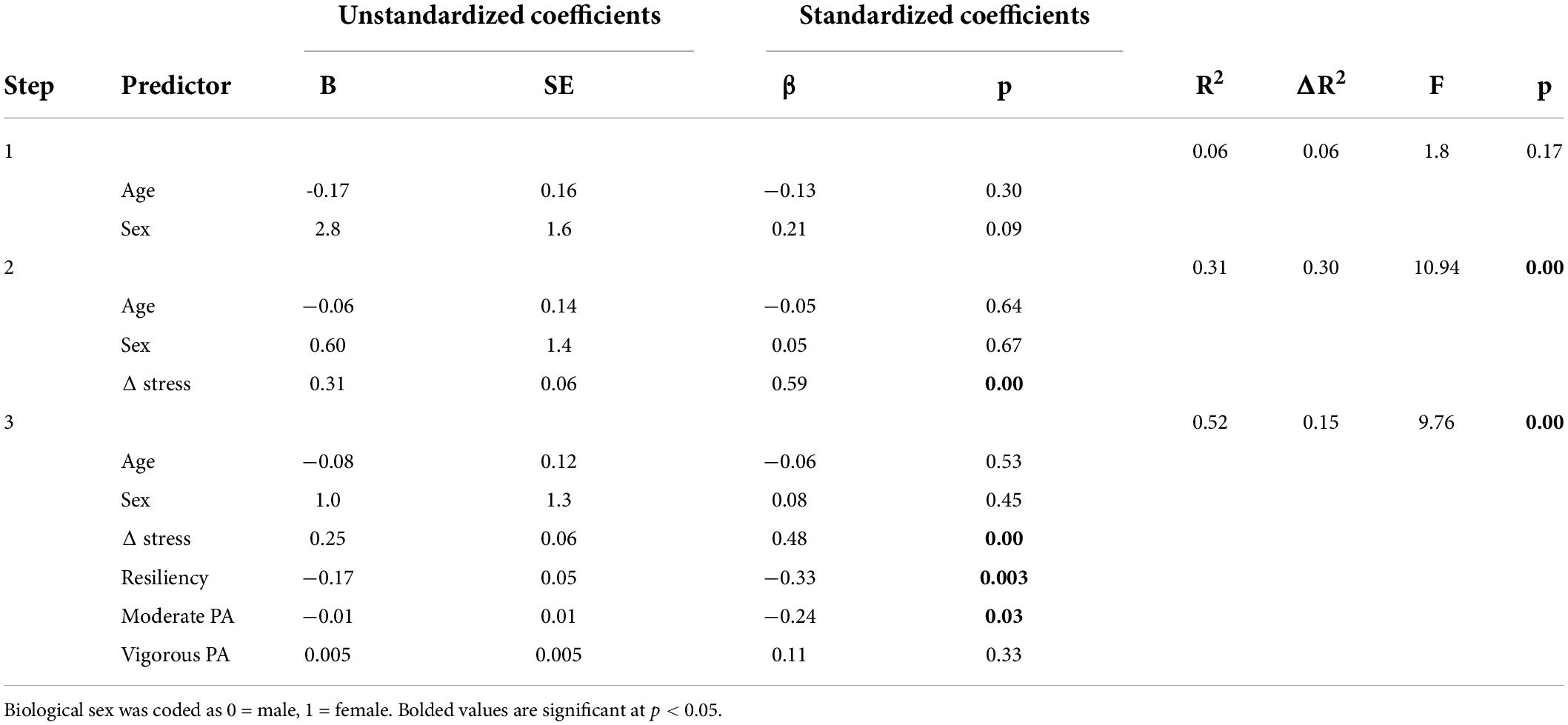
Anxiety
Hierarchical regression coefficients for anxiety are displayed in Table 4. Change in stress explained 31% of the variance (b = 0.58, p < 0.001, f2 = 0.30) (step 2, ΔF(3, 57) = 27.56, p < 0.001), indicating that participants who reported more academic stress since the onset of the pandemic were more anxious. An additional 15% of variance was explained by resiliency (b = -0.32, p = 0.003, f2 = 0.09) and moderate physical activity (b = −0.25, p = 0.03, f2 = 0.04), (step 3, ΔF(6, 54) = 5.81, p > 0.001), indicating that higher resiliency and more moderate physical activity levels buffered against stress-induced anxiety.
