- 1Department of Intensive Care Unit, Haikou Orthopedic and Diabetes Hospital, Haikou, Hainan, China
- 2Department of International College of Nursing, Hainan Vocational University of Science and Technology, Haikou, China
- 3Haikou City People's Hospital, Xiangya School of Medicine, Central South University, Haikou, China
- 4Hainan Women and Children's Medical Center, Haikou, China
- 5Kunming Municipal Hospital of Traditional Chinese Medicine, The Third Affiliated Hospital of Yunnan University of Chinese Medicine, Yunnan, China
- 6Department of Nursing, Shanghai Health and Medical Center, Wuxi, China
Objective: This study evaluated the efficacy of the Bridge-in, Objective, Pre-test, Participatory Learning, Post-test, Summary (BOPPPS) teaching model in improving the knowledge, skills, and attitudes of nursing students on end-of-life care.
Methods: The students enrolled in the fourth year of the 2021 nursing technology program were divided into control (n = 173) and experimental (n = 180) groups. The control group was taught using the traditional method for end-of-life care, and the experimental group was instructed using the BOPPPS method. Standard validated questionnaires, namely Frommelt Attitude Toward Care of the Dying Scale Form B (FATCOD-B) and Templer’s Death Anxiety Scale (T-DAS), were used to measure the attitudes of the students and their emotional responses to end-of-life care following the course. Test–retest was used to assess the reliability of the questionnaires. The academic performance of the students was determined using written and skill-based assessments. Semi-structured interviews were conducted with 12 experimental group participants to obtain qualitative feedback on the BOPPPS instruction. The interviews were audio-recorded, transcribed, and analyzed thematically.
Results: Both the FATCOD-B (Cronbach’s α = 0.891) and T-DAS (Cronbach’s α = 0.943) had a high internal consistency. Compared to the control group, the experimental group showed significantly higher FATCOD-B scores (89.21 ± 4.96 vs. 87.82 ± 5.29, p < 0.01), T-DAS scores (32.66 ± 9.23 vs. 30.04 ± 9.05, p < 0.01), and total academic scores (90.36 ± 14.45 vs. 81.97 ± 19.77, p < 0.001). The thematic analysis revealed three key benefits of the BOPPPS instruction method: enhanced pre-class engagement, reduced apprehension in terminal care, and improved critical thinking with knowledge internalization.
Conclusion: The BOPPPS instructional framework effectively optimizes hospice care education by simultaneously developing nursing students’ knowledge acquisition, clinical skills, and professional attitudes, thereby better preparing them for end-of-life care challenges.
1 Introduction
During the past few years, China has witnessed a critical demographic shift, with the population aged 60 years and above projected to exceed 30% of the total population by year 2035. Because of an increase in the aging population, a large number of people are expected to die from chronic illnesses and require end-of-life care. End-of-life care, centered on patients and their families, plays a pivotal role in assisting individuals through their final life stages (Brassil et al., 2021; Ling et al., 2020). Therefore, there is a crucial need to provide training to professional caregivers to enable them to effectively address the physical and psychosocial challenges experienced by patients during the final stages of the disease (Chen L. et al., 2022; Minjeong et al., 2023).
End-of-life care, a specialized component of the basic nursing curricula, aims to address the professional aspects of care for dying patients (Dalcali and Akay 2022). The curriculum is designed to equip students with the knowledge of the clinical factors leading to death and the nursing interventions required to assist dying patients. This training also enables students to change their attitudes and behaviors toward death and prepares them to confront the emotional challenges associated with caring for dying patients objectively and rationally (Fatma et al., 2023).
Currently, the majority of higher vocational nursing students in China are aged 16–19 years. Because the students are very young, they tend to have a limited understanding and experience of end-of-life care. Moreover, their knowledge regarding the needs of patients at the end-of-life stage is limited by their educational background and traditional viewpoints. The higher vocational education nursing curricula also tend to focus predominantly on practical nursing skills while neglecting humane care as a critical aspect, resulting in the marginalization of end-of-life care education (Lv et al., 2023; Ma et al., 2021a; Zhu and Shi, 2011). Consequently, there is a crucial need to develop training interventions designed to improve the necessary skills and knowledge of nursing students to address the medical and psychosocial needs of terminally ill patients (La Sala Rachele et al., 2023; Tang et al., 2015).
The Bridge-In, Outcomes, Pre-assessment, Participatory Learning, Post-assessment, and Summary (BOPPPS) is an instructional planning framework designed to facilitate the development of professional knowledge, human care skills, and critical thinking skills (Murnane et al., 2023; Cao et al., 2022). This model aims to enhance the efficiency and quality of students’ learning through clear learning objectives, pre-testing of knowledge, participatory learning activities, timely feedback on learning outcomes, and summarization of learning content (Shen et al., 2024). Both active learning and a highly interactive classroom atmosphere facilitated by the BOPPPS model have shown positive effects on students’ interest in learning in various educational medical programs (Wang et al., 2024).
Although the BOPPPS teaching model has already been implemented in nursing disciplines such as internal medicine, surgery, and emergency medicine (Li Z. et al., 2023; Li P. et al., 2023; Wang et al., 2023; Xu and Ji, 2023), to our knowledge, no studies have reported the application of the BOPPPS teaching method to equip nursing students with the knowledge, skills, and attitudes required to care for dying patients. Therefore, in the present study, we aimed to compare the efficacy of the BOPPPS teaching model and traditional lecture-based teaching methods in improving the knowledge, skills, and attitudes of higher vocational nursing students on end-of-life care. The research questions for this study are as follows:
1. How effective is the BOPPPS teaching model compared to traditional instructional methods in hospice care education?
2. Can the structured pedagogical process based on pre-class preparation, in-class participation, and post-class summarization enhance students’ engagement?