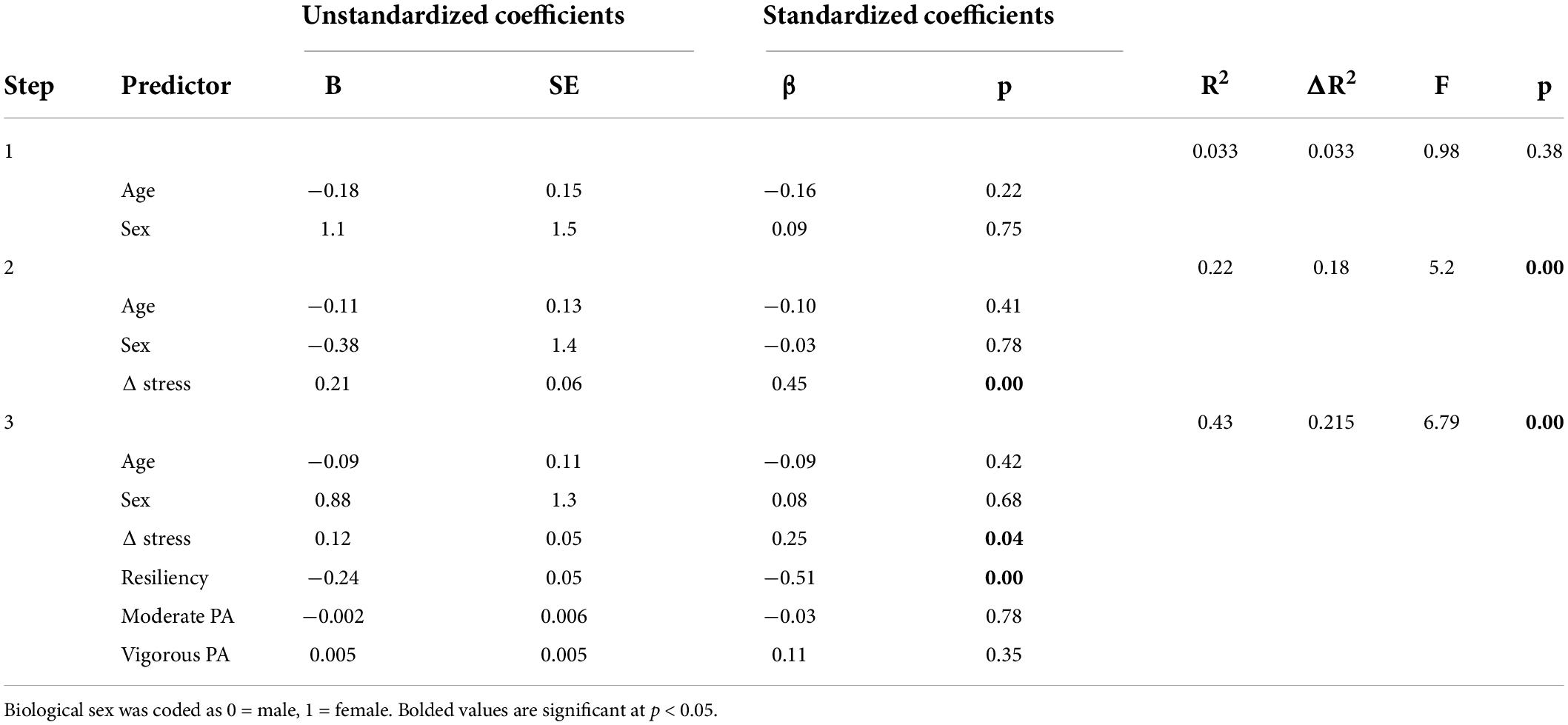
Depression
Hierarchical regression coefficients for depression are displayed in Table 5. Change in stress explained 18% of the variance (b = 0.21, p < 0.001, f2 = 0.18) (step 2, ΔF(3, 57) = 13.24, p < 0.001), indicating that participants who reported more stress since the onset of the pandemic were more depressed. An additional 22% of variance was explained by resiliency (b = −0.24, p < 0.001, f2 = 0.20) (step 3, ΔF(6, 54) = 6.79, p < 0.001), indicating that participants with higher resiliency buffered against stress-induced depression.
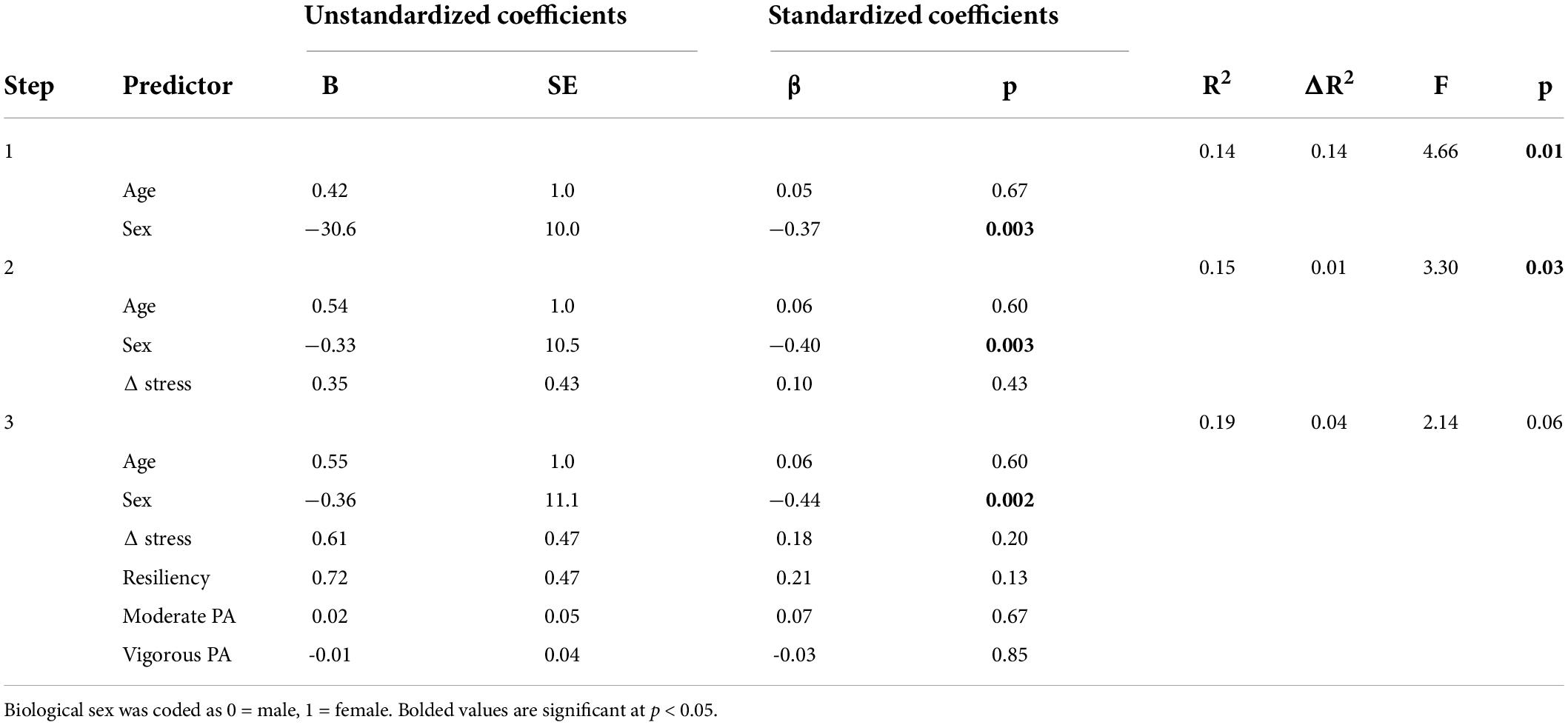
HRV
Hierarchical regression coefficients for HRV are displayed in Table 6. Biological sex explained 14% of variance (b = −0.37, p = 0.003, f2 = 0.13) (step 1, ΔF(2, 58) = 4.66, p = 0.01), indicating higher (i.e., more favorable) HRV for males than females. No other associations were significant.
Discussion
The current study aimed to explore changes in perceived graduate school-related stressors brought on by the COVID-19 pandemic and to test whether physical activity and trait resiliency buffered the effect of stress. In a sample of Canadian research-based graduate students, those who experienced greater increases in academic stressors since the onset of the COVID pandemic were more anxious and depressed. However, those who engaged in more moderate physical activity were less anxious, and those with higher resiliency were less anxious and depressed, suggesting protective effects. Females had higher resting heart rate, lower HRV, and greater increases in stress than males, suggesting that females may be at greater risk of stress-induced mental illness. Furthermore, lower HRV was associated with higher depression scores (Table 3).
Moderate but not vigorous physical activity was associated with less anxiety. Although past research examining the effects of exercise on anxiety are mixed (Aylett et al., 2018; Henriksson et al., 2022), we have previously demonstrated that moderate exercise (and not vigorous exercise) may be more suitable for Lucibello et al. (2020) and offers better protection against stress-induced anxiety (Paolucci et al., 2018). Other studies suggest moderate exercise is better for individuals suffering with anxiety sensitivity who become more anxious when experiencing somatic symptoms of anxiety such as labored breathing and elevated heart rate which are both elicited by vigorous exercise (Zinbarg et al., 1999; Tabor et al., 2019). Institutional-level efforts to foster access to lower-to-moderate intensity physical activities may be met through the development of on-campus spaces such as Yoga and/or cycling studios, and green spaces. The use of physical activity as a tool to manage symptoms of mental health is well supported, however it is important to recognize the interaction between anxiety and exercise addiction. Specifically, it is suggested that higher levels of anxiety may be associated with an increased need for exercise as well as more frequent and intense sessions which may subsequently lead to over-training syndrome and exacerbated anxiety symptoms (Berczik et al., 2012). This is thought to be especially relevant during stressful situations (Berczik et al., 2012). Efforts to increase physical activity levels in at-risk populations (i.e., females) should take these potential reciprocal effects into account.
Although anxiety and depression tend to be comorbid, neither moderate nor vigorous physical activity were associated with depression. This finding contrasts with prior studies and may be due to the unprecedented circumstances surrounding the pandemic. Notably, the lack of social engagement that is typically part of a physical activity program but was missing during the pandemic is an important factor that may be impacting the effects of physical activity on depression (Harvey et al., 2010; Hallgren et al., 2017; Marashi et al., 2021).