2 Materials and methods
2.1 Setting
This study was conducted at the College of Health and Wellness Professions in Hainan Province, China. Five nursing programs were evaluated. The Life Support Nursing Techniques is a mandatory course for nursing students. The basic nursing technology study unit in the first, second, and third years of the course aims to prepare students for their internships in the fifth year of the program. As part of this study unit, the students are required to learn about end-of-life care. Approximately 353 students are enrolled in this course each year. The purpose of this course is to enable students to understand and care for the physical, psychological, social, and spiritual needs of terminally ill patients.
2.2 Establishment of the teaching team
The course was delivered between June 5 and June 17, 2023, and supervised by a designated coordinator who assembled the teaching team. This teaching team comprised six academic educators and six clinical instructors (2 for each of the 6 classes). All academic educators were full-time faculty members with extensive experience in end-of-life care education, underpinned by a robust foundation in the theoretical aspects of end-of-life care.
The instructors of the experimental group included senior head nurses, associate chief nurses, and nursing supervisors. Each of the three classes of the experimental group had two clinical instructors. The clinical instructors had more than a decade of clinical frontline experience in end-of-life care. The clinical lecturers were fully trained in the theoretical and practical aspects of the BOPPPS model.
The control group instructors were professional college lecturers with extensive experience in palliative care training. Each of the three classes of the control group had 2 college lecturers, totaling 6 college lecturers.
2.3 Eligibility criteria
This study utilized a quasi-experimental research design. The study population included all 353 nursing students from the six nursing classes of the 2021 cohort of the five-year integrated nursing technology program who had enrolled in the mandatory “Hospice Care” module and voluntarily provided written informed consent to participate in this study. Students who did not complete the full hospice care curriculum for health or other personal reasons and those who performed clinical internships or had extensive clinical experience within a hospice care setting were excluded. Students in classes 1, 2, and 3 (n = 180) were enrolled in the experimental group and were trained using the BOPPPS teaching method. On the other hand, students in classes 4, 5, and 6 (n = 173) were enrolled in the control group and were trained using traditional teaching methods.
2.4 Teaching methods
The same textbooks, curriculum schedule, and post-teaching assessments were used for both the experimental and control groups. Each group received 12 theoretical live teaching sessions. The duration of each lecture was 45 min. The instructors organized the teaching sessions to ensure that the aims and objectives of the curriculum were met. The teaching sessions of both groups were based on the criteria of the People’s Health Publishing House APP essential knowledge on end-of-life care, which includes the psychological state of terminally ill patients, nursing needs, end-of-life stages, and ethical and legal issues. The theoretical assessment of this study unit consisted of multiple-choice questions, terminology explanations, fill-in-the-blank questions, and short-answer questions. Both groups were provided with the same pre- and post-class teaching materials. However, the method used to deliver the content varied between the experimental and control groups as shown in Table 1.
2.4.1 Pre- and post-class sessions
Seven days before the delivery of the class session, the instructors uploaded an array of educational materials to the Chaoxing Learning Platform. The pre-class material consisted of a comprehensive package of resources, including PowerPoint presentations, case studies, instructional videos, pertinent theoretical information, updates on recent professional developments, and clinical procedural videos. The students were asked to independently review the uploaded material on the online learning platform as part of their preparatory study. Subsequently, students’ understanding of the subject was assessed using the online theoretical assessment developed by the People’s health Publishing House APP. The instructors analyzed the assessment results to identify the topics where misunderstandings were common. During the lectures, the difficult topics were focused more to enhance their understanding. After the lectures, the instructors provided further practical learning materials to students through WeChat groups. This approach was designed to encourage students facing difficulties with task completion to engage in collaborative group discussions and thus foster a culture of collective problem-solving. In cases where issues remained unresolved through group efforts, the instructors intervened by providing strategic approaches to problem-solving rather than direct answers. This teaching method was used for both students in the control and experimental groups.
2.4.2 Control group teaching methods
Control group students were trained using traditional lecture-based methods, and their curriculum was aligned with established educational reform policies. Both groups used the same textbooks, curriculum schedule, and post-class assessments.
2.4.3 Experimental group teaching methods
The students were divided into five groups according to their seating arrangements in class and were asked to select a group leader to facilitate collaborative activities. The teaching strategy was structured into six phases, as indicated by the BOPPPS teaching model:
Phase 1–Bridge-in (B): During the Bridge-in phase, the students were introduced to the theoretical concepts of end-of-life care and their importance through videos and questions. Throughout this part of the course program, the students were required to understand the psychological stages of terminally ill patients and their characteristics as well as the corresponding nursing requirements.
Phase 2–Objectives (O): The goals and requirements were clearly outlined: students were expected to understand the basic principles of end-of-life care, the nursing care requirements of terminally ill patients, and the physiological and psychological changes experienced by these patients. Additionally, they needed to learn about the stages of death and the specifics of caring for the bereaved. The aim was to enhance students’ technical skills in end-of-life care, improve their communication abilities, and develop teamwork.
Phase 3–Pre-test: The goals of this phase are divided into knowledge, attitude, and skills. Regarding knowledge, students should understand the clinical factors leading to the end-of-life stage and the required nursing intervention measures. Moreover, they should develop a more compassionate and empathetic attitude towards terminally ill patients, with improved communication and teamwork skills.
Phase 4–Participatory Learning: Theoretical knowledge was imparted through interactive teaching methods, such as case studies, classroom demonstrations, and sharing of personal experiences, to capture students’ interest.
Phase 5–Post-test: Assessment was conducted using practice questions from the People’s Health Publishing House APP.