Trait resiliency was associated with both anxiety and depression. This finding aligns with the neurovisceral integration model which describes self-regulatory processes as underpinning appropriate cognitive responses to stress (Thayer et al., 2009). The relationship between resiliency and mental health measures may be due to its association with self-regulation (Mestre et al., 2017). Indeed, several items on the RS-14 describe a capacity to self-regulate during difficult or threatening situations (Ex: “In an emergency, I’m someone people can generally rely on”, “When I’m in a difficult situation, I can usually find my way out of it”). Students scoring high on resiliency may have adequate self-regulatory capacity, enabling them to respond more favorably to stress and preventing symptoms of anxiety and depression. Importantly, resiliency can be increased by intervention efforts that include mindfulness mediation (Kemper and Khirallah, 2015); stress management training that focuses on reframing stressful life experiences through principles such as gratitude, acceptance, and compassion (Magtibay et al., 2017); and cognitive behavioral approaches (Mache et al., 2015).
Although HRV was not associated with resiliency or physical activity (as predicted), it was influenced by biological sex, which is consistent with the literature (Koenig and Thayer, 2016). Females displayed significantly lower (i.e., unfavorable) resting HRV than males, and experienced greater increases in stress since the onset of the pandemic despite being exposed to similar environmental stressors. Given that HRV provides an index of one’s stress reactivity (Souza et al., 2007) and one’s stress reactivity predicts the development of mental illness (Charles et al., 2013), HRV may be an indicator of the biological disposition that predisposes females to experience higher rates of stress-induced mental illness than males. It is also important to acknowledge that our sample was predominately females who, under normal circumstances, are more susceptible to stress and mental illness (Gater et al., 1998; Brougham et al., 2009).
We expected resiliency and physical activity to be associated with HRV, but they were not. We believe this is a limitation of our cross-sectional design, and the multitude of factors that can influence HRV including cannabis use (Williams et al., 2021), sleep measures (da Estrela et al., 2021), nutrition (Young and Benton, 2018) and menstrual cycle phase (Brar et al., 2015) that were not controlled here. A longitudinal study design controlling for the above covariates is needed to examine the dynamic interrelationship between HRV, resiliency, physical activity, and mental health. One key advantage of using HRV is its relative accessibility and non-invasive nature. Therefore, developing sound transdiagnostic measures of mental health that are accessible and non-invasive provide a seamless way for health practitioners and researchers to diagnose, treat and monitor the health of patients or clients suffering from mental illness. It is important to note that we employed an unsupervised measure of HRV which may have impacted the accuracy of readings. However, although validated in research contexts (Plews et al., 2017), the mobile application used in our study was designed for commercial use which likely limited user-related errors. As well, participants were instructed to only store “Optimal” readings, which strengthens our confidence in the findings.
The negative relationship between depression and HRV noted in our correlational analyses is in line with literature exploring the link between HRV and general vulnerability to psychopathology. A wide range of psychiatric disorders (including depression) are characterized by low, and in some rare cases abnormally high (Heiss et al., 2021), resting HRV (Henje Blom et al., 2010; Kemp et al., 2012; Pittig et al., 2013; Chalmers et al., 2014; Beauchaine and Thayer, 2015). This finding may support the neurovisceral integration model suggesting that favorable responses to stress result partially from optimal inhibitory function of the prefrontal cortex over regions of the brain that govern emotional responses to stress (Thayer and Lane, 2000).
Limitations of our study include a convenience sample of graduate students predominately from kinesiology, psychology, and health science backgrounds, and who report high levels of physical activity, and thus, may not be representative of the Canadian graduate student population. It is also important to recognize that we did not collect demographic information pertaining to race or ethnicity which also limits our ability to generalize our findings. Our measure of change in stress is also a limitation as we asked participants to recall their stress levels prior to COVID-19. Longitudinal research is needed to explore changes in graduate-school related stress over time to explore its causal pathway with mental health measures, physical activity, and resiliency. Lastly, although we used a validated questionnaire, physical activity data was self-reported and is therefore subject to recall bias.
Conclusion
In summary, in a sample of graduate students, individuals experiencing more academic stressors since the onset of the COVID-19 pandemic were more anxious and depressed. However, students engaging in more moderate physical activity were less anxious, and those with higher resiliency were less anxious and depressed. Sex differences were also observed such that females had a lower resting HRV as well as larger increases in stress since the onset of the pandemic suggesting that HRV may be a potential biological mechanism for sex differences in susceptibility to stress-induced mental illness.
There is a dearth of literature examining efficacious tools to address mental health in graduate students even under normal circumstances. Results from our study provide groundwork for future research interested in addressing mental health concerns in this population. Overall, the results suggest that resiliency and physical activity may offer unique protection against symptoms of anxiety and depression in graduate students experiencing stress during COVID-19 and institutions of higher education should consider investing in programs that encourage physical activity and promote trait resiliency by teaching mindfulness, stress management and cognitive behavioral approaches.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by McMaster University MREB. The patients/participants provided their written informed consent to participate in this study.
Author contributions
MM and JH: conceptualization and writing (review and editing). MM: data collection, data analysis, and writing (first draft). Both authors contributed to the article and approved the submitted version.