Phase 6–Summary: This final phase involved a review of the key knowledge points, including the psychological state staging of terminally ill patients and their care, the correct implementation of postmortem care, and the provision of high-quality, compassionate service to terminally ill patients and their families.
The BOPPPS implementation process diagram is shown in Figure 1.
2.5 Evaluation indicators
2.5.1 Assessment of students’ attitudes toward end-of-life care
The Frommelt Attitude Toward Care of the Dying Scale Form B (FATCOD-B), originally developed by Frommelt (1991), was culturally adapted for the Chinese context by Yang et al. (2016). This scale comprises 30 items divided into two dimensions: “Positive Attitude” with 17 items and “Nursing Perception” with 13 items. Each item on the FATCOD-B scale is rated using a 5-point Likert scale, ranging from “Strongly Disagree” (1 point) to “Strongly Agree” (5 points). Representative items are as follows:
“I consider caring for terminally ill patients to be a crucial component of nursing practice” (Scale: 1 = Strongly disagree, 5 = Strongly agree).
“I am willing to discuss death-related topics with terminally ill patients and their families” (Scale: 1 = Strongly disagree, 5 = Strongly agree). The total score on the questionnaire can vary from 30 to 150 points. According to Yang et al. (2016), a total score of 100 or higher indicates a more positive and empathetic attitude toward end-of-life care. A study by Jingyi et al. (2025) showed that this scale has good internal consistency for this tool with a Cronbach’s α coefficient of 0.805. In our study, we tested the reliability of the questionnaire developed by Song (2021), and the Cronbach’s α coefficient was 0.891.
2.5.2 Anxiety and emotional preparedness assessment
The Templer’s Death Anxiety Scale (T-DAS) was developed based on the “Research Questionnaire on the Offering of Death Education Courses in Taiwanese Universities” compiled by Tianzhong in Taiwan, China, and later revised by Tang et al. (2015). The T-DAS version used in our study comprised 15 items aimed at assessing students’ comfort levels with death discussion, death anxiety, and emotional preparedness. Each item is rated on a 5-point Likert scale as follows: “Strongly Agree” (5 points), “Agree” (4 points), “No Opinion” (3 points), “Disagree” (2 points), and “Strongly Disagree” (1 point). The T-DAS score ranges from 15 to 75 points; higher scores on the scale indicate a more positive attitude toward end-of-life care. Following cross-cultural adaptation and validation in the Chinese context, the instrument has demonstrated satisfactory psychometric properties (Cronbach’s α = 0.840) (Zhu and Shi, 2011). In our study, two repeated questionnaire surveys were conducted on a group of students. The scale achieved a Cronbach’s α coefficient of 0.943, thus demonstrating even higher reliability.
2.5.3 Academic performance
Academic performance assessment was divided into three parts: written examination (25%), practical skill test (50%), and classroom participation (25%). The written assessment consisted of a 1-h examination comprising multiple-choice questions; true/false questions; fill-in-the-blank questions; terminology explanations; and case studies designed to assess students’ knowledge of various essential end-of-life topics, including special care and emergency measures. The practical skill test included 4 simulated case scenarios to examine students’ ability to apply their knowledge and skills related to pain management, effective communication, and patient care to actual situations. The classroom participation scores evaluated students’ performance in class and their enthusiasm for participating in group discussions.
2.5.4 Qualitative assessment through semi-structured interviews
Following the completion of the course, 12 students in the experimental group were invited to participate in a 20-min semi-structured interview to evaluate their perceptions of the application of the BOPPPS teaching model in end-of-life care education. A purposive sampling strategy was used to include students from different genders, age groups, and academic performances (highest and lowest) within each class, which ensured a diverse and representative sample. The interview process was continued until thematic saturation was achieved, indicated by the emergence of no new themes or information.
The interviews were conducted in a quiet, isolated classroom by the researcher to minimize disruption. All interviews were recorded and transcribed within 24 h after the completion of the interview for easy tracking and verification. During the interview, the students were reassured that they could answer freely as their responses would not affect their final score. They were also informed that the interviews would be coded to avoid disclosure of personal identifying information. Before the interview, the students were informed about the purpose and had freedom to decline their participation in the interview. A consent form was signed by the students who accepted to be interviewed.
First, a pilot study with 2 students was performed to assess the interview questions. The interview questions were then refined based on the responses of these students. The final interview framework contained three questions. The students were first asked to share their individual experiences and reflections on applying the BOPPPS model as part of their end-of-life care education. Subsequently, the students were encouraged to discuss the differences and improvements between the BOPPPS model and other learning methods they had previously encountered. Finally, the students were asked to explain their perceived level of understanding of end-of-life care acquired by the end of the course. The interviews were stopped when data saturation was reached and all the data for each class were obtained. All interviews were recorded and transcribed within 24 h after the end of the interview to facilitate tracking and verification.
The research method was implemented by referring to the method reported by Liamputtong et al., (2009) (Qualitative Research Methods: A Data Collector’s Field Guide). In the present study, the number of individuals participating in the qualitative analysis was 12 students from the experimental group.
2.6 Ethical considerations
The ethics committee of our institution approved this study (approval number: SC20240029). The students in the control group had their training before the experimental group and received the same training provided to previous students. The students enrolled in the experimental group were informed about the purpose of the study and the potential benefits of the BOPPPS model at the beginning of the course, and all of them agreed to participate in this study. We acknowledge that the control group students had a disadvantage compared to the experimental group students; however, the former group was informed that they could ask for additional support whenever required.