Funding
This research was supported by the Natural Sciences and Engineering Research Council of Canada (NSERC) Discovery Grant 296518 to JH, and the Social Sciences and Humanities Research Council (SSHRC) Canada Graduate Scholarship to MM.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
Aylett, E., Small, N., and Bower, P. (2018). Exercise in the treatment of clinical anxiety in general practice–a systematic review and meta-analysis. BMC Health Serv. Res. 18:559. doi: 10.1186/s12913-018-3313-5
Beauchaine, T. P., and Thayer, J. F. (2015). Heart rate variability as a transdiagnostic biomarker of Psychopathology. Int. J. Psychophysiol. 98, 338–350. doi: 10.1016/j.ijpsycho.2015.08.004
Berczik, K., Szabó, A., Griffiths, M. D., Kurimay, T., Kun, B., Urbán, R., et al. (2012). Exercise addiction: Symptoms, diagnosis, epidemiology, and etiology. Substance Use Misuse 47, 403–417. doi: 10.3109/10826084.2011.639120
Brar, T. K., Singh, K. D., and Kumar, A. (2015). Effect of different phases of menstrual cycle on Heart Rate Variability (HRV). J. Clin. Diagn. Res. 9, CC01–CC4. doi: 10.7860/JCDR/2015/13795.6592
Brougham, R. R., Zail, C. M., Mendoza, C. M., and Miller, J. R. (2009). Stress, sex differences, and coping strategies among college students. Curr. Psychol. 28, 85–97. doi: 10.1007/s12144-009-9047-0
Chalmers, J. A., Quintana, D. S., Abbott, M. J. A., and Kemp, A. H. (2014). Anxiety disorders are associated with reduced heart rate variability: A meta-analysis. Front. Psychiatry 5:80. doi: 10.3389/fpsyt.2014.00080
Charles, S. T., Piazza, J. R., Mogle, J., Sliwinski, M. J., and Almeida, D. M. (2013). The wear and tear of daily stressors on mental health. Psychol. Sci. 24, 733–741. doi: 10.1177/0956797612462222
Chirikov, I., Soria, K. M., Horgos, B., and Org, E. (2020). Undergraduate and graduate students’ mental health during the COVID-19 Pandemic. SERU Consortium. Los Angeles, CA: University of California.
da Estrela, C., McGrath, J., Booij, L., and Gouin, J. P. (2021). Heart rate variability, sleep quality, and depression in the context of chronic stress. Ann. Behav. Med. 55, 155–164. doi: 10.1093/abm/kaaa039
Dobbs, W. C., Fedewa, M. V., MacDonald, H. V., Holmes, C. J., Cicone, Z. S., Plews, D. J., et al. (2019). The accuracy of acquiring heart rate variability from portable devices: A systematic review and meta-analysis. Sports Med. 49, 417–435. doi: 10.1007/s40279-019-01061-5
Faul, F., Erdfelder, E., Lang, A.-G., and Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39, 175–191. doi: 10.3758/BF03193146
Gater, R., Tansella, M., Korten, A., Tiemens, B. G., Mavreas, V. G., and Olatawura, M. O. (1998). Sex differences in the prevalence and detection of depressive and anxiety disorders in general health care settings: Report from the World Health Organization collaborative study on psychological problems in general health care. Arch. Gen. Psychiatry 55, 405–413. doi: 10.1001/archpsyc.55.5.405
George, D., and Mallery, P. (2019). IBM SPSS statistics 26 step by step: A simple guide and reference. New York, NY: Routledge.
Gerber, M., Lindwall, M., Lindegård, A., Börjesson, M., and Jonsdottir, I. H. (2013). Cardiorespiratory fitness protects against stress-related symptoms of burnout and depression. Patient Educ. Couns. 93, 146–152. doi: 10.1016/j.pec.2013.03.021
Gerber, M., and Pühse, U. (2009). Do exercise and fitness protect against stress-induced health complaints? A review of the literature. Scand. J. Public Health 37, 801–819. doi: 10.1177/1403494809350522
Gilbody, S., Richards, D., Brealey, S., and Hewitt, C. (2007). Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): A diagnostic meta-analysis. J. Gen. Internal Med. 22, 1596–1602. doi: 10.1007/s11606-007-0333-y
Hallgren, M., Lundin, A., Tee, F. Y., Burström, B., and Forsell, Y. (2017). Somebody to lean on: Social relationships predict post-treatment depression severity in adults. Psychiatry Res. 249, 261–267. doi: 10.1016/j.psychres.2016.12.060
Hallman, D. M., Holtermann, A., Søgaard, K., Krustrup, P., Kristiansen, J., and Korshøj, M. (2017). Effect of an aerobic exercise intervention on cardiac autonomic regulation: A worksite RCT among cleaners. Physiol. Behav. 169, 90–97. doi: 10.1016/j.physbeh.2016.11.031
Harvey, S. B., Hotopf, M., Øverland, S., and Mykletun, A. (2010). Physical activity and common mental disorders. Br. J. Psychiatry 197, 357–364. doi: 10.1192/bjp.bp.109.075176
Heiss, S., Vaschillo, B., Vaschillo, E. G., Timko, C. A., and Hormes, J. M. (2021). Heart rate variability as a biobehavioral marker of diverse psychopathologies: A review and argument for an “ideal range.”. Neurosci. Biobehav. Rev. 121, 144–155. doi: 10.1016/j.neubiorev.2020.12.004
Henje Blom, E., Olsson, E. M., Serlachius, E., Ericson, M., and Ingvar, M. (2010). Heart rate variability (HRV) in adolescent females with anxiety disorders and major depressive disorder. Int. J. Paediatr. 99, 604–611. doi: 10.1111/j.1651-2227.2009.01657.x
Henriksson, M., Wall, A., Nyberg, J., Adiels, M., Lundin, K., Bergh, Y., et al. (2022). Effects of exercise on symptoms of anxiety in primary care patients: A randomized controlled trial. J. Affect. Disord. 297, 26–34. doi: 10.1016/j.jad.2021.10.006
Hill, L. B. K., Siebenbrock, A., Sollers, J. J., and Thayer, J. F. (2009). Are all measures created equal? Heart rate variability and respiration. Biomed. Sci. Instr. 45, 71–76.