2.7 Data analysis
Statistical Package for Social Sciences Software (SPSS) version 26.0 was used to analyze the quantitative data. A power calculation was performed to determine the appropriate sample size, which ensured that the study had sufficient power to detect a statistically significant effect while minimizing errors. Categorical data were expressed as frequencies and percentages (%), and continuous data were expressed as mean ± standard deviation (χ ± s). The chi-square (χ2) test was used to compare the categorical variables between the two teaching groups. Continuous data with normal distribution were compared with t-tests. For all statistical tests, a p-value of <0.05 was considered statistically significant.
The qualitative data obtained from semi-structured interviews were analyzed through thematic analysis. This process involves six stages: data familiarization, data coding, theme generation, theme review, theme definition and naming, and detailed reporting.
3 Results
3.1 Demographic characteristics of the students
A total of 353 nursing students were enrolled in the study. Their demographic and educational characteristics are summarized in Figure 1. The experimental and control groups showed no significant difference in demographics and educational background.
The evaluated demographic variables, including age, gender, ethnicity, religion, only-child status, place of origin, and previous end-of-life care experience, aimed to provide a comprehensive understanding of the study population and explore potential factors that may affect the research results. These variables are relevant to end-of-life care education because they may influence students’ attitudes, beliefs, and experiences regarding end-of-life care (Table 2).
The results indicate that students’ age and previous experience did not affect their acceptance and understanding of the importance of end-of-life care. Additionally, no significant differences were noted in the cultural backgrounds and religious beliefs of students.
3.2 FATCOD-B questionnaire scores after training
The experimental and control groups showed no significant differences in positive attitude scores. However, after course completion, the experimental group had a significantly higher nursing perception score, which eventually resulted in a higher total FATCOD-B score (Table 3).
The results of this study showed that the BOPPPS teaching model positively affected students’ care perception. “Care perception” refers to students’ perception and understanding of the care for terminally ill patients. It reflects the awareness of students regarding care needs, care methods, and care responsibilities.
3.3 Death education classroom feedback questionnaire score after training
The experimental group showed significantly higher Death Education Classroom Feedback Questionnaire score than the control group (Table 4).

Table 4. Comparative analysis of FATCOD-B questionnaire scores between the experimental and control groups.
3.4 Written examination scores
Compared to the control group, the experimental group exhibited significantly higher objective and subjective examination scores, class participation, and total overall scores (Table 5).

Table 5. Comparative analysis of the Death Education Classroom Feedback Questionnaire scores between the experimental and control groups.
The experimental group students scored higher in the written and practical tests than the control group students and had higher classroom participation scores.
3.5 Interview outcomes
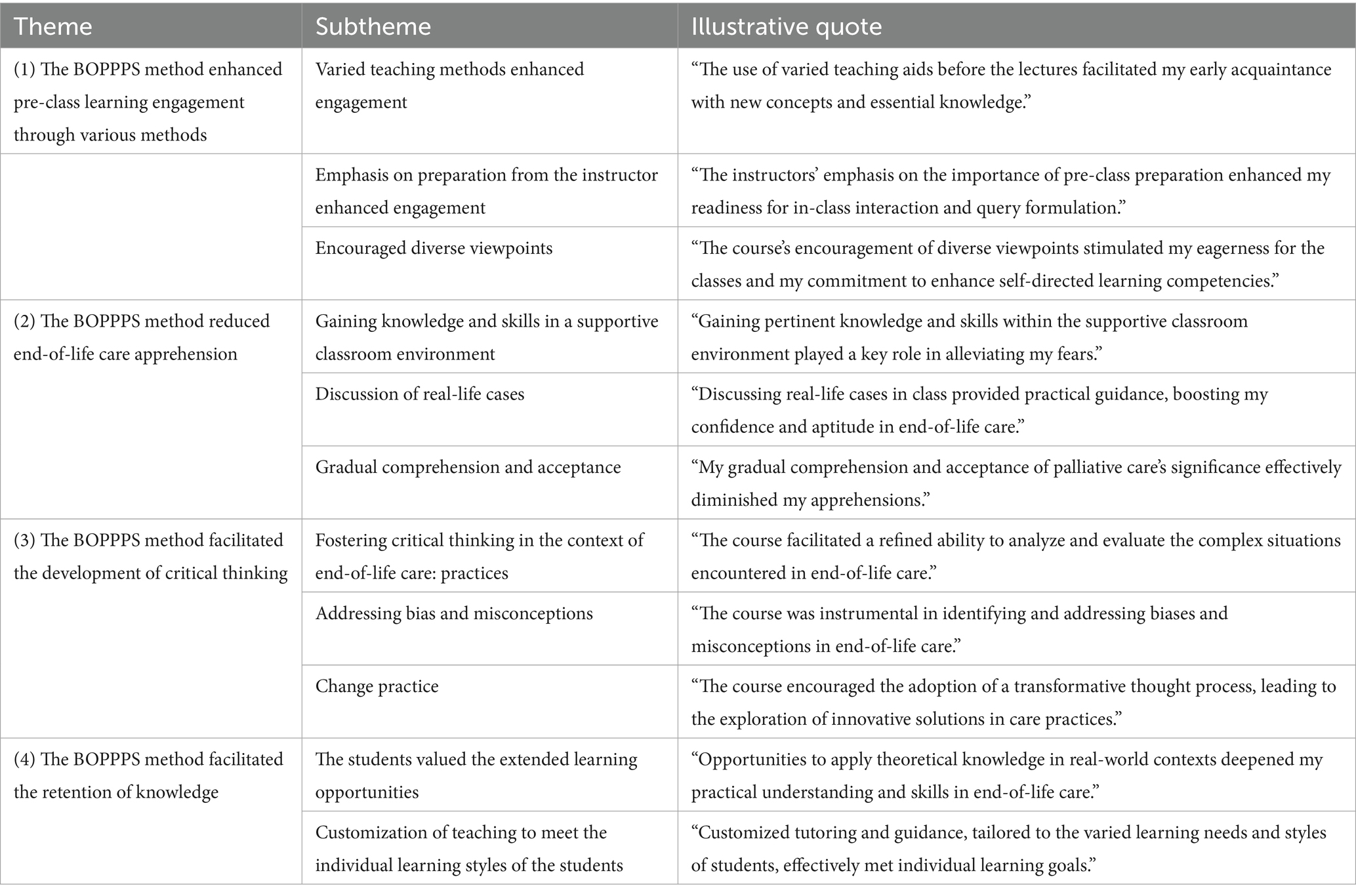
The thematic analysis of the semi-structured interviews conducted with the nursing students yielded four main themes; (1) increased pre-class learning engagement, (2) reduced end-of-life care apprehension, (3) development of critical thinking skills, and (4) retention of knowledge. The themes and subthemes together with illustrative quotes are summarized in Tables 6, 7.