Jacob, L., Tully, M. A., Barnett, Y., Lopez-Sanchez, G. F., Butler, L., Schuch, F., et al. (2020). The relationship between physical activity and mental health in a sample of the UK public: A cross-sectional study during the implementation of COVID-19 social distancing measures. Ment. Health Phys. Act. 19:100345. doi: 10.1016/j.mhpa.2020.100345
Kandola, A., Ashdown-Franks, G., Stubbs, B., Osborn, D. P. J., and Hayes, J. F. (2019). The association between cardiorespiratory fitness and the incidence of common mental health disorders: A systematic review and meta-analysis. J. Affect. Disord. 257, 748–757. doi: 10.1016/j.jad.2019.07.088
Kavčič, T., Avsec, A., and Zager Kocjan, G. (2021). Psychological Functioning of Slovene Adults during the COVID-19 Pandemic: Does Resilience Matter? Psychiatr. Q. 92, 207–216. doi: 10.1007/s11126-020-09789-4
Kemp, A. H., Quintana, D. S., Felmingham, K. L., Matthews, S., and Jelinek, H. F. (2012). Depression, comorbid anxiety disorders, and heart rate variability in physically healthy, unmedicated patients: Implications for cardiovascular risk. PLoS One 7:e30777. doi: 10.1371/journal.pone.0030777
Kemper, K. J., and Khirallah, M. (2015). Acute effects of online mind–body skills training on resilience, mindfulness, and empathy. J. Evid. Based Complement. Altern. Med. 20, 247–253. doi: 10.1177/2156587215575816
Kessler, R. C., Amminger, G. P., Aguilar-Gaxiola, S., Alonso, J., Lee, S., and Ustun, T. B. (2007). Age of onset of mental disorders: A review of recent literature. Curr. Opin. Psychiatry 20, 359–364. doi: 10.1097/YCO.0b013e32816ebc8c
Kim, H. Y. (2013). Statistical notes for clinical researchers: Assessing normal distribution (2) using Skewness and kurtosis. Restor. Dent. Endod. 38, 52–54. doi: 10.5395/rde.2013.38.1.52
Klaperski, S., von Dawans, B., Heinrichs, M., and Fuchs, R. (2014). Effects of a 12-week endurance training program on the physiological response to psychosocial stress in men: A randomized controlled trial. J. Behav. Med. 37, 1118–1133. doi: 10.1007/s10865-014-9562-9
Kleiger, R. E., Stein, P. K., and Bigger, J. T. (2005). Heart rate variability: Measurement and clinical utility. Annals of Noninvasive Electrocardiology 10, 88–101. doi: 10.1111/j.1542-474X.2005.10101.x
Koenig, J., and Thayer, J. F. (2016). Sex differences in healthy human heart rate variability: A meta-analysis. Neurosci. Biobehav. Rev. 64, 288–310. doi: 10.1016/j.neubiorev.2016.03.007
Kroenke, K., and Spitzer, R. L. (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatr. Ann. 32, 509–515. doi: 10.3928/0048-5713-20020901-06
Levy, W. C., Cerqueira, M. D., Harp, G. D., Johannessen, K. A., Abrass, I. B., Schwarte, R. S., et al. (1998). Effect of endurance exercise training on heart rate variability at rest in healthy young and older men. Am. J. Cardiol. 82, 1236–1241. doi: 10.1016/S0002-9149(98)00611-0
Lucibello, K. M., Paolucci, E. M., Graham, J. D., and Heisz, J. J. (2020). A randomized control trial investigating high-intensity interval training and mental health: A novel non-responder phenotype related to anxiety in young adults. Ment. Health Phys. Act. 18:100327. doi: 10.1016/j.mhpa.2020.100327
Luthar, S. S., Cicchetti, D., and Becker, B. (2000). The construct of resilience: A critical evaluation and guidelines for future work. Child Dev. 71, 543–562. doi: 10.1111/1467-8624.00164
Mache, S., Vitzthum, K., Klapp, B. F., and Groneberg, D. A. (2015). Evaluation of a multicomponent psychosocial skill training program for junior physicians in their first year at work. Fam. Med. 47, 693–698.