Table 6. Comparative analysis of course examination scores between the experimental and control groups ( ± s).
4 Discussion
End-of-life care involves addressing the physical, psychological, and social needs of patients during their final days of life. Deming et al. showed that traditional classroom settings often result in suboptimal knowledge acquisition on end-of-life care, with students mastering less than 70% of the material. Given the unique nature of end-of-life care, this topic necessitates distinct pedagogical approaches that encourage student engagement, self-directed learning, and knowledge retention (Escribano et al., 2021; Yu et al., 2022).
In the present study, we evaluated the efficacy of the BOPPPS teaching method and traditional teaching methods in improving the attitudes, knowledge, and skills of higher vocational nursing students on end-of-life care. In our study, the students taught using traditional teaching methods had lower average attitude scores (75.74 ± 14.53) than the scores reported by Guo and Guo (2021) (99.05 ± 5.72) for third-year full-time undergraduate nursing students and Dong and Li (2020) (106.22 ± 9.39) for practicing nurses. However, the experimental group taught using the BOPPPS teaching model exhibited a significantly higher mean positive attitude score (31.12 ± 6.66) than the control group. During the pivotal transition from adolescence to adulthood, the five-year higher vocational nursing course should aim to foster a positive attitude toward end-of-life care (Nancy et al., 2022). This period significantly influences the perspectives and attitudes of young students, highlighting the need for an educational approach that is both scientifically sound and effective (Lv et al., 2023). The BOPPPS teaching model plays a vital role in this regard, as it is designed to enable the students to develop an interest in end-of-life care and enhance their knowledge and attitude toward the subject (Ma et al., 2022). This model has remarkable efficacy, given that students’ perceptions of end-of-life care are shaped by various factors, including personal beliefs and backgrounds. Despite these promising results, students’ knowledge of the end-of-life care did not vary significantly between the experimental and control groups. This may be attributed to the inherent challenges and complexities faced in end-of-life care, which are not immediately resolved through theoretical learning. End-of-life care requires extensive professional knowledge, emotional resilience, and skillful patient care, demanding a more prolonged and experiential approach to education. These findings suggest a need for a broader implementation of the BOPPPS teaching model in nursing education. However, theoretical knowledge must be further reinforced with practical training, individualized emotional support, and refined teaching strategies (Chen L. et al., 2022; Chen X. et al., 2022; Hao et al., 2021).
The BOPPPS model has improved student-teacher interaction, collaboration, and teamwork by promoting group discussions, cooperative learning, and interactive activities among students. The collaborative ability is reflected in students’ active speaking in group discussions and close cooperation with group members to resolve complex cases. The students could present their own viewpoints and ideas, reflecting the enhancement of student-teacher interaction; in practical activities, students can jointly complete care tasks, reflecting the spirit of teamwork. The BOPPPS teaching model has played a positive role in promoting interaction, collaboration, and teamwork among students and between students and teachers.
The adoption of the BOPPPS teaching model in our end-of-life care course significantly enhanced student-teacher interaction, student collaboration, and ultimately teamwork (Osakwe et al., 2023b). As a result, compared to traditional teaching methods, the BOPPPS teaching method significantly improved objective and subjective testing scores, classroom participation scores, and overall scores of nursing students. Our findings were consistent with the study of Zhang et al. (2022), who also reported an improvement in the knowledge of surgical nursing care in higher vocational nursing students when instructed using the BOPPPS model. The BOPPPS model is instrumental in cultivating a comprehensive understanding of nursing-specific knowledge while also developing preparatory learning and critical thinking skills (Ma et al., 2022). The active learning environment provided by the model engages students’ attention, enhancing their initiative and strengthening their communication and cooperation abilities. Acquiring nursing knowledge through this model leads to an enriched understanding of attitudes toward end-of-life care (Graham and Emerson, 2024). This teaching strategy nurtures a deeper need for proficiency in nursing practices, personal growth, and emotional experiences. Additionally, the model encourages students to proactively learn through flexible and customizable learning activities that can be performed before and after classes. This approach aligns with current educational paradigms as it emphasizes skill development, technical proficiency, and innovation, in addition to knowledge acquisition. Consequently, the BOPPPS model is increasingly being used in nursing education because of its inherent flexibility and interactive nature (Hu et al., 2022; Liu et al., 2022; Ma et al., 2021b).
The BOPPPS model primarily emphasizes on preparatory learning, which equips students for more engaged and informed participation during classes (Li Z. et al., 2023; Li P. et al., 2023). This approach not only increases student involvement but also nurtures independent learning skills. By meticulously reviewing materials and formulating relevant questions before class, students can engage more in active and meaningful classroom discussions, thus facilitating a deeper understanding of new knowledge and foundational concepts (Shouqin et al., 2022; Wang et al., 2022). A notable benefit of the BOPPPS model, as reported by students, is its effectiveness in reducing anxiety surrounding end-of-life care (Osakwe et al., 2023a). The incorporation of a supportive classroom atmosphere and discussions of real-life cases enabled our students to better comprehend and embrace the complexities of end-of-life care, thus allowing them to be better informed and emotionally prepared to face the demands of terminally ill patients. The BOPPPS model also actively fosters critical thinking among nursing students. It encourages them to analytically assess various situations within the scope of end-of-life care, thereby promoting the identification and rectification of biases and misconceptions. Our study further corroborates the findings of previous studies (Yoong et al., 2023; Wang et al., 2022) regarding the effect of a positive classroom atmosphere on self-assessed learning outcomes. The cultivation of critical thinking skills, integral to this process, not only augments the professional competencies of nursing students but also invigorates their innovative thinking, fostering the development of novel solutions to complex problems. This study also suggests that practical applications in real-life scenarios could substantially enhance the comprehension and practical proficiency of students in end-of-life care techniques (Zahran et al., 2022). Furthermore, providing personalized guidance and instructional support, tailored to meet the diverse needs and learning styles of nursing students, appears to be a pivotal factor in enhancing their overall satisfaction with the classroom experience. Thus, the implementation of the BOPPPS teaching model in end-of-life care education for nursing students within the five-year higher vocational programs has shown considerable promise in elevating their classroom satisfaction levels. By instilling a proactive attitude toward preparatory learning, mitigating apprehensions related to end-of-life care, nurturing critical thinking, and offering customized educational support, the BOPPPS model has been instrumental in stimulating students’ engagement and participation. This approach not only strengthens their professional skill set but also improves their confidence. Additionally, personalized guidance after class ensures sustained learning and effective application of the knowledge in practical settings.
This study has several limitations that should be acknowledged. First, because the course developers performed the interview, the student may have felt hesitant to provide honest responses about their experiences. Moreover, the assessors were not blinded to group allocation, resulting in a risk of assessment bias, which might affect the study’s objectivity and reliability. To address this issue, future studies should implement a blinding approach, ensuring that assessors are unaware of group assignments. This would help maintain impartial evaluations and enhance the validity of the results. Second, the sample size was restricted to students from a single institution attending the five-year higher vocational nursing program, which may limit the generalizability of the findings. Additionally, the limited duration of the study precluded an extensive assessment of the long-term effectiveness of the BOPPPS teaching model. Therefore, multicenter studies are recommended to enhance the generalizability of the teaching model in enhancing the clinical skills of students from diverse backgrounds. Third, the study did not evaluate the impact of counseling on enabling the students to manage their emotions and enhance their learning experience. Future research should focus on the development of counseling strategies that could be used to optimize emotional support.
This new teaching model is expected to have significant implications in improving clinical practice by better preparing students to deliver holistic care to terminally ill patients. Families also benefit from improved communication and support, fostering trust and satisfaction with the care provided. Additionally, the model helps nurses develop stronger coping mechanisms, reducing emotional burnout and stress, ultimately contributing to a more resilient and sustainable hospice nursing workforce. Future studies should integrate the BOPPPS model with clinical internships to enable students to apply classroom-acquired competencies to real-world patient care, thereby holistically developing their clinical acumen and emotional resilience. The use of real-life clinical assessment as opposed to simulated assessments may also provide valuable insights into the impact of the BOPPPS teaching method on clinical practice.
5 Conclusion
This study provides robust evidence supporting the effectiveness of the BOPPPS teaching model in end-of-life care education within the context of five-year higher vocational nursing programs. The application of the BOPPPS teaching model considerably enhances students’ understanding and practical application of end-of-life care techniques, resulting in improved academic performance. Furthermore, the model facilitates the development of essential skills, including preparatory self-directed learning and critical thinking, which are crucial for fostering lifelong learning capabilities.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Haikou People’s Hospital in Hainan Province, China (Ethics number: SC20240029). Written informed consent to participate in this study was obtained from all interviewed students. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
QZX: Data curation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing, Conceptualization, Formal analysis, Resources, Software, Visualization. JC: Conceptualization, Methodology, Writing – review & editing, Formal analysis, Resources, Validation, Visualization. QX: Writing – original draft, Data curation, Investigation, Methodology, Project administration, Supervision. JZ: Conceptualization, Data curation, Formal analysis, Methodology, Supervision, Validation, Writing – review & editing. YY: Conceptualization, Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Correction note
This article has been corrected with minor changes. These changes do not impact the scientific content of the article.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Brassil, M., Gallegos-Kearin, V., and Tolchin, D. W. (2021). Subspecialty training: hospice and palliative medicine [Journal Article]. Am. J. Phys. Med. Rehabil. 100, 189–192. doi: 10.1097/PHM.0000000000001489,
Cao, W., Li, C., Zhang, Q., and Tong, H. (2022). Perceptions on the current content and pedagogical approaches used in end-of-life care education among undergraduate nursing students: a qualitative, descriptive study. BMC Med Educ 22:553.