MacIntosh, B. R., Murias, J. M., Keir, D. A., and Weir, J. M. (2021). What is moderate to vigorous exercise intensity? Front. Physiol. 12:682233. doi: 10.3389/fphys.2021.682233
Magtibay, D. L., Chesak, S. S., Coughlin, K., and Sood, A. (2017). Decreasing stress and burnout in nurses: Efficacy of blended learning with stress management and resilience training program. J. Nurs. Adm. 47, 391–395. doi: 10.1097/NNA.0000000000000501
Marashi, M. Y., Nicholson, E., Ogrodnik, M., Fenesi, B., and Heisz, J. J. (2021). A mental health paradox: Mental health was both a motivator and barrier to physical activity during the COVID-19 pandemic. PLoS One 16:e0239244. doi: 10.1371/journal.pone.0239244
McCorry, L. K. (2007). Physiology of the autonomic nervous system. Am. J. Pharm. Educ. 71:78. doi: 10.5688/aj710478
McCraty, R., and Shaffer, F. (2015). Heart rate variability: New perspectives on physiological mechanisms, assessment of self-regulatory capacity, and health risk. Glob. Adv. Health Med. 4, 46–61. doi: 10.7453/gahmj.2014.073
McLaughlin, K. A., Conron, K. J., Koenen, K. C., and Gilman, S. E. (2010). Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: A test of the stress sensitization hypothesis in a population-based sample of adults. Psychol. Med. 40, 1647–1658. doi: 10.1017/S0033291709992121
Mestre, J. M., Núñez-Lozano, J. M., Gómez-Molinero, R., Zayas, A., and Guil, R. (2017). Emotion regulation ability and resilience in a sample of adolescents from a suburban area. Front. Psychol. 8:1980. doi: 10.3389/fpsyg.2017.01980
Mulcahy, J. S., Larsson, D. E., Garfinkel, S. N., and Critchley, H. D. (2019). Heart rate variability as a biomarker in health and affective disorders: A perspective on neuroimaging studies. Neuroimage 202:116072. doi: 10.1016/j.neuroimage.2019.116072
Munoz, M. L., van Roon, A., Riese, H., Thio, C., Oostenbroek, E., Westrik, I., et al. (2015). Validity of (Ultra-)Short recordings for heart rate variability measurements. PLoS One 10:e0138921. doi: 10.1371/journal.pone.0138921
Nanchen, D. (2018). Resting heart rate: What is normal? Heart 104, 1077–1085. doi: 10.1136/heartjnl-2017-312731
Paolucci, E. M., Loukov, D., Bowdish, D. M. E., and Heisz, J. J. (2018). Exercise reduces depression and inflammation but intensity matters. Biol. Psychol. 133, 79–84. doi: 10.1016/j.biopsycho.2018.01.015
Papasavvas, T., Bonow, R. O., Alhashemi, M., and Micklewright, D. (2016). Depression symptom severity and cardiorespiratory fitness in healthy and depressed adults: A systematic review and meta-analysis. Sports Med. 46, 219–230. doi: 10.1007/s40279-015-0409-5
Pittig, A., Arch, J. J., Lam, C. W. R., and Craske, M. G. (2013). Heart rate and heart rate variability in panic, social anxiety, obsessive-compulsive, and generalized anxiety disorders at baseline and in response to relaxation and hyperventilation. Int. J. Psychophysiol. 87, 19–27. doi: 10.1016/j.ijpsycho.2012.10.012
Plews, D. J., Scott, B., Altini, M., Wood, M., Kilding, A. E., and Laursen, P. B. (2017). Comparison of heart-rate-variability recording with smartphone photoplethysmography, Polar H7 Chest Strap, and Electrocardiography. Int. J. Sports Physiol. Perform. 12, 1324–1328. doi: 10.1123/ijspp.2016-0668
Rocha-Singh, I. A. (1994). Perceived stress among graduate students: Development and validation of the graduate stress inventory. Educ. Psychol. Meas. 54, 714–727. doi: 10.1177/0013164494054003018
Rogowska, A. M., Pavlova, I., Kuśnierz, C., Ochnik, D., Bodnar, I., and Petrytsa, P. (2020). Does physical activity matter for the mental health of university students during the COVID-19 pandemic? J. Clin. Med. 9:3494. doi: 10.3390/jcm9113494
Ross, R., Chaput, J.-P., Giangregorio, L. M., Janssen, I., Saunders, T. J., Kho, M. E., et al. (2020). Canadian 24-Hour Movement Guidelines for Adults aged 18–64 years and Adults aged 65 years or older: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 45, S57–S102. doi: 10.1139/apnm-2020-0467
Sandercock, G. R. H., Bromley, P. D., and Brodie, D. A. (2005). Effects of exercise on heart rate variability: Inferences from meta-analysis. Med. Sci. Sports Exerc. 37, 433–439. doi: 10.1249/01.MSS.0000155388.39002.9D
Shaffer, F., and Ginsberg, J. P. (2017). An overview of heart rate variability metrics and norms. Front. Public Health 5:258. doi: 10.3389/fpubh.2017.00258
Silverman, M. N., and Deuster, P. A. (2014). Biological mechanisms underlying the role of physical fitness in health and resilience. Interface Focus. 4:20140040. doi: 10.1098/rsfs.2014.0040
Souza, G. G. L., Mendonça-de-Souza, A. C. F., Barros, E. M., Coutinho, E. F. S., Olivera, L., Mendlowicz, M. V., et al. (2007). Resilience and vagal tone predict cardiac recovery from acute social stress. Stress 10, 368–371. doi: 10.1080/10253890701419886
Spitzer, R. L., Kroenke, K., Williams, J. B. W., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder. Arch. Intern. Med. 166, 1092–1097. doi: 10.1001/archinte.166.10.1092
Statistics Canada (2019). Table 37-10-0031-01 Postsecondary graduates, by location of residence at interview and level of study. Ottawa, ON: Statistics Canada.