Chen, L., Tang, X. J., Chen, X. K., Ke, N., and Liu, Q. (2022). Effect of the BOPPPS model combined with case-based learning versus lecture-based learning on ophthalmology education for five-year paediatric undergraduates in Southwest China. BMC Med. Educ. 22:437. doi: 10.1186/s12909-022-03514-4,
Chen, X., Zhang, Y., Arber, A., Huo, X., Liu, J., Sun, C., et al. (2022). The training effects of a continuing education program on nurses' knowledge and attitudes to palliative care: a cross sectional study. BMC Palliat. Care 21:56. doi: 10.1186/s12904-022-00953-0,
Dalcali, B. K., and Akay, B. (2022). The Relationship Between the Attitudes of Nursing Students Towards Providing Care for a Dying Patient and Their Empathic Tendencies. Omega, 90, 225–236. doi: 10.1177/00302228221100900
Dong, Y., and Li, L. (2020). Relationship between hospital ethical climate and nurses' attitude toward care of the dying. J. Nurs. 35, 90–92. doi: 10.3870/j.issn.1001-4152.2020.18.090
Escribano, S., Cabañero-Martínez, M. J., Fernández-Alcántara, M., García-Sanjuán, S., Montoya-Juárez, R., Juliá-Sanchis, R., et al. (2021). Efficacy of a Standardised Patient Simulation Programme for Chronicity and End-of-Life Care Training in Undergraduate Nursing Students. Int J Environ Res Public Health. 18:11673. doi: 10.3390/ijerph182111673
Fatma, T., Rumeysa, D., and Esma, A. (2023). The relationship between the levels of thanatophobia and the attitudes towards the care of dying patients among student nurses. Omega-Int. J. Manag. Sci. doi: 10.1177/00302228231177393
Frommelt, K. H. (1991). The effects of death education on nurses' attitudes toward caring for terminally ill persons and their families. Am. J. Hospice Palliative Med. 8, 37–43. doi: 10.1177/104990919100800509,
Graham, L., and Emerson, K. (2024). An Innovative Academic-Practice Partnership Using Simulation to Provide End-of-Life Education for Undergraduate Nursing Students in Rural Settings. Nursing education perspectives 45, 126–128. doi: 10.1097/01.NEP.0000000000001073
Guo, Q. H., and Guo, K. S. (2021). Effects of aging experience combined with death highlights on nursing students' hospice care attitude and death anxiety. Nurs. Res. 35, 3377–3379. doi: 10.12102/j.issn.1009-6493.2021.18.037
Hao, Y., Zhan, L., Huang, M., Cui, X., Zhou, Y., and Xu, E. (2021). Nurses' knowledge and attitudes towards palliative care and death: a learning intervention. BMC Palliat. Care 20:50. doi: 10.1186/s12904-021-00738-x,
Hu, K., Ma, R. J., Ma, C., Zheng, Q. K., and Sun, Z. G. (2022). Comparison of the BOPPPS model and traditional instructional approaches in thoracic surgery education. BMC Med. Educ. 22:447. doi: 10.1186/s12909-022-03526-0,
Jingyi, L., Guanguan, L., Qunfang, M., Yueyan, Z., Xiaoning, W., Pingping, Q., et al. (2025). Latent profile analysis and influencing factors of self-coping capacity with death-related work among clinical nurses. J. Nurs. 32, 13–18. doi: 10.16460/j.issn1008-9969.2025.01.013
Liamputtong, P., and Ezzy, D. (2009). Qualitative research methods: A guide for health and related professionals: Chongqing University Press. Available at: https://book.kongfz.com/669317/7425863113
Li, Z., Cai, X., Zhou, K., Qin, J., Zhang, J., Yang, Q., et al. (2023). Effects of BOPPPS combined with TBL in surgical nursing for nursing undergraduates: a mixed-method study. BMC Nurs. 22:133. doi: 10.1186/s12912-023-01281-1,
Li, P., Lan, X., Ren, L., Xie, X., Xie, H., and Liu, S. (2023). Research and practice of the BOPPPS teaching model based on the OBE concept in clinical basic laboratory experiment teaching. BMC Med. Educ. 23:882. doi: 10.1186/s12909-023-04822-z,
Ling, M., Wang, X., Ma, Y., and Long, Y. (2020). A review of the current state of hospice care in China [Journal Article; Research Support, Non-U.S. Gov't; Review]. Curr. Oncol. Rep. 22:99. doi: 10.1007/s11912-020-00959-y,
Liu, X. Y., Lu, C., Zhu, H., Wang, X., Jia, S., Zhang, Y., et al. (2022). Assessment of the effectiveness of BOPPPS-based hybrid teaching model in physiology education. BMC Med. Educ. 22:217. doi: 10.1186/s12909-022-03269-y,
Lv, T., Li, L., Wang, H., Zhao, H., Chen, F., He, X., et al. (2023). Relationship between death coping and death cognition and meaning in life among nurses: a cross-sectional study. Omega J. Death and Dying 91:27526017. doi: 10.1177/00302228231158911,
Ma, X., Ma, X., Li, L., Luo, X., Zhang, H., and Liu, Y. (2021). Effect of blended learning with BOPPPS model on Chinese student outcomes and perceptions in an introduction course of health services management. Adv. Physiol. Educ. 45, 409–417. doi: 10.1152/advan.00180.2020,
Ma, X., Zeng, D., Wang, J., Xu, K., and Li, L. (2022). Effectiveness of bridge-in, objective, pre-assessment, participatory learning, post-assessment, and summary teaching strategy in Chinese medical education: a systematic review and meta-analysis Systematic Review. Front. Med. 9:975229. doi: 10.3389/fmed.2022.975229,
Minjeong, J., Mihyun, P., and Kyoungsun, Y. (2023). Effects of advance care planning training on advanced practice nurse students' knowledge, confidence, and perception of end-of-life care: a mixed-method study. Nurse Educ. Pract. 67:103555. doi: 10.1016/j.nepr.2023.103555