Suart, C., Nowlan Suart, T., Graham, K., and Truant, R. (2021). When the labs closed: Graduate students’ and postdoctoral fellows’ experiences of disrupted research during the COVID-19 pandemic. FACETS 6, 966–997. doi: 10.1139/facets-2020-0077
Tabor, A., Vollaard, N., Keogh, E., and Eccleston, C. (2019). Predicting the consequences of physical activity: An investigation into the relationship between anxiety sensitivity, interoceptive accuracy and action. PLoS One 14:e44706. doi: 10.1371/journal.pone.0210853
Thayer, J. F., and Lane, R. D. (2000). A model of neurovisceral integration in emotion regulation and dysregulation. J. Affect. Disord. 61, 201–216. doi: 10.1016/S0165-0327(00)00338-4
Thayer, J. F., Hansen, A. L., Saus-Rose, E., and Johnsen, B. H. (2009). Heart rate variability, prefrontal neural function, and cognitive performance: the neurovisceral integration perspective on self-regulation, adaptation, and health. Ann. Behav. Med. 37, 141–153. doi: 10.1007/s12160-009-9101-z
Varma, P., Junge, M., Meaklim, H., and Jackson, M. L. (2021). Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog. Neuropsychopharmacol. Biol. Psychiatry 109:110236. doi: 10.1016/j.pnpbp.2020.110236
von Haaren, B., Ottenbacher, J., Muenz, J., Neumann, R., Boes, K., and Ebner-Priemer, U. (2016). Does a 20-week aerobic exercise training programme increase our capabilities to buffer real-life stressors? A randomized, controlled trial using ambulatory assessment. Eur. J. Appl. Physiol. 116, 383–394. doi: 10.1007/s00421-015-3284-8
Wagnild, G. (2009). A review of the resilience scale. J. Nurs. Meas. 17, 105–113. doi: 10.1891/1061-3749.17.2.105
Wagnild, G. (2016). The resilience scale user’s guide for the US english version of the Resilience Scale and the 14-Item Resilience Scale (RS-14). Worden, MT: The Resilience Centre.
Wanner, M., Probst-Hensch, N., Kriemler, S., Meier, F., Autenrieth, C., and Martin, B. W. (2016). Validation of the long international physical activity questionnaire: Influence of age and language region. Prev. Med. Rep. 3, 250–256. doi: 10.1016/j.pmedr.2016.03.003
Williams, N., Ewell, T. R., Abbotts, K., Harms, K. J., Woelfel, K. A., Dooley, G. P., et al. (2021). Comparison of five oral cannabidiol preparations in adult humans: Pharmacokinetics, body composition, and heart rate variability. Pharmaceuticals 14:35. doi: 10.3390/ph14010035
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., et al. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 277, 55–64. doi: 10.1016/j.jad.2020.08.001
Young, H. A., and Benton, D. (2018). Heart-rate variability: A biomarker to study the influence of nutrition on physiological and psychological health? Behav. Pharmacol. 29, 140–151. doi: 10.1097/FBP.0000000000000383
Keywords: mental health, COVID-19, graduate student, physical activity, resiliency, heart rate variability (HRV)
Citation: Marashi M and Heisz JJ (2022) Predictors of psychological and physiological measures of graduate student health during COVID-19. Front. Educ. 7:941871. doi: 10.3389/feduc.2022.941871
Received: 17 June 2022; Accepted: 08 August 2022;
Published: 29 August 2022.
Edited by:
Roberto Burro, University of Verona, ItalyReviewed by:
Estíbaliz Royuela Colomer, University of Deusto, SpainIsabel Mercader Rubio, University of Almería, Spain
Emily Hotez, UCLA Health System, United States
Copyright © 2022 Marashi and Heisz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maryam Marashi, bWFyeWFtLm1hcmFzaGlAbWFpbC51dG9yb250by5jYQ==
 Maryam Marashi
Maryam Marashi Jennifer J. Heisz
Jennifer J. Heisz