Murnane, S., Purcell, G., and Reidy, M. (2023). Death, dying and caring: exploring the student nurse experience of palliative and end-of-life education. Br J Nurs. 32, 526–531. doi: 10.12968/bjon.2023.32.11.526
Nancy, I., Bryan, P., and A, G. S. (2022). Undergraduate nursing students' responses to an end-of-life educational session. Gerontol. Geriatr. Educ. doi: 10.1080/02701960.2022.2089981
Osakwe, Z. T., Horton, J. R., Ottah, J., Eisner, J., Atairu, M., and Stefancic, A. (2023a). Academic–clinical collaborations to build undergraduate nursing education in hospice and palliative care. J. Gerontol. Nurs. 49, 13–18. doi: 10.3928/00989134-20230515-01,
Osakwe, Z. T., Jacobowitz, W., Horton, J. R., Klainberg, M., Calixte, R., Jacobs, C., et al. (2023b). Hospice and palliative care for undergraduate nursing education. Home Healthc. Now 41, 197–206. doi: 10.1097/NHH.0000000000001178,
Rachele, L. S., Serena, C., Rossana, C., Giuseppe, M., Michele, M., Debora, C., et al. (2023). Education nursing students' in palliative care and pain therapy: an observational study. Acta Bio-Medica 94:e2023038. doi: 10.23750/abm.v94i1.13912,
Shen, B., Chen, Y., Wu, Y., Lan, Y., He, X., Wang, N., et al. (2024). Development and effectiveness of a BOPPPS teaching model-based workshop for community pharmacists training. BMC Med. Educ. 24:293. doi: 10.1186/s12909-024-05282-9,
Shouqin, L., Zhaoxin, Z., and Xiubin, Z. (2022). A qualitative study exploring nursing students' perspectives on and attitudes towards hospice care in China nurse education today, 119. doi: 10.1016/j.nedt.2022.105384
Song, LJ. (2021). Death education and curriculum development for undergraduate medical students [PhD dissertation]. Naval medical university, people's liberation Army of China. doi: 10.26998/d.cnki.gjuyu.2021.000081
Tang, L., Zhou, L. J., Li, Y. X., Zhang, L., Cui, J., Meng, X. L., et al. (2015). Construction and implementation of the death education curriculum. Chin. J. Nurs. 50, 223–229. doi: 10.3761/j.issn.0254-1769.2015.02.022
Wang, Y., Chen, Y., Wang, L., Wang, W., Kong, X., and Li, X. (2024). Assessment of the effectiveness of the BOPPPS model combined with case-based learning on nursing residency education for newly recruited nurses in China: a mixed methods study. BMC Med. Educ. 24:215. doi: 10.1186/s12909-024-05202-x,
Wang, W., Wu, C., Bai, D., Chen, H., Cai, M., Gao, J., et al. (2022). A meta-analysis of nursing students’ knowledge and attitude0.123s about end-of-life care. Nurse Educ Today. 119:105570. doi: 10.1016/j.nedt.2022.105570
Wang, M., Zhang, M., Liu, C.F., Luo, X., Qu, J.M., and He, X.F. (2023). Case scenario simulation based on BOPPPS model in first aid training for nurses J. Nurs., 38, 77–79, 83. doi: 10.3870/j.issn.1001-4152.2023.11.077
Xu, M. Y., and Ji, Y. H. (2023). Application of mixed teaching model based on BOPPPS in health education training of residency nurses in general surgery. Health Vocat. Educ. 41, 94–96. doi: 10.20037/j.issn.1671-1246.2023.14.30
Yang, H., Lu, Y. H., Zhao, Y. Y., Gu, Y. H., and Zhang, L. Y. (2016). Cross-cultural adaptation of the Chinese version of the end-of-life care attitude scale. J. Nurs. 23, 50–53. doi: 10.16460/j.issn1008-9969.2016.05.050
Yoong, S. Q., Schmidt, L. T., Devi, K. M., and Zhang, H. (2023). Using palliative and end-of-life simulation to enhance pre-licensure nursing students’ emotional intelligence, palliative care knowledge and reflective abilities: A single group, pretest-posttest study. Nurse education today 130:105923. doi: 10.1016/j.nedt.2023.105923
Yu, H., Sun, C., Xie, L., Wang, L., Song, J., Zhu, Y., et al. (2022). Using a mediating model of death attitude and meaning in life to understand nursing students attitude about hospice care. Nurse Educ. Today 116:105448. doi: 10.1016/j.nedt.2022.105448,
Zahran, Z., Hamdan, K. M., Hamdan-Mansour, A. M., Allari, R. S., Alzayyat, A. A., and Shaheen, A. M. (2022). Nursing students' attitudes towards death and caring for dying patients. Nurs. Open 9, 614–623. doi: 10.1002/nop2.1107
Zhang, J., Fu, Y., Zhang, H., Tang, T., Yin, M., and Shi, L. (2022). Analysis of factors influencing the attitudes towards the elderly of nursing students based on empathy and end-of-life care: a cross-sectional study. Nurs. Open 9, 2348–2355. doi: 10.1002/nop2.1245,
Keywords: BOPPPS teaching model, education, end-of-life care, nursing students, China
Citation: Xu QZ, Chen J, Xu Q, Zhang J and Yang Y (2025) Efficacy of the BOPPPS teaching model in enhancing end-of-life care education and attitudinal outcomes among Chinese nursing students. Front. Educ. 10:1548835. doi: 10.3389/feduc.2025.1548835
Edited by:
Yuke Tien Fong, Singapore General Hospital, SingaporeReviewed by:
Eila Burns, JAMK University of Applied Sciences, FinlandVlatka Sotošek, University of Rijeka, Croatia
Copyright © 2025 Xu, Chen, Xu, Zhang and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiu Zhu Xu, MTIzODQ1ODlAcXEuY29t
†ORCID: Qiu Zhu Xu, https://orcid.org/0009-0006-2933-2190
 Qiu Zhu Xu
Qiu Zhu Xu Junxi Chen3
Junxi Chen3 Jiali Zhang
Jiali Zhang Yingzi Yang
Yingzi Yang